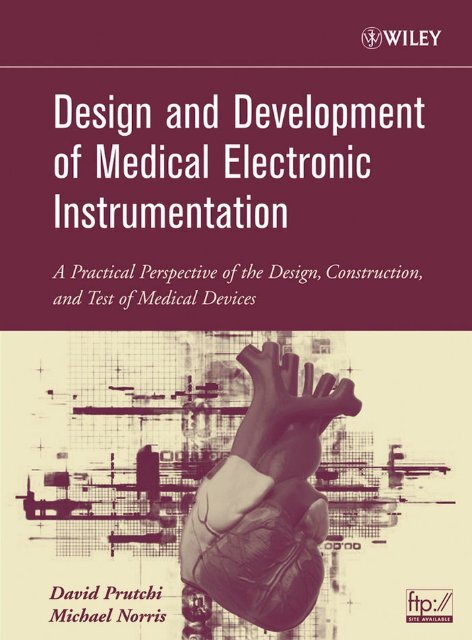
DESIGN AND DEVELOPMENT OF MEDICAL ELECTRONIC ...
DESIGN AND DEVELOPMENT OF MEDICAL ELECTRONIC ...
DESIGN AND DEVELOPMENT OF MEDICAL ELECTRONIC ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>DESIGN</strong> <strong>AND</strong> <strong>DEVELOPMENT</strong><strong>OF</strong> <strong>MEDICAL</strong> <strong>ELECTRONIC</strong>INSTRUMENTATION
<strong>DESIGN</strong> <strong>AND</strong> <strong>DEVELOPMENT</strong><strong>OF</strong> <strong>MEDICAL</strong> <strong>ELECTRONIC</strong>INSTRUMENTATIONA Practical Perspective of the Design, Construction,and Test of Medical DevicesDAVID PRUTCHIMICHAEL NORRIS
Copyright © 2005 by John Wiley & Sons, Inc. All rights reserved.Published by John Wiley & Sons, Inc., Hoboken, New Jersey.Published simultaneously in Canada.No part of this publication may be reproduced, stored in a retrieval system, or transmitted in any form or byany means, electronic, mechanical, photocopying, recording, scanning, or otherwise, except as permittedunder Section 107 or 108 of the 1976 United States Copyright Act, without either the prior writtenpermission of the Publisher, or authorization through payment of the appropriate per-copy fee to theCopyright Clearance Center, Inc., 222 Rosewood Drive, Danvers, MA 01923, 978-750-8400, fax 978-646-8600, or on the web at www.copyright.com. Requests to the Publisher for permission should be addressedto the Permissions Department, John Wiley & Sons, Inc., 111 River Street, Hoboken, NJ 07030, (201) 748-6011, fax (201) 748-6008.Limit of Liability/Disclaimer of Warranty: While the publisher and author have used their best efforts inpreparing this book, they make no representations or warranties with respect to the accuracy orcompleteness of the contents of this book and specifically disclaim any implied warranties ofmerchantability or fitness for a particular purpose. No warranty may be created or extended by salesrepresentatives or written sales materials. The advice and strategies contained herein may not be suitablefor your situation. You should consult with a professional where appropriate. Neither the publisher norauthor shall be liable for any loss of profit or any other commercial damages, including but not limited tospecial, incidental, consequential, or other damages.For general information on our other products and services please contact our Customer Care Departmentwithin the U.S. at 877-762-2974, outside the U.S. at 317-572-3993 or fax 317-572-4002.Wiley also publishes its books in a variety of electronic formats. Some content that appears in print, however,may not be available in electronic format.Library of Congress Cataloging-in-Publication Data:Prutchi, David.Design and development of medical electronic instrumentation: a practical perspective ofthe design, construction, and test of material devices / David Prutchi, Michael Norris.p. cm.Includes bibliographical references and index.ISBN 0-471-67623-3 (cloth)1. Medical instruments and apparatus–Design and construction. I. Norris, Michael. II.Title.R856.P78 2004681’.761–dc222004040853Printed in the United States of America10 9 8 7 6 5 4 3 2 1
In memory of Prof. Mircea Arcan,who was a caring teacher, a true friend,and a most compassionate human being.—David
CONTENTSPREFACEDISCLAIMERABOUT THE AUTHORSixxiiixv1 BIOPOTENTIAL AMPLIFIERS 12 B<strong>AND</strong>PASS SELECTION FOR BIOPOTENTIAL AMPLIFIERS 413 <strong>DESIGN</strong> <strong>OF</strong> SAFE <strong>MEDICAL</strong> DEVICE PROTOTYPES 974 ELECTROMAGNETIC COMPATIBILITY <strong>AND</strong><strong>MEDICAL</strong> DEVICES 1475 SIGNAL CONDITIONING, DATA ACQUISITION,<strong>AND</strong> SPECTRAL ANALYSIS 2056 SIGNAL SOURCES FOR SIMULATION, TESTING,<strong>AND</strong> CALIBRATION 2497 STIMULATION <strong>OF</strong> EXCITABLE TISSUES 3058 CARDIAC PACING <strong>AND</strong> DEFIBRILLATION 369EPILOGUE 441APPENDIX A: SOURCES FOR MATERIALS <strong>AND</strong> COMPONENTS 447APPENDIX B: ACCOMPANYING CD-ROM CONTENT 451INDEX 457vii
PREFACEThe medical devices industry is booming. Growth in the industry has not stopped despiteglobally fluctuating economies. The main reason for this success is probably the self-sustainingnature of health care. In essence, the same technology that makes it possible forpeople to live longer engenders the need for more health-care technologies to enhance thequality of an extended lifetime. It comes as no surprise, then, that the demand for trainedmedical-device designers has increased tremendously over the past few years. Unfortunately,college courses and textbooks most often provide only a cursory view of the technologybehind medical instrumentation. This book supplements the existing literature byproviding background and examples of how medical instrumentation is actually designedand tested. Rather than delve into deep theoretical considerations, the book will walk youthrough the various practical aspects of implementing medical devices.The projects presented in the book are truly unique. College-level books in the field ofbiomedical instrumentation present block-diagram views of equipment, and high-levelhobby books restrict their scope to science-fair projects. In contrast, this book will helpyou discover the challenge and secrets of building practical electronic medical devices,giving you basic, tested blocks for the design and development of new instrumentation.The projects range from simple biopotential amplifiers all the way to a computer-controlleddefibrillator. The circuits actually work, and the schematics are completely readable.The project descriptions are targeted to an audience that has an understanding ofcircuit design as well as experience in electronic prototype construction. You will understandall of the math if you are an electrical engineer who still remembers Laplace transforms,electromagnetic fields, and programming. However, the tested modular circuits andsoftware are easy to combine into practical instrumentation even if you look at them as“black boxes” without digging into their theoretical basis. We will also assume that youhave basic knowledge of physiology, especially how electrically excitable cells work, aswell as how the aggregate activities of many excitable cells result in the various biopotentialsignals that can be detected from the body. For a primer (or a refresher), we recommendreading Chapters 6 and 7 of Intermediate Physics for Medicine and Biology, 3rd ed.,by Russell K. Hobbie (1997).Whether you are a student, hobbyist, or practicing engineer, this book will show youhow easy it is to get involved in the booming biomedical industry by building sophisticatedinstruments at a small fraction of the comparable commercial cost.ix
xPREFACEThe book addresses the practical aspects of amplifying, processing, simulating, andevoking these biopotentials. In addition, in two chapters we address the issue of safety inthe development of electronic medical devices, bypassing the difficult math and providinglots of insider advice.In Chapter 1 we present the development of amplifiers designed specifically for thedetection of biopotential signals. A refresher on op-amp-based amplifiers is presented in thecontext of the amplification of biopotentials. Projects for this chapter include chloriding silverelectrodes, high-impedance electrode buffer array, pasteless bioelectrode, single-endedelectrocardiographic (ECG) amplifier array, body potential driver, differential biopotentialamplifier, instrumentation-amplifier biopotential amplifier, and switched-capacitor surfacearray electromyographic amplifier.In Chapter 2 we look at the frequency content of various biopotential signals and discussthe need for filtering and the basics of selecting and designing RC filters, active filters, notchfilters, and specialized filters for biopotential signals. Projects include a dc-coupled biopotentialamplifier with automatic offset cancellation, biopotential amplifier with dc rejection,ac-coupled biopotential amplifier front end, bootstrapped ac-coupled biopotential amplifier,biopotential amplifier with selectable RC bandpass filters, state-variable filter with tunablecutoff frequency, twin-T notch filter, gyrator notch filter, universal harmonic eliminatornotch comb filter, basic switched-capacitor filters, slew-rate limiter, ECG amplifier withpacemaker spike detection, “scratch and rumble” filter for ECG, and an intracardiac electrogramevoked-potential amplifier.In Chapter 3 we introduce safety considerations in the design of medical device prototypes.We include a survey of applicable standards and a discussion on mitigating the dangersof electrical shock. We also look at the way in which equipment should be tested forcompliance with safety standards. Projects include the design of an isolated biopotentialamplifier, transformer-coupled analog isolator module, carrier-based optically coupled analogisolator, linear optically coupled analog isolator with compensation, isolated eight-channel12-bit analog-to-digital converter, isolated analog-signal multiplexer, ground bondintegrity tester, microammeter for safety testing, and basic high-potential tester.In Chapter 4 we discuss international regulations regarding electromagnetic compatibilityand medical devices. This includes mechanisms of emission of and immunity againstradiated and conducted electromagnetic disturbances as well as design practices for electromagneticcompatibility. Projects include a radio-frequency spectrum analyzer, near-fieldH-field and E-field probes, comb generator, conducted emissions probe, line impedance stabilizationnetwork, electrostatic discharge simulators, conducted-disturbance generator,magnetic field generator, and wideband transmitter for susceptibility testing.In Chapter 5 we present the new breed of “smart” sensors that can be used to detectphysiological signals with minimal design effort. We discuss analog-to-digital conversionof physiological signals as well as methods for high-resolution spectral analysis. Projectsinclude a universal sensor interface, sensor signal conditioners, using the PC sound card asa data acquisition card, voltage-controlled oscillator for dc-correct signal acquisitionthrough a sound card, as well as fast Fourier transform and high-resolution spectral estimationsoftware.In Chapter 6 we discuss the need for artificial signal sources in medical equipmentdesign and testing. The chapter covers the basics of digital signal synthesis, arbitrary signalgeneration, and volume conductor experiments. Projects include a general-purpose signalgenerator, direct-digital-synthesis sine generator, two-channel digital arbitrary waveformgenerator, multichannel analog arbitrary signal source, cardiac simulator for pacemakertesting, and how to perform volume-conductor experiments with a voltage-to-current converterand physical models of the body.In Chapter 7 we look at the principles and clinical applications of electrical stimulationof excitable tissues. Projects include the design of stimulation circuits for implantable
PREFACExipulse generators, fabrication of implantable stimulation electrodes, external neuromuscularstimulator, TENS device for pain relief, and transcutaneous/transcranial pulsed-magneticneural stimulator.In Chapter 8 we discuss the principles of cardiac pacing and defibrillation, providing abasic review of the electrophysiology of the heart, especially its conduction deficienciesand arrhythmias. Projects include a demonstration implantable pacemaker, external cardiacpacemaker, impedance plethysmograph, intracardiac impedance sensor, externaldefibrillator, intracardiac defibrillation shock box, and cardiac fibrillator.The Epilogue is an engineer’s perspective on bringing a medical device to market. Theregulatory path, Food and Drug Administration (FDA) classification of medical devices,and process of submitting applications to the FDA are discussed and we look at the valueof patents and how to recruit venture capital.Finally, in Appendix A we provide addresses, Web sites, telephone numbers, and faxnumbers for suppliers of components used in the projects described in the book. The contentsof the book’s ftp site, which contains software and information used for many ofthese projects, is given in Appendix B.DAVID PRUTCHIMICHAEL NORRIS
DISCLAIMERThe projects in this book are presented solely as examples of engineering building blocksused in the design of experimental electromedical devices. The construction of any and allexperimental systems must be supervised by an engineer experienced and skilled withrespect to such subject matter and materials, who will assume full responsibility for thesafe and ethical use of such systems.The authors do not suggest that the circuits and software presented herein can orshould be used by the reader or anyone else to acquire or process signals from, or stimulatethe living tissues of, human subjects or experimental animals. Neither do theauthors suggest that they can or should be used in place of or as an adjunct to professionalmedical treatment or advice. Sole responsibility for the use of these circuitsand/or software or of systems incorporating these circuits and/or software lies with thereader, who must apply for any and all approvals and certifications that the law mayrequire for their use. Furthermore, safe operation of these circuits requires the use of isolatedpower supplies, and connection to external signal acquisition/processing/monitoringequipment should be done only through signal isolators with the proper isolationratings.The authors and publisher do not make any representations as to the completeness oraccuracy of the information contained herein, and disclaim any liability for damage orinjuries, whether caused by or arising from a lack of completeness, inaccuracy of information,misinterpretation of directions, misapplication of circuits and information, or otherwise.The authors and publisher expressly disclaim any implied warranties ofmerchantability and of fitness of use for any particular purpose, even if a particularpurpose is indicated in the book.References to manufacturers’ products made in this book do not constitute anendorsement of these products but are included for the purpose of illustration and clarification.It is not the authors’ intent that any technical information and interface datapresented in this book supersede information provided by individual manufacturers. Inthe same way, various government and industry standards cited in the book are includedsolely for the purpose of reference and should not be used as a basis for design ortesting.Since some of the equipment and circuitry described in this book may relate to or becovered by U.S. or other patents, the authors disclaim any liability for the infringement ofxiii
xivDISCLAIMERsuch patents by the making, using, or selling of such equipment or circuitry, and suggestthat anyone interested in such projects seek proper legal counsel.Finally, the authors and publisher are not responsible to the reader or third parties for anyclaim of special or consequential damages, in accordance with the foregoing disclaimer.
ABOUT THE AUTHORSDavid Prutchi is Vice President of Engineering at Impulse Dynamics, where he is responsiblefor the development of implantable devices intended to treat congestive heart failure,obesity, and diabetes. His prior experience includes the development of Sulzer-Intermedics’ next-generation cardiac pacemaker, as well as a number of other industrialand academic positions conducting biomedical R&D and developing medical electronicinstrumentation. David Prutchi holds a Ph.D. in biomedical engineering from Tel-AvivUniversity and conducted postdoctoral research at Washington University, where he taughta graduate course in neuroelectric systems. Dr. Prutchi has over 40 technical publicationsand in excess of 60 patents in the field of active implantable medical devices.Michael Norris is a Senior Electronics Engineer at Impulse Dynamics, where he has developedmany cardiac stimulation devices, cardiac contractility sensors, and physiological signalacquisition systems. His 25 years of experience in electronics include the developmentof cardiac stimulation prototype devices at Sulzer-Intermedics as well as the design, construction,and deployment of telemetric power monitoring systems at Nabla Inc. in Houston,and instrumentation and controls at General Electric. Michael Norris has authored varioustechnical publications and holds patents related to medical instrumentation.xv
1BIOPOTENTIAL AMPLIFIERSIn general, signals resulting from physiological activity have very small amplitudes andmust therefore be amplified before their processing and display can be accomplished. Thespecifications and lists of characteristics of biopotential amplifiers can be as long and confusingas those for any other amplifier. However, for most typical medical applications, themost relevant amplifier characterizing parameters are the seven described below.1. Gain. The signals resulting from electrophysiological activity usually have amplitudes onthe order of a few microvolts to a few millivolts. The voltage of such signals must be amplifiedto levels suitable for driving display and recording equipment. Thus, most biopotentialamplifiers must have gains of 1000 or greater. Most often the gain of an amplifier is measuredin decibels (dB). Linear gain can be translated into its decibel form through the use ofGain(dB) 20 log 10 (linear gain)2. Frequency response. The frequency bandwidth of a biopotential amplifier should besuch as to amplify, without attenuation, all frequencies present in the electrophysiologicalsignal of interest. The bandwidth of any amplifier, as shown in Figure 1.1, is the differencebetween the upper cutoff frequency f 2 and the lower cutoff frequency f 1 . The gain at thesecutoff frequencies is 0.707 of the gain in the midfrequency plateau. If the percentile gainis normalized to that of the midfrequency gain, the gain at the cutoff frequencies hasdecreased to 70.7%. The cutoff points are also referred to as the half-power points, due tothe fact that at 70.7% of the signal the power will be (0.707) 2 0.5. These are also knownas the 3-dB points, since the gain at the cutoff points is lower by 3 dB than the gain inthe midfrequency plateau: 3dB 20 log 10 (0.707).3. Common-mode rejection. The human body is a good conductor and thus will act asan antenna to pick up electromagnetic radiation present in the environment. As shown inFigure 1.2, one common type of electromagnetic radiation is the 50/60-Hz wave and itsharmonics coming from the power line and radiated by power cords. In addition, otherspectral components are added by fluorescent lighting, electrical machinery, computers,Design and Development of Medical Electronic Instrumentation By David Prutchi and Michael NorrisISBN 0-471-67623-3 Copyright © 2005 John Wiley & Sons, Inc.1
2 BIOPOTENTIAL AMPLIFIERSGainG70.7%G0f1 f 2Figure 1.1 Frequency response of a biopotential amplifier.Frequency(Hz)Power LinesBiopot entialAmplifierFigure 1.2EarthCoupling of power line interference to a biopotential recording setup.and so on. The resulting interference on a single-ended bioelectrode is so large that it oftenobscures the underlying electrophysiological signals.The common-mode rejection ratio (CMRR) of a biopotential amplifier is measurementof its capability to reject common-mode signals (e.g., power line interference), and it isdefined as the ratio between the amplitude of the common-mode signal to the amplitude ofan equivalent differential signal (the biopotential signal under investigation) that wouldproduce the same output from the amplifier. Common-mode rejection is often expressed indecibels according to the relationshipCommon-mode rejection (CMR) (dB) 20 log 10 CMRR
BIOPOTENTIAL AMPLIFIERS 34. Noise and drift. Noise and drift are additional unwanted signals that contaminate abiopotential signal under measurement. Both noise and drift are generated within theamplifier circuitry. The former generally refers to undesirable signals with spectralcomponents above 0.1 Hz, while the latter generally refers to slow changes in the baselineat frequencies below 0.1 Hz.The noise produced within amplifier circuitry is usually measured either in microvoltspeak to peak (µV p-p ) or microvolts root mean square (RMS) (µV RMS ), and applies as if itwere a differential input voltage. Drift is usually measured, as noise is measured, in microvoltsand again, applies as if it were a differential input voltage. Because of its intrinsic lowfrequencycharacter, drift is most often described as peak-to-peak variation of the baseline.5. Recovery. Certain conditions, such as high offset voltages at the electrodes caused bymovement, stimulation currents, defibrillation pulses, and so on, cause transient interruptionsof operation in a biopotential amplifier. This is due to saturation of the amplifiercaused by high-amplitude input transient signals. The amplifier remains in saturation for afinite period of time and then drifts back to the original baseline. The time required for thereturn of normal operational conditions of the biopotential amplifier after the end of thesaturating stimulus is known as recovery time.6. Input impedance. The input impedance of a biopotential amplifier must besufficiently high so as not to attenuate considerably the electrophysiological signal undermeasurement. Figure 1.3a presents the general case for the recording of biopotentials.Each electrode–tissue interface has a finite impedance that depends on many factors, suchas the type of interface layer (e.g., fat, prepared or unprepared skin), area of electrode surface,or temperature of the electrolyte interface.In Figure 1.3b, the electrode–tissue has been replaced by an equivalent resistance network.This is an oversimplification, especially because the electrode–tissue interface is notmerely a resistive impedance but has very important reactive components. A more correctrepresentation of the situation is presented in Figure 1.3c, where the final signal recorded asthe output of a biopotential amplifier is the result of a series of transformations among theparameters of voltage, impedance, and current at each stage of the signal transfer. As shownin the figure, the electrophysiological activity is a current source that causes current flow i ein the extracellular fluid and other conductive paths through the tissue. As these extracellularcurrents act against the small but nonzero resistance of the extracellular fluids R e , theyproduce a potential V e , which in turn induces a small current flow i in in the circuit made upof the reactive impedance of the electrode surface X Ce and the mostly resistive impedanceof the amplifier Z in . After amplification in the first stage, the currents from each of the bipolarcontacts produce voltage drops across input resistors R in in the summing amplifier,where their difference is computed and amplified to finally produce an output voltage V out .The skin between the potential source and the electrode can be modeled as a seriesimpedance, split between the outer (epidermis) and the inner (dermis) layers. The outerlayer of the epidermis—the stratum corneum—consists primarily of dead, dried-up cellswhich have a high resistance and capacitance. For a 1-cm 2 area, the impedance of the stratumcorneum varies from 200 kΩ at 1 Hz down to 200 Ω at 1 MHz. Mechanical abrasionwill reduce skin resistance to between 1 and 10 kΩ at 1 Hz.7. Electrode polarization. Electrodes are usually made of metal and are in contact withan electrolyte, which may be electrode paste or simply perspiration under the electrode.Ion–electron exchange occurs between the electrode and the electrolyte, which results involtage known as the half-cell potential. The front end of a biopotential amplifier must beable to deal with extremely weak signals in the presence of such dc polarization components.These dc potentials must be considered in the selection of a biopotential amplifier gain, sincethey can saturate the amplifier, preventing the detection of low-level ac components.International standards regulating the specific performance of biopotential recording systems
4 BIOPOTENTIAL AMPLIFIERSVolumeConductor(Tissue)CurrentfromSourcesVinRinOutputBiopotentialSourceCurrenttoSourcesElectrodeElectrode-TissueInterfaceBiopotentialAmplifier(a)RinterfaceiinBiopotentialSourceVinRinOutputRinterfaceTissue(b)TissueXceiinXinBiopotentialSourceRinReVeElectrodeTissueInterfaceVinXinRinOutputVoutFigure 1.3Xce(c)BiopotentialAmplifier(a) Simplified view of the recording of biopotentials; (b) equivalent circuit; (c) generalized equivalent circuit.
LOW-POLARIZATION SURFACE ELECTRODES 5usually specify the electrode offsets that are commonly present for the application coveredby the standard. For example, the standards issued by the Association for the Advancementof Medical Instrumentation (AAMI) specify that electrocardiography (ECG) amplifiers musttolerate a dc component of up to 300 mV resulting from electrode–skin contact.Commercial ECG electrodes have electrode offsets that are usually low enough, ensuringlittle danger of exceeding the maximum allowable dc input offset specifications of thestandards. However, the design of a biopotential amplifier must consider that there aretimes when the dc offset may be much larger. For example, neonatal ECG monitoringapplications often use sets of stainless-steel needle electrodes, whose offsets are muchhigher than those of commercial self-adhesive surface ECG electrodes. In addition, manyphysicians still prefer to use nondisposable suction cup electrodes (which have a rubbersqueeze bulb attached to a silver-plated brass hemispherical cup). After the silver platingwears off, these brass cup electrodes can introduce very large offsets.LOW-POLARIZATION SURFACE ELECTRODESSilver (Ag) is a good choice for metallic skin-surface electrodes because silver forms aslightly soluble salt, silver chloride (AgCl), which quickly saturates and comes to equilibrium.A cup-shaped electrode provides enough volume to contain an electrolyte, includingchlorine ions. In these electrodes, the skin never touches the electrode material directly.Rather, the interface is through an ionic solution.One simple method to fabricate Ag/AgCl electrodes is to use electrolysis to chloride asilver base electrode (e.g., a small silver disk or silver wire). The silver substrate isimmersed in a chlorine-ion-rich solution, and electrolysis is performed using a common 9-V battery connected via a series 10-kΩ potentiometer and a milliammeter. The positive terminalof the battery should be connected to the silver metal, and a plate of platinum or silvershould be connected to the negative terminal and used as the opposite electrode in the solution.Our favorite electrolyte is prepared by mixing 1 part distilled water (the supermarketkind is okay), 1/2 part HCl 25%, and FeCl 3 at a rate of 0.5 g per milliliter of water.If you want to make your own electrodes, use refined silver metal (99.9 to 99.99% Ag)to make the base electrode. Before chloriding, degrease and clean the silver using a concentratedaqueous ammonia solution (10 to 25%). Leave the electrodes immersed in thecleaning solution for several hours until all traces of tarnish are gone. Rinse thoroughlywith deionized water (supermarket distilled water is okay) and blot-dry with clean filterpaper. Don’t touch the electrode surface with bare hands after cleaning. Suspend the electrodesin a suitably sized glass container so that they don’t touch the sides or bottom. Pourthe electrolyte into the container until the electrodes are covered, but be careful not toimmerse the solder connections or leads that you will use to hook up to the electrode.When the silver metal is immersed, the silver oxidation reaction with concomitant silverchloride precipitation occurs and the current jumps to its maximal value. As the thicknessof the AgCl layer deposited increases, the reaction rate decreases and the currentdrops. This process continues, and the current approaches zero. Adjust the potentiometerto get an initial current density of about 2.5 mA/cm 2 , making sure that no hydrogen bubblesevolve at the return electrode (large platinum or silver plate). You should remove theelectrode from the solution once the current density drops to about 10 µA/cm 2 . Coatingshould take no more than 15 to 20 minutes. Once done, remove the electrodes and rinsethem thoroughly but carefully under running (tap) water.An alternative to the electrolysis method is to immerse the silver electrode in a strong bleachsolution. Yet another way of making a Ag/AgCl electrode is to coat by dipping the silver metalin molten silver chloride. To do so, heat AgCl in a small ceramic crucible with a gas flame untilit melts to a dark brown liquid, then simply dip the electrode in the molten silver chloride.
6 BIOPOTENTIAL AMPLIFIERSWarning! The materials used to form Ag/AgCl electrodes are relatively dangerous.Do not breathe dust or mist and do not get in eyes, on skin, or on clothing. When workingwith these materials, safety goggles must be worn. Contact lenses are not protectivedevices. Appropriate eye and face protection must be worn instead of, or in conjunctionwith, contact lenses. Wear disposable protective clothing to prevent exposure. Protectiveclothing includes lab coat and apron, flame- and chemical-resistant coveralls, gloves, andboots to prevent skin contact. Follow good hygiene and housekeeping practices whenworking with these materials. Do not eat, drink, or smoke while working with them.Wash hands before eating, drinking, smoking, or applying cosmetics.If you don’t want to fabricate your own electrodes, you can buy all sorts of very stableAg/AgCl electrodes from In Vivo Metric. They make them using a very fine grained homogeneousmixture of silver and silver chloride powder, which is then compressed and sinteredinto various configurations. Alternatively, Ag/AgCl electrodes are cheap enough thatyou may get a few pregelled disposable electrodes free just by asking at the nurse’s stationin the emergency department or cardiology service of your local hospital.Recording gel is available at medical supply stores (also from In Vivo Metric). However,if you really want a home brew, heat some sodium alginate (pure seaweed, commonly usedto thicken food) and water with low-sodium salt (e.g., Morton Lite Salt) into a thick soupthat when cooled can be applied between the electrodes and skin. Note that there is no guaranteethat this concoction will be hypoallergenic! A milder paste can be made by dissolving0.9 g of pure NaCl in 100 mL of deionized water. Add 2 g of pharmaceutical-gradeKaraya gum and agitate in a magnetic stirrer for 2 hours. Add 0.09 g of methyl paraben and0.045 g of propyl paraben as preservatives and keep in a clean capped container.SINGLE-ENDED BIOPOTENTIAL AMPLIFIERSMost biopotential amplifiers are operational-amplifier-based circuits. As a refresher, thevoltage present at the output of the operational amplifier is proportional to the differentialvoltage across its inputs. Thus, the noninverting input produces an in-phase output signal,while the inverting input produces an output signal that is 180 out of phase with the input.In the circuit of Figure 1.4, an input signal V in is presented through resistor R in to theinverting input of an ideal operational amplifier. Resistor R f provides feedback from theamplifier’s output to its inverting input. The noninverting input is grounded, and due to thefact that in an ideal op-amp the setting conditions at one input will effectively set the sameconditions at the other input, point A can be treated as it were also grounded. The powerconnections have been deleted for the sake of simplicity.Ideal op-amps have an infinite input impedance, which implies that the input currenti in is zero. The inverting input will neither sink nor source any current. According toKirchhoff’s current law, the total current at junction A must sum to zero. Hence, i in i fBut by Ohm’s law, the currents are defined byandini in V Rinouti f V Rf
SINGLE-ENDED BIOPOTENTIAL AMPLIFIERS 7IfRfIinRinA-+-VCCVin+VCCVoutFigure 1.4Inverting voltage amplifier.Therefore, by substitution and by solving for V out ,This equation can be rewritten asf VinV out R RinV out GV inwhere G represents the voltage gain constant R f /R in .The circuit presented in Figure 1.5 is a noninverting voltage amplifier, also known as anoninverting follower, which can be analyzed in a similar manner. The setting of the noninvertinginput at input voltage V in will force the same potential at point A. Thus,i in V Randi f V out V inRfBut in the noninverting amplifier i in i out , so by replacing and solving for V out , we obtainV out 1 RfR V inThe voltage gain in this case isinininRfG 1 RA special case of this configuration is shown in Figure 1.6. Here R f 0, and R in is unnecessary,which leads to a resistance ratio R f /R in 0, which in turn results in unity gain.This configuration, termed a unity-gain buffer or voltage follower, is often used in biomedicalinstrumentation to couple a high-impedance signal source, through the (almost)infinite input impedance of the op-amp, to a low-impedance processing circuit connectedto the very low impedance output of the op-amp.in
8 BIOPOTENTIAL AMPLIFIERSIfRf-VccRinIinA-++VccVoutVinFigure 1.5Noninverting op-amp voltage amplifier; also known as a noninverting follower.-VCC-+Vin+VCCVoutFigure 1.6 A unity-gain buffer is a special case of the noninverting voltage amplifier in which theresistance ratio is R f /R in 0, which translates into unity gain. This configuration is often used in biomedicalinstrumentation to buffer a high-impedance signal source.ULTRAHIGH-IMPEDANCE ELECTRODE BUFFER ARRAYSA group of ultrahigh-impedance, low-power, low-noise op-amp voltage followers is commonlyused as a buffer for signals collected from biopotential electrode arrays. Thesecircuits are usually placed in close proximity to the subject or preparation to avoid contaminationand degradation of biopotential signals. The circuit of Figure 1.7 comprises 32 unity-gain
ULTRAHIGH-IMPEDANCE ELECTRODE BUFFER ARRAYS 9+VIN-1IN-2GuardRingGuardRing45+6-11-V43+2-11ICxB7TLC27L4ICxA1TLC27L4OUT-1OUT-2J1-1J1-2J1-3J1-4J1-5J1-6J1-7J1-8J1-9J1-10J1-11J1-12J1-13J1-14J1-15J1-16In1In2In3In4In1In2In3In4In1In2In3In4In1In2In3In4IC1IC2IC3IC4Out1Out2Out3Out4Out1Out2Out3Out4Out1Out2Out3Out4Out1Out2Out3Out4J2-34J2-1J2-33J2-2J2-32J2-3J2-31J2-4J2-30J2-5J2-29J2-6J2-29J2-7J2-27J2-8IN-3GuardRing412+13-11ICxD14TLC27L4OUT-3J1-17J1-18J1-19J1-20J1-21J1-22J1-23J1-24In1In2In3In4In1In2In3In4IC5IC6Out1Out2Out3Out4Out1Out2Out3Out4J2-26J2-9J2-25J2-10J2-24J2-11J2-23J2-12IN-4GuardRing410+9-11ICxC8TLC27L4OUT-4J1-25J1-26J1-27J1-28J1-29J1-30J1-31J1-32In1In2In3In4In1In2In3In4IC7IC8Out1Out2Out3Out4Out1Out2Out3Out4J2-22J2-13J2-21J2-14J2-20J2-15J2-19J2-16Figure 1.7 CMOS-input unity-gain buffers are often placed in close proximity to high-impedance electrodes to provide impedance conversion,making it possible to transmit the signal over relatively long distances without picking up noise, despite the fact that the contactimpedance of the electrodes may range into the thousands of megohms.buffers, which present an ultrahigh input impedance to an array of up to 32 electrodes. Eachbuffer in the array is implemented using a LinCMOS 1 precision op-amp operated as a unitygainvoltage follower. An output signal has the same amplitude as that of its correspondinginput. The output impedance is very low, however (in the few kilohm range) and can source orsink a maximum of 25 mA. As a result of this impedance transformation, the signal at thebuffer’s output can be transmitted over long distances without picking up noise, despite the factthat the contact impedance of the electrodes may range into the thousands of megohms. Powerfor the circuit must be symmetrical 3 to 9 V dc with real or virtual ground.In the circuit, input signals at J1 are buffered by eight TLC27L4 precision quad op-amp.The buffered output is available at J2. Despite its apparent simplicity, the circuit must be1 LinCMOS is a trademark of Texas Instruments Incorporated.
10 BIOPOTENTIAL AMPLIFIERSFigure 1.8 Printed circuit board for a high-input-impedance buffer array. The output of each channelis used to drive guard rings which form low-impedance isopotential barriers that shield all inputpaths from leakage currents.laid out and constructed with care to take advantage of the op-amp’s high input impedance.As shown in the PCB layout of Figure 1.8, the output of each channel is used to drive guardrings that form low-impedance isopotential barriers that shield all input paths from leakagecurrents.The selection of op-amps from the TLC27 family has the additional advantage thatelectrostatic display (ESD) protection circuits that may degrade high input impedance areunnecessary because LinCMOS chips have internal safeguards against high-voltage staticcharges. Applications requiring ultrahigh input impedances (on the order of 10 10 Ω) necessitateadditional precautions to minimize stray leakage. These precautions include maintainingall surfaces of the printed circuit board (PCB), connectors, and components free ofcontaminants, such as smoke particles, dust, and humidity. Residue-free electronic-gradeaerosols can be used effectively to dust off particles from surfaces. Humidity must beleached out from the relatively hygroscopic PCB material by drying the circuit board in alow-pressure oven at 40C for 24 hours and storing in sealed containers with dry silica gel.If even higher input impedances are required, approaching the maximal input impedanceof the TLC24L4, you may consider using Teflon 2 PCB material instead of the more commonglass–epoxy type.Typical applications for this circuit include active medallions, which are electrode connectorblocks mounted in close proximity to the subject or preparation. The low inputnoise (68 nV/ Hz) and high bandwidth (dc—10 kHz) make it suitable for a broad range ofapplications. For example, 32 standard Ag/AgCl electroencephalography (EEG) electrodesfor a brain activity mapper could be connected to such a medallion placed on a headcap.Figure 1.9 shows another application for the circuit as an active electrode array in electromyography(EMG). Here eight arrays were used to pick up muscle signals from 256points. Connectors J1 in each of the circuits were made of L-shaped gold-plated pins that areused as electrodes to form an array with a spatial sampling period of 2.54 mm (given by thepitch of a standard connector with 0.1-in. pin center to center). The outputs of the op-ampbuffers can then carry signals to the main biopotential signal amplifiers and signal processors2 Teflon is a trademark of the DuPont Corporation.
PASTELESS BIOPOTENTIAL ELECTRODES 11Figure 1.9 Eight high-input-impedance buffer arrays are used to detect muscle signals from 256points for a high-resolution large-array surface electromyography system. Arrays of gold-plated pinssoldered directly to array inputs are used as the electrodes.using a long flat cable. Power could be supplied either locally, using a single 9-V battery andtwo 10-kΩ resistors, to create a virtual ground, or directly from a remotely placed symmetricalisolated power supply.Low-impedance op-amp outputs are compatible with the inputs of most biopotentialamplifiers. Wires from J2 can be connected to the inputs of instrumentation just as normalelectrodes would. The isolated common post of the biopotential amplifiers should be connectedto the ground electrode on the subject or preparation as well as to the ground pointof the buffer array.PASTELESS BIOPOTENTIAL ELECTRODESOp-amp voltage followers are often used to buffer signals detected from biopotentialsources with intrinsically high input impedance. One such application is detecting biopotentialsignals through capacitive bioelectrodes. One area in which these electrodes are particularlyuseful is in the measurement and analysis of biopotentials in humans subjected toconditions similar to those existing during flight. Knowledge regarding physiological reactionsto flight maneuvers has resulted in the development of devices capable of predicting,detecting, and preventing certain conditions that might endanger the lives of crew members.For example, the detection of gravitationally induced loss of consciousness (loss of consciousnesscaused by extreme g-forces during sharp high-speed flight maneuvers in warplanes) may save many pilots and their aircraft by allowing an onboard computer to takeover the controls while the aviator regains consciousness [Whinnery et al., 1987]. G z -induced loss of consciousness (GLOC) detection is achieved through the analysis of variousbiosignals, the most important of which is the electroencephalogram (EEG).Another new application is the use of the electrocardiography (ECG) signal to synchronizethe inflation and deflation of pressure suits adaptively to gain an increase in thelevel of gravitational accelerations that an airman is capable of tolerating. Additional applications,such as the use of the processed electromyography (EMG) signal as a measure ofmuscle fatigue and pain as well as an analysis of eye blinks and eyeball movement throughthe detection of biopotentials around the eye as a measure of pilot alertness, constitute thepromise of added safety in air operations.One problem in making these techniques practical is that most electrodes used for thedetection of bioelectric signals require skin preparation to decrease the electrical impedance
12 BIOPOTENTIAL AMPLIFIERSof the skin–electrode interface. This preparation often involves shaving, scrubbing the skin,and applying an electrolyte paste: actions unacceptable as part of routine preflight procedures.In addition, the electrical interface characteristics deteriorate during long-term use ofthese electrodes as a result of skin reactions and electrolyte drying. Dry or pasteless electrodescan be used to get around the constraints of electrolyte–interface electrodes. Pastelesselectrodes incorporate a bare or dielectric-coated metal plate, in direct contact with the skin,to form a very high impedance interface. By using an integral high-input-impedanceamplifier, it is possible to record a signal through the capacitive or resistive interface.Figure 1.10 presents the constitutive elements of a capacitive pasteless bioelectrode. Init, a highly dielectric material is used to form a capacitive interface between the skin anda conductive plate electrode. Ideally, this dielectric layer has infinite leakage resistance, butin reality this resistance is finite and decreases as the dielectric deteriorates. Signalspresented to the buffer stage result from capacitive coupling of biopotentials to the networkformed by series resistor R1 and the input impedance Z in of the buffer amplifier. In addition,circuitry that is often used to protect the buffer stage from ESD further attenuatesavailable signals. Shielding is usually provided in the enclosure of a bioelectrode assemblyto protect it from interfering noise. The signal at the output of the buffer amplifier haslow impedance and can be relayed to remotely placed processing apparatus without attenuation.External power must be supplied for operation of the active buffer circuitry.A dielectric substance is used in capacitive biopotential electrodes to form a capacitorbetween the skin and the recording surface. Thin layers of aluminum anodization, pyrevarnish, silicon dioxide, and other dielectrics have been used in these electrodes. Forexample, 17.5-µm (0.7-mil) film is easily prepared by anodic treatment, resulting in electrodeplates that have a dc resistance greater than 1 GΩ and a capacitance of 5000 pF atFigure 1.10 Block diagram of a typical capacitive active bioelectrode. A highly dielectric materialis used to form a capacitive interface between the skin and a conductive plate electrode. Signals presentedto the buffer stage result from capacitive coupling of biopotentials to the network formed byseries resistor R1 and the input impedance Z in of the buffer amplifier. (Reprinted from Prutchi andSagi-Dolev [1993], with permission from the Aerospace Medical Association.)
PASTELESS BIOPOTENTIAL ELECTRODES 1330 Hz. Unfortunately, standard anodization breaks down in the presence of saline (e.g.,from sweat), making the electrodes unreliable for long-term use.A relatively new anodization process was used by Lisa Sagi-Dolev, the former head ofR&D at the Israeli Airforce Aeromedical Center, and one of us [Prutchi and Sagi-Dolev,1993] to manufacture pasteless EEG electrodes that could be embedded in flight helmets.The hard anodization Super coating process developed by the Sanford Process Corporation 3is formed on the surface of an aluminum part and penetrates in a uniform manner, makingit very stable and resistant. The main characteristics of this type of coating are hardness(strength types Rockwell 50c–70c), high resistance to erosion (exceeding military standardMIL-A-8625), high resistance to corrosion (complete stability after 1200 hours in a saltwaterchamber), stable dielectric properties at high voltages (up to 1500 V with a coating thicknessof 50 µm, and up to 4500 V with a coating thickness of 170 µm), and high uniformity.Hard anodization Super has been authorized as a coating for aluminum kitchen utensils,and it proves to be very stable even under high temperatures and the presence of corrosivesubstances used while cooking. The coating does not wear off with the use ofabrasive scrubbing pads and detergents. These properties indicate that no toxic substancesare released in the presence of heat, alkaline or acid solutions, and organic solvents. Thismakes its use safe as a material in direct contact with skin, and resistant to sweat, bodyoils, and erosion due to skin friction.Figure 1.11 is a circuit diagram of a prototype active pasteless bioelectrode. The biopotentialsource is coupled to buffer IC1A through resistor R1 and the capacitor formed bythe biological tissues, aluminum oxide dielectric, and aluminum electrode plate.Operational amplifier IC1A is configured as a unity-gain buffer and is used to transformthe extremely high impedance of the electrode interface into a low-impedance source thatcan carry the biopotential signal to processing equipment with low loss and free ofFlatCableAnodizedPlateDrivenShieldR110KC2J20.01uF 1-V1J1+VR2100R310K784+-IC1B56TL082C15pFIC1ATL08283+2-41C30.01uF1J3OutputShieldFigure 1.11 Schematic diagram of a capacitive active bioelectrode. Biopotentials are coupled to buffer IC1A through resistor R1 and thecapacitor formed by the biological tissues, aluminum oxide dielectric, and aluminum electrode plate. Operational amplifier IC1A is configuredas a unity-gain buffer. IC1B drives a shield that protects the input from current leakage and noise. Resistors R3 and R2 reduce the gain of theshield driver to just under unity to improve the stability of the guarding circuit. C1 limits the bandwidth of input signals buffered by IC1.3 Hard anodization Super is a process licensed by the Sanfor Process Corporation (United States) to ElgatAerospace Finishing Services (Israel) and is described in Elgat Technical Publication 100, Hard Anodizing:“Super’’ Design and Applications.
14 BIOPOTENTIAL AMPLIFIERScontamination. IC1B, also a unity-gain buffer, is fed by the input signal, and its outputdrives a shield that protects the input from leaks and noise. Resistors R3 and R2 reduce thegain of the shield driver to just under unity in order to improve the stability of the guardingcircuit. Capacitor C1 limits the bandwidth of input signals buffered by IC1A. The circuitis powered by a single supply of 4 V dc. Miniature power supply decouplingcapacitors are mounted in close proximity to the op-amp.IC1A and IC1B are each one-half of a TLC277 precision dual op-amp’s IC. Here again,the selection of op-amps from the TLC27 family has the additional advantage that ESDprotection circuits which may degrade high input impedance are unnecessary becauseLinCMOS chips have internal safeguards against high-voltage static charges. Note that thiscircuit shows no obvious path for op-amp dc bias current. This is true if we assume that allelements are ideal or close to ideal. However, the imperfections in the electrode anodization,as well as in the dielectric separations and circuit board, provide sufficient paths forthe very weak dc bias required by the TL082 op-amp.The circuit is constructed on a miniature PCB in which ground planes, driven shieldplanes, and rings have been etched. The circuit is placed on top of a 1-cm 2 plate of thinaluminum coated with hard anodization Super used as the bioelectrode. A grounded conductivefilm layer shields the encapsulated bioelectrode and flexible printed circuit ribboncable, which carries power for both the circuit and the signal output.Figure 1.12 presents a prototype bioelectrode array designed to record frontal EEG signalsmeasured differentially (between positions Fp1 and Fp2 of the International 10-20System), as required for an experimental GLOC detection system. One of the bioelectrodescontains the same circuitry as that described above. The second, in addition to thebuffer and shield drive circuits, also contains a high-accuracy monolithic instrumentationamplifier and filters. Such a configuration provides high-level filtered signals which maybe carried to remotely placed processing stages with minimal signal contamination fromnoisy electronics in the helmet and elsewhere in the cockpit.A miniaturized version of the circuit may be assembled on a single flexible printed circuit.Driven and ground shields, as well as the flat cables used to interconnect the electrodesand carry power and output lines, may be etched on the same printed circuit. Asshown in Figure 1.13, the thin assembly may then be encapsulated and embedded at theappropriate position within the inner padding of a flight helmet. Nonactive reference forthe instrumentation amplifier may be established by using conductive foam lining theheadphone cavities (approximating positions A1 and A2 of the International 10-20System) or as cushioning for the chin strap.Figure 1.12 Block diagram of a capacitive bioelectrode array with integrated amplification and filter circuits designed to record frontal EEGsignals. One of the bioelectrodes contains the same circuitry as Figure 1.11. The second also contains a high-accuracy monolithic instrumentationamplifier and filters. (Reprinted from Prutchi and Sagi-Dolev [1993], with permission from the Aerospace Medical Association.)
SINGLE-ENDED BIOPOTENTIAL AMPLIFIER ARRAYS 15Figure 1.13 A miniaturized version of the capacitive bioelectrode array may be assembled on asingle flexible printed circuit. This assembly can be encapsulated and embedded at the appropriateposition within the inner padding of a flight helmet for differential measurement of the EEG betweenpositions Fp1 and Fp2 of the International 10-20 System. Conductive foam is used to establish nonactivereference either at positions A1 and A2 or at the chin of the subject. (Reprinted from Prutchiand Sagi-Dolev [1993], with permission from the Aerospace Medical Association.)EEG and ECG signals recorded using the new pasteless bioelectrodes compare very wellto recordings obtained through standard Ag/AgCl electrodes. Figure 1.14 presents adigitized tracing of a single-lead ECG signal detected with a capacitive pasteless bioelectrodeas well as with a standard Ag/AgCl electrode. Figure 1.15 shows digitized EEG signalsrecorded from a frontal differential pair with a reference at A2 using a pastelessbiopotential electrode array and with standard Ag/AgCl electrodes.SINGLE-ENDED BIOPOTENTIAL AMPLIFIER ARRAYSSingle-ended op-amp amplifiers were in the past used as front-end stages for biopotentialamplifiers. As we will see later, the advent of low-cost integrated instrumentationamplifiers has virtually eliminated the need to design single-ended biopotential amplifiers,and as such, the use of single-ended biopotential amplifiers is not recommended. Despitethis, this section has strong educational value because it demonstrates the design principlesof using single-ended amplifiers, which are common in the stages that follow thebioamplifier’s front end. Figure 1.16 shows an array of 16 single-ended biopotentialamplifiers. A number of these circuits may be stacked up to form very large arrays, whichmade them common for applications such as body potential mapping electrocardiographyin the days when single op-amps were expensive.Each biopotential amplification channel features high-impedance ESD-protectedinputs, current limiting, and defibrillation protection. Individual shield drives are used toprotect each input lead from external noise. Each channel provides a fixed gain of 1000within a fixed (3-dB) bandpass of 0.2 to 100 Hz. The chief advantage of the singleendedconfiguration is its simplicity, but this comes at the cost of lacking high immunityto common-mode signals. Because of this, single-ended biopotential amplifiers areusually found in equipment that incorporates other ways of suppressing common-modesignals. In this circuit, an onboard adjustable 50/60-Hz notch filter is connected at theoutput of each channel. The schematic diagram of Figure 1.17 shows how each channel
16 BIOPOTENTIAL AMPLIFIERSFigure 1.14 Single-lead ECG recordings: (a) using an Ag/AgCl standard bioelectrode; (b) usingthe capacitive active bioelectrode. (Reprinted from Prutchi and Sagi-Dolev [1993], with permissionfrom the Aerospace Medical Association.)is built around one-half of two TL064 quad op-amps. Eight copies of this circuitconstitute the 16 identical biopotential amplification channels. Operation of a singlechannel is described in the following discussion.A biopotential signal detected by a bioelectrode is coupled to the noninverting inputs ofthe first-stage amplifier and the shield driver amplifier. The input impedance is givenmostly by the input impedance of the front-stage op-amps, yielding 100 MΩ paralleledwith 100 pF. R1 limits the current that can flow through the input lead, while diodes D1and D2 shunt to ground any signal that exceeds their zener voltage. This arrangement protectsthe inputs of the amplifiers from ESD and from the high voltages present during cardiacdefibrillation. Furthermore, it protects the subject from currents that may leak backfrom the amplifiers or associated circuitry.The shield driver is configured as a unity-gain buffer. The actual drive, however, determinedby R2 and R3, is set to 99% of the signal magnitude at the inner wire to stabilize
SINGLE-ENDED BIOPOTENTIAL AMPLIFIER ARRAYS 17Figure 1.15 EEG measured differentially between positions Fp1 and Fp2 showing eyeblink EMG artifacts:(a) using an Ag/AgCl standard bioelectrode; (b) using the capacitive active bioelectrode. (Reprintedfrom Prutchi and Sagi-Dolev [1993], with permission from the Aerospace Medical Association.)the driver circuit while reducing the effective input cable capacitance by two orders ofmagnitude. The first amplification stage has a gain determined byG 1 1 R 5 11R4C2 and R5 form a low-pass filter with a (3-dB) cutoff frequency of 160 Hz, which stabilizesthe amplifier’s operation. In addition, R1 and C1 (plus the capacitances of D1 andD2) also form a low-pass filter, which further prevents oscillatory behavior and rejectshigh-frequency noise.The amplified signal is high-pass filtered by C3 and R13, with a (3-dB) cutoff frequencyof 0.16 Hz, before being amplified by the second stage. The gain of this stage is set byG 2 1 R 8 101R7
18 BIOPOTENTIAL AMPLIFIERSFigure 1.16 Array of 16 single-ended biopotential amplifiers. A number of these circuits may bestacked up to form very large arrays, making them ideally suited for applications such as body potentialmapping electrocardiography.The last processing stage of each channel is an active notch filter, which can be tuned tothe power line frequency by adjusting R12. Supply voltage to this circuit must be symmetricaland within the range of 5 V (minimum) to 18 V (absolute maximum). Two9-V alkaline batteries can be used efficiently due to the circuit’s very low power consumption.Capacitors C9–C12 are used to decouple the power supply and filter noise fromthe op-amp power lines.To minimize electrical interference, the circuit should be built with a compact layout onan appropriate printed circuit board or small piece of stripboard. The construction of thecircuit is straightforward, but care must be taken to keep wiring as short and clean as possible.Leads to the bioelectrodes should be low-loss coaxial cables, whose shields are connectedto their respective shield drives at J1 (J1x-2 for left-side channels and J1y-1 forright-side channels). The circuit’s ground should be connected to the subject’s reference(patient ground) electrode. When connected to a test subject, the circuit must always bepowered from batteries or through a properly rated isolation power supply. The same isolationrequirements apply to the outputs of the amplifier channels.It is important to note that the performance of a complete system is determined primarilyby its input circuitry. Equivalent input noise is practically that of the first stage(approximately 10 µV p-p within the amplifier’s 3-dB bandwidth of 0.2 to 100 Hz).BODY POTENTIAL DRIVERSRejection of common-mode signals in the prior circuit example is limited to the singleendedperformance of the input-stage op-amp and the 50/60-Hz rejection of the notch filter.Often, however, environmental noise (e.g., power line interference) is so large that common-modepotentials eclipse the weak biopotentials that can be picked up through singleendedamplifiers. Notch filters do not necessarily remove interfering signals in a substantialmanner either. The first few harmonics of the power line constitute strong interfering signalsin the recording of biopotentials. The range of these signals, however, is by no meansconfined to 100 or 200 Hz. High-frequency interference originating from fluorescent andother high-efficiency lamps commonly occurs with a maximal spectral density of approximately1 kHz and with amplitudes of up to 50% of the 50/60-Hz harmonic.
1J2x-1Output X1J2x-21J2y-2Output Y1J2y-1+V-VShieldRx310KRx2100IC1BTL06474+-11Rx120KDx11N914Dx21N914Cx1220pF-VRx5100KCx30.1uFRx610KRx1310M4+-5656Rx410K32411+-Cx20.01uFIC1ATL0641Rx71K11Rx8100KCx40.01uFIC2BTL0647Cx50.1uFCx6.047uFRx9120KCx7.047uFRx10120KCx8.047uF23114-++VIC2ATL0641Rx118.2K213Rx1210KShieldRy310KRy2100Ry120KDy2 Cy1Dy110M1N914 1N914 220pFIC1CRy5TL0644+8-11109Ry410K12134+14-11100KCy20.01uFIC1DTL064Cy3 Ry6IC2C0.1uF 10KRy13Ry71K1094+8-11Ry8100KCy40.01uFTL064Cy50.1uFRy9 Ry10120K 120KCy6 Cy7 Cy8.047uF .047uF.047uF131211-+4IC2DTL064Ry118.2K14123Ry1210KFigure 1.17 Each channel of the single-ended biopotential amplifier array is built around one-half of two TL064 quad op-amps. Eightcopies of this circuit constitute the 16 identical biopotential amplification channels.Electrode XShield XElectrode YShield Y19
20 BIOPOTENTIAL AMPLIFIERSA way of improving the common-mode rejection problem is to use single-endedamplifiers concurrently with body potential driver (BPD) circuits to cancel out commonmodesignals. Power line and other contaminating common-mode signals are capacitivelycoupled to the body, causing current to flow through it and into ground. The body, actingas a resistor through which a current flows, causes a voltage difference between any twopoints on it. The goal of a BPD is to detect and eliminate this voltage, effectively reducingcommon-mode signals between biopotential detection electrodes in the vicinity of its senseelectrode.A BPD is implemented by detecting the common-mode potential in the area of interestand then feeding into the body a 180 version of the same signal. A feedback loop is thusestablished which cancels out the common-mode potential. Circuits that have feedback areinherently unstable, and oscillatory behavior must be prevented to make a BPD useful.This, however, limits the BPD to a range well under its first resonance. The performanceof the circuit within this range is dependent on the internal delay of the loop and variesaccording to the frequency of common-mode signal components.The common-mode potential used for a BPD is often acquired from the outputs of thefront stages of differential biopotential amplifiers. In electrocardiography, for example, acomposite signal is often generated by summing the various differential leads. This signalis inverted and fed back to the subject’s body through the right-leg electrode. This practice,commonly referred to as right-leg driving, is not optimal, especially at higher frequencieswhere the additional delay caused by the front stages and summing circuitsdegrades BPD performance.Superior performance can be obtained by implementing a separate BPD circuit whichuses an additional electrode (sense). Any modern operational amplifier operated in openloopmode (with a feedback capacitor in the order of a few picofarads) can be used as theheart of the BPD [Levkov, 1982, 1988]. In the circuit of Figure 1.18, the common-modesignal is measured between the sense and common electrodes. This signal is appliedthrough current-limiting resistor R2 to the inverting input of one-half of op-amp IC1.Operated in open-loop mode, a 180 out-of-phase signal is injected into the body throughthe drive electrode in order to cancel the common-mode voltage. D3 and D4 clip the BPDoutput so as not to exceed a safe current determined by resistor R3. In addition, this measureprotects the circuit from defibrillation pulses. D1 and D2 are used to protect the inputof the BPD from ESD and other transients. The low-pass filter formed by R2 and C5, aswell as the presence of feedback capacitor C2, stabilize the circuit and prevent it fromentering into oscillation.The output of the BPD op-amp is rectified by the full-wave bridge formed by D5–D8and then amplified by the differential amplifier built using the other half of IC1. The outputof this op-amp is measured and displayed by the bar graph voltmeter formed by IC3 inconjunction with a 10-element LED display DISP1. The LM3914 bar graph driver IC hasconstant-current outputs, and thus series resistors are not required with the LEDs. The currentis controlled by the value of resistors R8 and R9. Resistor values also set the rangeover which the input voltage produces a moving dot on the display. Power for the circuitis supplied by a single 9-V alkaline battery. The 9-V supply required by IC1 is generatedusing IC2, an integrated-circuit voltage converter. C3, D9, and C4 are required by IC2to produce an inverted output of the power fed through pin 8.An additional advantage of using the BPD is the possibility of monitoring the skin–electrodeimpedance of every electrode connected to the input of a single-ended biopotentialamplifier system. To do so, a test voltage V test fed into the inverting input of the BPDthrough J1-4 induces an additional component on each of the amplified output signals.Phased demodulation of one of these signals removes components corresponding todetected biopotentials, leaving only an amplified version of the detected test signal V i .Assuming that an ideal BPD is used, the amplitude of this signal depends on the
+9VDriveComSenseJ1-4R247KD31N473871 18 17161514131211105 6 4 9 8 3 212IC310LM3914SIGIN REFOUTLED1LED2LED3MODE LED4REF ADJ LED5LED6V+LED7V-J1-5J1-6J1-1J1-2C310uF, 25V tant.+9VR1470K+ C7+1uF, 25V tant.-9VD11N4148D21N4148678D41N4738IC2ICL7660CPA24 CAP+CAP-LVOSCV+3VOUT565-+48-9VIC1BTL082+7C410uF, 25V tant.D51N4148D61N4148D81N4148D71N4148R447K32+-84-9VIC1ATL0821C50.1uFC60.1uFR81.2K2 3 4 5 6 7 81918DISP11615R9101413C90.1uF911+9VGNDGNDTestSignalJ1-3R34.7K+9VC15pFD91N4148C25pFR547KR647K+9VR742M+9V12017RHIRLOLED8LED9LED10+C84.7uF, 25V t ant .Figure 1.18 A body potential driver is implemented by detecting the common mode potential in the area of interest and then feeding thebody a 180 version of the same signal. A feedback loop is thus established, which cancels out common-mode potentials.SubjectElectrodes21
22 BIOPOTENTIAL AMPLIFIERSskin– electrode impedance and is given byV i G i V test( Z i R2)R1 where G i is the gain of each amplifier in the array.For simplicity and convenience, the test signal can be generated by a computerand phased demodulation can be implemented in software. Impedance tests can beperformed just prior to data collection as well as at selected times throughout anexperiment, making it easy to locate faulty electrode–skin connections even in largeamplifier arrays. Further theoretical and practical considerations regarding the constructionof large single-ended biopotential amplifier arrays may be found in a paper by VanRijn et al. [1990].To use the BPD circuit in conjunction with biopotential amplifiers, connect the BPDreference terminal (J1-1) to the reference electrode (subject ground) of the biopotentialamplifier system. Place the sense electrode (e.g., a standard Ag/AgCl ECG electrode) incontact with the body in the proximity of the biopotential amplifier’s active electrode(s)and connect it to J1-2 of the BPD circuit using shielded cable (with the shield connectedto J1-1). A similar electrode placed at a distant point on the body should be connected tothe “drive’’ output (J1-3) of the BPD. Upon hooking up a 9-V alkaline battery to the appropriatepower inputs ( terminal to J1-5 and terminal to J1-6), common-mode signalsshould be neutralized. The moving dot on the display shows the relative maximum amplitudeof the BPD voltage. This can be used to assess the conditions of the recording environment.In general, use of a separate sense electrode is not be recommended for any newlydesigned equipment. Whenever active common-mode suppression is required, the instrumentshould be designed such that the common-mode potential used for BPD is obtainedfrom the outputs of the biopotential amplifier’s front end. However, a stand-alone BPDsuch as the one shown in Figure 1.19 can be used to boost the performance of olderFigure 1.19 A body potential driver can be constructed as a stand-alone unit powered by a 9-V battery.This circuit can be used in conjunction with existing biopotential amplifiers to boost the common-moderejection of older equipment. The LED display shows the relative maximum amplitudeof the BPD voltage to assess the conditions of the recording environment.
DIFFERENTIAL AMPLIFIERS 23equipment. For example, when the BPD is used in conjunction with an existing singleendedECG channel, J1-1 should be connected to the right-leg cable, and the other twoelectrodes can be placed at convenient sites on the body.DIFFERENTIAL AMPLIFIERSWhen a differential voltage is applied to the input terminals of an op-amp as depicted inFigure 1.20, the transfer function of the inverting follower must be rewritten asRfV out (V R 1 V 2 )Similarly, the transfer function of the noninverting follower must be modified toV out 1 RfR (V 1 V 2 )ininV1VdiffV2VoutVcmFigure 1.20Differential and common-mode voltages applied to the input of an op-amp.R110KR3100K++V-VinR210K-VVoutR4100KR1=R2R3=R4Vout=(R3/R1)VinFigure 1.21 Differential amplifier implemented with an op-amp.
24 BIOPOTENTIAL AMPLIFIERSFigure 1.21 presents a differential amplifier based on a single op-amp. If R1 R2 andR3 R4, the gain of the stage is given byIn this case, the transfer function isG R 3 R 4R2R1V out V in R 4R1orV out V in R 3R2where V 1 V 2 is the differential voltage V in .The balance of a differential amplifier is critical to preserve the property of an ideal opampby which its common-mode rejection ratio is infinite. If V 1 V 2 , an output voltage ofzero should be obtained, disregarding any common-mode voltage V CM . If the resistor equalitiesR1 R2 and R3 R4 are not preserved, the common-mode rejection deteriorates.The main problem regarding use of a simple differential amplifier as a biopotentialamplifier is its low input impedance. Especially in older equipment, where thisconfiguration was used to amplify differential biopotentials, high-input-impedance JFETtransistors or MOSFET-input op-amp unity-gain voltage followers were used to buffereach input of the differential amplifier. Despite the enhanced CMR of the differentialamplifier configuration over that of a single-ended system, use of a BPD circuit canincrease considerably the CMR of differential biopotential amplifiers. This is especiallytrue regarding the rejection of interfering signals with high-frequency components.C10.1uFR410M-9V+9VInputR110KR210KR310M234 5-+7 1+9VIC1TL0816R51MC21uFC30.47uFR61M327 1+-4 5-9VIC2TL081612J1BNCFigure 1.22 In this simple differential biopotential amplifier, signals originating from electrophysiological activity in the body are detectedby measuring the potential differences between electrodes connected to the inputs. If the sensing bioelectrodes are placed in the proximityof the biopotential source, common-mode electrical interference affects both probes more or less equally and are rejected by the differentialamplifier stage.
DIFFERENTIAL AMPLIFIERS 25Simple Differential Biopotential AmplifierFigure 1.22 presents the circuit diagram of a simple differential biopotential amplifier.Potential differences originating from electrophysiological activity in the body may bedetected with this circuit by attaching bioelectrodes and measuring the potential differencesbetween them. If the sensing bioelectrodes are placed in the proximity of a biopotentialsource, electrical interference induced from the power line or originating from other sourcesof biopotentials in more remote parts of the body will affect both probes more or less equally.The changes of signal detected simultaneously by both electrodes are rejected by the first stageof the preamplifier. This stage is made up by op-amp IC1 wired as a differential amplifier.For low-frequency signals, the gain of the differential stage is given byG R 3 R 4 1 0 MΩ 1000R2R110kΩAt high frequencies, however, C1 has low impedance, forcing the first stage to act as a lowpassfilter. In addition to limiting the bandwidth of the amplifier, C1 and C3 damp oscillationsand instabilities of the circuit. Note that a gain of 1000 requires that large dc offsetvoltages not be present on the biopotential signal. At this gain, the circuit will stop operatingif the offset voltage exceeds a mere 10 mV. If higher offset voltages are expected, thegain of the amplifier formed around IC1 must be decreased. For example, to use this circuitas part of a surface ECG amplifier, the gain must be recalculated to cope with offsetpotentials of up to 300 mV.The output of IC1 is ac-coupled via C2 to IC2. The 3-dB cutoff for the high-pass filterformed by C2 and R6 is approximately 0.16 Hz. The filtered signal is then buffered byunity-gain voltage follower IC2. To minimize electrical interference, the circuit should bebuilt with a compact layout on an appropriate printed circuit board or small piece of stripboard.The construction of the circuit is straightforward, but care must be taken to keepwiring as short and clean as possible. Leads to the electrodes are coaxial cables with theirshields connected to ground at the circuit board.This circuit is very useful to demonstrate how to measure the CMR and input impedanceof a biopotential amplifier. First, test and calibrate the circuit. You will need a twochanneloscilloscope and a signal generator. Take the following steps:1. Connect the oscilloscope and the signal generator to the biopotential amplifier asshown in Figure 1.23a.2. Apply a 10-Hz signal of 1-mV amplitude as measured by channel 2 of the oscilloscope.3. Verify that the output signal is an amplified version of the input signal.4. Determine the theoretical gain of the equivalent circuit and confirm that the outputsignal has an amplitude of G noninverting 1mV.5. Without changing the settings of the instruments, connect the oscilloscope and thesignal generator to the biopotential amplifier as shown in Figure 1.23b.6. Verify that the output signal is an amplified and inverted (opposite phase) versionof the input signal. Determine the theoretical gain of the equivalent circuit andconfirm that the output signal has an amplitude of G inverting 1mV.To measure the CMR, do the following:1. Connect the equipment as shown in Figure 1.24.2. Adjust the signal generator to produce a 60-Hz 5-V p-p common-mode input signalV in CM .3. Measure the corresponding common-mode output voltage V out CM .
26 BIOPOTENTIAL AMPLIFIERSOscilloscopeBiopotential Amplifier10mV p-p10Hz+IN-INREFOUTInput 1 Input 2(a)Oscilloscope10mV p-p10Hz-INREFBiopotential AmplifierOUTInput1 Input 2+INFigure 1.23 The gain of a differential biopotential amplifier can be measured by injecting a signal (e.g., 10-Hz sinusoidal) at an amplitudesimilar to that expected from the biopotential (e.g., 1 mV) to the inputs. (a) When the amplifer is configured as single-ended, the output signalshould be an amplified version of the input signal. (b) When the circuit is reconfigured to use the inverting input, the output signal shouldbe an amplified and inverted (opposite phase) version of the input signal.(b)4. Calculate the common-mode gain G CM V out CM /V in CM .5. Considering that the differential gain of this biopotential amplifier is given by theratio between the resistor pairs (i.e., G differential 10 MΩ/10 kΩ 1000), calculatethe common-mode rejection ratio, CMRR G differential /G CM , and common-moderejection, CMR(dB) 20 log 10 (G differential /G CM ).Next, measure the input impedance of the biopotential amplifier. You will need an ohmmeter(e.g., a digital multimeter or VOM) and a 10-MΩ multiturn potentiometer in additionto the oscilloscope and signal generator. Follow this procedure:1. Connect the equipment as depicted in Figure 1.25.2. Adjust the signal generator to produce a 100-Hz sinusoidal wave with an amplitudeof 1 mV p-p . This signal is measured by channel 2 of the oscilloscope.3. Set the potentiometer to 0 Ω and measure the amplifier’s peak-to-peak output voltageon channel 1. Record this value.4. Carefully adjust the 10-MΩ potentiometer until the voltage measured on channel 1reaches half the value recorded in the preceding step.
OP-AMP INSTRUMENTATION AMPLIFIERS 27OscilloscopeBiopotential Amplifier+INOUTV out cmInput1Input 2Vin cm5V p-p60Hz-INREFFigure 1.24 To measure the CMR of a biopotential amplifier, the differential inputs should be shorted and a relatively large common-modesignal (e.g., 60-Hz 5-V p-p sinusoidal) injected between the shorted differential inputs and the biopotential amplifier’s common referenceinput. The common-mode rejection is then calculated as CMR (dB) 20 log 10 (G differential /G CM ).OscilloscopeR110M+INBiopotential Amplifier1mV p-pOUTInput 1 Input 2-INREFFigure 1.25 To measure the input impedance of the biopotential amplifier, inject an in-band test signal of known amplitude (e.g., 1 mV) tothe biopotential amplifier’s inputs through a 10-MΩ potentiometer. Adjust the potentiometer until the output voltage is half of the amplitudeobtained with the potentiometer set to 0 Ω. The resistance of the potentiometer at the half-output point is equal to the input impedance of thebiopotential amplifier at the test frequency. This measurement should be repeated for a number of in-band frequencies to compute the capacitiveand resistive components of the input.5. Without changing the setting of the potentiometer, measure its resistance with theohmeter. This value is equal to the input impedance of the biopotential amplifier atthe specified frequency.6. Repeat the experiment for various frequencies from 0.1 Hz to 20 kHz. Use appropriatesettings for the oscilloscope’s time base. Compute the capacitive and resistivecomponents of the input impedance based on the data obtained.OP-AMP INSTRUMENTATION AMPLIFIERSAn alternative to the simple differential amplifier is the multiple op-amp configuration presentedin Figure 1.26. This differential configuration, known as an instrumentation
28 BIOPOTENTIAL AMPLIFIERS+15VV 1327 1+A1-4 8-15VIC1OP-076R250k, 1.0%VaR510k, 0.1%R610k, 0.1%J112-IN+INR11.0k, 1.0%-15VIC34 8 OP-07J22 -6V1A3out3 +2OUTPUTV 223-15V4 8-A2+IC2OP-076R350k, 1.0%R410k, 0.1%7 1+15VR710k, 0.1%7 1+15VFigure 1.26VbOp-amp instrumentation amplifier.amplifier, has the advantage of preserving the high input impedance of the noninvertingfollower, yet offering gain. Input amplifiers A1 and A2 can be analyzed as noninvertingamplifiers which produce output voltages ofV A 1 R 2 R1V 1 (R 2)V 2R1andV B 1 R 3 R1V 2 (R 3)V 1R1Initially, if it is assumed that the gain of amplifier A3 is unity and that R2 R3, thenV out V B V ASubstituting into the two preceding equations gives the output voltage:V out (V 2 V 1 ) 1 2 RR 2 1Whenever the gain of amplifier A3 is greater than unity, this equation must be multipliedby the gain of the differential stage. If R4 R5 and R6 R7, the overall voltage gain ofthe instrumentation amplifier is given byV out (V 2 V 1 ) 1 2 RR 2 1R 6R 5
OP-AMP INSTRUMENTATION AMPLIFIERS 29Biopotential amplifiers are seldom built these days using individual op-amps. Instead, anintegrated circuit instrumentation amplifier (ICIA) combines in a single package most ofthe components required to make an instrumentation amplifier. ICIAs typically require oneor two external resistors to set their gain. These resistors do not affect the high CMRRvalue or the high input impedance achieved in ICIAs through precise matching of theirinternal components.Instrumentation Biopotential AmplifierThe circuit of Figure 1.27 is a typical ICIA-based biopotential amplifier. This high-inputimpedancecircuit combines a programmable-gain instrumentation amplifier and an accoupled(LPF: 3 dB at 0.5 Hz; HPF: 3 dB at 500 Hz) configurable bandpass filter toform a highly versatile, compact, stand-alone biopotential amplifier. Differentialamplification of the biopotential signal is achieved with high CMR ( 90 dB at 60 Hz)through the use of a high-accuracy monolithic instrumentation amplifier IC. The low-noise(1 µV p-p between 0.5 and 100 Hz) front end can be programmed to have a gain of 10,100, or 1000, while a fixed second stage and a configurable third stage further amplify thesignal to an overall gain of up to 1 million.Typical applications for this biopotential amplifier are as a front-end and main amplifierfor standard and topographic EEG, evoked potential tests (BAER, MLAR, VER, SER),and for cognitive signals and long-latency studies. The heart of the circuit is IC1, Burr-Brown’s INA102 programmable monolithic IC instrumentation amplifier. Biopotentialsare dc-coupled to the instrumentation amplifier through current-limiting resistors R1 andR2. An INA102 gain of 1, 10, 100, or 1000 is selected by programming jumpers JP1 andJP2 as shown in Table 1.1. Since the amplifier is dc-coupled, care must be exercised in theselection of gain so that the amplifier is not saturated by dc offset voltages accompanyingthe biopotential signal. For example, to use this circuit as part of a surface ECG amplifier,the gain must be calculated to cope with offset potentials of up to 300 mV.The INA102 is ac-coupled (3 dB at 0.5 Hz) to a second amplification stage with a fixedgain of 100. Resistor R5 and capacitor C2 form a low-pass filter with 3-dB cutoff at500 Hz. R6, R7, R8, C3, C4, and C5 are used to select the desired passband of two stages offiltering. R6–R8 and C3–C5, along with one-half of IC3, form a third-order (18 dB/octave)Butterworth low-pass active filter stage. The design of these filters is discussed in Chapter 2.Finally, the ac output of the filter is presented to an inverting amplifier prior to output.The gain of this last stage is given by G IC3B R10/R9. As shown in Figure 1.28, componentsR6–R9 and C3–C5 can be soldered onto a DIP header which is inserted in a 14-pinDIP socket. A number of these DIP-header modules may be assembled to provide anassortment of desired passband and gain characteristics. If the listed resistors and capacitorsare used, the low-pass 3-dB point is fixed at 22 Hz, with a third-stage gain of 10.The supply voltage to the circuit must be symmetrical and within the range 5 V (minimum)to 16 V (absolute maximum). Rated specifications are obtained using a supply of15 V. Diodes D1 and D2 provide protection against incorrect supply voltage polarity, andcapacitors C7–C14 are used to decouple and filter the power supply. Because of the verysmall quiescent maximal supply current used by this circuit, a pair of 9-V alkaline batteriesconstitute a suitable power supply for most applications. Preferably, leads to the bioelectrodesshould be low-loss low-capacitance coaxial cables whose shields are connectedto the subject ground terminal of the biopotential amplifier. Construction of this biopotentialamplifier is simple and straightforward, but care must be taken to keep all wiring asshort and as clean as possible.In using this biopotential amplifier it is desirable to keep the gain of the first stage low(e.g., 10), and to reach the required overall gain by selecting a high gain for the third stage.In addition, optimal rejection of unwanted signal components is best achieved by careful
X1KX100X10JP2Sense3 2 13 2 14 5 6JP1GainC50.47uF, mono.11 4J1 R11234 J3J2 123C12 C1IC2R6R7R8R2IC1R3 R4R5C39C2D1R10C7C9 C11 C1312C8C10 C1410K10K1N41481uF, tant. 35V1uF, tant. 35V1514++7 6 5 4 3 2+-10INA102KP0.01uF110.01uF1uF330K0.01u F0.01uF 0.01uF 0.01uF1K+VIC1-V91232+V7+-4-V3300 pF, mono.+VIC2-V4187OPA276100K+VIC3-V48100K314 16213100KOutput12 10100K571M48C4234-+-+-V18IC3BTL08265+V0.1uF, mono. 0.01uF, mono.IC3ATL0828C61uF, tant., 35VR9100K+7D21N4148Figure 1.27 This high-input-impedance circuit combines a Burr-Brown’s INA102 programmable-gain instrumentation amplifier and anac-coupled (LPF: 3 dB at 0.5 Hz, HPF: 3 dB at 500 Hz) configurable bandpass filter to form a highly versatile, compact, stand-alonebiopotential amplifier.COM-IN+INCOM+VccGnd-Vcc30
OP-AMP INSTRUMENTATION AMPLIFIERS 31TABLE 1.1 The Gain of the INA102 ICIA ofFigure 1.27 Is Jumper-Programmable Accordingto These Settings for JP1 and JP2Gain JP1 JP21 None 2–310 1–6 2–3100 2–5 2–31000 3–4 1–2Figure 1.28 The components that select gain and bandpass filter characteristics (R6–R9 andC3–C5) for the ICIA-based biopotential amplifier can be soldered onto a DIP header which isinserted in a standard 14-pin DIP socket. A number of these DIP-header modules may be assembledto provide an assortment of desired passband and gain characteristics.selection and preparation of electrode placement on the subject, and by keeping the bandpasscharacteristics of the biopotential amplifier as tight as possible. When connected to atest subject, the circuit must always be powered from batteries or through a properly ratedisolation power supply. The same isolation requirements apply to the output of the amplifier.To test and calibrate the unit, you will need a two-channel oscilloscope and a signalgenerator. Take the following steps:1. Assemble the DIP header according to your requirements and install in the 14-pinsocket.2. After verifying the connections, power the biopotential amplifier circuit with asymmetrical power supply.3. Short both inputs (J1-2 and J1-3) of the biopotential amplifier to ground (J1-1,4).Configure JP1 and JP2 for a gain of 10.4. Connect the oscilloscope’s input to the output of the biopotential amplifier circuit(J3-1) and the oscilloscope’s ground to that of the biopotential amplifier’s (J3-2).5. The output signal should be stable and should present no oscillatory behavior ordrift. At very high gains, the peak-to-peak input noise of the circuit can be measured.6. Short the inverting (J1-2) input terminal of the biopotential amplifier to the subjectground terminal (J1-1,4), and connect these to the ground terminal of a signal
32 BIOPOTENTIAL AMPLIFIERSgenerator. Connect the output of the signal generator to the noninverting input (J1-2) of the biopotential amplifier.7. Adjust the signal generator to produce a sinusoidal wave with an amplitude of1mV p-p at a frequency within the passband of the filter configuration selected.8. Check that changes in the configuration of JP1 and JP2 cause correspondingchanges in the amplitude of the output signal.9. Set the gain to 10, and using the second channel of the oscilloscope, check thatthere is no phase difference between the signal at the output of the ICIA and that atthe noninverting input.10. Without changing the settings of the instruments, short the noninverting (J1-3) inputterminal of the biopotential amplifier to the subject ground terminal (J1-1,4), andconnect these to the ground terminal of the signal generator. Connect the output ofthe signal generator to the inverting input (J1-2) of the biopotential amplifier.11. Verify that the output signal is an amplified and inverted version (opposite phase)of the input signal. Verify that the gain remained constant.While the signal generator is connected, monitor the output of the biopotential amplifierwhile increasing and decreasing the frequency of the signal generator. You can verify yourchoice of components used for the filter stages by observing that the decay in output amplitudeindeed occurs at the expected frequencies. The procedure is as follows:1. Set the gain of the biopotential amplifier front gain to unity.2. Adjust the input sine wave to exactly 0.07 V and the frequency to the midpoint ofthe bandpass expected. Make this adjustment as accurately as possible.3. Check that the output signal is of the amplitude expected. Readjust the signal generatorif necessary.4. Slowly increase the input frequency until the output amplitude decreases to 0.05 V(70.7% of the midrange gain). Measure the frequency at this point. This is the highfrequencycutoff point of the biopotential amplifier.5. Repeat the preceding steps for gain factors of 10, 100, and 1000 using appropriatesettings for the signal generator and the oscilloscope.6. Reset the gain of the biopotential amplifier front end to unity.7. Connect a 1-µF nonpolar capacitor in series between the signal generator and theinput to the biopotential amplifier.8. Slowly sweep the frequency of the input signal starting from dc and measure thefrequency at the two points where the output signal is 0.05 V (70.7% of themidrange gain). This is the low-frequency cutoff point of the biopotential amplifier.9. Plot the response of this last configuration on a semilogarithmic graph.This amplifier is suitable for applications involving low-level low-frequency signals.Thus, you may want to measure the amplifier’s equivalent noise level. To do this you willneed a digital storage oscilloscope or chart recorder. Follow this procedure:1. Short both inputs of the biopotential amplifier to the patient ground terminal.2. Connect the oscilloscope to the output of the biopotential amplifier.3. Set the oscilloscope for a 10-second total sweep and dc coupling.4. Set the overall gain of the biopotential amplifier to 100,000.5. Set the gain of the oscilloscope up to a point where the peak events of the widefuzzy noise signal can be measured.
OP-AMP INSTRUMENTATION AMPLIFIERS 336. Typical peak-to-peak noise measurements are found by reading the maximumpeak-to-peak voltage noise of the circuit’s output for three observation periods of10 seconds each, then dividing by the gain of the amplifier (i.e., 100,000).You may want to compare the CMR of the ICIA to that of the differential amplifierdescribed in the earlier project. Use a procedure similar to the one used earlier to measurethe CMR of the instrumentation biopotential amplifier:1. Connect the equipment, shorting the differential inputs as shown in Figure 1.24.2. Adjust the signal generator to produce a 60-Hz, 5-V p-p input signal V in CM .3. Measure the corresponding common-mode output voltage V out CM .4. Calculate the common-mode gain G CM V out CM /V in CM .Using the measured gain of the biopotential amplifier, calculate the common-moderejection:CMR(dB) 20 log 10 G differentialGCMSwitched-Capacitor Instrumentation Biopotential AmplifierDifferential biopotential signal recordings can be done through circuits other than classicalop-amp differential or instrumentation amplifiers. The simplified circuit in Figure 1.29implements a simple but precise instrumentation amplifier that uses a switched-capacitorbuilding block. It converts differential signals from a preamplified electrode pair to a single-endedoutput while rejecting common-mode signals in an effective manner. In this circuit,a solid-state dual-pole dual-throw (DPDT) switch block converts the differential inputto a ground-referred single-ended signal which may then be amplified by a noninvertingfollower op-amp configuration.During the time that the input switches are closed (Φ odd), sampling capacitor C Sacquires the input signal V in diff . When the input switches open (Φ even), hold capacitorC H receives the sampled charge. Switching C S continuously between the inputFigure 1.29 In this switched-capacitor instrumentation amplifier, a solid-state DPDT switch blockconverts the differential input to a ground-referred single-ended signal which is then amplified by anoninverting follower operational amplifier configuration.
34 BIOPOTENTIAL AMPLIFIERSFigure 1.30 Switched-capacitor instrumentation amplifier timing and equivalent circuits:(a) basic equivalent circuit; (b) switching timing; (c) first odd-phase equivalent circuit; (d ) first evenphaseequivalent; (e) generalized even-phase equivalent circuit; ( f ) analog equivalent circuit.voltage and C H causes output voltage V out to track the difference between the circuit’sinputs V in diff , rejecting common-mode voltages V in CM . Assuming that the characteristicsof the op-amp approach those of an ideal op-amp, the transfer characteristics of the circuitmay be determined by following conventional network analysis methods. The equivalent
OP-AMP INSTRUMENTATION AMPLIFIERS 35circuit is presented in Figure 1.30a. For the purpose of analysis, inputvoltage V in is assumed to be constant during the sampling period. It is further assumed thatthe switches are thrown back and forth continuously with a clock period T according to thetiming diagram of Figure 1.30b and that their connections shift instantly with no overlap.During the first odd-phase interval (n 1) t/T (n 1 2 ), the circuit is equivalent toFigure 1.30c, and C S is charged instantaneously to V Φoddin (n 1):V CS (t) V Φ in odd [(n 1)T] V Φ in odd (n 1)While the odd-phase output voltage V Φ out odd is equal to the voltage of V CH,V CH (t) V Φ out odd [(n 1)T] V Φ out odd (n 1)During the even-phase interval (n 1 2 ) t/T n that follows, the circuit is equivalent tothat of Figure 1.30d, and charges are redistributed between C S and C H , which results in anew output voltage. The analysis of the charge transaction is simplified by assuming thealternative equivalent circuit of Figure 1.30e with uncharged capacitors. By applying theinitial voltages of the capacitors represented by the sources as step functions edged att (n 1)T, the new output voltage isV Φ out even n 1 2 CSCV Φ in oddH(n 1) V C S C HCS C Φ out odd (n 1)HDuring the odd-phase interval n t/T (n 1 2 ) , capacitor C H remains undisturbed, andthus the output voltage is represented by the expressionV Φ out odd (n) V Φ out even n 1 2 A general expression representing the odd-phase output voltage may now be writtenV Φ out odd CS(n) V Φ in oddCH(n 1) V Φ out odd (n 1)CS C HCS C HApplying the z-transform to this equation, we obtainV Φ out odd CS(z) V Φ in odd CHz (z) 1 V Φ out odd (z)CS C HC S CHThe odd-phase discrete-frequency-domain transfer function may then be solved directly:H Φinodd;Φoutodd ΦoddV out ( z)1z(z) 1VΦoddin ( z)1 C CH/C S 1H/CS z 11 C /CBy replacing z by e jωT and using Euler’s formula, the time-domain representation of thisequation can be written asH Φ inodd;Φoutodd (e jωT ) V V Φ ΦoddoutoddinjωTejωTe1(1 C H /C S ) cos ωT C H /C S j (1 C H /C S ) sin ωTwhere ω is the frequency of an applied sinusoidal signal and T is the clock period. Fromthis equation it is possible to determine the magnitude response and phase shift of theswitched-capacitor instrumentation block. In addition, a capacitance ratio C H /C S thatHS
36 BIOPOTENTIAL AMPLIFIERSresults in an appropriate frequency response may be selected. Assuming that the switchingfrequency allows for a large oversampling of the desired passband, z can be approximatedby the continuous Laplace term (1 sT ); thenH Φinodd;Φoutodd z1sT(z) ⎯⎯→ H(s) sT(1 C1H/C S ) 1Comparing this to the continuous frequency-domain transfer function of a simple RC lowpassfilter yields1H(s) (s/ω 1)1where ω 1 1/RC. Then a cutoff frequency of f 3dB 1/2πRC may be obtained through acapacitance ratio of C H 1C 2πfSThe analogy to an RC low-pass filter is not a mere coincidence, because the DPDTswitches together with C S constitute the parallel switched-capacitor resistor realization ofFigure 1.30f, whose value is given by3dBTR equivalent TC SThe capacitance of C S must be computed to comply with a desired input impedance, whichis dependent on the sampling frequency. It must be noted that because of the fact that common-modesignals are not sampled, their spectral content may well exceed the samplingfrequency without encountering aliasing.It may be seen from the analysis presented above that after charge reorganization hasbeen achieved during an even-phase interval, the output voltage is held as long as the samplingcapacitor does not bring a new sample in contact with the hold capacitor. This propertymay be used to reject stimulation artifacts (i.e., high-amplitude spikes caused bycurrents caused by a pulse generator intended to cause tissue stimulation) by extending theeven-phase interval, making it slightly longer than the stimulation pulse to be rejected. Thistechnique effectively isolates the stimulation artifact from the high-gain amplification andprocessing circuitry, following the instrumentation stage, allowing for the immediately consecutivedetection of biopotentials.Although switched-capacitor instrumentation stages are not very common in patientmonitors, they are often used as the core of biopotential amplifiers in implantable devices(e.g., pacemakers). In addition, many modern analog signal processing applications relyon switched-capacitor sampled-data processing techniques implemented through the useof CMOS charge manipulation circuits. In these applications, CMOS application-specificICs (ASICs) contain switches and capacitors that are used as an economical means of massproducing sophisticated signal processing functions, such as amplification, analog arithmetic,nonlinear functions, and filtering [Allen and Sanchez-Sinencio, 1984].In the circuit of Figure 1.31, IC3, a monolithic charge-balanced dual switched-capacitorinstrumentation building block (Linear Technology’s LTC1043), implements all of therequired charge manipulation functions. Within this integrated circuit, a nonoverlappingclock controls two DPDT CMOS switch sections. If the switched-capacitor stage IC3would be connected directly to a differential biopotential source detected by small-areasurface electrodes, and the sampling frequency is chosen to be 100 times that of the highestspectral component of the signal, the optimal value of the sampling capacitor wouldresult in the picofarad range to present an input impedance in the gigaohm range.
Vout1J3+V32910+-411-+-V114-V+V1IC1ATL084IC1CTL0848R1V2V1561312+--+411+V114-VR2R3-V+V7IC1BTL084IC1DTL08414VAVBC1+V-V78131465181511121641723IC3S1AS2AS3AS4AS1BS2BS3BS4BCA+CA-CB+CB-COSCV+V-SHASHBLTC10431101J4CH32+V7 1+-4 5-V= even6IC2TL081R5R4Clock In= oddFigure 1.31 In the switched-capacitor-based biopotential instrumentation amplifier, the op-amps of IC1 form an ultrahigh-impedancedifferential-in/differential-out amplifier, while a switched-capacitor block together with IC2 form a differential stage.11J1J2V1V237
38 BIOPOTENTIAL AMPLIFIERSUsing off-the-shelf components, however, the construction of such a circuit would introduceparasitic capacitances in the same order of magnitude as the sample-and-hold capacitances,resulting in errors that the internal charge-balancing circuitry within the integratedcircuit cannot cancel. For this reason, this design includes two noninverting amplifiers IC1Band IC1D which present the switched-capacitor block with a signal level that is compatiblewith a larger-valued sampling capacitor, effectively eliminating the problems related to parasiticcapacitances. The output of each of these amplifiers is given byandV A 1 R 2R1V 1 (R 2)V 2R1V B 1 R 3R1V 2 (R 3)V 1R1Thus, if R2 R3, the theoretical differential voltage presented to the sampling capacitor isV A V B (V 2 V 1 ) 1 2R 2 R1CMOS op-amps IC1A and IC1C are configured as unity-gain buffers and serve as ultrahighimpedance to low-impedance transformers so that the biopotential signal may be carriedwith negligible loss and contamination to the instrumentation stage. In criticalapplications, these could be mounted in close proximity to the electrodes used to detect thebiopotentials. In addition, if the biopotential amplifier can be mounted close enough to thesubject, IC1A and IC1C may be omitted.In order not to reduce the high common-mode rejection that may be achieved throughuse of a switched-capacitor instrumentation block, the use of high-precision componentsis mandatory, so that the gain of the chain formed by IC1A and IC1B will closely matchthat of IC1C and IC1D. In addition, an adequate layout of the printed circuit board orbreadboard, using guard rings and shielding the sampling capacitor from external parasiticcapacitances, is necessary to preserve the common-mode rejection from being degraded.This also helps maintain the inherent ultrahigh impedance of the CMOS input buffers.An additional high-performance CMOS operational amplifier IC2, configured as a noninvertingfollower, amplifies the single-ended output of the instrumentation stage. The ultrahighinput impedance of this amplifier ensures that the performance of the switched-capacitor stageis not affected by the output load. The dc gain of the noninverting follower is given byG IC2 1 R 5R4which is multiplied by its own transfer function, the dc gain of the input amplifiers andbuffers, their transfer function, and the transfer function of the switched-capacitor instrumentationblock to yield the frequency-dependent gain of the complete system. However, theflat-response bandwidth of any modern operational amplifier is by far wider than that ofbiopotential signals, and by selecting a very high sampling frequency and the correct capacitanceratio, a virtually flat frequency response within the bandwidth of interest is achievable.Figure 1.32 shows an array of these switched-capacitor instrumentation amplifiers used todetect myoelectric signals from muscle fibers stimulated by an electrical current. Artifactsinduced by the high-voltage surface neuromuscular stimulation can be rejected by extendingthe even-phase switching interval during stimulation. To do so, an external clock drives theswitched-capacitor timing logic. Just prior to stimulation, the clock is isolated from theamplifiers by a logic <strong>AND</strong> gate, and all switched-capacitor blocks are set unconditionally toeven-phase mode. Shortly after stimulation ceases, switching at clock speed is restored.
OP-AMP INSTRUMENTATION AMPLIFIERS 39Figure 1.32 Switched-capacitor biopotential amplifier array setup for detecting propagating activityin electrically stimulated muscle. Stimulation artifacts are isolated from the high-gainamplification stages by extending the even-phase switching interval throughout a stimulation pulse.Initial rejection of the stimulus artifact is effected through differential measurement ofEMG signals. Rippling caused by the instantaneous change in switching period are minimizedby sample-and-hold and low-pass filter properties of the switched-capacitor instrumentationamplifier. Further rejection of the induced discontinuity are easily rejectedthrough a low-pass filter as well as through decreasing the slew rate of the output op-amp.Figure 1.33 presents results from such an array recording used to record EMG signalsfrom the biceps brachii muscle. Signals were differentially recorded using 32 surface electrodes2.54 mm apart. The ultrahigh-impedance buffer array circuit presented earlier in thischapter was used as the electrode buffer. Switched capacitors were clocked at 100 kHz bya 50% duty-cycle oscillator. A separate oscillator triggered a high-voltage surface neuromuscularstimulator at a rate of 18 Hz. One-half millisecond before generation of a 1.06-ms compensated stimulation pulse, all switched-capacitor stages are forced to aneven-phase state and remain that way for an additional 1 ms after the stimulation pulseceases.The 31 single-differential EMG signals clearly show a compound potential originatingunder channel 20 and propagating bidirectionally toward channels 1 and 31. The artifactresulting from stimulation currents and switching discontinuity in the biopotential amplifiers
40 BIOPOTENTIAL AMPLIFIERSFigure 1.33 Bipolar array recording of composite propagating EMG activity evoked by a single surface stimulation pulse. The artifactresulting from stimulation currents and switching discontinuity is indicated between brackets. [Reprinted from Med. Eng. Phys., 17, D.Prutchi, A High-Resolution Large Array (HRLA) Surface EMG System, pages 442–454, 1995, with permission from Elsevier.]is present on all channels simultaneosly. Please note that the level of interference it causes(shown between brackets) is minimal compared to the amplitude of evoked potentials.Recently, multichannel recordings such as these have gained wide popularity inresearch and diagnostic uses of electrophysiological activity. For example, 32-channel systemshave been used in EEG and evoked potentials, and 64-channel systems have beendeveloped for body potential mapping (BPM) ECG. In electromyography, surface electrodearrays have been used to detect propagating electrical activity in skeletal muscles,enabling noninvasive estimation of muscle fiber conduction velocity and innervation zone.REFERENCESAllen, P. E., and E. Sanchez-Sinencio, Switched Capacitor Circuits, Van Nostrand Reinhold, NewYork, 1984.Levkov, Ch. L., Amplification of Biosignals by Body Potential Driving, Medical and BiologicalEngineering and Computing, 20, 248–250, 1982.Levkov, Ch. L., Amplification of Biosignals by Body Potential Driving. Analysis of the CircuitPerformance, Medical and Biological Engineering and Computing, 26, 389–396, 1988.Prutchi, D., and A. Sagi-Dolev, New Technologies for In-Flight Pasteless Bioelectrodes, Aviation,Space and Environmental Medicine, 64, 552–556, 1993.Van Rijn, A. C., A. Peper, and C. A. Grimbergen, High-Quality Recording of Bioelectric Events—Part 1: Interference Reduction, Theory and Practice, Medical and Biological Engineering andComputing, 28, 389–397, 1990.Whinnery, J. E., D. H. Glaister, and R. R. Burton, G z -Induced Loss of Consciousness and AircraftRecovery, Aviation Space and Environmental Medicine, 58, 600–603, 1987.
2B<strong>AND</strong>PASS SELECTION FORBIOPOTENTIAL AMPLIFIERSAs shown in Table 2.1, common biopotential signals span the range dc to 10 kHz. Underideal conditions, a biopotential amplifier with wideband response would serve most applications.However, the presence of common-mode potentials, electrode polarization, andother interfering signals often obscure the biopotential signal under investigation. As such,the frequency response of a biopotential amplifier should be tuned to the specific spectralcontent expected from the application at hand.Spectral analysis is the most common way of determining the bandwidth required toprocess physiological signals. For a first estimate, however, the rigors of spectral analysiscan be avoided simply by evaluating the durations of high- and low-frequency componentsof the signal. Koide [1996] proposed a method for estimating the 3-dB bandpass basedon acceptable distortion.The duration of the highest-frequency component, t HF , is estimated from a stereotypicalsignal to be the minimum rise or fall time of a signal variation. The duration of the lowestfrequencycomponent, t LF , on the other hand, is measured from the tilt of the baseline orof the lowest-frequency component of interest. Koide illustrated this with an example.Figure 2.1 shows a stereotypical intracellular potential measured from the pacemaker cellsin a mammalian heart SA node. In this example, t HF 75 ms and t LF 610 ms. Using theformulas of Table 2.2, the amplification system must have a 3-dB bandpass of 0.0026 to41.3 Hz to reproduce the signal with negligible distortion (1%). Acceptable distortion,usually considered to be 5% or less for physiological signals, would require a narrower3-dB bandpass, of 0.013 to 18.7 Hz.WIDEB<strong>AND</strong> BIOPOTENTIAL AMPLIFIERThe biopotential amplifier circuit described by the schematic diagrams of Figures 2.2 and2.3 covers the complete frequency range of commonly recorded biopotentials with highCMR. In this circuit, a Burr-Brown INA110AG ICIA is dc-coupled to the electrodes viacurrent-limiting resistors R22 and R23. Two Ohmic Instruments IS-1-3.3DP semiconductorDesign and Development of Medical Electronic Instrumentation By David Prutchi and Michael NorrisISBN 0-471-67623-3 Copyright © 2005 John Wiley & Sons, Inc.41
42 B<strong>AND</strong>PASS SELECTION FOR BIOPOTENTIAL AMPLIFIERSTABLE 2.1ApplicationFrequency Ranges of Various Biopotential SignalsFrequency RangeAction potentials detected with transmembranedc–2 kHzpipette electrodesElectroneurogram (ENG): nerve bundle potentials10 Hz–1 kHzdetected with needle electrodeElectroretinogram (ERG): potentials generated0.2–200 Hzby retina in response to a flash of light; detectedwith implanted electrodesElectrooculogram (EOG): eye potentials useddc–100 Hzto measure eye position; detected with surface electrodepairs: left/right and above/below eyesElectrogastrogram (EGG): stomach potentials detected0.01–0.55 Hzwith surface electrodes placed on abdomenElectroencephalogram (EEG): rhythmic brain potentials Delta waves 0.5–4 Hzdetected with surface electrodes placed on head Theta waves 4–7.5 HzAlpha waves7.5–13 HzLow beta waves13–15 HzBeta waves15–20 HzHigh beta waves20–38 HzGamma waves38–42 HzBrain evoked potentials: brain potentials evoked by stimuli; Visual evoked potential (VEP) 1–300 Hzdetected with surface electrodes placed on head Auditory evoked potential (AEP) 100 Hz–3 kHzSomatosensory evokedpotential (SSEP)2 Hz–3 kHzElectrocardiogram (ECG): heart potentials detected with Heart rates (R-R intervals) 0.5–3.5 Hzsurface electrodes placed on chest, back, and/or limbsR-R variability due tothermoregulation0.01–0.04 HzR-R variability due to baroreflexdynamics0.04–0.15 HzR-R variability due to respiration0.15–0.4 HzP,QRS,T complex0.05–100 HzVentricular late potentials40–200 HzBandwith requirement forclinical ECG/rate monitors0.67–40 HzClinical cardiac electrophysiology: analysis of cardiac Intracardiac electrograms 10 Hz–1 kHzpotentials detected with catheter electrodes placed inMonophasic actioncontact with the myocardium potentials (MAPs) dc–2 kHzElectromyogram (EMG): muscle potentials detected Surface EMG 2–500 Hzwith surface electrodes or indwelling needle Motor unit action potentials 5 Hz–10 kHzelectrodes Single fiber electromyogram 500 Hz–10 kHzGalvanic skin response (GSR): battery potentialsdc–5 Hzproduced by sweat on skin electrodescurrent limiters are used for redundant protection of the subject from leakage currents. C25,C27, and C26 are used to protect the amplifier from high-frequency currents, such as thoseused in electrosurgery and ablation procedures. R21 and R24 limit the impedance of eachinput to 10 MΩ referred to the circuit’s isolated ground. These resistors provide enough biasto maintain high immunity to common-mode signals without the need of a patient groundelectrode. Diodes D7–D10 are used to protect the inputs of IC5 from high-voltage transientssuch as those expected from defibrillation and electrostatic discharge.
WIDEB<strong>AND</strong> BIOPOTENTIAL AMPLIFIER 43mV200-200 0.5 1.0 1.5Time(s)-40610 ms-6075 msFigure 2.1 A stereotypical intracellular potential measured from the pacemaker cells in a mammalianheart SA node has a minimum rise time of t HF 75 ms and a tilt of t LF 610 ms. The 3-dBbandpass needed to reproduce this signal with 1% distortion is of 0.0026 to 41.3 Hz.TABLE 2.2 Approximate 3-dB Frequencies Required for the Reproductionof Physiological Signals with Negligible and Acceptable Levels of Distortion3-dB Point Negligible Distortion (1%) Acceptable Distortion (5%)High-pass (Hz) 0 . 0016 0 .008tLF(s)t L F( s)3.11.4Low-pass (Hz) tH ( s)tH ( s)FFIC5 is powered via a Burr-Brown ISO107 isolation amplifier IC3, which generatesisolated 12 V when powered from 12 V. L1, C6, C7, and C8 form a pi filter to cleanthe isolated 12-V power line generated by the ISO107 from switching noise. An identicalnetwork is used to filter the negative isolated supply rail. A pi filter formed by L3, C15,C16, and C17 is used to decouple the positive input power rail of IC3 so that switchingnoise within IC3 does not find its way into the postisolation amplifier stages (IC2 and IC4).R10 and C21 form a low-pass filter with 3dB of approximately 7 kHz to eliminate anyremaining trace of the carrier used to convey the signal across IC3’s isolation barrier.Op-amp IC2B is configured as a noninverting amplifier. The gain of this amplifier canbe selected through potentiometers R16–R20 that are switched via SW3. These providedifferent levels of feedback to IC2B, depending on their setting. The output of this amplificationstage is filtered via R9 and C20 with a 3dB low-pass cutoff of approximately7 kHz to eliminate any residual switching noise that may have coupled through the inputor power supply and amplified by IC2B. The amplified signal is buffered and further lowpassfiltered via fixed-gain noninverting amplifier IC4 before being presented to the outputconnector J1.Since the biopotential amplifier is dc-coupled and there are occasions when the signalof interest may have a relatively large input dc offset, an automatic zero-offset circuit hasbeen implemented through IC2A. Whenever offset nulling is desired, momentary pushbuttonswitch SW1 should be pressed. Doing so presents a sample of the output signal tothe integrating sample-and-hold (S&H) circuit formed by IC2A, R5, and C9. The hold capacitorshould be a low-leakage type, and the path between the capacitor and the inverting
44 B<strong>AND</strong>PASS SELECTION FOR BIOPOTENTIAL AMPLIFIERSISO_GND-12V_ISO+12V_ISOJ3-VIN 12mmC25100pFJ2ISO1 R22+VIN 12mm IS-1-3.3DP 100kISO1IS-1-3.3DPC27100pFR23100kISO_GNDR2110MR2410MD7FDH300D9+12V_IS<strong>OF</strong>DH300D8FDH300D10-12V_ISOC261nFFDH300+12V_ISOJP11 23 45 67 8-12V_ISOC290.01uF211312161134587C280.01uFIC5INA110AG+IN OUT-INOSENSEX10X100 REFX200X500 OOADJOOADJRGIOADJIOADJ+VCC-VCCFRONT_END_OUT91061415ISO_GNDISO_GNDFigure 2.2 This wideband dc-coupled biopotential amplifier front end covers the complete frequency range of commonly recorded biopotentials.A Burr-Brown INA110AG ICIA is dc-coupled to the electrodes via current-limiting resistors R22 and R23 and IS-1-3.3DP faultcurrentlimiters. Capacitors and diodes are used to protect the amplifier from high-frequency currents, such as those used in electrosurgeryand ablation procedures as well as from high-voltage transients such as those that may be expected from defibrillation and electrostaticdischarge.input of the op-amp should be shielded against stray and leakage currents through a guardring on the circuit board. The output of the integrator/S&H is summed with the output ofIC2B via R4. The output of IC2A is also attenuated via R6 and R8 and summed with theoutput of the isolation amplifier (IC3) via R7. This trick allows offsets that would otherwisesaturate amplifier IC2B to be canceled in a very effective way.A typical application for a dc-coupled wideband biopotential amplifier is the measurementof transmembrane potentials as well as for the detection of cardiac monophasicaction potentials (MAPs). Dc coupling is important for these applications because they areusually related to measuring the timing and amplitude of shifts in potentials that have a dcoffset.BIOPOTENTIAL AMPLIFIER WITH DC REJECTIONUnlike transmembrane and MAP signals, most biopotential recordings made with extracellularelectrodes contain signals of physiological interest only at frequencies above dc.In fact, very low frequency components are usually the result of unwanted electrochemicalprocesses at the electrodes, generating potentials that disturb or obscure the signal ofinterest. Dc potentials caused by electrode polarization and “injury” currents limit the gainthat can be given to input stages so as to keep them away from saturation. In addition, theeffect of changes in electrode contact, temperature, and hydration induce slow changes inthe level of polarization, which shows in dc-coupled biopotential recordings as baselinewander.
Figure 2.3 The output of the ISO107 isolation amplifier is fed to IC2B, which has its gain selectable through switch SW3. The circuit builtaround IC2A nulls dc offsets automatically when SW1 is closed. The features of this biopotential amplifier make it an ideal choice for recordingcardiac monophasic action potentials (MAPs) using electrodes in direct contact with the heart.45
46 B<strong>AND</strong>PASS SELECTION FOR BIOPOTENTIAL AMPLIFIERSIn the biopotential amplifier of Figure 2.4, dc and very low frequency potentials are preventedfrom propagating beyond the front-end amplifier through a technique commonlyreferred to as dc rejection. In the circuit, signals picked up by electrodes attached to thepatient’s skin are dc-coupled and amplified by IC1, a Burr-Brown INA110 instrumentationamplifier IC. The gain of the front-end stage is programmable between unity and 500 byjumpers JP11–JP14. Potentiometer R17 is used to trim the input offset to IC1. Since IC1is dc-coupled, care must be exercised in the selection of gain so that the amplifier is notsaturated by dc offset voltages accompanying the biopotential signal. For example, to usethis circuit as part of a surface ECG amplifier, the gain must be calculated to cope withoffset potentials of up to 300 mV. In general, IC1’s gain should be kept low so thatdc-coupling does not result in its saturation.To reject dc, IC4C together with R11 and C17 are used to offset IC1’s reference tosuppress a baseline composed of components in the range dc to 0.48 Hz. Once the dc componentis removed, the dc-free biopotential signals are amplified via IC4A and IC4B.Notice that we used clipping diodes at the inputs and feedback paths of this specific implementation.Our application involved measuring the small electrical response of cardiaccells after the delivery of large stimuli. If you build this circuit, you may chose to leaveD4–D7 and D9–D12 out of the circuit.Galvanic isolation is provided by IC2, a Burr-Brown ISO107 isolation amplifier IC. Inaddition to providing a signal channel across the isolation barrier, the ISO107 has an internaldc–dc converter which powers the isolated side of the ISO107 circuitry as well as providingisolated power (15 V at 15 mA typical) for the rest of the circuitry of the isolatedfront end (i.e., IC1 and IC4). The output gain of IC2 is selected through jumpers JP4–JP6to provide gains of 1, 10, or 100. IC3’s output is then low-pass filtered by IC3.AC-COUPLED INSTRUMENTATION BIOPOTENTIALAMPLIFIER FRONT ENDThe circuit of Figure 2.5 embodies the classic implementation of a medium-impedance(10-MΩ) instrumentation biopotential amplifier based on the popular AD521 ICIA byAnalog Devices. The gain of this circuit is adjustable between 10 and 1000 and maintainsa CMR of at least 110 dB. This circuit offers superior dynamic performance with a minimalac-coupled signal bandwidth (3 dB) of 40 kHz and low noise (1 µV p-p at G 10,0.1–100 Hz). This circuit is an example of a biopotential amplifier front end suitable forrecording EMG or ECG signals or as a general-purpose high-impedance ac-coupled transduceramplifier.The heart of the circuit is IC1, the monolithic IC instrumentation amplifier. Biopotentialsare ac-coupled to the amplifier’s inputs through C1 and C2. Although instrumentation amplifiershave differential inputs, bias currents would charge stray capacitances at the amplifier’sinput. As such, resistors R1 and R2 are required to provide a dc path to ground for the amplifier’sinput bias currents. These resistors limit the impedance of each input to 10 MΩ referredto ground. The high-pass filter, formed by the ac-coupling capacitor and the bias shunt resistoron each of the ICIA’s inputs, has a 3-dB cutoff frequency of 0.12 Hz.The gain of IC1 is determined by the ratio between R3 and R4. Using a 20-kΩ multiturnpotentiometer, and given that the value of the range-setting resistor R3 is 100 kΩ, thedifferential gain of the amplifier can be trimmed between 5 and 1000. The output offset ofthe amplifier can be trimmed through R5, which, at any given gain, introduces an outputoffset equal and opposite to the input offset voltage multiplied by the gain. Thus, the totaloutput offset can be reduced to zero by adjusting this potentiometer. The instrumentationamplifier provides a low-impedance output (0.1 Ω) with a permissible swing of 10 V andcan source or sink up to 10 mA.
Figure 2.4 Dc and very low frequency potentials are prevented from propagating beyond the front-end amplifier through a technique commonlyreferred to as dc rejection. Here, IC4C, together with R11 and C17, are used to offset IC1’s reference to suppress a baseline composedof components in the range dc to 0.48 Hz.47
48 B<strong>AND</strong>PASS SELECTION FOR BIOPOTENTIAL AMPLIFIERS+VccD1J2123-Vcc+VccC10.1uFR3100K, 1%1N4148C310uF, 25V, tant.+C40.01uFGainR420K13 108 142 12AC1 In+In-InAC2 InJ112345R110M, 1%R210M, 1%1113+-IC171 2J3OutputAD521JD564C20.1uFR510KOffsetC50.01uF+D21N4148C610uF, 25V, tant.Figure 2.5 This is a classic medium-impedance (10-MΩ) instrumentation biopotential amplifier based on the popular Analog Devices’AD521 ICIA. The gain is adjustable between 10 and 1000 and maintains a CMR of at least 110 dB. The 40-kHz signal bandwidth makesthis front end suitable for recording EMG or ECG signals or as a general-purpose high-impedance ac-coupled transducer amplifier.-VccSupply voltage to the AD521 must be symmetrical and within the range 5 V (minimum)to 18 V (absolute maximum). D1 and D2 provide protection against incorrect supplyvoltage polarity, and capacitors C3–C6 are used to decouple and filter the powersupply. With a quiescent maximal supply current of 5 mA, a pair of 9-V alkaline batteriesconstitute a suitable power supply for most applications.To minimize electrical interference the circuit should be built with a compact layout onan appropriate PCB or small piece of strip board. The construction of the circuit is straightforward,but care must be taken to keep wiring as short and clean as possible. Preferably,leads to the bioelectrodes should be low-loss low-capacitance coaxial cables, whoseshields are connected to the subject ground terminal of the circuit. The construction ofsystems incorporating this circuit is simple, but care must be taken to keep all wiringas short and as clean as possible. When connected to a test subject, the circuit must always
PASSIVE FILTERS 49be powered from batteries or through a properly rated isolation power supply. The sameisolation requirements apply to the output of the amplifier.BOOTSTRAPPED AC-COUPLED BIOPOTENTIAL AMPLIFIERDirect ac coupling of the instrumentation amplifier’s inputs by way of RC high-pass filtersacross the inputs degrades the performance of the amplifier. This practice loads the inputof the amplifier, which substantially lowers input impedance and degrades the CMRR ofthe differential amplifier. Although unity-gain input buffers can be used to present a highinputimpedance to the biopotential source, any impedance mismatch in the ac coupling ofthese to an instrumentation amplifier stage degrades the CMR performance of the biopotentialamplifier.Suesserman has proposed an interesting modification of the standard biopotential instrumentationamplifier to yield an ac-coupled differential amplifier that retains all of the superiorperformance inherent in dc-coupled instrumentation amplifier designs. The circuit ofFigure 2.6 is described by Suesserman [1994] in U.S. patent 5,300,896. If capacitors C3 andC4 were not present, the circuit of Figure 2.6 would be very similar to that of the ac-coupledinstrumentation amplifier described earlier in the chapter. ICIA IC1 without C3 and C4would be ac-coupled to the biopotential signal via capacitors C1 and C2. Just as in the earlierac-coupled biopotential amplifier, resistors R1, R2, R3, and R4 are needed to provide a dcpath to ground for the amplifier’s input bias currents. In this circuit, these resistors wouldlimit the ac impedance of each input to 2 MΩ (R1 R2 and R3 R4) referred to ground.With C3 and C4 as part of the circuit, however, ac voltages from the outputs of theICIA’s differential input stage are fed to the inverting inputs of their respective amplifiers.This causes the ac voltage drop across R1 and R4 to be virtually zero. Ac current flowthrough resistors R1 and R4 is practically zero, while dc bias currents can flow freely toground. This technique is known as bootstrapping, referring allegorically to the way inwhich the amplifier nulls its own ac input currents, as when one pulls his or her own bootstrapsto put boots on.Since bootstrapping capacitors C3 and C4 almost completely eliminate ac current flowthrough R1 and R4, the input current through ac-coupling capacitors C1 and C2 would alsodrop close to zero, which by Ohm’s law translates into an almost infinite input impedance(since R V/i; R tends to ∞ as i approaches 0). Suesserman described this biopotentialamplifier as having an impressive 120-dB CMRR (at 100 Hz) with an input impedance ofmore than 75 MΩ.PASSIVE FILTERSThe simplest filters are those that comprise only passive components. These filters containsome combination of resistive (R), capacitive (C), and inductive (L) elements. The inductiveand/or capacitive components are required because these elements present varying impedanceto ac currents at different frequencies. As a refresher, you may remember that inductivereactance increases with frequency, whereas capacitive reactance decreases with frequency.Most passive filters used in the processing of biopotential signals are the resistive–capacitiveor RC kind. This is because relatively large and heavy inductors would be required toimplement filters at the low-frequency bands where biopotential signals reside, makinginductive–capacitive (LC) filters impractical.Despite their simplicity, RC filters are very common and effective in processing a widevariety of biopotential signals. Take, for example, the complete biopotential amplifier
50 B<strong>AND</strong>PASS SELECTION FOR BIOPOTENTIAL AMPLIFIERS+15VC50.01uFC11uFR11M11312IC1-ING=100G=20050-+-+20K8V+10K-IN+INJ112R21MR31MC31uFC41uF11163G=500RG1RG2VB20K10K-+10K10KSENSEOUTREF109612J2VOUTCOMMC21uFR41M2+IN50+-+-AD624V-7C60.01uF-15VFigure 2.6 This bootstrapped design yields an ac-coupled differential amplifier that retains all of the superior performance inherent in dccoupledinstrumentation amplifiers. Ac voltages from the outputs of the ICIA’s differential input stage are fed to the inverting inputs of theirrespective amplifiers via C3 and C4. This causes the ac voltage drop across R1 and R4 to be virtually zero. Ac current flow through resistorsR1 and R4 is practically zero, while dc bias currents can flow freely to ground.presented in the schematic circuits of Figures 2.7 through 2.12. In this design, biopotentialsignals are amplified by IC5, a Burr-Brown INA128U instrumentation amplifier.Its gain is fixed at 138 through resistor R7. The input of the amplifier is protectedfrom high-voltage transients and electrosurgery currents by a network of resistors,capacitors, and diodes. Back-to-back zener diodes D2 and D4 clamp high-voltage transientsinduced into the electrodes by defibrillation currents to a level that can be handledby the rest of the protection network. C21 acts as a shunt for radio-frequency currentsthat may be induced into the electrodes and leads by sources of electromagnetic interference.This capacitor by itself has inherent filtering capability for high-frequency alternatingcurrent because capacitive reactance X C (in ohms) is inversely proportional tofrequency:1X C 2π fC
INVERTING INPUTD2BZD27C11D4BZD27C11NON-INVERTING INPUTC214.7nFR547kD3HSMS2802R947k231R647kC22470pFR1047k5V_ISOC20100nF2.5V_ISOIIR7360R8100kC231uFC24220nFC30560nFC2547nFC31100nFC3222nFC2610nFC274.7nFA6 A7A5 A8A4 A9A3 A10A2 A11A1 A12C28R4 1MI2.2nF2374 8-+327 1+-4 8 5IC5INA128U665V_ISOC29100nFISW1ASW ROTARY 2P-12WIC4UPC4250G2LOW PASS 1Hz 1LOW PASS 2Hz 1LOW PASS 5Hz 1LOW PASS 10Hz 1LOW PASS 20Hz 1LOW PASS 50Hz 1LOW PASS 100Hz 1LOW PASS 200Hz 1LOW PASS 500Hz 1AIB1 B2 B B12B11B3 B4 B5 B10B9B8B6 B7LOW-PASS FREQ.CUT-<strong>OF</strong>F SELECTIONSW1BSW ROTARY 2P-12WC33 C36 C34 C37 C35 C38 C39 C41 C401uF 560nF 220nF 100nF 47nF 22nF 10nF 4.7nF 2.2NFR121 MSW2First Order (Open) / Second Order (Closed) SelectorR11100kI234 8-+6IC6UPC4250G2LOW PASS OUT75V_ISOIC42100nFFigure 2.7 In this biopotential amplifier, biopotentials are amplified by a Burr-Brown INA128U instrumentation amplifier. R5, R6, R9,R10, and C22 implement a low-pass filter with a cutoff of approximately 3.6 kHz. The biopotential amplifier’s main low-pass filters areimplemented by two cascaded RC passive filters with selectable cutoff frequency. IC4 buffers the signals between the cascaded sections. Thetwo RC sections are identical, therefore setting a pole at the same frequency. However, the effect of the second RC can be suppressed by disconnectingits capacitor through switch SW2.51
52 B<strong>AND</strong>PASS SELECTION FOR BIOPOTENTIAL AMPLIFIERSAs such, this capacitor is practically a short circuit for RF currents, while it leaves lowfrequencysignals pass unimpeded.R5, R6, R9, R10, and C22 implement a low-pass filter. Because of the virtual-groundproperty governing the inputs of an op-amp, we can assume that the low-pass characteristicsof this filter are given by a 94-kΩ resistor (either R5 and R6 in series, or R9 andR10 in series) and the 470-pF capacitor. The 3-dB cutoff frequency for an RC low-passfilter isf 3dB 2π1RC which provides the input network with a first-order low-pass cutoff of approximately3.6 kHz.The biopotential amplifier’s main low-pass filters are implemented by two cascaded RCpassive filters. An op-amp unity-gain follower (IC4) buffers the signals between the cascadedsections. Both RC sections are identical, therefore setting a pole at the same frequency.However, the effect of the second RC can be suppressed by disconnecting itscapacitor through switch SW2. When SW2 is open, signals at the output of IC4 are fed tounity-gain buffer IC6 through R11. Since the input impedance of IC6 is practically infinite,R11 has no effect on the signal. However, when SW2 is closed, R11 and the capacitorselected by SW1B form a low-pass filter. The nominal cutoff frequencies that can beselected for the second-order filter were selected to be close to 1, 2, 5, 10, 20, 50, 100, 200,and 500 Hz. The exact 3-dB cutoff frequencies are shown in Table 2.3.The high-pass filters are implemented in essentially the same way as the low-pass sections.In Figure 2.8, however, the RC elements are reversed. Each high-pass section has acapacitor (C50 and C53) which opposes current flow with an impedance that variesinversely with frequency, and a resistor of selectable value that shunts the load. Both RCsections are identical, therefore setting a pole at the same frequency. However, the effectof the second RC can be suppressed by shorting C53 through SW5. Op-amp IC13 buffersthe signal between the stages. The nominal cutoff frequencies that can be selected for thesecond-order filter were selected to be close to 1, 2, 5, 10, 20, 50, 100, 200, and 500 Hz.The exact 3-dB cutoff frequencies are shown in Table 2.4.The first follower (IC13) in the high-pass filter is implemented using a LTC1152 insteadof a UPC4250 op-amp as in the case of the other followers because higher current outputis required to drive the lowest resistor values associated with the highest 3-dB cutoffTABLE 2.3 Low-Pass 3-dB Cutoff Frequencies for the BiopotentialAmplifier of Figure 2.7 Selected through SW1 a3-dB Cutoff Frequency for 3-dB Cutoff Frequency forSecond-Order Low-Pass Filter First-Order Low-Pass FilterSW1 Position (Hz) (SW2 Closed) (Hz) (SW2 Open)1 1.02 1.592 1.83 2.843 4.65 7.234 10.22 15.925 21.75 33.866 46.47 72.347 102.2 159.28 217.5 338.69 464.7 723.4aSW2 selects between first- or second-order response.
C50100nFR322.4MR28470KR351.2MR36240KR29120R3051KR3424KA6 A7A5 A8A4 A9A3A2A1B1B2B3ABR3112KA10A11A12B4 B9B5 B8B6 B75V_ISOSW4ASW ROTARY 2P-12WIB12B11B10R335.1KSW4BSW ROTARY 2P-12WI234-+7 8High-PassFrequencyCutoffSelection6C51100nFIIC13LTC1152CS8C52100nFFirst Order(Open)/Second Order(Closed) SelectorSW5C53100nFR46 12MHIGH PASS 1Hz 1HIGH PASS 2Hz 1HIGH PASS 5Hz 1HIGH PASS 10Hz 1HIGH PASS 20Hz 1HIGH PASS 50Hz 1HIGH PASS 100Hz 1HIGH PASS 200Hz 1HIGH PASS 500Hz 1I2374 8-+65V_ISOIC54100nFIC14UPC4250G2HIGH PASS OUTR372.4MR431. 2MR38470KR41240KR39120KR4451KR4024KR4212KR455.1KFigure 2.8 The high-pass filters for the amplifier of Figure 2.7 are implemented in essentially the same way as the low-pass sections. Eachhigh-pass section has capacitors (C50 and C53) which oppose current flow with an impedance that varies inversely with frequency and aresistor of selectable value that shunts the load. The RC sections are identical, therefore setting a pole at the same frequency. However, theeffect of the second RC can be suppressed by shorting C53 through SW5. Op-amp IC13 buffers the signal between the stages.LOW PASS OUT53
54 B<strong>AND</strong>PASS SELECTION FOR BIOPOTENTIAL AMPLIFIERSTABLE 2.4 High-Pass 3-dB Cutoff Frequencies for the BiopotentialAmplifier of Figure 2.8 Selected through SW4 a3-dB Cutoff Frequency for 3-dB Cutoff Frequency forSecond-Order High-Pass Filter First-Order High-Pass FilterSW4 Position (Hz) (SW5 Open) (Hz) (SW5 Closed)1 1.03 0.662 2.06 1.333 5.27 3.394 10.32 6.635 20.65 13.266 48.59 31.217 103.3 66.318 206.5 132.69 485.9 312.1aSW5 selects between first- or second-order response.frequencies when SW5 is closed. Figure 2.9 shows the notch filters that are used to filterpower line interference. More detail will be presented on notch filters later in the chapter.Suffice it to say for now that one filter (built around IC15 and IC17) has a notch at around50 Hz, while the other (built around IC16 and IC18) has a notch at 60 Hz. Trimmers R59and R60 are used to fine-tune the notch frequency, while R57 and R58 select the notchdepth.The circuit of Figure 2.10 can be made to process the output signal coming outof the notch filters. This circuit performs full-wave rectification on the input signal.Zero-threshold rectification is achieved by placing the rectifier diodes (D6) within thefeedback loop of op-amp IC11. Full-wave rectification results from adding an invertedhalf-wave-rectified signal at double amplitude to the original signal in the summingamplifier IC12. Full-wave rectification is an operation that is often used when the desiredinformation can be extracted by analyzing the energy conveyed by the biopotential signal.For example, the EMG signal is often rectified and then low-pass-filtered to yield asignal proportional to the force generated by a muscle. The full-wave rectifier can bebypassed through SW3.The signal is then buffered by IC10 in Figure 2.11 before it is optically isolated fromrecording instruments connected at output connector J2. Galvanic isolation ensures that thesource of biopotential signals (e.g., a patient) is not exposed to dangerous currents leakedfrom power lines through the subject’s heart. This function is implemented through aHewlett-Packard HCNR201 high-linearity analog optocoupler. This optocoupler includesone LED and two photodiodes, the output photodiode and an input photodiode designedto receive the same light intensity from the LED as the output photodiode. The LED currentis controlled through a feedback loop so that the current at the input photodiode isproportional to the voltage of the analog signal at the input of IC10. Under the hypothesisthat both photodiodes receive the same light intensity, the current at the output photodiodealso follows the input analog signal.Op-amp IC8 and capacitor C43 integrate the difference between the current through R18and the current through the input photodiode. The output of this integrator drives the LEDso that these currents are equalized. Therefore, the current through the input photodiode(which will be equal to the current of the output photodiode) is equal to the input analogsignal divided by R18. The analog signal is recovered at the output through the bandwidthlimitedcurrent-to-voltage converter implemented by IC9, R15, and C44. The output of theintegrator of the input stage drives the LED through a constant-transconductance stageimplemented by Q1, R16, R14, R13, and R17.
NOTCH OUTR47100kR48100kR501MR49HIGH PASS OUTR51100k2R5910kR53100k3113R5524.9kR5710k2R6330.1kI23C5510nFI7324 8-+7+-4 8R611MIC15UPC4250G265V_ISOIC17UPC4250G26IC56100nF5V_ISOC59100nFIR52100kR54100k2R6010k3113C5710nFR5634.8kR6424.9kR5810k2I1M23I7324 8-+7+-R621M4 8IC16UPC4250G265V_ISOIC18UPC4250G26C58100nFI5V_ISOIC60100nFC62C61R6630.1k1uFR6524.9k1uF2.5V_ISO2.5V_IS<strong>OF</strong>igure 2.9 Two notch filters are used to reduce power line interference that may be picked up by the amplifier of Figure 2.7. The filter builtaround IC15 and IC17 has a notch at around 50 Hz, while the other (built around IC16 and IC18) has a notch at 60 Hz.55
56 B<strong>AND</strong>PASS SELECTION FOR BIOPOTENTIAL AMPLIFIERS5V_ISO5V_ISO2.5V_ISONOTCH OUTR2110k327 5+-IC11LM425062.5V_ISOR20620k327 5+-IC12LM42506SW3ISO CHANNELOUTR2510k4 8 1IR221M213R241.2MD6HSMS28024 8 1R262.4MIR231MRectifier In/Out SelectorR272.4MFigure 2.10 This circuit can be used to full-wave-rectify the signal at the output of the notch filters of Figure 2.9. This signal-processingoperation is often used in electromyography (EMG) to yield a signal proportional to the force generated by a muscle. The full-wave rectifiercan be bypassed through SW3.Power for the circuit is supplied by the two isolated dc/dc converters (IC2 and IC3)shown in Figure 2.12. 5V_ISO feeds the parts of the circuit that are in galvanic connectionwith the biopotential source, while 5V_DATA_ACQ feeds the analog signal isolator’soutput circuit. IC1 buffers the output of the resistor divider formed by R2 and R3 togenerate a synthetic analog ground halfway between the isolated ground and the isolatedsupply (5V_ISO). The dc/dc converters operate from a single 15-V power supply. Anappropriate choice is a switched ac/dc medical-grade power supply, manufactured byCondor, model GLM75-15.ACTIVE FILTERSPassive filters have their advantages: They consist of simple components, use no gainelements, and require no power supply. Their noise contribution to biopotential signals islimited to the thermal noise from their resistive components, and they can be used in applicationswhich require them to handle large currents and voltages. Despite this, there are manyapplications which require filter functions that a passive filter could not achieve withoutthe use of inductors or which would become cumbersome and impractical because of theinteractions between successive stages. This is where active filters come to the rescue. Activefilters use op-amps, along with resistors and capacitors, to implement the desired filter function.Op-amps can be used to simulate the characteristics of an inductor but without thebulk and expense. In addition, higher-order filters can be implemented with ease becausecascaded stages have little interaction with each other.
5V_ISOQ1MMBT2907AR13120R163.3k5V_ISOC49100nFC4347pFC47R19 1M 100nF5V_ISOIISO CHANNEL OUT234 87-+R172.2kI6IR141.8kC45100nF6IC8LTC1152IC10UPC4250G28I47-+23I2R18221kIC7HCNR20113 64 5GND DATA ACQISOLATION BARRIER >12 mm creepagedistance or 7mm airclearance234-+7 8R15221kC4433pF+5V DATA ACQIC9LTC11526C46100nFC48100nFGND DATA ACQD51BZD27C6V82GND DATA ACQFigure 2.11 The signal at the output of Figure 2.10 is buffered by IC10 and then optically isolated from recording instruments connectedat output connector J2. Galvanic isolation to protect the subject from dangerous leakage currents is done through a Hewlett-PackardHCNR201 high-linearity analog optocoupler.1OUTPUTJ22GND DATA ACQ57
5V_ISOIR25.1MR35.1MIR11M2374 8-+65V_ISOIIC1UPC4250G2C1100nF2.5V_ISOJ121+15VIN+15VINGNDINC2100nFC31nFIC21112 +VIN1 +VOUT1+VIN2 +VOUT2 12231324-VIN1 -VOUT1-VIN2 -VOUT2 14PWR1312AC4100nFC51nF1FL1B2 3PSG CGBNX002-015 6CB4C6100uFC7100nFL1100uHC8100uFC9100nF5V_ISOC101nF5.1V/0.5WD1CGCGISOLATION BARRIERS> 12 mm creepagedistance or 7mm airclearanceI+15V fromMedical-GradePower SupplyC11100nFC121nFIC31112+VIN1 +VOUT1+VIN2 +VOUT212231324-VIN1 -VOUT1-VIN2 -VOUT2 14PWR1312AC13 C14FL2100nF 1nF 14C15BCB2 3PSG CGBNX002-015 6100uFC16100nFL2100uHC17100uFC18100nF+5V DATA ACQC191nFCGCGGND DATA ACQFigure 2.12 Power for the circuit of Figures 2.7 to 2.11 is supplied by two isolated dc/dc converters (IC2 and IC3). 5V_ISO feeds the partsof the circuit that are in galvanic connection with the biopotential source, and 5V_DATA_ACQ feeds the analog signal isolator’s outputcircuit. IC1 generates a synthetic analog ground. The dc/dc converters should be operated from a medical-grade 15-V power supply.58
ACTIVE FILTERS 59Many good books and articles have been written on the design of active filters, and wewill not try to duplicate their efforts. In our view, the books with the most practical approachfor the experimentalist are:• D. Lancaster, Active Filter Cookbook, Synergistics Press, 1995.• P. Horowitz and W. Hill, The Art of Electronics, 2nd ed., Cambridge University Press,New York, 1989.• H. M. Berlin, The Design of Active Filters, with Experiments, Howard W. Sams,Indianapolis, IN, 1974.Designing active filters is not difficult. There are a number of free software packagesthat will take your input parameters and provide you automatically with a schematic diagramand calculate capacitor and resistor values for specific filter implementations. Thisdoesn’t mean that the programs will do everything for you. You still have to decide whattype of filter response and implementation suit your application.Filter response refers to the shape of a filter’s transfer function. Everyone’s first approximationto filtering physiological signals is to assume a frequency-domain rectangularpassband containing the spectral components of interest while excluding potential interferencesources. However, real-world filters do not yield a perfect step in the frequencydomain. In fact, to produce such a response would require an infinite number of poles(implemented through an infinite number of amplifiers, resistors, and capacitors) andwould result in a filter that is inherently unstable in the time domain. Because of these reasons,real-world filters make use of stable approximations to a perfect step in the frequencydomain. Some of the most common filter responses are the Butterworth, Chebyshev, andBessel. Each of these filter responses has advantages and disadvantages, and it is thedesigners task to find a suitable compromise that best fits the task at hand. Table 2.5 summarizesthe frequency- and time-domain characteristics of these filters, and Figure 2.13shows the magnitude and phase responses for fourth-order Chebyshev, Butterworth, andBessel transfer functions with a 3-dB cutoff frequency of 30 Hz.The Butterworth response (also known as maximally flat) is nearly flat in the passbandand rolls off smoothly and monotonically. In addition, it has virtually no ripple in eitherthe passband or the stopband. For these reasons, many designers regard the Butterworthfilter transfer function as the best compromise between attenuation and phase response forgeneral-purpose applications. This transfer function is certainly the most commonly usedin the design of analog biopotential signal filters. Despite this, applications that require aprecise estimation of phase shift are better served by Bessel filters, since its phase shift islinear, a property that is not shared by Butterworth or Chebyshev filters.The next step to designing a filter is to select a suitable implementation. Here again,a compromise has to be made to achieve the desired filter transfer function with realworldanalog components. The most common active filter topologies are describedbelow.TABLE 2.5Characteristics of Some Common Filter Transfer FunctionsTransferFrequency-Domain CharacteristicsTime-Domain CharacteristicsFunction Ripple Stopband Phase Group DelayChebyshev Equal ripple flat Steep Poor PoorButterworth Smooth Moderate Moderate ModerateBessel Maximum smoothness Weak Very flat Very flat
60 B<strong>AND</strong>PASS SELECTION FOR BIOPOTENTIAL AMPLIFIERSAttenuation (dB)100-10-20-30-40-50-60-70-80-90Phase:ChebyshevButterworthBesselMagnitude:ChebyshevButterworthBesselPhase (deg.)-10010 100 1000Frequency (Hz)Figure 2.13 Real-world filters do not yield a perfect step in the frequency domain. Some of the mostcommon filter responses are the Butterworth, Chebyshev, and Bessel. Each of these filter responseshas advantages and disadvantages, and it is the designer’s task to find a suitable compromise that bestfits the task at hand from phase- and amplitude-response graphs such as this one for fourth-order filterswith a 3-dB cutoff frequency of 30 Hz.0-100-200-300-4001. Sallen–Key topology (also known as the voltage-controlled voltage-source topology)uses an op-amp as a gain block. Because of this, the Sallen–Key configuration is relativelyindependent of op-amp specifications and requires the op-amp’s bandwidth only to extendslightly beyond the filter stopband frequency. The Sallen–Key topology features goodphase response, but its frequency response and Q are sensitive to the gain setting.2. Multiple-feedback topology uses op-amps as integrators that need a minimum loopgain of 20 dB (open-loop gain 10 times the closed-loop gain) to avoid Q enhancement, makingit difficult to get high-Q performance. However, this filter configuration is relativelyinsensitive to passive-component values.3. State-variable topology uses op-amps as amplifiers and integrators, which again needa minimum loop gain of 20 dB. In addition, the op-amps need a frequency response that isflat to beyond the stopband frequency. Despite this, state-variable filters provide independentcontrol over gain, cutoff frequency, Q, and other parameters but require more passivecomponents. A very nice feature of this topology is that the same circuit yieldslow-pass, high-pass, and bandpass response.4. Impedance-converter topology (also known as frequency-dependent negative-resistancetopology) requires op-amps with a minimum loop gain of 20 dB at the resonant negativeresistance frequency. Multiple op-amps are needed, and use of dual-packaged devices is recommendedfor matched performance in each leg. FET-input op-amps are used because oftheir low bias currents. Although the impedance-converter approach requires more components,it is relatively insensitive to variations in their values.Since biopotential signal filtering applications commonly have bandwidths limited to theaudio range, the biggest trade-off is often the number of op-amps versus the level of controlthat a designer has over the filter. For a person inexperienced with the design of active filters,
ACTIVE FILTERS 61we recommend that you try the two and three op-amp topologies that will allow you moreability to “tweak” the end result. In addition, a good way of designing well-behaved filters isto base them on one of the various active filter building blocks offered by analog IC vendors.For example, Burr-Brown (now part of Texas Instruments) offers the UAF42, a universalactive filter that can be configured for a wide range of low-pass, high-pass, and bandpassfilters. It implements filter functions through a state-variable topology with an invertingamplifier and two integrators. The integrators include on-chip 1000-pF capacitors trimmedto 0.5%. This solves the difficult problems of obtaining tight-tolerance low-loss capacitors.The UAF42 is available in 14-pin DIP and SOL-16 surface-mounted packages.Burr-Brown’s free DOS-compatible FilterPro program lets you design Butterworth,Chebyshev, and Bessel filters, enter the desired performance, and then obtain the passivevalues required. You can force the program to use the nearest 1% resistors, set some resistorvalues, enter realistic or measured capacitor values, and then plot the actual gain/phase versusfrequency performance. Similarly, Microchip’s Windows-based FilterLab lets you designSallen–Key or multiple-feedback low-pass filters with either Butterworth, Chebyshev, orBessel responses using their MCP60x family of single-supply op-amps.Maxim also offers a line of state-variable filter ICs, the MAX274 and MAX275. TheseICs have independent cascadable second-order sections that can each implement all-polebandpass or low-pass filter responses, such as Butterworth, Bessel, and Chebyshev, and isprogrammed by four external resistors. The MAX274 has four second-order sections, permittingeighth-order filters to be realized with center frequencies up to 150 kHz. TheMAX275 has two second-order sections, permitting fourth-order filters to be realized withcenter frequencies up to 300 kHz. Both filters operate from a single 5-V supply or fromdual 5-V supplies. A free DOS-based filter design program is available from Maxim tosupport the development of applications based on the MAX274 state-variable filter IC.State-variable filter realizations have the distinct advantage that they provide simultaneouslow-pass, bandpass, and high-pass outputs from the same filter circuit. In addition,the filter parameters are independent of each other. For example, the cutoff frequency ofthe active-feedback state-variable filter circuit of Figure 2.14 is given by1f C 2π(R3 )(C1)where R3 R4 and C1 C2. As shown in the ac-sweep PSpice simulation analysis ofFigure 2.15, this filter yields simultaneous low-pass and high-pass responses with a -3-dBcutoff frequency f C and a bandpass response centered at the same frequency. In this example,the resistor values selected for R4 and R6 give the filter a cutoff frequency of approximately50 Hz. The Butterworth response on a state-variable filter gives it a value Q -3 dB and anin-band gain of the bandpass filter equal to Q ( 0.707), making all curves cross at thesame point.Since the cutoff frequency of a state-variable filter depends on the value of two resistors(R3 and R4 in the prior example), it is relatively easy to design a tunable filter by substitutingthese resistors by two tracking variable resistors. The filter can also be made tohave a cutoff frequency that is proportional to a control voltage by using circuits that presenta variable resistance as a function of an input voltage.Although FETs and variable transconductance amplifiers can be used as voltagedependentresistors, better results are easier to achieve using analog multipliers in serieswith a resistor as the control elements. The circuit of Figure 2.16 shows how R3 and R4of the circuit of Figure 2.14 have been replaced by two Analog Devices AD633 precisionanalog multipliers. The transfer function of the AD633 is given byV out (x 1 x 2)(y 1 y 2 ) z10V
62Figure 2.14 State-variable filter realizations have the distinct advantage that they provide simultaneous low-pass, bandpass, and high-passoutputs from the same filter circuit at a 3-dB cutoff frequency f c 1/2π(R3)(C1).
Figure 2.15 A PSpice simulation ac sweep of the state-variable filter of Figure 2.14 yields simultaneous low- and high-pass responses witha 3-dB cutoff frequency f c and a bandpass response centered at the same frequency. In this example, the resistor values selected for R4 andR6 give the filter a cutoff frequency of approximately 50 Hz.63
64Figure 2.16 Since the cutoff frequency of a state-variable filter depends on the value of two resistors, it is possible to design a voltagecontrolledtunable filter by substituting these resistors by two circuits that present a variable resistance as a function of an input voltage.For example, Analog Devices’AD633 precision analog multipliers can be configured such that the apparent impedance between x 1 and theiroutput is proportional to the control voltage at y 1 . This makes the cutoff frequency of the high- and low-pass filter outputs as well as thecenter frequency of the bandpass section be f c (control voltage)/20π(R3)(C1).
50/60-Hz NOTCH FILTERS 65where z is an offset input. In the tunable filter of Figure 2.16, the AD633 is configured suchthat the apparent impedance between x 1 and the output is proportional to the control voltageat y 1 . This makes the cutoff frequency of the high- and low-pass filter outputs, as wellas the center frequency of the bandpass section,f c c ontrolvoltage20π(R3)( C1)PSpice simulation results shown in Figure 2.17 demonstrate the effect of varying the controlvoltage presented to the y 1 inputs of the AD633s. Although the circuit is shown set upfor PSpice simulation, it can be built using real components. Output buffering using Burr-Brown BUF634 buffers make this a very useful stand-alone lab instrument that can be usedto filter amplified biopotential signals selectively prior to recording. A digitally programmableversion of the tunable filter can be made by substituting two multiplying D/A convertersfor the AD633s. In this case, the control voltage is replaced by a digital controlword supplied to the input of the D/A converters.50/60-Hz NOTCH FILTERSProbably the most common problem in the detection and processing of biopotential signalsis power line interference. Sixty hertz (50 Hz in Europe) and its harmonics manages to creepinto low-level signals despite the use of differential amplification methods and active bodypotential driving which attempt to eliminate common-mode signals. Unfortunately,50/60 Hz falls right within the band where biopotentials and other physiological signalshave most of their energy. The usual solution to reject unwanted in-band frequencies is thenotch filter.As shown in Figure 2.18, simple implementation of a notch filter known as a twin-T filterrequires only three resistors and three capacitors. If C1 C3, C2 2C1, R1 R3, andR2 R1/2, the notch frequency occurs where the capacitive reactance equals the resistance(X C R) and is given by1f notch 2π(R1 )(C1)As such, the twin-T notch filter works by phase cancellation of the input signal. When thephase shift in the two sections is exactly 90 and 90, the tuned frequency is canceledcompletely. Signals passed by the filter will experience some distortion since the twin-Tnotch shifts the phase of low-frequency components ( f notch ) by 90 and high-frequencycomponents (f notch ) by 90. The insertion loss of the filter will depend on the load thatis connected to the output, so the resistors should be of much lower value than the load forminimal loss. The depth and width of the response can be adjusted somewhat with thevalue of R2 and by adding some resistance across the capacitors.Twin-T notch filters can achieve very good suppression at their center frequency.However, the use of precise and tightly matched components is extremely important toyield a deep notch at the required frequency. The depth of the notch is defined as the outputsignal ratio between an out-of-notch component and a component at the notch frequency.In practice, a twin-T notch built with tightly matched components can yield prettygood notch-frequency attenuations. Passive notch filters can be built into small enclosuresand placed between equipment stages. For example, the notch filter of Figure 2.19 wasbuilt inside a Pomona Electronics model 2391 box, which comes with BNC connectors oneach end, making it easy to place it at the input of oscilloscopes and signal recorders.For most practical applications, however, an op-amp needs to be added to the twin-Tnetwork to increase its notch depth as well as to make it insensitive to the impedance of
66Figure 2.17 PSpice simulation results of the voltage-tunable state-variable filter of Figure 2.16 demonstrate the effect of varying the controlvoltage presented to the y 1 inputs of the AD633s: (a) a cutoff frequency of 50 Hz at 1-V shifts to (b) 300 Hz at 6 V.
Figure 2.17 (Continued)67
68 B<strong>AND</strong>PASS SELECTION FOR BIOPOTENTIAL AMPLIFIERSR1RC22CR3RINPUTOUTPUTC1R20.5RC3CCFigure 2.18 The notch frequency of the simple twin-T filter is f notch 1/2π(R1)(C1) if C1 C3, C2 2C1, R1 R3, and R2 R1/2.However, the use of precise and tightly matched components is extremely important to yield a deep notch at the required frequency.Figure 2.19 Passive notch filters can be built into small enclosures with BNC connectors on eachend and placed between equipment stages.the output load. The circuit of Figure 2.20 shows how a unity-gain follower bootstraps thenetwork in an active twin-T notch filter. Since output of the op-amp presents a very lowimpedance, the notch frequency and depth are not changed. However, the Q value of thefilter increases proportionately to the level of signal that is fed back to the junction of R2and C2 (the point that is grounded in a passive twin-T notch filter).A very high Q value is not always desirable to filter power line interference. The powerline frequency in many countries deviates quite a bit from the nominal 50 or 60 Hz. A secondop-amp can be added as shown in Figure 2.21 to control the Q value of the filter. Here,the amount of feedback that is provided to the R2/C2 junction is set by potentiometer R4.An op-amp is needed to buffer the feedback signal to ensure a constant low impedance atthe R2/C2 junction so that the notch frequency and depth do not change as a function ofthe potentiometer setting.
50/60-Hz NOTCH FILTERS 69R1RR3R+12VINPUTC22C7 132+-IC1TL0816OUTPUT4 5C1R20.5RC3-12VGNDCCGNDFigure 2.20 An op-amp in unity-gain configuration can be added to the twin-T network to increase its notch depth as well as to make itinsensitive to the impedance of the output load. Since the output of the op-amp presents a very low impedance, the notch frequency and depthare not changed. However, the Q value of the filter increases proportionately to the level of signal that is fed back to the twin-T.INPUTR1RC22CR3R+12V832+-IC1ATL0821OUTPUTC1R20.5RC34-12VCCGNDGND-12VIC1BTL08274-+6550kR4Q-Adjust8Figure 2.21 An op-amp can be added to the filter of Figure 2.20 to control the Q value of the filter by changing the amount of feedbackthat is provided to the twin-T. The op-amp is needed to buffer the feedback signal to ensure a constant low impedance at the twin-T so thatthe notch frequency and depth do not change as a function of the potentiometer setting.+12V
70 B<strong>AND</strong>PASS SELECTION FOR BIOPOTENTIAL AMPLIFIERSAnother popular notch filter is the gyrator filter. This is the type of notch filter that wasimplemented for the biopotential amplifier of Figure 2.9. For the sake of clarity, one notchfilter section has been redrawn, simplified, and relabeled in Figure 2.22. In essence, theproperties of an inductor are simulated by a simple op-amp circuit called a synthetic inductoror gyrator. The impedance at the noninverting input of the synthetic inductor op-ampR1-V100kINPUTR2100kR3100k42 -3 +C110nF8+VIC1A1GENERIC OP-AMP(i.e. 1/2 TL-082)OUTPUTR424.9k321R510kGENERIC OP-AMP(i.e. 1/2 TL-082)+VIC1B.+V.1R610k2568+-7328+-1R=RA+RB3R730.1kC21uF4-VRAC4-VL=CxRAxRBR830.1kRBSYNTHETICINDUCTORFigure 2.22 The properties of an inductor are simulated in this notch filter by a simple op-amp circuit called a synthetic inductor or gyrator.The impedance at the noninverting input of the synthetic inductor op-amp is equivalent to that of an inductor L CR A R B in series witha loss resistance R R A R B . For the values shown in the circuit, the equivalent inductance has an approximate value of 900 H, yielding anotch frequency of11f notch 53 Hz2π LC 2π(900H)( 10nF)The output of IC1A tracks the filter’s input except for signals close to the notch. The depth of the notch is controlled via R5, while the exactnotch center frequency can be trimmed via R6.
HARMONIC ELIMINATOR 71is equivalent to that of an inductor L CR A R B in series with a loss resistance R R A R B .For the values shown in the circuit, the equivalent inductance has an approximate value of900 H. When this inductor is placed in series with a 10-nF capacitor (C1), ac signals reachingthe noninverting input of op-amp IC1A are shunted to ground via the series resistances(R4 R5 R6 R7 R8) only for frequencies close to1 2π LC12π(900H)( 10nF)53 HzThe output of IC1A tracks the filter’s input except for signals close to the notch. The depthof the notch is controlled via R5 (lower value deeper notch), while the exact notch centerfrequency can be trimmed via R6.Yet another approach to the design of a notch filter is to combine a low- and a high-passfilter to yield a filter that excludes only notch frequencies from its bandpass. You will recallfrom our earlier discussion that a state-variable filter produces simultaneous high-pass,low-pass, and bandpass outputs. Looking at the intersection of the low- and high-pass outputsof the state-variable filter shown in Figure 2.15, it is easy to see how an additionalop-amp configured to sum the high-pass output with the low-pass output would yield a signalnotched at the common cutoff frequency. The circuit of Figure 2.23 shows a notch filterimplemented using a Burr-Brown UAF42 state-variable filter IC. This IC incorporatesprecision 1000-pF capacitors for the op-amp integrators and an auxiliary op-amp that isused to sum the low- and high-pass outputs. As such, all that is needed to implement anotch filter with this IC are five external resistors. The notch frequency is set via R1 andR2 (where R1 R2) and is given by1f notch 2π(R1)( 1000 pF)Whatever notch filter you chose to use, you must remember that the notch filter will notonly remove the power line interference but will also take away parts of the signal of interest.In addition, the notch filter may introduce nonlinear phase shifts in frequency componentswithin the filter’s passband.Take, for example, applications that require very subtle analysis of the ECG signal.Arbitrary removal of power line frequency signals may not pose a problem for standardECG signals since the main frequency components of P-, R-, and T-waves are far below60 Hz. However, when ECGs are examined for small variations that are indicative of scartissue due to previous myocardial infarction, removal of power line interference has to bedone with utmost care not to eliminate or distort the ventricular late potentials, microvoltlevel(1 to 20 µV) waveforms that are continuous with the QRS complex, last into the STsegment, and occupy a relatively wide frequency band (40 to 200 Hz) that peaks exactlywithin the range 50 to 60 Hz.HARMONIC ELIMINATORUnfortunately, power line interference is not limited to 50 or 60 Hz. Fluorescent lights,dimmers, and other nonlinearities introduce powerful components at the harmonics of thepower line frequency. A number of independent notch filters at 60, 120, 180 Hz, and so on(or their 50-Hz counterparts), could be cascaded to yield a comb filter to eliminate powerline interference at the main frequency and its harmonics. However, an n-path filter is abetter way than this of implementing a comb filter. This filter implementation generates thenecessary poles by switching a sequence of capacitors in synchronism to the power linefundamental frequency.
OUTOutputOut GND6R42kIC 1UAF42 8High-pass Out13R12.65MBand-pass Out7R22.65M14Low-pass Out1R32k5R512.1kR_i150kR_i250kC_i11000pFC_i21000pF-+-+-+-+2R_i350kR_i450k3R64.99kC10.01uF910C20.01uF114++C310uF-15V+15VC410uFFigure 2.23 Summing the high-pass output with the low-pass output of a state-variable filter yields a signal notched at the common cutofffrequency. The Burr-Brown UAF42 state-variable filter IC incorporates precision 1000-pF capacitors for the op-amp integrators and an auxiliaryop-amp that can be used to sum the low- and high-pass outputs. All that is needed to implement a notch filter with this IC are five externalresistors. The notch frequency is1f notch 2π(R1)( 1000 pF) if R1 R2InInputIn GND72
The simplified circuit of Figure 2.24 can be used to explain the process by which sucha filter operates. Here, eight capacitors are switched to ground in synchronism with thepower line, making this circuit an eight-path filter. A power line sample obtained fromtransformer T1 and coupled through R8 and C14 is fed to a 74HC4046 phase-locked loop(PLL). A PLL consists of a phase comparator, a loop filter, and a voltage-controlled oscillator.In this application, the phase comparator compares the phase and frequency of thepower line sample against those of the internal oscillator and adjusts the oscillator frequencyso that it equals some exact multiple of the incoming reference. A 74HC161 isclocked at 16 times the power line frequency by the output of the PLL’s oscillator, generatingeight digital addresses addresses (on outputs QB–QD) that divide the power linecycle evenly into eight segments. A 74HC4051 is driven by the digital sequence, selectingwhich one of eight capacitors is connected to ground throughout the power line cycle.During the time that one such capacitor is connected to ground, it samples the filter’s inputsignal (the biopotential signal to be comb-filtered, not the power line reference) with a timeconstant given by R2. The output of the eight-path filter is inverted by IC1C and added tothe original input signal to yield the comb response. Please note that IC1D is used to generatea virtual ground at 2.5 V. However, a split power supply would work equally well bysubstituting ground by 2.5 V, 2.5 V by ground, and 5 V by 2.5 V.An intuitive explanation of the comb filter’s transfer function is that the capacitors of then-stage filter charge to a portion of the difference between the current signal voltage and thevoltage integrated over the same time segment on previous power line cycles. Each capacitorcan be assumed to store an average of the signal at the specific time segment of thepower line cycle. Since the components of interest in the signal to be filtered are in mostcases uncorrelated to the power line, the capacitors store only a sample of signal componentslocked to the power line frequency (i.e., the power line fundamental and its harmonicsalong with any other correlated noise). The output signal is then cleaned from repetitivepower line noise when the power line–locked average is subtracted from the input signal.This type of filter has unique advantages over fixed-frequency notch filters. First, thefilter automatically adapts the frequency of its notches to whatever power line frequencyis present at the reference port. Second, the filter does not affect the signal when no interferenceis present. Last, power line–frequency biopotential signal components not lockedto the power line are not affected since this filter excludes only signals that maintain aphase lock to the power line for a number of power line cycles. In addition, unlike thenotch filters described earlier, changes in component values in this circuit have minimaleffect on the filter’s response, making it maintenance free.This filter is not a continous-time system. The use of switched capacitors makes this asampled system that is bound by Nyquist’s sampling theorem. This limits the theoreticalbandwidth of the filter to one-half the sampling frequency. Since the signal is sampledeight times during the power line cycle, the theoretical bandwidth of the filter is four timesthe reference frequency, making it possible to reject only the fundamental, first, and secondharmonics (60, 120, and 180 Hz for a 60-Hz reference). Higher bandwidth with rejectionof higher harmonics requires increasing the number of sampling capacitors. Forexample, a 16-path filter at 60 Hz would have a theoretical bandwidth of 480 Hz.The comb filter of Figure 2.24 needs additional components to reject more noise thanthat which it introduces by its switching action. This is usually accomplished throughvarious bandpass filters placed at the output of the n-stage filter as well as at the outputof the summing amplifier. A family of ready-made universal eliminator modules basedon this principle is available from Electronic Design & Research Inc. Models EDR-82534and EDR-82534A are adaptive comb filters designed specifically for integration withinmedical instrumentation. These modules comprise a 64-path filter and support a signalbandwidth of dc to 500 Hz (EDR-82534) or dc to 1200 Hz (EDR-82534A). Figure 2.25shows the pinout and connection to the module. The module’s internal block diagram isHARMONIC ELIMINATOR 73
-OUTOUTGNDININPUTINGND11R5100k1213+-411IC1D14TL084+2.5VIC274HC4051+5V109+-411IC1CTL0848ABCEN3+ C1010uF+2.5VC110.1uF32+5V+-+5V4R6100kIC1A1TL084R21MC90.1uF+5VC10.1uFC20.1uFC30.1uFC40.1uFN-STAGEFILTERC50.1uFC60.1uFC70.1uFC120.1uFC80.1uF+2.5VR121M+5VR11C181M1000pFR110kR310k+2.5V56+R4+5V41110kIC1B7TL084+2.5V111096167VDDVEEXX0X1X2X3X4X5X6X7131415121524OUTPUTAC HPOWERLINEAC N1T154 8R8330k6.3VACC140.1uFC15 39nFC160.1uFR9100k+5VC130.1uF9314671112 DEMO516CINSINC1AC1BR1R2INHVDDR7330kVCOINVCOUTP1P2P3PP421315110+5V9107126543IC3LOADENTENPCLRCLKDCBARCOQDQCQBQA74HC1611511121314LockPLLR10180kC170.1uFIC474HC4046Figure 2.24 An n-path filter can be used to implement a comb notch filter to filter the power line main frequency and its harmonics. In thiseight-path filter, eight capacitors are switched to ground in synchronism with the power line. The capacitors charge to a portion of thedifference between the current signal voltage and the voltage integrated over the same time segment on previous power line cycles. Sincethe signal of interest is uncorrelated to the power line, the capacitors only store a sample of signal components locked to the power line frequency.The output signal is then cleaned from power line noise when the power line–locked average is subtracted from the input signal.74
OUTOUTPUTOUTGNDIC1EDR-82534A1. .SIGNAL INPUT CIRCUIT2 C_f64C_f1C_f2.. . .SIGNAL OUTPUT CIRCUIT& 1.2kHz FILTER7MULTIPLEXER81T156.3VAC4 8341k13TLP1276PLLCOUNTER4LED PROTECTION+V-V5C18C290.1uFC30.1uFC4++10uF10uF+12V-12VFigure 2.25 Electronic Design & Research Inc.’s EDR-82534 and EDR-82534A are adaptive comb filters designed specifically for integrationwithin medical instrumentation. These modules comprise a 64-path filter and support a signal bandwidth of dc to 500 Hz (EDR-82534)or dc to 1200 Hz (EDR-82534A).ININPUT(10Vp-p max.)INGNDAC HPOWERLINEAC N75
76 B<strong>AND</strong>PASS SELECTION FOR BIOPOTENTIAL AMPLIFIERSpresented by the authors for reference purposes only and is not necessarily what ElectronicDesign & Research places within their “black boxes.” No external components (besidespower supply and reference signal source) are needed to use these modules. These modulesare definitely recommended for applications that can tolerate their size (3.9 in. 2 in.footprint, 1 in. height) and cost ($221 for the EDR-82534 and $324 for the EDR-82534Ain single units).SWITCHED-CAPACITOR FILTERSLately, many designers have opted for switched-capacitor filters as substitutes for continuous-timeactive filters. Switched-capacitor filters allow sophisticated, accurate, and tunableanalog filter circuits to be manufactured without resistors. The advantage of this is thatresistors take up considerable room on integrated circuits and that it is next to impossibleto maintain a consistent absolute resistance value from manufacturing run to manufacturingrun.In Chapter 1 we showed how a sampling capacitor C S , which switches continuouslybetween an input voltage and a hold capacitor C H with a clock period T, acts as a low-passfilter with a 3-dB cutoff frequency defined by the capacitor ratioCH1C 2πfSCapacitor ratios are much easier to maintain from batch to batch of an IC than are preciseresistor values. In addition, resistor values that would be prohibitive for integration caneasily be synthesized through the resistor equivalence of the switched capacitor. Finally,equivalent resistor values can be tuned simply by changing the switching frequency.Commercial switched-capacitor ICs based on the same principle offer complete ornearly complete high-order filters in small, inexpensive packages. By switching the capacitorat around 100 times the corner frequency, these filters can attain a good approximationof theoretical performance. Switched-capacitor ICs are available as complete filters or asuniversal building blocks that require few external capacitors or resistors. Driving clocksmay be internal or external to the filter itself. Varying clock frequency permits programmingfilters “on the fly.”If you are not sure which filter transfer function will work best in your application,switched-capacitor filters can help you try out various possibilities without rewiring yourcircuit. This is because switched-capacitor manufacturers offer filters with the varioustransfer functions in pin-compatible packages. For example, the Maxim MAX290 familyof low-pass filters offers interchangeable chips that implement Bessel, Butterworth, andelliptic-response transfer functions.Switched-capacitor filters do have disadvantages. For one, since a switched-capacitorfilter is a sampling device, it can result in aliasing errors. Frequency components near andabove half the sampling frequency must be eliminated to ensure accuracy. In addition, theoutput of a switched-capacitor filter usually needs to be low-pass filtered with a continuous-timefilter to eliminate clocking signals that always manage to feed through.The use of switched-capacitor filters can present other traps to the designer of biopotentialamplifiers. This is because high-speed clock signals can easily couple to the high-impedanceinputs and ground lines. Furthermore, the internal amplifiers within switched-capacitorfilter ICs can generate noise and harmonic distortion on processed biopotential signals.Regardless of the precautions that one may take in the design, continuous-time activefilters end up being at least 20 to 40 dB quieter than their switched-capacitor counterparts.3dB T
With these warnings in mind, let us look at some of the most popular switched-capacitorfilter choices for processing biopotential signals.1. Maxim MAX280. This IC is a fifth-order all-pole low-pass filter with no dc error,making it an excellent choice for processing low-frequency biopotential signals. As shownin Figure 2.26, the filter IC uses an external resistor and capacitor to isolate the fourthorderfilter implemented within the IC from the dc signal path. The external resistor andcapacitor are used as part of the filter’s feedback loop and also form one pole for the overallfilter circuit. The values of these components should be chosen such that1. 62f cutoff 2π(R 1)(C1)where R1 is usually chosen to be around 20 kΩ.The chip’s internal four-pole switched-capacitor filter is driven by an internal clock thatdetermines the filter’s cutoff frequency. For a maximally flat amplitude response, the clockshould be 100 times the desired cutoff frequency. The internal oscillator runs at a nominalfrequency of 140 kHz that can be modified by connecting an external capacitor (C2)between pin 5 and ground. The clock frequency is given byf clock 140 kHz 33pF33 pF C2 SWITCHED-CAPACITOR FILTERS 77ININPUT(6Vp-p max.)R1OUTOUTPUTINGNDC1OUTGNDIC1C2+5V154763FBCLKDIVRTOOUTV+V-BOUTAGND82R2C3C4MAX2800.1uF0.1uFC5C6++10uF10uF+5V-5VFigure 2.26 The Maxim MAX280 IC is a fifth-order all-pole low-pass filter with no dc error, makingit an excellent choice for processing low-frequency biopotential signals. It uses an external resistorand capacitor to isolate the fourth-order filter implemented within the IC from the dc signal path.The internal switched capacitor filter is driven by an internal clock that determines the filter’s cutofffrequency. If pin 4 is tied to V, the filter has a cutoff frequency ratio of 100 : 1; when tied to ground,200 : 1; and when tied to V, of 400 : 1.
78 B<strong>AND</strong>PASS SELECTION FOR BIOPOTENTIAL AMPLIFIERSA series resistor (R2) can be added to trim the oscillation frequency. In this case, the newclock frequency is given byf R20clockf clock 1 4(R2)(C2) f R20clockwhere f R20 is the oscillator frequency when R2 is not present (obtained through the priorclockequation). Pin 5 of the MAX280 can also be driven from an external clock. In addition, thestate of pin 4 must be taken into account to determine the effective clock frequency. If pin4 is tied to V, the filter has a cutoff frequency ratio of 100 : 1; when tied to ground,200 : 1; and when tied to V-, 400 : 1.2. Maxim MAX29x. This is a family of easy-to-use eighth-order low-pass filters that canbe set up with corner frequencies from 0.1 to 25 kHz (MAX291/MAX292) or 0.1 Hz to50 kHz (MAX295/MAX296). The MAX291 and MAX295 filters provide a Butterworthresponse, while the MAX292 and MAX296 yield a Bessel response. The clock frequencyto-cutofffrequency ratio for the MAX291 and MAX292 is 100 : 1; a ratio of 50 : 1 is usedin the MAX295 and MAX296. As shown in Figure 2.27, an external capacitor is used toset the clock frequency of an internal oscillator according to510f clock (kHz) 3C 1(pF)Of course, the internal clock can also be driven externally. The MAX29x family has aninternal uncommitted op-amp that has its noninverting input tied to ground. This op-ampcan be used to build a continuous-time low-pass filter for prefilter antialiasing or clockattenuation at the switched-capacitor’s filter output.IC1ININPUT(8Vp-p max.)INGND84172INOPIN-CLKV+V-OUTOPOUTAGND536OUTPUTOUTOUTGNDC1MAX291C2C30.1uFC4+10uF0.1uFC5+10uF+5V-5VFigure 2.27 Maxim MAX29x ICs are eighth-order low-pass filters that can be set up with corner frequencies from 0.1 to either 25 or50 kHz with either a Butterworth or a Bessel response. The clock frequency-to-cutoff frequency ratio for the MAX291 and MAX292 is100 : 1; a ratio of 50 : 1 is used in the MAX295 and MAX296. An external capacitor is used to set the clock frequency of an internal oscillatoraccording to f clock (kHz) 10 5 /3C1(pF).
SWITCHED-CAPACITOR FILTERS 793. National Semiconductor MF4 (or Texas Instruments TLC04). This IC is an easy-touse,fourth-order Butterworth low-pass filter. The ratio of the clock frequency to the lowpasscutoff frequency is set internally to 50 : 1. A Schmitt trigger clock input stage allowstwo clocking options, either self-clocking (via an external resistor and capacitor) for standaloneapplications, or for tighter cutoff frequency control an external TTL or CMOS logiccompatible clock can be applied. The MF4-50 applies a 50 : 1 clock to cutoff frequencyratio, while the MF4-100 applies a 100 : 1 ratio. The clock frequency of the circuit shownin Figure 2.28 is given by1f clock 1.69(R 1)(C1)4. National Semiconductor and Maxim MF10. This IC consists of two independent andgeneral-purpose switched-capacitor active filter building blocks. Each block, together withan external clock and three to four resistors, can produce various second-order functions.Each building block has three output pins. One of the outputs can be configured to performeither an all-pass, high-pass, or notch function; the remaining two output pins performlow-pass and bandpass functions. The center frequency of the low-pass and bandpasssecond-order functions can be either directly dependent on the clock frequency, or they candepend on both clock frequency and external resistor ratios. The center frequency of thenotch and all-pass functions depends directly on the clock frequency, while the high-passcenter frequency depends on both the resistor ratio and the clock. Any of the classical filtertransfer functions can be implemented by selecting the right component values. Thespecific design methods and equations for the MF10 are available in the datasheet for theseproducts as well as in National Semiconductor Application Note 307.Other useful universal switched-capacitor filters are Linear Technologies’ LTC1068and the LTC1562 as well as Maxim’s MAX 265 and MAX 266. Maxim also offers twomicroprocessor-programmable universal switched-capacitor filters: the MAX261 andR1ININPUT(8Vp-p max.)INGNDIC18 5FILTIN FILTOUT1374CLKINLSHV+V-CLK RAGND26OUTOUTPUTOUTGNDC2C1C3MF40.1uFC4+10uF0.1uFC5+10uF+5V-5VFigure 2.28 National Semiconductor’s MF4 IC is a fourth-order Butterworth low-pass filter with a clock-to-cutoff frequency ratio of 50 : 1.The clock frequency is set via a capacitor and a resistor according to f clock ≈ 1/1.69(R1)(C1).
80 B<strong>AND</strong>PASS SELECTION FOR BIOPOTENTIAL AMPLIFIERS+5VR256ININPUTINGNDC1IC18 5FILTIN FILTOUT1374CLKINLSHV+V-MF4R1CLK RAGND26C70.01uFC60.01uF7 83+2-4 1 5R3566IC2AD620OUTHIGH-PASS OUTPUTOUTGNDC2C3-5V0.1uF0.1uFC4C5+10uF+10uFLOW-PASSFILTER+5V-5VFigure 2.29 An instrumentation amplifier can be used to convert a low-pass filter into its high-pass counterpart. In this example, the inputsignal is fed to the AD620 instrumentation amplifier both directly and through the low-pass filter. This results in a high-pass function, sincethe output of the amplifier is the original signal minus the attenuated low-frequency components.MAX262. One thing that you won’t find with ease is a high-pass version of the low-pass filterchips (such as the MAX280 or the MF4). However, there is an alternative to using a universalfilter IC. Figure 2.29 shows how an instrumentation amplifier can be used to convert a lowpassfilter into its high-pass counterpart. The input signal is fed to the AD620 instrumentationamplifier both directly (to the noninverting input) and through the low-pass filter (intothe inverting input). At low frequencies, both inputs of the instrumentation amplifier see thesame signal since the low-pass filter passes the signal unaffected. The output of the amplifiershould thus be zero. At high frequencies, however, signals are attenuated by the filter and theamplifier outputs the difference. This results in a high-pass function, since the output of theamplifier is the original signal minus the attenuated low-frequency components. If youdecide to use this technique with a switched-capacitor filter, take precautions to avoid clocknoise from affecting the performance of the filter. If possible, filter the amplifier’s powerinput lines (the figure shows these lines filtered through R2/C7 and R3/C6), and use acontinuous-time low-pass filter at the output of the switched-capacitor low-pass filter.SLEW-RATE LIMITINGSometimes, artifacts that obscure or distort a biopotential signal have significant spectralcomponents within the bandpass of interest. However, there are times when the morphologyof the artifact is sufficiently different from the signal of interest as to allow for its automatic
SLEW-RATE LIMITING 81identification and removal. A good example of this are the artifacts produced by cardiacpacemakers on the ECG signal. The Association for the Advancement of Medical Instrumentation(AAMI) recommends designing ECG equipment assuming the ECG waveformof Figure 2.30. The highest slew rate for an ECG can be estimated by dividing the maximumpeak amplitude within the AAMI range of 0.5 to 5 mV and dividing it by the minimum risetime of the QR interval within the AAMI range of 17.5 to 52.5 ms. This gives a maximumslew rate of 5 mV/17.5 ms 0.28 V/s for a worst-case ECG pulse. The slew rate of apacing pulse is much higher than this, making it possible to design a slew-rate filter thatlimits the rate of change in the signal rather than a specific frequency band.This slew-rate filter technique is also useful in other applications that require limitingartifacts from fast transients. For example, it can be used to filter large artifacts producedby magnetic-resonance imaging (MRI) equipment, allowing a patient’s vital signs to bemonitored during procedures involving this imaging technique. Removing “pop” artifacts(fast transients caused by movement) from EEG recordings and limiting stimulus artifactsin devices designed to measure nerve conduction are also possible through the use of slewratelimiters.A simple slew-rate limiting filter is shown in Figure 2.31. This filter, designed by Williams[1998], is a simple op-amp buffered RC low-pass filter modified by the addition of a bidirectionaldiode clipping network. Whenever the input voltage to op-amp IC1 differs from itsoutput voltage by at least one forward diode drop, the forward-biased diodes will conduct.Under these conditions, the voltage at the output and noninverting input of the op-amp areequal, causing the voltage across R2 to remain approximately constant at one forward diodedrop, V F DIODE .A constant voltage across R2 forces a constant current that charges C1 linearly rather thanexponentially. If R2 R1, the maximum slope (∆V out /∆time) of the signal at the output isgiven by∆VoutVFDIODEslope max ∆ time ( R2)(C1)Input signals with a slope higher than this cause a constant rate of change at the outputequal to this limit. A signal segment with a slope lower than this limit passes through thea r0.5 mV max½ sinewavea sad TTd = 37.5 ms mind QTFigure 2.30 The AAMI stereotype ECG waveform has a maximum slew rate of 0.28 V/s, which allows separating the ECG’s signalcomponents from artifacts with higher slew rates, such as those from pacing and MRI.
82 B<strong>AND</strong>PASS SELECTION FOR BIOPOTENTIAL AMPLIFIERS+15VC2VINJ112R110KR21.8MC11uF0.01uF327 1+-4 5IC1TL0816J212VOUTD1C30.01uF-15V1N4148D21N4148Figure 2.31 A simple slew-rate-limiting filter is based on a simple op-amp buffered RC low-pass filter modified by the addition of a bidirectionaldiode clipping network. Whenever the input voltage to op-amp IC1 differs from its output voltage by at least one forward diodedrop, the forward-biased diodes will conduct. In this region, R2 forces a constant current that charges C1 linearly rather than exponentially,thus limiting the slope of signals at the output of the filter.circuit without attenuation. With the values shown in the schematic diagram, signals witha slope of less than 0.33 V/s pass unaffected, allowing ECGs to be filtered from fast artifactswithout distorting their worst-case 0.28-V/s slopes.J. Moore has proposed a different slew-rate limiter that can be used to filter ECG signalsfrom fast transients. The following circuit is described by Moore [1991] in U.S. Patent4,991,580 as part of an ECG recorder that is immune to artifacts induced by MRI equipment.When the patient is placed inside the bore of a magnetic-resonance imager, thestrong time-varying magnetic fields produced by the MRI system can induce voltagespikes on the ECG leads with an amplitude of 65 mV and a duration of 0.5 ms.In the circuit of Figure 2.32, when the output of op-amp IC1A is positive, diodes D2and D3 are forward biased and diodes D1 and D4 are reverse biased. Under these conditions,zener diode D5 is in series with diodes D1 and D4, cathode positive and anode negative.If the op-amp’s output voltage exceeds the D5’s breakdown voltage plus two diodeforward voltage drops, the voltage at the junction between R1 and R2 will be limited to thezener voltage plus the two diode drops. With a 6.2-V zener, the limiting voltage is approximately7.4 V. Negative voltage swings will have a similar effect, placing the zener diodein series with D1 and D4, limiting the negative swing at the junction between R1 and R2to 7.4 V.In operation, the voltage past the rectified-zener limiting bridge is converted by R2 to acurrent. Since the voltage at the input of the resistor is limited to 7.4 V, the currentflowing through the resistor will be within the range 0.74 µA. This current chargescapacitor C3. The change in voltage across this capacitor is then limited by its capacitancesince dV C /dt I C /C. For a 1-µF capacitor, and with a current of no more than 0.74 µA,the slew rate of the signal buffered by IC1B is limited to 7 V/s. The slew-rate limitingapplied to the biopotential signal is calculated by dividing 7 V/s by the gain of the stagespreceding the slew-rate limiter. For example, if the front-end biopotential amplifier has again of 21, the slew-rate limiting referred back to the biopotential amplifier’s input signalis 0.33 V/s.
ECG AMPLIFIER WITH PACEMAKER PULSE DETECTION <strong>AND</strong> ARTIFACT REJECTION 83-15VVINJ11223-+C1-15V0.01uFIC1B4IC1A46 TL082-R1R2 R37J281TL08210M10M100C31uF5+8+15V12VOUT+15VC20.01uFD1D21N4148D51N41486.2VD31N709AD41N41481N4148Figure 2.32 This slew-rate limiter filters fast transients such as MRI artifacts from ECG signals that can be used to filter ECG signals fromfast transients. The circuit around IC1A acts as a precision-rectified zener diode. R2 converts the voltage of the bridge into a current that islimited by the zener voltage and which charges C3. The change in voltage across this capacitor is limited by its capacitance, thus limitingthe slew rate of signals at the input of buffer IC1B.ECG AMPLIFIER WITH PACEMAKER PULSE DETECTION<strong>AND</strong> ARTIFACT REJECTIONPatients with cardiac pacemakers may have difficulties, especially just after implantationof the pacemaker and lead system, from failure of the pacing system to properly sense theheart’s intrinsic signals or to evoke heartbeats (capture the myocardium). This may reflectproblems in the electronics, the leads, the placement of the leads, or the myocardium itself.The most catastrophic event is failure of the pacemaker to capture the heart when thepatient’s intrinsic rate is slow or nonexistent. To ensure that pacing therapy is being deliveredin an appropriate manner, patients must be monitored to determine if the pacemakeris functioning properly and if appropriate benefit is being derived from the therapy.Specifically, it is important to know how often and why a pacemaker is activated, whetherit is firing at appropriate times, and whether it is, in fact, capturing the heart to produce aheartbeat in response to the electrical stimulation.
84 B<strong>AND</strong>PASS SELECTION FOR BIOPOTENTIAL AMPLIFIERS10msa)b)0.5 - 8VTR = TF = 20ns0.5mV17.5ms0.5 ms20 msFigure 2.33 A typical pacing pulse consists of a main pulse that stimulates the heart and a discharge phase used to deplete the charge onthe capacitive coupling generated by the delivery of the pacing pulse. Simple biopotential amplifiers unduly distort ECG signals from pacemakerpatients because of the large amplitude difference between (a) pacing pulses and (b) the heart’s intrinsic signals.As shown in Figure 2.33a, a typical pacing pulse consists of two components, amain pulse and a discharge phase. The main pulse, which is used to stimulate the heart, ischaracterized by its narrow width, sharp rise and fall, and large variation in amplitude. Theactual shape of the pacing pulse depends on the output coupling design of the pacemaker.The discharge phase is used to deplete the capacitive coupling generated by the delivery ofthe pacing pulse charge built up between the heart’s tissue and the pacemaker’s electrodes.The shape and size of the discharge phase is a function of the energy content of the pacingpulse and the amount of capacitive coupling.The problem with using a simple biopotential amplifier to diagnose patients with pacemakersis the large voltage ratio between the artifact caused by the pacing pulse and thetrue ECG signal. When this ratio is large, the ECG signal baseline will be shifted to thedischarge baseline of the pacer artifact signal, thus distorting the ECG. A large artifact signalcan also produce amplifier overloads, preventing observation of the heart’s electricalactivity following pacing. To overcome this problem, ECG amplifiers designed to followup on patients receiving pacing therapy have the means to separate and separately processthe ECG and pacing pulse artifact signals, and augment the pacer artifact by providing auniform pacing pulse artifact.Figures 2.34 and 2.35 illustrate a four-lead ECG amplifier useful for evaluating patientsimplanted with a cardiac pacemaker. In this circuit, op-amps IC1B, IC1C, and IC1D bufferthe biopotential signals detected by electrodes placed in the right arm, left arm, left leg,and chest of the patient. IC1A buffers the ECG signal detected from an electrode placedon one of the precordial electrodes.The buffered left-arm, right-arm, and left-leg signals are summed by resistors R8, R9,and R10 prior to being buffered by IC2B to derive the Wilson central terminal (WCT)potential, which is considered to be the reference potential for ECG recording from the
ECG AMPLIFIER WITH PACEMAKER PULSE DETECTION <strong>AND</strong> ARTIFACT REJECTION 85+15VISO+15VISO+15VISOJ11ChestElectrodeR1330KD11N4007D21N4007IC1ATL07443 +2 -111C1.01uFIJ31Right ArmElectrodeR3330KD41N4007D51N4007+15VISOIC1CTL074410 +89 -11-15VISO-15VISOC2.01uFI-15VISO-15VISO+15VISO+15VISOJ21Left ArmElectrodeR2330K-15VISOD31N4007D41N4007+15VISOIC1BTL07445 +76 -11-15VISOJ41Left LegElectrodeR4330K-15VISOD61N4007D71N4007+15VISOIC1DTL074412 +1413 -11-15VISOIIIIIICHESTRARALAWCTSW1ECG+ECG-SW ROTARY 2P-4W+15VISO+15VISOJ51Right LegElectrodeD91N4007R5330KD101N4007-15VISOR610M8 IC2A1+-324TL072C3-15VVISO100pFIR749.9K-15VISOIC2BTL07247- 6+ 58C4.01uFIR833.2KR933.2KR10+15VISOC5.01uFI33.2KWilson Central TerminalFigure 2.34 This four-lead ECG amplifier separates and independently processes the ECG and pacing pulse artifact signals. The Wilsoncentral terminal is synthesized by R8–R10 together with IC2B and is used for right-leg driving after being inverted IC2A. SW1 selects thelead to be amplified by instrumentation amplifier IC3 of Figure 2.35.chest electrode. The level of this signal is closely related to the common-mode potentialseen by the limb electrodes. As such, it is used to reduce common-mode interference bydriving the right-leg electrode through inverting amplifier IC2A.SW1, a two-pole four-position rotary switch with insulated shaft and 5-kV contact-tocaseinsulation rating selects which buffered signals are presented to the inverting and noninvertinginputs of instrumentation amplifier IC3 of Figure 2.35. The bipolar limb leadsare obtained as follows:• Lead I: tracing of the potential difference generated by the heart between the left andright arms, where the left arm (L) is the noninverting input and the right arm (R) theinverting input
86Figure 2.35 The slew-rate limiter and pacing pulse detector implemented around IC4A and IC4D split the amplified signal into the ECG andpacing pulse components. It then restores the baseline and isolates the artifact-free ECG signal and augments the pacing artifact by providing auniform pacing pulse indicator.
ECG AMPLIFIER WITH PACEMAKER PULSE DETECTION <strong>AND</strong> ARTIFACT REJECTION 87• Lead II: tracing of the potential difference between the left leg (F) and the right arm,where the left leg is the noninverting input• Lead III: tracing of the potential difference between the left leg and the left arm,where the left leg is the noninverting inputA unipolar chest lead is obtained by connecting the chest electrode to the noninvertinginput, while the WCT is connected to the inverting input. The specific chest lead (V1–V6)is obtained by placing the chest electrode on specific anatomical landmarks according tointernational standards:• V1• V2• V3• V4• V5• V6in the fourth intercostal, at the right side of the sternumin the fourth intercostal, at the left side of the sternumhalfway between V2 and V4in the fifth intercostal, left mid clavicularin the same horizontal plane as V4, halfway between V4 and V6 (anterior axially)in the same horizontal plane as V4, left mid axiallyV1 and V2 are thus placed above the right ventricle, V3–V6 above the left ventricle.The output of IC3 contains an amplified version of the true ECG signal and the pacingpulse artifact. This signal is separated into the two components via the slew-rate limiterand pacing pulse detector circuits implemented around IC4A and IC4D. Once a certainslew rate has been exceeded by the output of IC3, the slew-rate limiter limits the excursionsof the output signal to a specified rate of change. When the input voltage to IC4A iszero, the current flowing through R11 and R12 is the same, and thus the output of the slewratelimiter is zero (neglecting possible op-amp offset). When a positive-going signalappears at the noninverting input terminal of IC4A, the output of IC4A will go positive,and current through R12 will be sourced by the op-amp. At the same time, current will besourced by capacitor 46. As long as slewing-rate conditions given by the values ofR11 R12 and C10 are not exceeded, the slew-rate limiter’s output voltage tracks IC4A’sinput voltage. However, if a pacing pulse artifact is presented to the noninverting input ofIC4A, the slew-rate limit imposed by the time constant of R11 R12 and C10 is exceededand capacitor C10 will charge (or discharge) at a rate limited by the value of R11 R12.At the time of the slew rate limiting, the output signal’s slew rate will be limited to thecharge or discharge rate of capacitor C10. Soon after the slew rate of the input signal fallsunder the slew-rate limit, op-amp IC4A returns from saturation, and the output of the slewratelimiter tracks IC4A’s noninverting input. Once the ECG signal has been cleaned by theslew-rate limiter from the pacing pulse artifact, baseline zeroing is accomplished by feedingthe inverted baseline level (derived by inverting and heavily low-pass filtering theslew-rate limiter’s output) to the reference pin of IC3.Pacing pulse detection exploits the fact that the output of IC4A rails when the slew rateof its input exceeds the set limit. IC4D rectifies IC4A’s output. Whenever the slew-ratelimit is violated (which is assumed to happen only whenever a pacing pulse is present), apositive pulse appears at the trigger input of nonretriggerable one-shot IC5. The artifactfreeECG signal is amplified further via IC4C before it is presented to a Burr-BrownISO107 isolation amplifier. Every time a pacing pulse is detected, an optically isolated 5-ms pulse is added to the isolated and filtered ECG signal via R27 and R28 before beingbuffered by IC8B.The circuits in galvanic contact with the patient are powered via ISO107, which generatesisolated 12 V when powered from 12 V. L2, C24, C25, and C26 form a pi filter toclean the isolated 12-V power line generated by ISO107 from switching noise. An identicalnetwork is used to filter the negative isolated supply rail. A pi filter formed by L1,
88 B<strong>AND</strong>PASS SELECTION FOR BIOPOTENTIAL AMPLIFIERSC21, and C23 is used to decouple the positive input power rail of IC6 so that switchingnoise within IC6 does not find its way into the postisolation circuits.SCRATCH, RUMBLE, CLICK, <strong>AND</strong> POPOur good British friend and colleague André Routh has held many positions as a biomedicalengineer and scientist at various cardiac pacemaker and diagnostic device companiesfor over 20 years. In the tradition of British electronics aficionados, his hobby is hi-fi, especiallywhen it’s done using valves (vacuum tubes). André’s expertise is in biomedical signalprocessing, and some time ago he implemented a specialized filter for cardiac signalsbased on the way in which audio professionals filter surface noises from old records(remember vinyl?). In the hi-fifield, these circuits are known as scratch or “click and pop”filters. Another device, the rumble filter, cuts down low-pitched noises, such as vibrationfrom the phonograph motor.The circuit of Figures 2.36 to 2.39 is a high-pass filter with a cutoff frequency of 0.5 Hzfor baseline offset rejection and a low-pass filter with a cutoff frequency of 500 Hz fornoise rejection and antialias filtering. The gain of this filter unit can be varied continuouslyin three ranges, from 0 to a maximum of 100. What makes this filter so unique is its rapidrecovery from transient overloads. This is achieved through an input “blanking” schemethat can reject impulses such as pacing spikes. The high-pass filter with its long time constantcan cause output saturation when faced with a step-type input or slow decay processsuch as a defibrillation shock. An output overload detection circuit changes the time constantof the high-pass filter. The cutoff frequency is increased to approximately 50 Hz untilthe output is within the allowable range for the signal acquisition equipment that followsthe filter.Typically, this filter circuit would be used between an isolated biopotential amplifierand an instrumentation tape recorder or data acquisition unit. The output of the filter ismonitored on a LED bar graph display which has a VU meter response with fast attack andslow decay times. Additionally, there are two LEDs to indicate either input or output overloads.In a typical application, an input signal arrives via J2 from the output of an isolatedbiopotential amplifier. R1, D1, and D2 form an input signal clamp that limits at approximately8.2 V. R1 and C1 form a low-pass filter with a cutoff frequency of 5.3 kHz. R2 is apassive attenuator whose wiper is connected to the noninverting input of IC1A. The gainof this op-amp is defined by R3 and R4. R4 should be selected to have a resistance equalto R2, so that when R2 is set to maximum the voltage at IC1A’s output is equal to the inputvoltage at J2.IC1B and associated components form a second-order Butterworth (maximally flatamplitude) low-pass filter. With the components selected, the cutoff frequency calculatedis 509 Hz. Front-panel SW1 can be used to bypass the low-pass filter. IC2 is a quad CMOStransmission gate (digitally controlled analog switch). Under normal conditions (i.e., withno input overload), IC2A is closed and IC2B is open, allowing the signal at the wiper ofswitch SW1 to feed the second-order Butterworth high-pass filter built around IC1C(Figure 2.37). With the components selected, the cutoff frequency is 0.49 Hz. As long asthere is no output overload, analog switches IC2C and IC2D are open, and as such, undernormal conditions they do not interfere with the nominal operation of the high-pass filter.Front-panel switch SW2 can be used to bypass the high-pass filter.IC1D is configured as a switchable gain amplifier. The gains available are 1, 10, and100, depending on the setting of front-panel switch SW3. The low-pass action of C6depends on the gain of the amplifier stage. At 100 the cutoff frequency is approximately4.8 kHz; at 10 it is about 53 kHz. Potentiometer R13 in conjunction with resistor R14allows the output offset to be nulled. R18 and C7 form a low-pass filter with a cutoff
+15V141 2IC4ACD40106B32+-+15V4111IC3ATL074BR2010K65-+R2110K-15V11IC3BTL074B7+15V4 1414IC5B+15V-7.5VIC3CTL074B-15V-15V -15V910131211-+-+4114+15V8IC3DTL074B14D91N4148D101N4148-8VR1922.1KD111N4148C833nFC9100nFR2422.1KR231MD121N4148+15V141275 67IC4CCD40106B+15V143 47+8VIC4BCD40106BIC5ACD4093B356+15V+8VLED1LEDR251.5KOVERLOAD INDICATORCD4093B4BR110kD17V5D27V5C13.3nFR2100K32+-+15V411-15VNominal value.Select to matchR2IC1AOP4701R310KR4100KR522.1KR622.1KC310nFC210nF56+15VR744.2KSW1BYPASSLPF7-8VLPF_OUT1 2IC2A406631+-4-15VIC1BOP4707LPF = 500HzONIC2 is poweredfrom +8, -8Volts7-8V1110AIC2B406612FILTER_INFigure 2.36 This ECG signal filter, designed by André Routh, uses the principles of hi-fi “pop and click” filters to ensure fast recoveryfrom transients without distorting the signal of interest. This is the low-pass filter portion of the instrument. In addition, this figure includespart of the control circuit that enables the unique functionality of this filter is built around IC3, which is configured as a window comparator.With no input overload, IC2A presents the low-pass output to the high-pass filter of Figure 2.37. When the input saturates, the input ofthe high-pass filter is grounded.+7.5VJ212BNC+15VR1910KINPUT89
J3OUTPUTBNC2CR81.05KIC 2C406654 3LPF_OUTC52.2uF9R112.10KIC2D64066109+-+15V411CIC1COP4708BYPASS<strong>OF</strong>FSETNULL1213R141M+15V+-411IC1DOP47014C6330pFR15100Kx10R18301JP11 2D31N4148D41N4148D51N4148D1R10210KR9105K-15VR12232KONR131MHPF+15V-15VSW2-15VS3x100R169.09K1 2 3Cx1SW3C7100nFD61N4148D71N4148D81N41488HPF = 0.5HzR171KJUMPER+/- 2V CLAMPLPF = 5.3 kHzFigure 2.37 Under normal conditions, this filter has a high-pass cutoff of 0.5 Hz. When a transient overload is detected, the high-pass cutofffrequency is increased to approximately 50 Hz and the gain falls to zero until the output is within the allowable range for the signal acquisitionequipment that follows the filter.C42.2u FFilter_In90
frequency of 5.3 kHz. When jumper JP1 is closed, the output swing is clamped at approximately2 V by diodes D3–D8.The unique functionality of this filter comes into action when an overload occurs. IC3in Figure 2.36 is configured as a window comparator. Potentiometer R19 is adjusted to7.5 V. IC3B is a unity-gain inverter whose output will be at 7.5 V. IC3C and IC3Dfunction as comparators. With no input overload, both IC3C’s and IC3D’s outputs are low(i.e., close to 15 V). If the input voltage rises above 7.5 V, IC3C will switch and D9will be forward biased. If the input falls below 7.5 V, IC3D will switch and D10 will beforward biased. D9, D10, and R19 form a wired OR gate. D11 prevents the inputs of IC4A,IC4B, and IC4C from receiving voltages below 0 V. C9, R23, and the hysteresis of theSchmitt action of IC4 form a one-shot that acts as a pulse stretcher, causing LED1 to illuminate.R24 and D12 clamp the positive voltage reaching IC5A to 8 V. IC5A and IC5Bare connected as series inverters whose outputs, labeled A and B, drive transmission gatesIC2A and IC2B. Note that A is also <strong>AND</strong>ed via D13 into IC5C (Figure 2.38).On receipt of an input overload, IC2A will open and IC2B will close, thereby disconnectingthe high-pass filter from the overload. This action is enhanced when the low-passfilter is in the circuit (i.e., SW1 is not set to bypass) because the low-pass filter introducesa delay to the signal. The net effect is that IC2A opens and IC2B closes before the overloadsignal has emerged at the output of the low-pass filter.The circuit’s output (marked D in Figure 2.37) is fed to the precision full-wave rectifierof Figure 2.38 configured around IC6A and IC6B. For positive half-cycles, D14 is forwardbiased and the circuit behaves like a cascaded unity noninverting amplifier. C10 ensuresstability. For negative half-cycles, IC6A and D15 form a precision half-wave rectifierwhose output (at D15 anode) is fed to the unity-gain inverter formed by IC6B/R26/R28.The net result is a fast full-wave rectifier that requires only two matched resistors (R26and R28).The output of the full-wave rectifier is fed to a comparator formed by IC6D. R30, D16,and D17 limit the comparator output to the 8 V range for application to N<strong>AND</strong> gateIC5C. The output from IC5C is inverted by IC5D, whose output is labeled C. Under normalconditions (i.e., not output overload or input overload), C is low. If an overload occurs,the magic of the circuit kicks in, C goes high, thereby enabling transmission gates IC2Cand IC2D. R8 and R11 are switched in parallel with R9 and R10, respectively, when IC2Cand IC2D close. The cutoff frequency of the high-pass filter of Figure 2.37 formed aroundIC1C is increased to approximately 50 Hz and the output of the filter rapidly settles toward0 V as C4 and C5 discharge.The rest of the circuit is used to drive a TSM39168 VU LED bar graph display. The outputfrom the full-wave rectifier is fed to the precision half-wave rectifier formed by IC6and D18. R32, R33, and C11 form an attack/decay circuit where the attack time (i.e.,charge time of C11) is determined predominantly by R32/C11 and the decay time byR33/C11. The bar graph display of Figure 2.39 has an integrated driver circuit with VUmeter calibration. The scale factor is set by R33 and R34. The transition from the greenLEDs to the orange LEDs occurs at 1 V. The tenth LED (red) is activated when the voltagereaches 1.5 V. The output from this last LED is taken to a comparator formed by IC7Aand resistor divider R34 and R35. The comparator output feeds the one-shot formed byD19, R36, and C13 and the Schmitt inverters IC4D, IC4E, and IC4F. The stretched pulseilluminates LED2 to indicate that the output level is too high.A voltage of 15 V for the filter unit is supplied via connector J1. C15, C16, C19, andC20 from input filters for the 15-V supply to reduce crosstalk between channels. IC8 andIC9 are low-power 8-V regulators to supply the analog transmission gates (IC2) and thequad N<strong>AND</strong> gate (IC5). The 5-V power for the bar graph display has a separate groundcircuit and is filtered by C23, R38, and C12 to prevent noise from being fed into theamplifier stages.SCRATCH, RUMBLE, CLICK, <strong>AND</strong> POP 91
IC5DCD4093B11CDisplay_InAD131N414841IC6ATL074D151N4148+15V+8V141213R3210K147+-C1147nF+8VR311MC1410nF+15V11-15VR2910KD141N4148+15VC1047pFR2710K131256+15V11-+4-15V+-411IC6DTL074-15V14IC 6BTL0747R3010K+8V-8VD161N4148D171N4148109+-+15V411-15VIC5CCD4093BIC6CTL0748897-8VD181N414810R33475K+8V-8VR26R2810K10KFigure 2.38 This is the circuit that controls the shift in frequency and gain of the high-pass filter of Figure 2.37. The HPF output (markedD) is fed to a precision full-wave rectifier configured around IC6A and IC6B, the output of which is fed to a comparator formed by IC6D.Under normal conditions (i.e., not output overload or input overload), C is low. If an overload occurs, C goes high, thereby increasing theHPF cutoff to 50 Hz and changing its gain to zero.32D92
SCRATCH, RUMBLE, CLICK, <strong>AND</strong> POP 93+15V+5VR3810C1222uF+15V14 IC4DCD40106B9 8+15VLED2OVERLOADINDICATOR+-15V7+15VR391.5KDISP1TSM39168Display_In64 101 12Display 135789R341K+15VR3610K2311 IC7ATL074-1+4+15VD191N4148R381MC13100nF11147+15VIC4ECD 40106B10R35121R372K14 IC4FCD40106B13 127J112345678910+5V C2310nFC15100uFC19100uF+15V++-15VC1610nFC2010nF13IC8L78M08/TO220VINVINIC931VOUTVOUTL7908/TO220Figure 2.39 Signal levels are indicated by a TSM39168 VU LED bar graph display. The transition from the green LEDs to the orangeLEDs occurs at 1 V. The tenth LED (red) is activated when the voltage reaches 1.5 V. LED2 indicates that the output level is too high.A voltage of 15 V power for the filter unit is supplied via connector J1. IC8 and IC9 are low-power 8-V regulators to supply the analogtransmission gate (IC2) and the quad N<strong>AND</strong> gate (IC5). The 5-V power for the bar graph display has a separate input.C1710nFC2110nFGND GND2C18470nFC22470nF2+8V-8VMore recently, André designed an intracardiac electrogram signal amplifier that implementsa similar transient-elimination technique to enable detection of evoked-responseevents from the heart soon after the delivery of pacing or defibrillation pulses. The amplifierof Figure 2.40 receives a digital BLANK command just before (e.g., 1 ms) the transientevent (e.g., a pacing or defibrillation pulse) is delivered to the heart. Under normalconditions, the electrogram signal detected via intracardiac electrodes (from pacing leadsor a mapping catheter) is presented to an INA128 instrumentation amplifier (IC3) via accouplingcapacitors C3 and C6. Resistors R4 and R8, together with C5 and C7, low-passthe input signals. The output of the instrumentation amplifier is filtered by the secondorderButterworth high-pass filter built around IC1B.When a BLANK signal is delivered to the biopotential amplifier circuit, the inputs ofthe instrumentation amplifier are shorted to the analog signal ground via analog switches
OUT+5V_ISOC122uF3284+-IC1A1OPA2130+2.5VLocal AnalogGro undNotes:Components marked * must be matchedwithin 0.5%.1516IC 2BMAX39214+5V_ISOIIC 2CMAX392C233nF*R422.1K*R8*C515nFR51MR656.231827IC3INA1286R722.1K109C433nF11654-+8R344.2KIC1BOPA2130722.1K*C715nF6IC2DMAX3923IC 2AMAX392135R91M4 54+2.5V7 82 1IBLANKFigure 2.40 This intracardiac electrogram signal amplifier enables detection of evoked-response events from the heart soon after the deliveryof pacing or defibrillation pulses. A digital BLANK command is supplied just before the stimulus pulse is delivered to the heart. Thiscommand shorts the inputs of the instrumentation amplifier and changes the configuration of IC1B to an amplifier with a gain of zero.Recovery occurs within a few milliseconds after the blanking signal is released.R11MR21M*C33.3nF*C63.3nF+IN-IN94
REFERENCES 95IC2A and IC2D. At the same time, the capacitors of the high-pass filter are shorted, whichchanges the configuration of IC1B to an inverting amplifier with a gain of zero. After thestimulus subsides, the blanking signal is released, and the amplifier recovers within millisecondsto allow detection of evoked or intrinsic potentials. Note that the circuit is poweredfrom a single 5-V supply. IC1A is used to buffer the 2.5-V voltage produced byresistor divider R1 and R2 and filtered by C1. The 2.5 V at the output of IC1A is used asan analog reference potential for the circuit.REFERENCESKoide, F. T., Quick Estimate of Signal Bandwidth, Electronic Design, 115–116, December 16, 1996.Moore, J. C., Method of Improving the Quality of an Electrocardiogram Obtained from a PatientUndergoing Magnetic Resonance Imaging, U.S. patent 4,991,580, 1991.Suesserman, M., Bootstrapped, AC-Coupled Differential Amplifier, U.S. patent 5,300,896, 1994.Williams, A., Special Low-Pass Filter Limits Slope, Electronic Design, May 25, 1998.
3<strong>DESIGN</strong> <strong>OF</strong> SAFE <strong>MEDICAL</strong>DEVICE PROTOTYPESMilitary downsizing, government cutbacks, and corporate reengineering had the oppositeeffect on the medical industry as they did on all other areas of technology. As R&D budgetsshrank, early-generation technologies that had long been considered obsolete for space,security, and military applications suddenly found a thriving environment in the developmentof new medical devices. For example, cruise-missile tracking technology has beenadapted to steer powerful x-ray beams to destroy brain and spinal-cord tumors preciselywithout the need of surgery; software used for interpreting spy-satellite images has beenused as the basis for detecting subtle but highly virulent breast cancers that were oftenoverseen in visual interpretations of mamographic images; and miniaturized high-energycapacitors developed for portable laser weapons may make it possible to build smaller andlighter automatic implantable cardiac defibrillators.Many other examples of these dual-use technologies continue to appear with no end insight, making medical electronics one of today’s fastest-growing and most promising technology-basedindustries. Fortunately for the entrepreneurs among us, prototypes of manynew medical instruments can still be developed in a garage-turned-laboratory without theneed for esoteric technologies recycled from multibillion-dollar satellite and weapons programs.Rather, a fresh idea, a personal computer, and some simple interface circuitry is allit may take to start the next revolution in medical care.Despite how simple or complex a medical electronic instrument prototype may be,however, safety must be the primary objective throughout the development effort. Becomingintimately familiar with electrical safety standards is probably the most important thingthat a newcomer to the field can do, because the dangers involved in interfacing with thehuman body are often counterintuitive to an otherwise knowledgeable engineer. For example,did you know that a 60-Hz current of barely 10 A flowing through the heart has thepotential of causing permanent damage and even death?The objective of this chapter is to introduce the basics of designing and constructingelectrically safe medical instrument prototypes. We first present an overview of electricalsafety compliance requirements, proceed to look at a number of circuits that enable safeinterfacing with medical electronics, then review safety testing methods, and finally, showDesign and Development of Medical Electronic Instrumentation By David Prutchi and Michael NorrisISBN 0-471-67623-3 Copyright © 2005 John Wiley & Sons, Inc.97
98 <strong>DESIGN</strong> <strong>OF</strong> SAFE <strong>MEDICAL</strong> DEVICE PROTOTYPESthe construction of a number of useful test instruments suitable for assessing the electricalsafety of medical electronic instruments.ST<strong>AND</strong>ARDS FOR PROTECTION AGAINST ELECTRICAL SHOCKIt has been a long time now that medical electronic devices left the realm of experimentationand were transformed into irreplaceable tools of modern medicine. This widespread use of avery diverse variety of electronic devices compelled countries to impose regulations thatensure their efficacy and safety. In the United States, the Food and Drug Administration(FDA) is responsible for the regulation of medical devices. In the European Union (EU), aseries of directives establishes the requirements that manufacturers of medical devices mustmeet before they can obtain CE marking for their products, to authorize their sale and use.In addition, however, individual nations of the EU may impose local regulations throughinternal regulatory bodies. Other countries, including Canada, Japan, Australia, and NewZealand, have their own regulations, which although similar to the harmonized European andU.S. standards, have certain particulars of their own.Safety standards are sponsored by organizations such as the American NationalStandards Institute (ANSI), the Association for Advancement of Medical Instrumentation(AAMI), the International Electrotechnical Commission (IEC), and Underwriters’Laboratories, Inc. (UL), among many others. These standards are written by committeescomprised of representatives of the medical devices industry, insurance industry, academia,physicians, and other users in the medical community, test laboratories, and the public. Thepurpose of creating these broad-spectrum committees is to ensure that standards address theneeds of all parties involved in the development, manufacture, and use of medical devices.Thus, through a consensus process, emerging standards are deemed to capture the state ofthe art and are recognized at national and international levels.In general, safety regulations for medical equipment address the risks of electric shock,fire, burns, or tissue damage due to contact with high-energy sources, exposure to ionizingradiation, physical injury due to mechanical hazards, and malfunction due to electromagneticinterference or electrostatic discharge. The most significant technical standard is IEC-601,Medical Electrical Equipment, adopted by Europe as EN-60601, which has been harmonizedwith UL Standard 2601-1 for the United States, CAN/CSA-C22.2 601.1 for Canada, andAS3200.1 and NZS6150 for Australia and New Zealand, respectively.According to IEC-601, a possible risk for electrical shock is present whenever an operatorcan be exposed to a part at a voltage exceeding 25 V RMS or 60 V dc, while an energyrisk is present for circuits with residual voltages above 60 V or residual energy in excessof 2 mJ. Obviously, the enclosure of the device is the first barrier of protection that can protectthe operator or patient from intentional or unintentional contact with these hazards. Assuch, the enclosure must be selected to be strong enough mechanically to withstand anticipateduse and misuse of the instrument and must serve as a protection against fires thatmay start within the instrument due to failures in the circuitry.Beyond the electrical protection supplied by the enclosure, however, the circuitry of themedical instrument must be designed with other safety barriers to maintain leakage currentswithin the limits allowed by the safety standards. Since patient and operator safetymust be ensured under both normal and single-fault conditions, regulatory agencies haveclassified the risks posed by various parts of a medical instrument and have imposedspecifications on the isolation barriers to be used between different parts. The first type ofpart is the accessible part, a part that can be touched without the use of a tool. Touchingin this context not only assumes that contact is made with the exterior of the enclosure orany exposed control knob, connector, or display, but that it could be made accidentally: forexample, by poking a finger or pencil through an opening in the enclosure. In fact, most
ST<strong>AND</strong>ARDS FOR PROTECTION AGAINST ELECTRICAL SHOCK 99standards define rigid and articulated probes that must be used to verify the acceptabilityof enclosure openings.The second type of part is the live part, a part that when contacted can cause the leakagecurrent to ground or to an accessible part of the equipment to exceed the limits establishedby the standard. One form of live part is the mains part, defined as a circuit connecteddirectly to the power line.The third type of part comprises signal-input and signal-output parts, referring to circuitsused to interface a medical instrument to other instruments: for example, for the purposesof displaying, recording, or processing data. The fourth and most critical part of amedical instrument is that which deliberately comes into physical contact with the patient.Such a part, called an applied part, may include a number of patient connections whichprovide an electrical pathway between it and the patient. The patient circuit comprises allpatient connections as well as all other parts and circuits of the medical instrument that arenot electrically isolated from these connections.The level of electrical shock protection provided to patients by the isolation of appliedparts classifies them as follows:• Type B: applied parts that provide a direct ground connection to a patient• Type BF (the F stands for “floating”): indicates that the applied part is isolated from allother parts of the equipment to such a degree that the leakage current flowing through apatient to ground does not exceed the allowable level even when a voltage equal to 110%of the rated power line voltage is applied directly between the applied part and ground• Type CF: similar to type BF, but refers to applied parts providing a higher degree ofprotection, to allow direct connection to the heartThe use of F-type applied parts is preferable in all cases to type B applied parts. This isbecause patient environments often involve simultaneous use of multiple electronic instrumentsconnected to the patient. In any case, type B applied parts are prohibited wheneverpatient connections provide either low-impedance or semipermanent connections to thepatient (e.g., through recording bioelectrodes as in ECG or EEG, or for stimulation of tissues,such as TENS). Furthermore, all medical electrical equipment intended for direct cardiacapplication (e.g., intracardiac electrophysiology catheters, invasive cardiac pacing) must containonly CF-type applied parts. Additionally, the applied parts of instruments for cardiacdiagnosis and therapy are often designed to withstand the application of high-voltage highenergyshocks, such as those used for cardiac cardioversion and defibrillation.These classifications have more than academic purpose. The standards provide thedesigner with clear indications regarding the minimal level of circuit separation and theapplication of insulation between these parts to accomplish acceptable levels of isolation.As such, insulation is not only defined as a solid insulating material applied to acircuit, but also to spacings that establish creepage distances and air clearance betweenparts. The separation of two conductive parts by air alone constitutes a clearing distance,while the separation of conductive parts on a nonconductive plane (e.g., tracks on aprinted circuit board) is a creepage distance. The minimum separation distance betweenelements of two parts is determined by the working voltage between parts as well as bythe insulation rating required to afford protection against electrical shock.A basic insulation barrier is applied to live parts to provide basic protection againstelectrical shock. For example, its use applies to the separation between a live part and anaccessible conductive part that is protected by connection to ground. Supplementary insulationis an independent insulation barrier applied in addition to basic insulation in orderto provide protection against electrical shock in the event of failure of the basic insulation.Double insulation and reinforced insulation provide protection equivalent to the use ofboth basic and supplementary insulation.
100 <strong>DESIGN</strong> <strong>OF</strong> SAFE <strong>MEDICAL</strong> DEVICE PROTOTYPESTABLE 3.1 Spacings (Millimeters) Required to Provide Various Levels of Insulationbetween Parts of a Medical DeviceAc Voltage: 125 V 250 V 380 VDc Voltage: 150 V 300 V 450 VBasic insulation (between Air clearance 1 1.6 2.4parts of opposite polarity) Creepage distance 2 3 4Double or supplementary Air clearance 1.6 2.5 3.5insulation Creepage distance 3 4 6Double or reinforced Air clearance 3.2 5 7Reinforced insulation Creepage distance 6 8 12Figure 3.1 and Table 3.1 present a partial view of how to achieve the minimal requiredinsulation ratings between parts. Although these are only a subset of all possibilities contemplatedby the standards, they certainly provide a very practical reference for the designer.LEAKAGE CURRENTSEvidently, the purpose of the various isolation barriers is to ensure that leakage currentsare maintained within safe values even when a single-fault condition occurs. Three typesof leakage currents are defined within the standards:<strong>MEDICAL</strong>INSTRUMENTAC PowerBSBInput/OutputPart withConnection toGroundRLive Part(Mains Part)Live PartRFloating-TypeApplied PartPatient ConnectionsBRNon-Live PartSRConductive EnclosureConnected to Protective GroundBFigure 3.1 Some of the requirements for insulation between the parts of a medical instrument. Insulation types: B, basic; S, supplementary;R, reinforced.
LEAKAGE CURRENTS 1011. Ground leakage current: current flowing from all mains parts through or across theinsulation into the protective ground conductor of the grounded power cord2. Enclosure leakage current: total current flowing from the enclosure and all accessibleparts (but excluding applied parts) through an external conductive connectionother than the protective ground conductor to ground or another part of the enclosure3. Patient leakage current: current flowing from the applied part by way of the patientto ground, or flowing from the patient via an F-type applied part to ground; originatesfrom the unintended appearance of voltage from an external source on thepatientIt must be noted, however, that these leakage currents must not be confused with currentsgenerated intentionally by the medical device to produce a physiological effect on thepatient, or used by the applied part to facilitate measurement without producing a physiologicaleffect. Examples of patient intentional currents are those used for the stimulationof nerves and muscle, cardiac pacing and defibrillation, and cutting and cauterizationwith radio frequency. Patient auxiliary currents are used to bias the front-end amplifiersdesigned to detect biopotentials, to enable the measurement of impedance of living tissues,and so on.In the standards, the terms voltage and current refer to the root-mean-square (RMS)values of an alternating, direct, or composite voltage or current. Remember that bydefinition, the RMS value of an alternating voltage V across a resistor R equals the directvoltage, causing the same dissipation level in R. For a sinusoidal waveform, the RMS voltageV RMS is related to the peak-to-peak voltage V p-p byV p-p V RMS 2 1.414V RMSA similarly corresponding definition applies to the value of an RMS current. In the case ofcomposite (ac dc) signals, the RMS value is calculated fromV RMS V 2 dcV 2acRMSAs shown in Table 3.2, allowable patient leakage and auxiliary currents are defined forboth normal and single-fault conditions, assuming that the equipment is operating at maximumload and that the supply is set at 110% of the maximum rated supply voltage. Singlefaultconditions are defined as conditions in which a single means of protection against aTABLE 3.2 Some Allowable Values of Continuous Leakage and Patient Auxiliary Currents under Normal andSingle-Fault Conditions (Milliamperes)Equipment TypeB BF CFCondition Normal Single fault Normal Single fault Normal Single faultGround leakage current 0.5 1 0.5 1 0.5 1Enclosure leakage current 0.1 0.5 0.1 0.5 0.1 0.5Patient leakage current 0.1 0.5 0.1 0.5 0.01 0.05Patient leakage current — — — 5 — 0.05(with power line voltageon the applied part)Dc patient auxiliary current 0.01 0.05 0.01 0.05 0.01 0.05Ac patient auxiliary current 0.1 0.5 0.1 0.5 0.01 0.05
102 <strong>DESIGN</strong> <strong>OF</strong> SAFE <strong>MEDICAL</strong> DEVICE PROTOTYPESsafety hazard in the equipment is defective or a single external abnormal condition ispresent. These include interruption of the supply by opening the neutral conductor as wellas interruption of the protective ground conductor. Patient leakage current between anF-type applied part and ground assumes that an external voltage equal to 110% of the maximumrated supply voltage is connected directly to the applied part. For battery-poweredequipment, the external voltage that is assumed to be connected to the F-type applied partis 250 V. In addition, it must be noted that grounding of the patient is considered to be anormal condition.The allowable leakage current levels have been set as a compromise between achievableperformance and overall risk. Although a 60-Hz current as low as 10 A flowing throughthe heart may cause ventricular fibrillation (a disorganized quivering of the lower chambersof the heart muscle that quickly leads to death) under highly specific conditions, the probabilityof such an event is only 0.2%. Under more realistic clinical conditions, however, a50-A current flowing from a CF-type applied part through an intracardiac catheter has anoverall probability of just 0.1% of causing ventricular fibrillation. This probability is verysimilar to that of causing fibrillation due to the irritation caused by mere mechanical contactof the catheter with the heart wall. Obviously, for equipment that does not come indirect contact with the heart, allowable leakage currents have been increased up to the pointwhere even under single-fault condition, the probability of causing ventricular fibrillation isno higher than 0.1%, even though the actual current may be perceptible to the patient.<strong>DESIGN</strong> EXAMPLE: ISOLATED DIFFERENTIAL ECG AMPLIFIERLet’s use a simple circuit as an example to illustrate the various considerations regardingthe safe design of a medical instrument. Figure 3.2 presents the schematic diagram of asimple biopotential amplifier intended to detect a differential ECG signal through surfaceECG electrodes. In the circuit, signals picked up by electrodes attached to the patient’sskin are amplified by IC1, a Burr-Brown INA110 instrumentation amplifier IC. The gainof the front-end stage is programmable between unity and 500 by jumpers JP2–JP5. SinceIC1 is dc-coupled, care must be exercised in the selection of gain so that the amplifier isnot saturated by dc offset voltages accompanying the biopotential signal. For example, touse this circuit as part of a surface ECG amplifier, the gain must be calculated to cope withoffset potentials of up to 300 mV. In general, IC1’s gain should be kept low so that dccoupling does not result in its saturation. Potentiometer R1 is used to trim the input offsetto IC1. R1–R3 can be omitted from the circuit for most applications that do not requireextreme dc precision.Direct connection of IC1’s inputs to patient electrodes is possible since the amplifier usesa maximum bias current of 50 pA, and the FDH300 low-leakage diodes used to protect theinputs of IC1 contribute no more than an additional 1 nA each to the patient auxiliary current.The total 54 nA maximum is well under the allowed 0.01 mA auxiliary current for CFtypeapplied parts. If the application permits it, however (e.g., if the skin–electrode interfacehas a sufficiently low impedance), it is a good idea to add resistors larger than 300 k inseries with the patient connections. These resistors would effectively limit the auxiliary currentflowing through the patient to less than 0.05 mA in case a fault in IC1 or in D1–D4short-circuit the patient’s connection with one of the isolated power rails.Depending on the biopotential signal being amplified, either dc or ac coupling arerequired. For dc coupling, IC1 is referenced to the isolated ground plane I G1 , which alsoserves as the patient common input. Since the INA110 has FET inputs, bias currents drawnthrough input source resistances have a negligible effect on dc accuracy. However, a returnpath must always be provided to prevent charging of stray capacitances which may saturatethe INA110. If this amplifier would be needed to amplify completely floating sources
Figure 3.2 A universal differential biopotential amplifier serves as an example of designing medical electronic instruments for safety. AnINA110 instrumentation amplifier acts as an impedance buffer and provides gain to weak electrical activity detected by electrodes on thepatient’s body. For use as a single-lead ECG amplifier, a protection network is used to limit currents during defibrillation or electrosurgeryprocedures. Galvanic isolation for the amplified signal is provided by an ISO107 isolation amplifier IC. This IC also provides isolated powerto operate the circuitry of the applied part.103
104 <strong>DESIGN</strong> <strong>OF</strong> SAFE <strong>MEDICAL</strong> DEVICE PROTOTYPESor capacitively coupled sensors, a 10-M resistor to the isolated ground plane from eachinput should be used. When ac coupling is desired, IC4A, R8, and C5 are used to offsetIC1’s reference to suppress a baseline composed of components in the range dc to 0.48 Hz.Also for ac coupling, any remaining baseline at IC1’s output may be eliminated by a highpassfilter (1.59 Hz at 3 dB) formed by C6 and R9.IC1’s output signal is amplified by IC4b. Notice that the gain of this stage is fixed at101. Galvanic isolation is provided by IC3, a Burr-Brown ISO107 isolation amplifier IC.This type of IC resembles an operational amplifier but is designed with an internal isolationbarrier between its input and output pins. The ISO107’s signal channel has a smallsignalbandwidth of 20 kHz and provides an isolation barrier rated at a continuous 2500 V.In addition to providing a signal channel across the isolation barrier, the ISO107 has aninternal dc/dc converter which powers the isolated side of the ISO107 circuitry and providesisolated power (15 V at 15 mA typical) for the rest of the circuitry of the appliedpart (i.e., IC1 and IC2). The isolation rating of the barrier for the dc/dc converter is thesame as that for the signal channel. In total, the 60-Hz leakage current through IC3 doesnot exceed 2 A with 240 V ac applied across its isolation barrier. The output gain of IC3is selected through jumpers JP7–JP9 to provide gains of 1, 10, or 100. IC3’s output is thenlow-pass filtered by IC4C. With the component values shown, the filter has a cutoff frequencyof 300 Hz. You may recalculate these values to match the bandwidth required byyour application.In one position of SW1, the filter’s output is buffered directly by IC4D and presented tothe output of the biopotential amplifier. In the other position, SW1 redirects the output ofIC4C to a tunable-frequency notch filter before being buffered by IC4D. This makes it easyto eliminate 50/60-Hz power line hum that may have been picked up through commonmodeimbalances between the differential patient connections.As shown up to this point, patient leakage and auxiliary currents have been kept withinallowed limits by virtue of appropriate selection of the components for the circuit. However,appropriate layout and interconnection are as important in ensuring a safe design. To do so,every conductive point belonging to the isolated portion of the circuit must be separated fromevery conductive point in the nonisolated side of the circuit by the required air clearance andcreepage distances corresponding to reinforced insulation at the rated working voltage. Thelayout of a prototype instrument that incorporates this ECG amplifier is shown in Figure 3.3.Since there is a 30-mm separation between the closest pins across the ISO107 isolationbarrier, and considering that the internal isolation barrier is rated at a continuous 2500 Vat 60 Hz, the standards would consider this barrier to be equivalent to 1000 V ac–rated reinforcedinsulation. This separation would also be needed between all other isolated andnonisolated points of the circuit. Most commonly, a biopotential amplifier is operated inenvironments where the power line voltage is the highest potential of concern and has amaximum rated value of 240 V RMS . According to Table 3.1, this would require an air clearanceof 5 mm and an 8-mm creepage distance. Remember that these distances also applyto the separation of any point on the isolated side and any conductive fastening means inconnection with any nonisolated part of a medical instrument.Amplifying the electrical activity produced by the heart introduces a number of additionalrequirements addressed by the front-end protection circuit shown in Figure 3.2.Physicians conducting electrophysiological diagnosis and therapy of conditions involvingthe heart assume the possibility of ventricular fibrillation during a procedure. Revertingfibrillation back into a normal rhythm driven by the sinus node of the heart involves brieflyforcing high current through the heart. To overcome tissue resistivity, this implies thedelivery of a high-energy, high-voltage pulse.Typical external defibrillators deliver this pulse by discharging a 32-F capacitor chargedup to 5000 V dc through a 500-H inductor directly into paddle electrodes placed on thechest of the patient, who may be assumed to act as a 100- resistor. A sizable fraction of
<strong>DESIGN</strong> EXAMPLE: ISOLATED DIFFERENTIAL ECG AMPLIFIER 105Figure 3.3 Layout of an instrument that incorporates the ECG amplifier of Figure 3.2. Note thatthe gap in components and conductors which forms the insulation barrier is traversed only by theISO107 isolation amplifier. An external ELPAC model MED113TT medical-grade power supply isused to power the circuit from the 120 V ac power line.the defibrillation pulse may appear at the ECG recording electrodes as well as between theisolated patient ground and the power line ground. The front-end protection circuit places330-k resistors (R4 in series with R6, R25, and R5 in series with R7) in series with thepatient leads to limit the peak defibrillator input current to under 10 mA. For this application,2-W carbon-composition high-voltage-rating resistors are chosen, to withstand theseveral dozen watts of instantaneous power that may be dissipated during each defibrillationpulse.Since voltages close to the full 5000-V defibrillator capacitor initial voltage couldappear across these resistors, care must be taken to ensure that current does not find analternative path by producing a spark or by creeping across the printed circuit. The insulationrequired to withstand the peak voltage of the defibrillator pulse should be chosen tobe a minimum air clearance of 7 mm and a minimum creepage distance of 1 2 mm. Thisseparation would also apply to the isolation barrier between the applied part and all otherparts of the medical instrument.A second consideration must be made for equipment that may be used in the operatingroom. Here the applied part of the instrument may be exposed to very strong RF currentscoming from an electrosurgery (ESU) unit used for either cauterizing wounds or cuttingtissue. Usually, continuous-wave or gated damped sinusoids are applied between a largeareaelectrode on the patient’s back and the scalpel electrode. Through RF heating, tissuesare cut and blood is coagulated, causing small ruptured vessels to close. The RF componentof the ESU waveform typically is within the range 200 kHz to 3 MHz, and powerlevels into a 500- load range from 80 to 750 W. Open-circuit voltages range from approximately300 V and can be as high as 9 kV.If the circuit of Figure 3.2 were used in the presence of ESU, the path of RF leakagecurrent would probably be from the ESU electrodes into one or more of the device’s patient
106 <strong>DESIGN</strong> <strong>OF</strong> SAFE <strong>MEDICAL</strong> DEVICE PROTOTYPESelectrodes, through the coupling capacitance of the ISO107, through the stray capacitanceof the power supply transformer, into the power line, and back through the stray capacitanceof the ESU generator’s power transformer. To deal with these RF currents, medicalelectronic equipment often includes filters that attenuate RF signals before they can bedetected by the circuit’s nonlinearities. In our front-end protection circuit, RF appearing atthe ECG and ECG electrodes is sinked to the isolated ground by C2 and C3. C4 is usedto eliminate any remaining RF that can be demodulated differentially by D1–D4 or IC1’scircuitry. Here again, currents driven by very high RF voltages must not find alternativepaths such as corona discharge or creepage, and for these reasons, appropriate spacingsmust be observed.ST<strong>AND</strong>-ALONE ANALOG ISOLATORSThe previous design example demonstrated the use of the ISO107 isolation amplifier embeddedwithin a circuit to provide a signal path across the isolation barrier. In many cases, havinginstead a self-contained general-purpose isolation module like that of Figure 3.4 cansimplify the design of prototype and experimental equipment. The circuit diagram for sucha module is shown in Figure 3.5. This module was designed as a stand-alone isolation boardto protect subjects connected to isolated biopotential amplifiers from lethal ground fault currentsas well as those originating from defibrillator pulses. The heart of the module is IC1,an Analog Devices’ 284J isolation amplifier. This device meets leakage standards of 2 Amaximum at 115 V ac, 60 Hz. This performance results from the carrier isolation technique,which is used to transfer signals and power across the isolation barrier, providing a maximumisolation of 2500 V RMS at 60 Hz for 1 minute, and 2500 V p-p maximum continuous ac, dc,or 10-ms pulses at 0.1 Hz.Figure 3.4 A stand-alone signal isolator can be built using an Analog Devices’ 284J isolationamplifier. The input voltage range for this module is 5V differential at unity gain. However, thismodule can also be used for the direct low-level amplification of biopotential signals with a low inputnoise 10 V P-P , medium input impedance 10 8 , and high CMR (110-dB inputs to output, 78-dBinputs to guard). The module can generate isolated power for input circuitry, such as biopotentialsignal buffer preamplifiers or instrumentation amplifiers.
-15VC6+15VC5.01uFIC2.01uF UA741 -15V +15V234 5-+6123456J3+15 VGND-15 VGNDOutputSignal ComGuard-In+InJ1+VisoGNDiso-VisoGuard123JP1-1JP1-2J2JP1-34321R1510KGain5612IC1284J+-3C1.01uFC2.01uF478019R2200C4.01uFC3.01uFC7.01uF7 1+15VR325KR410K, 1%R510K, 1%+15V-15V+ C86.8uF, 35V+ C96.8uF, 35VFigure 3.5 This isolation amplifier meets leakage standards of 2.0 A at 115 V ac, 60 Hz, providing a maximum isolation of 2500 V RMS at60 Hz for 1 minute, and 2500 V P-P maximum continuous ac, dc, or 10-s pulses at 0.1 Hz.107
108 <strong>DESIGN</strong> <strong>OF</strong> SAFE <strong>MEDICAL</strong> DEVICE PROTOTYPESBipolar input signals, present at J1-3, and referenced to isolated ground at J1-2, areintroduced into the isolated signal input of IC1. IC1’s gain can be set in the range 1 to 10by changing the value of a resistor connected between JP1-1 and JP1-2 according to100kgain 1 10.7k Ri (k)To preserve high CMR, this resistor and all connections to it must be guarded with ashield connected to JP1-3. Best performance is achieved by placing a shorting jumperbetween JP1-1 and JP1-2 and operating the circuit at a gain of 10. Leaving JP1 openresults in unity gain.The bandwidth supported by the 284J is dc to 1 kHz (small signal), dc to 700 Hz (fullpower G 1), and dc to 200 Hz (full power G 10). IC1’s output is buffered by IC2, aunity-gain buffer, in order to drive low-impedance loads connected between the module’soutput at J3-5 and nonisolated ground at J3-6. Trimmer R3 is used to zero the output offsetvoltage over the gain range. IC1’s output is low-pass filtered to roll off noise and outputripple. Cutoff (3 dB) of the low-pass filter is given by1f 3dB (Hz) 2C4(F) 1000 Use of a 1-F capacitor results in a cutoff frequency of approximately 160 Hz.The input voltage range for this module is 5 V differential at unity gain. However, thismodule can also be used for the direct low-level amplification of biopotential signals witha low input noise 10 V p-p , medium input impedance of 10 8 , and high CMR (110-dBinputs to output, 78-dB inputs to guard). Differential measurement of biopotential signalsis achieved between J1-3 (noninverting input) and J1-2 (inverting input), while CMR isoptimized by connecting J1-1 to a distant reference electrode. If the module is used as abiopotential amplifier, the leads to the electrodes should be low-loss low-capacitance coaxialcables, whose shields are connected to J1-1. This module should be operated using asymmetric 15 V regulated power supply (J3-1 15 V, J3-2 nonisolated ground,J3-3 15 V). Dual 8.5 V dc at 5 mA of isolated power are provided at J2. These linesmay be used to power floating input circuitry such as biopotential signal buffer preamplifiersor instrumentation amplifiers.THREE-PORT ISOLATIONMost isolation amplifier ICs on the market that contain an internal dc/dc converter topower the isolated side of the amplifier (as well as support circuitry) are labeled as inputor output isolation amplifiers. This refers to the direction in which power is sent across theisolation barrier. An input isolation amplifier thus powers the isolated input side of theamplifier through an internal isolating dc/dc converter while operating its output side fromthe same source that powers the dc/dc. Conversely, an output isolation amplifier uses thepower directly to supply the input side of the amplifier and the dc/dc converter, while theoutput of the dc/dc is used to power the isolated output stage of the amplifier. Since mostisolation amplifiers with internal dc/dc converters have additional power capacity, inputisolation amplifiers typically make extra power available on the isolated input side for drivingexternal signal conditioners or preamplifiers, while an output isolation amplifier makesextra power available on the isolated output side for driving external loads.Although most applications in medical devices require input isolation amplifiers, thereare cases in which a signal generated by the device is required to be sent to a floating appliedpart. For example, a stimulus waveform may be generated using a D/A on a nonisolated sideof the device and delivered to a stimulation circuit using an output isolation amplifier. Aninteresting isolation amplifier that can fulfill both roles is Analog Devices’ AD210. This
ANALOG SIGNAL ISOLATION USING OPTICAL ISOLATION BARRIERS 109component has a true three-port design structure, which permits it to be applied as an inputor output isolator, in single- or multichannel applications. In the AD210, each port (input,output, and power) remains independent, with 2500 V RMS (continuous) and 3500 V p-pisolation between any two ports.In the circuit of Figure 3.6, an AD210BN is used to power and isolate a general-purposeinstrumentation biopotential amplifier front end. Biopotential signals detected by electrodesconnected to input connector J1 are dc-coupled to the inputs of an AD620 instrumentationamplifier via input resistors R5 and R8. Low-leakage diodes D1–D4 are used to protect theAD620 from high-voltage transients. Resistors R3 and R9 provide a dc path for bias currentswhenever the amplifier is used to detect signals from capacitive sensors.IC2 is used to buffer the offset voltage set by trimmer potentiometer R10. The offset levelis fed directly to the reference pin of the instrumentation amplifier. Gains of 1, 2, 10,and 100 are selected through jumpers JP1–JP3. The output of the instrumentation amplifieris fed to the input of the AD210 isolation amplifier. The output of the isolation amplifieris filtered by the active low-pass filter formed around IC4. Isolated 15 V to power IC1 andIC2 is generated by the AD210. The AD210 also produces a separate, isolated 15 V whichis used to power IC4. A single 15 V at 80 mA supply is all that is needed to power the completecircuit, thanks to the AD210’s three-port feature. Figure 3.7 shows an implementationof this circuit where the various insulation barriers can be seen clearly.ANALOG SIGNAL ISOLATION USING OPTICAL ISOLATION BARRIERSHigh performance usually comes at a high price, and the ISO107, 284J, and AD210BN areno exceptions. The unit price for each of these is over $100, making their use prohibitive inmany low-cost designs as well as in instruments that involve a large number of analogsignals crossing the isolation barrier. In these cases, analog isolators can be built using lowcostoptoisolators as isolation channels. Optoisolators or optocouplers operate by emittingand detecting modulated light. An input current drives a light-emitting device internal to theoptocoupler, and an internal photodetector drives the output circuitry. Optoisolators usuallyconsist of an LED and a phototransistor which are galvanically isolated from each other andare located opposite each other in a lighttight package.The simplest form of optical isolation for an analog signal is implemented by the circuitof Figure 3.8. In this circuit, an input voltage is converted by IC1 and transistor Q1 toa proportional current to drive a LED. The light output of the LED is proportional to thedrive current between 500 A and 40 A. However, since the best linear behavior for opticaloutput flux versus input current occurs in the range 5 to 20 A, offset is introduced inthe voltage-to-current conversion. A 1.2-V reference voltage is generated across referencediode D1. Resistor R5 and potentiometer R6 select the fraction of the reference voltagethat should be used as an offset. The voltage divider formed by resistors R1 and R2 andpotentiometer R3 are used to scale the input signal.The LED D2 and a photodiode D3 are mounted across from each other inside a pieceof dark PVC pipe. The silicon photodiode, operating as a light-controlled current source,generates an output current that is proportional to the incident optical flux supplied by theLED emitter. Translating the photodiode current back to a voltage is done with series resistorR10. IC2 buffers the voltage across the current-sensing resistor and cancels the offsetcaused by keeping the LED always illuminating the photodiode. Although operation of thiscircuit seems straightforward, its performance leaves a lot to be desired, especially as faras stability is concerned. The problem is that the optical output of a LED as a function ofdrive current is very unstable, changing widely with the LED’s age, temperature, and thedynamics of the drive current. For this reason, this circuit is not recommended except forapplications where good linearity and precision are not required.
SIG OUTSIG COM+15PWR COMJ212J312I2FL1NFM51R1 32R510KFDH300I1C13.01uF+15V1FB+VOSS+15V1C6ICOM-VOSS-15V2FDH300.01uF-15V1C7C10C8D3C16C17C18C19.01uF 10uF .01uF 10uFR8.01uF10uF.01uF10K 10uFI2FDH300D2D4C2.01uFI1J1-15V112321 3NFM51RFL 2<strong>OF</strong>FSET ADJ.R10100K, 10T312C14.01uFR111MR310MI1I1+15V1234 5-+7 1+15V1IC2TL071/ SO6I1C15.01uFJP11 2JUMPERJP21 2JUMPERJP31 2JUMPERI1 -15V1+15V1-15V1FDH300+15V1-15V1D1R910MI1R1210K3274+-815-15V1IC1AD6206No Jumpers Installed,Gain X1R1 49.9KR2 5.49KR4 499I1+ C5I1GainX2GainX10GainX100Input IsolationMaintain 7mm AirClearance, 12mmCreepage+IC3AD210_BN191714151618+IN-IN+VISS-VISS30 29VOOCOM3412+I2R65.49K++15V2I2R724.3KOutput IsolationMaintain 7mm AirClearance, 12mmCreepageC4.01uFC1.047uF500Hzlpf32+15V27 1+-4 5-15V2Power IsolationMaintain 7mm AirClearance, 12mmCreepage6IC4TL071/SOC1110uFI2I2C3.01uFPWRPWRCOMC9.01uF+C12.01uFFigure 3.6 In this biopotential amplifier, each port (input, output, and power) of the AD210 isolation amplifier remains independent with2500 V RMS (continuous) and 3500 V P-P isolation from any of the other ports.110
LINEAR ANALOG ISOLATION USING OPTOISOLATORS 111Figure 3.7 This implementation of the general-purpose biopotential amplifier of Figure 3.6 requires a single supply of 15 V at 80 mA,thanks to the AD210’s three-port feature.Figure 3.9 shows a circuit that implements an interesting way of somewhat linearizingthe response of an optoisolator while simplifying the circuitry needed to introduce offsetto pass bipolar signals. This isolated EEG amplifier is an adaptation of a circuit by Porr[2000]. Here, an Analog Devices AMP01 instrumentation amplifier is used as the highinput-impedancefront-end amplifier for the biopotentials collected from EEG scalp-surfaceelectrodes. The gain of this stage is 20. IC1’s output is high-pass filtered by C5, C6,and R3 to introduce a 3-dB cutoff frequency of 0.32 Hz. A selectable-gain stage is implementedaround op-amp IC2 to boost IC1’s output signal approximately 100, 200, 500, or1000 times. A Sallen–Key second-order low-pass filter built around IC3A is then used tolimit the bandpass of the EEG amplifier to approximately 34 Hz.IC3B drives the LEDs of optoisolators IC4 and IC5. The phototransistor in IC4 is usedto set the inverting input of IC3B such that the LED is driven to a point that balances thesignal at IC3’s noninverting input. When the phototransistor in IC5 is not illuminated, itscollector is pulled up to the nonisolated positive supply rail by R21. However, as signalscause IC3B to drive the LED, the phototransistor pulls the collector toward the nonisolatednegative supply rail. The isolated signal is high-pass filtered by C18 and R22 and bufferedvia IC8 before being presented to the output.LINEAR ANALOG ISOLATION USING OPTOISOLATORSA way of using an optoisolator for analog signals while maintaining good linearity is firstto convert the analog signal into a pulse train of variable frequency (or pulse width), whichis then used to drive the optoisolator. At the other side of the optoisolator, the pulse train isdemodulated to render the original signal. Another possibility is to place the optoisolatorwithin a servo loop that makes use of the loop’s error to convey a high-linearity analogsignal. Yet another solution is to convey true-digital data through the optoisolator.The analog isolator circuit of Figure 3.10 works by pulse-width modulating a pulse trainin proportion to the input voltage. As shown in Figure 3.11, an input signal is presented to
112Figure 3.8 The simplest form of optical isolation for an analog signal is implemented by driving an LED with a current proportional to theinput signal. Offset is introduced to operate the LED in the range where optical output flux versus input current is almost linear. A photodiodemounted across the LED inside a piece of dark PVC pipe generates an output current that is proportional to the incident optical fluxsupplied by the LED.
LINEAR ANALOG ISOLATION USING OPTOISOLATORS 113Figure 3.9 In this EEG amplifier, an extra optoisolator is used to introduce offset automatically to pass bipolar signals and to linearize theresponse of the isolation amplifier. IC3B drives the LEDs of optoisolators IC4 and IC5. The phototransistor in IC4 is used to set the invertinginput of IC3B such that the LED is driven to a point that balances the signal at IC3’s noninverting input. When the phototransistor in IC5is not illuminated, its collector is pulled up to the nonisolated positive supply rail by R21. However, as signals cause IC3B to drive the LED,the phototransistor pulls the collector towards the nonisolated negative supply rail.the differential amplifier implemented by IC1A. This differential amplifier has unity gainand is used to add an offset voltage that is set via potentiometer R3. The input signal is thenlow-pass filtered through R6 and C6 to the dc–65 Hz modulation bandwidth, which can besupported by the pulse-width modulator implemented around IC1B. The pulse-train outputfrom the pulse-width modulator drives an LED inside optocoupler IC2 via transistor Q1.The Optek OPI1264 optoisolator used in this circuit was selected because it has a veryrespectable 10-kV isolation rating (although its UL file rates it at 3500 V ac for 1 minute).At the phototransistor end of IC2, the light pulses generated by the LED are receivedand converted into a replica of the original pulse train through the RC high-pass filterformed by R13 and C8. The circuit centered on IC3A acts as a pulse-train demodulator toreconstruct the original modulating signal, which, depending on the characteristics of theinput signal, may have an offset. Finally, the low-pass filter implemented around IC3Bremoves any remnants of the pulse train’s carrier.
114 <strong>DESIGN</strong> <strong>OF</strong> SAFE <strong>MEDICAL</strong> DEVICE PROTOTYPESFigure 3.10 In this analog signal isolator, the analog signal is converted into a pulse train of variablepulse width, which is then used to drive the optoisolator. At the other side of the optoisolator,the pulse train is demodulated to render the original signal. The large cylinder at the center of theboard is an Optek OPI1264 optoisolator through which isolation levels of 10 kV can be obtained.A similar circuit can be built using an integrated voltage-to-frequency converter. Thecircuit of Figure 3.12 is an application suggested by Analog Devices for its ADVFC32integrated circuit. This chip is an industry-standard, low-cost monolithic voltage-to-frequency(V/F) converter or frequency-to-voltage (F/V) converter with good linearity andoperating frequency up to 500 kHz. In the V/F configuration, positive or negative inputvoltages or currents can be converted to a proportional frequency using only a few externalcomponents. For F/V conversion, the same components are used with a simple biasingnetwork to accommodate a wide range of input logic levels.In an analog isolator circuit, an input signal in the range 0 to 10 V drives IC1, anADVFC32 configured as a V/F converter. Input resistor R1 and offset resistor R2 havebeen selected such that a 0-V input causes IC1 to oscillate at 50 kHz, while a 10-V inputyields an output of 500 kHz. IC2 is a bandgap voltage regulator used to generate the offsetvoltage reference. IC3, a high-frequency optoisolator with a high isolation voltage rating,is used to transmit the frequency-modulated signal generated by IC1 across the isolationbarrier to IC4, an ADVFC32 configured as a F/V converter. Integration for the V/F functionis provided by an internal op-amp that has C12 within its feedback loop. This capacitordefines the frequency response of the isolation amplifier circuit. With 1000 pF, thebandwidth of the amplifier is dc to 3 kHz. The output of the V/F is offset to reproduce theinput range 0 to 10 V by summing a current produced through R9 and R10 by a secondbandgap reference IC5. Prior to exiting the circuit, any remaining carrier is filtered via R6and C13, which form a 3-kHz low-pass filter.In the new generation of analog optocouplers that have appeared on the market, the LEDthey use has widely variable electrical-to-optical transfer characteristics, just as in any otheroptocoupler. However, these optocouplers have a second photodetector, which is used aspart of a feedback loop to stabilize the LED’s optical output. The circuit of Figure 3.13 isvery similar to the simple optical analog isolator of Figure 3.8. The main difference is thatIC1’s output is not simply a current proportional to its input voltage. Rather, part of theLED’s optical flux is detected by the second photodiode and used to provide feedback tothe op-amp current source. Since the stability of a photodiode is not usually a concern, andsince the characteristics of both photodiodes are closely matched during manufacture, the
NON ISO.POWERSignalOutputJP312ISO.POWERSignalInputJP421R350K+9Viso31JP1212345+15VR16+15V+9VisoR14C10 C11+9Viso3.3K.01uF 10uFR15IC2 C88C12 C13143.01uF10uF10KC1421R190.1uF2.21K2 3100K 8IC1BIC1A10uFR6R13TL08234 TL0821TL082 24.3K6D1OP I1264C 10K427R20Q152N3904C16 C17R21C61K1N4148100K.01uF 10uF40.1uF-15V8C18 C19R22R24330R23.01uF-9Viso10uF100K100KR25R26D37.5KR274.75K1N5232B100KD5I-9VisoIR28100KC200.1uF+-+9VisoII++II-+5.6V5.6VISOLATED SIDE1N5232BI+IINON ISOLATED SIDE+- IC3A++12V12VR1739.2KD21N5242BD41N5242BR1839.2KC15.047uFC90.1uF+15V56-15V84+-IC3B7TL082JP212345-9VisoIFigure 3.11 In this pulse-width modulation optical isolation amplifier, the input signal is first offset by IC1A. IC1B implements the pulsewidthmodulator, which drives the LED of an Optek OPI1264 optoisolator through transistor Q1. The pulse train at the optoisolator’s isdemodulated via IC3A and low-pass filtered by IC3B.115
VoutJ4Non-IsoPower InJ31234+15VISOJ1J21 3 +E EOUT2-E+15VISO-15VISO+5V +15VC1212R142.2KC20.01uF+15VISO-15VISOC50.1uFC147pFIC40.1uFIC2AD580/TOIC1ADVFC32141 +IN VOUT-IN FOUT10COMPIN5CAP124 +VS-VS11137C31000pFR2100KC60.1uFIR31.5K23IC3HCNW26118 56R1112KR52.2KIC4ADVFC3213 147 VOUT +IN 1FOUT -IN10COMPIN5CAP1211+VS-VS4C100.1uFGainC1147pFR710K+15V-15VC90.1uFR838.3K1000pFR1090.9K2R65.11KR920KEOUTOffsetIC5AD580/TO13+E-EC130.01uFGND+5VC70.1uFR41KC81000pFC14-15V12GND+5V+15V0.01uFIIsolatedSideNon-IsolatedSideFigure 3.12 An optical isolation amplifier can be built using a voltage-to-frequency (V/F) converter that drives the optoisolator and a frequency-to-voltage(F/V) converter to recover the original signal. The ADVFC32 can be used to implement both functions. An input signalin the range 0 to 10 V causes the LED inside the optoisolator to be flashed at a frequency between 50 and 500 kHz.IsoPowerInVin(0-10V)116
ISOLATEDPOWERINPUTJ4ISOLATED SIDENON-ISOLATED SIDE1 VCC234 +9V_ISO-9V_ISO+9V-9V+9VJ3123C10NON-ISOLATEDPOWER INPUTLM385-1.2-9V_ISO48ISOLATEDSIGNALINPUTR106.8kD2R910kJ1BNC12II VCC<strong>OF</strong>FSETADJUSTR82kR318kGAINADJUSTIC50.1uFIR41.5kR51kR72k-9V_ISO234 5C2.01uF+9V_ISOIIC120pFR21k+9V_ISO213R610k-9V_ISOR11kQ12N2222I+ C447uF341IC22 5IL300876+ C647uFR142kMaintain: 5mm AirClearance8mm CreepageDistanceR156.8kR1220kIC3LM74123-9V4 5-+-+7 1C7.01uF6IC1LM741I+ C310uF+9VR1110kReinforced IsolationBarrier7 1+9VR1318kC9.01uF6C8.01uF8.01uFD14LM385-1.212J2BNCNON-ISOLATEDOUTPUTFigure 3.13 Unlike the open-loop isolation amplifier of Figure 3.8, the output of IC1 in this closed-loop circuit is not simply a current proportionalto its input voltage. Rather, part of the LED’s optical flux is detected by the second photodiode and used to provide feedback to theop-amp current source. Since the stability of a photodiode is not usually a concern, and since the characteristics of both photodiodes areclosely matched during manufacture, the transfer characteristic of the complete circuit is highly linear regardless of LED nonlinearity, aging,temperature, or LED drive current dynamics.117
118 <strong>DESIGN</strong> <strong>OF</strong> SAFE <strong>MEDICAL</strong> DEVICE PROTOTYPEStransfer characteristic of the complete circuit is highly linear regardless of LED nonlinearity,aging, temperature, or LED drive current dynamics.In this circuit, the LED driver is prebiased by introducing a negative offset voltage into theinverting input of op-amp IC1. The feedback photodiode sources current to R7, which is translatedinto the control voltage for the servo loop. The op-amp will drive transistor Q1 to supplyLED current to force sufficient photocurrent to keep the voltage at the noninverting input ofIC1 equal to that at its inverting input. The output photodiode is connected to a noninvertingvoltage follower amplifier. The photodiode load resistor R11 performs the current-to-voltageconversion. IC3 is used to buffer R11 as well as to zero-offset the output signal’s baseline.Note that none of the optocoupler-based isolators described above generate their ownisolated power. Once an isolation dc/dc converter has to be added, and considering the limitedperformance of these circuits, applications that require only one or two isolated signalchannels may be better off using commercial, self-contained analog isolation ICs. Isolatorslike the optocoupler circuits shown are most often found in multichannel applications,where the cost of a large number of self-contained isolation ICs would be prohibitive.DIGITAL ALTERNATIVE TO SIGNAL ISOLATIONThe large majority of modern medical electronic instruments make use of either an embeddedmicrocomputer or an external PC for control, data processing, and display. This impliesthat in most cases, an analog-to-digital converter is used at some point within the instrumentto support data acquisition functions. The circuit of Figure 3.14 places the A/D converter indirect connection with the applied part of the medical instrument, and relays digital ratherthan analog signals across the isolation barrier. This alternative over analog signal isolationhas the advantage that the additional noise, nonlinearity, and complexity of the latter can beavoided by translating signals to digital format early in the process. Furthermore, optoisolatorsfor high-speed digital signals are inexpensive and widely available. In addition, serialdata formats can be used to minimize the number of digital signals that must be communicatedconcurrently through the isolation barrier.Many modern high-end medical instruments make extensive use of this philosophy. Ifyou have the opportunity, examine the circuit schematics of one of today’s electrocardio-Figure 3.14 The majority of modern medical electronic instruments make use of either an embeddedmicrocomputer or an external PC for control, data processing, and display, meaning that an A/Dconverter is used at some point within the instrument to support data acquisition functions. Thiscircuit places the A/D converter in direct connection with the applied part of the medical instrument,and relays digital rather than analog signals across an optical isolation barrier.
DIGITAL ALTERNATIVE TO SIGNAL ISOLATION 119graphy instruments. You will probably find an elegant design comprising instrumentationamplifiers for each lead followed directly by an A/D converter and optical isolation leadingto a DSP microprocessor. Often, the complete applied part is contained within a“medallion” to which the patient leads are directly connected, and digital signals to andfrom the embedded microcomputer are relayed through optical fiber.The sample circuit of Figure 3.15 is not as complex as those of high-end commercialinstruments but provides a very simple and convenient interface between analogoutputapplied parts and most PCs on the market. Instead of connecting to the computer’sFigure 3.15 A MAX187 low-power 12-bit A/D converter IC forms the core of the isolated A/D converter module. A two-wire serial interfaceconveys data from the MAX187 through optoisolators back to the PC through the printer port. The PC also controls an isolated signalmultiplexer that allows one of eight analog signals to be presented to the input of the A/D.
120 <strong>DESIGN</strong> <strong>OF</strong> SAFE <strong>MEDICAL</strong> DEVICE PROTOTYPES*CSSTARTCONVERSION>0.25µsSCLKDOUT1 2 3 4 5 6 7 8 9 10 11 12 13D11 D10 D9 D8 D7 D6 D5 D4 D3 D2 D1 D0END <strong>OF</strong>CONVERSION>8.5 µsFigure 3.16 Data acquisition and serial protocol timing for the MAX187. A/D conversion is initiated by a falling edge on the *CS line. Afterconversion, data are read out in serial format, shifted from the sequential-approximation register on each falling-edge transition of SCLK.expansion bus, it plugs into one of the parallel printer ports, which is used as a serial I/Ofor an eight-channel A/D converter. As shown in the diagram, at the heart of the circuitis a MAX187. This IC is one of Maxim’s single-chip A/Ds featuring a 12-bit 8.5-ssuccessive-approximation converter, 1.5-s track-and-hold, on-chip clock, precision4.096-V reference, 1 LSB nonlinearity, and high-speed three-wire serial interface.2One of eight isolated analog signals to be measured is presented to the analog input lineAIN of the MAX187 by way of a DG508A analog multiplexer IC. Voltages within therange 0 to 4.096 V can be converted by the A/D into distinct digital codes for every 1 mVof change. MAX187’s A/D conversion initiation and data-read operations are controlled bythe *CS (chip select) and SCLK (serial clock) lines. As shown in Figure 3.16, an A/D conversionis initiated by a falling edge on the *CS line. At this point, the track-and-hold holdsthe input voltage and the successive-approximation process begins. The start of conversionis acknowledged by the MAX187 changing the state of the DOUT line from highimpedance to the low state. After an internally timed 8.5-s conversion period, the end ofconversion (EOC) is signaled by the DOUT line going high.Once a conversion is completed, data can be obtained in serial format, shifted from thesequential-approximation register on each falling-edge transition of SCLK. Since there are12 bits, a minimum of 13 falling-edge pulses are required to shift out the A/D result. Isolationbetween the PC’s printer port and the MAX187 is provided by IC4–IC7. Bits 1 and 2 of thePC’s LPT 8-bit output port (hex address 378 for LPT1:) are toggled by software to implementthe control portion of the MAX187 serial protocol. Bit 6 of the printer status port register(hex address 379 for LPT1:) is used to receive the serial data from the MAX187. Bits3–5 of the output port are used to control the analog signal multiplexer. Bit 0 of the outputport is an auxiliary line that may be used in the control of the applied part’s circuitry.Power for the MAX187 must be supplied from a patient-contact-rated isolated powersupply capable of delivering 5 V. A pi filter formed by C1–C4 and L1 ensures a clean supplyto the A/D. In addition, you may notice that two separate isolated ground planes, oneanalog and one digital, are shown in Figure 3.15. Ideally, the signal ground plane, used asthe reference for the analog input signal, should be constructed to shield the analog portionsof the A/D and signal multiplexer: namely, the input network and voltage reference filteringand decoupling capacitors. The analog and digital ground planes should be connected at asingle point, preferably directly to the isolated ground line supplying the circuit.S<strong>OF</strong>TWARE FOR THE ISOLATED A/DThe sample program that follows is for driving the isolated A/D converter from the printerport of a PC. The program flow starts by initializing the ports. Notice that use of the standard
S<strong>OF</strong>TWARE FOR THE ISOLATED A/D 121LPT1: is assumed, and you may need to change the output port and status port locations tosuit your specific installation.' ATODSAFE.BAS is a QuickBasic sample program to acquire data using' the 8-channel, isolated 12-bit A/D converter. The use of LPT1:' is assumed.'' Printer port locations' -----------------------------CONST prinop &H378 ' Printer Output Port (could be &H278 or &H3BC)CONST prinstat &H379 ' Printer Status Port (could be &H279 or &H3BD)'' Define control pin locations' ------------------------------------------CONST aux 1, notcs 2, sclk 4, sela 16, selb 32, selc 64'' Initialize' ----------OUT prinop, 0 ' clear printer portCLS' clear screenINPUT “Please input channel to acquire ”; chan' determine control bits for desired channelselas (chan <strong>AND</strong> 1) * selaselbs (chan <strong>AND</strong> 2) / 2 * selbselcs (chan <strong>AND</strong> 4) / 4 * selc'' Acquisition and display control' -------------------------------start:SCREEN 2 ' CGA graphics mode 640 200GOSUB acquire' determine first display pointy INT((4.096 vout) * 45) 10' compute position of startingpointstart1:CLS' refresh screenLOCATE 2, 2: PRINT “4.096V”;' place y-axis labelsLOCATE 7, 2: PRINT “3.000V”;LOCATE 13, 2: PRINT “2.000V”;LOCATE 19, 2: PRINT “1.000V”;LOCATE 25, 2: PRINT “0.000V”;PSET (60, y)' place first sampleFOR x 60 TO 640' horizontal sweepGOSUB acquire' acquire a sampley INT((4.096 vout) * 45) 10 ' compute position on screenLINE (x, y)' display dataIF INKEY$ “ ” THEN GOTO progend ' press any key to escapeNEXT x' next sampleGOTO start1' start a new screenprogend:'
122 <strong>DESIGN</strong> <strong>OF</strong> SAFE <strong>MEDICAL</strong> DEVICE PROTOTYPES' Leave program' -------------OUT prinop, 0SCREEN 0END' clear printer port' return to text mode screenacquire:'' Acquisition loop' ----------------OUT prinop, selas selbs ' keep CS’ deassertedselcs notcsconvert:OUT prinop, selas selbs selcs ' convert by asserting CS’loop1:bit (INP(prinstat) <strong>AND</strong> 64) / 64 ' read status port and filter DOUTIF bit 0 THEN GOTO loop1' wait for EOC signaldat 0' clear A/D accumulatorFOR clocknum 11 TO 0 STEP –1' clock 12 bits seriallyOUT prinop, selas selbs ' clock pulse rising edgeselcs sclkOUT prinop, selas selbs selcs ' clock pulse falling edgebit (INP(prinstat) <strong>AND</strong> 64) / 64 ' read status port and filter DOUTdat dat (2 ^ clocknum) * bit ' accumulate from bit 11 to bit 0NEXT clocknum' next bitOUT prinop, selas selbs ' one more clock to reset A/Dselcs sclkOUT prinop, selas selbs selcsOUT prinop, selas selbs ' deassert CS’selcs notcsvout dat * .001' translate A/D data to VoltsRETURNThe program is presented only as an example and for the sake of simplicity will run theA/D converter as fast as the PC is able to drive its lines. Sampling rate control could beimplemented either by inserting for-to loops adaptively to introduce controlled delaybetween samples [Prutchi, 1996] or by controlling the acquisition process from interruptsgenerated by high-resolution hardware timing [Ackerman, 1991–1992; Schulze, 1991].The actual acquisition subroutine starts by setting up the multiplexer while keeping*CS deasserted. Conversion for the channel selected is then initiated by asserting *CSand polling for the end-of-conversion signal before attempting to read the conversiondata. At this point, the A/D accumulator variable is cleared, and each of the 12 bits isclocked-in serially. The value of each bit is read from the status port and is multiplied bythe decimal value of its binary position before being accumulated. Finally, one moreclock pulse is inserted to reset the A/D, the *CS line is deasserted, and A/D data are translatedto volts.ISOLATED ANALOG MULTIPLEXERThe number of channels that can be acquired through the isolated A/D can be expandedby using additional multiplexers. Figure 3.17 shows a PCB that implements a 64-channel
POWER SUPPLIES 123Figure 3.17 The number of channels that can be acquired through the isolated A/D can beexpanded by using additional multiplexers. This circuit implements a 64-channel analog signal multiplexerwith isolated control.analog signal multiplexer with isolated control. Through its use, up to 64 high-level analogsignals may be connected selectively to an A/D or other acquisition and recordinginstrumentation. Signals may originate from biopotential amplifiers, physiological sensors,or a combination of both.The channel addressing is controlled digitally through a parallel asynchronous input.Optical isolation is implemented onboard to maintain patient-contact-rated isolation betweenthe analog electronics and the digital control. Additional multiplexer circuits may be stackedto increase the channel capability of a system. In PC-based data acquisition systems, thisboard may be used to collect analog signals from up to 64 channels through a single analoginput of the A/D. The digital control is easily obtainable from a parallel output port availablein most every PC data acquisition board.Typical multichannel biopotential signal acquisition applications include topographicbrain mappers, body potential mapping (BPM) ECG, the recording of surface arrayEMG signals, and so on. The signal range for the DG508 multiplexers in the circuit ofFigure 3.18 is 12 V with a bandwidth of at least 50 kHz. The in–out resistance ofa selected channel is less than 600 . Scanning of an array can be done at a maximumfrequency of 1000 channels/s. Channel selection is accomplished via optoisolators,which can be driven directly by TTL logic. The circuit requires 12 V isolated powerto operate.POWER SUPPLIESAs Figure 3.1 showed, having reinforced insulation between the applied part and everyother part of the medical instrument does not mean that similarly strong insulation is notneeded between a mains part and other live or nonlive parts besides the applied part. Thisimplies that although you may be using a component which itself powers the applied partacross an appropriate isolation barrier (e.g., ISO107, 284J), the instrument’s power supplymust still meet the same requirements as a safety isolation transformer.
124 <strong>DESIGN</strong> <strong>OF</strong> SAFE <strong>MEDICAL</strong> DEVICE PROTOTYPESFigure 3.18 Using this circuit, up to 64 high-level analog signals may be connected selectively to an A/D or other acquisition and recordinginstrumentation. Signals may originate from biopotential amplifiers, physiological sensors, or a combination. Channel addressing is digitallycontrolled through a parallel, optically isolated asynchronous input. Additional multiplexer circuits may be stacked to increase thechannel capability of a system.To accomplish the required levels of isolation, medical instruments are often designed toincorporate a safety extra-low-voltage (SELV) transformer to derive their operating powerfrom the power line. This type of transformer supplies a voltage under 25 V ac through anoutput winding that is electrically separated from ground and the body of the transformerby at least basic insulation, and which is separated from the input winding by at least doubleinsulation or reinforced insulation.
ADDITIONAL PROTECTION 125In addition, SELV transformers for medical equipment usually have an electrostaticshield that is tightly wound over the insulation of the primary windings. This shieldreduces capacitive coupling between primary and secondary windings, thus reducing leakagecurrents at the power line frequency. The shield is coated with reinforced insulation tocreate a reinforced insulation barrier between the primary and secondary windings. Thecore itself is isolated from the windings by supplementary or reinforced insulation.Another convenient alternative for powering medical instruments is the use of batteries.This substitution not only ensures inherently low leakage currents but can make theequipment highly portable. Considering that you may need to travel all the way to SouthAmerica, Eastern Europe, or Asia to run your first tests, the independence provided by abattery-operated power supply is certainly a welcome blessing for an evaluation prototype.Whatever the choice in power supply, it is generally a good idea to purchase it asan approved OEM (original equipment manufacturer) assembly. This helps you concentrateyour efforts on the core of your instrument rather than having to deal with theheadaches of designing and constructing supplies that perform as required by the safetystandards.Along the same philosophical lines, designing an instrument to make use of preapprovedcomponents can help considerably to receive and maintain safety approval onceyou embark on the production and sale of a medical product. You can still use componentsthat have not been certified by a U.S. Nationally Recognized Testing Laboratory (NRTL,or its equivalent in other countries); however, the assured continuity of safety performancewill have to be investigated for each device to be used. This is complicated further by thefact that once you receive approval for your product, any change in any component willrequire requalification of the complete assembly. Finally, keep in mind that safety standardsusually impose special performance characteristics for certain components, such aspower cords, switches, line filters, fuse holders, optoisolators, CRTs and displays, andprinted circuit boards.ADDITIONAL PROTECTIONRegardless of how carefully you designed your instrument, absolute safety cannot be guaranteedin the real world. Despite all the safety testing and evaluation required by the FDA,medical device manufacturers still pay a premium for insurance to protect themselves fromexposure against liability. For this reason, it often happens that additional or redundanthardware to ensure safety beyond the minimum requirements is cost-effective, since it willbring concomitant savings in insurance costs due to reduced risk.Being extra conservative is especially important at the prototyping stage, since as anentrepreneur you probably do not have the legal and financial umbrella of a large corporationto protect you against an unintentional mishap. Our personal preference is tointroduce, at the very least, an additional but independent layer of protection againstelectrical shock at the patient interface. A very practical method to accomplish this is touse Ohmic Instruments’ Iso-Switch patient-lead fault interruptors. These devices, shownin Figure 3.19, are two-lead semiconductor devices that can be placed, almost transparently,in series with every patient connection to break the patient circuit in case an overcurrentfault develops.As shown in the V–I plot of Figure 3.20, an Iso-Switch patient-lead fault interruptorrated at 10 A acts as a 40-k resistor. Once the trip point of the Iso-Switch is exceeded,the device presents a negative-slope resistance of magnitude equal to that of the positiveslope within the trip boundaries. The trip time under an overcurrent condition is veryfast, typically 10 s. Once the device trips, the resistance of the Iso-Switch increases to
126 <strong>DESIGN</strong> <strong>OF</strong> SAFE <strong>MEDICAL</strong> DEVICE PROTOTYPESFigure 3.19 Ohmic Instruments’ Iso-Switch patient-lead fault interruptors are two-lead semiconductordevices that can be placed, almost transparently, in series with every patient connection tobreak the patient circuit in case an overcurrent fault develops. Various models are available fordifferent applications, with trip currents ranging from 1 A to 100 A. Various operating voltageranges are also offered: 325 V for 115-V ac instruments, 720 V for 220-V ac equipment, andthe DP (defibrillation-proof) series that withstands pulses of 5 kV for 10 ms.IF(µΑ)9.4961.582/div0-6.330-2.0000 2.000VF: 0.4V/ div.Figure 3.20 V–I plot of an IS-10 Iso-Switch patient-lead fault interruptor. Between 7.9 and7.9 A (rated 10 A), the device acts as a 40-k resistor. Beyond the trip point, the resistanceof the Iso-Switch increases to approximately 1000 M at the maximum absolute operating voltageof 325 V.approximately 1000 M at the maximum absolute operating voltage for the device. Oncethe overload is removed, the device resets itself automatically.Various Iso-Switch models are available for different applications, with trip currentsranging from 1 A to 100 A. Various operating voltage ranges are also offered:325 V for 115-V ac instruments and 720 V for 220-V ac equipment; and the DP series
TESTING FOR COMPLIANCE 127designed for applications where defibrillation protection is desired, withstands pulses of upto 5 kV for 10 s. At prices in the range $29 to $34 each (one patient connection), theadded protection provided by these fault interruptors is certainly affordable for evaluationprototypes, and sometimes even for the final design.TESTING FOR COMPLIANCEAlthough the presentation of medical device electrical safety standards above is by nomeans intended to replace the actual standards in scope or in content, it hopefully introducedmany of the most important design requirements covered by the major standards.With medical equipment, however, designing solely for compliance is not sufficient. Theconsequences of a malfunctioning device can be so serious that testing to ensure properperformance is of utmost importance. As such, construction standards are only one aspectcovered by applicable safety standards. The other major aspect defined by the standardscomprises performance requirements.Within this second category, standards specify the multiple tests which are applicableto diverse types of equipment and to identify in detail the criteria for compliance. In fact,almost every construction requirement is linked to a certain performance requirementwhich defines the testing that is performed to verify the acceptability of the construction.In essence, the electrical tests described by the standards are designed to probe insulation,components, and constructional features which could lead to a safety hazard under eithernormal or single-fault conditions.Ground IntegritySince the enclosure of the medical device is the first barrier of protection against the risksof electrical shock, the first test to be conducted is one to assess the integrity of the protectiveground which guards a metallic enclosure and any other grounded exposed part. ULstandard 2601-1 establishes that the impedance between the protective ground pin in thepower plug and each accessible part which could become live in case the basic insulationfailed should be less than 0.1 . The standard also requires that the test be conducted byapplying a 50- or 60-Hz ac current with an RMS value of 10 to 25 A for 5 seconds. Despitethis, however, a reasonable approximation of this measurement can be obtained by usingthe 1-A dc current supplied by the circuit of Figure 3.21. Resistance is then assessed bymeasuring the voltage across the grounding path.Here, op-amp IC2 and power FET Q1 form a voltage-to-current converter that is drivenby a reference voltage set by R6 to maintain a 1-A constant current on a conductor connectedbetween the ground terminal of J5 and connector J4. Power for the circuit is derivedfrom three alkaline D cells, providing a maximum voltage compliance of approximately4.5 V. Because full-range operation of the circuit is accomplished by driving the gate ofQ1 well above its source-to-drain voltage, IC2 is operated from 12 V generated by chargepump IC1.You may notice that J2 and J3 are labeled to be connected to a Kelvin probe. This typeof test probe separates the point through which current is introduced from that throughwhich the voltage across the unknown resistance is measured. The use of such a techniqueis required for low-resistance measurements because it effectively excludes the resistanceof the test leads and avoids the voltage measurement errors that are often introducedby high-current-density concentrations on the current-injection terminals. As shown inFigure 3.22, a large alligator clip (e.g., Radio Shack 270-344) can easily be converted intoa Kelvin probe by replacing the standard metallic axis by a nylon bolt with nylon spacersto isolate the jaws from each other and by covering the ends of the inner spring with a
KELVINPROBEToDVMBT21.5V "D" CellF11.5ASW1POWERR4C6 C15605100uF 4.7uFIC124C1+ C2+C8C11 D3C213C9 0.1uF 0.47uF 1N4001C1- C2-J1D20.22uF0.22uFLED 8Hospital-GradeSHDN76R1GND VOUT3.3k1 2MAX662C34.7uFC741.2V8R6D1C410k,10-Turn7 5 IC2LTC1152.01uF LM385-1.2/TO923R2CurrentSetC50.1uF12VC10.001uF100kR5Female AC Plug1323Q1IRF510/TOJ21GreenJ31GreenVCCBT11.5V "D" CellBT31.5V "D" Cell24 8 16.01uFCurrent SenseResistorR30.1, 1%, 1WJ31RedJ51Black100kFigure 3.21 This simple adapter permits the measurement of milliohm resistances with any digital voltmeter. The circuit operates by generatinga 1-A constant current on the unknown resistance of the ground path between the ground terminal of J1 and connector J2. A voltmeterconnected across the power cord ground conductor measures resistance on a scale of 1 V/.128
TESTING FOR COMPLIANCE 129Voltage-MeasurementJawNylon Boltand NutsSpringHeat-ShrinkTubingLead to J3Current-InjectionJawDielectricSeparatorLead to J2Figure 3.22 An alligator clip can be converted into a Kelvin probe by replacing the standard metallic axis by a nylon bolt with nylonspacers to isolate the jaws from each other. For the same reason, the ends of the inner spring must also be insulated.suitable insulator. Two separate leads are then used to connect to the jaws of the probe, oneto inject current and the other to sense voltage.Once the circuit and the probe are assembled, calibrate the adapter to produce exactly 1 A.Plug the power cord of the instrument under test to the hospital-grade ac plug J1, and clip theKelvin probe to an exposed conductive point of the case that is supposed to be protectivelygrounded. A digital voltmeter connected between J4 and J5 will directly read the protectiveground resistance on a scale of 1 V/. It must be remembered, however, that the measurementof resistance provided by this instrument only approximates the impedance test intendedby the standards. The discrepancy between the methods is especially evident for high-powercircuits, since a dc measurement of resistance does not convey any information regarding theinductive component of impedance. Moreover, dc ohmmeters are usually fooled by the polarizedinterface that results when an oxidation layer forms between connections in a defectiveground system. This last concern may be alleviated by running the test once again but withthe current injection polarity reversed. Nonlinear polarization indicating oxidation must besuspected if resistance measurements taken with opposite current injection polarities do notagree to a high degree. Failing this test is an immediate show-stopper. Before proceedingwith any further testing, you must locate the faulty connection responsible for compromisingthe integrity of the protective ground.Measuring Leakage and Patient Auxiliary CurrentsLeakage and auxiliary current tests are the most important tests to establish the electricalsafety of a medical electronic instrument. These are also the tests that are most commonlyfailed during safety approval submissions as well as during the periodic tests that hospitalsconduct to ensure the safety of medical electronic devices throughout their service life. Inthe case of medical electronic instruments, measurements of leakage and auxiliary currentsare taken using a load that simulates the impedance of a human patient. The AAMI load isa simple RC network that presents an almost purely resistive impedance of 1 k for frequenciesup to 1 kHz. As shown in Figure 3.23a, this load constitutes the core of the currentmeasuring device. If a 1-A current is forced through the AAMI load at differentfrequencies, the high-impedance RMS voltmeter within the measuring device would readthe values presented in the graph of Figure 3.23b.
130 <strong>DESIGN</strong> <strong>OF</strong> SAFE <strong>MEDICAL</strong> DEVICE PROTOTYPESMEASURING DEVICEAAMI LOADOUTPUTV+–I1AC=1 uAR11kR210kC1.015uHigh-Impendancerms Voltmeter0 0 0 0(a)Figure 3.23 Leakage and auxiliary currents are measured using a load that simulates the impedance of a human patient. (a) The AAMI loadis the core of the current-measuring device defined by safety standards harmonized with EN-601-1. (b) This load presents an impedance ofapproximately 1 k for frequencies up to 1 kHz.
TESTING FOR COMPLIANCE 131The frequency-response characteristics of the AAMI load have been selected to approximatethe inverse of the risk current curve as a function of frequency. In turn, this risk currentcurve was derived from strength/frequency data for perceptible and lethal currents.These data showed that between 1 and 100 kHz, the current necessary to pose the samerisk increases proportionately to 100 times the risk current between dc and 1 kHz. Sinceinsufficient data exist above 100 kHz, AAMI decided not to extrapolate beyond 100 kHz,but rather, to maintain the same risk current level corresponding to 100 kHz.Actual current measurements should be conducted after preconditioning the deviceunder test in a humidity cabinet. For this treatment, all access covers that can be removedwithout the use of a tool must be opened and detached. Humidity-sensitive componentswhich in themselves do not contribute significantly to the risk of electrocution may also beremoved. Next, the equipment is placed in the humidity cabinet containing air with a relativehumidity of 91 to 95% and a temperature t within the range 20 to 32°C for 48 hours(or 7 days if the instrument is supposed to be drip-proof or splash-proof). Prior to placingit in the humidity cabinet, however, the equipment must be warmed to a temperaturebetween t and t 4°C.The measurement should then be carried out 1 hour after the end of the humidity preconditioningtreatment. Throughout this waiting period and during testing, the same temperaturet must be maintained, but the relative humidity of the environment must onlybe 45 to 65%. Testing should be performed with the equipment’s on–off switch in bothconditions while connected to a power supply set at 110% of the maximum rated supplyvoltage. When operational, the maximum rated load must be used. As mentioned in thefirst part of this chapter, allowable patient leakage and auxiliary currents are defined forboth normal and single-fault conditions. Single-fault conditions are defined as conditionsin which a single means of protection against a safety hazard in the equipment is defectiveor a single external abnormal condition is present. Specific single-fault conditions thatmust be simulated during testing include interruption of the supply by opening the neutralconductor as well as the interruption of the protective ground conductor. Patient leakagecurrent between an F-type applied part and ground assumes that an external voltage equalto 110% of the maximum rated supply voltage is in direct connection with the applied part.For battery-powered equipment, the external voltage that is assumed to be connected to theF-type applied part is 250 V.Leakage current tests are conducted as shown in Figure 3.24a–d, with the device’spower switch in the on and off conditions and creating the single-fault conditions specifiedin the figure. If the enclosure or a part thereof is made of insulating material, a piece ofmetal foil 20 cm 10 cm applied to the nonconductive part of the enclosure must be usedas the protectively grounded enclosure connection. The metal foil is wrapped on the surfaceof the insulating enclosure, simulating the way in which a human hand could act as acapacitively coupled electrode.The connections for measuring patient auxiliary currents are shown in Figure 3.24e.Here, the current flowing between each patient connection and every other patient connectionis measured under normal and single-fault conditions. For this test, the measuringinstrument should be capable of differentiating the ac components from the dc componentsof the RMS current reading. As you can see from Table 3.2, different ac and dc auxiliarycurrent levels are permitted to flow through the patient, depending on the use intended forthe equipment.Versatile MicroammeterFigures 3.25 to 3.28 present the schematic diagrams of a versatile instrument for the measurementof leakage and auxiliary currents. The core of the circuit is an AAMI load thatconverts a leakage or auxiliary current into a voltage waveform with a factor of 1 V/mA
PatientConnectionsPatientConnectionsNormal/ReversePolarityOpen/NormalNeutralInstrument Under TestNHMains PartF-TypeAppliedPartMeasuringDeviceGNormal/ReversePolarityOpen/NormalNeutralInstrument Under TestNHMains PartF-TypeAppliedPartGProbeMeasuringDeviceFigure 3.24 Leakage current measurements are obtained with the device’s power switch in the on and off conditions as well as while inducingsingle-fault conditions in the circuit as shown. (a) Ground leakage current is measured between the protective ground conductor of thegrounded power cord and ground. (b) The enclosure leakage current measured is the total current flowing from the enclosure and all accessibleparts through an external conductive connection other than the protective ground conductor to ground. (c) Patient leakage current ismeasured between each and all patient connections and protective ground. (d) A second test for leakage current involves applying power linevoltage to the applied parts. (e) The patient auxiliary current is measured between every patient connection and all other patient connections.(a)NeutralHotGround(b)NeutralHotGround132
SelectorSelectorPatientConnectionsPatientConnectionsInstrument Under TestMains PartF-TypeAppliedPartInstrument Under TestMains PartF-TypeAppliedPartTestMeasuringDeviceFigure 3.24 (Continued)Open/NormalNeutralNHGOpen/NormalGroundMeasuringDeviceNHG125VAC @ 1mA maxNormal/ReversePolarityNormal/ReversePolarity(c)NeutralHotGround(d)NeutralHotGround133
MeasuringDeviceSelectorPatientConnectionsSelectorInstrument Under TestMains PartF-TypeAppliedPartFigure 3.24 (Continued)NHGOpen/NormalNeutralOpen/NormalGroundNormal/ReversePolarity(e)NeutralHotGround134
+V_LCD-V_LCDC110.01uFR1462kR1362kC6.47uFSW1R1262kC5.47uFC4.47uF+15Vrms CURRENT MEASUREMENT MODE SWITCHOPEN: DC OnlyCLOSED:DC+AC110VAC Hot110VAC NeutralT1110/6.3VAC100V 1Abridge- +C8100uF,25V+1C100.01uFIC3LM78L05A/TO39VIN VOUT3DNG2C9100uF, 25V+AAMI LOADR410k,2WD4FDH300AMP REFNON-INDUCTIVECOMPONENTS!R151k,25W,1%R620MR510k,2WR16100,1%C7-15V.015uF,500V,1% IC1+15V21 +IN -INOUT13 OSENSED212 X106FDH30016 X100 REF11 X200X500 OOADJ3 RGOOADJ45R3100C2.015uF-15VD1FDH300R2100kD3FDH300R1100kR11100k+15V-15V87IOADJIOADJ+VCC-VCCINA1109101415RMS-to-DCGainSettingIC21 5EIN R5 13R13 24812<strong>OF</strong>ST2<strong>OF</strong>ST4<strong>OF</strong>ST8<strong>OF</strong>ST124341EOUT6C310uF+R710kR81MR10100kDVMRANGESETTINGMod1 3-1/2Digit DVM+Vin-Vin+V_LCD+15VC1.01uF+15VR910k-15VRMS-to-DC RangeSetting-V_LCDFigure 3.25 An AAMI load converts currents into voltage signals that are amplified by an instrumentation amplifier. The RMS value of theamplified signal is converted by IC2 into a dc voltage that is measured by a 3 1 -digit DVM module.2135
136 <strong>DESIGN</strong> <strong>OF</strong> SAFE <strong>MEDICAL</strong> DEVICE PROTOTYPESfor frequencies under 1 kHz. The output of the AAMI load is amplified with a gain of 10by instrumentation amplifier IC1. The RMS value of the amplified signal is then computedby IC2, a true-RMS-to-dc converter IC, and displayed by a 3 1 -digit DVM module. Note2that some modules need to be supplied from a power supply that floats in relation to thereference potential of the voltage to be measured. If necessary, use the circuit shown inthe insert of Figure 3.25 to supply floating power to the DVM module.R1 must be set to produce a reading of zero with no current flowing through the AAMIload. Potentiometers R7 and R9 should be set to produce a reading of 1999 counts on theDVM for a 1.999-mA dc current through the AAMI load. In this same circuit, notice thatan RC low-pass filter network can be interposed between the AAMI load and the voltageamplifying circuit. This serves to allow the measurement of the dc component of a patientauxiliary current.The circuit presented in Figure 3.26 makes it possible easily to configure a measurementsetup to conduct the various leakage and auxiliary current tests required by the safety standards.In this circuit, switch SW3 selects the connection of the AAMI load to measure eithera patient current, the current on the protective ground pin, or the enclosure leakage current.Switch SW4 is used to select the source of a patient current among the different possiblecombinations of patient connections. Also through this circuit, power line–level voltagescan be applied to the patient connections by way of relay K1. The figure shows the connectiondistribution suitable for testing a 12-lead ECG; however, the connections of anyother applied part can be substituted. The connectors used for establishing connection to theleads of an applied part must be selected carefully so as not to contribute themselves to themeasured leakage or auxiliary currents. A good choice are Ohmic Instruments’ 301PB ECGbinding posts, which can accommodate either the standard snap-ons or the pin tips used forestablishing connection to ECG patient electrodes.The construction of the AAMI load, its power supply, and its switching networkdeserves special attention, since stray coupling within the circuit can render measurementsuseless. This is because wiring and/or PCB traces that are part of the AAMI loadand the voltmeter may be coupled capacitively to ground or the power line. Some forethoughtin the layout will avoid a lot of aggravation later when you try to calibratethe instrument. The circuit of Figure 3.27 controls the power supplied through J13 to thedevice under test. SPDT relays with contacts rated for 125 V ac at 20 A are used to reversethe power line polarity at J13 as well as to cause open-ground and open-neutral singlefaultconditions.Three neon lamps are used to indicate that the measurement instrument is powered aswell as to verify that the ac plug from which power is obtained is wired correctly. Normaland fault conditions are shown in Table 3.3. In addition, the figure shows the 115-V ac isolationtransformers and the voltage-divider network formed by R17–R19, which are usedto generate 125 V ac for measuring the patient leakage current with applied power linevoltage. Notice that R20 limits the current that can be delivered by this circuit to approximately1 mA.Finally, Figure 3.28 presents the dc power supply section of the measurement instrument.Linear regulators are used to generate the various power levels required by themicroammeter. In addition, R24–R26 are used to derive an ac signal to balance the measurementcircuit during application of 125 V ac to the patient connections. When measuringcurrents, place the equipment under test on a nonconductive bench, away from groundedmetal surfaces. In addition, make sure that all external parts of an applied part, includingpatient cords, are placed on a dielectric insulating stand (e.g., a polystyrene box) approximately1 m above a grounded metal surface.Finally, a word of caution: Be very careful when using this instrument! Remember thatunrestricted power line voltages are used to power the device under test, making the riskof electrocution or fire very real. Moreover, single-fault conditions forced during testing
ISOLATED 125 VACAC BALANCE125VAC TO APPLIED PARTSSWITCHOpen: UnpoweredClosed: 125VAC Applied+12VSW2K1RELAY DPDTC8.001uFSW4a6 7 8 9105 4 321116 7 8 91054 3216 7 8 91054 321SW4b11SW4c11UNIVERSAL ECGCONNECTORBINDING POSTSJ21"Right Arm"J31"Left Arm"AMP REFAAMI LOADDUT GND SENSE444SW3aSW3bSW3c123123123GND CURRENTMODE SWITCHPATIENT CURRENTENCLOSURECURRENTPostition 1: Patient Leakage CurrentPostition 2: Ground Leakage CurrentPostition 3: Enclosure Leakage CurrentPATIENT LEAKAGE-CURRENT REFERENCE1J1CASESENSEBANANAJACK1BANANAPLUGALLIGATOR CLIP TOENCLOSURE <strong>OF</strong>DEVICE-UNDER-TESTPATIENT CONNECTIONSELECTOR SWITCHLeakage Current Between:Position 1: All Leads to GNDPosition 2: Right Leg to GNDPosition 3: Right Arm to GNDPosition 4: Left Arm to GNDPosition 5: Left Leg to GNDPosition 6: V-Leads to GNDPosition 7: Right Arm to Left ArmPosition 8: Right Arm to Right LegPosition 9: Left Arm to Right LegPosition 10: Isolation Test6 7 8 9105 4 35432216 7 8 91016 7 8 91054 3 21SW4d11SW4e11SW4f11J41"Right Leg"J51"Left Leg"J61J71J81J91J101J111"V1""V2""V3""V4""V5""V6"Figure 3.26 The various current measurements required by the standards are conveniently selected through switches SW3 and SW4.Patient connections are shown for a 12-lead ECG; however, the connections of any other applied part can be substituted. In addition, powerline voltage can be applied to the patient connections to conduct the live patient leakage current test.137
15VAC115VAC2ISO 125VACDUT GND SENSEHOTF1SW5T1115VAC/15-0/15VAC @ 1A16AHospital-GradePower Cord20A RATINGPOWERSWITCHR21330kR22330kR23330kNOT TOEARTH-GROUND !R17T2 R2010k100kNEUTRALLP1LAMP NEONHOT-NEULP2LAMP NEONHOT-GNDLP2LAMP NEONNEU-GNDT3115VAC/115VAC@ 0.13AISOLATIONTRANSFORMERR1862kR1950k+12VOPEN NEUTRAL SWITCHOpen: NormalClosed: Open NeutralSW6K2115VAC/115VAC @0.13A ISOLATIONTRANSFORMERK3SW7RELAY SPDTPOLARITY SWITCHOpen: NormalClosed: ReversedRELAY SPDTSW8K4J13HOSPITAL-GRADEFEMALE AC PLUGOPEN GND SWITCHOpen: NormalClosed: Open GNDRELAY SPDTK5RELAY SPDTFigure 3.27 Power-control relays are used to reverse power line polarity and cause single-fault conditions for analyzing the instrumentunder test. Two 115-V ac isolation transformers and the voltage-divider network formed by R17–R19 are used to generate the 125 V ac formeasuring the patient leakage current with applied power line voltage.J12138
TABLE 3.3 Normal and Fault Conditions Detected by Three Neon Lamps Used in the Circuit ofFigure 3.27 to Verify That the AC Plug from Which Power Is Obtained Is Wired CorrectlyIndicator LightLP1 (Hot–Neutral) LP2 (Hot–Ground) LP3 (Neutral–Ground)ConditionTESTING FOR COMPLIANCE 139Off Off Off Instrument off or open hotOff On Off Open neutralOff On On Hot–ground reversedOn Off Off Open groundOn Off On Hot–neutral reversedOn On Off Correct, or ground–neutral reversedmay result in enclosure of the device under test becoming live, threatening anyone whowould come in touch with it accidentally. In addition, since power line–level voltages canbe injected into patient connections and the associated power system, never conduct thesetests in the vicinity of a patient or on a power system branch that is used to power medicalelectronic instruments connected to patients.HiPot TestingOnce compliance with current leakage limits is established, high-potential application testing,commonly known as hiPot testing, is used to assess the suitability of the insulation barriersbetween isolated parts of a medical instrument. In essence, very high voltage is applieddifferentially between the parts separated by the isolation barrier under test. As shown inTable 3.4, the test voltage is dependent on the voltage U to which the barrier is subjectedunder normal operating conditions at the rated supply voltage. While high voltage is applied,current is monitored to ensure that no arc breakdown occurs. HiPot testers have internal circuitrythat automatically disconnects the high-voltage supply across the insulation under testwhenever current exceeds a preset threshold value.Although slight corona discharges are allowed by the standards, excessive RMS leakagecurrent measurement is not sufficient for reliable detection of dielectric breakdown.Rather, milliampere-level current spikes or pulses should be monitored, since these areindications of the type of arc breakdown that occurs on insulation prior to catastrophic anddestructive breakdown. Here again, the test voltage is supposed to be within the ratedoperating frequency for the instrument under test, and measured magnitudes refer to theirac RMS values. Despite this, the technique is sometimes modified by applying the dcequivalent to the peak-to-peak amplitude of the ac RMS voltage required. This obviouslyreduces current leakage between parts, since capacitive and inductive coupling disappear,leaving a current signal that directly conveys information about insulation breakdownprocesses at the peak of the dielectric stress.As an example of applying this technique, if the highest-rated supply voltage foran instrument is 125 V ac, the standard requires that testing of basic insulation be conductedat 1000 V RMS . The peak-to-peak voltage of the ac test signal required would thusbe 1000 V RMS 1.41 1410 V P-P . As such, 1410 V dc would be applied, for example,between a wire connecting the hot and neutral of the power cord and another wire attachedto the protective ground connection of the instrument. Similarly, the insulation barrierbetween an F-type applied part and any other point of the instrument of the example isrequired to be tested at 3000 V RMS , which corresponds to a 4230 V dc voltage for themodified test. Breakdown of the insulation would then be indicated by current spikes thatwould appear while the high voltage is applied between a point that ties together all patient
+12V+15V+7V-15V-7V+ C176.8uF+ C166.8uFIC3LM7812C/TO2201 3IN OUT221D81N4001D71N4001C210.1uF2C220.1uF+ C23100uF211+ C92200uFD61N4001C200.1uF+ C192200uFR28860R2510k, 10-TurnR261.2kISOLATIONBALANCETRIMMERD5BR62- ++C122200uFC110.1uF2 3IN OUT1C130.1uF+C142200uFD97VR27860D107VC180.1uFGNDGNDC100.1uFIC4LM7815C/TO2201 3IN OUTDNG2R241.2kIC5LM7915C/TO220C150.1uFFigure 3.28 Linear regulators generate the various voltages required by the ammeter’s circuitry. In addition, R24–R26 are used to derivean ac signal to balance the measurement circuit during application of 125 V ac to the patient connections.15VAC 1AC BALANCE15VAC 2140
TESTING FOR COMPLIANCE 141TABLE 3.4Some Voltages Used for HiPot Testing of Insulation BarriersHiPot Test Voltages for Reference Voltage U (V)Insulation Type U 50 50 U 150 150 U 250 250 U 1000 1000 U 10,000Basic 500 1000 1500 2U 1000 U 2000Supplementary 500 2000 2500 2U 2000 U 3000Reinforced 500 3000 4000 2(2U 1500) 2(U 2500)connections and a point that ties all nonisolated I/O lines and the hot, neutral, and groundconnections of the power cord.It must be noted, however, that despite its convenience, this method is not alwaysaccepted by regulatory bodies as a reasonable substitute for the tests specified by the standards.In any case, make sure that the hiPot tester that you use can detect the precatastrophicbreakdowns, since otherwise, the insulation in your instrument may break down,delivering an instantaneous lethal level of current.HiPot testing should be conducted after the equipment is preconditioned in a humiditycabinet. As before, all access covers that can be removed without the use of a tool must bedetached. Humidity-sensitive components which in themselves do not contribute significantlyto the risk of electrocution may also be removed. In addition, however, voltage-limitingdevices (e.g., spark-gap transient-voltage suppressors, Iso-Switches) in parallel with insulationto be tested can be removed if the test voltage would make them become operative duringthe hiPot.HiPot tests of the various insulation methods must be conducted with the instrument ina humidity cabinet. For each test the voltage should be increased slowly from zero to thetarget potential over a 10-second period and then kept at the required test level for 1 minute.If breakdown does not occur, tripping the hiPot tester’s automatic shutoff, the test is completedby lowering the voltage back to zero over a 10-second period.Finally, it must be noted that the standards do not except battery-powered equipmentfrom hiPot testing. Instead, the reference voltage U is set to be 250 V. Fully or partially nonconductiveenclosures are not excluded either. In these cases, the same metal-foil methodused for current leakage testing must be used, being careful that flashover does not occur atthe edges of the foil at very high hiPot test levels.Most of the circuitry inside commercial hipot testers is really used to control high-voltagesource and detecting currents that exceed a set threshold. If the $1000 or so needed tobuy a low-end hipot tester are outside your budget, you may conduct design-time testsusing the circuit shown in Figure 3.29. Here, variac T1 is used to change the supply voltageto the primary of a high-voltage transformer T2. We used a surplus transformer with aground-referenced secondary rated for a maximum output of 5 kV at 5 mA. Not any highvoltagetransformer should be used for this application. A unit with good voltage regulationis needed. Avoid using neon-light transformers because these are built to provide aconstant current to the load. Under unloaded conditions, they will present a voltage of 9 to15 kV at the load.The high voltage applied to the device under test starts as 117 V ac. This voltage is controlledusing a Crydom solid-state relay. If the AC_ENABLE signal is a logic high, 12 Vdc is applied to the control inputs of the Crydom solid-state relay, and if SW2, the ARMkey switch, is in the on position, 117 V ac will be applied to the inputs of variac T2. T1, aMagnatek-Triad step-up transformer, is fed directly by the variac’s output. The high voltageproduced by T2 is then applied to the device under test through a touch-proof bananaconnector as shown in Figure 3.30.The current-trip circuit of Figure 3.31 acts as a milliammeter-controlled relay that disconnectsthe supply to the variac if the isolation barrier under test should fail. Ac current
117VACHOTNEUTRAL12MAIN ACPOWERSW2SW-SPSTJ2PLUG AC MALE3EARTHHOTD11N4004+12VSolid StateRelayK1CRYDOMD1210ARM KEYSWITCHSW2SW-KEY-SPSTT2VARIACT1MAGNATEK-TRIAD N685-7070J1TOUCH-PRO<strong>OF</strong> BANANAV1HV OUTHIGH-VOLTAGEHIGH-IMPEDANCE ACVOLTMETERNEUTRALAC_ENABLER110kD21N4148R18Q12N2222A470kHOTNEUTRAL117VACF-118X 24VAC CT, 0.7A TransformerD34, 1N4004 Diodes- +1000uF, 35VDCC41000uF, 35VDCC1++C20.33uFC50.33uFIC1NJM78M12 /TO1 3IN OUT2IN21IC2NJM79M12/TO3+12VC3100nFC6100nFGND GNDT3OUT-12VFigure 3.29 A simple hiPot tester for design time can be constructed using a variac to change the supply voltage to the primary of a highvoltagetransformer. The variac’s supply is controlled through a Crydom solid-state relay.142
TESTING FOR COMPLIANCE 143HI-POTHV OUTTouch-Proof BananaConnector, M aleTouch-ProofBananaConnector,FemaleDEVICEUNDERTESTHV RETURNFigure 3.30 The high voltage produced by T2 of Figure 3.29 is applied to the device under test through a touch-proof banana connector.The current that leaks through the DUT’s barriers is returned to the hiPot’s sense resistor via a second touch-proof connector.flowing through the device under test flows from the HV OUT terminal, J1, and throughJ3, the HV RETURN, and then through R9, the current-sensing resistor to ground. Thedirection of the current flow is reversed on the opposite phase of the ac waveform appliedto the device under test. The voltage that appears across R9 is proportional to the currentflow through the device under test. A current of 1 mA flowing through the device undertest appears as 7 V RMS across R9. This voltage is buffered by IC1A and full-waverectified by IC1B and IC1C. The peak of the current-sense voltage across R9 is comparedto the dc voltage level from R13 by IC1D. If the peak current-sense voltage is greater thanthe voltage from R13, the output from IC1D will be 12 V dc, a logic level high. Thislogic high causes IC2B to be reset, setting the AC_ENABLE output low, switching off K1and the high voltage to the device under test. IC3A provides a power-on reset circuit, sothe control flip-flop, IC2B, always powers on in a reset or off condition. Switch SW3 providesa way to stop the test by resetting the control flip-flop manually to the off state.To start a test, first the reset input to the control flip-flop is a logic low, meaning that thecomparator output is a logic low, and SW3 is open. SW4 is pressed and a logic level highis input to the clock input of the control flip-flop. The Q output will switch to a logic highstate. This high output on AC_ENABLE will switch K1 on, applying high voltage to thedevice under test. As the control knob on the variac is increased, the high voltage to thedevice under test is increased. If the current flowing through R9 (i.e., the current leakingthrough the device under test) increases above the level set by R13, the output of IC1Dswitches to a high state, resetting the control flip-flop and switching K1 off, disconnectingthe high voltage from the device under test. Because the reset input to the flip-flip has priorityover the clock input to the flip-flop, the Q output cannot be turned on anytime the current-sensevoltage is greater than the trip level set by R13. This is done for safety purposes,so that if there is an overcurrent condition, the high voltage must first be reduced to thepoint where the overcurrent condition is removed before the test can be restarted by pressingSW4. IC3B and IC3D are connected in parallel to provide enough current to drive thehigh-voltage-indicator LED, D9.Utmost care should be exercised when using a hiPot tester. High voltage below the current-tripthreshold can give a nasty or lethal shock. In addition, dielectric breakdown carriesthe associated risk of ignition. Be prepared to deal with emergencies. In addition, consider
TRIPD61N4148BufferR220k 1.0%Precision Full-Wave RectifierComparatorHV RETURNJ3TOUCH-PRO<strong>OF</strong> BANANA11mA = 7V RMSR94.99k10KVC710nFC810nF32+12V411+--12VIC1ATL084A1R720k 1.0%R1115k65R320k 1.0%-12V114-++12VIC1BTL084A71N4148D41N4148D5R410k 1.0%R126.19kR520k 1.0%910-12V114-++12VIC1CTL084A8R13R810k+12V1213+12V411+--12VR610MIC1DTL084A14R1010k+12VC10+12VPower-On ResetOver-CurrentTrip SettingAdjust100k,10T 1 32C910nFR14100k+ C11D71N414810uF, tant.100nF141 27IC3ACD40106BD81N4148AC_ENABLE+12VR154.99k+12VSW3PB SWITCHSW4PB SWITCHD111N4148R1749.9k10111498IC2BCD4013BDSRCLKVDD7QQ1312143 47IC3BCD40106BD9LEDGND+12VSTOP TESTTRIPSTART TESTD101N4148R1649.9k+12VC12100nF14+12V+12V9 87IC3DCD40106BHighVoltageFigure 3.31 The current-trip circuit acts as a milliammeter-controlled switch that disconnects the supply to the variac if the isolation barrierunder test should fail.144
TESTING FOR COMPLIANCE 145that dielectric breakdown or single-fault conditions may result in any part of the device undertest becoming electrified at very high voltage, threatening anyone who came close to it.Testing for Other RisksYou will probably be able to get by just by being able to pass the tests outlined above aslong as evaluation of the prototype is conducted on a very limited number of patients whileunder the supervision of a physician. As long as the instrument is built solidly enough toinspire confidence, we have seldom encountered situations where an engineering evaluationprototype would be required to pass the battery of tests specified by the standards toensure compliance with the mechanical and labeling requirements demanded for prereleaseor commercial products. However, there are other very realistic risks in a clinicalenvironment, and you should make sure that you will not cause undue interference or harmthrough mechanisms other than leakage currents.For an evaluation prototype, you should at least test for and verify that the followingconditions are met:• The equipment has been designed to minimize the risk of fire and explosion. Safetystandards typically limit temperature rises allowed for components as well as definingenclosure requirements for containing fires within the instrument. Whenever possible,select materials to be compliant with UL-94V (Flammability of Plastic Materials forParts in Devices and Appliances). In addition, if the device is supposed to operate inareas where flammable anesthetics or oxygen-enriched atmospheres are used (e.g.,operating rooms, hospital rooms), special requirements must be met to ensure thatthese explosive atmospheres are not ignited.• If intentional sources of ionizing radiation are present, the equipment must be evaluatedby the Center for Devices and Radiological Health (CDRH). If components areused that may generate ionizing radiation which is not used for a diagnostic or therapeuticpurpose (e.g., from CRTs), you must ensure that the exposure at a distance of5 cm from any accessible part of the equipment, averaged over a 10-cm 2 area, is lessthan 0.5 milliroentgen per hour. Devices that make use of ultraviolet radiation andlasers should also be investigated to ensure safety. In addition, devices that makeuse of ultrasound and RF emissions are also regulated in specific substandards of theIEC-601-2 series.• The equipment must not emit electromagnetic interference (EMI), which may causeother equipment to malfunction. The device should also be designed to be immune toelectromagnetic interference, power line “glitches,” and electrostatic discharge. Wedeal with these issues in Chapter 4.• Applied parts designed to come in contact with the biological tissues, cells, or bodyfluids of a patient must be assessed as to their biocompatibility. Diligent prudenceshould be applied in the selection of materials, making sure to test for biologicaleffects, including cytotoxicity, sensitization, irritation, intracutaneous reactivity, andso on.• The medical device and all peripheral equipment should be fitted with the means necessaryto disconnect them from a patient immediately and completely should an emergencyarise. In addition, connectors used on patient connections are identified clearly anduniquely and must be of a type that cannot be plugged into the power line accidentallyor form an electrical path to any point when they are not connected to the equipment.In addition to establishing reasonable safety, take the time to educate clinical staff memberswho support your evaluations as to the potential dangers posed by an instrument,
146 <strong>DESIGN</strong> <strong>OF</strong> SAFE <strong>MEDICAL</strong> DEVICE PROTOTYPESregardless of how remote and unlikely they may be. Remember that if something goeswrong, it is the clinical staff who will have to save the patient’s life!CONCLUDING REMARKSApplying the principles and requirements described by the safety standards is importantfor even the first engineering evaluation prototype of a medical electronic device. This isbecause the biomedical equipment department of any hospital hosting the preclinical trialswill demand that the device passes, at a bare minimum, all electrical safety tests. Furthermore,since we live in a litigious society, it is a good idea to maintain good records showingthat careful consideration was given to the standards and regulations all the way fromthe beginning of the design.As you can appreciate from even the brief overview of limited scope presented in thischapter, the safety and performance requirements for medical devices are many and verystringent. However, we believe that these requirements are not enforced by regulatoryagencies with the intent of discouraging the advancement of the medical sciences. Rather,it is our perception that applicable standards and regulations are there to help the designerdevelop a product that provides true benefit to the patient at the same time that it reducesforeseeable risks. We encourage you to pursue data that clearly demonstrate clinical efficacyfor an idea that you may have for a medical product. In addition, we urge you to realizethat to be approved, new medical technology must absolutely be based on solidphysiological and technical grounds. Armed with this information, and if you can adapt toa changing regulatory environment, we are convinced that a very receptive audience ofinvestors eagerly awaits to back your idea.REFERENCESAckerman, B., High-Resolution Timing on a PC, Circuit Cellar INK, 24, 46–49, December 1991–January 1992.Association for the Advancement of Medical Instrumentation, Safe Current Limits forElectromedical Apparatus, ANSI/AAMI Standard ES1, 1993.IEC-601-1, Medical Electrical Equipment—Part 1: General Requirements for Safety, 1988;Amendments 1, 1991, and 2, 1995.IEC-601-1-1, Medical Electrical Equipment—Part 1: General Requirements for Safety; Section 1:Collateral Standard: Safety Requirements for Medical Electrical Systems, 1992.IEC-601-2-27, Medical Electrical Equipment—Part 2: Particular Requirements for the Safety ofElectrocardiographic Monitoring Equipment, 1994.Porr, B., EEG Preamp: Anti Alias Filter and Isolation Circuit, www.cn.stir.ac.uk/~bp1/eegviewer/preamp/, 2000.Prutchi, D., LPT:Analog!—a 12-Bit A/D Converter Printer Port Adapter, Circuit Cellar INK, 67,26–33, February 1996.Schulze, D. P., A PC Stopwatch, Circuit Cellar INK, 19, 22–23, February–March 1991.UL-94V, Flammability of Plastic Materials for Parts in Devices and Appliances, UL-2601-1,Standard for Safety: Medical Electrical Equipment—Part 1: General Requirements for Safety,2nd ed., 1997.
4ELECTROMAGNETIC COMPATIBILITY<strong>AND</strong> <strong>MEDICAL</strong> DEVICESHave you heard about the wheelchair that moved on its own every time a police car passedby? No, it’s not part of a joke. This actually happened, and several people were seriouslyinjured when radio signals from the two-way communications equipment on emergencyvehicles and boats, CB, and amateur radios interfered with proper operation of the controlcircuitry of powered wheelchairs, sending some off curbs and piers. Similar reports ofimproper operation of apnea monitors, anesthetic gas monitors, and ECG and EEG monitorsdue to electromagnetic interference prompted government agencies to look carefullyat these occurrences and establish regulations by which equipment must possess sufficientimmunity to operate as intended in the presence of interference.Complying with these regulations is not easy. The technologies involved in modern circuitdesign have considerably blurred the boundaries between the digital and analogworlds. Suddenly, multihundred megahertz and even gigahertz clocks became commonplacein high-performance digital circuits, making it necessary to consider every connectionbetween components as an RF transmission line. At the same time that the need forhigher performance pushes designers toward high-speed technology, the marketplace isdemanding more compact, lighter, and less power-hungry devices. With smaller size, analogeffects again enter into consideration, because as components and conductors comeinto close proximity, coupling between circuit sections becomes a real problem.Obviously, self-interference within a circuit must be eliminated to make the productworkable, but this still does not make the product marketworthy. This is because strict regulationsconcerning electromagnetic compatibility are now being enforced around theworld in an effort to ensure that devices do not interfere with each other. In the UnitedStates the FCC regulates the testing and certification of all electronic devices that generateor use clock rates above 9 kHz [Dash and Strauss, 1995]. In principle, the FCC’s charter isto protect communications from unwanted electromagnetic interference (EMI). In theEuropean Common Market, on the other hand, an electromagnetic compatibility (EMC)directive is now in effect, which not only establishes requirements against causing undueinterference to radio and telecommunications equipment, but also institutes requirementsDesign and Development of Medical Electronic Instrumentation By David Prutchi and Michael NorrisISBN 0-471-67623-3 Copyright © 2005 John Wiley & Sons, Inc.147
148 ELECTROMAGNETIC COMPATIBILITY <strong>AND</strong> <strong>MEDICAL</strong> DEVICESby which equipment must possess sufficient immunity to operate as intended in the presenceof interference [Gubisch, 1995].Regulatory bodies around the world have developed standards and regulations coveringboth emissions and immunity that designers must take very seriously. Failure to complywith EMI and EMC regulations can have a serious impact on everyone associated with aproduct, starting with the designer, through the manufacturer, the marketing and distributionnetwork, and extending even to customers. The consequences of noncomplianceinclude halting manufacturing and distribution, levying fines, and the publication of publicnotices of noncompliance to warn potential customers and other agencies. These considerationsbecome especially important in the case of medical equipment, since it ofteninvolves sensitive electronics that can be affected adversely by electromagnetic interference,leading to potentially serious hazards to patients and health-care providers.The European Community regulates emissions and immunity of medical devicesthrough the EN-60601-1-2 standard (Medical Electrical Equipment—Part 1: GeneralRequirements for Safety; Section 2: Collateral Standard: Electromagnetic Compatibility—Requirements and Tests) as well as the EN-55011 standard (Limits and Methods of Measurementof Radio Disturbance Characteristics of Industrial, Scientific and Medical RadioFrequency Equipment). In EN-60601-1-2, pass/fail criteria are defined by the manufacturer.As a result, the manufacturer may chose to classify a failure mode that does not posea hazard to the patient as a “pass.” In the United States, the FDA is adopting many of theIEC-60601-1-2 requirements but is imposing restrictions on a manufacturer’s ability toadopt pass/fail criteria. The FDA prescribes that a passing result corresponds to maintainingclinical utility. In addition, there are discrepancies between the immunity levels recommendedby European authorities and the FDA. Because of these differences in opinion,as well as because the standards are relatively new, changes occur often, and we adviseengineers to keep updated on the latest versions.Assuring compliance with the rules involves an extensive series of tests. The EMI andEMC standards enforced by the various regulatory agencies clearly define the constructionof test sites as well as the test procedures to be followed. Even a fairly spartan facilitycapable of conducting these tests ends up costing over $100,000 just to set up, and for thisreason, most companies hire an outside test lab at the rate of $1500 to $3000 per day toconduct testing. Considering how fast charges can accumulate during testing, it is obviouslynot a smart move simply to hire a test lab and wait for the results. Rather, designersshould familiarize themselves with the relevant EMI and EMC standards and make surethat compliance requirements are considered at every stage in the design process.In this chapter we present the major EMI/EMC requirements for medical devices, lookat the theory of how circuits produce EMI, and describe some low-cost tools and methodsthat will allow you to identify and isolate the sources of EMI that inevitably make it intoa circuit.EMISSIONS FROM <strong>MEDICAL</strong> DEVICESThe FCC’s main concern with RF emissions from electronic devices is possible interferencewith communications devices such as commercial radio and TV receivers. From thepoint of view of agencies regulating medical devices (in the United States the FDA), theconcern about unintentional electromagnetic emissions extends to the way in which theycould interfere with diagnostic or therapeutic medical devices. Note the word unintentional,since these standards do not apply directly to medical devices that intentionallygenerate electromagnetic signals (e.g., telemetry ECG transmitters, electrosurgery equipment,magnetic resonance imagers) which require special emissions that limit exemptionsat specifically allocated frequency bands.
RADIATED EMISSIONS FROM DIGITAL CIRCUITS 149EN-60601-1-2 sets forth requirements for emissions based on the CISPR-11 standarddeveloped by the International Electrotechnical Commission’s Special Committee on RadioInterference (CISPR). These requirements address both radiated emissions (i.e., electromagneticinterference coupled to victim receivers over wireless paths), as well as conductedemissions (i.e., electromagnetic interference coupled to power lines and other conductors)from medical equipment.Emission limits are set based on the type of setting the device will be used. Class Arequirements are the least stringent and apply to medical devices intended to operate inareas where receivers are not usually present. Class B requirements apply to equipmentthat may operate in close proximity to radio and TV receivers, such as in a patient’s homeor hospital room.Conducted emissions are tested below 30 MHz, while radiated emissions are tested above30 MHz. Although both emission mechanisms overlap, regulatory agencies set this boundarybecause low-frequency interference is primarily conducted (since low frequencies donot radiate very efficiently without intentionally designed antenna elements) and highfrequencyinterference is primarily radiated (since high frequencies are conducted poorlythrough inductive wires).RADIATED EMISSIONS FROM DIGITAL CIRCUITSAs they operate, digital circuits constantly switch the state of lines between a high-voltagelevel and a low-voltage level to represent binary states. As shown in Figure 4.1a, the resultingtime-domain waveform on any single line of a digital circuit can thus be idealized asa train of trapezoidal pulses of amplitude (either current I or voltage V) A, rise time t r , falltime t f (between 10 and 90% of the amplitude), pulse width τ (at 50% of the amplitude),and period T.The Fourier envelope of all frequency-domain components generated by such a periodicpulse train can be approximated by the nomogram of Figure 4.1b. The frequency spectrumis composed mainly of a series of discrete sine-wave harmonics starting at the fundamentalfrequency f 0 1/T and continuing for all integer multiples of f 0 . The nomogramidentifies two frequencies of interest. The first is f 1 , above which the locus of the maximumamplitudes rolls off with a 1/f slope. The second, f 2 , is the limit above which the locus rollsoff at a more abrupt rate of 1/f 2 . These frequencies are located atand1f 1 0. 32 π t τ1f 2 0. 32 π t twhere t is the faster of (t r , t f ).The envelope of harmonic amplitude (in either amperes or volts) is then simplified to2A(τ t) f f 1[V or I] 0. 64A 20 dB/decade roll-off fTf1 f f 2 0 . 2ATtf240 dB/decade roll-off f 2 f
150 ELECTROMAGNETIC COMPATIBILITY <strong>AND</strong> <strong>MEDICAL</strong> DEVICES(a)trtF90% AA50% Aτ10% AT(b)20 dB/decadeHarmonic Amplitude[Volts or Amps]40 dB/decadeFF1 F2Figure 4.1 A pulse train with the characteristics shown in (a) produces a spectrum with an envelopethat can be approximated by the nomogram of (b).For nonperiodic trains, the nomogram must be modified to account for the broadbandnature of the source. To do so, a nomogram of the spectral density envelope of the signalcan be defined for a unity bandwidth of 1 MHz bydBVdBA(V or I) or M HzM Hz6 20 log(Aτ) f f 120 log(A) 4 20 log[ f(MHz)] f 1 f f 2A20 log 14 40 log[ f(MHz)]τ( s)f 2 fDepending on its internal impedance, a circuit carrying such a pulse train will create in itsvicinity a field that is principally electric or magnetic. At a greater distance from thesource, the field becomes electromagnetic, regardless of the source impedance. If there isa coupling mechanism, which can be either conduction or radiation, some or all of thefrequency components in the digital pulse train’s spectrum will be absorbed by some“victim” receiver circuit.
RADIATED EMISSIONS FROM DIGITAL CIRCUITS 151To illustrate the magnitude of the problem, imagine a medical instrument’s main circuitboard, consisting of a CPU, some glue logic, and memory ICs, that has been housed in anunshielded plastic case. Let’s assume that at any given time, a number of these ICs are togglingstates synchronously, at a frequency of 100 MHz, for instance. Furthermore, assumethat the total power switched at any given instant during a synchronous transition isapproximately 10 W. Now, in a real circuit, efficiency is not 100%, and a small fraction ofthese 10 W will not do either useful work or be dissipated as heat by the ICs and wiring,but rather, will be radiated into space. Assuming a reasonable fraction value of 10 6 of thetotal switched power at the fundamental frequency, the power radiated is 10 µW.Now, let’s assume that an FM radio is placed at a distance of 5 m from the device. Thefield strength E produced by the 10 µW at this distance may be approximated by theformula30 radiated power (W)distance (m)E 3 0 1 0 5 1 0 6 3.46 m V 70.79 dB V mmConsidering that the minimum field strength required for good reception quality by a typicalFM receiver is approximately 50 dBµV/m, the radiated computer clock would causeconsiderable interference to the reception of a radio station in the same frequency. In fact,interference caused by the computer of this example may extend up to 50 m or more away!From the past discussion, it is easy to conclude that a first method for reducing radiatedemissions is to maintain clock speeds low as well as to make rise and fall times as slow aspossible for the specific application. At the same time, it is desirable to maintain the totalpower per transition to the bare minimum. Transition times and powers depend primarilyon the technology used. As shown in Table 4.1, the ac parameters of each technologystrongly influence the equivalent radiation bandwidth. In addition, the voltage swing, incombination with the source impedance and load characteristics of each technology, determinesthe amount of power used and thus the power of radiated emissions on each transition.Figure 4.2 shows how the selection of technology plays a crucial role in establishingthe bandwidth and power levels of radiated emissions that will require control throughoutthe design effort.Another problematic circuit often found in medical devices is the switching power supply.Here, high-power switching at frequencies of 100 kHz and above produce significantharmonics up to and above 30 MHz, requiring careful circuit layout and filtering. FullyTABLE 4.1 The Most Popular Logic Families Have Very Different Timing and Driving Parameters, Resulting in RadiatedEmissions Spectra with Different CharacteristicsMinimum Minimum Typical Bit Equivalent Single-Load Output SourceVoltage Transition Pulse Bandwidth Input ImpedanceTechnology Swing (V) Time t (ns) Width τ (ns) (MHz) Capacitance (pF) (Low/High) (Ω)5-V CMOS 5 70 500 4.5 5 300/30012-V CMOS 12 25 250 12 5 300/300HCMOS 5 3.5 50 92 4 160/160TTL 3 8 50 4 5 30/150TTL-S 3 2.5 30 125 4 15/50TTL-LS 3 5 50 65 5.5 30/160TTL-FAST 3 2.5 25 125 4.5 15/40ECL 0.8 2 20 160 3 7/7GaAs 1 0.1 2 3200 1 N/A
152 ELECTROMAGNETIC COMPATIBILITY <strong>AND</strong> <strong>MEDICAL</strong> DEVICESFigure 4.2 The characteristic voltage spectrum envelope of emissions by every logic gate is highlydependent on the technology being used.integrated filters are available for dc power lines. For example, Figure 4.3 shows the wayin which muRata BNX002 block filters are used to filter the raw dc power outputs producedby two C&D Technologies’ HB04U15D12 isolating dc/dc converters. In the circuit,each dc/dc (IC1 and IC2) produces unregulated 24 V (12 V if the center-tap common isused), which is isolated from the 15 V dc power input by an isolation barrier rated at3000 V dc (continuous, tested at 8 kV, 60 Hz for 10 s). The outputs of the dc/dc convertersare filtered via filters FILT1 and FILT2, which internally incorporate multiple EMI filtersimplemented with feed-through capacitors, monolithic chip capacitors, and ferrite-beadinductors. Each of these filters attenuates RF by at least 40 dB in the range 1 MHz to1 GHz. C1/C4 and C7/C10 are used to reduce ripple, and the circuits following thesecapacitors are linear regulators that yield regulated 24 V at 50 mA to the applied part forwhich this isolation power supply was designed.Another filter worth mentioning is muRata’s PLTxR53C common-mode choke coil.This family of modules is ideal for suppressing noise from a few megahertz (1 to 5 MHz,depending on the model) to several hundred megahertz (10 MHz to 1 GHz, depending onthe model) from dc power supplies. This module is useful in suppressing noise radiatedfrom the cable connecting a device to an external wall-mounted or “brick” ac adapter.ELECTROMAGNETIC FIELDSEMI standards establish that radiated-emissions test measurements should be performed ata distance of 10 to 30 m, depending on the device’s classification. For compliance testing,the device under test should be placed on a nonconductive table 0.8 m above a ground
+24VISOC6100nFIsoC12100nFIso15IC1+Vin-Vin+12COMM-12234HBO4U15D12C2100nFC31n F12FILT1BPSGBNX002CBCGC1100 uF/50V43+C4100nFR1220Q1BD139IC3R212KTL431R427KR3220KC5100uF/50V+15IC2+Vin-Vin+12COMM-12234HBO4U15D12C8100nFC91nF12FILT2BPSGBNX002CBCG43C7100uF/50V+C10100nFR5220Q2BD139IsoIC6R612KR7220KC11+TL431100uF/50VR827K-24VIS<strong>OF</strong>igure 4.3 BNX002 block filters by muRata are used to filter the raw dc power outputs produced by two isolating dc/dc converters. Thesefilters internally incorporate multiple EMI filters implemented with feed-through capacitors, monolithic chip capacitors, and ferrite-beadinductors.+15VINGNDIN153
154 ELECTROMAGNETIC COMPATIBILITY <strong>AND</strong> <strong>MEDICAL</strong> DEVICESTABLE 4.2EN-55011 Radiated Emissions Limits for Group 1 Devices aField Strength (dBµV/m)Frequency (MHz) Test Distance (m) Class A Class B30–230 10 40 30230–1000 10 47 37aThe lower limits apply at the transition frequency.plane. The table is typically centered on a motorized turntable that allows 360° rotation. Ameasurement antenna is positioned at a distance of 10 to 30 m as measured from the closestpoint of the device under test. The radiated emissions are maximized by configuringand rotating the device under test as well as by raising and lowering the antenna from 1 to4 m. A spectrum analyzer with peak detection capabilities is used to find the maxima of theradiated emissions during the testing. Then, final measurements are taken using a spectrumanalyzer with quasi-peak function with a measurement bandwidth of 120 kHz. The testsetup is shown in Figure 4.4. The limits for radiated emissions per EN-55011 for group 1devices are presented in Table 4.2.In reality, devices to be tested are not usually taken directly to the open-field test site.Rather, they are first scanned for potentially offensive radiated emissions in a small shieldedroom. The compliance testing is then conducted in the 10-m open-field test site, payingspecial attention to peak emissions detected in the shielded room. This is almost a practicalnecessity, because open-field test sites, even when located far from large metropolitanareas, are still inundated by human-made RF signals. As an example, Table 4.3 showsresults obtained recently when testing an implantable-device programmer for radiatedemissions. The specific frequencies selected for testing were identified the night beforetaking the device to an open-field test site in the middle of Texas’s hill country. Figure 4.5shows the device being tested at the open-field site. The device sits atop a motorizedturntable. A biconical antenna can be seen placed 10 m away from the device undertest. At the 10-m distance specified for the tests, radiated emissions have their electric-field1 TO 4 METERSEUT3 TO 30 METERS80 cmNON-CONDUCTIVE TABLECOAXIAL CABLETURNTABLEGROUND PLANEFigure 4.4 Setup for conducting radiated-emission measurements in an open-field test site. The device under test is placed on a nonconductivetable 0.8 m above a ground plane, and the distance between the device and the antenna is 10 m.
ELECTROMAGNETIC FIELDS 155TABLE 4.3EN-55011 Sample Worksheet for Testing Radiated Emissions aMeasurement distance: 10 mAntenna polarization: verticalDetector function: quasi-peakEUT Antenna Antenna CorrectedFrequency Direction Elevation Recorded Amplifier Factor Cable Level Limit Margin(MHz) (deg) (m) Level (dBµV) Gain (dB) (dB/m) Loss (dB) (dBµV/m) (dBµV/m) (dB)112.7 0 1.0 30.9 27.1 12.2 1.6 17.6 40 22.4130.0 270 1.0 42.8 27.0 11.8 1.7 29.3 40 10.760.0 270 1.0 38.5 27.3 8.9 1.0 21.1 40 18.9200.0 270 1.0 28.5 26.7 10.8 2.1 14.7 40 25.3298.9 150 1.0 30.2 26.5 13.9 2.6 20.2 47 26.8400.0 90 3.5 30.3 27.2 15.3 3.0 21.4 47 25.677.0 210 1.0 33.0 27.3 6.3 1.2 13.3 40 26.7110.0 300 1.0 39.0 27.1 12.1 1.6 25.6 40 14.4aCorrected level recorded level antenna factor cable loss. The frequencies of interest were selected during a precompliance scan ofthe device in a shielded room.Figure 4.5 A prototype implantable-device programmer is being tested at an open-field test site.The device sits atop a motorized turntable. A biconical antenna is placed 10 m away from the deviceunder test.E and magnetic-field H vectors orthogonal to each other but in the same plane. Under theseconditions, electromagnetic propagation occurs as a plane wave.If the test probe is brought closer and closer to the device under test, however, the natureof the electromagnetic field changes. Near the source of the radiation, the field producedis mostly a function of the impedance of the source. If the field is generated by a circuit
156 ELECTROMAGNETIC COMPATIBILITY <strong>AND</strong> <strong>MEDICAL</strong> DEVICEScarrying high current and low voltage, the field will be mostly magnetic in nature. If on theother hand, the field is produced by an element placed at high voltage but carrying little orno current, the field will be mostly electric in nature. This is the domain of the near field,while the plane wave is in the domain of the far field.The ideal generator for a magnetic field, or H-field as it is known, is thus a circular loopof area S(m 2 ) carrying an ac current I of wavelength λ. It should be noted that although astatic field is generated by a dc current and can be calculated with the method to follow,static H-fields do not cause radiated emissions and are thus disregarded for EMI purposes.If the loop size is smaller than the observation distance D, the magnitudes of the E and Hvectors can be found using the solutions derived from Maxwell’s equations. In the nearfield, the simplified values for these magnitudes areZ0ISE(V/m) 2 λD2andISH(A/m) 4π D 3where Z 0 equals the impedance of free space, 120π or 377 Ω. Inspecting these equations,we find that in the near field, H is independent of λ and decreases drastically with theinverse of the cube of the distance. At the same time, the electric field increases as frequencyincreases and falls off with the inverse of the square of distance.The wave impedance may be defined as the division of E by H in an electromagneticversion of Ohm’s law:E( V/m)Z wave (Ω) H ( A/ m)Thus,Z wave Z 0 2 πDλwhere D 48/f(MHz). In the far field [i.e., D 48/f(MHz)], on the other hand, both E- andH-fields decrease as the inverse of the observation distance as described byE(V/m) Z 0πISIS H(A/m) 2λ Dλπ2Dwhich maintains a constant impedance equal to Z 0 , allowing direct calculation of radiatedpower density in W/m 2 simply by multiplying E and H. Notice that E and H, and thuspower, increase with the square of frequency. This shows, once again, that limiting thebandwidth of radiated signals by a pulse train is of utmost importance in controlling EMI.The region dividing the near field from the far field is called the transition region [i.e.,at D48/f(MHz)]. In it, abrupt transitions occur on the near-field characteristics until asmooth blending leads to the far-field characteristics. Electromagnetic fields can also becreated by passing an alternating current through a straight wire dipole, just as in a radioantenna. In this case, the near-field electric and magnetic vector amplitudes areZ0IlλE(V/m) 82π D 3
ELECTROMAGNETIC FIELDS 157andIlH(A/m) 4π Dwhere l is the dipole length in meters. In contrast with the near-field H of a loop which fallswith the inverse of D 3 , the near-field H of a dipole falls off as 1/D 2 . Similarly, the near-fieldE of a dipole falls off as 1/D 3 , in contrast to the near-field E of a loop that falls as 1/D 2 . Thewave impedance of emissions radiated by a dipole is also affected differently by frequency: 2Z0λZ wave 2 πDCompare this equation with the equation describing Z wave in the near field. The change inwave impedance as a function of frequency in the case of a dipole is inverse to that of a loop.In the far field, the behavior of the E- and H-fields is again similar to that of electromagneticradiation from a loop; that is, they decrease as the observation distance increasesas described byZ0IlE(V/m) 2 λDIlH(A/m) 2λ DBeyond the transitional point, the wave impedance again remains constant at the value ofZ 0 . The result of a constant impedance in the far field means that the ratio of E to H componentsremains constant regardless of how the field was generated.Of course, real-life circuits are neither ideal open wires nor perfect loops, but rather,hybrids of these two. In a simplified form, as shown in Figure 4.6, a more realistic modelof a circuit which radiates electromagnetic emissions can assume that an ac voltage sourceZ SOURCEV o @ fProbeFigure 4.6 A simplified but realistic model of a circuit that radiates electromagnetic emissions. In it, an ac voltage source causes the flowof a current I in a rectangular loop enclosing an area S. The voltage seen by the load depends on the source and load impedances.
158 ELECTROMAGNETIC COMPATIBILITY <strong>AND</strong> <strong>MEDICAL</strong> DEVICEScauses the flow of a current I in a rectangular loop enclosing an area S. The source impedanceis Z source , and the impedance of the load is Z load , resulting in an overall equivalentimpedance of Z circuit Z source Z load .In the near field, the electric- and magnetic-field vector magnitudes are given bywhere Z circuit 7.9D(m)f(MHz), orwhere Z circuit 7.9D(m)f(MHz), andV0SE(V/m) 4 πD 3E(V/m) 0.63Sl f( MHz)2DISH(A/m) 4π D 3In the far field, the electric- and magnetic-field vector magnitudes are given byandE(V/m) Z 0 H H(A/m) 0.013V 0 S[ f(MHz)] 2DZ circuit35 10 6 IS[f(MHz)] 2DThe second lesson of controlling radiated emission leaps out from these equations-keep thearea enclosed by loops carrying strong time-varying currents to the minimum possible.Similarly, traces carrying high voltages should be kept as short as possible and be properlyterminated.Besides directing our attention to the parameters affecting radiated emissions, theseequations are very useful when designing for compliance with EMI requirements. Asexemplified by Figure 4.7, near- and far-field ballpark estimates of EMI can be obtainedfrom known circuit parameters for a large number of common circuit topologies.PROBING E- <strong>AND</strong> H-FIELDS IN THE NEAR FIELDThe main reason why EMI standards establish that testing should be performed in the farfield is that as demonstrated above, a constant impedance in the far field causes the ratio ofE to H components to remain constant regardless of how the field was generated. Thismeans that measurements can be reproduced with reliability and standardized methods oftesting can be defined with ease. From the past equations, however, it would seem possibleto establish a quantitative correlation that would allow far-field estimates from near-fieldmeasurements. Unfortunately, in practice, this is not the case. Near-field measurements areextremely dependent on the exact geometry of the source, the position of the near-fieldprobe, and the interaction between the probe and the source to accomplish the exact measurementsnecessary for calculating the behavior of the radiation in the far-field region.Although not applicable to predict the outcome of compliance tests, near-field measurementscan nevertheless be very useful to the designer in locating potential sources ofradiated emissions. Here, near-field qualitative measurements with simple instruments
PROBING E- <strong>AND</strong> H-FIELDS IN THE NEAR FIELD 159Figure 4.7 Simple differential-mode radiating circuit configurations are created when an ac current flows on a current path that forms aloop enclosing a certain area S. (a) Transient power demands of an IC are supplied by a decoupling capacitor, causing brief, strong currentsthat circulate on a loop formed by the supply-bus PCB tracks. (b) Fast digital signals driving low-impedance inputs form EMI-radiating loopswhen current returns through distant ground paths.can accurately pinpoint sources of EMI and identify their basic characteristics. Inessence, if a strong E-field is detected from a certain circuit section but a relatively weakH-field is sensed at the same point, the culprit can usually be traced to a train of highvoltagepulses on a long wire, an unterminated line, or a trace driving a high-impedanceload. Conversely, if the H-field is strong but the E-field probe detects little activity, thesource of EMI is most probably a looplike circuit through which strong currents circulate.Examples of such situations are PCB tracks carrying strong currents, inductors inswitching power supplies, and eddy currents induced in metal enclosures by strong fieldsinside the case.Since the same equations used to describe emission of radiation are applicable to thereception of emissions, it is apparent that a small loop of wire can act as a near-field probewhich is mostly sensitive to H-fields. E-fields, on the other hand, would then be detected,preferably by a short exposed wire. Measurements can then be taken with either a widebandac voltmeter or a spectrum analyzer. Even a simple single-turn wire loop at the endof a coax cable can be a very effective H-field probe. With this arrangement, maximumoutput from the probe is recorded when the loop is in immediate proximity and alignedwith a current-carrying wire. This directionality is very useful for pinpointing the exactsource of a suspicious signal.The diameter of the loop makes a large difference on H-field measurements [Kraz,1995]. The area enclosed by the loop influences the sensitivity of the probe, since it determinesthe number of magnetic flux lines that are intercepted to produce a detectable signal.A larger loop will obviously develop a larger voltage at the input of the voltmeter or spectrumanalyzer. On the other hand, larger loops have inherently larger self-inductance andequivalent capacitance than small loops. As inductance increases, the network formed withthe complex impedance of the measurement setup resonates at lower frequencies, beyondwhich the probe cannot be used. Moreover, larger loops make it much more difficult to identifythe exact source of an interfering signal, because their size does not allow them to pickup radiations selectively from single lines when a multitude of the latter are clustered closetogether. Coils with multiple turns can be used to increase the sensitivity without appreciably
160 ELECTROMAGNETIC COMPATIBILITY <strong>AND</strong> <strong>MEDICAL</strong> DEVICESincreasing the physical size of the coil. However, this solution will again result in reducedspectral response due to increased self-inductance. It is clear, then, that loop geometry mustbe chosen for every specific instance based on a solution of compromise. In general, it is agood idea to keep a variety of probes handy to tackle different problems.Another convenient H-field probe can be constructed similar to ac tongs. In this case, amagnetically permeable material concentrates the magnetic flux lines created by the circuitunder test. The resulting magnetic flux is then detected by a coil with multiple turns.If the tongs were to enclose completely the conductor through which a current is flowing,the voltage developed across the coil would be proportional to the vector sum of the currentsthrough the conductor. This is, of course, impractical for the needs of sniffing H-fields, and a structure with open-ended tongs is more suitable for probing a circuit withoutmodifying it.The probe can be built as shown in Figure 4.8, using a small ferrite bead (e.g., 0.1 in.thick, 0.3 in. in outside diameter) that has been sectioned in half. The actual constructiondepends on the actual ferrite that you select, but in general, 40 to 50 turns of thin enameledcopper wire provide suitable sensitivity. The terminals of the coil should be solderedto the center and shield of coaxial cable. After insulating the central conductor connection,a portion of the braid should be used to cover the assembly, thus E-field-shielding the coil.The assembly can then be mounted at the end of a small plastic tube and embedded withina glob of epoxy. For the prototype probe, a virtually flat bandwidth was measured fromaround 600 kHz to approximately 10 MHz.Better bandwidth can be achieved by using a VCR magnetic head instead of the ferriteassembly. Video heads are designed for broadband detection of magnetic fluctuations, andfor this reason they can be used for sniffing H-fields from 2 MHz up to approximately120 MHz with relatively flat response. To construct the probe, carefully remove one of theCoaxPlastic TubeEpoxy GlobE-Field Shield~0.3Ferrite “U”Figure 4.8 A useful H-field probe can be constructed from a small ferrite bead that has been sectionedin half. Approximately 40 turns of thin enameled wire are used to detect the magnetic fluxconcentrated by the ferrite. A small portion of the coax cable braid is used as an E-field shield forthe coil. The assembly is mounted at the end of a small plastic tube that serves as a handle andembedded in a glob of epoxy.
BARE-BONES SPECTRUM ANALYZER 161magnetic heads from a discarded drum. Even a very worn-out head will work well in thisapplication. Very soiled heads should be cleaned with a swab and pure alcohol. Degaussingwill also help improve the sensitivity of an old head. All other aspects of constructing andusing this probe are the same as for the ferrite-bead probe.For E-fields, the simplest near-field probe is a coax cable in which a short segment ofthe center conductor extends beyond the braid at the unterminated end of the coax. Similarto the loop probe, a longer wire will pick up a stronger signal at the expense of specificityand bandwidth. In general, the length of the wire should be selected so that measurementscan be performed with a sensitivity of approximately 3 mV/m. At this level, potentiallyproblematic emissions can be identified without causing undue concern about low-levelemissions.Constructing the ideal H- or E-field probe for a specific job may take some trial anderror, since the effort of electromagnetic modeling required for proper design is most probablyan overkill for most applications. One test that you may nevertheless want to performon a probe is to determine the existence of resonances within the desired spectral range.To conduct the test, a wideband probe should be connected to an RF generator set up totrack the tuning frequency of a wideband spectrum analyzer. The probe under test shouldbe located in close proximity to the emitting probe and connected to the input of the spectrumanalyzer. The limit of the useful bandwidth of a probe is the point at which the firstabrupt resonance appears.Before even plugging the spectrum analyzer to the power line, however, the first step inconducting a near-field EMI study should be to draw a component placement diagram ofthe assembly to be probed. The diagram should indicate circuit points identified in themathematical circuit harmonic analysis as potential sources for EMI radiation. Only afterthis preliminary work has been done should bench testing begin. A coarse near-field sweepshould be conducted at relatively high gain to identify EMI hot spots in the assembly. Atechnique that works well is to log the frequencies at which strong components appearwhen scanning the unit under test. Detailed scanning using a more discriminating probecan then concentrate on the hot spots to identify the culprit circuit generating offendingemissions.A very valuable source of clues for future troubleshooting can be built along the way byprinting the spectral estimate at each point in which measurements strongly agree or disagreewith the circuit’s harmonic analysis. In any case, keep detailed and organized notesof the near-field scans, since these will certainly prove to be invaluable when attemptingquick fixes while the clock is running at the far-field compliance-testing facility.BARE-BONES SPECTRUM ANALYZERWhile an ac voltmeter can provide an indication of the field strength to which a probe isexposed, it does not provide any indication of the spectral contents of an emission. A spectrumanalyzer is a tool that certainly cannot be beaten in the search for offending signals.Unfortunately, spectrum analyzers are often beyond the reach of a designer on a tight budget.For near-field sniffing, however, even the crudest spectrum analyzer will do a magnificentjob.Figure 4.9 shows a simple home-brewed adapter to convert any triggered oscilloscopeinto a spectrum analyzer capable of providing qualitative spectral estimates with a bandwidthof 100 kHz to 400 MHz. As shown in Figure 4.10, a voltage-controlled TV tuner IC1forms the basis of the spectrum analyzer. Most any voltage-controlled tuner will work, andyou may be able to get one free from a discarded TV or VCR printed circuit board. The connectionpoints and distribution vary from device to device, but the pinout is usuallyidentified by stampings on the metallic can of the device.
162 ELECTROMAGNETIC COMPATIBILITY <strong>AND</strong> <strong>MEDICAL</strong> DEVICESFigure 4.9 A simple circuit can be used to convert any triggered oscilloscope into a 100-kHz to 400-MHz spectrum analyzer suitable fornear-field EMI sniffing.Varactor-controlled TV tuners receive signals on their RF input at a frequency determinedby the voltage applied to the VTUNE input. With power applied to the UHF section ofa tuner, typical control voltages between 0 and 32 V span a frequency range of approximately450 to 850 MHz. The sensitivity of the tuner can be adjusted through the AGCinput. The output of the tuner is a standard 45-MHz IF. However, 450 to 850 MHz is not arange that is directly applicable to the large bulk of EMI sniffing work. For this reason, themore appropriate range 100 kHz to 400 MHz is up-converted to the tuner’s input rangethrough a circuit formed by IC4–IC7 (manufactured by Mini-Circuits). Here, signals fromthe probe are low-pass filtered by IC6 and injected into the IF port of a TUF-2 mixer. TheLO input of the mixer is fed with the output of IC4, a self-contained voltage-controlledoscillator tuned to 450 MHz by potentiometer R20. The RF port of the mixer outputs signalswith frequency components at the sum and difference between the IF input and theLO frequency. This output is high-pass filtered by IC5 to ensure that only up-convertedcomponents are fed to the tuner input.Sweeping the tuner across its range is accomplished by a sawtooth waveform thatspans approximately 1 to 31 V. The basic sawtooth is generated by IC3 and Q1 andbuffered by IC2B. The span of the sawtooth is set by attenuator R10, while the center ofthe sweep is adjusted by introducing an offset on IC2A by means of R13. The output ofIC2A is amplified by transistor Q2. Q2 should be selected for a gain of 50 or less. Thefinal span and linearity of the sweep is adjusted in three ranges by R1, R2, and R3.The IF output of the tuner is attenuated to a level suitable for processing by R7, R8, andR9. The actual value of the resistors for this attenuator must be selected based on the outputlevel of the specific tuner that you use. Then, in the circuit of Figure 4.11, IC8, a NE/SA605
45MHz_IFR813R982L2L1L<strong>OF</strong>REQUENCYADJUSTFROMPROBER2010kC140.01uF+ C1510uF+12V+ C1747uF81IC6PL P-4501 8IN OUTIC4POS-535-VCOV2J1BNC 1+ C1210uFC110.01uF18uH0.1-400MHzC160.01uF+12VV_TUNELOW-PASSFILTER+3 4 5 6 7R F_OUT2IC7TUF-2_MIXER2450MHz4C80.01uFIF RF+ C9RFSHIELD110uF18uHIC5PHP-400C100.01uFHIGH-PASSFILTER1 8IN OUT+ C1347uFTV_TUNER+12V450-850MHzIC11 2 3 4 5 6 7 9GND0+12VR713GND1GND2GND3GND4GND5GND6GNDGND1GND2GND3GND4GND5GND6LORF_INV_TUNEB+VHFAGCB+LO_VHFB+UHFB+MED_VHFIF_OUTGND1GND2GND3GND4GND5R1447k2 3 4 5 6 732 3 4 5 6 7R510k+12V4RQDISTHRIC3NE555376R191kBLANKCENTER FREQUENCYADJUSTR162.2kR1710k2+12V31R184.7kQ12N2907+ C66.8uFR1547k-12V56R1325k411+12VSWEEPSPANADJUST+--12V+ C4+710uFC510uFIC2BTL084R1025kR1247k32+12V411+--12VR1147k1IC2ATL084R1147k231R3100kQ22N3904+32VD21N5252R2100kLINEARITYADJUSTD11N524 5R1100kC20.01uF+C310uFR610kTUNERGAINADJUSTC10.01uFFigure 4.10 A varactor-based TV tuner is the heart of a simple spectrum analyzer. Signals of 100 kHz to 400 MHz from a sniffing probeare up-converted to the 450- to 850-MHz UHF band, where the tuner can be swept by a sawtooth waveform. The tuner produces a 45-MHzintermediate frequency that can be processed to derive the input signal spectrum. Direct connection of the probe to the tuner input extendsthe range of the spectrum analyzer to the high-VHF/UHF region (450 to 850 MHz).2TR5CVC70.01uF163
164Figure 4.11 The intermediate-frequency output of the tuner is detected by IC8, a single-chip IF processor. The received signal strengthindicator (RSSI) output as a function of the sawtooth signal driving the tuner is a logarithmic representation of the spectrum of the signalpicked up by the probe.
single-chip IF processor, takes care of detecting the signal and producing a logarithmic outputof signal strength.In this portion of the circuit, the 45-MHz IF signal is coupled to the input of a RF mixerinternal to IC8 by way of a tuned circuit formed by C18, C19, and L3. The LO input ofthis mixer is fed from a 44.5-MHz crystal-controlled oscillator. The resulting 455-kHz IFis filtered by two ceramic filters, FLT1 and FLT2. An internal received signal strength indicator(RSSI) circuit is used as a detector and linear-to-logarithmic converter. The RSSIoutput, as a function of the sawtooth signal driving the tuner, is thus a logarithmic representationof the spectrum of the signal picked up by the probe. RSSI is a current signal thatrequires conversion to a voltage by the network formed by R21–R23 and D3. C24 lowpassfilters the RSSI output to produce a smooth display, and IC2C acts as a buffer andimpedance transformer for the current-to-voltage converter. Finally, IC9A blanks the outputduring retrace.Figure 4.12 presents the power supply circuit for the adapter. Most of the circuitry, includingthe up-converter, tuner, and sawtooth generator, is powered by 12 V; 5 V powers the IFprocessor. The 32 V to drive the tuner’s varactors is obtained by multiplying the 12 V ac inputto 48 V, reaching the desired voltage through IC10, an LM317 adjustable linear regulator.To operate the spectrum analyzer, the Y output of the adapter is connected to the verticalinput of the oscilloscope, and the TRIGGER output is connected to the trigger synchronizationinput of the scope. The horizontal frequency of the oscilloscope is set suchthat one full sweep caused by the sawtooth fits the full graticule on the oscilloscope’sscreen. Fine-tuning can be accomplished either by trimming the time base of the scope orby adjusting the value of R18 appropriately. Alternatively, a two-channel oscilloscope canbe operated in the X–Y mode by injecting the sawtooth available at pin 7 of IC2A to theappropriately scaled X-axis channel.The comb generator circuit of Figure 4.13 can be used for calibrating the adapter. Thecircuit is simply a TTL-compatible 40-MHz crystal-controlled oscillator module feeding asynchronous binary counter. It is called a comb generator because the spectral pattern ofany of its outputs resembles an ordinary hair comb with its prongs pointing up. Becausethese spectral components occur at harmonic multiples of the fundamental square-wavefrequency selected, it follows that the frequency difference between consecutive “prongs”must be the same as the value of the fundamental frequency of the square wave.Figure 4.14 presents the pattern obtained when the 20-MHz comb output of the generatoris probed by a commercial spectrum analyzer. Ac coupling was accomplished througha series-connection 15-pF capacitor, and termination to ground of the output side of thiscapacitor was performed through a 50-Ω noninductive resistor. This is the gold standardagainst which the adapter should be calibrated.Start testing the adapter by setting the sawtooth generator to vary the voltage at theVTUNE input of the tuner between approximately 1 and 31 V. Initially, set R6 to apply2.5 V dc to the AGC pin of IC1. The up-converter LO frequency should be adjusted to450 MHz by trimming R20. 9.6 V dc at the VTUNE input of IC4 will typically result in thedesired LO frequency. L4 should be trimmed to achieve stable oscillation of the 44.5-MHzIF LO oscillator. With a 40-MHz comb applied to the input of the adapter through a 15-pFcoupling capacitor and with 50-Ω termination, adjust L3 to obtain an approximation of theexpected 40-MHz comb pattern on the oscilloscope. After achieving a satisfactory displayfor the 40-MHz comb, calibrate the linearity of the adapter using a 20-MHz comb by firsttrimming R3 to produce equal spacing between spectral lines throughout the lower thirdof the display. Then linearize the midrange by trimming R2, and finally, the high range bytrimming R1.BARE-BONES SPECTRUM ANALYZER 165
166 ELECTROMAGNETIC COMPATIBILITY <strong>AND</strong> <strong>MEDICAL</strong> DEVICESC34470uF+D41 21N4005D51 21N4005+ C33470uFD61 21N4005+ C35470uF48VC360.1uF3IC10LM317HV/ TOVINADJ1R3950kVOUT2R3082C380.1uF+ C39100uF+32VC370.01uF115VACT112VAC 1AD71 21N4005+ C40C41IC11LM7812C/TO2201 3INOUTGNDC42+ C43+12V2200uF0.1uF20.1uF100uF1IC12LM78L05A/TO39VIN VOUT2+5VC44100uF+C450.01uFGND3C460.01uF+C47100uF+ C48100uFD82 11N4005C492200uF+C500.1uFIC13LM7912C/TO33 2INOUTGND1C510.1uFC52+ 100uF-12VFigure 4.12 Dc power for the various circuits of the spectrum analyzer is derived from a single 12-V ac input. A voltage of 12 V powersmost of the circuitry, including the up-converter, tuner, and sawtooth generator; 5 V powers the IF processor. Sweeping the tuner acrossits 450 to 850 MHz range requires up to 32 V to drive its varactors. A voltage of 12 V is used as bias to ensure that sweeping can beaccomplished within any desired portion of the full range.CONDUCTED EMISSIONSConducted emissions measurements are made to determine the line-to-ground radio noisefrom each power-input terminal of a line-powered medical device. Measurements aretaken using a line impedance stabilization network (LISN). A spectrum analyzer and aquasi-peak adapter with a measurement bandwidth of 9 kHz are typically used to recordthe conducted emissions. As shown in Figure 4.15, tests are performed in a shieldedroom.A LISN is a passive RCL network that connects between the ac power line and thedevice under test. The purpose of the LISN is to present a standard line impedance tothe device under test regardless of local power line impedance conditions. The LISN also
CONDUCTED EMISSIONS 167J2BNC1220MHz COMB+5V1J3BNC10MHz COMBC6140.01uFIC340MHz_OSC 7GND VCCOUT8+5V151109144511IC2ABCDQAQBQCQDRCO326713CLKGD/ULOAD 12MX/MN74F1912J4BNC15MHz COMB2J5BNC12.5MHz COMB212U4A74F32345910U4B74F32U4CJ1BNC6 140MHz COMB28121374F32U4D1174F32S11IC1LM78L05A/TO39VINVOUT2+5V9VBT1+ C3100uFC10.01uFGND3C20.01uF+C4100uFC70.01uFC50.01uFFigure 4.13 High-frequency clocks and fast logic generate broadband signals extending well into the hundreds of megahertz. This generatorproduces various comb patterns which are useful in the calibration of spectrum analyzers.isolates the device under test from unwanted interference signals on the power line andprovides a test point to probe emissions conducted from the device under test toward thepower line. Figure 4.16 presents the circuit for a 50 Ω/50 µH LISN following the definitionof standard CISPR-16-1. This circuit provides a 50-Ω output impedance for measurementof RF emissions produced by the device under test. This impedance was selected becausetheoretical and empirical data have shown that the power circuitry statistically looks like a50-Ω impedance to standard electronic equipment, and RF test equipment is typicallydesigned for 50-Ω input. The bandwidth is typically determined by the operating frequencyof the potential victims of the device under test’s conducted emissions. For themajority of medical devices, emission measurements are carried out from 150 kHz to30 MHz. This ensures that devices do not interfere with VLF or HF radio communicationsystems and other electronic devices operating at these frequencies.
168 ELECTROMAGNETIC COMPATIBILITY <strong>AND</strong> <strong>MEDICAL</strong> DEVICESFigure 4.14 The spectral pattern obtained from the output of the comb generator can be used as a frequency ruler because it presents strongspectral lines at every harmonic of the fundamental square wave. Notice the similarity between the envelope formed by the spectral componentsof this 20-MHz comb and the nomograms of Figure 4.2.Each of the 50-µH inductors and 1-µF capacitors form an unbalanced filter. The inductorsmust be of sufficiently large wire gauge to carry the full ac current demanded by thedevice under test with less than a 2-V drop. Conducted emissions are then measured usinga spectrum analyzer with quasi-peak detection. Measurements are taken between hot toground and then between neutral to ground. A 50-Ω resistor needs to be connected acrossthe 1-kΩ resistor, which is not connected to the spectrum analyzer’s 50-Ω input. SwitchSW1 accomplishes phase selection and automatic shunting of the LISN leg not beingobserved.Note that the LISN established by the standards presents a 1-µF capacitance betweenthe hot line and the LISN and device under the test’s safety ground. A ground fault couldlead to potentially lethal currents to operators in contact with the LISN or the device undertest. For this reason, it is advisable to wire the LISN’s ground terminal permanently toground.A safer way of running design-time tests is to use a LISN made from a modified powerprotector designed to filter power line glitches prior to supplying power to computers andother electronic equipment. The circuit for this LISN is shown in Figure 4.17. The inputconnector and power cord, circuit breaker F1, and neon light are found almost universallyin power protector strips. You may also leave any MOVs that you find in the power strip.
CONDUCTED EMISSIONS 169LISN40 cmLISNEUT1 x 1.5 METER TABLE3.6 m x 4.9 m SHIELDED ENCLOSURECONTROLLERQUASI-PEAKADAPTERSPECTRUMANALYZERFigure 4.15 Setup for performing conducted emissions testing in a shielded room. Measurements are taken using a line impedance stabilizationnetwork (LISN). A spectrum analyzer and a quasi-peak adapter with a measurement bandwidth of 9 kHz are typically used to recordthe conducted emissions.Modify the filter circuitry and configure it as shown in the schematic diagram. You mayremove all except one of the power outlets to accommodate the components. The poweroutlet used to connect to the device under test (J2) would be one of the power strip’s originalpower outlets.Emissions radiated from this LISN are coupled inductively to a spectrum analyzer. L3is a single loop of No. 14 stranded insulated wire that exits and reenters the power strip’senclosure. The H-field probe made of a VCR head, described above, would then be usedto pick up conducted emissions. Although this LISN does not yield results identical tothose of the standards, it makes it easy to detect emissions conducted by the device undertest into the power line. In addition, although conducted emissions tests should be performedon both phases (hot and neutral) of the power line, most offensive units revealthemselves with just the hot-to-ground measurement provided by this LISN.When the device is prepared for testing, the power cord in excess of the distance isfolded back and forth, forming a bundle 30 to 40 cm long in the approximate center of thecable. Power supply cords for any peripheral equipment should be powered from an auxiliaryLISN. Excess interface cable lengths should be bundled separately in a noninductivearrangement at the approximate center of the cable with the bundle 30 to 40 cm inlength. The emissions conducted are maximized by varying the operating states andconfiguration of the device under test. The limits for conducted emissions per EN-55011for group 1 devices are shown in Table 4.4. As an example, Table 4.5 shows the resultswe obtained recently when testing an implantable-device programmer for conductedemissions.
Metal BoxHot(Black)L150uHC11.0uF 400VACC30.1uF 600VACJ1ToPowerline13Ground(Green)R11KPhase Selection SwitchHotNeutral3J2 1ToDeviceUnderTest2Neutral(White)C21.0uF400VACL2R21KC40.1uF600VACS1SW DPDTR350250uHJ321BNCPermanent Connectionto GroundTo 50 ohmSpectrumAnalyzerFigure 4.16 A 50 Ω/50µH LISN as defined by standard CISPR16-1. This circuit provides a 50-Ω output impedance for measurement ofRF emissions produced by the device under test. Conducted emission measurements are carried out from 150 kHz to 30 MHz.To Spectrum AnalyzerSA 1SA 2Metal Box5L3184H-FieldProbeInsulated WireHOTBlackCB11 2L1500 uHL450 uHHOTBlack1J13GROUNDGreen12R2LA1110V Neon Lamp Assy.C20.22uF 600 VACR147GROUNDGreenJ2312C11uF 400 VACC32uF 400 VAC2NEUTRALWhiteL2500 uHNEUTRALWhite120 VFigure 4.17 A safer way of running lab tests is to use a LISN in which radiated emissions are coupled inductively to a spectrum analyzer.L3 is a single loop of No. 14 stranded insulated wire which is coupled to an H-field probe made of a VCR head.170
SUSCEPTIBILITY 171TABLE 4.4EN-55011 Conducted Emissions Limits for Group 1 Devices aClass AMaximum RF Line Voltage (dBµV)Class BFrequency (MHz) Quasi-peak Average Quasi-peak Average0.15–0.5 79 66 66, decreasing with log 56, decreasing withof frequency to 56 log of frequency to 460.5–5.0 73 60 56 465.0–30.0 73 60 60 50aThe limit decreases linearly with the logarithm of the frequency in the range 0.15 to 0.5 MHz. The lower limits apply atthe transition frequencies.TABLE 4.5EN-55011 Sample Worksheet for Testing Conducted EmissionsLine measured: phaseFrequency Reading Correction Correction Limit DetectorInput (MHz) input (dBµV) Factor (dB) Reading (dBµV) (dBµV) Margin (dB) Function0.257 45.5 0.8 46.3 66 19.7 Peak0.323 42.7 0.7 43.4 66 22.6 Peak0.195 41.9 1.0 42.9 66 23.1 Peak0.385 38.8 0.6 39.4 66 26.6 Peak0.451 34.8 0.6 35.4 66 30.6 Peak20.100 57.3 1.8 59.1 60 0.9 Peak18.100 56.0 1.5 57.5 60 2.5 Peak18.500 53.1 1.6 54.7 60 5.3 Peak19.000 50.8 1.7 52.5 60 7.5 PeakSUSCEPTIBILITYIt is really surprising that regulatory agencies around the world took so long to take stepsthat would protect patients and health-care providers from EMI-induced medical-devicefailures. Although the military and aviation industries had been developing hardwareimmune to EMI for many years, it was only in 1994 that the FDA started taking action bywarning the medical device industry about their concerns regarding EMI-induced failures,as well as by making specific recommendations for immunity levels for critical devices. In1998, European agencies advanced this process by making it mandatory for medical devicesto comply with a fairly comprehensive EMC standard to be marketable in Europe. Today,most nations which require medical devices to comply with EMC requirements make useof standards based on the EN-60601-1-2 immunity requirements shown in Table 4.6, whichcover electrostatic discharge (ESD), radio-frequency interference (RFI), and a variety ofpower disturbances. IEC-60601-1-2 itself cites extensively the test methods and immunitylevels of the basic IEC-61000-4 series of standards.At the time of this writing, EN-60601-1-2, pass/fail criteria are ultimately defined bythe manufacturer. This is because the current immunity criteria for medical products aredefined in this standard as “equipment and/or system continues to perform its intendedfunction as specified by the manufacturer or fails without creating a safety hazard.” A safetyhazard is then defined as a “potentially detrimental effect on the patient, other persons,animals, or the surroundings arising directly from equipment.” As a result, the manufacturer
172 ELECTROMAGNETIC COMPATIBILITY <strong>AND</strong> <strong>MEDICAL</strong> DEVICESTABLE 4.6EN-60601-1-2 Immunity RequirementsSusceptibility Test Requirements Relevant StandardElectrostatic discharge (ESD) 3-kV contact to conductive accessible parts and coupling planes; 8-kV air IEC-61000-4-2discharge to nonconductive accessible partsRadiated emissions (EMIs) 3 V/m, 26 MHz to 1 GHz, modulated at passband or 1 kHz IEC-61000-4-3Conducted emissions Test from 150 kHz to 80 MHz into power line to 3 V/m; bulk current injection IEC-61000-4-6for patient cablesPower line voltage dips, 100% dropout for 1 cycle, 60% sag for 5 cycles, 30% sag for 25 cycles; IEC-61000-4-112interruptions, and variations low-powered equipment maintains clinical utility, high-powered equipmentremains safeElectrical fast transients (EFTs) 1 kV at power line for plug-connected equipment; 2 kV at power line for IEC-61000-4-4permanently installed equipment; 0.5 kV for signal lines longer than 3 mSurge 1 kV differential mode at power line, 2 kV common mode at power line; IEC-61000-4-5signal lines not testedMagnetic fields 10 A/m at power line frequency IEC-61000-4-8may chose to classify a failure mode that does not pose a risk to the patient (or other surroundingtargets) as a pass. For example, the manufacturer may pass a device that fails tostart operating or stops operating when exposed to EMI threats as long as these modes donot pose a threat to the patient. A common classification for device performance duringtesting is as follows:• Criteria level A: normal performance within equipment specifications• Criteria level B: degradation or loss of function or performance which is selfrecoverablewhen the interfering signal is removed• Criteria level C: degradation or loss of function or performance that requires systemreset or operator intervention when the interfering signal is removedIn the United States, the FDA is adopting many of the IEC-60601-1-2 requirements butimposes restrictions on the manufacturer’s ability to adopt pass/fail criteria. The FDA prescribesthat a passing result corresponds to maintaining clinical utility. Some of the sameconcerns are also being adopted for revised versions of IEC-60601-1-2 and drafts showthat the failure criteria will change in focus from the safety hazard to specified performancecompliance. Because of the fast-changing nature of this field, we present this sectionas a primer on the issue of immunity to EMI, but strongly advise you to keep updated onthe latest versions of applicable standards.Susceptibility to Electrostatic DischargeDo you know what is the potential difference between you and the doorknob before youshout “ouch!” on those winter days that electrostatic charges seem to love? 6 kV! But thereare also occasional 15-kV discharges—the kind that make you hope that someone else willopen the door for you. Regardless of the specific number of kilovolts, such dischargessuffice to fry many static-sensitive ICs. However, the primary concern with ESD events isthe large amount of RF energy they convey over an extremely wide band of frequencies.IEC-61000-4-2 considers ESD between a human being and a medical device as the primarysource of ESD-related failures. Testing is done by delivering 3-kV dischargesdirectly to a device’s exposed conductive components and 8-kV air discharges to parts thatmay be recessed.
SUSCEPTIBILITY 173The human body model of Figure 4.18 represents the discharge from the fingertip of astanding person delivered to a device, modeled here by a 150-pF capacitor dischargedthrough a switching component and a 330-Ω series resistor into the device under test. Thismodel, which hasn’t changed much since it was developed in the nineteenth century, wasoriginally used to investigate explosive gas mixtures in mines. An ESD simulator is notmore than an instrument implementing this model. A high-voltage power supply is used tocharge a 150-pF capacitor via a charging resistor. The capacitor’s charge is then deliveredto the device under test by way of a 330-Ω resistor. The switch may be a vacuum relay, ahigh-voltage semiconductor switch, or a spark gap.Construction of the ESD simulator should enable it to generate a discharge waveformwith the parameters shown in Table 4.7. Obviously, the most critical design considerationis being able to generate the ESD with a rise time of 0.7 to 1 ns. The frequency content ofsuch an ESD waveform is flat to around 300 MHz before it begins to roll off, so it containssignificant energy at 1 GHz and above. Short rise time is so important because it is thepulse’s dV/dt as well as the dI/dt that it causes which allow ESD to induce currents andvoltages in a device’s circuits which lead to failures. Suppose, for example, that a PCBtrack within the medical device’s circuit has an inductance of 10 nH/cm. If current from anESD event is directly or indirectly coupled to that PCB track, the voltage induced along alength l of that track will be given byV 10(nH/cm) l(cm) d IdtRCHARGESCHARGE330SESDHigh VoltageDC Supply150pFDeviceUnderTestFigure 4.18 The human body model of ESD represents discharge delivered to a device from thefingertip of a standing person. It is modeled by a 150-pF capacitor discharged through a switchingcomponent and a 330-Ω series resistor into the device under test.TABLE 4.7IEC-801-2 (1991) ESD Waveform ParametersFirst PeakSeverity Voltage Current of Discharge Rise Time Current at Current atLevel (kV) (5%) (A) (10%) (ns) 30 ns (A) (30%) 60 ns (A) (30%)1 2 7.5 0.7–1 4 22 4 15 0.7–1 8 43 6 22.5 0.7–1 12 64 8 30 0.7–1 16 8
174 ELECTROMAGNETIC COMPATIBILITY <strong>AND</strong> <strong>MEDICAL</strong> DEVICESSince even a modest ESD event can develop a current of 10 A in 1 ns, the voltage inducedacross 1 cm of PCB track will be as high as 100 V! Similarly, high currents can flowthrough capacitances on and across circuit components. Current flowing through a capacitoris given byI C dVdtIf an ESD event causes a change in potential of 1 kV within 1 ns, the current flowingthrough an unprotected input with 10-pF capacitance would be as high as 10 A.Testing for Immunity against ESD Two ESD testing techniques are used to check medicaldevices. The first is air discharge; the second is contact discharge. Testing by air dischargeconsists of charging the ESD simulator to the required test voltage and slowly moving thesimulator’s discharge electrode toward the device under test until discharge occurs. This isvery similar to what happens when a charged human approaches a device. However, testresults obtained through this technique are notoriously unrepeatable, since the tester’s rateof approach, exact angle of approach, conditions of the air around the device, and othervariables influence the magnitude and path the discharge will take through the device undertest.The contact test technique was developed in an attempt to improve repeatability. In thistest, the discharge electrode of the ESD simulator is held in contact with a metallic surfaceon the device under test when the discharge switch closes. The actual discharge occurswithin the ESD simulator in a controlled environment, and the current can be injected atthe same contact point each time. The test requires an unpainted conductive contact areaon the device under test. As such, this test applies only for devices that have a conductivesurface from which paint can be removed and is not applicable when no metallic surfacesare directly accessible.Testing to EN-61000-4-2 involves delivering air discharges of up to 8 kV (using an8-mm round tip to simulate a human finger) to everything nonmetallic that is normallyaccessible to the operator. Contact discharges of up to 3 kV (using a sharp tip that istouched against the product before the discharge) are applied to operator-accessible metalparts. Test voltages are increased gradually from low values, often using the settings 25%,50%, 75%, and then 100% of the test voltage. This is because ESD failures are sometimesseen to occur at lower voltages but not at the maximum test level. The highest test level onan ESD test is not necessarily the one most likely to cause a failure.It must be noted that the contact test is more severe than the air-discharge test. This isbecause the former yields faster rise times than the latter. In turn, faster rise times yieldhigher bandwidth for the EMI generated by the ESD event. An 8-kV air discharge is in thesame category as a 6-kV contact discharge, and a 15-kV air discharge is as severe as an8-kV contact discharge. Note the nonlinear relationship. European regulatory agencies areconsidering increasing the 3-kV contact test level to 6 kV, so keep yourself up to date withthe standards.Despite the simplicity of the human discharge model, ESD simulators are not all thatsimple, and commercial units are certainly expensive. However, for development-time testingmeant to give you a good “gut feeling,” there are some simple alternatives to buying afully compliant ESD test system. Tiwari [1996] proposed modifying a piezoelectric typeof kitchen gas lighter as a fast-static-charge generator which can produce an ESD-like dischargethrough air.As shown in Figure 4.19, the modification involves removing the gas reservoir andreplacing the gas feed line by a pin which extends beyond the gas lighter’s tip. When thehandle is squeezed and the tip of this makeshift ESD gun is placed in close proximity(e.g., 1 4 in.) to a conductive member of the device under test, a spark jumps, conveying
SUSCEPTIBILITY 175Gas delivery tube replacedby # 10 insulated wireGAS RESERVOIRREMOVED50 OhmTo earth groundDischarge return electrodeconnected to 2 meterinsulated wireTo fast oscilloscopeFigure 4.19 A piezoelectric-ignition gas lighter can be modified to generate ESD-like events. The modification involves removing the gasreservoir and replacing the gas feed line by a pin that extends beyond the gas lighter’s tip. Typical ignition piezoelectric crystals can generatedischarges conveying approximately 0.2 µC within a total pulse of 100 ns to 1 µs. To assess the current and waveform delivered by thedischarge, use a 50-Ω resistor in series with the ESD gun’s ground terminal as a current shunt.approximately 0.2 µC within a total ESD pulse of 100 ns to 1 µs. To assess the current andwaveform delivered by the discharge, use a 50-Ω resistor in series with the ESD gun’sground terminal as a current shunt.A simulator which produces waveforms that are closer to a professional unit compliantwith IEC-801-2 [1991] can be built for under $100 using surplus high-voltage components.In the circuit of Figure 4.20, a TDK model PCU-554 dc-to-ac inverter is used to drive aCockroft–Walton quintupler. The dc-to-ac inverter is originally sold as a cold-cathode fluorescentlamp driver for LCD screen backlighting and may be substituted by any similar partcapable of delivering at least 1.2 kV RMS at 10 mA. The module produces a high-voltage outputthat is proportional to its dc input. Dc power for the module is supplied by a variable powersupply built around IC1, a LM317 adjustable voltage regulator. The PCU-544 operates wellfor input voltages in the range 1.5 to 5 V.The output polarity of the Cockroft–Walton multiplier depends on the way in which itsdiodes are oriented. Since ESD standards call for testing with discharges of both polarities,the multiplier was designed to yield either positive or negative output. If the high-voltageac output of the dc-to-ac inverter is connected to point A of the voltage multiplier and pointB is connected to ground, the output at point D will be positive. If, however, point Creceives the high-voltage ac and point D is connected to ground, point B will be negative.The multiplier can be built on a piece of perfboard, with square-pin connectors at pointsA, B, C, and D. Ideally, the multiplier assembly should be potted in RTV silicone rubber.This board can then be disconnected from the main circuit and turned around to changepolarity.Switching C5, the ESD model capacitor, between the output of the voltage quintupler andthe output is accomplished by K1, a vacuum relay. Vacuum relays are much better at generatingfast-rise-time waveforms than most other switches (e.g., firing thyratrons) and yieldmore reproducible waveforms than those of spark gaps. Vacuum relays can be expensive (afew hundred dollars), and it is better to search the inventory of electronic surplus stores such
176 ELECTROMAGNETIC COMPATIBILITY <strong>AND</strong> <strong>MEDICAL</strong> DEVICES12 VINJ7+ 12- C1 + 100uF C20.01uFIC131VINADJ2VOUTR1LM317/TO220240R25KC30.01uF+ C4100uFSW1VINTDK PCU-554OSCILLATORHVOUTOUT1OUT 2HVACHVGNDVoltage MultiplierCHVout5 4R4100R5100R6100K1>10KVDC SPDT VACUUMRELAYR730J5ESDPROBE(a)SW2ESD FIRER3750GNDOUT GND3C5150pF,15KV1 2D11N4007SP1+12V Piezo Buzzer-Alligator ClipC06J1 0.001uF, 2KVAD2D3C070.001uF, 2KVD4D5C080.001uF, 2KVD6D7C090.001uF, 2KVD8C100.001uF, 2KVD9D10C110.001uF, 2KVD11J3CJ2BRG53RG53C120.001uF, 2KVRG53RG53C130.001uF, 2KVRG53RG53C140.001uF, 2KVRG53RG53C150.001uF, 2KVRG53C160.001uF, 2KVRG53J4D(b)(b)HVACVM1HVACCHVGNDHVGN DHVoutVoltage Multiplier50M, 15kV ratingC5150pF, 15k V1N 40074123R4100R4100K1, >10kVDC, Vacuum RelayR4100R430ESD ProbeSW 2(c)+12VFigure 4.20 A simulator which produces waveforms that are closer to a professional unit compliant with IEC801-2 (1991) can be builtusing surplus high-voltage components. (a) A cold-cathode fluorescent lamp driver and a quintupler produce the high voltage to charge theESD model capacitor. A vacuum relay transfers the charge to the device under test via the ESD resistor network. (b) The quintupler shouldbe built as a stand-alone module, making it possible to reverse the ESD polarity. (c) If necessary, a SPST vacuum relay can replace the SPDTunit.as Surplus Sales of Nebraska and Fair Radio Sales for a suitable SPDT relay with at least a10-kV contact rating and a 12-V dc coil. If you cannot find a suitable SPDT relay, you canuse a 50-MΩ resistor (with at least a 15-kV rating) to charge the 150-pF capacitor constantly,and use a SPST vacuum relay to deliver the ESD to the ESD resistor network.Use carbon-composition (noninductive), high-voltage resistors for R4–R7 and build thehigh-voltage discharge path with the shortest possible lead lengths. This will ensure lowpath inductance and fast ESD pulse rise times. When pushbutton switch SW2 energizesK1, high voltage will be present at the ESD probe. A piezoelectric buzzer is used to warn
SUSCEPTIBILITY 177the user that the probe is potentially charged. To comply with the standard, the probe musthave specific dimensions. However, good results are obtained using a 3 -in. smooth roundedheadbolt as the probe tip for air discharge. For contact-discharge tests, use the pointed8edge of a 1 -in. steel nail.4During operation, the discharge return ground cable of the generator must be connectedto earth ground. The ground cable should be at least 2 m long and have insulation rated at12 kV or more. Dc power for the ESD gun can be obtained from a 12-V battery pack or a12-V dc adapter with a current rating of at least 400 mA. Finally, make a calibration dialto be placed around the shaft of potentiometer R2 by measuring the voltage across C5using a high-impedance high-voltage probe and a digital voltmeter.The standards call for a ground reference plane to be placed in the floor of the laboratory.The plane should be an aluminum or copper sheet no thinner than 0.25 mm, coveringan area no smaller than 1 m 2 , and projecting at least 0.5 m beyond all sides of the deviceunder test. This is the ground reference to which the ESD simulator should connect. Theplane must also be connected to the protective earth ground. The device under test shouldbe placed on a nonconductive test table 0.8 m high. All nonconductive construction (e.g.,all wood) is necessary because metal objects in the table construction would distort the RFfields radiated by the ESD event field. The table should be placed no closer than 1 m to thewalls of the laboratory or any other metallic object. A 1.6 m 0.8 m metallic sheet horizontalcoupling plane covered with a 0.5-mm insulating support is placed between thetabletop and the device under test. This coupling plane must be connected to the referenceground plane via two 470-kΩ resistors in series.Indirect Injection of ESD Fields Since ESD events generate large amounts of RFI, it isnot always necessary for the ESD event to happen between a charged body and the medicaldevice itself. A discharge between two bodies in the vicinity of the medical device maysuffice to cause a failure. For this reason, IEC-61000-4-2 specifies that testing shall also bedone by generating EMI fields through ESD between the ESD simulator and the isolatedhorizontal coupling plane, as well as between the ESD simulator and an isolated verticalcoupling plane. The vertical coupling plane is effectively an antenna of dimensions0.5 m 0.5 m that is placed on the horizontal coupling plane but is isolated from it. AnESD generator is then placed in the center of the vertical edge, and at least 10 impulses ofeither polarity are applied. The vertical coupling plane must also be connected to the referenceground plane via two 470-kΩ resistors in series.Susceptibility to Radiated Electromagnetic InterferenceIEC-61000-4-3 specifies a modulated RFI test of 3 V/m as representative of the radiatedelectromagnetic interference that may be caused on a medical device by wireless communicationequipment. For critical equipment such as life-support devices, 10 V/m is used fortesting. Currently, tests should be performed at frequencies of 26 MHz through 1 GHz with1 kHz at 80% amplitude modulation, but there is serious talk about extending the upper limitto 3 GHz. The frequency band is covered in steps of 1% of the fundamental frequency. Forfrequencies of 26 to 200 MHz, a biconical transmit antenna is commonly used. For frequenciesabove 200 MHz, a double-ridged horn transmit antenna is the popular choice.As shown in Figure 4.21, the testing is usually performed in a shielded enclosure withanechoic material placed throughout the enclosure to minimize reflections. The transmitantenna is typically located 3 m from the device under test. An isotropic field strengthmeter is placed inside the room at a location physically close to the device under test andused as a secondary indication of the field strength. Testing is performed utilizing linearlypolarized antennas, with the device under test exposed to both vertically and horizontallypolarized fields on each of four sides. In addition to the frequency sweep, the device under
178 ELECTROMAGNETIC COMPATIBILITY <strong>AND</strong> <strong>MEDICAL</strong> DEVICESSemi Anechoic ChamberEUTField DensityProbeNonconductiveSupport Table withTurntable (80 cm high)AntennaGeneratorAmplifierControllerFigure 4.21 Setup for assessing the susceptibility of a medical device to radiated emissions.Testing is performed in a shielded enclosure with anechoic material placed throughout the enclosureto minimize reflections. The transmit antenna is typically located 3 m from the device under test. Anisotropic field strength meter is placed inside the room to yield an indication of the field strength.test is also exposed to a 3-V/m field of 900 MHz modulated with a 200-Hz square waveand modulated with 50% duty cycle in both vertical and horizontal polarizations.Sometimes, additional test and monitoring equipment is needed to generate test signalsand to evaluate the performance of the device under test. Figure 4.22 shows the experimentalsetup used to test the RFI susceptibility of a prototype implantable-device programmer.The implantable device programmed by this device is meant to interact with the patient’sheart. Although the implantable device itself was not the subject of this specific test, it hadto be in communication with the programmer so that the performance of the programmercould be evaluated while being exposed to the 3-V/m RFI. In addition, since the programmerhas an ECG input, a patient simulator had to be connected to the programmer during thetests. The patient simulator as well as the implantable device were placed under an aluminumfoil shield. A shielded closed-circuit TV camera relayed the image from the programmer’scomputer screen to those who were monitoring the device outside the shielded room.Because of the amount of EMI generated, there is no easy legal way of conducting this testoutside a shielded room. As such, the common engineering practice is to apply good designpractice and then cross fingers when running the test at a qualified facility. Design-lab testing
SUSCEPTIBILITY 179Figure 4.22 A prototype implantable-device programmer is being tested to assess its susceptibility toradiated EMI. An implantable device and a simulator need to interact with the device under test to assessits behavior. These test accessories are placed under the aluminum foil shield. A TV camera relays theimage from the programmer’s computer screen to the control station outside the shielded room.will probably become more popular in the future. Since cellular telephones and handheldtransceivers can produce field strengths above 3 V/m, regulatory agencies are consideringincreasing the EMI field level to 10 V/m for all medical electronic equipment. Passing 10 V/mwill be a very difficult challenge for the designers of sensitive patient-connected devices!A beefed-up indirect-injection ESD test can serve as the basis for a test to give a roughindication of a device’s susceptibility to radiated EMI. This is the way in which the militarytest equipment hardened against electromagnetic pulses (EMP) generated either by nuclearexplosions. A cheap wideband EMI generator, albeit not nearly as powerful as that used to testfor EMP susceptibility, can be built using a high-voltage generator that charges a capacitor andreleases its energy into an antenna. The trick is to produce a very fast rise time (less than 1 ns,if possible) and a relatively long total duration (100 ns or more). One way of doing this isshown in Figure 4.23. The core of this wideband EMI generator is Blumlein’s pulse generator.The capacitances of two transmission lines are charged by a high-voltage power supplyvia a series charging resistor R charge . When charging, the transmission lines are effectively inparallel because inductor L bypass does not present any substantial impedance to low-frequencysignals. When a certain voltage is developed across the transmission line, the spark gap breaksdown, effectively shorting one end of transmission line 1. This causes a very fast pulse toappear across the wideband antenna. Blumlein generators are often used to power nitrogenlasers, ground-penetrating radar, and other instruments that require sharp, high-voltage pulses.A traveling-wave TEM horn antenna can be used to radiate the pulse generated by theBlumlein generator toward the device under test. A traveling-wave TEM horn consists ofa pair of triangular conductors forming a V structure in which a spherical TEM-like modewave propagates along the axis of the V. The schematic diagram for an experimental widebandgenerator circuit is shown in Figure 4.24. Here, a push-pull oscillator drives a TVflyback. The original primary of the flyback transformer is not used. Instead, new primariesare made by winding two sets of four turns each of insulated No.18 wire around theexposed core of the flyback transformer. Feedback for the oscillator is obtained through anadditional coil of four turns of No.24 wire wound around the core.
180 ELECTROMAGNETIC COMPATIBILITY <strong>AND</strong> <strong>MEDICAL</strong> DEVICESR chargeSpark GapHVSour ceTransmissionLine 1L BypassTransmissionLine 2Wideband AntennaFigure 4.23 A beefed-up indirect-injection ESD test can serve as the basis for wideband assessmentof a device’s susceptibility to radiated EMI. The transmission lines of a Blumlein pulse generatorare charged by a high-voltage power supply via R charge . When a certain voltage is developedacross the transmission line, the spark gap triggers, causing a very fast pulse to be delivered to awideband antenna.Applied at the input of the flyback driver, 12 V should produce 15 to 20 kV dc at theoutput of the flyback’s tripler. This high voltage is used to charge two transmission linecapacitors Z1 and Z2 which are etched on a double-sided 0.4-mm-thick copper-clad PCBas shown in Figure 4.25. The TEM horn antenna is formed from two truncated triangularpieces of single-sided PCB and edge-soldered to the Blumlein generator board. The sparkgap is simply a copper or bronze U shape with a bolt and nuts that permit the dischargegap width to be adjusted.Susceptibility to Conducted Electromagnetic InterferenceEMI susceptibility tests for medical devices conducted according to IEC-61000-4-6involve injecting RF voltages onto the power line and bulk RF currents into other signalcables. A current probe is clamped around the entire cable bundle, and radio-frequencyWarning! This is a dangerous device! It produces high voltages that can cause verypainful or lethal electrical shocks. In operation, the spark gap produces significant levelsof ultraviolet radiation, which must be shielded to prevent eye damage. In addition, sparkdischarges can ignite flammable or volatile atmospheres. Finally, the EMI levels generatedby this circuit are certainly above what the FCC likes to see dumped into the atmosphere.Thus, this generator should only be operated inside a properly shielded room.
SUSCEPTIBILITY 181+12VSW 1*= HeatsinkD11N4007SW SPST*Q12N305 5+ C11000uFprimary aR11Kprimary bT1TV Flyback with voltage multiplierIntegrated TriplerTEM HornWIDEB<strong>AND</strong> EMIfeedback+15KVL1R2110 Ohm 2WD11N4007*Q22N3055SG1SPARKGAPZ1Z2Blumlein Pulse GeneratorFigure 4.24 In this experimental wideband generator, a push-pull oscillator drives a TV flyback to produce 15 to 20 kV dc. This high voltageis used to charge two transmission line capacitors, Z1 and Z2, which are etched on a double-sided PCB.energy is injected. The frequency range for immunity tests is 150 kHz to 80 MHz, and theinjected RF has an amplitude of 3 V. Figure 4.26 shows a typical test setup. The deviceunder test is placed in the approximate center and 10 cm above a reference ground plane,and is powered and operated in a normal configuration. Injection of RF into the ac powerleads is performed with the coupling network shown in Figure 4.27. Testing of signal inputleads is performed via a current clamp on the leads.Susceptibility to Fast Power Line TransientsIEC-61000-4-4 deals with the immunity that devices must present against repetitive fasttransients that may be induced, for example, by inductive disconnects on the power line circuitfrom which the medical device is powered. Electrical fast transients (EFTs) are causedany time that gaseous discharge occurs (a spark in air or other gas), the most common beingthe opening of a switch through which current is flowing. As the switch is opened, arcingoccurs between the contacts: first at low voltage and high frequency while contacts are closetogether, and later at a higher voltage and lower frequency as the contacts separate.Figure 4.28 shows the experimental setup to test for susceptibility to EFT. The deviceunder test is placed in the approximate center of a reference ground plane and is poweredand operated under worst-case conditions. Throughout the test, the device under test isobserved for any indications of erratic operation. Transients are applied to the power leadsthrough the use of a coupling/decoupling network. In this network, 33-nF capacitors couplethe high-voltage pulses from the EFT burst generator between ground and the live andneutral lines of the device under test’s power input. The network also includes a filter toprevent the high-voltage pulses from coupling into the real power line.The device under test is subjected to 1-kV discharges to the ac power input leads. Eachpulse should reach 900 V by 5 ns 30% and should spend no more than 50 ns 30%above 500 V. The burst of pulses is delivered with a 5-kHz repetition rate. Both positiveand negative polarity discharges are applied. For each discharge sequence the duration is
182 ELECTROMAGNETIC COMPATIBILITY <strong>AND</strong> <strong>MEDICAL</strong> DEVICES+15kV+15kV5cmNylon SupportsSGSGZ1Z12.5cmL1TEM Horn15cmL1Z2Z215cm5cm30cmSIDE VIEW5cm30cmFRONT VIEWFigure 4.25 Construction details for the Blumlein generator. The TEM horn antenna is formed from two truncated triangular pieces of single-sidedPCB and edge-soldered to the Blumlein generator board. The spark gap is in a bronze U shape with a bolt that permits the dischargegap to be adjusted.5cm1 minute with a 1-minute pause between sequences. EFT is capable of inducing EMIwithin the device under test over a 60-MHz bandwidth.A capacitive coupling clamp is used to couple bursts onto signal, data, I/O, and telecommunicationslines. The coupling clamp is really a 1-m-long metallic plate that couples theEFT to signal lines without galvanic connection. This plate is suspended by insulatorblocks 10 cm over a reference ground plane. An EFT generator is a relatively complexpiece of equipment. However, for design-time testing, Guettler [1999] proposed a simpleline-disturbance simulator which generates inductive-disconnect transients through the useof a fluorescent-lamp ballast inductor and a modified glow-discharge starter. In the circuitshown in Figure 4.29, a fluorescent-lamp glow-discharge starter is modified by removingits noise-suppression capacitor. In operation, when SW2 is closed, the glow-dischargestarter SW3 switches on and off at random. The abrupt current variations through the
SUSCEPTIBILITY 183Ground PlaneControllerGeneratorAmplifierSignal Line(s)Signal Coupling Clamp10 cmPeripheralsEUTNonconductiveInsulator, 10cmFigure 4.26 Setup for assessing the susceptibility of a medical device to conducted emissions. Thetest involves injecting RF voltages onto the power line and bulk RF currents into other signal cables.A current probe is clamped around the entire cable bundle, and radio-frequency energy is injected.The frequency range for conducted immunity tests is 150 kHz to 80 MHz.Figure 4.27Coupling network used to inject RF into the ac power leads of the device under test.
184 ELECTROMAGNETIC COMPATIBILITY <strong>AND</strong> <strong>MEDICAL</strong> DEVICESControllerComputerEFT MainTest UnitPower InterfaceCableCoupling ClampLoad/PeripheralI/O CablesEUTFigure 4.28 Setup for assessing the susceptibility of a medical device to electrical fast transients(EFTs). This test simulates the power line transients that are caused by switching off an inductiveload.fluorescent lamp ballast L5 induce noise at the device under the test’s power line input. AnLRC network filters the transients so that they do not flow back into the real power line.Susceptibility to High-Energy Power Line TransientsIEC-61000-4-5 deals with large surges that may directly reach the device’s power linebecause of lightning. The surge pulses for this test are much wider than those used in EFTtesting. The pulses of IEC-61000-4-5 are tens of microseconds wide, making them able toinduce EMI within the device under test over a 300-kHz bandwidth. Figure 4.30 presentsa typical setup for testing a medical device’s susceptibility to high-energy power linesurges. The device under test is placed in the approximate center of a reference groundplane and is powered and operated in a normal configuration. Throughout the test, thedevice under test is observed for indications that a failure has occurred. Transients areapplied to the ac power line leads as well as to I/O lines through coupling/decoupling networks.The surge is applied in the common mode (line to ground) at 2 kV. The surge is thenapplied in the differential mode (line to line) at 1 kV. A series of six positive and six negativesurges are applied with a 1-minute interval between surges.The impulse generator for these tests uses a 20-µF capacitor charged to the test voltage,which is discharged through a switch into the device under test via a series coupling capacitorand a 40-Ω resistor. In addition, a 50-Ω resistor placed just after the switch is used forshaping the test pulse. For line-to-ground testing, the coupling capacitor has a value of18 µF. For line-to-line testing the capacitor is 9 µF with a 10-Ω resistor added in series. Justas with the coupling/decoupling networks for EFT testing, a filter is placed in series withthe real power line to avoid transients from entering it.
J2To D evi ceUnd er Te stAC Power PlugMetal BoxHot (Black)CB 11 2S1L150uHL3R3J1CIRCUIT BREAKERSW SPSTDS1LAMP NEONC1R1474700pFBEAD FERRITE0.47SW 2SW SPSTL5FluorescentlampballastC2SW3AC Power PlugR247Modifiedglow-dischargestarterL4R4Neutral (White)L250uHBEAD FERRITE0.47Protective EarthFigure 4.29 This simple line-disturbance simulator generates inductive-disconnect transients like those of the EFT test through the use ofa fluorescent-lamp ballast inductor and a modified glow-discharge starter.185
186 ELECTROMAGNETIC COMPATIBILITY <strong>AND</strong> <strong>MEDICAL</strong> DEVICESControllerComputerSurge MainTest UnitCM - I/O CD(I/O Signal LineCoupler/Decoupler)PowerCordEUTI/O LineFigure 4.30 Setup for assessing the susceptibility of a medical device to high-energy power linesurges. Transients are applied to the ac power line leads as well as to I/O lines through the use ofcoupling–decoupling networks. This tests simulates the transient variations in power line voltage thatmay be induced by a lightning strike.High-energy power line transients are not easy to generate without a pulse generator suchas the one described by the standard. Because of the voltages and energies involved, we recommendusing a commercial unit. However, if you decide to build your own, follow the componentvalues suggested by IEC-61000-4-5, use conservative ratings, and above all, keep itsafe.Susceptibility to Voltage Dips, Short Interruptions, and Voltage VariationsIEC-61000-4-11 covers power line voltage dips and interruptions. The voltage variationsand their duration are as follows:• 30% Reduction for 10 ms• 60% Reduction for 100 ms• 95% Reduction for 5000 ms• 10% Voltage variationFor this test, the performance of the device under test is assessed for each combinationof test level and duration selected with a sequence of three dips/interruption with intervalsof 10 seconds minimum between each test event. Each representative mode of operationof the device under test should be assessed. For each voltage variation, a different pass/failcriterion may be used. However, the equipment must exhibit safe conditions followinglong outages.The implication of this test to designers is the need to provide energy reserves in theequipment power supply to maintain operation through brief dips and outages, at least forcritical functions. Designers must also ensure that a device cannot power-up in an unsafe
SUSCEPTIBILITY 187mode after a prolonged power outage. A simple way of simulating these conditions duringthe design phase is to use a variac. Although timing an exact 10 ms for a dip is not an easymanual task, good approximations for these dips and interruptions can be achieved, especiallywhen the variac’s output is monitored with an oscilloscope. Remember, however,that power line voltages are present, and an oscilloscope with grounded input channelsshould not be used without appropriate isolation. As shown in Figure 4.31, a small filamenttransformer (e.g., 110 V ac/6.3 V ac at 100 mA) provides appropriate isolation for monitoringthe variac’s output with a grounded oscilloscope.Susceptibility to Magnetic FieldsIEC-61000-4-8 deals with interference that may be caused on a device by low-frequencymagnetic fields, such as those generated by the power lines. These magnetic fields can producejitter on CRT displays, distortion in amplified signals equipment, or false readings inequipment magnetic or electromagnetic field sensors. As shown in Figure 4.32, the deviceunder test is placed in the approximate center of a referenced ground plane at a height of10 cm and is powered and operated in a normal configuration. The magnetic field isincreased to 10 A/m (approximately 125 mG) and is applied to three axes of the deviceunder test. The field is maintained for a period of approximately 5 minutes for each ofthree axes, while the device under test is monitored for any indication of erratic operation.As shown in Figure 4.33, a test system for design-time evaluation is easy to build. Usefour pieces of 92-cm-long 3 -in. PVC pipe, four 4 3 -in. PVC pipe elbows, and one 4 3 -in. PVC4pipe tee to construct the 1 m 1 m frame for the current loop. Thread No. 18 insulated copperthrough the loop to form two complete turns. Solder a flexible twisted-pair cable to theloop wires where they exit the pipe. R1 will be used to monitor the RMS current flowingthrough the coil. The coil is powered by a transformer rated at 24 V at 10 A, which is inturn powered from the power line through a variac.J1T1VariacJ2To DeviceUnder TestAC Power Plug MaleAC Power Plug Female110VT21 56.3V4 8J3BNC1ToOscilloscope2Figure 4.31 A simple way of simulating power line voltage dips and interruptions is to use a variac. Although timing an exact 10 ms for adip is not an easy manual task, good approximations for these dips and interruptions can be achieved when the variac’s output is monitoredwith an oscilloscope. A small filament transformer provides appropriate isolation for connection with a grounded oscilloscope.
188 ELECTROMAGNETIC COMPATIBILITY <strong>AND</strong> <strong>MEDICAL</strong> DEVICESMultimeterEUTLoop AntennaAC Power SupplyGroundPlaneFigure 4.32 Setup for assessing the susceptibility of a medical device to magnetic fields. The magnetic field applied to three axes of thedevice under test is 10 A/m. This test simulates interference that may be caused on a device by low-frequency magnetic fields, such as thosegenerated by the power lines.1 meterL1PVC ElbowJ1T1VariacAC Power Plug1T25110VAC 24V,10A To RMS4 8 DVM1J2#18 solidBN C insulated2 R1 wire1 Ohm, 20WPVC "T"3/4" PVC Pipe1 meterReferenceGroundPlaneFigure 4.33 A magnetic-field induction generator can be built from a coil of wire inside some PVC pipe. This assembly is driven by avariac–transformer combination to produce the desired magnetic field at the center of the coil.
GOOD <strong>DESIGN</strong> PRACTICES, REMEDIES, <strong>AND</strong> DUCT TAPE 189To use the test system, increase the variac’s output until you read 5.55 V RMS across R1.At this point, 4.5 A should be circulating through the two loops of L1. Correcting for thedifference in magnetic field produced by a square loop versus that of a circular loop, andapplying the Biot–Savart law, the magnetic field at the center of the loop should be(4.5 A 2)/0.9 m 10 A/m.GOOD <strong>DESIGN</strong> PRACTICES, REMEDIES, <strong>AND</strong> DUCT TAPENo cure for EMC problems is better than prevention. Trouble avoidance in EMC is accomplishedby considering the emissions and susceptibility aspects of EMC at every stage ofthe design process. The following important questions must be part of the circuit design,selection of components, and packaging:• Will this part of the design generate or be susceptible to interference?• What are the characteristics of the interference?• At what frequency or frequencies does it occur?• From where is it most likely to originate?• Which radiated and/or conducted path(s) can the interference take from source tovictim?Once potential sources of interference are identified, you must decide what to do toreduce their impact. There are four broad solutions to an individual EMC problem:1. Prevention. Eliminate the sources of potential interference.2. Reflection. Keep internally generated signals inside the device and keep externalinterference outside the device’s enclosure.3. Absorption. Use filter networks and filtering materials to absorb interfering signals.4. Conduction. Divert interfering signals to the device’s RF ground.Fortunately, most of the rules and perils are known in the war against EMI. Designingan instrument to pass EMC testing is, in all likelihood, all that will be needed to ensureproper performance under real-world situations. Avoid overdesign. The authors are notaware of a single medical device malfunction attributed to interference by unknown UFOradiation. All you need to do is figure out the potential level of interference that you mayencounter, and design within these limits.Kendall [1998] proposed a simple way of estimating the amount of protection that maybe needed in a medical device to counteract an EMI threat. His step-by-step proceduredemonstrates how to estimate the protection that needs to be incorporated in the design ofan analog comparator with 5-mV sensitivity.1. Start by identifying the RF threat level. For example, if the applicable standard foryour device establishes immunity against radiated interference at 3 V/m, use thislevel for your calculations.2. Multiply the threat level by the field uniformity of the test chamber in which thedevice will be exposed to EMI. A factor of 2 is appropriate for ferrite-lined chambers,while a factor of 4 is typically used for semianechoic chambers. Assuming a ferritelinedchamber, the uniform field will be 2 3(V/m) 6(V/m) 136(dBµV/m).3. Account for losses between the source and the victim. A minimum theoretical lossof 14 dB would happen in the case in which the source and the victim are both
190 ELECTROMAGNETIC COMPATIBILITY <strong>AND</strong> <strong>MEDICAL</strong> DEVICESconnected to perfectly tuned dipole antennas. However, more severe losses can beassumed for less perfect situations, such as when the length of the signal line underconsideration is much shorter than one-fourth wavelength of the offending spectralcomponent for which the threat analysis is conducted. Assume for this example thatthe line of interest presents an impedance of 100 Ω at the frequency of interest andthat the coupling between the offending source and the signal line under analysis is10 dB below ideal.4. Calculate the coefficient to be used for the offending signal at the victim circuit. Inthe example 136(dB) 14(dB) 10(dB) yields 112 dBµV across the signal line’sload impedance of 100 Ω.5. Convert this level back to linear units: 112 dBµV 400 mV. This will be the voltageinduced by the offending source at the frequency of interest on the signal line underanalysis. Note that if the load impedance increases, so will the induced voltage. Forexample, for a 100-kΩ load, the induced voltage will be as high as 2 V.6. Compare the induced voltage levels against typical circuit threshold values at all susceptiblefrequencies. For example, if 26 MHz is within the bandwidth of the processingcircuit connected to the line under analysis, and since the threshold value forthis example was chosen to be 5 mV, the protection level required for a load impedanceof 100 Ω would be 20 log(400 mV/5 mV) 38 dB. For a 100-kΩ load impedance,the protection need would increase to 52 dB.With this approximation in hand, it is possible to select shielding, grounding, and filteringcomponents that will afford a combined protection that surpasses the estimate by a certainsafety margin.Shields Up!Shielding and grounding (reflection and conduction) are the primary methods of guardingagainst EMI entry and exit to and from a circuit. Chances are that you will not build yourown enclosure. Rather, you will probably use an off-the-shelf case or hire an enclosuremanufacturer to supply you with custom-made enclosures. In either case, look at the enclosure’sdata sheets for EMC specifications. The authors’ preference is to use enclosureswhich have a conductive cage that is contained completely inside a plastic enclosure withoutany exposed metallic parts.If a conductive enclosure is chosen, ensure that the conductive surface is as electricallycontinuous as possible. For a split enclosure, ensure as good an electrical contact as possiblebetween the parts. Openings in the case that are required for display windows, coolingslots, and so on, must be kept as small as possible. If the size of the opening is largerthan 1 of a potential offending EMI component, use transparent grilles to close the RF gap.20Finally, ensure that unshielded lines that carry offending signals do not pass directlythrough a shielded enclosure. Use shielded cables for high-sensitivity inputs.EMI grounding requires different, sometimes conflicting considerations from thoseused to protect low-frequency low-level signal lines. The first difference is the issue of single-pointversus distributed grounding. Single-point grounding of circuits is a commonpractice in the design of low-noise electronic circuits because it eliminates ground loops.This assumption is valid only up to a few megahertz. At higher frequencies in the radiospectrum, line inductances and parasitic capacitances become significant elements, voidingthe effectiveness of single-point grounding. For example, for the 300-MHz components ofan ESD event, a 0.25-cm length of wire or PCB track acts as a one-fourth wavelengthantenna, providing maximum voltage at the ungrounded end. As such, any cable that islonger than 1 to 10 1 of offending spectral components should be grounded at both ends. If20
GOOD <strong>DESIGN</strong> PRACTICES, REMEDIES, <strong>AND</strong> DUCT TAPE 191this poses a ground-loop problem for low-frequency signals, one end can be coupled toground through a 0.01-µF capacitor.Whenever possible, the shield of external cables should be properly terminated to theequipment enclosure. Poor termination, which may be imposed by leakage current and isolationrequirements, may result in capacitive coupling of EMI to signal lines. So, by allmeans, and as long as isolation and leakage requirements permit, bond the cable shielddirectly to the device’s conductive enclosure. Contrary to the suggestions above, when thepotential problem is ESD, the effective solution is not to shield with a conductive layerbut rather, to insulate. By not allowing an ESD spark to occur at all, there are no bursts ofelectric and magnetic fields to radiate EMI.For this purpose, plastic enclosures, plastic knobs and switch caps, membrane keyboards,plastic display windows, and molded lampholders help eliminate ESD discharge points. Asa rule of thumb, a 1-mm thickness of PVC, ABS, polyester, or polycarbonate suffices to protectfrom 8-kV ESD events. The area protected by a nonconductive cover is more difficult toassess because surface contamination by fingerprints and dust attract moisture from the airto form a somewhat conductivity paths through which ESD can creep. During 8-kV testing,an ESD gun can produce sparks that follow random paths over a supposedly nonconductivesurface all the way to a metallic part 5 cm away. The same happens on metallic surfacespainted with nonconductive paint, where surface sparks seek pinhole defects on the paint.A very common design mistake is to assume that 15-kV-rated insulation on LCD displays,membrane keypads, potentiometers, and switches is sufficient to protect circuitryconnected to these components. The problem is that although ESD won’t go through theinsulation, it will creep to the edges of the insulation and hit wiring on the edges of thesecomponents. As such, extend the dielectric protection of panel-mounted controls to preventor at least divert ESD currents from reaching vulnerable internal circuits.The Real Bandwidth of Signal LinesProtecting medical devices from EMI is especially difficult because it often involvessensitive electronics that can pick up and demodulate RFI. Interfering signals can berecognized as real features of physiological signals, leading to potentially serious risksto patients and health-care providers. Take, for example, the polling of a cellular phone,which happens at a frequency close to that of the heart’s normal rhythm. If detected andinterpreted incorrectly, a pacemaker could assume that the EMI bursts are really the heartbeating at an appropriate rhythm, causing it to inhibit the delivery of pacing therapy.A common mistake in the design of medical instrumentation, especially of biopotentialamplification and processing stages is to assume that the RF bandwidth of the circuit islimited to the intended operational bandwidth. The limited bandwidth of an op-amp or ofa low-pass filter intended to limit the bandwidth of biopotential signals will do little toprohibit pickup and demodulation of RF signals. If not controlled, RFI can easily inducevolt-level RF currents in biopotential amplifiers designed to detect micro- or millivolt-levelsignals. These RF currents will surely find nonlinear paths (e.g., zener protection diodesand parasitic diodes) that demodulate them, yielding high-level in-band signals that obscure,if not completely swamp, real biopotentials.Besides using proper shielding, one effective solution is to place RF filters on every lineconnected to the outside world, especially those that convey low-level signals from patientsensors and electrodes to high-input-impedance analog circuits. Figure 4.34 shows theinput filters placed in immediate proximity of the signal-input connector of an amplifierused to record intracardiac electrograms. In this circuit, individual NFM51R00P106 single-linechip filters made by muRata are used to shunt RF signals to the isolated ground planewithout affecting low-frequency signals. These filters have a nominal 3-dB cutofffrequency of 10 MHz, yielding a minimum attenuation of 5 dB at 20 MHz, 25 dB at
192 ELECTROMAGNETIC COMPATIBILITY <strong>AND</strong> <strong>MEDICAL</strong> DEVICESTo biopotentional amplifier+-D1BZD227C10D2BZD227C10C114700pF J1 J2 12ISOC24700pFIS<strong>OF</strong>ILT1NFM51R00P1061 3FILT2NFM51R00P1061 32ISOISO2 32 3+ From-intracardiacelectrodesRefRefD3BZD227C10FILT3NFM51R00P1061 3C34700pFISO2IS<strong>OF</strong>igure 4.34 RF filters are often needed on every line connected to the outside world. In this intracardiac electrogram signal input circuit,individual single-line chip filters are used to shunt RF signals to the isolated ground plane without affecting low-frequency signals. Thesefilters have a nominal 3-dB cutoff frequency of 10 MHz, yielding a minimum attenuation of 5 dB at 20 MHz, 25 dB at 100 MHz, and 30 dBabove 500 MHz. 4700-pF capacitors shunt RF signals that may be induced by electrosurgery. Zener diodes with their cathodes connected toa common point to limit surge voltages that may be caused by defibrillation.100 MHz, and 30 dB above 500 MHz. The 4700 pF following these filters is used to shuntRF signals that may be induced by electrosurgery tools. The value of 4700 pF was selectedfor this design to reduce the possibility that electrosurgery currents circulating through theelectrodes in contact with the heart would reach a level capable of ablating myocardial tissue.Finally, zener diodes with their cathodes connected to a common point are used tolimit the voltage imposed on the inputs of the amplifier by high-voltage transients such asdefibrillation.It is a good idea to filter every line connected to the outside world, even those that carryhigh-level signals over low-impedance paths (e.g., high-level analog or digital outputs)because if left unfiltered, that line can act as an antenna picking up EMI from outside thedevice and reradiating it within the device’s enclosure. One of the most sensitive and oftendisregarded lines in a medical device is the reset line. This is because EMI or ESD couplinginto a reset line can cause a reset, often leading to temporary interruption of service,which may leave a patient without the support of a life-sustaining therapy until function isrestored. For this reason, reset lines and components that can evoke reset events (e.g., resetswitches, microprocessor watchdogs, and power supply supervisors) must be thoroughlyshielded and decoupled.
GOOD <strong>DESIGN</strong> PRACTICES, REMEDIES, <strong>AND</strong> DUCT TAPE 193Although designers usually protect power supplies from the high-voltage transients thatmay be encountered under the conditions simulated by EFT and high-energy surges, theEMI component of these events is often forgotten. High-voltage surges may bypass thepower supply and associated filters completely and attack the device’s circuitry directly.The same filtering recommendations apply then to protecting sensitive analog and digitalcircuits against the EMI produced by power line surges.Paying Attention to PCB LayoutAlthough in earlier sections we advocated maintaining clock speeds low, as well as rise andfall times as slow as possible, some medical device applications really demand lightningfastprocessing. Let’s digress and imagine what it would be like to own a Ferrari F40, capableof achieving a speed of 200 mph!—its magnificent turbo-charged V-12 engine purringwhile cruising down the road at a speed at the limit of human reflexes. Waking up to reality,though, you would seldom (if ever) be able to floor the gas pedal of this marvel. Evenif disregarding the legal limit, our roads are just not designed to support much more thanhalf the maximum speed of a loaded sports car. The awesome power of sports engines canbe let loose only in special race tracks, constructed with the right materials and slants.Although you may not consider adding a Ferrari to your estate at this moment, its powerdoes relate to the topic of this chapter, as you are probably using increasingly fast logicand microprocessors in your projects. However, in close resemblance to the sports caranalogy, very high bus speeds result in interconnection delays within the same order ofmagnitude as on-chip gate delays, and for this reason typical PCB design, which considerstraces as low-frequency conductors rather than as high-frequency transmission lines,will ensure that such a project turns into a very impressive and expensive paperweight.Some 20 years ago, while some of us were building microcomputers with 2-MHz Z80s,8080s, and CDP1802s, engineers designing with ECL technology already faced problemsrelated to the implementation of printed circuit boards, backplanes, and wiring for highspeedlogic circuits. Today, however, multihundred megahertz and even gigahertz buses arecommonplace, and we face strict regulations on the RF emissions escaping from suchwideband sources. For this reason, we should all acknowledge that the utopian idea thatdigital signals behave as ones and zeros must be replaced by a more realistic approach thatinvolves RF transmission line theory. Through this new approach, printed circuits aredesigned to convey pulse transmissions with minimal distortion through channels of appropriatebandwidth—no quasi-dc signals anymore! Interestingly, the same PCB layout practicesthat are useful in the design of high-speed circuitry apply to the design of circuitrywith increased immunity against EMI.Transmission Line Model of PCB TrackPCB design for high-speed logic and RFI immunity demands the use of power and groundplanes, and plain double-sided PCBs are not recommended. In the former, a surfacestripline track such as that depicted in Figure 4.35 will have an impedance Z t given by87 5.98hZ t lnε 1.41 0. 8wwhere ε is the dielectric constant of the PCB dielectric, h the height of the track above theground or power plane, and w t and t t the width and thickness of the track, respectively. APCB track buried within the fiberglass–epoxy laminate will have its impedance reduced byabout 20% compared with that of a surface track.This PCB track can be modeled as a transmission line [Magid, 1972], and a short pulseapplied to one end of this transmission line will appear on the other side, supplying thett t
194 ELECTROMAGNETIC COMPATIBILITY <strong>AND</strong> <strong>MEDICAL</strong> DEVICESLayer 1 {t tW tSurface TrackLayer 2 {Layer 3 {buriedtrackhPCBdielectricGroundPlaneLayer 4 {Layer 5 {V cc PlaneLayer 6 {Figure 4.35 The transmission line impedance of a stripline PCB track is affected by its position relative to the ground or power plane aswell as by its geometry and by the dielectric constants of the board and the surrounding medium.load impedance Z l with a distorted version of the pulse, and presenting an effective delayτ. On a typical surface PCB track, the pulse conduction velocity is approximately0.15 ns/in. 0.06 ns/cm, so τ 0.15l t (ns) represents the total delay caused by a track oflength l t (measured in inches).If the load impedance does not match the track’s impedance perfectly, a part of thearriving signal will be reflected back into the transmission line. In general, pulse reflectionoccurs whenever transmission lines with different impedances are interconnected or whena discontinuity occurs in a single transmission line. For a connection between two transmissionlines of impedances Z 0 and Z 1 , the reflected voltage V r is related to the incidentvoltage V i throughV r Z 1Z0 VZ Z i1The ratio Γ V r /V i , called the reflection coefficient, describes what portion of the pulseincident from Z 0 on Z 1 will be reflected back into Z 0 . Γ, V i , and V r are usually complexquantities because they deal with both the magnitude and phase of the signals that travelalong transmission lines.Using tracks buried within the PCB between the power and ground planes is aneffective way of controlling RFI and ESD threats. In contrast with one- or two-sidedPCBs, multilayered PCBs with ground and power planes keep ground impedances andloop lengths sufficiently low to avoid circuit tracks from picking up significant levels ofRFI. Typically, PCBs with signal tracks sandwiched between ground and power planesare a full order of magnitude less sensitive to RFI than are well-designed two-sidedboards.For nonmedical equipment, the power and ground planes are usually grounded to thechassis. In medical equipment, however, it is usually the most sensitive circuits that needto float, making it impossible to apply classical EMC techniques for proper signal-pathdecoupling and shielding. For floating circuits that end up being sensitive to EMI, try toform a capacitive grounding path between the power and ground planes of the PCB and0
GOOD <strong>DESIGN</strong> PRACTICES, REMEDIES, <strong>AND</strong> DUCT TAPE 195the chassis. Of course, the level of coupling must fall well within the amount of enclosureleakage permitted for the floating part.Pulse Reflection and Termination TechniquesIn a typical circuit, a driving logic element and a receiving logic element are connected bya PCB track. In the equivalent circuit shown in Figure 4.36, a pulse with amplitude V d isinjected by the driver logic element, which presents an output impedance Z d into a PCBtrack of length l t and impedance Z t . The pulse carried by the PCB track is then presentedto the input impedance Z r of the receiving element. If we suppose that a Z t 100 Ω trackcarries the pulse, and after looking at the data sheets for a selected 5-V family of highspeedlogic, we find that the output and input impedances at our frequency of interest areZ d 50 Ω and Z r 10 kΩ, respectively, then upon reaching the receiver, a reflected pulsestarts traveling back toward the driver with amplitude that can be approximated byV r Z r Zt VZr Z d 1 0,000 100 (5 V) 4.9 Vt 10,000 100which assumes a negligible attenuation of the pulse throughout its conduction, and whichtakes into consideration only the real parts of the variables. This reflected pulse will berereflected back toward the receiver upon hitting the driver with an amplitude approximatedbyZd Zt50 100V r V Z Z r (4.9 V) 1.63 V5 0 100dtThis negative signal will interact with the original incident pulse with a delay equivalentto the time it takes for the pulse to travel back and forth along the track τ(ns) 0.31t r.Depending on the length of the PCB track, the 1.63-V reflection could distort theleading edge of the pulse so much that it will cause the false detection of a logic-low(Figure 4.37). A different combination of impedances could have caused the reflected pulseV dZdI tPCB TrackZrZ tDriverGND PlaneReceiverFigure 4.36 The output of a logic element connected through a PCB track to the input of anotherlogic element can be modeled as an ideal voltage step generator that drives a transmission line ofimpedance Z t through an output impedance Z d . The transmission line is then terminated by thereceiver’s input impedance Z r .
196 ELECTROMAGNETIC COMPATIBILITY <strong>AND</strong> <strong>MEDICAL</strong> DEVICESV receiverIdeal Leading-Edge5VV HIMINV LO MAXReceived Step + Re-reflection0“1”Received Data:Time“0”Figure 4.37 A critical length of PCB track could cause the rereflected pulse to distort the leadingedge of the pulse so much that it will cause, in this case, the false detection of a logic-low.to be positive, possibly causing the false detection of a logic-high, or the false activationof an edge-sensitive device. Moreover, a reflected pulse presented to the receiver will causeyet another reflected pulse, which although with far less amplitude, may still be able tocause erroneous operation of a circuit.Obviously, the solution to the reflected-pulse problem is to match the impedances inthe best possible way. This design procedure, called transmission line termination, canbe accomplished in four different ways: series, parallel, Thévenin, and ac, as shown inFigure 4.38. Series termination is recommended whenever Z d Z t and the line is drivinga reduced number of receivers. This technique, which gives good results in most highspeedTTL circuits, consumes negligible power and requires the addition of only oneresistor, the value of which is given byR term Z t Z dThe major drawback of the series termination technique as far as logic signal integrity goesis that it increases signal rise and fall times. However, the same is a blessing as far asreducing electromagnetic emissions.In contrast to series termination, which eliminates pulse reflection at the driver end, allother techniques eliminate reflection at the receiver end of the PCB track. Parallel terminationR term Z t as well as Thévenin termination R term 2Z t techniques consume largeamounts of power; however, they provide very clean signals. Ac termination R term Z t ,which uses a small capacitor to couple only ac components to ground, is not as power hungryas the preceding methods but adds capacitive load to the driver and increases the timedelay due to its inherent RC constant.Parallel Path Skew and Track Length EqualizationParallel transmission over data and address buses requires that all signals arrive at theirdestination concurrently. Often, however, pulses sent down parallel paths do not arrive atthe same time because of differences in the length of these paths. As shown in Figure 4.39,
GOOD <strong>DESIGN</strong> PRACTICES, REMEDIES, <strong>AND</strong> DUCT TAPE 197(a)Receivers(b)ReceiversDriverRtermZtDriverZ tR term(c)ReceiversVcc(d)ReceiversDriverZ tRtermDriverZ tR termR termFigure 4.38termination.Transmission line termination techniques: (a) series termination; (b) parallel termination; (c) Thévenin termination; (d) acDriver OutputReceived DataParallelData Busabca= < cbSkewed StreamErrorFigure 4.39Unequal lengths of PCB track on a parallel bus will cause skew between the pulse streams, leading to reception errors.the skew induced in bit sequences sent along parallel paths of different lengths can causeerrors in the communication between circuits, especially when transmitter and receiver circuitsare placed in different boards interconnected through backplanes or ribbon cables.The obvious solution is to keep parallel paths as short as possible and ensure equal PCBtrack lengths for all parallel paths.Skew also deserves very serious consideration in the design of high-speed microprocessorclock distribution networks. In general, all logic computation during a singleclock cycle has to be performed within the very short time left over by the delays suffered
198 ELECTROMAGNETIC COMPATIBILITY <strong>AND</strong> <strong>MEDICAL</strong> DEVICESby logic signals during that clock period: path delays, setup and latchup times, logic gatepropagation delays, and skew. As clock frequencies increase, the time left over for logicalcomputation decreases, up to the point that skew often causes system failures due toincomplete processing during a clock cycle.For this reason, PCB tracks that distribute the clock must be tuned so that the delayfrom the clock driver to each load is the same. Whenever possible, the loading on eachtrack carrying the clock should be the same, and in this case skew is minimized by makingall tracks the same length. For unbalanced loads, delay times can be tuned through RCterminations or by careful adjustment of the track lengths.Crosstalk and Vulnerable PathsCrosstalk is the noise induced into a track by the presence of a pulse stream in an adjacenttrack. In essence, crosstalk is EMI caused by the product on itself. The amount of crosstalkis affected by track spacing, routing, signal direction, and grounding. The major problemwith crosstalk arises when the voltages induced on a quiet line are sufficient to be detectedas a change in logic state by the receivers of that line. In high-speed systems, the capacitiveand inductive coupling between lines is considerable, and crosstalk must be reducedthrough appropriate design.First, proper transmission line termination reduces the amount of radiated energy from adriven track, and spurious emissions that nevertheless escape can be shielded through theuse of grounded guards. This design consideration is particularly important for lines drivenwith high-voltage, high-current, and high-frequency signals. Floating lines connected to highimpedancereceivers are notably sensitive to crosstalk, and proper shielding, as well as maintainingthem at a distance from possible radiating tracks, must be ensured. In addition, it ispossible to see from transmission line theory that crosstalk between two adjacent tracks isminimized if the two signals flow in the same direction.The analysis should be extended to identifying potential coupling paths between signallines and RFI sources (including ESD) and then taking steps to minimize them throughproper placement of PCB tracks and components. For example, shields can be reinforcedwhere transformers and heat sinks are placed, the areas of loops formed by PCB tracksshould be minimized, and magnetic coupling paths should be oriented orthogonally.Finally, remember that components, connectors, and mounting parts that can beaccessed from the outer world are very often the paths of entry into a device’s circuit forEMI and especially for ESD. Even an exposed metallic screw on an otherwise insulatingpanel can make it possible for unwanted signals to get into the circuit and cause interference.Common panel-mounted vulnerable parts include membrane keyboards, LEDs, potentiometers,connectors, and switches, together with their mounting hardware.Analysis of Circuit Board PerformanceAlthough you may consider such tools as a time-domain reflectometer or an RF network analyzeras belonging strictly to a communications lab, these can aid considerably in the designof circuit boards for high-speed and high-immunity applications. These tools are capable ofmeasuring the actual impedances, time delays, and complex reflection coefficients of a circuit.These measurements often show that calculations of these parameters result in verycrude estimates that have to be improved on for good circuit performance. In most cases, theiterative process of design will require building and evaluating a test board to determine ifthe original design considerations were effective. This test board is usually not populatedwith the actual active components, but the PCB tracks, passive components, sockets, andconnectors, as well as the terminated dummy IC packages, form a network of transmissionlines that can be analyzed with confidence.
GOOD <strong>DESIGN</strong> PRACTICES, REMEDIES, <strong>AND</strong> DUCT TAPE 199The time-domain reflectometer (TDR) [Strassberg, 1993] of Figure 4.40, which is oftenused in the troubleshooting of LANs, injects a very sharp pulse V i into the transmission lineunder analysis. Then an oscilloscope or a computer fitted with a high-speed A/D receivesthe reflected pulses. The time delay and shape of the reflected pulses contain the informationrequired to estimate the impedance of the line and its termination (Figure 4.37).In contrast to TDR, network analyzers such as that in Figure 4.41 operate in the frequencydomain and enable exact measurement of the complex reflection coefficient as afunction of frequency, measurement of crosstalk between lines, and measurement of phaseskew between signals [Montgomery, 1982]. A network analyzer can also be used to identifytracks on which resonance problems could arise and to perform objective crosstalkmeasurements.Digital Storage OscilloscopePCB TrackV iZ tZ rTime-Domain ReflectometerFigure 4.40 In a time-domain reflectometer, a voltage step with very short rise time is injected intoa transmission line. After a certain delay, a reflected pulse adds up to the step. The timing and waveshapeof the reflected pulse contain information regarding the characteristics of the transmission lineand of the termination.ComputerFrequencyControlTrackingReceiverViVrZ t'Zt"V tRampDirectionalCouplersVCOZR' ZR"DirectionalCouplerNetwork Under TestSweep GeneratorFrequency-Domain Network AnalyzerFigure 4.41 In a frequency-domain RF network analyzer, a sweeping sinusoidal signal is injected into the input of the transmission lineleading to the subnetwork under test. Directional couplers feed a synchronized RF receiver with samples of the incident, reflected, and transmittedportions of the signal. A computer is used to calculate and display the complex reflection and transmission functions, as well as otherrelevant parameters.
200 ELECTROMAGNETIC COMPATIBILITY <strong>AND</strong> <strong>MEDICAL</strong> DEVICESIn fact, ignoring capacitor and inductor resonance is the most common mistake indesigning circuits with good EMI/EMC characteristics. Parasitic inductance and capacitancecause components and PCB tracks to resonate, often at frequencies as low as 1 to30 MHz. For example, many 10-nF decoupling capacitors with 1 -in. leads resonate at2around 20 MHz. Above the resonant point, capacitors act as inductors and inductors act ascapacitors, which typically render filters useless against high frequencies.Regardless of the usefulness of these RF test tools, their price puts them out of reachfor most electronics hobbyists and small engineering firms. But don’t be discouraged:Building successful high-immunity and high-speed circuits on a budget is possible byadopting conservative design policies. As you may realize by now, an analog circuit simulatorcould be as helpful as a digital circuit simulator in the design of your next circuit.For critical circuits, do not assume ideal capacitors and inductors, but rather, consider theRF characteristics of these components in your analysis.If possible, use ceramic surface-mounted capacitors and short, fat PCB tracks to keepinductance low. As far as inductors are concerned, ferrites perform better than wire-woundtypes. This is because ferrites have high resonant frequencies and absorb large amountsof energy at resonance. If wire-wound inductors are nevertheless required, place smallferrites in series with the inductor (e.g., mount small ferrite beads on the inductor’s leads)to protect the circuit over a wider bandwidth. Of course, make sure that the magnetic fluxcreated by currents flowing through wire-wound inductors does not couple to adjacentcomponents and PCB traces.Duct Tape and Test-Time BandagesDespite thorough engineering, surprises do happen during compliance testing. Inevitably,while you are still giving the last touches to your design, the marketing department hasalready sold a few dozen units to their most prestigious customers and eagerly awaits gettingtheir hands on the very prototype you are testing for the next trade show. “This is notgood,” you think. Next comes the calculation of how long you can live on your credit cardsbefore finding another job in a distant corner of the world where no one would have heardabout your mistake.In reality, vulnerabilities in well-designed devices can often be patched up at thetest site. Understand, however, that any modifications you make to pass the tests willhave to be implemented in the actual product. Don’t go overboard implementing everypossible solution at once. Although adding a capacitor here, a ferrite there, and someshielding to a cable may sound trivial, each of these modifications can turn into a logisticnightmare during production. Moreover, unbudgeted additions multiplied by the numberof units to be produced over time may end up reducing the profit margin to intolerablelevels.In addition, and before applying any corrective measures to a medical device prototype,however, make sure that by filtering or shielding a specific line, component, or assembly,you do not violate insulation or leakage requirements. With that said, let’s look at theessential elements of a first-aid kit.Ferrites Ferrites are the first thing most people use to try to clean the signals from a suspectline. A huge variety of ferrites are available; they come in all sizes and provide attenuationat diverse frequency ranges. Ferrites also come with various installation options:Some require you to pass the cable or lead component through them, while some haveclamps that make it easy to retrofit equipment without disconnecting wires. Ferrites arealso available to specifically treat differential or common-mode problems. Ferrite diagnostickits are available from various vendors (e.g., Fair-Rite), and test houses usually haveplenty of ferrite beads and chokes available for their customers.
GOOD <strong>DESIGN</strong> PRACTICES, REMEDIES, <strong>AND</strong> DUCT TAPE 201Ferrite is even available in tape form (actually, it is a ferrite-coated tape) and can beapplied to PCBs and as a shield on the chassis, enclosure, or other surfaces. Before buyingtape specifically for this application, try the magnetic backing sold in arts and craftstores to make refrigerator magnets out of photographs. It works wonders!Connector Filters If a signal line on a connector is a suspect for noncompliance, theeasiest and cleanest way to apply in-line filtering is either to exchange the original connectorfor a filtered one or to insert a filtered adapter between the original plug and its target socket.D-type filtered connectors and filtering adaptors are widely available and come with afeedthrough capacitor in the range 50 to 2000 pF with or without ferrite inductors. You shouldalso consider using ferrite plates with holes to match your connectors’ pinout configuration.Connector Shields Very often, shielded wires are used to protect sensitive or noisy lines,only to terminate at an unshielded connector. Connector backshields can easily beretrofitted onto many cables. Make sure, however, that by connecting the cable’s shield toan exposed metallic connector you do not violate insulation requirements.Capacitors and In-Line Filters Small capacitors can be tacked on to suspect lines. Theseare especially useful when dealing with problems that may be occurring on a PCB. It isalways a good idea to take an assortment of pF- and nF-range chip capacitors to the testhouse. If additional filtering is needed, some surgery can be done to a PCB to retrofit inlinefilter modules. Beware, however, that the addition of capacitors to the circuit of a medicaldevice may change its leakage characteristics, causing the device to fail leakage and/orhipot safety tests.Cable Shielding Cable shielding is the next step in troubleshooting and fixing EMCproblems. Mesh with and without zip-on sheaths, as well as conductive foils with or withoutadhesive backing, are available and can be applied to cables with ease. You will needto decide how thick a shield you use and how you connect the shield to ground.Enclosure Gaskets Metallic enclosures are often assumed to be bulletproof barriersagainst EMI, both incoming as well as outgoing. However, no instrument is perfectlysealed, since cables, displays, and controls couple the inside of the instrument to the outsideenvironment. In fact, a metallic case can sometimes act as a resonator, guiding EMIto (or from) the vulnerable (or offensive) circuit.Assuming that filtering and shielding of cables and controls has not sufficed to controlan EMI problem, the next step is looking for gaps in the enclosure which may requireshielding. Here, you can use metallic foils and tapes to improve contact along enclosureseams and determine if a permanent solution could be achieved through the use of conductiveEMC gaskets. In addition, temporary application of conductive foils to displaywindows and ventilation apertures is a very useful diagnostic to determine if conductivetransparent screens (e.g., very fine wire mesh) need to be applied to these openings. Manyof these shielding materials are available from Chomerics.If the problem is ESD, consider even tiny gaps or joints in enclosure shields which areweak spots, because they divert very large fast currents as they flow around the enclosure,causing current density hot spots that emit strong EMI through the shield and into theenclosure. In fact, for the very high frequency components of ESD pulses, gaps and jointsmay act as slot antennas that help get EMI into the enclosure.On a different front, consider that metallic shields can sometimes be completely transparentto offensive fields that have a dominant magnetic components. In these cases, vulnerableparts of the metallic enclosure may require further shielding with a material that
202 ELECTROMAGNETIC COMPATIBILITY <strong>AND</strong> <strong>MEDICAL</strong> DEVICESprovides a low-reluctance magnetic path for the interference field. The idea is to make theshield attract flux lines to itself and divert the magnetic field away from the sensitive component.The magnetic sheets mentioned above are a good start for solving these problems.If nonmagnetic shields are needed (e.g., to form a shield close to a CRT or a magnetic sensor),you may try one of the shielding alloys produced by Magnetic Shield Corporation.Magnetic Shield sells a $150 engineering kit that includes various 10 in. 15 in. sheets aswell as some braided sleeving made of their CO-NETIC and NETIC alloys. The kit evenincludes an ac magnetic field probe that can be used with a DVM or oscilloscope to measuremagnetic fields from 10 Hz to 3 kHz.Conductive Spray Paint Many medical devices are not built with metallic enclosures. Ifextensive shielding of the case becomes necessary, an alternative to changing the design touse a conductive enclosure is to spray-paint the enclosure using conductive paint. EMIspray paints are available to provide varying degrees of EMI shielding, all the way fromlight, graphite-based paints to provide mild shielding against ESD through nickel/chromeloadedsprays that can divert strong magnetic fields away from sensitive components.Shielding Components If you got this far down the list of quick patches, chances are thatyou may need to go back to the drawing board (or more likely, the PCB layout station).Before going back home, though, you may try to shield individual components. You couldapply one of various available conductive foils and tapes directly to PCBs (to shield tracks)or to components. There are even precut conductive cardboard boxes that can be used toshield entire sections of a circuit. However, if you need to build a complete village of protectivehousings on your PCB, it may be worthwhile biting the bullet and going back to thelab to reengineer the product.CONCLUDING REMARKSDesigning medical equipment that can pass EMI/EMC compliance testing without fixes ordelays never happens by mistake. Rather, it involves considering compliance with EMI andEMC regulations from the very beginning of product formulation and design. A head startin the battle against EMI can be obtained by developing a first prototype free of foreseeabletrouble. This is possible by carefully selecting the technologies that fulfill the productrequirements while minimizing EMI, observing good design and construction practices,and making extensive use of circuit simulation tools. Near-field probing of the first prototypeshould reveal real-world EMI effects that escaped from the limited view of initialmodeling. In addition, RF techniques prove to be essential in the design of circuits that canexploit the power of modern high-speed processors. Correcting any problems throughfiltering, shielding, or redesign is still inexpensive at this early stage in the design, and thesecond prototype will already have a good chance of passing compliance testing with minimalrework.In this chapter we have presented only a few of the ways in which technology selection,circuit design, and layout techniques influence the generation of and immunity against EMI.A discussion of detailed techniques to control EMI by virtue of good design is beyond thescope of this book. However, many books and articles have been published that disclose thesecrets of the EMI/EMC world, all the way from Maxwell’s equations, through the legalitiesof regulation, into the tricks of the trade for taming EMI [Mardiguian, 1992; Marshman,1992; Williams, 1999]. Considering the stiff economical, technical, and legal penaltiesbrought by manufacturing a medical product that does not comply with EMI and EMC regulations,you should be motivated to keep EMC in sight at every turn of the design process.
REFERENCES 203REFERENCESDash, G., and I. Strauss, Inside Part 15—Digital Device Approval, Compliance Engineering, 1995Annual Reference Guide, A11–A18.EN-55011, Limits and Methods of Measurement of Radio Disturbance Characteristics of Industrial,Scientific and Medical Radio Frequency Equipment, 1998.EN-60601-1-2, Medical Electrical Equipment—Part 1: General Requirements for Safety; Section 2:Collateral Standard: Electromagnetic Compatibility—Requirements and Tests, 1998.EN-61000-4-3, Electromagnetic Compatibility—Part 4: Testing and Measurement Techniques;Section 3: Radiated, Radio-Frequency, Electromagnetic Field Immunity Test, 1995.EN-61000-4-4, Electromagnetic Compatibility—Part 4: Testing and Measurement Techniques;Section 4: Electrical Fast Transient/Burst Immunity Test Basic Publication, 1995.EN-61000-4-5, Electromagnetic Compatibility—Part 4: Testing and Measurement Techniques;Section 5: Surge Immunity Test, 1995.EN-61000-4-6, Electromagnetic Compatibility—Part 4: Testing and Measurement Techniques;Section 6: Immunity to Conducted Disturbances, Induced by Radio-Frequency Fields, 1996.EN-61000-4-8, Electromagnetic Compatibility—Part 4: Testing and Measurement Techniques;Section 8: Power Frequency Magnetic Field Immunity Test Basic, EMC Publication, 1993.EN-61000-4-11, Electromagnetic Compatibility—Part 4: Testing and Measuring Techniques;Section 11: Voltage Dips, Short Interruptions and Voltage Variation Immunity Tests, 1993.Gubisch, R. W., The European Union’s EMC Directive, Compliance Engineering, 1995 AnnualReference Guide, A55–A64.Guettler, P., Disturbance Simulator Checks Lines, EDN, 152, October 14, 1999.IEC-60601-1-2, Medical Electrical Equipment—Part 1: General Requirements for Safety; Section2: Collateral Standard: Electromagnetic Compatibility Requirements and Tests, 1993.Kendall, C. M., Protecting Circuits against Electromagnetic Threats, Medical Device and DiagnosticIndustry, 78–82, March 1998.Kraz, V., Near-Field Methods of Locating EMI Sources, Compliance Engineering, 43–51, May–June1995.Magid, L. M., Electromagnetic Fields, Energy, and Waves, Wiley, New York, 1972.Mardiguian, M., Controlling Radiated Emissions by Design, Van Nostrand Reinhold, New York,1992.Marshman, C., The Guide to the EMC Directive, IEEE Press, Piscataway, NJ, 1992.Montgomery, D., Borrowing RF Techniques for Digital Design, Computer Design, 207–217, May1982.Strassberg, D., Time-Domain Reflectometry: In 50-MHz Digital Design, Measurements Are aMust, EDN, 65–72, August 19, 1993.Tiwari, S. S., Simple ESD Gun Tests IC, EDN, September 12, 1996.Williams, T., EMC for Product Designers, 2nd ed., Newnes, Oxford, 1999.
5SIGNAL CONDITIONING, DATA ACQUISITION,<strong>AND</strong> SPECTRAL ANALYSISSo far we have seen how to design electrodes, amplifiers, and filters to detect electrophysiologicalsignals that result from electrochemical events occurring in the living body.However, biopotentials are only a small fraction of the signals generated by physiologicalprocesses. Think about it for a second—physicians most often assess your health conditionby looking at changes in weight, heart and lung sounds, arterial blood pressure, andtemperature—none of these involve recording biopotential signals.Mimicking what your doctor does today, the next mirror in your bathroom, your nextbathroom scale, and your future shower and toilet will probably be loaded with sensorsthat can automatically and unobtrusively measure your temperature, look at skin marks,analyze your body composition, and examine your secretions for the telltale signs of infectionsor chemical imbalance. A behind-the-scenes computer will scan the sensor data setand suggest that you visit your doctor if it finds suspicious changes.It will take a while before we develop instruments sophisticated enough to make“Bones” McCoy feel cozy, but the trend of embedding sensors and intelligence intoeven the simplest medical instruments and home health appliances will continue togrow in the years to come. In fact, a recent study by a major technology-developmentcompany demonstrated that the largest emerging markets for the decade of the 2000swill be based on affordable, highly specific, very reliable sensors. This trend hasalready resulted in the development of many self-contained sensors that incorporate allthe necessary front-end electronics. Typically, these only need a power input to producea high-level output signal proportional to the measured variable. As shown in Table 5.1,many sensors with onboard electronics are already available to measure temperature,pressure, acceleration, gas concentrations, flow, magnetic fields, and so on. Althoughthe robo-doc may not be here yet, these sensors are being designed for incorporationinto consumer appliances, and as such they are becoming more available and moreaffordable by the day.Design and Development of Medical Electronic Instrumentation By David Prutchi and Michael NorrisISBN 0-471-67623-3 Copyright © 2005 John Wiley & Sons, Inc.205
206 SIGNAL CONDITIONING, DATA ACQUISITION, <strong>AND</strong> SPECTRAL ANALYSISTABLE 5.1Some of the Sensors with Onboard Electronics Widely Available to Measure a Diversity of Physical VariablesSensor Manufacturer Representative Part Excitation Range OutputTemperature Analog Devices AD590 4 to 30 V dc 55 to 150°C 1 mA/°KPeripheral pressure UFI 1010 None (piezoelectric) Typical human pulse 20–40 mVpulse pressure from finger into 1 MΩRespiration UFI Pneumotrace II None (piezoelectric) Typical human chest 20–100 mVexpansioninto 1 MΩAcceleration Analog Devices ADXL05 5 V dc Selectable 1 g Selectable 200 mV/gor 5 gor 1 V/gFluid pressure MSI MPS3102 10 to 32 V dc 0 to 1000 psi 4 mV/psiBarometric pressure Sensortechnics 144SC0811-BARO 7 to 24 V dc 800 to 1100 mbar 16 mV/mbarMagnetic field Honeywell HMC2003 6 to 15 V dc 2 G 1 V/GGas concentration Capteur Various with driver 5 V dc Sensor dependent 0 to 5 V range,(CO, combustible circuit sensor dependentgases, etc.)Ac or dc current Lem Heme LTA50P 15 V dc 0 to 50 A 100 mV/A(no contact)Air/gas flow Honeywell AWM3300V 10 V dc 0 to 1 L/min 4 V/L/minHumidity Thermometrics RHU-217 5 V dc 30 to 90% RH 33 mV/%RHUNIVERSAL SENSOR INTERFACE 1The device of Figure 5.1 is a simple sensor interface that plugs into the printer port of thePC. With it, it is possible to excite, control, and read a wide variety of sensors directly froma personal computer. This universal sensor interface features an eight-channel 12-bit A/Dconverter with user-selectable input ranges, two 12-bit D/A converters, two 100-µA currentsources for direct sensor excitation, and an uncommitted current mirror and multipledigital I/O lines.A block diagram of the universal sensor interface is shown in Figure 5.2. Note that thecircuit can accept and read analog signals from up to eight sensors. The sensor-derived signalsare fed through individual prescalers and applied to an eight-channel multiplexer, permittingthe user to select a particular sensor-generated signal. At any given time, one of theeight scaled input signals is presented at the output of the multiplexer to a 12-bit A/D converter.The voltage reference for the A/D is provided by a precision 2.5-V reference IC.Analog outputs are generated by the universal sensor interface through dual voltageoutputD/A converters. The resolution of the D/A converters is also 12 bits. To simplify thereading of resistive sensors, the universal sensor interface also includes a precision currentreferenceIC which incorporates two 100-µA current sources and an uncommitted currentmirror. These can be configured to provide constant-current excitation in the range 100 to400 µA.Power for the A/D section is obtained directly from the printer port. The D/A convertersand current sources are powered from an internal 5-V linear regulator. Whenever theD/A converters or the current sources are needed, an external 9-V to 12-V supply mustbe provided. This power supply is not required if only the A/D converter section is used.Finally, the digital inputs and outputs of the printer port which are not used by the circuitrywithin the universal sensor interface are made available to the user as general-purpose I/Olines. These can be used to read switches, provide power to sensors with integrated electronics,or effect real-time control of devices based on information gathered from sensors.1The material in this section appeared originally in Popular Electronics [Prutchi, 1999].
UNIVERSAL SENSOR INTERFACE 207Figure 5.1 The universal sensor interface is a simple device that plugs into the printer port of thePC. It can excite, control, and read a wide variety of sensors directly from a PC.Unlike ordinary data acquisition setups, the universal sensor interface offers a greatdegree of flexibility and portability. Virtually all PCs come equipped with a parallel printerport, and reconnecting this data acquisition system to the computer typically does notrequire delving into the enclosure. Moreover, since the use of the printer port is standardized,the same software will run on any PC without the need for reconfiguration. As longas the signals to be converted are correctly scaled and sampled, the universal sensor interfaceshould have you experimenting with the new generation of sensors in no time at all.A/D ConverterAs shown in Figure 5.3, a Linear Technology LTC1285 integrated circuit (IC1) is at theheart of the A/D circuitry within the universal sensor interface. This IC implements a 12-bit successive-approximation A/D converter, complete with a sample-and-hold and a highspeedthree-wire serial interface. A 2.5-V reference voltage is regulated by D1 andsupplied to the VREF input of the A/D converter.The serial interface to the LTC1285 requires only three digital lines. Data-conversion initiationand data-read operations are controlled by the *CS (chip select) and SCLK (serialclock) lines. Data are obtained serially through the DOUT line. As shown in Figure 5.4a,an A/D conversion is initiated by a falling edge on the *CS line. At this point, the sampleand-holdstores the input voltage and the successive-approximation process commences.
SCLKDOUT*CSMUXD0MUXD1MUXD2ANALOG TO DIGITAL CONVERTERA/D_POWER#1A/D_POWER#2*A/D_SERIAL_CLOCK*A/D_SERIAL_DATA_OUT*A/D_CHIP_SELECTA/D_MUX_D0A/D_MUX_D1A/D_MUX_D2A/D CHANNEL 1A/D CHANNEL 2A/D CHANNE L 3A/D CHANNEL 4A/D CHANNEL 5A/D CHANNEL 6A/D CHANNEL 7A/D CHANNEL 891087654321R5R41 162 153 144 135 126 117 108 9100uA21 820 719 618 517 422 910231124122513J2DB25J3Analog Input #1Signal GNDAnalog Input #2Signal GNDAnalog Input #3100 uA out #1Analog Input #414 115 214216 315316417 100 uA out #2DB25151861972082192210231124122513Analog Input #5Current Mirror CommonAnalog Input #6Current Mirror InputAnalog Input #7Current Mirror OutputAnalog Input #8Digital Output #1Analog Output #1Digital Output #2Analog Output #2Digital Input #1Digital Input #2+ InterruptDigital Input #3Digital Input #4GROUNDBattery +Battery -(Power andDigital GND)100uA+9VBT1Current Mirror InCurrent Mirror OutCurrent Mirror CommonPOWER REGULATOR+5VPOWER OUTPOWER INGNDD/A CONVERTERS*DACLKDADAT*DACSPOWER*D/A_SERIAL_CLOCKD/A_SERIAL_DATA_INPUT*D/A_CHIP_SELECTD/A_CHANNEL2D/A_CHANNEL1GNDFigure 5.2 Block diagram of the universal sensor interface. This device features an eight-channel 12-bit A/D converter with user-selectableinput ranges, two 12-bit D/A converters, two 100-µA current sources for direct sensor excitation, as well as an uncommitted current mirrorand multiple digital I/O lines. (From Prutchi [1999]. Reprinted with permission from Popular Electronics, June 1999 © GernsbackPublications Inc.)Control_*D0Control_*D1Out_D0In_D0Out_D1Control_D2Out_D2Control_*D3Out_D3Out_D4Out_D5Out_D6Out_D7In_D10In_*D7In_D5In_D411421531641751861972082192210231124122513J1DB25208
Figure 5.3 Schematic diagram of the universal sensor interface. The micropower components of the A/D section are supplied directly fromthe printer port. The D/A and current sources require an external power supply. (From Prutchi [1999]. Reprinted with permission fromPopular Electronics, June 1999 © Gernsback Publications Inc.)209
210Figure 5.4 Timing diagram for the serial protocols of the A/D and D/A converters of the universal sensor interface: (a) timing diagram forthe A/D section; (b) protocol for the LTC1446 D/A IC. (From Prutchi [1999]. Reprinted with permission from Popular Electronics, June1999 © Gernsback Publications Inc.)
UNIVERSAL SENSOR INTERFACE 211As conversion takes place, data are obtained in serial format on each falling-edge transitionof SCLK after the third clock pulse. Since there are 12 bits, a minimum of 14 fallingedgepulses are required to shift out the A/D result. Bits 0 and 1 of the LPT 8-bit outputport (hex address 378 for LPT1:) are toggled by software to implement the control portionof the A/D’s serial protocol. Bit 0 of the printer status port register (hex address 379 forLPT1:) is used to receive the serial data from the A/D.A 3-bit parallel interface using bits 4, 5, and 6 of the LPT 8-bit output port (hex address378 for LPT1:) controls the analog input multiplexer (IC2) that selects which one of theeight analog inputs is presented to the input of the A/D converter. Power for the A/D converter,the 2.5-V reference, and the multiplexer is supplied directly from the lines controlledby bits 2 and 3 of the parallel printer port.The following VisualBasic code module (DECLARATIONS.BAS) shows the exactlocation of the control bits for the universal sensor interface.' This module contains the general declarations required' to operate the Universal Sensor Interface'''' Declare DLL to enable I/O through the printer port' --------------------------------------------------'Public Declare Function Inp Lib "inpout32.dll" _Alias "Inp32" (ByVal PortAddress As Integer) As BytePublic Declare Sub Out Lib "inpout32.dll" _Alias "Out32" (ByVal PortAddress As Integer, ByVal Value As Byte)'' Printer port locations' ----------------------Global Const prinop1 &H378 ' Printer Output Port for LPT1Global Const prinstat1 &H379 ' Printer Status Port for LPT1Global Const princont1 &H37A ' Printer Control Port for LPT1Global Const prinop2 &H278 ' Printer Output Port for LPT2Global Const prinstat2 &H279 ' Printer Status Port for LPT2Global Const princont2 &H27A ' Printer Control Port for LPT2Global Const prinop3 &H3BC ' Printer Output Port for LPT3Global Const prinstat3 &H3BD ' Printer Status Port for LPT3Global Const princont3 &H3BE ' Printer Control Port for LPT3'' Define control pin locations for LPT:Analog! model 8c-I/O' ---------------------------------------------------------Global Const notdaclk 1, notdacs 2, dadat 4' notdaclk is the D/A serial clock line (active low)' notdacs is the D/A chip select line (active low)' dadat is the D/A serial data input lineGlobal Const power 12, notcs 1, sclk 2, muxd0 16, muxd1 32, muxd2 64' power are the two D/A power supply lines' notcs is the A/D chip select line (active low)' sclk is the A/D serial clock line' muxd0 is the A/D input multiplexer data line 0' muxd1 is the A/D input multiplexer data line 1' muxd2 is the A/D input multiplexer data line 2
212 SIGNAL CONDITIONING, DATA ACQUISITION, <strong>AND</strong> SPECTRAL ANALYSIS'' Define variables for printer port location' ------------------------------------------Global prinop ' Printer Port Output Port location variableGlobal prinstat ' Printer Port Status Port location variableGlobal princont ' Printer Port Control Port location variableThe following VisualBasic code module (ACQUIRE.BAS) shows how the serialprotocol for the A/D is implemented.Function Acquire (mux) As Single'' Function Acquire (mux) executes the A/D protocol on the' channel specified by mux. The A/D’s result in A/D counts is' returned via the Acquire variable.'''' Define variables' ---------------Dim clocknum As Integer ' clock counter variableDim dat As Integer' accumulated data variableDim bit As Integer' filtered data bit variableDim bit7 As Integer ' current value of Out D7' Acquisition loop' ----------------bit7 Inp (prinop) And 2 ^ 7' evaluate current value of OutD7Out prinop, power notcs sclk mux bit7 ' power up but keep CS’deasserted and' do not upset bit 7 of OutputportOut prinop, power mux bit7' convert by asserting CS’, pullSCLK low' without upsetting bit 7 of' Output portFor clocknum 1 To 2' two clock pulses are requiredto startOut prinop, power sclk mux bit7 ' conversion processOut prinop, power mux bit7Next clocknumdat 0' clear A/D accumulator variableFor clocknum 11 To 0 Step 1 ' clock 12 bits seriallyOut prinop, power sclk mux bit7 ' clock pulse rising edge without' upsetting' bit 7 of Output portOut prinop, power mux bit7' clock pulse falling edge without' upsetting' bit 7 of Output portbit (Inp (prinstat) And 8) / 8 ' read Status port and filter bit' corresponding' to A/D’s serial data output
UNIVERSAL SENSOR INTERFACE 213dat dat (2 ^ clocknum) * bit ' accumulate from bit 11 to bit 0Next clocknum' next bitOut prinop, power notcs mux bit7 ' deassert *CS without upsetting bit 7Acquire dat' return 12-bit A/D countEnd FunctionSignal ConditioningInput signals rarely fit exactly within the universal sensor interface’s input range of 0 to2.5 V. Signals of smaller amplitude than the full range waste resolution, while signals outsidethe full range will end up being clipped to the limits of the range. Please note thatinput signals presented to the A/D multiplexer exceeding the range 0 to 2.5 V may causepermanent damage to the circuitry of the interface. Measuring a signal that spans 0 V anda value larger than 2.5 V is easily accomplished. A resistive voltage divider such as that ofFigure 5.5a can scale a large unipolar signal to the desired range. For ease of use, the universalsensor interface has onboard locations reserved for resistive voltage dividers. Thevoltage-divider resistor packs are marked R4 and R5. To use them, first select the appropriate10-pin single-in-line bussed resistor array for R5. Then select either a DIP resistorpack or individual 1 4 -W precision resistors to be placed on R4.Logging data from the sensors on a hyperbaric chamber (a pressurized vessel used tostudy the therapeutic use of high atmospheric pressures) provides a good example of howto select components for R4 and R5. Table 5.2 shows typical ranges for sensors that monitora small hyperbaric chamber. For this application, the range for analog channels 1 to 4of the universal sensor interface should be 0 to 5 V, the range for channel 5 should be 0 to10 V, and the range of channels 6 to 8 should remain at 2.5 V. Assume that an impedanceof 10 kΩ is appropriate for all channels.For this example, R5 can be selected to be a 10-pin bused 10 -kΩ resistor pack. A suitabledevice is a CTS 770-series 10-kΩ, single-in-line conformal 10-pin bused resistor network(Digi-Key part 770-101-10K-ND) or similar (e.g., Jameco 24643). 1% 1 4-W resistorsfor R4 are selected using the following formula:10kΩ2.5 V V max R4 10kΩAs such, 10-kΩ resistors should be placed between pads pairs [1,16], [2,15], [3,14], and[4,13] of R4 to yield a range of 0 to 5 V for channels 1 to 4. For channel 5, the formularequires a 30-kΩ resistor for a range of 0 to 10 V. Since 30 kΩ is not a standard value, a30.1-kΩ 1% resistor should be selected and soldered between pads 5 and 12 of R4. Channels6 to 8 do not require scaling, and thus pad pairs [6,11], [7,10], and [8,9] should be jumpered.As shown in Figure 5.5b, a small unipolar signal requires just an op-amp-based amplifierto take advantage of the full resolution of the A/D. Signals riding on a median different thanthe A/D’s midpoint (1.25 V) can be offset appropriately by using the circuit of Figure 5.5c.Alternatively, a “quick and dirty” way of introducing offset that can sometimes be used toenable measurement of bipolar signals is to place a 1.5-V battery in series with the signalsource.Current measurements can be obtained by using a suitable shunt. For example, asshown in Figure 5.5d, the popular 4- to 20-mA current loop used to convey informationfrom many industrial instruments and sensors can be converted to a voltage by using ametal-film 124 Ω 1% resistor shunt across the input terminals of the universal sensorinterface. Since the 4- to 20-mA current will be translated into the range 0.496 to 2.48 V,some measurement resolution will end up being wasted. If the full 12-bit resolution isdesired, you may use a 154 Ω 1% resistor instead and use an op-amp to introduce a0.616-V offset to the measurement.
214 SIGNAL CONDITIONING, DATA ACQUISITION, <strong>AND</strong> SPECTRAL ANALYSIS(a)(b)+5VR17 13+2-TL08160 TO 2.5V0V = < Vin = < VmaxR10 TO 2.5V0V = < Vin < 2.5V4 5-5VR2R2R3R22.5V = Vmax= R2R1 + R22.5V = V max =R1+ 1R3 - R1(c)(d)+9VABS(DELTA(Vin)) < 2.5V100k327 1+-TL0816100kVout = Vin = Voff0.496 TO 2.48V-9V < Vin < +9V100 k100 k4 5-9VI = 4-20mA124 Ohm-9V<strong>OF</strong>FSET10 k+9VVoff10uF+.01uF10uF+Vout = I = 125Figure 5.5 Simple circuits can be used to scale different signals to fit within the range 0 to 2.5 V of the universal sensor interface. (a) Largeunipolar signals can be attenuated by a voltage divider. (b) Small unipolar signals can be amplified to make use of the A/D’s full resolution.(c) Bipolar signals can be converted into unipolar signals by introducing offset. (d) 4- to 20-mA current loop signals can be read through aresistive shunt. (From Prutchi [1999]. Reprinted with permission from Popular Electronics, June 1999 © Gernsback Publications Inc.)D/A ConverterAnalog outputs are generated by the universal sensor interface through a LTC1446 dualvoltage-output D/A converter IC (IC4). The resolution of the D/A converters is 12 bits,providing 1 mV per bit over the range 0 to 4.096 V. There may be an offset error of up to18 mV (less than 3 mV typical), and the nonlinearity is 0.5 LSB maximum. The D/Aoutputs have a maximum current-handling capability of 100 mA, and their maximumsource impedance to ground is 120 Ω . In practice, the rail-to-rail buffered outputs cansource or sink 5 mA when operating with a 5-V supply while pulling to within 300 mV ofthe positive supply voltage or ground. The outputs swing to within a few millivolts ofeither supply rail when unloaded and have an equivalent output resistance of 40 Ω whendriving a load to the rails. The D/A buffer amplifiers can drive 1000 pF without going intooscillation.
UNIVERSAL SENSOR INTERFACE 215TABLE 5.2 Some Output Ranges of Sensors Used for EnvironmentalConditions in a Small Hyperbaric Research ChamberADC Channel Sensor Output Range (V)1 Inside oxygen partial pressure 0–52 Inside CO 2 partial pressure 0–53 Atmospheric pressure 0–54 Hyperbaric chamber pressure 0–55 Inside relative humidity 0–106 Inside ambient temperature 0–1.27 Outside ambient temperature 0–1.28 Specimen temperature 0–1.2The D/A converters are powered from a 5-V linear regulator (IC3). Whenever eitherthe D/A converters or the current sources are needed, an external 9- to 12-V supplymust be provided. In some cases, powering the A/D section through an external power supplymay also be desirable. To do so, do not install R1, R2, C3, and L1. Instead, install R3and place a jumper on JP1. These changes supply the A/D section of the Universal SensorInterface from the regulated 5 V supplied by IC3.The D/A converters are controlled through a serial protocol that requires only three digitallines. Bits 0 to 2 of the LPT control port (hex address 37A for LPT1:) are used for thispurpose. As shown in Figure 5.4b, data-conversion initiation and data-write operations arecontrolled by the *DACS (D/A chip select) and DACLK (D/A serial clock) lines. Data aresupplied to the D/A converters serially through the DADAT line. The data on the DADATinput are loaded into a shift register (internal to the D/A converter control circuitry) on therising edge of the DACLK clock. Data are loaded as one 24-bit word where the first 12 bitsare for DAC 1 and the second 12 are for DAC 2. For each 12-bit segment the MSB isloaded first. Data from the shift register are loaded into the D/A register when *DACS ispulled high. The clock is disabled internally when *DACS is high. DACLK must be lowbefore *DACS is pulled low to avoid an extra internal clock pulse.The following VisualBasic code module (DTOA.BAS) shows how the D/A serial controlprotocol is implemented.Function dtoa(dtoa1 As Integer, dtoa2 As Integer) As Integer'' Function DtoA (dtoa1, dtoa2) executes the serial protocol to update D/A' converters with the values defined by dtoa1 and dtoa2, where' dtoa1 contains the code for the desired D/A channel 1 output' dtoa2 contains the code for the desired D/A channel 2 output'''' Define variables' ---------------Dim bit3 As Integer ' value of Control *D3Dim clocknum As Integer' clock pulse counterDim delay As Integer' delay loop dummy variabe' D/A loop' --------bit3 Inp(princont) And 8 ' evaluate current status of Control *D3Out princont, notdaclk bit3' set D/A clock line low without' upsetting bit 3 of the Control port
216 SIGNAL CONDITIONING, DATA ACQUISITION, <strong>AND</strong> SPECTRAL ANALYSISOut princont, notdaclk notdacs bit3 ' assert D/A CS’ line without' upsetting bit 3 of the Control' portFor clocknum 11 To 0 Step 1 ' clock 12 bits of D/A channel 1' from MSB to LSBIf (dtoa1 And (2 ^ clocknum)) 0 Then ' if current bit converts to 0Out princont, notdacs bit3' then do not set data bit high' while causing a clock rising edge' all without upsetting bit 3 of the' Control portFor delay 1 To 5: Next delayOut princont, notdacs notdaclk bit3 ' return clock line to low' without upsetting bit 3 of theControl portElse' if, on the other hand, current' bit converts to oneOut princont, notdacs notdaclk dadat bit3 ' then set data bit high' while' maintaining the 'CS and clock' and do not' upset bit 3 of the Control' port' lines lowFor delay 1 To 5: Next delay ' introduce delay to comply with IC’s' timing requirementsOut princont, notdacs dadat bit3 ' cause clock rising edge to' clock data bit in without' upsetting' bit 3 of the Control portFor delay 1 To 5: Next delay ' introduce delay to comply withIC’s' timing requirementsOut princont, notdacs notdaclk dadat bit3 ' return clock line to' low without' upsetting bit 3 of the' Control portEnd IfNext clocknum' next bitFor delay 1 To 5: Next delayFor clocknum 11 To 0 Step 1 ' clock 12 bits of D/A channel 2' in the same wayIf (dtoa2 And (2 ^ clocknum)) 0 ThenOut princont, notdacs bit3For delay 1 To 5: Next delayOut princont, notdacs notdaclk bit3ElseOut princont, notdacs notdaclk dadat bit3For delay 1 To 5: Next delayOut princont, notdacs dadat bit3For delay 1 To 5: Next delayOut princont, notdacs notdaclk dadat bit3End If
UNIVERSAL SENSOR INTERFACE 217For delay 1 To 5: Next delayNext clocknumOut princont, bit3' update D/A data by deasserting ’CS' without upsetting bit 3 of the Control port' under this condition, clock and' data states are of no relevancedtoa 0 ' dummy return variable 0End FunctionCurrent SourcesA Burr-Brown REF200 IC is used to make two 100-µA current sources and an uncommittedcurrent mirror available on the universal sensor interface. Constant-current sources arehighly useful for the excitation of resistive sensors. Figure 5.6 shows various ways in whichthe current source outputs and the current mirror can be connected to obtain the following:• Two 100-µA sources• One 200-µA source• One 300-µA source• One 400-µA source100uA16 100uA Out100uA16100uA16100uA17 100uA Out100uA17200uA Out100uA17Current Mirror InCurrent Mirror Out1920Current Mirror InCurrent Mirror Out1920Current Mirror InCurrent Mirror Out1920+5VCurrent Mirror Common18Not usedCurrent Mirror Common18Not usedCurrent Mirror Common18Two 100uA Sources200uA Source300uA Source300uA Sink100uA16100uA16100uA Out100uA16100uA17100uA17100uA17Current Mirror InCurrent Mirror Out1920Current Mirror In 19+5V Current Mirror Out 20100uA SinkCurrent Mirror InCurrent Mirror Out1920200uA SinkCurrent Mirror Common18400uA OutCurrent Mirror Common18Current Mirror Common400uA Source100uA Source and200uA Sink100uA SinkFigure 5.6 The current sources and current mirror can be wired to obtain various configurations within the range 100 to 400 µA. (FromPrutchi [1999]. Reprinted with permission from Popular Electronics, June 1999 © Gernsback Publications Inc.)18
218 SIGNAL CONDITIONING, DATA ACQUISITION, <strong>AND</strong> SPECTRAL ANALYSIS• One 100-µA source and one 100-µA sink• One 200-µA sinkThe accuracy of these sources and sinks is typically better than 1%, and the voltagecompliance is 3.6 V.Digital I/OThe digital inputs and outputs available on the analog and digital I/O connector of theUniversal Sensor Interface are direct pass-throughs of the unused I/O lines from the printerport. The four digital input lines are acquired through bits 4, 5, 6, and 7 of the LPT statusport (hex address 379 for LPT1:). Please note that in the standard parallel port, bits 1 to 3of the status byte do not convey line state information. In addition, digital input 2 (bit 6 ofthe status port) can be used to drive interrupt-driven acquisition programs. The two digitaloutput lines are controlled through bit 3 of the LPT control port (hex address 37A forLPT1:) and bit 7 of the LPT output port (hex address 378 for LPT1:).The following VisualBasic code module shows how to read and filter the four digitalinputs available on the universal sensor interface.status Inp(prinstat)' Acquire data from digital inputsdin1 (status And 128) / 128 ' evaluate digital input #1If din1 1 Then din1 0 Else din1 1 ' invert din1din3 (status And 32) / 32 ' evaluate digital input #2din2 (status And 64) / 64 ' evaluate digital input #3din4 (status And 16) / 16 ' evaluate digital input #4Construction of the Universal Sensor InterfaceThe universal sensor interface can be constructed on a small prototyping board using pointto-pointwiring techniques. To achieve good A/D performance, build separate analog anddigital ground planes and join these at a single point close to the ground connection on J1.If possible, build the universal sensor interface on a four-layer PCB. The entire assemblycan be made to fit neatly in a 3-in. hood enclosure with DB25 connectors at the ends.Software for the Universal Sensor InterfaceSoftware for the universal sensor interface is available in the universal sensor interfacedirectory at the Wiley ftp site associated with this book. This directory contains a numberof data acquisition utilities as well as drivers and program examples. The program examplesare thoroughly commented and should be self-explanatory.Figure 5.7 presents the control panel for the VisualBasic (v5.0) application projectLPT8_DVM.VBP. This is an example of how to develop a virtual instrument to acquireanalog and digital data as well as to control the D/A and digital outputs of the UniversalSensor Interface. A 32-bit I/O DLL (Dynamic Link Library) is used to allow input and outputoperations to be performed on the printer port under the command of VisualBasic. If16-bit operation is required, modify the programs to make use of the 16-bit CUSER2.DLLfile. LPT8_LOGGER.VBP is basically the same as LPT8_DVM.VBP, but a file dialog hasbeen added to make it possible to log acquired data directly to disk.In addition, the archive also contains the following examples in QuickBasic:1. LPTAN8.BAS is a simple program for driving the universal sensor interface A/D.Notice that use of the standard LPT1: is assumed, and you may need to change the output
UNIVERSAL SENSOR INTERFACE 219Figure 5.7 Virtual instruments such as this eight-channel DVM based on the universal sensor interfacecan easily be built using VisualBasic. (From Prutchi [1999]. Reprinted with permission fromPopular Electronics, June 1999 © Gernsback Publications Inc.)port and status port locations to suit your specific installation. This program will acquireand display data on the screen at the maximum rate supported by your computer whenrunning QuickBasic.2. ACQUIRE8.BAS implements an eight-channel oscilloscope/four-channel logic analyzer.In this program, the sampling rate is regulated by inserting for–to loops to introducedelay between samples. The number of loops required to reach the correct delay is basedon a calculation of the time that it takes the computer to complete a single data acquisitionand display operation, as well as of the delay introduced by the addition of a for-to loop.The performance of this program depends on the processor speed of the computer, theresources available to the processor, the access speed to the video card, and so on. Sometypical acquisition rates achieved by this program are shown in Table 5.3.3. LPT8FAST.BAS is the same as ACQUIRE8.BAS, but provisions have been made toallow acquired data to be recorded on disk. The compiled version (LPT8FAST.EXE) ofthis program is intended to be run from a bootable diskette in which CONFIG.SYS firstinitializes a RAM drive. In contrast to writing to a hard drive, writing to a RAM drive isvirtually instantaneous, so LPT8FAST stores data in real time on the RAM drive, and onlythen copies the generated file onto the desired file on the hard drive. Disk writing is donein ASCII format, allowing you to import acquired data directly into virtually any of themost popular application programs (spreadsheets, data analysis software, etc.).4. The LPT8FAST.EXE utility is meant to be executed from a bootable diskette drive.To create the bootable diskette, first format a new diskette and transfer into it the systemfiles, your DOS COMM<strong>AND</strong>.COM, HIMEM.SYS, and RAMDRIVE.SYS files. Then
220 SIGNAL CONDITIONING, DATA ACQUISITION, <strong>AND</strong> SPECTRAL ANALYSISTABLE 5.3 Representative Maximum Sampling Rates Achieved by the Compiled Version ofACQUIRE8 to Run the Universal Sensor Interface as an Oscilloscope/Logic Analyzer1 Analog Channel 8 Analog Channels Acquisition/Computer 4 Digital Inputs (samples/s) 4 Digital Inputs (samples/s)486, 66 MHz 834 205Pentium, 133 MHz 2260 523Pentium, 166 MHz 2314 561Pentium, 200 MHz 2766 743copy the LPT8FAST.EXE file under the root directory of the diskette. Boot your computerfrom the diskette you created. This should take you to the utility’s setup dialog. Whenasked for it, enter the path and file name under which the program will store acquired data(e.g., C:\MYDATA.TXT). Within this utility, the computer will calculate the maximumsampling rate that can be achieved by this program using the Universal Sensor Interface inconjunction with your computer. You may then select any sampling rate up to the maximumrate calculated for your computer. In addition, you may need to select a differentdrive letter than the default D: for the RAM drive created by the bootup process. Pay attentionto the letter assignment made for the RAM drive when RAMDRIVE.SYS runs (justafter booting from the diskette that you created). After entering the desired acquisitionsetup, data will be acquired into the RAM drive and displayed simultaneously in the computerscreen. Stop the data acquisition process by pressing any key. Upon doing so, theacq8.txt file on the RAM drive will be saved to the file you specified.This program is intended only as an example of implementing the serial protocol requiredto collect data from the universal sensor interface through the PC printer port, and majorenhancements could be made to it. First, QuickBasic imposes a major limit on data acquisitionspeed. Even running on a 200-MHz Pentium PC, the single-channel sampling rate is limitedto about 2.7 kHz. True compilers with in-line assembly (e.g., C) can increase the effectivesampling rate to the vicinity of the 7.5-kHz maximum sampling rate supported by the A/D inthe universal sensor interface. Another improvement that can be made is to eliminate the insertionof delay loops to control timing, and instead, to control the acquisition process from interruptsgenerated by high-resolution hardware timing [Schulze, 1991; Ackerman, 1992].5. ATOD_SL8.BAS is similar to LPTAN8.BAS, but acquisition is regulated through theTIMER command. Through it, data frames are acquired at desired intervals in the range 1 to86,400 seconds (1 second to 24 hours between samples). Data frames are acquired and storedon an array. After acquisition is complete, the array is stored to a file on disk.6. DTOA.BAS is a simple program that implements the serial protocol to write valuesto the D/A converters.Signal ConditioningSensors that do not produce an output voltage directly can also be measured by the universalsensor interface. For example, Figure 5.8 shows the typical setup for reading a resistivesensor. Here a thermistor (Radio Shack Catalog 271-110) is excited by one of the100-µA sources. The voltage developed across the thermistor by the constant-current excitationis related to temperature. THERMOM.BAS, a QuickBasic program also in theaccompanying disk, is used to read temperature in °C and °F using this circuit. Other resistivesensors, such as piezoresistors, resistive position indicators, resistive humidity sensors,photoresistors, and so on, can be measured in the same way.The circuit of Figure 5.9 shows how the universal sensor interface can be used for readingsensors that require automatic baseline cancellation. For example, a strain-gauge load cell
UNIVERSAL SENSOR INTERFACE 22111421531641751861972082192210231124122513100uA EXCITATIONTBATTERY - (POWER<strong>AND</strong> DIGITAL GROUND)R1RS-271-110A+Figure 5.8 Resistive sensors such as the thermistor shown can be read by injecting a known currentinto the sensor and measuring the voltage developed across the sensor. (From Prutchi [1999].Reprinted with permission from Popular Electronics, June 1999 © Gernsback Publications Inc.)Warning! Be extremely careful when using the universal sensor interface to controlline-powered devices. Life-threatening voltages and currents are present in these circuits.Isolate and fuse all circuitry properly on the power line path.from an inexpensive digital kitchen scale can be excited from an op-amp (IC1A) driven byD/A converter 2. When the scale is not loaded, the output from the cell is a voltage that floatssomewhere in the range of 0 to the drive voltage generated by A/D converter 2. This outputvoltage is slightly amplified by IC1B (gain 1.78). IC1C is used to cancel the load cell’s baselinelevel by offsetting the output of IC1B by the amount established by D/A converter 1. Thesignal developed by a real load is further amplified by IC1D before being fed to analog input1. Resistor R4 and zener diode D1 protect the A/D input from output voltages produced byIC1D, which may be beyond the acceptable input range. SCALE.BAS is the QuickBasic programthat implements an auto-zeroing digital scale by controlling the sensor’s output offset.The Universal Sensor Interface is also ideal for implementing low-cost process or environmentalcontrol systems. For this type of application, the device’s digital outputs are oftenrequired to switch ac loads such as heaters, lamps, or motors. As shown in Figure 5.10, thedigital outputs of the universal sensor interface can be used to control an ac load connectedto the power line through an opto-isolated triac. The digital output signal is used to drive a2N2222 transistor, which in turn controls the LED inside the optocoupler (IC1). The optodevice selected for this application is a zero-voltage switching triac which is used to drivea power triac (Q1) capable of handling the necessary switching power. A device that can beused to switch light loads is the Q4004.Digital inputs can also be isolated. The circuit of Figure 5.11 shows how a PS2506 can beused to sense an ac or dc voltage safely to signal a digital input line. R1 should be selectedto produce no more than 20 mA of current through the LED of the PS2506.
TO J1UNIVERSALSENSORINTERFACECONNECTOR DB25J1LOAD CELL+9V-9VR3STRAIN GAUGE 2R85.6k56+9V+--9 VR510kR2100k+9V+-+-IC1ATL084R1STRAIN GAUGE 14IC1BTL08471094-9VIC1CTL084R910k1213+9V4+--9VIC1DTL08414GAINR4100414 115 216 3111118111117 418 519 620 721 822 910231124122513DRIVE TOLOADCELLR10100kR6100kR7100kD/A CONVERTER 1 OUTPUTIS USED TO AUTO-ZEROD11N5227B+9V+ C3C4+9VSOURCED/A CONVERTER 2 OUTPUT IS USEDTO SET DRIVE VOLTAGE TO EXCITELOAD CELL10uF.01uF+ C5C610uF.01uFSOURCE-9VFigure 5.9 A very precise scale can be built for the PC from the load cell of an inexpensive kitchen scale and a simple signal-conditioningcircuit. (From Prutchi [1999]. Reprinted with permission from Popular Electronics, June 1999 © Gernsback Publications Inc.)C1.01uF32C2.01uFB19VB29V222
UNIVERSAL SENSOR INTERFACE 223TO J2 <strong>OF</strong> UNIVERSALSENSOR INTERFACE114215R1316456017518619720821R59221k102311241225131IC1MOC30316R2100TR1 RLOAD24C1ZERO0.1uFQ4004CROSSCIRCUITQ22N2222B19V +R31.2k117VACCONNECTOR DB25BATTERY - (POWER <strong>AND</strong> DIGITAL GND)Figure 5.10 The digital-output lines of the universal sensor interface can be used to control ac loads in response to sensor inputs. This linecontrolinterface is suitable for turning on or off relatively light ac-powered loads. (From Prutchi [1999]. Reprinted with permission fromPopular Electronics, June 1999 © Gernsback Publications Inc.)TO J2 <strong>OF</strong> UNIVERSALSENSOR INTERFACE11421531641751861972082192210231124122513B19VIC2MC78L05CP3 1VIN VOUT43R2220IC1PS250612RDROPAC OR DCINPUTCONNECTOR DB25C1.01uFGND2C1.01uFFigure 5.11 Use this circuit to translate and safely isolate external ac or dc levels (e.g., power switch closures) to signals that can be readby the digital input lines of the universal sensor interface. (From Prutchi [1999]. Reprinted with permission from Popular Electronics, June1999 © Gernsback Publications Inc.)
224 SIGNAL CONDITIONING, DATA ACQUISITION, <strong>AND</strong> SPECTRAL ANALYSISSAMPLING RATE <strong>AND</strong> THE NYQUIST THEOREMWithout doubt you have heard that according to the Nyquist theorem, a signal should besampled at twice its frequency. Yes, and no. There is no data acquisition concept that ismore quoted and less well understood than the Nyquist theorem. Let’s explore what thistheorem actually implies for proper data acquisition. Nyquist stated that any bandwidthlimitedsignal can be reconstructed from its digitized equivalent if the sample rate is at leasttwice the highest-frequency component.Signal components with a frequency above half the sampling rate are aliased and showup in a reconstruction as a component with a frequency at the difference between its realfrequency and the sampling rate. This effect is commonly seen in films of moving cars,where the wheels seem to be rotating impossibly slow, or even going backward. The aliasedrotation frequency is caused by the slow shutter rate of the camera relative to the fast rotationalspeed of the wheels’ rims. For a dramatic demonstration, pay attention to the apparentbehavior of the wheels of a speeding stagecoach in virtually any old western movie.The way of preventing aliasing is to ensure that there are absolutely no signal componentsat frequencies above half the sampling rate. Assuming that to sample a signal ofapproximately x hertz you simply need to select an A/D rate of 2x just doesn’t cut it. Theonly ways of making sure are to supersample 2 the signal and to apply antialiasing filtering.Perfectionists insist that all signals to be sampled must be low-pass filtered to preventaliasing. In reality, however, many signals can be sampled fast enough that they are naturallylow-pass filtered by the response of the sensor or by the process being measured. Forexample, temperature changes in the body occur so slowly that sampling a temperaturesensor even once per minute suffices to eliminate aliases by supersampling. Despite this,care must be taken that power line noise or other high-frequency interference does not contaminatethe sensor signal by using appropriate shielding, differential amplification, and/ora simple RC low-pass filter. A good rule of thumb to avoid aliasing when an antiliasingfilter is not used is to supersample at a sampling rate of at least 10 times the highestexpected (unfiltered) signal component.Ten times supersampling can be unachievable when your application involves theacquisition of high-frequency signals. Here, the use of antialiasing filters is unavoidable.The ideal antialias filter would be a sharp low-pass filter that passes all frequencies belowits cutoff at half the sampling frequency and totally eliminates any components above thatfrequency. As we saw in Chapter 2, however, real-world filters do not yield a perfect stepin the frequency domain, and they will always allow through some components above theircorner frequency. This means that, in practice, sampling must happen at a rate higher thantwice the filter’s cutoff frequency. Please note that the antialiasing filter must be an analogimplementation—it is too late to use digital filtering once you have done the sampling.The other common misunderstanding about the Nyquist theorem is that although itstates that all the information needed to reconstruct the signal is provided by samplingat least at twice the highest signal frequency, it does not say that the samples will looklike the signal. Figure 5.12 shows a 48-Hz signal that is sampled at 100 Hz—fast enoughaccording to Nyquist’s theorem—barely more than twice per cycle. It is clear from Figure5.12c, though, that if straight lines are drawn between the samples, the signal looksamplitude modulated (although the signal’s frequency is correctly reproduced). Thiseffect arises because each cycle is taken at a slightly different part of the original signal’scycle. Many engineers would take the modulated signal as an indication that it was sampledimproperly. On the contrary, there is enough information to reproduce the original2Most engineers have heard the term oversampling applied to data acquisition. Although it is intuitive that samplingand playing back something at a higher rate looks better than a lower rate—more points in the waveform forincreased accuracy—that’s not what oversampling usually means. In fact, oversampling usually refers to outputoversampling and it means generating more samples from a waveform that has already been digitally recorded.
SAMPLING RATE <strong>AND</strong> THE NYQUIST THEOREM 225Figure 5.12 Nyquist stated that all the information needed to reconstruct a signal is provided by sampling at twice the highest signal frequencyat least, which does not imply that the samples will look like the signal. (a) A 48-Hz signal (b) is sampled at 100 Hz (circles). (c)Simply drawing lines between the samples does not reconstruct the original signal.signal, but the correct reproduction is not achieved just by drawing straight lines betweenthe samples.The correct way of reconstructing a sampled signal is by using an interpolating filter. Thelow-pass reconstruction filter interpolates between the samples to make a smoothly varyingoutput signal. Let’s assume for a moment that the reconstruction filter is an ideal low-passfilter which has an infinitely steep cutoff. It eliminates all frequencies above the cutoff andhas no effect on either the amplitude of phase of frequencies below the cutoff. The impulseresponse of this low-pass filter is the sin function (sin x)/x. For the reconstruction, the stimulifed to this filter are the series of discrete impulses that are the original digitized samples.Every time an impulse hits the filter, it “rings”—and it is the superposition of all these peakyrings that reconstructs the proper signal. If the signal contains frequency components thatare close to one-half the sampling rate, the reconstruction filter has to be very sharp indeed.This means that it will have a very long impulse response—long enough to fill in the signaleven in region of the low-amplitude samples.Channel skew is another issue that must be considered when establishing how to sampledata. Channel skew is the undesirable effect of time-shifting sampled data points thatotherwise should be time aligned. Let’s assume that you are sampling multiple biopotentialsignals acquired from the same source through an electrode array. Take, for example,the signals displayed in Figure 1.33, which were recorded differentially using 32 surfaceelectrodes placed 2.54 mm apart over the biceps brachii muscle. A proper sampling rate forthese signals is about 10 kHz. Sequential sampling of the 32 channels would result in a
226 SIGNAL CONDITIONING, DATA ACQUISITION, <strong>AND</strong> SPECTRAL ANALYSIStime skew of 3.1 ms between the first and last channels, a situation that is intolerable formany applications. The way of eliminating time skew between channels is to sample-andholdeach channel individually at the same time. Digitization can then occur at the A/D’sleisure. Most often, however, the impact of channel skew is minimized by a techniquecalled burst sampling. Here, all EMG channels would be sampled at the maximum rate ofthe converter once every 1/10,000 of a second. Assuming the use of a 1-MHz A/D, themaximum time skew between the first and last channels drops to barely 31 µs.Channel skewing has become a very critical consideration, since multichannel recordingsenjoy wide popularity in research and diagnostic uses of electrophysiological activity.For example, 32-, 64-, and even 128-channel systems are commonly used in the acquisitionof EEG and evoked potentials; and 64-channel systems are now commercially availablefor body potential mapping (BPM) ECG.FREE DATA ACQUISITION CARD IN YOUR COMPUTERIf you need to measure one or two audio-frequency signals that do not include a dc component,don’t overlook the data-acquisition card that your PC probably has already—your PC’ssound card. Audio-range signals can be applied to a sound card via stereo 1 -in. mini jacks.8Inside the sound card, these signals are ac-coupled, with one pair of inputs being sent throughpreamplifiers for boosting low-level signals (intended to amplify microphone signals), andanother pair feeding signals within a 0.5 V p-p range directly into the card’s analog multiplexer/mixer.The input impedance of a sound card is typically above 10 kΩ, and channelstypically respond within the frequency band 20 Hz to 20 kHz. Signals at the output of themixer/multiplexer are digitized by a delta-sigma A/D that is part of the sound card’s codec IC.Consumer-grade sound cards offer 11.025-kHz (“telephone quality”), 22.05-kHz (“musicquality”), and 44.1-kHz (“CD quality”) sampling rates. Low-cost sound cards often use a singlecodec chip that is multiplexed between the two input channels, which means that thesesound cards would sample both inputs only at 22.05 kHz or lower. Better cards feature twoA/D converters or at least two sample-and-hold devices so they can sample both inputs simultaneouslyat rates up to 44 kHz. There are some “professional-quality” sound cards that featuremore input channels, higher resolution, and dc input response, but they require proprietarysoftware to operate, and their prices are similar to those of a full-function data acquisition card.Of course, the most common use for a sound card is to generate the various annoyingsounds of explosions, phasers, and kicks that make video games so realistic. The outputjack of a typical sound card carries an amplified ac-coupled signal capable of driving 8-Ωspeakers directly with some 2 W of power. Sounds are generated by using an FM synthesizerwithin the sound card to combine harmonically related sine waves or by selectingdata from a wave table that contains digitized samples from various musical instruments.A third option available on higher-end sound cards is to use an onboard musical instrumentdigital (MIDI) synthesizer to produce an even wider variety of sounds.There is quite a bit of free software available on the Web to turn a PC equipped with asound card into all sorts of audio-range virtual instruments, such as two-channel oscilloscopes,spectrum analyzers, signal generators, frequency counters, and noise generators.The following are some of the freeware packages that deserve special attention.Signal Generator• BIP Electronics Labs Sine Wave Generator v3.0 (sine30.zip, freeware for Windows3.1, but works well in most cases under Windows 9x) by Marcel Veldhuijzen• Sweep Sine Wave Generator v2.0 (swpgen20.zip, freeware for Windows 9x) byDavid Taylor
FREE DATA ACQUISITION CARD IN YOUR COMPUTER 227Audio Oscilloscopes• BIP Electronics Labs Digital Scope v3.0 (scope30.zip, freeware for Windows 3.1, butworks well in most cases under Windows 9x) by Marcel Veldhuijzen• Oscilloscope for Windows v2.51 (osc2511.zip, freeware for Windows 9x) byKonstantin ZeldovichAudio Spectrum Analyzers• Spectrogram v5.0.5, Dual Channel Audio Spectrum Analyzer (gram501.zip freewarefor Windows 9x) by Richard Horne• Audio Wavelet Analyzer v1.0 (audiowaveletanalyse.zip freeware for Windows 9x) byChristoph LauerAnother very neat thing that can be done with a sound card is to use it as the basis for atransfer-function analyzer. In essence, a full-duplex sound card can be used to generate a testsignal (e.g., a sweeping tone) that is fed to the input of a system under test. The output of thesystem is recorded by the sound card and analyzed in the context of the excitation waveform.For example, you could play back a sweeping tone through your stereo set and acquire thesound using a good microphone placed at a favorite listening spot in the room. A plot of thefrequency response of the complete system (amplifier, speakers, room acoustics, and microphone)would show distortions, room resonances, and other effects that alter the music thatyou listen to. One such software package is the RightMark Audio Analyzer v2.5 (rmaa25.zipfreeware for Windows 9x, 2000 and NT) by Alexey Lukin and Max Liadov.The flexibility and potential of a PC sound card as a simple data acquisition system hasbeen recognized by commercial software vendors, and some major data processing packages(e.g., Matlab by The MathWorks Inc.) include commands to acquire data directly intoits environment from the sound card (e.g., wavrecord.m) and output data streams as sound(e.g., wavplay.m). Interfacing a signal line to a sound card requires some experimentation.First, you will need a way of delivering the signals to the sound card’s stereo 1 -in. jack.8Avoid using premade cable splitters. Instead, build your own cables using RG-174 miniaturecoaxial cable and metal-shell 1 -in. plugs.8Next, use a good signal generator to feed a signal to the sound card. Find settings forthe generator’s output (the range is usually limited to 0.5 V p-p ) and the sound card’smixer (accessed through the speaker icon in your Windows tray) that give you a full-scaledeflection without clipping. You could use the microphone input for better sensitivity, butthe noise floor is higher, and many cards output a voltage for the microphone supply. If thatinput is used, a capacitor for blocking the microphone bias voltage is necessary.Remember that a sound card’s signal return connects to the ac power ground throughthe PC’s chassis, which opens up the possibility of introducing interference into measurementsby forming unwanted ground loops. If the input signal does not include a dc component,you can use a 1 : 1 audio transformer for signal isolation or to convert a differentialinput into the single-ended input expected by the sound card.Consider the fact that sound cards are designed to be very inexpensive, so that soundcard manufacturers do not usually spend the few extra cents necessary to include overvoltageprotection components, making sound cards vulnerable to destructive overloads.In addition, older sound cards sometimes include permanently enabled automatic gaincontrol (AGC), which can produce misleading measurements because it compresses signalpeaks. Finally, since our ears don’t care much about a compressive versus an expansivewaveform, signals may be inverted by the sound card when acquired. The best adviceis that you should always use a real oscilloscope to compare the input signal against thesignal acquired by the sound card before you trust the acquisition setup.
228 SIGNAL CONDITIONING, DATA ACQUISITION, <strong>AND</strong> SPECTRAL ANALYSISConverting the Sound Card into a Precision DC-Coupled A/DSound cards suffer serious limitations when used for acquiring physiological signals; forone, typical PC sound cards are ac coupled through series capacitors on the signal path.Typical high-pass cutoff frequencies are above 20 Hz, making it impossible to record waveformscontaining dc or low-frequency components, a characteristic shared by most biopotentialand physiological signals. Furthermore, consumer-grade sound cards often exhibitpoor sound-recording quality characteristics, especially a lack of passband flatness andharmonic generation, which results in signal distortion.However, a voltage-controlled oscillator (VCO) and some software can turn a soundcard into a precision dc-coupled A/D. The VCO of Figure 5.13 generates an audio tonethat varies in frequency as a function of a control signal input. The VCO’s output is awhistling sound that is easily recorded even with low-end sound cards. The original signalis then recovered by software FM demodulation of the VCO audio recorded. IC3 isan Exar XR-2206 function generator that implements the VCO. The carrier frequency (inhertz) is given by 1/(R13 R14)C4. Good performance is achieved with most soundcards by setting the carrier frequency somewhere in the range 2 to 10 kHz. The frequencyof oscillation is modulated by applying a control current in the 3 mA range to pin 7,which is biased within the XR-2206 at 3 V. R16 sets the offset voltage of IC2A suchthat zero control voltage applied to IC2B results in zero current across R15 and R18. R18adjusts the modulation level (frequency deviation per volt). A good range for most soundcards is around 80% of the carrier for the full-control voltage input range. The soundcard sampling rate should be selected to be at least five times higher than the highest VCOfrequency expected.R6 and R7 are used to trim the harmonic distortion of IC3’s sinusoidal output. Theunadjusted distortion is specified to be 2.5%, so R4, R6, R7, and R9 are optional. R3should be adjusted together with the sound card’s slider volume control to produce aclean-sounding tone. Please note that the stability of the VCO circuit depends on thestability of the frequency-setting components. Proper performance requires the use oflow-temperature-coefficient, high-tolerance components. Resistors should be precision1% tolerance type of the RN60D variety. Capacitors should be Mylar, polyester film,or other types that remain stable with age and which are not sensitive to temperaturevariations.The following Matlab code shows how easy it is to obtain digitized data (vector x) fromthe VCO audio (vector y):Fc 2144; % Select VCO carrier frequencyvcok 0.176; % Select VCO constantFs 40000; % Select sound card sampling frequencysamptime 3; % Select sampling time (in seconds)y wavrecord (samptime*Fs, Fs, ‘double’); % Sample sound into ywavplay(y, Fs); % Play the recorded soundx (demod(y,Fc,Fs,‘fm’,vcok)); % FM demodulate the soundcutoff100/(Fs/2); % Cutoff frequency for post-demodulator low-pass filterin radians/s is desired cutoff/(1/2 sampling frequency)[b,a] butter(4,cutoff); % Design Butterworth low-pass filterxfilt filter(b,a,x); % Filter demodulated signaltime 1/Fs:(1/Fs):samptime; % Generate time vectorplot(time,xfilt) % Plot filtered data vs timegrid % Overlay grid on plotxlabel(‘time [s]’) % Label x axisylabel(‘Input [Volts]’) % Label y axis
OUTOUTGNDTOSOUNDCARDR1C110kR21000.1uFAMPLITUDEADJUSTR350k+12V+12VR51M+ C210uF<strong>OF</strong>FSETADJUSTR8100kR105.1kC30.01uFC40.01uF123467XR-2206AM INOUTPUTMULT OUTVCCTC1TC2TR1SYMETRY ADJ 2SYMETRY ADJ 1WAVE ADJ 2WAVE ADJ 1GNDSYNC OUTBIASTR2 FSK IN155 128SINESYMETRYADJUST16141311109+C510uFR41kR625kR9 300R71kSINEDISTORTIONADJUSTIC178L05IN OUTR221MR2168kIC3R151kREFC80.1uF56+-+12V84R1610k~3VIC2BTL0827R1768kR2068kR1968k32+-+12V84-12V+ C610uF1IC2ATL082R115.1kR1230kR18100kMODULATIONADJUSTR139kR141MCARRIERFREQUENCYADJUST+12VC90.1uFC11+10uFC100.1uFC12+10uF-12V-12VFigure 5.13 A VCO and some software can turn a sound card into a precision dc-coupled A/D. IC3 is a VCO that generates an audio tonethat varies in frequency as a function of a control signal input. The original signal is then recovered by software FM demodulation of theVCO audio recorded.C70.1uF+12VININPUTINGND229
230 SIGNAL CONDITIONING, DATA ACQUISITION, <strong>AND</strong> SPECTRAL ANALYSISYou can use the following Matlab command to look at the actual frequency shift anddistortion of the VCO signal sampled through the sound card:specgram(y,512,Fs,kaiser(256,5),220)If you are not a Matlab user, here is how you can write a program to determine theinstantaneous frequency (or phase) of the sampled VCO output:1. Transform the incoming signal to a complex data stream using a Hilbert transform. 3This gives I (in-phase) and Q (quadrature-phase) data. A true Hilbert transform isunrealizable, but you can get excellent approximations with FIR or IIR filters. A thoroughdescription of how to implement the discrete Hilbert transform is available inP. A. Regalia, Special Filter Designs, in S. K. Mitra and J. F. Kaiser (eds.), Handbookfor Digital Signal Processing, Wiley, New York, 1993.2. Pass these complex samples through a polar discriminator (i.e., multiply the newcomplex sample by the conjugate of the old sample).3. The output is the phase difference vector from the two samples.4. Compute arctan(Q/I) to get the phase angle of the vector. You can use an easy polynomialfit, Taylor series, or lookup table to estimate the arctan() function in orderto extract the phase angle.Figure 5.14 displays a signal acquired through this method. The artificial ECG test signalwas generated by an Agilent 33120A ARB. Note that the demodulated signal faithfullyreproduces the dc offset and low-frequency components of the ECG.Since the VCO output is in the audible range, the modulated signal can be transmitted tothe sound card via a voice radio or telephonic link for remote data acquisition. This is theprinciple of ECG transtelephonic monitoring, a common technique used to follow up pacemakerpatients using a transmitter such as that of Figure 5.15. To do so, however, the tonefrequencies produced by the VCO for a full-scale input must be limited within the bandpassof the communications channel. For a plain telephone line, this range is 400 Hz to 3 kHz,while a commercial FM audio link is specified to cover the audio bandwidth 30 Hz to15 kHz. Another interesting possibility is to use a small 1 : 1 audio isolation transformer anda floating power supply to turn the VCO into an isolated data acquisition front end.It should be noted that the full bandwidth of a single sound card channel can be sharedby multiple VCOs occupying separate audio bands to convey various simultaneous lowfrequencysignals to an array of software bandpass filters and demodulators. This is exactlywhat FM telemetry systems do, and the U.S. Army’s Inter-Range Instrumentation Groupof the Range Commanders Council (IRIG) has established a standard (IRIG-106-96) thatcovers all aspects of frequency modulation (FM) and pulse code modulation (PCM) telemetry,including transmitters, receivers, and tape recorders. Owing to its success as a provenstandard and its wide support by telemetry equipment manufacturers, most commercialdata acquisition systems use the same IRIG standard channels.The IRIG standard specifies ways of performing frequency-division multiplexing (FDM)over a telemetry channel, that is, how to generate a composite signal consisting of a groupof subcarriers arranged so that their frequencies do not overlap or interfere with each other.Various FM subcarrier and deviation schemes are available to accommodate different3The Hilbert transform is a mathematical operation that decomposes a waveform into an instantaneous phase andan instantaneous amplitude waveform. If the input is a pure sine wave, the output instantaneous amplitude waveformwill have a constant value while the phase will increase linearly over time. If the sine wave were amplitudemodulated, the instantaneous amplitude waveform would show this modulation. Similarly, frequency modulationwill affect the instantaneous phase waveform.
FREE DATA ACQUISITION CARD IN YOUR COMPUTER 231Figure 5.14 An artificial ECG test signal generated by an Agilent 33120A ARB was acquired using the circuit of Figure 5.13 and a softwareFM demodulator. Note that the demodulated signal faithfully reproduces the dc offset and low-frequency components of the ECG.channel needs. For example, Table 5.4 shows some of the IRIG subcarrier frequencies andFM deviations used to yield channels whose bandwidths are constant and independent oftheir carrier frequency. On the other hand, Table 5.5 shows some choices for subcarrier frequenciesand deviations which result in channels where their bandwidth is proportional totheir carrier frequency. For a consumer-grade sound card, the maximum sampling rate is44.1 kHz, which imposes an absolute maximum tone frequency limit of around 18 kHz,which ultimately constrains the number of channels that can be sampled simultaneouslywith the FM carrier technique.IRIG publications can be ordered from:Defense Technical Information CenterAttn: DTIC-OCPJohn J. Kingman Road, Suite 0944Fort Belvoir, VA 22060-6218(703) 767-8019(703) 767-8032 (fax)The complete VCO circuit of Figure 5.13 (one channel) can be built for under $10. However,if you have a cost-sensitive application that can tolerate somewhat lower precision and
232 SIGNAL CONDITIONING, DATA ACQUISITION, <strong>AND</strong> SPECTRAL ANALYSISFigure 5.15 A transtelephonic ECG monitor provides a simple, effective solution for monitoringpacemaker patients from the comfort of their home. To transmit real-time ECGs, the patientsimply dials the receiving center and places the telephone handset on the transmitter’s cradle.These monitors typically use a center frequency of 1965 Hz with a deviation of 100 Hz/mV to conveya 0.5 to 100 Hz ECG signal detected through three chest electrodes that are dampened withwater.linearity, you may design a simpler VCO using two op-amps or a 555 timer IC to producea square or pulsed output. Straightforward FM demodulation should not be used for thesewaveforms. Rather, a pulse-width or pulse-position demodulator should be used. TheMatlab demodulation command (demod.m) can be told to use these demodulation methodssimply by replacing ‘fm’ for ‘pwm’ or ‘ppm’ in its argument line.If your application requires remote acquisition with transmission of the modulated tonevia voice link, don’t do it with a pulsed waveform, since these are distorted significantlyby telephone lines and do not properly modulate conventional voice transmitters. If usinga VCO with sine-wave output (e.g., the XR-2206, Intersil’s ICL8038, or Maxim’s MAX038)is still out of the question, you can convert a frequency-modulated pulse train into a quasisinusoidaltone using the circuit [Allen, 1981] of Figure 5.16. A 4018 Johnson counter iswired to sequence resistors R1–R5 to produce a 10-step staircase waveform that approximatesthe shape of a sine wave. The sharp edges of the staircase are removed using a simpleRC low-pass filter formed by R6 and C4 before they are attenuated by R7 and ac-coupledby C5 so they can be fed to the microphone input of a telephone or voice transmitter. Sincethe square-to-sine converter divides the input frequency by 10, the VCO should be madeto output at a frequency range that is 10 times higher than the sinusoidal tone audio rangerequired.
SPECTRAL ANALYSIS 233TABLE 5.4 Some Center Frequencies and FrequencyDeviations Specified by IRIG to Yield Constant-BandwidthChannels for Acquisition through FM SubcarriersFrequency Deviation and NominalFrequency Response per Channel2 kHz 4 kHz 8 kHz 16 kHz 32 kHz400 Hz 800 Hz 1.6 kHz 3.2 kHz 6.4 kHzChannel Center Frequency (kHz)8 16 32 64 12816 32 64 128 25624 48 96 192 38432 64 128 256 512TABLE 5.5 Many Channels of Differing Bandwidth Can Be Accommodated by Selecting Channel BandwidthsProportional to Their Carrier Frequencies aIRIG Proportional Center Lower Deviation Upper Deviation Channel’s NominalBandwidth Channel Frequency Limit Limit Bandwidth Frequency Response7.5% Deviation Channels1 400 370 430 60 62 560 518 602 84 83 730 675 785 110 114 960 888 1,032 144 145 1,300 1,202 1,398 196 206 1,700 1,572 1,828 256 257 2,300 2,127 2,473 346 358 3,000 2,775 3,225 450 459 3,900 3,607 4,193 586 5910 5,400 4,995 5,805 810 8111 7,350 6,799 7,901 1,102 11012 10,500 9,712 11,288 1,576 16013 14,500 13,412 15,588 2,176 220aThese IRIG channels are useful for acquiring multiple physiological signals with different bandwidth requirements. For example, the subject’sskin conductance signal fits well within the 11-Hz bandwidth of channel 3, the 45-Hz bandwidth of channel 8 could accommodate anEEG channel, and a three-lead wideband ECG can be acquired through channels 11, 12, and 13.SPECTRAL ANALYSISThe analysis of a signal based on its frequency content is commonly referred to as spectralanalysis. Because of the rhythmic nature of practically every phenomenon in a livingbody, frequency-domain analysis is one of the most powerful tools in the examination ofphysiological signals. The mathematical basis for this operation, the Fourier transform, hasbeen known for many years, but it was the introduction of the fast Fourier transform (FFT)algorithm that made spectral analysis a practical reality. Implementing the FFT in personalcomputers and embedded DSP systems has allowed efficient and economical applicationof Fourier techniques to a wide variety of measurement and analysis tasks. Moreover,because the FFT has been found to be so valuable in applications such as medical signalprocessing, radar, and telecommunications, DSP chips are often designed to implement itwith the greatest efficiency.
+C110uFC20.1uFR1100k+12VR2C30.01uFIC1162379 I1I2I312 I4I514CLK110 D15 PRERSTQ1Q2Q3Q4Q5546111339kR330kR439k1/10 inputfrequencyGNDVCC40188R5100kR647kC4.005uFR7100kC50.22uFOUT TOOUTGNDMICROPHONEINPUTFigure 5.16 A 4018 Johnson counter can be made to convert a frequency-modulated pulse train into a quasi-sinusoidal tone for remotedata acquisition. IC1 is wired to sequence resistors R1–R5 to produce a 10-step staircase waveform that approximates the shape of a sinewave. Since the square-to-sine converter divides the input frequency by 10, the input frequency range should be 10 times higher than therequired sinusoidal tone audio range.INPUTFROMVCOININGND234
SPECTRAL ANALYSIS 235In most instances, the powerful Fourier techniques used in EEG systems and CT or ultrasoundscanners are hidden from the user, who does not have to worry about their mathematicalimplications. In other cases, however, human interpreters must make diagnosticdecisions based on frequency-domain representations of data processed through Fouriertransforms. For example, many digital storage oscilloscopes offer the user the option to converttime-domain signals into the frequency domain through the use of an FFT running onan embedded DSP that displays the results directly on screen. It is also common for scientistsand engineers to write short FFT-based routines to display a spectral representation ofexperimental data acquired into a personal computer. It is in these cases where the unwarymay fall into one of the many traps that FFTs conceal.FFT users often forget that real-world signals are seldom periodic, free of noise, anddistortion, and that signal and noise statistics play an important role in their analysis. Becauseof this, FFTs and other methods can only provide estimates of the actual spectrum of signals,which require competent interpretation by the user for their correct analysis. Moreover, theFFT has certain inherent problems that make it unsuitable for high-resolution applications.FFTs and the Power Spectral DensityUsing a typical data acquisition setup, a signal is sampled at a fixed rate of f S (samples/s), whichyields discrete data samples x 0 , x 1 , ..., x N1 . These N samples are then spaced equally by thediscrete sampling period ∆t(s) 1/f S . The discrete Fourier transform (DFT) represents thetime-domain data with N spaced samples in the frequency domain X 0 , X 1 , ..., X N1 throughN1X( f ) ∆t x n e 2πjf n ∆tn0where the frequency f(Hz) is defined over the interval ∆t/2 f ∆t/2. The FFT willefficiently evaluate this expression at a discrete set of N frequencies spaced equally by∆ f (Hz) 1/N ∆t.In its simplest form, the energy spectral density estimate of the time-domain data isgiven by the squared modulus of the FFT of these data, and the power spectral density(PSD) estimate P( f ) (or simply, the spectrum) at every discrete frequency f is obtained bydividing the latter by the time interval N ∆t:P( f m ) X m∆ 2 m 0,1,...,N 1N twhere f m (Hz) m ∆f. When real data are used (usually, the case when sampling from realworldsignals), the PSD for negative frequencies will be symmetrical to the PSD for positivefrequencies, making only half of the PSD useful. However, at times it may benecessary to compute the PSD for complex data, and relevant results will be obtained forboth positive and negative frequencies.Although obtaining the PSD seems to be as simple as computing the FFT and obtainingthe square modulus of the results, it must be noted that because the data set employedto obtain the Fourier transform is only a limited record of the actual data series, the PSDobtained is only an estimate of the true PSD. Moreover, as will be seen later, meaninglessspectral estimates may be obtained by using the estimate of P( f m ) without performingsome type of statistical averaging of the PSD.Pitfalls of the FFTWhen sampling a continuous signal, information may be lost because no data are availablebetween the sample points. As the sampling rate is increased, a larger portion of the
236 SIGNAL CONDITIONING, DATA ACQUISITION, <strong>AND</strong> SPECTRAL ANALYSISinformation is made available. We explained above that according to Nyquist’s theoremthe bare minimum sampling rate to avoid aliasing must be at least twice that of the highest-frequencycomponent of the waveform. Because aliased components cannot be distinguishedfrom real signals after sampling, aliasing is not just a minor source of error. Itis therefore of extreme importance that antialiasing filters with very high roll-off be usedfor all serious spectral analysis.Beyond appropriate sampling practices, the FFT still exposes other inherent traps whichcan potentially make impossible the analysis of a signal. The most important of these problemsare leakage and the picket-fence effect. The first problem is caused by the fact thatthe FFT works on a short portion of the signal. This is called windowing because the FFTcan only see the portion of the signal that falls within its sampling “window,” after whichthe FFT assumes that windowed data repeat themselves indefinitely. However, as shown inFigure 5.17, this assumption is seldom correct, and in most cases the FFT analyzes a distortedversion of the signal that contains discontinuities resulting from appending windoweddata to their duplicates. In the PSD, these discontinuities appear as leakage of theenergy of the real frequency components into sidelobes that show up at either side of apeak.The second problem, called the picket-fence effect or scalloping, is related inherently tothe discrete nature of the DFT. That is, the DFT will calculate the frequency content of asignal at very well defined discrete points in the frequency domain rather than producinga continuous spectrum. Now, assuming a perfect system, if a certain component of the signalwould have a frequency that falls between the discrete frequencies computed by theDFT, this component would not appear in the estimated PSD.To visualize this problem, suppose that an ideal signal is sampled at a rate of 2048 Hzand processed through a 256-point FFT. There will then be a spectral channel every 4 Hz:at dc, 4 Hz, 8 Hz, 12 Hz, and so on. Now suppose that the signal being analyzed is a pureFigure 5.17 A purely sinusoidal signal (a) has a single impulse as its true spectrum (b). However,the signal is viewed by the FFT through a finite window (c), and it is assumed that this record isrepeated beyond the FFT’s window (d). This leads to leakage of the main lobe to sidelobes in thespectral estimate (e).
w n x n e 2πjf n ∆t X( f ) ∆t N1SPECTRAL ANALYSIS 237TABLE 5.6 Typical Window Functions for Use with the FFT in Spectral Estimation3-dB Bandwidth Scallop Loss HighestWindow a (bins) (dB) Sidelobe (dB)Rectangular1 for Nw(n) 2 n N 2 10 for all other0.89 3.92 13Triangularw(n) 1 2n 1 for N N2 n N 2 10for all other1.28 1.82 27Hamming0.54 0.46 cos 2 π(2n 1) for N 2(N 1)2 n N 2 1w(n)0for all other1.30 1.78 43Hanning0.5 0.5 cos 2 π(2n 1) for N w(n) 2(N 1)2 n N 2 10for all other1.44 1.42 32aWindows are N-point long and are assumed here to be symmetric around n 0.sinusoidal with a frequency of 10 Hz. In a perfect system, this signal would not appear inthe PSD because it falls between two discrete frequency channels, much as a picket fenceallows us to see details in the scene behind it only if they happen to fall within a slotbetween the boards. In reality, however, because the FFT produces slightly overlapping“bins” of finite bandwidth, components with frequencies that fall between the theoreticaldiscrete lines are distributed among adjacent bins, but at reduced magnitudes. This attenuationis the actual picket-fence or scalloping error.Both of these problems are somewhat corrected by the use of an appropriate window. Sofar, all samples presented to the FFT have been considered equal, which means that a weightof 1 has been applied implicitly to all samples. The samples outside the FFT’s scope are notconsidered, and thus their effective weight is zero, resulting in a “rectangular”-shaped window.This ultimately leads to discontinuities that cause leakage. A number of windows havebeen devised that reduce the amplitude of samples at the edges of the window, whileincrease the relevance of samples toward its center. By doing so, these windows reduce thediscontinuity to zero, thus lowering the amplitude of the sidelobes that surround a peak inthe PSD. In addition, use of a nonrectangular window increases the bandwidth of each bin,which results in a decreased scalloping error.Some typical window functions and their characteristics are presented in Table 5.6. Inessence, these functions produce N weights w 0 , w 1 , ..., w N-1 which are weighted (multiplied)one to one with their corresponding data samples x 0 , x 1 , ..., x N-1 before subjectingthem to an FFT:n0
238 SIGNAL CONDITIONING, DATA ACQUISITION, <strong>AND</strong> SPECTRAL ANALYSISThe price paid for a reduction in leakage and scalloping through the use of a nonrectangularwindow is reduced resolution. In fact, if it is necessary to view two closely spacedpeaks, the rectangular window’s narrow main lobe will allow the user to obtain analysisresults that report the existence of these closely spaced components, whereas any of theother windows would end up fusing these two peaks into a single smooth crest.Use of a rectangular window is also appropriate for the analysis of transients. In thesecases, zero signal usually precedes and succeeds the transient. Thus, if the FFT is made tolook at the complete data record for the transient, no artificial discontinuities are introduced,and full resolution can be obtained without leakage. As you may well see, there isno single window that outperforms all others in every respect, and it is safe to say thatselecting the appropriate window for a specific application is more of an art than an exactscience.When the signal rides on a relatively high dc level or on a strong sinusoidal signal, it isadvisable to remove these components from the data before the PSD is estimated, becauseotherwise the biasing and strong sidelobes produced by them could easily obscure weakercomponents. Whenever expected physically, the dc component of a signal can usually beremoved by subtracting the sampled data mean x (1/N) N1 xn0n from each data sample toproduce a “purely ac” data sequence x 0 x, x 1 x, ..., x N1 x.Zero-Padding an FFTAn interesting property of the FFT is that simply adding zeros after a windowed data samplesequence x 0 , x 1 , ..., x N1 in order to create a longer record x 0 , x 1 , ..., x N1 ,0,0,...,0before performing an FFT will cause the FFT to interpolate transform values between the Noriginal transform values. This process, called zero padding, is often mistakenly thought ofas a trick to improve the inherent resolution of an FFT. Zero padding will also provide amuch smoother PSD and will help annul ambiguities regarding the power and location ofpeaks that may be scalloped by the non-zero-padded FFT.Classical MethodsAs mentioned before, a common mistake is to assume that the solution to P( f m ) X m 2 /N ∆t, m 0, 1, ..., N 1, the periodogram, is a reliable estimate of the PSD. Actualproof of this is beyond the scope of the book, but it has been demonstrated that regardlessof how large N (the number of available data samples) is, the statistical variance of the estimatedperiodogram spectrum does not tend to zero. This statistical inconsistency is responsiblefor the lack of reliability of the periodogram as a spectral estimator.The solution to this problem is simple, however. If a number of periodograms are computedfor different segments of a data record, their average results in a PSD estimate withgood statistical consistency. Based on this, Welch [1967] proposed a simple method todetermine the average of a number of periodograms computed from overlapping segmentsof the data record available. Welch’s PSD estimate P^( f ) of M data samples is the averageof K periodograms P( f ) of N points each:1P^( f ) K KP( f )where the P( f )’s are obtained by applying P( f m ) X m 2 /N ∆t, m 0, 1, ..., N 1toappropriately weighted data. It is obvious that if the original M-point data record is dividedinto segments of N points each, with a shift of S samples between adjacent segments, thenumber of periodograms that can be averaged isi1K integer M NS 1
SPECTRAL ANALYSIS 239High-Resolution MethodsThe main limitation of FFT-based methods is restricted spectral resolution. The highestinherent spectral resolution (in hertz) possible with the FFT is approximately equal to thereciprocal of the time interval (in seconds) over which data for the FFT are acquired. Thislimitation, which is further complicated by leakage and the picket-fence effect, is mostnoticeable when analyzing short data records.It is important to note that short data records not only result because of the lack of data,such as when sampling a short transient at a rate barely enough to satisfy Nyquist’s criterion,but also from data sampled from a process that varies slowly with time. Although there aremany applications in the medical field, the best example comes from the oil field. By analyzingthe vibrations picked up from an oil-well drill, the operator can monitor the buildupof resonance in the long pipe that carries torque to the drill bit, avoiding costly damages tothe equipment [Jangi and Jain, 1991]. Although a continuous signal from the vibration transducersis available for sampling, the vibrations on the drill assembly change rapidly, resultingin a limited number of data samples which represent each state of the drill bit. It is herethat high-resolution estimates would be desirable, even though the data available are limited.A number of high-resolution spectral estimators have been proposed. These alternativemethods do not assume, as the FFT does, that the signal outside the observation windowis merely a periodic replica of what is observed through the window. For example, one ofthese methods, the parametric estimator, relies on the selection of a model that suitablyrepresents the process that generates the signal in order to capture the true characteristicsof data outside the window. By determining the model’s parameters, the theoretical PSDimplied by the model can be calculated and should represent the signal’s PSD.Many signals encountered in real-world applications are well approximated by arational transfer function model. For example, human speech can be characterized by theresonances of the vocal tract that generate it. These resonances, in turn, are well representedby the poles of a digital filter. Parameters for the filter can then be estimated, suchthat the filter would turn a white noise input into the signal of interest, and from the filter’stransfer function we could easily estimate the PSD of the signal.Various kinds of filter structures exist, and they are often classified according to the typeof transfer function that they implement. An all-pole filter is called an autoregressive (AR)model, an all-zero filter is a moving-average (MA) model, and the general case of a pole–zero filter is called an autoregressive-moving-average (ARMA) model. Using the pastexample, the model best suited for speech is then an AR model. Although high-resolutionestimators have been implemented for all these models, AR model-based estimators are themost popular because many computationally efficient algorithms are available. A wellbehavedset of equations to determine the AR parameters with a computationally efficientalgorithm has been introduced by Marple [1987].In the model of Figure 5.18, the AR filter coefficients a 0 , a 1 , ..., a p are estimated byMarple’s algorithm based on the input data samples x 0 , x 1 , ..., x N-1 . The model assumesthat a white-noise source drives the filter, in which the output is regressed (thus the nameautoregressive) through a chain of delay elements z 1 , from which p taps feed the ARcoefficients. The system’s transfer function can then be computed efficiently through theFFT, resulting in an estimate of the signal’s PSD. The performance of Marple’s estimatoris startling. Figure 5.19b presents three spectral estimates obtained from a short 64-pointcomplex test data set suggested by Marple. Estimates obtained through the zero-paddedFFT periodogram, Welch’s averaged periodogram, and Marple’s method can be comparedto the theoretical spectrum of Figure 5.19a. Only positive-frequency PSD estimates areshown for clarity.Notice that the closely spaced components cannot be resolved by either of the classicalmethods, but they appear clearly separated in the estimate produced by Marple’s method.
240 SIGNAL CONDITIONING, DATA ACQUISITION, <strong>AND</strong> SPECTRAL ANALYSISFigure 5.18 In one implementation of a parametric high-resolution spectral estimator, the coefficients a 0 , a 1 , ..., a p of an AR filter aredetermined from input data through Marple’s algorithm. The transfer function of the filter is then evaluated efficiently by the FFT, resultingin a high-resolution estimate of the input data’s PSD.You may also notice that Marple’s estimate is “peaky” even for the smooth continuousspectral components at the far right and far left of the PSD. The reason for this is that apurely autoregressive filter will generate a spectrum based on pure resonances, and onlythrough use of a moving average could these resonances be damped to produce a perfectlysmooth spectrum in regions where this is necessary. Although this limitation of AR-basedestimators would lead to errors in the actual amplitudes of the PSD components, it is verywell suited for high-resolution detection of periodicities in the signal.A price must be paid for the increase in resolution, and just as you might suspect, thecomputational burden of these high-resolution methods far exceeds that for a simple FFT. Inaddition, like the selection of an appropriate window for the classical estimators, the rules forselecting an appropriate model, parameter estimation method, and model order are essentiallyinflexible.Implementing Spectral Analysis AlgorithmsProgram SPECTRUM.BAS at the Wiley ftp site for this book demonstrates implementationof the spectral estimation methods discussed above. The program was written inQuickBasic 4.5, but should run with little trouble under any other Basic compiler onany PC. The FFT, as well as Welch’s averaged periodogram and the AR spectral estimationroutines, are based on the Fortran programs that accompany Marple’s book.However, Basic does not support complex-number arithmetic, so explicit operationshave been used in which variable names with the suffix “r” represent the real portion ofthat variable, and those with the suffix “i” represent the imaginary portion of the same.The ftp site also includes a version of this program (LPT8SPEC8.BAS) that acquiresevenly sampled data through the Universal Sensor Interface described above and thendisplays the spectrum estimated via the zero-padded FFT, an averaged-periodogram
SPECTRAL ANALYSIS 241Figure 5.19 Positive-frequency spectral estimates for Marple’s 64-point complex data test set:(a) theoretical spectrum; (b) spectrum estimated using three different methods: (i) zero-paddedFFT periodogram (medium line); (ii) Welch’s method (bold line, N 32, S 16); (iii) Marple’smethod (thin line, p 15).
242 SIGNAL CONDITIONING, DATA ACQUISITION, <strong>AND</strong> SPECTRAL ANALYSISmethod (Welch’s estimator), and a parametric estimator (Marple’s autoregressivemethod).After being defined by the user, the program will read a file containing the N-data-pointsequence to be analyzed. These data can be either a single column of (plain ASCII)samples, or two columns, one containing the real and the other the imaginary parts of complexdata samples. The program will estimate the spectrum of the input data using threemethods:1. A single periodogram of the data record is obtained by zero-padding the data upto npsd data points (npsd 512 for complex data, 1024 for real input data), fromwhich the squared modulus of the FFT is computed. A rectangular window isassumed.2. Welch’s method with a Hamming window is applied using the number of samplesper periodogram and the shift specified by the user.3. Marple’s method is used to estimate the PSD of the data using an AR model withmodel order given by the user.Prior to its display in the output screen, the PSD is normalized relative to its maximum, andtransformed to decibels. For complex input data, both the positive- and negative-frequencysides of the spectrum are plotted. Otherwise, only the positive-frequency spectrum is presented.Because of screen resolution limitations, the number of PSD points computed for displayhas been limited to 512. If a larger PSD record is required, however, npsd can beincreased to any desired power of 2, and a file can be opened to receive the estimated PSDresults.A few simple demonstrations can be set up to compare the performance of the methods.First, you may generate a data file for a signal consisting of a single sinusoid at f s /4 withwhite noise added to it throughpi 3.14159262OPEN “noise.dat” FOR OUTPUT AS #1FOR i 1 TO 256x 2 * (RND .5) (SIN(2 * pi * i / 4))PRINT #1, xNEXT iCLOSE #1You may vary the signal-to-noise ratio by changing the value of the coefficient of thenoise component. You may also vary the frequency of the sinusoidal component by changingthe denominator of the sine’s argument. Of course, from Nyquist’s theorem, a denominatorsmaller than 2 will produce an aliased signal, and you may want to experiment withthe effect that this has on the PSD estimate. In addition, the resolving power of the estimatorsmay be compared by using a signal containing two closely separated sinusoidalcomponents. This can be accomplished by adding the second component to the programline that computes x: for example,x 2*(RND .5) (SIN(2*pi*i/4)) (SIN(2*pi*i/4.1))Regarding the AR model order that you should use, a rule of thumb that often helps is tokeep it smaller that one-third of the number of data samples available and to allow for atleast twice the number of spectral components expected. SPECTRUM.BAS will announcean error whenever mathematical ill-conditioning is encountered due to too-high a model
SPECTRAL ANALYSIS 243order, but an unreasonably “peaky” spectrum is often obtained before ill-conditioning canbe detected.Array Signal ProcessingThe greatest interest in high-resolution spectral estimators has been generated in the field ofarray signal processing. Here, a number of sensors are placed at various locations in spaceto detect traveling waves. For example, in seismology, a number of sensors capable ofdetecting the shock waves of a tremor or earthquake are spread over a certain area. As theshock waves travel under the sensor array, signals from each sensor can be sampled alongtime, producing a data record which also contains information regarding the spatial characteristicsof the waves (because the sensor locations are known). The processing of resultingspatiotemporal data is meant to estimate the number, vector velocity (speed and direction),and waveshape of the overlapping traveling waves in the presence of interference and noise.Array signal processing has been applied successfully to biomedical diagnosis and has beenused to track weak electrical potentials from the brain, nerves, and muscles. Other applicationsinvolve image reconstruction from projections, such as MRI and medical tomography.The most common form of traveling wave is the plane wave. In its simplest form, aplane wave is a sinusoidal wave that not only propagates through time t but also throughspace. In the direction of propagation r, this wave can be represented byg(t, r) A sin 2π ft r vwhere A is the amplitude of the wave, f its temporal frequency (in hertz 1/s), and v thevelocity (in m/s or any other suitable velocity units) at which the wave propagates throughspace.If one such simple plane wave is sampled discretely along time and space, we wouldobtain a record similar to that presented on the left side of Figure 5.20a. As you may wellsee, at any given time the spatial sampling of the wave will also form into a sinusoid withfrequency k 1 . The spatial frequency (in 1/m) of such a simple plane wave, called thewavenumber, is given by k f/v. Its physical meaning indicates that at a distance r fromthe origin, the phase of the wave accumulates by 2πkr radians.The two-dimensional spectrum of the plane wave in our example would be an impulseδ (the spectrum of a sinusoid) located in the frequency–wavenumber ( f–k) plane at f 1 , k 1 .Through this type of spectral analysis we can infer not only the components of the waveformbut also their velocity, because the slope at which the components are found is equal totheir propagation velocity. In this case, v 1 (m/s) f 1 (1/s)/k 1 (1/m).By adding a second component with a different frequency and propagation velocity(Figure 5.20b) to the original component, we obtain a plane wave (Figure 5.20c) thatregardless of its simplicity, can hardly be recognized in the space-time domain. However,the two-dimensional frequency–wavenumber spectrum of the signal clearly resolves thecomponents and their propagation velocities.The two-dimensional spectrum can be computed with ease knowing that the twodimensionalDFT is computable as a sequence of one-dimensional DFTs of the columnsof the data array, followed by a sequence of one-dimensional DFTs of the rows of this newarray, or vice versa. As such, the simplest two-dimensional PSD estimator is implementedthrough the FFT. In practice, however, due to the limited number of spatial samples(because only a few sensors are normally used), high-resolution estimators must be used.Since enough samples x 0 , x 1 , ..., x N1 can usually be obtained from each of the R sensorsthrough time, a hybrid two-dimensional spectral estimator can be implemented by combining
244 SIGNAL CONDITIONING, DATA ACQUISITION, <strong>AND</strong> SPECTRAL ANALYSISFigure 5.20 Frequency–wavenumber spectra of plane waves: (a) spatiotemporal (left) andfrequency–wavenumber (right) representations of a sinusoidal wave of frequency f 1 traveling atpropagation velocity v 1 ; (b) sinusoidal wave of frequency f 2 traveling at propagation velocity v 2 ; (c)sum of the above. The two-dimensional PSDs clearly show the component waveform spectra andpropagation velocity.the classical and high-resolution spectral estimation approaches. As shown in Figure 5.21,using spatiotemporal data g(t,r),g(t, r) x 0,0x 0,1...x 0, R1x 1,0x 1,1...x 1, R1………x N1,0x N1,1...x N1, R1
SPECTRAL ANALYSIS 245Figure 5.21 A hybrid two-dimensional spectral estimator: Spatiotemporal data (a) are transformed along the time domain into an intermediatearray (b) through the application of a windowed FFT to every row of the original data. Applying an AR PSD estimator to every columnof the intermediate array completes the two-dimensional PSD estimation process (c). [Reprinted from Med. Eng. Phys., 17, D. Prutchi,A High-Resolution Large Array (HRLA) Surface EMG System, pages 442–454, 1995, with permission from Elsevier.]an intermediate transform G int ( f, r) is computed by applying the FFT along each row (timedomain) of appropriately weighted data. The two-dimensional spectral estimate G( f, k) isthen completed by obtaining the AR-PSD of each column of complex numbers in the intermediatetransform. In the more general case, using an array of sensors spread out over anarea, and with a plane wave traveling in any direction under the array, a three-dimensionalhybrid spectral estimator can determine not only the wave’s components and their velocitiesbut also each component’s bearing.A practical example of the use of this method is the analysis of biopotentials that canbe picked up from skeletal muscle fibers using electrodes attached to the skin [Prutchi,1994, 1995]. These biopotentials are caused by the sum of currents from action potentialsthat travel down individual muscle fibers responsible for the contraction of muscles. Theconduction velocity, as well as the origin of these potentials, contains a wealth of informationthat can be used, for example, as an aid in the early diagnosis of nerve and musclediseases. The large number of convoluted signals and the very small differences betweentheir waveforms make it impossible to determine this information from spatiotemporaldata (Figure 5.22b) recorded differentially using 32 surface electrodes placed 2.54 mm
246 SIGNAL CONDITIONING, DATA ACQUISITION, <strong>AND</strong> SPECTRAL ANALYSISFigure 5.22 Frequency–wavenumber spectral estimation has been applied to analysis of the biopotentials recorded from a muscle twitch.(a) The complex spatiotemporal waveform has been analyzed to show information regarding the conduction velocity, origin, and location ofthe component potentials. Part (b) is a magnified view of the spatiotemporal data.
REFERENCES 247apart over the biceps brachii muscle. However, a complete analysis (Figure 5.22a) is possiblethrough the use of multidimensional spectral estimates.A Final Thought on Spectral EstimationOf course, the Basic program in the book’s ftp site may be too slow to cope with most realtimeapplications, but implementing both classical and high-resolution methods on a DSPis a relatively easy task. First, modern DSP chips are designed specifically to perform theconvolution, vector arithmetic, and FFT operations in a minimal number of clock cycles. Inaddition, optimized subroutines to implement the most popular high-resolution algorithmsare available, often in the public domain.Multidimensional PSD estimation has a very high intrinsic parallelism because spectralestimates are taken independently for every dimension and thus can be solved efficientlywithin a parallel architecture. In other words, in array signal processing, where tasksrequire specific operations to be performed on innumerable data blocks, a parallel systemexploits the full power of a number of processors that work concomitantly on different portionsof the data toward solution of the larger problem.As you can see, spectral analysis is a very convenient tool that can serve a numberof engineering applications. Moreover, today’s PCs have the power to implement modernPSD estimation algorithms with sufficient efficiency for experimenting and even for somereal applications. With the enhanced capabilities of DSP chips, PCs with DSP coprocessorsand laboratory spectrum analyzers with embedded DSPs become truly powerful anduseful instruments. However, as you certainly understand by now, obtaining good spectralestimates is not only a matter of applying the algorithm blindly and watching the screen.Rather, knowledge about the spectral estimation methods, as well as empirical experiencein their use, are of foremost importance in obtaining consistent results.REFERENCESAckerman, B., High-Resolution Timing on a PC, Circuit Cellar INK, 24, 46–49, December 1991–January 1992.Allen, G. R., Amateur Telemetry, 73 Magazine, 72–76, July 1981.Haykin, S., ed., Array Signal Processing, Prentice-Hall, Englewood Cliffs, NJ, 1985.Jangi, S., and Y. Jain, Embedding Spectral Analysis in Equipment, IEEE Spectrum, 40–43, February1991.Marple, S. L., Jr., Digital Spectral Analysis with Applications, Prentice-Hall, Englewood Cliffs, NJ,1987.Prutchi, D., DSP Methods for Frequency–Wavenumber Analysis of the Array Surface Electromyogram,Proceedings of the 5th International Conference on Signal Processing Applications andTechnology, 177–182, 1994.Prutchi, D., A High-Resolution Large Array (HRLA) Surface EMG System, Medical Engineeringand Physics, 17(6), 442–454, 1995.Prutchi, D., Universal Sensor Interface, Popular Electronics, 39–44, June 1999.Schulze, D. P., A PC Stopwatch, Circuit Cellar INK, 19, 22–23, February–March 1991.Welch, P. D., The Use of a Fast Fourier Transform for the Estimation of Power Spectra: A MethodBased on Time Averaging over Short Modified Periodograms, IEEE Transactions on Audio andElectroacoustics, AU-15(6), 70–73, 1967.
6SIGNAL SOURCES FOR SIMULATION,TESTING, <strong>AND</strong> CALIBRATIONA common practice in evaluating the behavior of signal processing or control circuitry isto make use of an analog function generator to produce the necessary test input signals.The typical cookbook waveforms of the function generator are then used to investigate thebehavior of the circuit when stimulated by sine, square, and triangle waves of differentamplitude and frequency. Take, for example, the circuit of Figure 6.1. This module generatesan extremely accurate sine-wave calibration signal. Its output signal is continuously variablewithin the range 10 µV p-p to 1 mV p-p . The frequency is set by component selection inthe range 2 MHz to 20 kHz. This circuit is meant for the precise calibration of biopotentialamplifiers. Because of its high stability (sine-wave distortion of less than 0.2%), this circuitis ideal for measuring channel phase shift in topographic brain mappers and otherbiopotential array amplifiers.As shown in Figure 6.2, the heart of the sine-wave generator circuit is Burr-Brown’sModel 4423 precision quadrature oscillator. The frequency of the stable sinusoidal signalthat appears at pin 1 is determined by the values of capacitors C6 and C7 as well as thevalues of resistors R1 and R2. A separate frequency-selection module should be assembledon an eight-pin DIP header for each frequency desired. The value and type of C6 and C7(where C6 C7) should be chosen according to Table 6.1.After selecting the capacitor value required for a desired frequency range, the value ofresistors R1 and R2 (where R1 R2) in kilohms can be obtained from the expressionR1 R2 3.785f (C6 0.001)42.05 2f (C6 0.001)where f is the frequency desired in hertz and C6 C7 is expressed in microfarads. It takesa certain amount of time to build up the amplitude of the sine-wave output to its full-scalevalue. By pressing the RESET pushbutton switch SW1 momentarily, the amplitude of thesinusoidal output is built up instantaneously. Degradation of signal distortion does notoccur, as resistor R3 does not remain connected permanently within the oscillation circuit.Resistors R4, R5, and R6 determine the gain of the op-amp (uncommited within the4423 package). The op-amp, in which oscillatory behavior is prevented by C5, is used as aDesign and Development of Medical Electronic Instrumentation By David Prutchi and Michael NorrisISBN 0-471-67623-3 Copyright © 2005 John Wiley & Sons, Inc.249
250 SIGNAL SOURCES FOR SIMULATION, TESTING, <strong>AND</strong> CALIBRATIONFigure 6.1 This module generates an extremely accurate, low-amplitude (10 µV p-p to 1 mV p-p ) sinewavesignal for precise calibration of biopotential amplifiers. Because of its high stability (sine-wavedistortion of less than 0.2%), this circuit is ideal for measuring channel phase shift in topographicbrain mappers and other biopotential array amplifiers.power output stage to decouple the precision quadrature oscillator from the output load. R5is used to trim the amplitude of the signal at the op-amp output to exactly 1 V p-p . R7 and R8form an attenuator that divides the signal at the output of the op-amp to any amplitudedesired between 10 µV p-p and 1 mV p-p . To calibrate a single-ended biopotential amplifier,connect the ACTIVE input of the amplifier to J1-1 and the REFERENCE input to J1-2. Fordifferential amplifiers, connect both REFERENCE and SUBJECT GROUND to J1-2.ANALOG GENERATION <strong>OF</strong> ARBITRARY WAVEFORMSIn many applications, repetitive sine, square, and triangle waves are seldom representativeof the signals that the equipment under test is designed to process. For example, the heart’selectrical signal is a waveform consisting of a complex mixture of these basic waveshapesintertwined with intermittent baseline segments. Since a constant live feed of such signalsmay be impractical or even dangerous for testing biomedical equipment, dedicated signalsources had to be developed to be capable of synthesizing waveforms similar to those generatedby their physiological counterparts. Similar requirements are evident for the generationof test signals representative of those produced by medical imaging sensors and othersources that cannot be simulated by plain sines, ramps, or square waves.Figure 6.3 shows a simple circuit that can generate multiple synchronized repetitivewaveforms of arbitrary shape. IC2 is a binary counter that causes the outputs of IC3 to gohigh in sequence. One at a time, each of these lines causes current to flow through R21 byway of its associated diode (D1–D15) and linear slider potentiometers (R1–R15). As thecounter cycles, a stepped waveform appears across R21.Think about a graphic equalizer—your stereo set probably has one, or you have seenthem in pictures of recording studios. This type of equalizer is a multiband variable audiofilter using slide controls as the amplitude-adjustable elements. It’s named graphic for thepositions of the sliders graphing the resulting frequency response of the equalizer. In a similarway, the basic shape of the stepped waveform across R21 tracks the shape describedby the linear slider potentiometers as shown in Figure 6.4. Counter IC2 is clocked by the
OUTPUTSW1C11uF,25VC30.1uF++15V-15VC21uF,25VC40.1uF+C50.01uFR6,1%R31k2123IC1BB44230 91+11 2 813141746FA1FA3FA5-VccVccFA4FA2FA6Sine OutCosine Out5510 kCOMM8R11.69k,1% R21.69k,1%R8C75k1uF1736C61uF 4R41k,1%R510kIC2-+R71M, 1%Figure 6.2 The sine-wave generator circuit is based on a Burr-Brown 4423 precision quadrature oscillator. The frequency of the stablesinusoidal signal is determined by the values of capacitors C6 and C7 as well as the values of resistors R1 and R2. A separate frequencyselectionmodule should be assembled on an eight-pin DIP header for each frequency desired. With the component values shown, oscillationwill occur at exactly 10 Hz.251
252 SIGNAL SOURCES FOR SIMULATION, TESTING, <strong>AND</strong> CALIBRATIONTABLE 6.1 Capacitor Values and Types for the PrecisionSine-Wave Generator of Figure 6.2Frequency Range C6 C7 (µF) Capacitor Type0.002–0.02 Hz 1000 Polycarbonate0.02–0.2 Hz 100 Polystyrene0.2–2 Hz 10 Teflon2–20 Hz 1 Teflon20–200 Hz 0.1 NPO ceramic200 Hz–2 kHz 0.01 NPO ceramic2–20 kHz — —astable multivibrator formed by IC1A and IC1B. An approximate frequency for this oscillatoris given by f s 1/1.39(R17 R18)C1. Counting can happen only when IC2’s enableline (pin 5) is set low. When trigger selector switch SW1 is in position 1, a trigger from theastable multivibrator formed by IC1C and IC1D clocks flip-flop IC4A, enabling IC2 tocount. Once IC2 reaches a count of hex FF, output S15 of IC3 goes high. Flip-flop IC4Bis clocked after the rising edge on output S15 propagates through Schmitt triggers IC1Eand IC1F. The output of the flip-flop goes high, which resets IC4A and thus inhibits thecounter. This action also pulls the counter’s parallel load line (IC2 pin 1), which asynchronouslyforces the counter to hex 00. This state lasts for half a cycle of the samplingclock, when IC4B is reset by IC1A. It is possible to trigger the signal generator externallyby supplying a 12-V clock signal to J1 and placing SW1 in position 2. Alternatively, placingSW1 in position 3 lets IC2 count freely, assigning equal time to each of its 16 cycles.The setting of R1 defines a baseline level for the stepped signal voltage. The baselinelevel lasts as long as the counter is in the hex 00 state. As such, the stepped waveformdeveloped across R21 is composed of a sequence of 14 levels (set by R2–R15), each presentedfor one cycle of the sample clock (output of IC1B), followed by a baseline level (setby R1) that lasts for one trigger clock cycle minus the time it takes the counter to clockthrough the 14 signal levels.Although the step levels defined by the linear slider potentiometers are analog in nature,the time domain for the waveform is discrete. Of course, few real-world signals are appropriatelyrepresented by a stepped waveform with coarse jumps. Exceptions such as videolikestreams from scanned sensor arrays do exist, but in most cases, the waveforms neededto develop or test a medical instrument should be representative of the smooth physiologicalsignals that they are designed to process.In Chapter 5 we discussed use of a low-pass filter to reconstruct a signal from samplesacquired at a rate close to the Nyquist frequency. The same considerations apply here.After the signal across R21 is offset to zero by IC5A, it is low-pass-filtered by R24 andC13 to reconstruct a smooth waveform. Selecting the proper sampling rate and filter cutoffrequires some consideration. Let’s take, for example, the way in which you would set upthe waveform generator to simulate an ECG signal. Figure 6.5 shows how the P–QRS–Tcomplex could be represented by the position of the 14-step linear slider potentiometers(let’s disregard the U-wave), while the isoelectric baseline level between the end of theT-wave and the start of the P-wave is set by R1. Each step would last 40 ms, which requiresa sampling clock frequency of 25 Hz. If C1 0.1 µF and R17 100 kΩ, R18 needs to beset somewhere near 187 kΩ 1 for the multivibrator to oscillate at 25 Hz.1The exact frequency of oscillation of a CMOS astable multivibrator also depends on the supply voltage and onthe logic threshold voltage of the specific 40106 chip being used. The logic threshold can vary from 33 to 67%of the supply voltage from device to device.
15+12V+12V147147TRIGGERCLOCKADJUSTC11+IC1A4010610uF2SAMPLECLOCKADJUST+12VIC1C401066J121R20500k+12VC4C10.1uFEXTERNAL TRIGGER INPUT3+14710uFIC1B401064C5+10uF11147IC1E4010610C70.01uF123C60.01uF+12V+12V531446IC4ACD4013BDRSCLKVDD7QQ12CHANNEL nOUTPUT12C20.01uFR26100kR2R5R9D161N914+12V-12VR27100kD11N914D51N914D61N914D81N914D101N914D111N914D141N914C130.1uFCHANNEL 1GNDGNDGNDC80.1uFR17100kC90.1uF+R18500k9R19100kC1210uF+12V147-12VIC1D401068+12VTRIGGER SOURCE:1. INTERNAL2. EXTERNAL3. CONTINUOUS+12VSW1SW ROTARY 4P-3W13147IC1F4010612+12VC30.01uF4121331519101691081114IC2CD4029BJ1J2J3J45 7CIN COUTCLKPREENBIN/DECUP/DNVDDDIC4BCLKQ1Q2Q3Q48CD4013BQQRSVDDCHANNEL n_1611142D1D2D3D4CHANNEL 21312D1D2D3D4OUTOUT+12VCHANNEL 2OUTPUT1223212223124IC3CD4514BD1D2D3D4INHSTBVDD12S0S1S2S3S4S5S6S7S8S9S10S11S12S13S14S1511910876541817201914131615<strong>OF</strong>FSETADJUST+12VR23100kC140.1uFR22100kR25100k+12V50k Linear Slider50k Linear Slider50k Linear Slider50k Linear Slider50k Linear Slider50k Linear Slider50k Linear Slider50k Linear Slider50k Linear Slider50k Linear Slider50k Linear Slider50k Linear SliderR11R1350k Linear Slider50k Linear Slider50k Linear SliderD171N91432+-R3R4R6R14R1584R1R7R8R10R12R1649.9kIC5ATL0821D21N914D31N914D41N914D71N914D91N914D121N914D131N914D151N914R24130kC100.01uF56C150.01uFR211M+-+12V84-12VIC5BTL0827J2OUTPUTCHANNEL 112Figure 6.3 In this analog arbitrary signal generator, a counter sequentially scans through an analog ROM (IC3, D1–D16, and associated potentiometers)to generate a stepped waveform across R35 that is later smoothed through a low-pass filter (R38, C13). IC1A and IC1B generate theclock, which scans through the samples before resting at a baseline level. The waveform repeats once a new trigger is received by IC4A.253
254 SIGNAL SOURCES FOR SIMULATION, TESTING, <strong>AND</strong> CALIBRATIONFigure 6.4 Just as in a graphic equalizer, the basic shape of the waveform generated by this arbitrarysignal generator tracks the shape described by a bank of linear slider potentiometers.40msRMidpointLinear Slider Potentiometer PositionBaselineS0S1PS2S3QS4S5S6SS7S8TS9S10S11S12S13S14S15 = S0BaselineFigure 6.5 The P–QRS–T complex can be reconstructed from 14 analog samples. One more sampleis needed to represent the isoelectric baseline level between the end of the T-wave and the startof the P-wave. Each step would last 40 ms, which requires a sampling clock frequency of 25 Hz. Thetrigger clock frequency needs to be 1 Hz to simulate a rate of 60 beats/min.
DIGITAL GENERATION <strong>OF</strong> ANALOG WAVEFORMS 255Figure 6.6 Synchronous signals can be added by connecting more channels to the clock data bus. This figure shows an oscilloscope printoutobtained from a two-channel cardiac signal generator set to simulate a patient’s ECG and left-ventricular blood pressure signals.The cutoff frequency of the output low-pass filter should be selected to be at least halfof the sampling rate. Then, for 25 Hz/2 1/2π(R24)(C13), and selecting C13 0.1 µF,R24 127,323 Ω, which can be approximated by a 130-kΩ resistor. If a heart rate of60 beats/min is chosen, R19, R20, C4, and C5 have to be selected to cause the trigger clockmultivibrator to oscillate at 1 Hz. If C4 C5 10 µF and R19 100 kΩ, R20 needs to setsomewhere near 43 kΩ to yield a period of 1 s.The capability of generating one or more synchronous signals can be added by connectingmore channels to the clock data bus. This is especially useful when working withmultiparameter monitors. In Figure 6.6, which shows the output of a two-channel cardiacsignal generator, channel 1 simulates the surface ECG and channel 2 simulates a cathetermeasuredleft-ventricular pressure waveform.DIGITAL GENERATION <strong>OF</strong> ANALOG WAVEFORMSMore complex, nonstandard, real-world stimuli waveforms can easily be created as anumerical array and played back through a digital-to-analog converter (D/A or DAC) toyield analog waveforms of arbitrary complexity. This is the operating principle of a digitalarbitrary waveform generator, or arb. Despite the simplicity of the concept, a PC programthat would copy digital values stored in an array into a DAC would severely limit the
256 SIGNAL SOURCES FOR SIMULATION, TESTING, <strong>AND</strong> CALIBRATIONmaximum frequency of spectral components for the arbitrary signal. Even an assemblylanguageprogram copying the contents of sequential addresses on RAM to an I/O locationwould result in DAC writing rates of a few megapoints per second at the most.Instead of having a DAC interfaced to memory through a microprocessor, arbs have dedicatedRAM that is interfaced directly to the DAC. In this way, update rates are limited onlyby the access time of the RAM and by the speed of the DAC. As such, commercial arbs cancurrently be purchased with maximum writing rates in the vicinity of 1 gigapoint/s, yieldingbandwidths of up to 500 MHz.Direct Digital SynthesisA generator capable of directly synthesizing an analog signal from digital data has at itscore a memory that contains the full time-domain digital representation of the waveformdesired. To generate the analog signal, the discretized point-by-point version of the waveformis played in a sequential manner through the generator’s DAC. A simple form of suchgenerator is a direct digital synthesizer (DDS). As shown in Figure 6.7, an address generatorcircuit controls the way in which samples stored in ROM are delivered to the DAC’sinput. On each clock pulse delivered to the address generator, a new address is issued tothe ROM such that data for the next point in the sequence are presented to the DAC.The ROM in a DDS generator most often contains data for generation of a completesingle cycle of a sinusoidal waveform. The address generator is a simple counter, and theaddresses it generates constitute the various phase angles φ for which samples of the sinewave sin φ are available in ROM. The series of values coming out of this ROM lookuptable as a function of incrementing phase angles is translated into an analog sine wave bya D/A converter (DAC).Obviously, if the clock presented to the phase accumulator counter remains constant,the rate at which phases are generated remains constant, and the end result is a sine wavePhase AccumulatorV outtCountern bitsAddressROMData OutSin ( )DACLow-PassFilterOutputPhaseIncrementRegisterSine Look-up TableAddressGeneratorCircuitFigure 6.7 In a direct digital synthesizer (DDS), an address generator circuit or phase accumulator controls the way in which samplesstored in a ROM lookup table are delivered to the DAC’s input. Control over the output frequency is achieved by selecting an appropriatephase accumulator increment.
DIGITAL GENERATION <strong>OF</strong> ANALOG WAVEFORMS 257of a specific frequency. However, there is a very simple way in which DDS generators canbe made to vary their sine output frequency without varying the clocking frequency. Thisis accomplished by allowing programmability of the phase increment value ∆φ. As such,if the output of the phase accumulator increments by ∆φ on each incoming clock pulse, thefrequency of the output sine wave is given byf sin e f clock∆φ360The frequency resolution f r of a DDS generator is thus defined by the number of bits n ofthe phase accumulator increment register and the clocking frequency:f r f clockn2and the output frequency is set directly by the value W of the phase accumulator incrementregister:f sin e W f cn lock2Since wide registers, large counters, and ample ROMs are easily integrated, IC DDS generatorsare becoming available capable of generating sine waves into the hundreds of MHzwith incredibly high resolution.Take, for example, the circuit presented in Figure 6.8. Here a Harris HSP45102 ICimplements the phase accumulator and sine lookup table. The phase accumulator incrementregister in this IC is 32 bits wide and accepts a clock frequency of up to 40 MHz. Inthis way, the DDS IC is capable of providing data for the generation of sine waves as lowas 0.009 Hz and as high as 20 MHz with a resolution of 0.009 Hz! The sinusoidal signal atthe DAC’s output is not infinitely pure, since at least some distortion is introduced by thefact that the digital samples presented to the DAC for translation are quantized in both timeand amplitude. Time quantization results from the fact that the signal can change only atspecific time intervals dictated by the clock. Amplitude quantization results from the discretenature of the digital system itself. Samples of the infinitely continuous series of a sineare stored in ROM with finite resolution.Obviously, time quantization errors are reduced by using as large a lookup table as possible.In the case of the Harris HSP45102, the lookup table is 8192 samples wide. It mustbe noted, however, that since the number of samples used to reconstruct the sinusoidal waveis equal to the ratio of the clock frequency (40 MHz) and the output frequency selected,time quantization errors get worse as the output frequency increases. Voltage quantizationerrors, on the other hand, are reduced by increasing the width of the data word presentedto the DAC. Because price and complexity of a high-frequency DDS circuit increases withthe DAC’s resolution, a number of hobbyist projects have been presented using only 8-bitvideo DACs to gain simplicity at the expense of not taking full advantage of the HSP45102’s12-bit amplitude resolution [Craswell, 1995; Portugal, 1995].In the DDS circuit of Figure 6.8, a 12-bit TTL-input-compatible ECL DAC takes fulladvantage of IC1’s data word width. High-frequency harmonics generated by aliasing arelow-passed by IC3. In more sophisticated systems, a very steep digitally tunable low-passfilter is used to pass the selected fundamental frequency and reject all of the samplingaliases. The use of an appropriate low-pass filter (usually, an elliptic filter) becomes criticalfor generating clean output at high frequencies since steps become increasingly large,and the DAC output resembles a sine wave less and less. For example, while a 40-kHz
OUTPUTJ2SMBR10502WJP1JUMPER 3JP2JUMPER 3JP3JUMPER 31325122411231022921231231JP6231JUMPERR110KIC1HSP451029610 SEL_L/M OUT11 543212882011 SFTEN OUT1018 MSB/LSB OUT9DL871912 LOAD OUT817 ENPHAC OUT761813 TXFR OUT614 SDOUT5 27517SCLK OUT4 2620OUT3 2541619 P0OUT2 24P1OUT1 2331516OUT0CLK2141+5VJP5 JUMPERIC540 MHZX1K20-ND8 CL+12VOSCILLATORDL11DL10DL9DL7DL6DL5DL4DL3DL2DL1DL0281234567891011262419171322IC2AD9713D1D2D3D4D5D6D7D8D9D10D11D12LERSETAMPINREFINANA RETURNREF GNDIOUTIOUTREFOUTAMPOUT14162018R520C40.1uFR250R350R47.5K-5V231R610KJP4JUMPER 3R810K32+12V7 1+-4 5-12VR790.9KC62pFC7IC3OPA6036R910K125IC4BUF6344V- V+AMPLITUDEADJUSTBWVIN+12VVOUTC10R115K0.1uFC11<strong>OF</strong>FSETADJUST3-12V0.01uF-12V0.1uFFigure 6.8 A simple and very versatile DDS generator can be built around a Harris HSP45102 IC, which implements the phase accumulatorand sine lookup table. An ECL DAC converts 12-bit sine data into an analog output which is then filtered, buffered, and scaled. TheDDS is programmed through the PC printer port.J1DB25258
ARB BASICS 259TABLE 6.2 Input Lines P0 and P1 (Pins 19 and 20)of the HSP45102 Control the Introduction of a PhaseOffset to the Output of the Phase AccumulatorP1 P0 Phase Shift0 0 00 1 901 0 2701 1 180output signal is generated using 1000 samples per cycle, a 13.33-MHz signal is generatedusing barely 3 samples per cycle!Two 32-bit phase accumulator increment registers are available onboard the HSP45102.A digital input on pin 9 selects which one of these registers is used at any given time forthe generation of a sine wave. This allows direct frequency-shift keying (FSK) modulationof the output. In addition, the DDS generator allows us to change the phase on the fly byselecting the state of the P0 and P1 lines (pins 19 and 20), as shown in Table 6.2. Theselines can then be used for selecting in-phase or quadrature data bits for QPSK modulationof the analog signal output.Programming the HSP45102 is accomplished by loading 64 bits of data for the twophaseaccumulator increment registers through the data input pin (SD) in serial format.While maintaining the shift-enable (*SFTEN) pin low, each data bit is fed by a risingedge on the clock input pin (SCLK) of IC11. Sine-wave generation is turned on and offby controlling the *ENPHAC pin. The TXFER* input line is used to control the transferof the phase accumulator increment register selected by the SEL_L/M* line (pin 9) to thephase accumulator’s input register. In this design we have retained printer port pin usecompatibility with a DDS generator described in QST [Craswell, 1995], since the controlsoftware for that DDS is freely available over the Web as freeware, downloadable fromwww2.arrl.org/files/qst-binaries/.ARB BASICSAs shown in Figure 6.9, an arbitrary waveform generator shares the basic building blocksof a DDS generator. Instead of a ROM sine lookup table, however, a full time-domain digitalrepresentation of the arbitrary waveform is downloaded into RAM. In addition, thecounter is not thought of as a phase accumulator, and the means are provided to be able todefine arbitrarily the last data point of the waveform cycle (end address). In this way, thewaveform can be replayed continuously by looping back from the last point of the waveform’ssequence to the address of the RAM location for the first point of the sequence (startaddress).For some applications, it is necessary that the waveform be issued only once after atrigger event. To do so, additional circuitry within the address generator can receive a triggersignal that is used to allow addresses to be cycled once between the beginning and endof a waveform sequence for every triggering event. A typical application requiring thiscapability is, for example, the testing ultrasonic echo systems, where the simulated “echo”generated by the arb must be synchronized to excitation of the transmitting transducer.One other difference with a DDS generator is that instead of maintaining the clock rateconstant and jumping over sample points to change the period of a cycle, the clock frequencyin an arb is programmable. In this way, the waveform can be compressed or expandedthrough time, resulting in a controlled shift in frequency of all spectral components of the
260 SIGNAL SOURCES FOR SIMULATION, TESTING, <strong>AND</strong> CALIBRATIONAnalog OutputsDACSignalConditioningChannel 1SampleClockExternalTriggerCLKEnableCounterResetControl LogicEnd AddressRegisterAddressData OutRAMData InDAC+Σ+SignalConditioningSignalConditioningDigital Markersa x (Channel 1)+ b x (Channel 2)Channel 2Digital BuffersComputerInterfaceFigure 6.9 An arbitrary waveform generator has at its core a RAM that contains the full time-domain digital representation of the waveformdesired. To generate the analog signal, the discretized point-by-point version of the waveform is played in a sequential manner throughthe generator’s DAC. Waveforms can be replayed continuously by looping back from the last point of the waveform’s sequence to the addressof the RAM location for the first point of the sequence. Triggered operation is also possible by cycling through the memory contents onlyupon receiving a trigger signal.waveform. Of course, reproducing a signal requires the stored waveform to have been sampledat a rate of at least twice its highest-frequency component, and an appropriate interpolatinglow-pass filter should be used. In turn, this means that the complexity and timeduration of the reproduced waveform are limited by the arb’s memory size, or depth. Thetime duration of the output waveform is given byT waveform number of waveform pointsfclockSpeech, for example, requires a sampling minimum speed of approximately 8 kilosamples/s.An arb with a depth of 32 kilosamples would then suffice for only 4.096 s of recording.When keeping the memory size fixed, longer waveform durations can be achievedonly by limiting the bandwidth to allow lower sampling rates. Obviously, limiting thebandwidth results in limiting the complexity of the waveform by reducing the number ofspectral components available to describe the details of waveform.end address start addressfclock
ARB BASICS 261If more than sufficient memory is available in an arb to generate a waveform, additionalmemory can be used for a second waveform channel. Since both channels are generatedusing a single clock, the two output waveforms are precisely synchronized in time. Thiscapability is essential for testing instruments that derive their measurements from thephase relationship between two signals. Additionally, purely digital lines or marker channelsare sometimes offered to provide synchronization and position markers which arecoincident with specified points of the arb waveform. These can be very useful for triggeringoscilloscopes or other external instruments at specific times within the arb waveformcycle.Beyond generating synchronized signals, however, the greatest advantage of having anadditional channel is the possibility of summing both channels. In this way, two synchronizedarbitrary components of a single waveform can be controlled independently, makingit possible to test the effect of each component on the system. For example, in order tostudy the immunity of a circuit to an unwanted phenomenon, channel 1 could be loadedwith the waveform that is normally seen by the system under test. Channel 2, however,could be loaded with the anomaly at the desired time within the normal waveform. Then,by varying the gain of channel 2, the amplitude of the anomaly can be adjusted withoutchanging the amplitude of the normal signal.Summing of two arb channels can also be used to extend the dynamic range of the combinedsignal beyond the maximum dynamic of each independent channel. Setting the gainof the summed channels to different values makes it possible to generate large signals thathave very small features. Here, the macroscopic changes would occupy the full dynamicrange of one of the channels. The smaller “details” of the waveform would then be programmedto occupy the full dynamic range of the other channel. By ratioing the gainsbetween channels correctly, the summed signal can have a theoretical maximum resolutionequal to the sum of the independent channels’ resolutions.PC-Programmable ArbThe instrument shown in Figure 6.10 is a simple arb built using standard SRAMs, a fewcounter ICs, some glue logic, and DAC ICs. In the arb project presented here, three 32k 8 bit RAMs are used to store two 12-bit waveforms. An additional RAM IC provides sevenmarker channels, and the additional bit is used to encode the last valid data sample of awaveform sequence. As shown in Figure 6.11, the 15-bit address generator of the arb isformed by a chain of 74LS191 synchronous counters (IC1–IC4). The output of the counterchain is presented to 50-ns access-time SRAMs (IC5–IC8). From Figure 6.12 it can beappreciated that as long as IC1 is enabled, each clock pulse supplied in parallel to allcounter ICs causes the address to advance. This process continues until the address pointsto a data element (D31) on IC8, in which bit 7 is low. This causes the asynchronous resetof the counter chain.Notice how the arb’s circuitry ensures that each sample of the waveform sequence hasequal length. Data contents presented on the RAM data bus (D0–D30) are latched on theopposite edges of the clock than those which cause address transitions. In this way, sincethe data at the output of latches IC9–IC12 lag the data at the inputs of these latches by halfof a clock cycle, the reset signal issued when the counters reach END_ADDRESS1 (thelocation in which bit 7 of IC8 is low) causes the address to be reset to zero without upsettingthe data corresponding to END_ADDRESS. The next falling edge on the clock linecauses the data contents of the first RAM address to be presented at the output of thelatches. Obviously, while the amount of time for which the first address is available isshorter than that of any other address, the data corresponding to it is presented at the outputof the latches for exactly the same amount of time as for any other address.
262 SIGNAL SOURCES FOR SIMULATION, TESTING, <strong>AND</strong> CALIBRATIONFigure 6.10 This simple yet versatile arbitrary waveform generator can be programmed from theprinter port of a PC. Once loaded with an array of digital data, this arb acts as a stand-alone instrumentcapable of delivering two simultaneous analog signals, each with an amplitude resolution of12 bits, and variable temporal resolution down to 50 ns (20 megapoints/s).When triggered rather than continuous cycling through the waveform is desired, flipflopIC14 is allowed to control IC1’s enable line by way of switch SW1. In the triggeredmode, the flip-flop’s *Q output goes low when enabled by the rising edge of a trigger pulsepresented to its clock input line. This state is maintained until reset at the end of the waveformcycle by the same reset pulse that zeroes the counter chain. In this mode, triggerambiguity is less than one clock cycle.Downloading and uploading RAM waveform data from and to the PC is done throughthe printer port under a simple serial protocol implemented in the software available inthe accompanying CD-ROM. On the Arb, the chain of 74LS323 ICs (IC16–IC19) ofFigure 6.13 forms a 32-bit serial-to-parallel and parallel-to-serial converter. When theremote mode of operation is selected by the computer (digital low on bit 1 of the outputport of the printer port), LOC/*REM goes low, causing IC20 to transfer control of theclock (CLK), address generator reset (*RESET), RAM output-enable (*OE), and RAMwrite (*WR) to the lines of the printer port. The mode control lines (pins 1 and 19) of the74LS323s select between hold, shift left, shift right, and parallel load of the bits of thechain’s 32-bit register. Data are clocked serially into IC16 and shifted down the chaintoward IC19 by each rising edge of the serial clock line (SCLK). Once a complete 32-bitword is positioned in the register of the chain, IC16–IC19 drive the RAM data bus, and awrite strobe is used to store the register’s contents in the current address. The address generatoris then advanced, and the cycle is repeated to store successive waveform data points.Data can be read from the RAM into the computer by reversing this process. Once anaddress is selected, data can be loaded from the RAM data bus into the register formed by
ARB BASICS 263Figure 6.11 The address generator of the arb is formed by a chain of synchronous counters. Upon reaching the end address, the addressgenerator resets, and the next data latched corresponds to that of the first RAM address. For nonvolatile operation, the RAMs should bemounted on Dallas Semiconductor’s DS1213D SmartSockets.the chain of IC16–IC19. The register’s contents are then shifted out of IC16 into one of thestatus input lines of the printer port (pin 10 of J4).As shown in Figure 6.14, two different DACs can be used with the arb. An AnalogDevices AD9713 high-speed ECL DAC capable of updating its output at up to100 megasamples(MS)/s can restore high-frequency signals with high resolution.Alternatively, the lower-cost AD667 provides more limited performance for applicationswhich require DAC writing speeds of no more than 300 kilosamples/s. Unfortunately, it isdifficult to take full advantage of the AD9713s, since when using these high-speed DACs,the arb’s speed will be limited by the RAMs’ access time. Under the direct addressing architectureused by this arb, RAMs with 50 ns access time will allow a maximum writing speedof 1/50 10 9 s 20 MS/s. Achieving 100-MS/s writing speeds would require 10-nsRAMs, which although available (e.g., cache RAM), are very costly, limited in size, andgenerally power-hungry.
264 SIGNAL SOURCES FOR SIMULATION, TESTING, <strong>AND</strong> CALIBRATIONClockEnd Address+1RAMAddressEnd Address-1End AddressAddress 00 Address 01 Address 02RAMData{ D0-D30D31Data @End Address-1Data @End AddressData @Address 00Data @Address 01Data @Address 02ResetData toDACs &Markers(DL0-DL30)Data @End Address-2D31=1 D31=0 D31=1Data @End Address-1Data @End AddressData @Address 00Data @Address 01Data @Address 02*LOC RESETIC15 Pin 3(*Counters Enable)TriggeredModeExternalTriggerRAMAddressEnd AddressEnd Address+1Address 00 Address 01Figure 6.12 Under operating conditions, the arb’s control logic ensures that each sample of the waveform sequence has equal length bypresenting the data contents only on the opposite edges of the clock from those that cause address transitions. In the triggered mode, triggerambiguity is less than one clock cycle.Rather than using a direct addressing scheme, very high speed arbs overcome theRAMs’ access time shortcomings by operating several RAM banks in parallel. In this multiplexedaddressing scheme, one or more RAM banks are being accessed and allowed tosettle while current data are taken from a different RAM. As the address is updated, dataare taken from one of the RAMs that already has valid data available. A 4 : 1 multiplexedmemory arb, for example, could use four low-cost 50-ns RAMs to achieve 80 MS/s. Wechose not to use the more complex multiplexed approach, since 20 MS/s provided us withsufficient flexibility for our applications in the generation of relatively low frequency signalsfor evaluating biomedical instruments.Once analog signals are available at the DAC outputs, the circuit provides for theiroffseting and scaling prior to being buffered for output. In addition, a summing channel isprovided to expand the arb’s versatility. The local sampling clock is generated by IC33,Maxim’s MAX038 high-frequency waveform generator IC. Although this IC is typicallyused as a function generator, it is used within the circuit of Figure 6.15 as an oscillatorwhose frequency can be controlled over the range 20 Hz to 20 MHz. Alternatively, the
D[0:31]D[0:31]+5VSW2R4510kJ3BNCCLK_LOCALEXTERNAL CLOCK+5V231191291118IC16G1G2S0S1QA'A/QAB/QBC/QCCLK D/QDCLR E/QESR F/QFSL74LS323G/QGH/QHQH'871361451541617D0D1D2D3D4D5D6D7SDATA_INLOC/*REM*OE_REM*RESET_REMCLK_R EM*WES0S1SCLKSDATA OUTR6 10K R7 10K R8 10K R910KIC17IC20*LOC_RESET*WE+5V2356111014131151A1B2A2B3A3B4A4BA/BG1Y2Y3Y4Y74LS15747912LOC/ *REMCLK*RESET*OEU4F13 1274LS04+5V+5V231191291118231191291118G1G2S0S1QA'A/QAB/QBC/QCCLK D/QDCLR E/QESR F/QFSL74LS323IC18G/QGH/QHQH'G1 QA'G2 A/QAS0 B/QBS1 C/QCCLK D/QDCLR E/QESR F/QFSL74LS323G/QGH/QHQH'871361451541617871361451541617D8D9D10D11D12D13D14D15D16D17D18D19D20D21D22D23+5VR210KR310KR410KR510K+5V231191291118IC19G1G2S0S1QA'A/QAB/QBC/QCCLK D/QDCLR E/QESR F/QFSL74LS323G/QGH/QHQH'871361451541617D24D25D26D27D28D29D30D31Figure 6.13 Downloading and uploading RAM waveform data from and to the PC is done through the printer port under a simple serialprotocol. The chain of 74LS323 ICs forms a 32-bit serial-to-parallel and parallel-to-serial converter.To PCPrinterPortJ411421531641751861972082192210231124122513DB25265
266 SIGNAL SOURCES FOR SIMULATION, TESTING, <strong>AND</strong> CALIBRATIONIC30OPA603Figure 6.14 Two different DACs can be used with the arb: A high-speed ECL DAC capable of updating its output at up to 100 megasamples/scan restore high-frequency signals with high resolution. Alternatively, a lower-cost DAC provides more limited performance forapplications that require writing speeds of up to 300 kilosamples/s. The DAC analog outputs are then offset and scaled as needed. In addition,a summing channel is provided to expand the arb’s versatility.sampling clock can be supplied by an external TTL-level clock through connector J3 andswitch SW2.The arb’s circuitry requires a supply of 5 V for the logic circuitry, 5 V for the ECLlogic of the high-speed DACs, and 12 V for the analog circuitry. The power supply ofFigure 6.16 generates these voltages from a 12-V ac input. As shown in these figures, thearb, will lose the waveform data as soon as power is removed. For nonvolatile operation,however, the RAMs may be mounted on Dallas Semiconductor’s SmartSocket DS1213Dintelligent sockets. Remember that these sockets are designed to be compatible withRAMs of up to 128k 8. For this reason, four more PCB pads than those required for eachRAM IC are required when using the DS1213Ds. The µPD43256B RAMs are thenmounted on pins 3–30 of the SmartSockets. Another option is to use Dallas SemiconductorDS1210 ICs to handle RAM power backup from a small battery [Bachiochi, 1990].
CLK_LOCALC330.022uFC342200pFSW3200kHz-2MHzC35180pFC3622pFC3722pFR46100K 10T7345108+5V+C3810uFC390.01uF-5V17 16 20IC33MAX038V+DV+V-DADJA0A1COSCIINFADJ2 9 6 11 18 15OUTREFSYNCPDOPDI191141213GNDGNDGNDGNDGNDDGNDC320.22uF20Hz-200Hz200Hz-2kHz2kHz-20kHz20kHz-200kHzWritingRate RangeSelector2MHz-20MHzFREQUENCYADJUST+5VR7612KR50100R4910KR47R4810K2K 10TC440.1uFFigure 6.15 The local sampling clock is generated by IC33, Maxim’s MAX038 high-frequency waveform generator IC. Although this ICis typically used as a function generator, it is used within the arb as a clock oscillator whose frequency can be controlled over the range 20 Hzto 20 MHz.C312.2uF267
T112VAC 1AD11N4005D31N4005+ C45+2200uFC532200uFC460.1uFC500.1uFIC34LM7812C/TO2201 3IN OUT2IC36LM7912C/TO2202 3IN OUTC470.1uFC550.1uF+12V-12V+ C48+1000uFC561000uFD21N4005D41N4005+ C49+ C57100uF2200uFC500.01uFC580.1uF1 3IN OUT2IC37LM7905/TO2201 3IN OUTC590.1uF+ C49+ C601000uF-5V1000uF+5VGND1IC35LM7805/TO2202C510.01uFGND GNDGND+12V+5VC1,C11,C17,C19,C25,C61,C63,C65,C670.01uFC13,C21,C270.1uF+C14,C22,C28,C62,C64,C66,C6810uFC42,C77,C79,C81,C830.01uF+C40,C78,C80,C82,C8410uFC2,C18,C20,C26,C69,C71,C73,C750.01uFC15,C23,C290.1uF+C16,C24,C30,C70,C72,C74,C7610uFC43,C85,C87,C89,C910.01uF+C41,C86,C88,C90,C9210uF-12V-5VFigure 6.16 The linear power supply for the arb requires a 12 V ac input to produce 5 V for the logic circuitry, 5 V for the ECL logicof the high-speed DACs, and 12 V for the analog circuitry. The same circuit can be used for powering the DDS generator.115VAC268
ARB BASICS 269Finally, a word of caution when building this arb. High-frequency clocks and signalsdemand proper layout techniques [Prutchi, 1994]. Preferably, use a multiple-layer printedcircuit board. Separate the analog ground from the digital ground and join them at a singlepoint at the power source. Maintain interconnection over the buses short and of equallength. In addition, use good-quality high-frequency capacitors to decouple the power railsin close proximity to the power input pins of each IC.Creating Arbitrary WaveformsSignal creation for reproduction by an arb is usually accomplished in one of two ways:(1) capturing an analog signal using a digital storage oscilloscope (DSO), or (2) creatingthe waveform on a PC by generating a numerical representation of the waveform’s mathematicalformulation. One of the most popular and useful packages used in the developmentof signal-processing algorithms is Matlab by The MathWorks Inc. Complexwaveforms can be generated by this package’s enormous library of mathematical functions.With an arb, test signals synthesized within Matlab or any other scientific programmingenvironment can be used to excite the real hardware of a medical instrument,not just its algorithms.The following Matlab function (mat2arb.m) is capable of saving two vector variablesfrom its environment in a format that can be loaded into the PC-programmable arbdescribed earlier.function v mat2arb(x, filename);%MAT2ARB saves 2 vectors as a file that can be loaded into the%2-channel Arbitrary Waveform Generator% x input matrix [vector 1 ; vector 2] sample value range 0 to 4095% filename filename where arb file is to be saved entered as 'filename.ext'%%%if min(min(x))0;disp('minimum sample value found')disp(min(min(x)))error('sample value range must be between 0 and 4095')endif max(max(x))>4095;disp('maximum sample value found')disp(max(max(x)))error(‘sample value range must be between 0 and 4095’)endn length(x);% n is the length of the vectorszerzeros(1, n);% generate vector of zeros for% marker channelsy 1 : n;% generate vector of sample% indexesv[x(1, y);x(2, y);zer(y);zer(y)]; % marker channels always lowfid fopen(filename, ‘w’);% open file for outputfprintf(fid,’ %1g , %1g ,% write file in format suitable%1g , %1g \r’, v);% for ARBfclose(fid)% close file
270 SIGNAL SOURCES FOR SIMULATION, TESTING, <strong>AND</strong> CALIBRATIONAlthough short Basic programs or numerical processing packages such as Matlab can beused to generate waveform data, truly flexible waveform creation is possible only throughdedicated software. One of our favorite packages is Pragmatic Instruments’ WaveWorksPro since it offers a very intuitive environment for the creation of waveforms from a comprehensivemenu of standard waveform templates, math operations, and transfer functions.Waveforms can also be imported from other programs or uploaded directly through GPIBor RS232 from popular DSOs. In addition, waveform synthesis and analysis can be performedin either the time or frequency domains.Figure 6.17 presents an example of how easy it is to create waveforms with a waveformdesign package such as WaveWorks Pro. The software has 30 standard waveshapes withprogrammable parameters. These alone provide immediate solutions for the generation oftest waveforms for general-purpose applications (e.g., sinusoidal, square, triangularwaves), communications testing (e.g., AM, FM, BFSK, QPSK, NTSC waveforms), as wellas other signals for advanced signal processing and control (e.g., sin(x)/x, ECG waveform,digital and analog noise). After a waveform is defined, it can be modified using the 20predefined transfer functions or 13 mathematical operators. Once the desired waveform iscreated, an FFT-based spectral estimator offers frequency analysis with the possibility ofspectral editing and IFFT-based transformation back into time domain. Finally, a long andFigure 6.17 It is easy to create complex waveforms with Pragmatic Instruments WaveWorks Pro. For example, a signal for testing electrocardiographyequipment can be created by first defining the basic components of the waveform from predefined templates. On the left: abeat corresponding to the heart’s normal sinus rhythm (NSR), a premature ventricular contraction (PVC), and 60-Hz sinusoidal interference.A seamless link of the signals “contaminated” by 60 Hz (right) results in a realistic-looking ECG containing normal beats mixed with PVCepisodes followed by a long compensatory pause before returning to NSR.
ARB BASICS 271complex waveform can be created within WaveWorks Pro by looping and seamless linkingof previously created waveforms.As you can imagine, the introduction of cheaper, faster, high-resolution DACs, widerRAMs, and higher-performance microprocessors is making it possible for digital waveformgenerators to replace analog sources rapidly in many applications. High-performanceintegrated DDS generators have taken over in the spread-spectrum communications fieldand are the key elements that enable low-cost high-speed data links to be integrated into awide variety of patient monitors and wirelessly networked medical instruments.Arbs are also becoming very popular with design and test engineers. Arbs are more versatilesources than their analog counterparts. In fact, even when generating “standard”waveforms, arbs can compete with analog generators. For example, arbs can output rampsand triangle waves with higher linearity and sharper corners than an analog generator.Similarly, an arb-generated sine can have far better THD and frequency accuracy than theone generated by an analog circuit.Of course, the neat control and waveform-design screens of commercial arbs, theirpowerful DSP microprocessors, and their exotic high-frequency mixed-mode circuitrymakes them costly pieces of equipment. Most commercial arbs are priced in the range$3000 to $7000. On the other hand, an analog signal generator with similar bandwidthcosts just a few hundred dollars. So don’t feel that your reliable analog waveform generatorno longer deserves its space on the workbench, but keep the arb in mind when yourapplication demands ultimate flexibility without a compromise on performance.PC Sound Card as an ArbThe PC sound card is a true audio-range arb (useful in the range of 20 Hz to 20 kHz). Ittakes the waveform definition stored in the computer’s memory and plays it back as ananalog signal. The simplest way of generating an arbitrary wave through the PC sound cardis to store it as a .wav file and play it back using Window’s Media Player utility. A .wavfile is just a series of samples, preceded by a header that tells the player program importantthings such as the sampling rate and the number of bits in the sample. The player programreads the header, sets up the sound card, and then feeds the samples to the card’sdigital-to-analog converter.PC multimedia data are often encoded in the RIFF file format. RIFF is based on chunksand subchunks. Each chunk has a type, represented by a four-character tag. This chunk typecomes first in the file, followed by the size of the chunk, then the contents of the chunk. The.wav format is a subset of RIFF used for storing digital audio and requires two types ofchunks: (1) the format (fmt) chunk, which describes the sample rate, sample width, and soon, and (2) the data chunk, which contains the actual samples. .wav can also contain anyother chunk type allowed by RIFF, including LIST chunks, which are used to containoptional kinds of data, such as the copyright date and author’s name. Chunks can appear inany order. In its simplest form, the .wav format starts with the RIFF header of Table 6.3.TABLE 6.3Contents of the RIFF Header of a .wav FileOffset Length (bytes) Contents0 4 RIFF4 4 file length - 8where the “8” is the length of the first two entries(i.e., the second entry is the number of bytesthat follow in the file)8 4 WAVE
272 SIGNAL SOURCES FOR SIMULATION, TESTING, <strong>AND</strong> CALIBRATIONThe .wav specification supports a number of different compression algorithms. The formattag entry in the fmt chunk indicates the type of compression used. A value of 1 indicateslinear pulse-code modulation (PCM), which is a straight, or uncompressed, encodingof the samples, which is just the exact amplitude of each sample. The fmt chunk describesthe sample format (Table 6.4), and the data chunk contains the sample data (Table 6.5). Allnumeric data fields are in the Intel format of low–high byte (usually referred to as littleendian).Eight-bit samples are stored as unsigned bytes, ranging from 0 to 255; 16-bit samplesare stored as 2's-complement signed integers, ranging from -32768 to 32767.If you are a Matlab user, you can avoid the hassle of file formatting by playing a datastream directly from within the Matlab environment using the “sound” command. Matlab canalso write .wav files from data variables or read the .wav file PCM-encoded signal into datathat can be manipulated by Matlab. Another possibility is to use a professional waveformTABLE 6.4Contents of the Format Chunk of a .wav FileOffset Length (bytes) Contents12 4 fmt16 4 0x00000010which is the length of the fmt data (16 bytes)20 2 0x0001which is the data-encoding format tag: 1 PCM22 2 channelswhich defines the number of channels: 1, mono; 2, stereo24 4 sample ratein samples per second (e.g., 44,100)28 4 bytes/secondsample rate block align32 2 block alignchannels bits/sample/834 2 bits/sample8 or 16TABLE 6.5The Data Chunk of a .wav File Contains the Actual Sample DataOffset Length (bytes) Contents36 4 data40 4 length of the data block44 As needed for data sample dataFor multichannel data, samples are interleavedbetween channels:sample 0 for channel 0sample 0 for channel 1sample 1 for channel 0sample 1 for channel 1...where channel 0 is the left channel and channel 1is the right channel; the sample data must endon an even byte boundary.
ARB BASICS 273design package such as WaveWorks’ Pro to create the desired signal, and then use softwarethat is freely available on the Web, which can play data written in plain ASCII straight throughthe PC’s sound card. For example, SoundArb version 1.02 (sasetup.exe freeware for Windows9x, NT) by David Sherman Engineering Co. is a free PC sound card signal generator programthat not only lets you select standard waveforms but also load and play arbitrary waveformsfrom a text wave table file with full control over frequency, amplitude, and trigger mode.Updates to SoundArb, as well as more sophisticated arb software, are available from DavidSherman at www.wavebuilder.com.The output jack of a typical sound card carries an amplified ac-coupled signal (20 Hzto 20 kHz) capable of direct driving of 8-Ω speakers with some 2 W of power. Theactual output level is uncalibrated and will depend on the settings of the volume lever(which you can access by double-clicking the speaker icon in the Windows tray). Theonly way to set the amplitude to a known voltage is by observing the waveform on anoscilloscope. Since sound cards are meant to output sound, the volume control usuallyhas a limited number of discrete steps (e.g., 16) that follow a two-part piecewiselogarithmiccurve.Converting the Sound Card into a Precision DC-Coupled ArbUnfortunately, the typical 20-Hz high-pass cutoff frequency of consumer-grade soundcards makes them unsuitable for simulating most physiological signals. In addition, theoutput stage of sound cards does not usually have the output linearity or passband flatnessrequired for accurate reproduction of low-frequency signals. However, a phase-locked loop(PLL) circuit and some software can turn a sound card into a precision dc-coupled arb. Theidea is to use a software FM modulator to turn the arbitrary signal to be generated into anaudio tone that is played through the PC sound card. The tone’s frequency varies as a functionof the arbitrary signal desired. The arbitrary signal is then recovered by hardware FMdemodulation of the audio signal.Matlab has a function (vco.m) that simulates operation of a voltage-controlled oscillator,essentially an FM modulator. The following code shows how easy it is to use this functionto generate an FM signal by modulating a carrier (of frequency Fc) with an arbitrarysignal contained in vector x (sampled at a rate Fs of more than twice Fc, with an amplituderange of 1):Fs 5000; % Select arbitrary signal sampling frequency in HzFc 1687; % Select VCO carrier frequency in Hzmoddev 40; % Percent FM frequency deviationy vco(x, [1-moddev/100 1+moddev/100]*Fc, Fs); % VCO simulationsound(y, Fs) % Play modulated signal through PC sound cardYou can use the following Matlab command to look at the spectrum of the FM signal thatis played through the sound card:specgram(y, 512, Fs, kaiser(256, 5), 220)If you are not a Matlab user, you can write a program to generate the FM signal fromthe arbitrary waveform by remembering that an FM signal s(t) is expressed bys(t) A c cos2πf c t 2πk f t 0 m(τ) ∂τ where m(t) is the modulating signal (the arbitrary waveform), f c the carrier frequency, A c thecarrier amplitude, and k f defines the frequency deviation caused by m(t). The instantaneous
274 SIGNAL SOURCES FOR SIMULATION, TESTING, <strong>AND</strong> CALIBRATIONfrequency of the signal is larger than the carrier frequency when the signal m(t) is positiveand is smaller when m(t) is negative.The circuit of Figure 6.18 is used to demodulate the FM signal from the sound card. Thesignal coming from the sound card is ac-coupled by C17 and amplitude-limited by IC1D.Then a NE565C PLL IC demodulates the FM signal. The PLL tracks the incoming carriersignal and internally estimates the signal based on the frequency of its internal VCO set byR2, R4, and C2. The “error” between the actual carrier frequency and the estimate is the datasignal when the PLL is locked. A suitable FM frequency deviation for this circuit is 40%,which allows the bandwidth of the arbitrary signal to be reproduced to be approximately18.5% of the carrier frequency. Table 6.6 gives the signal reproduction characteristics for someof the standard frequencies used in FM tape recorders, an application that uses the same FMmodulation/demodulation schemes. The loop output of the PLL IC is fed into a unity-gaindifferential amplifier (IC1C). The common-mode rejection of this amplifier is used to eliminateDC and high-frequency carrier components present at the output of the PLL.A Maxim MAX280 switched-capacitor filter IC is used to remove residual carrier-frequencysignal components from the waveform desired. This IC is a fifth-order all-polelow-pass filter with no dc error, making it an excellent choice for processing low-frequencysignals. The filter IC uses an external resistor (R9) and capacitor (C10) to isolate thefourth-order filter implemented within the IC from the dc signal path. The external resistorand capacitor are used as part of the filter’s feedback loop and also form one pole forthe overall filter circuit. The values of these components are chosen such thatf cutoff 1.622π(R9)(C10)where R9 should be around 20 kΩ.Now, for the Matlab code example given above, the demodulated signal bandwidth isexpected to be 18.5% f c 18.5% 1687 Hz 312 Hz, which is where the 3-dB cutofffrequency for the low-pass filter should be placed. Selecting the closest standard-valuecomponents, R9 18.2 kΩ and C10 0.047 µF, the 3-dB cutoff will be 301 Hz.The chip’s internal four-pole switched capacitor filter is driven by an internal clock thatdetermines the filter’s cutoff frequency. For a maximally flat amplitude response, the clockshould be 100 times the cutoff frequency desired. The filter has a cutoff frequency ratio of100 : 1. The internal oscillator runs at a nominal frequency of 140 kHz that can be modifiedby connecting an external capacitor (C11) between pin 5 and ground. The clock frequencyis given by33pFf clock 140 kHz 33 pF C11TABLE 6.6 Signal Characteristics for Various Standard FM Tape RecorderFrequencies (kHz) aCarrier Deviation LimitsCarrier(for 40% FM Deviation)Modulating FrequencyFrequency Plus Deviation Minus Deviation Bandwidth1.687 2.362 1.012 dc–0.3123.375 4.725 2.835 dc–0.6256.750 9.450 4.050 dc–1.25013.500 18.900 8.100 dc–2.50027.000 37.800 16.200 dc–5.000aThe response bandlimits (dB) for a 100-Hz frequency response are 1%.
OUTOUTPUTOUTGNDIC1BTL0847-5V+5V+5V+5VFROMSOUNDINC170.01uFCARD R19INGND4IC2LM565VOUTPLLFREQUENCYADJUSTVINININREFTCAPTRESVCON+VCC-VCCR1710k2357101698R141k1213R25kR45.6kC7C80.1uF0.0068uF+-+5V411-5VD11N914D2IC1DTL08414C50.001uFC9+5V-5V0.1uFC140.01uF1kC20.001uFR8100kR13100kR16100kSWITCHED-CAPCLOCK FREQUENCYADJUST109+-+5V411-5VR15100kC11120pFR185kIC1CTL0848+5VC18+R910uF<strong>OF</strong>FSETADJUST18.2kC120.1uFC13-5V0.1uFC19+10uFR110kR3100kR710kGAINADJUST+5V-5VC100.047uF15IC3MAX280FBCLK47 DIVRTOOUTV+V-2C30.01uFR10100kBOUT8R6100kR1168k32+-+5V411-5VR12100kIC1ATL0841R54.7kC60.01uF+5VC10.01uFC150.1uFC20+10uF56+-411-5VC40.01uFC160.1uFAGNDC21+10uF1N914Figure 6.18 This PLL-based FM demodulator is used to generate dc-coupled signals from frequency-modulated signals generated througha PC sound card. IC1D is a limiter for the input signal. IC2 is the PLL. The common-mode rejection of IC1C eliminates dc and high-frequencycarrier components present at the output of the PLL. IC3 is a fifth-order all-pole low-pass filter with no dc error used to remove residualcarrier-frequency signal components from the waveform desired. IC1A adjusts the gain of the circuit and removes any offset introducedby the preceding stages.275
276 SIGNAL SOURCES FOR SIMULATION, TESTING, <strong>AND</strong> CALIBRATIONFor the example, when the cutoff should be around 300 Hz, which requires that f clock 30 kHz, obtained with C11 120 pF, a series resistor (R18) can be added to trim the oscillationfrequency. In this case, the new clock frequency is given byf clock R18 0f clockR18 01 4 (R18)(C11) f clockR18 where f 0 clock is the oscillator frequency when R18 is not present (obtained through theprior equation). After filtering, the gain is adjusted through R10 and all offset from the precedingstages is compensated with IC1A by setting R3. Finally, the RC low-pass filterformed by R5 and C6 removes any switching noise introduced by IC3.The stability of the PLL circuit depends on the stability of the frequency-setting components.Proper performance requires the use of low-temperature-coefficient high-tolerancecomponents. Resistors should be precision 1% tolerance type of the RN60D variety.Capacitors should be Mylar, polyester film, or other types that remain stable with age andwhich are not sensitive to temperature variations. Figure 6.19 demonstrates the performanceof the technique. The test signal is a real ECG that was digitized at a sampling rateof 5 kHz with 12-bit resolution. Figure 6.19b shows the spectrum of the FM signal, andFigure 6.19 A real ECG signal that was digitized at a sampling rate of 5 kHz (a) is used to frequency-modulate a 2-kHz carrier using theMatlab vco.m function (b). The output of the PLL-based FM demodulator is shown in part (c), showing how the demodulated signal faithfullyreproduces the dc offset and low-frequency components of the ECG.
RESPONSIVE SIMULATORS 277Figure 6.19c shows how the demodulated signal faithfully reproduces the dc offset andlow-frequency components of the ECG.Since the sound card output is in the audible range, the modulated signal can be transmittedto the demodulator via a voice radio or telephonic link for remote signal generation.To do so, however, the tone frequencies produced by the sound card for a full-scaleinput must be limited to the bandpass of the communications channel. For a plain telephoneline, this range is 400 Hz to 3 kHz, while a commercial FM audio link is specifiedto cover the audio bandwidth 30 Hz to 15 kHz. Another interesting possibility is to use asmall 1 : 1 audio isolation transformer and a floating power supply to turn the demodulatorinto an isolated output stage. Finally, it should be noted that the full bandwidth of asingle sound card channel can be shared by multiple software modulators occupying separateaudio bands to convey various simultaneous low-frequency signals to an array ofPLL demodulatorsRESPONSIVE SIMULATORSSignal generators are OK for testing medical instruments that only measure, process, analyze,or display physiological signals. However, many medical devices are used to delivera therapy that dynamically changes the physiological signals that are measured. In thiscase, output-only signal generators are of only limited use. Take, for example, a DDDpacemaker, described in Chapter 8. This pacemaker can pace both the right atrium and theright ventricle separately at dynamically variable time delays to mimic the natural heartbeatwhenever one or both chambers fail to contract on their own. To do so, the pacemakercan sense intrinsic electrical signals from both chambers. Whenever timely intrinsic activityis present in both atrium and ventricle, the device inhibits pacing. However, when ventricularintrinsic activity does not follow the atrial activity in a timely manner, the devicetriggers pacing on the ventricle in sequence after the atrium.Testing a DDD pacemaker requires a simulator that is capable of emulating many of theheart’s electrophysiological properties. Many subtleties about the heart’s conduction systemneed to be designed into the simulator, including the way in which the atria and ventriclesbecome refractory for some time after being excited intrinsically or artificially. Inaddition, a cardiac simulator suitable for interacting with a pacemaker should be able toexhibit pacing thresholds similar to those of a typical heart, and the cardiac signals generatedby the simulator’s “chambers” must have morphologies, amplitudes, and timings similarto real P- and R-waves detected with intracradiac electrodes.We designed a responsive cardiac simulator as a test tool for three-chamber pacemakers(pacemakers that cannot only stimulate the right atrium and right ventricle, but can alsosynchronize the activity of the left ventricle to the pumping of the right heart). The circuitand timing characteristics for this responsive simulator are shown in Figures 6.20 to 6.28.The heart’s electrical activity as seen by intracardiac electrodes is simulated by theCENELEC signal. 2 Three signal generators, one corresponding to the heart’s right atrium,one to the right ventricle, and the last to the left ventricle, provide programmable, 0- to 9-mV CENELEC signal outputs. The following explanation refers to the signal generator forthe right atrium but is also applicable to the other two, since the right- and left-ventriclesignal generator circuits are similar. The CENELEC waveforms are stored as 12-bit values2CENELEC stands for “Comité Européen de Normalisation Electrotechnique” (European Committee for ElectrotechnicalStandardization). The CENELEC signal is specified in Figure FF.103 of the preliminary draft of theEN-45502-2-1 standard: Active Implantable Medical Devices—Part 2-1: Particular Requirements for ActiveImplantable Medical Devices Intended to Treat Bradyarrhythmia (Cardiac Pacemakers), January 2001. This waveformis intended as a test signal used for the exact determination of sensitivity (sensing threshold) of pacemakers.
278 SIGNAL SOURCES FOR SIMULATION, TESTING, <strong>AND</strong> CALIBRATIONin IC37, the PIC16C77 microcontroller shown in Figure 6.20. The 12-bit values are outputserially through the microcontroller’s SPI port to IC1, an LTC1451 D/A converter. Theoutput from each D/A converter is scaled by a programmable attenuator made up by IC3and the resistor network, R2 and R5–R14. A thumbwheel switch connected to analog multiplexerIC3 selects the resistor used in the attenuator circuit. The signal from the attenuatoris buffered by IC2A and changed from voltage to current by IC2B, IC2C, and IC2D.This current signal flows into R74, a 10-Ω resistor, and is seen by the device under test asa voltage signal. Figure 6.21 shows the schematic of the right-atrial and right-ventricularCENELEC signal generators.A typical cardiac cycle would start with generation of the right-atrial CENELEC signalfollowed by the right-ventricular CENELEC signal. The delay from the start of the right-atrialsignal to the beginning of the right-ventricular signal is fixed in this simulator at 100 ms. Theleft-ventricular signal would then start after the right-ventricular signal, with a time delay that+5VThumbwheelLV_DELAY_SW_1LV_DELAY_SW_2LV_DELAY_SW_3LV_DELAY_SW_412R98E47K5C5815pFY110.0MHZC5915pFR98F47K11 106C540.1uFR98G47K7C554.7uF+5VR98H47KZ_CS98R10310KIC371MCLRRB740234567891011121314151617181920RA0/ANORA1/AN1RA2/AN2RA3/AN3/VrefRA4/TOCKIRA5/SS/AN4RE0/RD/AN5RE1/WR/AN6RE2/CS/AN7VDD1VSS1OSC1/CLKINOSC2/CLKOUTRC0/T1OSO/T1CKIRC1/T1OS1/CCP2RC2/CCP1RC3/SCK/SCLRD0/PSP0RD1/PSP1RB6RB5RB4RB3RB2RB1RBO/INTVDD2VSS2RD7/PSP7RD6/PSP6RD5/PSP5RD4/PSP4RC7/RX/DTRC6/TX/CKRC5/SDORC4/SDI/SDARD3/PSP3RD2/PSP239383736353433323130292827262524232221PIC16C77R10410KV_PACE_DETECTLV_P_TRIGSDOA_PACE_DETECTSCLK+C564.7uF+5VLV PVCSWITCHLV_PVC_SWC570.1uFA_CSV_CSLV_CSECG_CSR105 150R106 150R107 150R108 150R109 150R110 150A_SENSE_LEDA_PACE_LEDV_SENSE_LEDV_PACE_LEDLV_SENSE_LEDLV_P_OUT_LEDLV_P_LEDR111 150Figure 6.20 The responsive cardiac simulator is controlled by a PIC16C77. In addition, this PIC contains digitized CENELEC, ECG, andimpedance waveforms that are played back via LTC1451 D/A converters to simulate the heart’s electrical and mechanical activities.
Figure 6.21 Right-atrial and right-ventricular intracardiac electrogram signal generators for the responsive cardiac simulator. The outputfrom each D/A converter is scaled by a programmable attenuator. A thumbwheel switch connected to an analog multiplexer selects the resistorused in the attenuator circuit. The signal from the attenuator is changed from voltage to current and converted into a perfect differentialvoltage across to be seen by the pacemaker under test as a voltage signal.279
280 SIGNAL SOURCES FOR SIMULATION, TESTING, <strong>AND</strong> CALIBRATIONcan be selected from the following settings: 1, 10, 20, 30, 40, 50, 60, 70, 80, 90, 100, 110,120, 130, 140, or 150 ms using the thumbwheel switch. Figure 6.22 show the timing relationshipof right-atrium, right-ventricle, and left-ventricular CENELEC signal generation.When a physician programs a pacemaker to the patient’s needs, the patient’s heart isusually monitored with a single-lead ECG. The cardiac simulator incorporates the simpleECG signal generator circuit of Figure 6.23 to provide an output that can be monitoredwith a standard single-lead ECG machine. An ECG signal is generated from digital valuesstored in IC37, a PIC16C77 microcontroller, and output through the microcontroller’s SPIport to D/A converter IC34. R99 and R100 attenuate the output of IC34 to approximately2 mV peak to peak. The P- and R-wave ECG signals are synchronized with the right-atrialand right-ventricular CENELEC output signals.In Chapter 8 we explain how pacemakers can use impedance signals to derive control informationbased on the heart’s contractile state. For the time being, suffice it to say that as theheart pumps, the volume of the blood pool around the electrodes changes. Since blood is moreconductive than is muscle tissue, these volume changes result in a varying electrical impedancebetween the electrodes. The cardiac simulator incorporates a voltage-to-impedance converterto simulate cardiac impedance signals. This circuit is based on an idea by Belusov[1996] and was designed by Greg Martin, now a project manager at HyTronics. As shown inFigure 6.24, IC36, an LTC1451 D/A converter, generates a voltage waveform that is stored inthe microcontroller’s ROM in the same way as are the ECG and CENELEC signals. In thiscase, however, the voltage output of the D/A is converted into an impedance signal.This impedance waveform is synchronized with the left-ventricular CENELEC output signal.R79 sets the baseline impedance value (typically, 500 Ω). IC35, a MAX038 sinusoidalwaveform generator, simulates the impedance variations caused by respiration. The frequencyof the respiratory component is set by R102. The intracardiac impedance andrespiration waveforms are summed into the inverting input of IC40A. The output ofIC40A, a summing, inverting amplifier circuit, is given byVV z Z V r1.6 2 Right AtrialCenelecSignal13ms 2msRight VentricularCenelec SignalLeft VentricularCenelec SignalStartFixed A-V Delayof 100msTime Delay Set byThumb Wheel SwitchFigure 6.22 A typical “cardiac” cycle starts with generation of a right-atrial CENELEC signal followed by the right-ventricular CENELECsignal. The delay from the start of the right-atrial signal to the beginning of the right-ventricular signal is fixed in the cardiac simulator at100 ms. The left-ventricular signal starts after the right-ventricular signal with a programmable time delay.
+15VCLKDINIC31LTC1451VCCVOUT+5VC390.1uF28DIC33ADG406S1S2S3S4S5S6S7S8S9S10S11S12S13S14S15S16A0A1A2A3EN+VCC-VCC192021222324251272611109+15VR873.63KR921.11KLV_GAIN_SW_1LV_GAIN_SW_2LV_GAIN_SW_3R93714R94344C38.047uF+C4010uFR8110M56411C41.01uF+-876541716151418-15V+ C367IC32BTL084A10uFR8410KR9610K14I_OUT = V_IN/10001411+-IC32DTL084A1213LV_V_TO_I_OUT2CS/LD REF4 5DOUT GND876R8210K3+5VR854.99KR864.29KR883.04KR892.49KR902.0KR911.54K32411+-IC32ATL084A18411R97+-IC32CTL084A109C37.01uFR9510KR831K12C45.01uF-15VC461uFC42.01uFC431uF116R98A47K314R98C47K413R98D47K10KC4447pF+5V12123IC34IC36CLKDINCS/LD REF4 5DOUT GNDLTC1451VCCVOUT876C520.1u FECG_SI G_OUTZ_SIG_OUTApprox. 2mV p-pResp Frequency~ 0.1 to 1 HzAdjustfor0.1HzR101130K+ C501uF+C5322 uF17201085IC35REFDA DJMAX03826179411A0183191615141312C48.01uFV +A13CLKDINCS/LD REF4 5DOUT GNDLTC1451VCCVOUT876+5VC490.1uFR9910 K-5VC51.01uFV-IINFADJCOSCOUTDV+DGNDSYNCPD IPDO+ C471uFRESP_WAVEGND4GND3GND2GND1GND0AGND2151R98B47KLV_GAIN_SW_4+5VR1004.99 ohms231R1021M, trimpotFigure 6.23 The responsive cardiac simulator incorporates a simple ECG signal generator circuit to provide an output that can be monitoredwith a standard single-lead ECG machine. An ECG signal is generated from digital values stored in the microcontroller and outputthrough the D/A converter IC34. R99 and R100 attenuate the output of IC34 to approximately 2 mV peak to peak.SCLKSDOLV_CSECG_CSZ_CS281
C791uFR112Z_SIG_OUTZ Amplitude~0-50 OhmsRESP_WAVEResp Amplitude~0-20 OhmsR11610K, trimpotR12210K, trimpot313122VwVrR11816KR12320KC70.01uFC73.01uFR1204.32K10KC711uF1uFC74++23114-+-15V+15VIC40ATL084A1-15VR11310KVz = -(Vz/1.6 + Vr/2)-2.5 VR1172. 5KC72.01uFR11410KR11920KR1213.92K65114-+R12410KR11510KIC40BTL084A7C75.01uFC761uF2.5 V - Vz/2++15V8AD633+X1-X2IC41AD633JN12R12520KR12620K91011-+IC40CTL084A84-15VC78.01uF++15VR127100C80.01uFC811uF+87 3W +Y1 4-Y2AD633+X1-X2IC42AD633JN12+VsZ6Y = Gain = 2-Vs+Vs7 3W +Y1 4-Y2Z6-VsC7712pF5X = -10 (Vz/4)/(2.5 - Vz/2) = 5Vz / (Vz -5)LS_2R = 100/(1 - XY/10) = 20(5-Vz)Vin1213411+-IC40DTL084A142 * Vin5-15VC82.01uF+C831uFR128R12910K10KFigure 6.24 The cardiac simulator incorporates a voltage-to-impedance converter to simulate cardiac impedance signals. The voltage outputof the D/A is converted into an impedance signal that is synchronized with the left-ventricular CENELEC output signal. R79 sets thebaseline impedance value (typically, 500 Ω). Impedance variations caused by respiration are simulated using the sinusoidal signal generatedby IC35 in Figure 6.23.282
RESPONSIVE SIMULATORS 283IC40B scales the summed signal and adds an offset of 2.5 V dc. IC40B’s output is thusV out 2.5 V Z2The change in impedance, which is seen between IC40D, pin 12, and ground, is given by100Z out 20 (5 V 1 XY/10Z )The function of a pacemaker is to stimulate the heart when the heart’s intrinsic pacemakeror conduction mechanisms fail to generate an action potential. This is where theresponsive behavior of the simulator comes into play. Pacing pulse detectors are used tosense pacing pulses generated by a pacemaker connected to the simulator. This cardiacsimulator responds to these stimuli by simulating the excitation of the heart chamberthrough which the pacing pulse was received. The atrial pacing detector circuit shown inFigure 6.25 is made up of IC7A, an inverting amplifier with a gain of 2, a comparator,IC8, and an inverter, IC9A. An external atrial pacing signal delivered by a pacemakeracross R73 and R74 is input to IC7A, which inverts and amplifies the pacing signal by afactor of 2. IC8 compares the voltage on its noninverting terminal, which is set to approximately1.0 V by trimmer R43. If the inverted pacing signal detected on pin 3 of IC8 isless than the voltage on pin 2, the output of the comparator is set high (5 V). This digitalhigh is inverted by IC9A to a low and input to the microcontroller’s RB6 input. Whenthe inverted pacing signal is greater than 1.0 V, the output of IC36 is low, which isinverted by IC35E to a high. This low-to-high transition generates a “change on port B”interrupt, which causes the microcontroller to execute the interrupt service routine code.R40 and C25 ensure that the pacing signal has sufficient amplitude and duration to tripthe comparator. This guarantees that narrow transients do not pass through and trigger themicrocontroller. The ventricular pacing detector circuit works in the same way as theatrial pacing detector described above, with the exception that the input pacing signal isinput across R75 and R76.The responsive cardiac simulator was designed to exercise three-chamber pacemakersand other devices intended to treat congestive heart failure. These sometimes deliverbipolar current pulses to the left ventricle, and it is important to monitor the approximatevalue of the positive and negative current pulses. The bar graph LED display of Figure6.26 shows the amplitude of the left-ventricle pacing pulse in 2-mA steps. D1 and D2steer each phase of the bipolar current pulse to the correct display circuitry. The currentfor the positive phase of the left-ventricular pacing pulse flows into the junction ofR52–R60. A minimum of 2 mA is required to turn on optocoupler IC19 and the first segmentof the bar graph display.For discussion purposes let’s suppose that the pacing pulse delivered to the left ventricleconsists of a 4-mA current pulse followed by a 4-mA pulse. Then 2 mA wouldflow through R61 and turn on the optocoupler and the first section of the bar graph display.The voltage across R61 will forward bias the base–emitter junction of the PNP transistorin IC19 (across pins 5 and 6). Once the PNP transistor is forward biased, the inputcurrent can also flow through the base–emitter junction of the NPN transistor. This currentflow switches on the NPN transistor in the IC and allows the additional 2 mA (what’sleft of our 4 mA) to flow through R52, the collector–emitter junction of the NPN transistorand the second LED of the bar graph display. Current will flow through the secondLED of the bar graph display and through R53 and should be enough to forward bias thenext PNP transistor (IC12). But there would not be enough remaining current flow to turnon the LED in the third section of the bar graph display. Each successive LED of the bar
284 SIGNAL SOURCES FOR SIMULATION, TESTING, <strong>AND</strong> CALIBRATIONR36200K+15V+5V-15VC231uF+R3720KR384.99K+5VA_PACE_INR39100KIC7ATL082 42-3 +1C24.01uFR405.11K4 13 -2 +IC8LM 311714 IC9A74HC141 2A_PACE_DETECTR4167K8+15VC261uF+C27.01uFC250.1uFA PaceDetect3Threshold2Set for 1.0volt at thewiper of the 1trimpot.5 6 8R4310K, trimpot+5VR42100KC281uF+C29.01uF7+15V+5VR44200KR4520KR464.99K+5VV_PACE_INR47100KIC7BTL082R4967K46 -5 +87R485.11KC300.1uFV PaceDetectThreshold2Set for 1.0volt at thewiper of the 1trimpot.34 13 -2 +5 6 8R5110K, trimpot+5VIC10LM3117R50100KC311uF+C32.01uF14 IC9B74HC143 47V_PACE_DETECTFigure 6.25 The atrial and ventricular pacing detector circuits sense the presence of external pacing signals delivered by a pacemaker undertest. The comparator circuits generate interrupts for the microcontroller. An RC network (R40 and C25 for the atrial pacing detector) ensurethat the pacing signals have sufficient amplitude and duration to “capture” the simulated heart.graph display will be on if there is enough current to forward bias each PNP transistor inthe IC, and each LED.When enough current flows through the internal LED of the optocoupler (IC19) to turnthe NPN transistor on, the input to IC9E is pulled to ground. This digital low is invertedby IC9E and signals the microcontroller of a left-ventricular pacing event. Either a positiveor a negative pacing signal can trigger a left-ventricular pacing event as the outputs ofthe optocouplers are wire-ORed together. Figure 6.27 shows the power supply for the simulator.An external “brick” type of power supply produces 15 V dc from 117 Vac. IC38and IC39 produce 5 V dc from the 15-V power supply. Diodes D3–D10 drop approximately0.6 V dc each and lower the input voltage to each voltage regulator. This reducesthe power dissipation by each device.
Figure 6.26 This bar graph display circuit monitors the intensity of bipolar current pulses delivered to the left ventricle.285
286 SIGNAL SOURCES FOR SIMULATION, TESTING, <strong>AND</strong> CALIBRATIONFigure 6.27 An external “brick” 15-V dc power supply is used to power the cardiac simulator. 5 V dc is generated onboard for thedigital portions of the circuit.Firmware for the Cardiac SimulatorFigure 6.28 shows the state machine for the main loop. The main routine performs thefollowing tasks:• Reads the LVS_Delay (left-ventricular sense time delay) hex switch setting and storesthe value.• Checks to see if the LV_P_IN signal was found outside the 180-ms window.• Checks for an atrial capture event (A_CAP_EVENT flag set to 1). If the atrial captureevent is true and the atrial capture action flag is enabled, the DO_A_CAP subroutineis run and the user returns to the main loop. The atrial capture action flag is used todisable atrial events in the main loop. If an atrial capture event is detected but theaction flag is not set to 1 (enabled), the event flag is cleared.• Checks for a ventricular capture event (V_CAP_EVENT flag set to 1). If the ventricularcapture event is true and the ventricular capture action flag is enabled, the DO_V_CAP
RESPONSIVE SIMULATORS 287A EventDetectedV EventDetectedDO ACAPMainDO VCAPTimeoutDOTIMEOUTFigure 6.28State machine diagram of the main loop of the responsive cardiac simulator.subroutine is run and the user returns to the main loop. The ventricular capture actionflag is used to disable ventricular events in the main loop. If a ventricular capture eventis seen but the action flag is not set to 1 (enabled), the event flag is cleared.• Checks to see if the PVC button was pressed (i.e., the LV_PVC_EVENT flag is set).If the event flag is set to 1 and the action flag (LV_PVC_ACTION_FLAG) is enabled,the DO_LV_PVC subroutine is executed. After execution the subroutine returns tothe main loop. If the action flag is not set, the event flag is cleared.• Controls the value stored in the delay timer of time spent in the main loop throughmain loop timeout. While inside the main loop the microcontroller checks continuouslyfor capture events. If no capture events are detected, the delay timer times out,and the subroutine whose pointer is stored in TIMEOUT_INDX is executed. Thedelay timer is decremented once every millisecond in the TIMER1 interrupt serviceroutine.The interrupt service routine is comprised of two main sections. The first section is theTIMER1 interrupt routine, which is executed once every 1 ms.• Z delay timer. A delay is used from the start of a ventricular event such as a pacedetect event to the beginning of the impedance waveform output. This delay is set to66 ms for a PVC event or 96 ms for a normal ventricular event. The Z delay timer isdecremented and tested for a value of zero each time the TIMER1 interrupt occurs.The Z delay timer is first decremented and if found equal to zero, the impedance outputflag is set to 1 (Z_FLAG 1), which starts the output of the impedance waveformdata from the microprocessor to the impedance D/A converter.• LVP window timer. The left ventricular pacing pulse from the device under testmust be completed within 180 ms after a right-ventricular event (either paced orintrinsic). The LV_P_WIN_TIMER is loaded with a value of 180 by theDO_V_CAP (capture event) or the DO_V_INTRIN (intrinsic event) routines. Eachtime through the TIMER1 interrupt service routine, the LV_P_WIN_TIMER isdecremented by 1 and the LV pacing input (LV_P_TRIG) is checked to see if it hastransitioned from a high to a low state (1 to a 0). If the LV_P_TRIG input does transitionfrom a high state to a low state within the 180-ms period, the LV_P_ON subroutineis executed setting the LV_P_LED output to a 1. The purpose of this test isto verify that the LV pacing pulse output by the device under test does not exceed
288 SIGNAL SOURCES FOR SIMULATION, TESTING, <strong>AND</strong> CALIBRATION180 ms beyond activation of the RV. This would be considered an intrusion into the“vulnerable period” of the heart.• A and V event timers. The A and V event timers are incremented each time throughthe TIMER1 interrupt service routine. These timers are used to calculate the timesince the last A and V events.• Right-ventricle event to left-ventricle sense delay timer. The right-ventricle event toleft-ventricle sense output time delay, if not equal to zero, is decremented each timethrough the TIMER1 interrupt service routine. If after decrementing the timer, thetimer is equal to zero, the left-ventricular sense waveform output is started. The delayis read from the front-panel hex thumbwheel switch.• LED timers. Each LED on the front panel is on for a fixed length of time. The on timefor each LED is loaded into a timer when the LED is switched to the on state by oneof the subroutines. Each of the LED timers, if not equal to zero, is decremented; afterdecrementing, if the timer is found to be equal to zero, the LED is switched off.• Delay timer. A general-purpose delay timer, if not equal to zero, is decremented eachtime through the TIMER 1 interrupt service routine, and if after decrementing isequal to zero, the DELAY_FLAG is cleared.• Test ECG out. Check to see if the ECG waveform output flag is enabled (ECG_FLAG 1). If the flag is enabled, write the next word in the ECG waveform table tothe ECG D/A converter.• Test Z out. Check to see if the Z waveform output flag is enabled (Z_FLAG 1). Ifthe flag is enabled, output the next word from the impedance waveform table to theimpedance D/A converter.The second section is the TIMER0 interrupt service routine, which is executed onceevery 200 µs:• Test port B inputs. Check if any of the inputs on the upper 4 bits of port B went froma low to a high state. If the enable flags for each of these inputs is set to a 1, the eventflag for each input is then set to a 1. The event flags are used to signal that one or moreexternal events have been detected.• Test the PVC switch input. Check to see if the PVC switch was pressed and that aLV_PVC_ENABLE event is not already pending. If not, signal an LV PVC event bysetting the LV_PVC_ENABLE flag.• Test A out. Check to see if the right-atrial CENELEC waveform output flag is enabled(A_FLAG 1). If the flag is enabled, write the next word from the CENELEC waveformtable (CEN_TABLE) to the A sense D/A converter.• Test V out. Check to see if the right-ventricular CENELEC waveform output flag isenabled (V_FLAG 1). If the flag is enabled, write the next word from the CEN-ELEC waveform table (CEN_TABLE) to the V sense D/A converter.• Test LVS out. Check to see if the left-ventricular CENELEC waveform output flag isenabled (LVS_FLAG 1). If the flag is enabled, write the next word from the CEN-ELEC waveform table (CEN_TABLE) to the LV sense D/A converter.When Radio Shack Parts Are Not the AnswerResponsive simulators such as the one described earlier can be designed to emulate thedeterministic behavior of a biological system. There are occasions, however, when the relevantphysical properties of the biological system are too complex for simulation with
RESPONSIVE SIMULATORS 289relatively simple electronic circuits. Here comes a story: Circa 1995, there were variousreports about implantable defibrillator patients being shocked when passing through electronicarticle surveillance (EAS) systems, such as those used in stores against shoplifting.There were also reports about pacemaker patients who fainted in the proximity of thesesystems, presumably because their pacemakers were inappropriately inhibited by EMIfrom the EAS.EAS systems consist of electromagnetic field emitters which illuminate and interrogatea uniquely identifiable “tag” which is affixed to an object. When the tagged object is in thefield produced by the EAS equipment, the EAS sensors detect its presence and activate aresponse. Back in our Intermedics 3 days, we conducted much of our research together withDr. Thomas Fåhræus in Lund, Sweden. He became very interested in the potential problemof pacemaker interference by EAS systems. After all, EAS systems are widely used totrack and monitor merchandise, for inventory control and theft prevention, and in somecases, to track living specimens. Because of their widespread use in retail stores and commercialestablishments, wearers of implantable medical devices have a high likelihood ofentering the fields produced by such systems.Thomas terminated a ventricular bipolar pacemaker lead with a LED to be able to tellwhen the pacemaker paced normally, and built a simple setup simulating an implantconfiguration (Figure 6.29). He programmed the pacemaker to the VVI mode and a lowpacing frequency (e.g., 40 ppm). He then toured the shops in Lund looking for signs ofEAS interference on his pacemaker implant simulation. If the LED stopped blinking, thatmeant that the EAS system was inhibiting the pacemaker. If the LED started to blink rapidly(e.g., 70 ppm), on the other hand, that meant that the pacemaker had entered its noisereversion mode.Thomas called us in alarm when he found that most of the EAS systems in town interferedwith his pacemaker setup. However, that observation was not consistent with whatwe were seeing with real implants. Patients were not falling dead like flies when walkingthrough EAS systems. In fact, most of the cell phone and EAS interference reports werehighly anecdotal, to the point where they reeked of urban myth. It wasn’t difficult toexplain the difference between the test setup and a real implant. The LED was acting asthe detector diode in a crystal radio. The interfering signals were really generated by theLED’s nonlinearity, an element that is negligible in the real implant situation.Thomas was very ingenious in replacing his pacing detector by a more realistic kind. Hefigured out that the tongue can detect the pacing pulses while making the electrode–tissueinterface similar to that of the real implant. This time he made us all accompany him withdifferent pacemaker models on his interference hunting trip. It was not even April 1, andthere we were, in the best stores of downtown Lund, with wires stuck in our mouths, movingbizarrely next to the shoplifting gates. Good that everyone in town knew that Fåhræuswas a respectable physician. End of the story: Our not-too-scientific study found noevidence of pacemaker interference by EAS systems. No one really wanted to checkwhether or not a defibrillator would react differently.This is why when determining the effects of electromagnetic environments onimplantable medical devices, it is essential that the measurements be performed while operatingthe test devices in an environment that simulates the absorption and shielding characteristicsof the human body. A common physical test environment consists of a 0.027 Msaline solution in a rectangular tank that is essentially transparent to the incident radiatedfield. The 0.027 M NaCl concentration has a resistivity of approximately 375 Ωcm, whichis used to simulate the electrical characteristics of the human body tissue and fluid.3Intermedics was the world’s third-largest implantable cardiac pacemaker/defibrillator company. It was acquiredby Guidant Corporation in 1998.
290 SIGNAL SOURCES FOR SIMULATION, TESTING, <strong>AND</strong> CALIBRATIONEAS SYSTEMOSCILLATORIMPLANTABLEPACEMAKERTELEMETRYCOILEAS TRANSMITTER ANTENNARV PACING CIRCUITRV TIPLEAD's INDUCTANCEPACEMAKERPACING LEAD4700pFRA PACE UNI/BIPOLARPACEMAKERCONTROL LOGICRV SENSE UNI/BIPOLARLEDRV RING4700pFEAS RECEIVER ANTENNATITANIUMCANPACEMAKER VDDLiI BatteryPACEMAKER VSSMagneticReed SwitchEAS RECEIVERFigure 6.29 A ventricular bipolar pacemaker lead with a LED does not make a good simulation setup to evaluate how electromagnetic environmentssuch as those generated by electronic article surveillance systems (EAS) interfere with implantable pacemakers and defibrillators.The LED acts as the detector diode in a crystal radio. Interfering signals are then demodulated by the LED, giving a false indication that thedevice is susceptible to electromagnetic interference.A torso simulator model standard is now used by the pacemaker industry. The setup isdescribed in ANSI/AAMI standard PC69:2000 (EMC Test Protocols for ImplantableCardiac Pacemakers and Implantable Cardioverter Defibrillators), Annex B, and wasbased on research by Ruggera et al. [1997]. Figure 6.30 shows a torso simulator that ourcolleague Paul Spehr constructed based on the standard to test the immunity of pacemakersagainst cellular telephone interference. The materials used were:• White louver light grid (nonconducting), Home Depot part 074567432008• Under-bed box 28-qt/27-L Sterilite No.1856 white, 23 1 in. 17 in. 6 in.4(59 cm 43 cm 15 cm)• Stainless steel nuts and bolts, 10-24 1 in. Phillips head and nut, four each2• Titanium sheet• Silicone adhesive sealant• Four-foot nylon threaded rod, 1 -13 2
Figure 6.30 A torso simulator model for electromagnetic interference studies can be constructed using some white louver light grid (used influorescent lamp assemblies) and a 28-qt under-bed plastic box. Tissue properties are simulated using 0.027 M saline solution. Four electrodeson the sides of the box are used to monitor operation of the “implanted” device as well as to inject simulated intracardiac electrogram signals.291
292 SIGNAL SOURCES FOR SIMULATION, TESTING, <strong>AND</strong> CALIBRATION• Nylon 1 -13 hex nut2• Monofilament, 20-lb test, Shakespeare OMNIFLEXR fishing line• Five gallons of supermarket distilled water• Sodium chloride, NaCl USP grade (Kosher salt works equally well)The titanium sheet stock was cut to four pieces 5 cm 5 cm. Holes were drilled in thecenter of each plate to allow for attachment with screws. Holes were drilled in the centerof each side of the 28-qt plastic box. Stainless steel screws were coated with silicone adhesiveand then used to attach the titanium pieces to the inside of the box, providing electricalconnection to the outside of the box. The louver grid was cut to give two pieces, onefitting the top ridges and one on the bottom. Six nylon nuts were attached to the bottomgrid with medical adhesive. The nylon threaded rod was cut to 4-in. lengths, six each. Aslot was cut in the top of each rod.The saline solution should be prepared to the proportions recommended by ANSI/AAMI PC69:2000, Table 2: 0.027 M 1.8 g/L or 0.18% NaCl concentration at 21°C. Todo so, the salt is first dried in an oven set at 200°C for 30 minutes. Then 30.6 g of dry saltcan be added to 17 L of distilled water to make enough solution with a concentration of1.8 g/L. Submersion in a conducting fluid facilitates monitoring of the implantable medicaldevice’s operation while minimizing the electromagnetic field distortion and detectioneffects of directly attached probes. Monitoring of the implantable medical device’sresponses to the applied electromagnetic environment is accomplished by sampling thetest device’s output pacing pulses via the square electrodes submerged in the saline solution.The potentially interfering signals are applied and their magnitude is graduallychanged while the response of the medical device is monitored.Pacemakers and defibrillators are usually tested in each of their normal operatingmodes, and test equipment is set up to determine if, and when, the test device is inhibitedor operating in its noise mode. To do so, these tests are conducted both with and withoutexternal simulated intracardiac electrogram signals injected via the saline solution into thesensing inputs of the test device.Shocking WaterWhereas simulating a single biopotential signal channel is not too complex, generatingaccurate signals to validate array processing methods is very problematic. Take, for example,the case of validating the performance of inverse solutions. In inverse electrocardiography,researchers attach a large array (e.g., 128 or 256 electrodes) of electrodes to thechest instead of the usual 12-lead ECG. The idea is to process the array ECG signals, takinginto consideration the specific geometry of the chest and body organs to create threedimensionalimages of the potentials in the heart muscle itself. The potential of such atechnique is tremendous. It would give physicians a noninvasive method to identifypatients at risk of sudden death, for specific diagnosis of rhythm disorders, and for localizationof disturbances in the heart in order to guide intervention.Several computational approaches that attempt to solve the electrocardiographic inverseproblem have been developed to estimate heart surface potential distributions in terms oftorso potentials, but to date their suitability for in vivo and clinical situations has not beenfirmly established. The same can be said about the solution of other inverse problems inbiomedical engineering, such as inverse electroencephalography and electrical impedancecomputed tomography. Before any inverse electrical imaging procedure can be used as anoninvasive diagnostic tool with confidence, it must first be validated so that recordedexperimental observations can be faithfully reproduced.
Experimental validation studies for inverse imaging solutions can involve animal preparations,completely synthetic physical materials, or even a combination of the two in order tosimulate the ideal conditions of biopotential sources inside a human body. Because of thetechnical challenges of measuring source parameters and geometry from animal models, mostvalidation studies for inverse problems use synthetic electrical sources embedded in conductingmedia as a way to obtain controlled physical models of the source organ and body.Early modeling of the heart for inverse electrocardiography experiments used a currentbipole to simulate the source because it is a direct equivalent of the single heart dipole vectorthat still serves as the basis of much of clinical electrocardiography. A potentiostat–galvanostat is a general-purpose instrument that may be used for controlling either thepotential difference between the electrodes of the bipole source (potentiostatic operation)or the current between them (galvanostatic operation).Figure 6.31 shows the circuit for a potentiostat–galvanostat. When the potentiostat–galvanostat switch (SW1) is set for potentiostatic (constant-voltage) operation, the potentialdifference between the “active” and “reference” electrodes is fed into the error amplifierIC1, where it is compared against the control voltage. Any error existing between thesetwo potentials will be amplified by IC1 and buffered by IC2, causing a current to flowbetween the active and reference electrodes. This imposed current will force the potentialdifference between the electrodes to move in a direction so as to reduce the error betweenit and the control voltage. In a very short time (~1 ms) a steady state will be achieved inwhich the current is just sufficient to maintain a very small error voltage.With the potentiostat–galvanostat select switch set for galvanostatic operation, the voltagefrom current-sensing resistor R1 is amplified by IC4 and fed into the error amplifierIC1, where it is compared against the control voltage. As described above, the erroramplifier will amplify any error existing between the two voltages, causing some additionalcurrent to flow between the electrodes so as to reduce the error voltage. A steadystate is achieved when the error becomes very small. However, in this case it is the current,not the electrode potential, which is maintained at the desired value.The control voltage can be dc or ac. With the component values shown in Figure 6.31,the electrode potential difference or electrode current will track the control voltage as longas the input signal is limited to the range dc to 300 Hz. IC5A and IC6A buffer the electrodevoltage and current signals from the outputs of IC3 and IC4. These can be monitoredthrough an oscilloscope to evaluate the dc or ac impedance of the electrodes.Probably the simplest physical models used to shed light on the inverse problem in electrocardiographywere two-dimensional models. Grayzel and Lizzi [1967] used conductivepaper (Teledeltos) to create two-dimensional inhomogeneous models of the human thorax,to which they attached current source–sink pairs (bipoles) to represent the heart. Teledeltospaper is a resistive paper that has uniform resistance. As shown in Figure 6.32, Teledeltospaper can simply be cut, after suitable scaling, to the shape of the body region to be investigated.Then electrodes are painted on the paper with conductive silver ink so that sources(voltage and current sources, and sinks or loads) can be attached to the paper at the appropriateplaces to set up an analog of the boundary conditions desired. The extent and valueof inhomogeneities are controlled by means of perforations or silver spots applied to theconductive paper. The ratio of hole diameter to hole spacing determines the relativeincrease in resistivity of the area punched. The ratio of silver-dot diameter to center spacingdetermines the relative decrease in resistivity.To find solutions, one simply reads out the field intensity values by using a sharp-tippedvoltmeter probe applied to the paper at any point that field intensity is desired. Thus, a verysimple laboratory setup can be used to solve sets of complicated partial differential equationsempirically without the user even knowing what partial differential equations he orshe is actually solving!RESPONSIVE SIMULATORS 293
294Figure 6.31 A potentiostat–galvanostat is a general-purpose instrument that may be used for controlling either the potential differencebetween the electrodes of the bipole source (potentiostatic operation) or the current between them (galvanostatic operation). The control voltagecan be dc or ac, and the electrode potential difference or electrode current will track the control voltage as long as the input signal is limitedto the range dc to 300 Hz.
RESPONSIVE SIMULATORS 295One Teledeltos Square∂Jy[ Jy +∂yδy ] δxJxδyδyδx[ Jx +∂Jx∂xδx]δyJyδxTeledeltos Torso cut-outHigh InputImpedanceDVMDCSupplyV to I ConverterPin holed regionCarbon PaperGraph PaperFigure 6.32 Teledeltos paper is a resistive paper that has uniform resistance. It can be cut to the scaled shape of the body region to be investigated.Electrodes painted with conductive ink allow connection to current–voltage sources. Inhomogeneities are introduced by means ofperforations or silver spots (e.g., pinhole region simulating lungs). Field intensity values are read with sharp-tipped voltmeter probes. A sheetof carbon copy paper and graph paper make it easy to trace equipotential lines and gradients.Consider how Teledeltos can be used to solve electrical field problems. The current flowis essentially in two dimensions (i.e., across the surface of the paper but not through itsthickness from one face to the other). Suppose that the vector J(A/m) represents the currentdensity per unit width at some point on the Teledeltos sheet. Then the electric field (orvoltage gradient) at the same point in the sheet isE Jρ(V/m)where ρ is the specific resistance of the sheet. Teledeltos paper has a uniform grid printedon it, and ρ represents the resistance between opposite sides of a grid square.
296 SIGNAL SOURCES FOR SIMULATION, TESTING, <strong>AND</strong> CALIBRATIONNow consider a square element of the surface of the Teledeltos paper. The net outflowof current from the element isδy J x ∂ Jx∂xJyδx δxJy ∂∂ δy yδyJx δxJy δy ∂ ∂ δx xδx ∂ ∂JxJδy y yneglecting terms in δy 2 and δy 2 . Since we are considering a steady state, there must be nonet rate of loss or accumulation of charge in the element. Thus, the expression given abovemust be equal to zero. Dividing by the area of the element yields ∂ J∂ x ∂ Jyx ∂ 0yThe relationship, called the equation of continuity, applies to the flow of any fluidlike materialwhose volume or quantity does not change when flowing across a region in steady conditions.It applies to the flow of heat, fluids, electricity, and mass particles. In this case itshows that the current flows completely through the element without shedding any charge.In the days before digital computers were able to run finite-element models, Teledeltospaper was used to quickly obtain practical solutions to tough electromagnetic, thermodynamic,and hydrodynamics problems.Back to our discussion on modeling with Teledeltos, the electric field E across the surfaceof the sheet may be expressed in terms of the potential V byE ∂ Vx ∂ Vy ∂x∂y∇Vwhere x and y are unit vectors along the x and y axes. Then the continuity equation can berewritten as ∂ 2V2V∂x2 ∂∂y2 ∇ 2 V 0This equation, commonly referred to as Laplace’s equation, at first glance looks difficultto solve. Although there are many known solutions, the problem is to find a solution thatfits the given boundary conditions. Obviously, the solution given by Teledeltos paper is theone that completely satisfies the analog boundary conditions modeled using cutouts and/orpainting conductive silver ink. Don’t disregard Teledeltos just because it is “old-fashioned.”By applying just a bit of common sense, you can use this simple, elegant method to solvevery complicated problems.PASCO Scientific sells black conductive paper to go along with its E-field mapping kit.One hundred sheets of conductive paper marked with a centimeter grid sells for $30 (partPK-9025). You can make electrodes using the type of conductive silver ink pen that is usedfor PCB repairs (which you can also buy from PASCO as part PK-9031B) or by attaching3M’s 1181 electrical tape, which is copper foil with a conductive acrylic adhesive.Using the simple Teledeltos model, Grayzel and Lizzi [1969] were able to find that the relationshipbetween source location and body surface, as expressed by the standard lead field,was much more variable and complex in the inhomogeneous than in the homogeneous torso.This led them to the conclusion that several “standard” lead systems of their day showed asharp deterioration in performance after adding inhomogeneities to the torso model.Burger and van Milaan [1948] opted for a more realistic three-dimensional model andconstructed an electrolytic tank out of a michaplast shell molded on the statue of a supinehuman to create a torso model. The tank split horizontally to provide access to the interior,which was filled with copper sulfate and outfitted with copper foil electrodes fixed to the
inner surface. Their heart source model was a set of copper disks oriented along one of thebody axes and adjustable from outside the tank by means of a rod. The tank includedinhomogeneous regions constructed from cork and sandbags to simulate the electrical distortionscaused by the spine, ribs, and lungs. Other investigators have used inflated doglungs and agar gel models of human lungs inserted into the tank.If your research calls for an electrolytic body-shaped tank, a visit to your local hobbyand crafts store will prove invaluable. Describe what part of your anatomy you would liketo make a cast of, and the store’s attendant’s will help you select the best materials andtechniques. (Hint: don’t ask for “michaplast.”) For the electrolyte solution you can use isoconductivesaline made by mixing 1.8 g of noniodized salt (use Kosher salt if you don’twant to overpay for analytical-grade NaCl) per liter of distilled water (supermarket distilledwater is okay). Electrodes should be Ag/AgCl, and inhomogeneous regions to simulatethe lungs and other organs can be cast of high-density agarose gel (e.g., any standardagarose gel with about 1200 g/cm 2 strength, melting range about 87 to 89°C, gelling rangeabout 36 to 39°C, sold by VWR Scientific) or synthetic sponge foam.As shown in Figure 6.33, a bipolar electrode to model cardiac potentials can be made fromtwo Ag/AgCl disk electrodes, some plastic tubing, and epoxy adhesive. This bipolar source isfashioned after the one described by Brandon et al. [1971]. It yields a source with uniform distributionsof current, 3 mm in diameter, separated by 12.7 mm. The potentiostat–galvanostatof Figure 6.31 makes an excellent current source to drive this bipolar electrode.Electrolyte tanks have also been used to investigate the way in which currents appliedthrough skin electrodes distribute within the body to cause tissue stimulation. This is animportant issue in external pacing, where high-voltage pacing pulses applied through skinsurfaceelectrodes not only cause the heart to contract, but cause quite a bit of pain to thepatient. Another area of special interest in the solution of the same problem of stimulationoverflow to nontarget tissue is functional neuromuscular stimulation (FNS; see Chapter 7).We [Sagi-Dolev et al., 1995] used a phantom model in which a saline tank model wasimproved by adding a layer to simulate skin impedance properties. The purpose of thestudy was to look for electrode array geometries required to achieve target muscle activationwith minimal overflow and to avoid pain or burning.The tank was a small 40 cm 30 cm 30 cm glass aquarium filled with isoconductivesaline solution to simulate the volume conductor of the human forearm. To simulate theway in which the skin’s epidermis and panniculus adiposus distort the spatiotemporal characteristicsof FNS stimulation pulses, we made a carbon-loaded silicone elastomer that hadsimilar electrical properties to skin.Rosell’s method for the measurement of skin impedance [Rosell et al., 1988] wasadapted to measure the electrode–skin impedance for the specific conductive-silicone electrodematerials used for FNS and for the specific spectral content of the FNS waveform(1 to 9 kHz). A stimulating ring with inside diameter 12.5 mm and outside diameter 15 mmwas constructed from carbon-loaded silicone electrode material (Ag/AgCl electrodesof similar dimensions were used by Rosell). Rectangular 2 mm 5 mm voltage-sensingelectrodes were positioned, one within the center of the stimulating ring and the secondparallel to the first at a distance of 2 mm from the ring as shown in Figure 6.34. The electrodeswere embedded at a depth of 1.5 mm within an isolating cast. The 1.5-mm cavitiesallowed for a consistent conductive gel volume. A large self-adhesive Ag/AgCl ECG electrodewas used as a reference. The isolated amplifier input impedances had an equivalentinput impedance of 1 MΩ in parallel with 20 pF.The average impedance measurements were 7.7 kΩ at 1 kHz and 4.8 kΩ at 10 kHz for a1-cm 2 electrode surface area. By assuming that a parallel resistor–capacitor suitably modelsthe skin impedance, these impedance values result in an equivalent of a 7.64-kΩ resistor inparallel to a 2479-pF capacitor for a 1-cm 2 electrode surface area. The artificial “skin” wasfabricated to match these values. Varying amounts of colloidal graphite (MacDermidPTF4150 flexible graphite conductive paste) and silicone rubber (RTV No. 159) wereRESPONSIVE SIMULATORS 297
298 SIGNAL SOURCES FOR SIMULATION, TESTING, <strong>AND</strong> CALIBRATIONFigure 6.33 A bipolar electrode to model cardiac potentials can be made from two Ag/AgCl disk electrodes, some plastic tubing, andepoxy adhesive: (a) perspective view; (b) section view. This bipolar configuration yields a source with uniform distributions of current, 3 mmin diameter, separated by 12.7 mm.thoroughly blended to form homogeneous pastes, which were then formed and cured intothin layers. Impedances of each sample were then measured using the same setup as before(Figure 6.34) but using a saline-soaked sponge to simulate the arm’s underlying tissues. Thecorrect graphite–silicone rubber ratio was found to be 20% (by weight).Signals within the physical model were measured as shown in Figure 6.35. A differentialprobe was constructed with two gold wires 1 mm in diameter, each exposed 1 mm to thesaline solution and placed 1 mm apart parallel to the y axis representing the long axis ofthe forearm. This distance was chosen because of its physiological significance, since thethreshold potential difference for stimulation of myelinated axons must be reached atapproximately the internodal distance.As shown in Figure 6.36, the computer triggered the delivery of one FNS stimulation pulseby strobing the TRIGGER input. Probe signals were amplified differentially through anAD521K instrumentation amplifier. The signal reference was established through a large plateelectrode placed external to the glass tank. The instrumentation amplifier output was integrated
VERY REALISTIC PHYSIOLOGICAL SIGNAL SOURCES 299OscilloscopeIsolationAmplifiersCH120pF1MICH220pF1MIForearm123ReferenceElectrode1M1.6µFI10Vp-pIsolatedSignalGenerator100KFigure 6.34 Rosell’s method applied to measure electrode–skin impedances using carbon-loaded silicone electrodes: 1, stimulating ringelectrode; 2 and 3, voltage-sensing electrodes. The electrodes are embedded at a depth of 1.5 mm within an isolating silicone rubber cast.(with a time constant given by R3 and C2) throughout the duration of the stimulation phase ofthe FNS pulse to emulate the integration process carried out by the excitable tissue membrane.After the stimulation phase, the integrated voltage was read through the computer’s A/D card.The actual position of the probe was measured by digitizing the voltage output from the x-, y-,and z-axis potentiometers linked to the three-dimensional manipulator. The computer reset theintegrator by strobing the RESET line prior to taking a new measurement.VERY REALISTIC PHYSIOLOGICAL SIGNAL SOURCESNo physical model can really replace the biological realism that can be achieved with anintact animal model with implanted instrumentation. However, the intact animal presentsthe problem that body geometry and exact organ configuration are very difficult to integrateas part of an experimental study. A compromise solution is to use an isolated preparationof the organ generating the biopotentials placed in a synthetic volume conductor thatsimulates the human cavity holding the organ.
300 SIGNAL SOURCES FOR SIMULATION, TESTING, <strong>AND</strong> CALIBRATIONsignalprocessorcomputerFNSstimulatorthree degrees-of-freedommanipulatorglass tanksimulated skin layersaline solutionprobereference plate electrodeFigure 6.35 An electrolyte tank can be used to investigate how FNS currents applied throughskin electrodes distribute within the body to cause tissue stimulation. The setup consists of a40 cm 30 cm 30 cm glass tank (a small aquarium) filled with isoconductive saline. A carbonloadedelastomer layer simulates the patient’s skin. A differential probe made with two gold wiresexposed 1 mm to the saline solution and placed parallel 1 mm apart simulate the stimulation spatialconstant of myelinated axons. (From Sagi-Dolev et al. [1995]. Reprinted with permission from theInternational Federation for Medical & Biological Engineering.)A common trend in recent studies for the validation of inverse electrocardiography hasbeen to replace the synthetic signal source with a perfused dog heart, thus achieving amuch higher degree of realism by eliminating the limitations of representing the heart asa single dipole rather than as a distributed source of bioelectric current. Obviously, themain advantages of this type of preparation over instrumented whole-animal experimentsare the relative ease of carrying out the experiments and the increased level of control theyprovide. The isolated heart is directly accessible when suspended in an electrolytic tank,which permits manipulations of its position, pacing site, coronary flow, and temperature.The simplified geometry of the tank also makes constructing customized geometric modelssimpler and faster than when a complete medical imaging scan is required for a wholeanimal.Isolated heart systems are available from Hugo Sachs Electronik (now part of HarvardApparatus). The isolated heart apparatus uses a synthetic bloodlike solution to provideoxygen and metabolic substrates for the heart to survive. Since the coronary system of theheart relies on the pressure created by the heart itself for flow, the heart must be assistedexternally after explant from the donor animal. This is accomplished by pumping fluiddirectly into the coronary system and removing fluid from the heart’s four chambers toease the burden using a technique called the Langendorff mode of perfusion. Once theheart is capable of maintaining pressures and flows independently, it is weaned out ofLangendorff mode and the native flow pattern is reestablished. At that point the heart issaid to be in the four-chamber working mode, in which it generates pressures in all fourchambers and is responsible for the work required to maintain flow through the coronarysystem, hence the name.
..--R+-111698134TO A/DIN1IN2IN3IN4V+V-J1OUTPUTIC2D1D2D3D4S1S2S3S4DG21112TTLSYNC+5VTTL REFFNSSTIMULATOROUTPUT~250VR1100kGAINADJUST+5VSTIMULATION PHASED1FDH300+15VD2FDH300+15V+15VR2100kTRIGGERTTL REFC10.1uF28 1410IC121510731411FNS STIMULATOR_1GLASS TANKOUT+OUT-TTL SYNCTRIGGER6TTLREF"SKIN"FNSELECTRODEARRAYR7100kR4100kR8100k+5VGRID3 D.O.F.MANIPULATORSALINESOLUTIONPROBE Z POSITIONPROBE Y POSITIONPROBE X POSITIONTOA/D-15VD3FD-15VD4FDH300C5C6R610M13+5 13 4 6 9-15V11712AD521K327 1+IC3TL08160.1uFR510M0.1uFC30.1uFR324kC23000pFC40.01uF+15VPROBEC8+1mm10uFC7C94 5+0.01uF -15V10uFNYLON BOLT+15V-15VREFERENCEELECTRODEARM SIMULATOR(SIDE VIEW)Figure 6.36 After the computer triggers the FNS stimulator, the energy deposited on the probe by the stimulation phase of the FNS signalis amplified through an instrumentation amplifier and integrated by R3 and C2. After the stimulation phase, the integrated voltage can beread through the computer’s A/D card. The actual position of the probe can be measured by digitizing the voltage output from the x-, y-, andz-axis potentiometers linked to the three-dimensional manipulator.TRIGGER301
302 SIGNAL SOURCES FOR SIMULATION, TESTING, <strong>AND</strong> CALIBRATIONUnfortunately, this preparation inevitably builds up metabolites and electrolytes whichchange its electrophysiological characteristics within a few hours of explant. To overcomethis problem, many investigators [MacLeod et al., 1995] use a second dog to provide circulatorysupport for the isolated heart, which achieves very stable physiologic conditionsover many hours (Figure 6.37). This preparation makes it possible to regulate coronaryflow rate and blood temperature. In addition, it allows the infusion of cardioactive drugs toexamine the effects of physiological change on forward and inverse solutions, since thesupport dog eliminates the drugs and their metabolites through its urine output.This model has a high level of realism, yet maintains adequate control over the relevantparameters. The tank can be made to have a shape identical to the human torso and can beinstrumented with an almost unlimited number of recording electrodes located both on thesurface and within the volume of the tank. Agarose or conductive polymer “lungs” and“ribs” can be placed in the tank to simulate volume conductor inhomogenities. The isolatedanimal heart provides a very realistic and versatile bioelectric source which can beinstrumented and manipulated to mimic many pathologies; for example, burns can bemade on the myocardium to simulate myocardial infarcts.Despite this flexibility, the model is not perfect. To start with, there is no autonomicnervous system present in the isolated heart, so that many responses to external physiologicalinfluences do not mimic the behavior of a real human heart. In addition, themechanical behavior is altered significantly because it hangs freely in the electrolyte withouta pericardium or the constraining influences of other organs.Blood flowJugular veinCarotidarteryIsolated dog heartSupportdogElectrodesTorso-shaped tankFigure 6.37 An isolated dog heart and human-shaped electrolytic tank have been used for validationof inverse electrocardiographic methods. This type of preparation uses a second dog to providecirculatory support for the isolated heart, which achieves very stable physiologic conditions overmany hours.
REFERENCES 303We believe that experimental studies in the bioengineering field should be done, aboveall, to advance the development of methods to diagnose and cure disease. At the end of theday we must remember that men are not mice—simulation can go only so far. There is nomodel that can substitute completely for a human patient.REFERENCESBachiochi, J., Creating a Nonvolatile RAM Module, Circuit Cellar INK, 65–71, August–September1990.Belusov, A., Programmable Impedance Has 12-bit Resolution, EDN, 105, May 23, 1996.Brandon, C. W., D. A. Brody, C. P. Eddlemon, H. A. Phillips, and F. H. Terry, A Bipolar Electrodeand Current Pump for Volume Conductor Experiments, IEEE Transactions on BiomedicalEngineering, (1), 70–71, 1971.Burger, H. C., and J. B. van Milaan, Heart-Vector and Leads—Part III: Geometrical Representation,British Heart Journal, 10, 229–233, 1948.Craswell, J., Weekend DigiVFO, QST, 30–32, May 1995.Grayzel, J., and F. Lizzi, The Combined Influence of Inhomogeneities and Dipole Location,American Heart Journal, 74, 503–512, 1967.Grayzel, J., and F. Lizzi, The Performance of VCG Leads in Homogeneous and HeterogeneousTorsos, Journal of Electrocardiology, 2(1), 17–26, 1969.MacLeod, R. S., B. Taccardi, and R. L. Lux, Electrocardiographic Mapping in a Realistic Torso TankPreparation, Proceedings of the IEEE Engineering in Medicine and Biology Society 17th AnnualInternational Conference, 245–246, IEEE Press, Piscataway, NJ, 1995.Portugal, R. J., Programmable Sinewave Generator, Electronics Now, 43–66, January 1995.Prutchi, D., Designing Printed Circuits for High-Speed Logic, Circuit Cellar INK, 38–43, January1994.Rosell, J. J., Colominas, P. Riu, R. Pallas-Areney, and J. G. Webster, Skin Impedance from 1 Hz to1 MHz, IEEE Transactions on Biomedical Engineering, 35, 649–651, 1988.Ruggera, P. S., et al., In Vitro Testing of Pacemakers for Digital Cellular Phone ElectromagneticInterference, Biomedical Instrumentation and Technology, 31(4), 358–371, 1997.Sagi-Dolev, A. M., D. Prutchi, and R. H. Nathan, Three-Dimensional Current Density Distributionunder Surface Stimulation Electrodes, Medical and Biological Engineering and Computing,33(3), 403–408, 1995.
7STIMULATION <strong>OF</strong> EXCITABLE TISSUESAn electrically excitable cell in its resting state is essentially a charged capacitor. The cellmembrane is the dielectric, the ionic solutions on either side of the membrane constitutethe plates, and differences in the concentrations of ions on each side generate a potentialdifference of about 70 to 90 mV (measured inside the cell against a reference in theextracellular fluid). To generate an action potential, the membrane capacitance must bedischarged by about 15 mV in a small region. This results in a brief sequence of openingsand closings of sodium and potassium channels in the membrane, which results in the flowof the action current. The action current depolarizes and then repolarizes adjacent regionsof the cell membrane, giving rise to the action potential.Excitable cells can be activated by a variety of stimuli, which include burning, mechanicaltrauma, electrical currents, and very intense variable magnetic fields. If sufficientlystrong, any of these stimuli can depolarize the membrane of the excitable cells to a thresholdvoltage level at which the regenerative mechanisms of the action potential take over.However, the most common method of stimulating excitable tissue artificially is to pass anelectrical current through the target tissue.Hodgkin and Huxley’s classical experiments on excitable cells were carried out by placingelectrodes inside the cells under study. They wisely chose a huge cell membrane (atleast as far as cells go), the giant squid axon, to make it easier to manipulate the electrodeswithout destroying cells. To analyze the nonlinear properties of ion conductances underlyingaction potentials, Hodgkin and Huxley [1952] used the voltage-clamp technique 1developed by Kenneth Cole. As shown in Figure 7.1, space-clamp experiments usuallyinvolve inserting two electrode wires into the axon, one for recording the transmembranevoltage and the other for passing current into the axon. In the voltage clamp, the same1Cell electrophysiology is outside the scope of this book. However, if you are interested in the subject, we wouldlike to refer you to what we consider is the most no-nonsense source of information on cell electrophysiologyand biophysics techniques: Axon Instruments Inc. publishes The Axon Guide for Electrophysiology & Biophysics,which is a practical laboratory guide covering a broad range of topics, from the biological basis of bioelectricityand a description of the basic experimental setup (including how to make pipette microelectrodes) to the principlesof operation of advanced electrophysiology lab hardware and software. Best of all, you can download thecomplete guide free from Axon’s Web site at www.axon.com/MR_Axon_Guide.html.Design and Development of Medical Electronic Instrumentation By David Prutchi and Michael NorrisISBN 0-471-67623-3 Copyright © 2005 John Wiley & Sons, Inc.305
306 STIMULATION <strong>OF</strong> EXCITABLE TISSUESiReferenceElectrodeExtracellularFluidStimulatingElectrodeAxonRecordingElectrodeV membraneFigure 7.1 The classical space-clamped current-pulse stimulation of the giant squid axon is simulated by the Matlab program HODKIN-HUXLEY.M using Hodgkin and Huxley’s membrane model.setup is used as in the space clamp, but the current source is driven by a voltage-feedbackcircuit to keep the transmembrane voltage constant (or “clamped”) at any value desired,providing a reading of the amount of current required to do a task. Since current is proportionalto conductance at a constant voltage, this gives a measurement of the membraneconductance. In contrast, a measurement of the membrane potential without the voltageclamp shows little about the membrane conductance.Using a voltage clamp, Hodgkin and Huxley forced open selective ion channels thatreside in the membrane and are normally closed at rest and reveal themselves by the currentthat suddenly flows through them. The potassium current was separated experimentallyby either bathing the axon in a sodium-free solution or by adding a selectivesodium-channel blocker, the puffer fish poison tetrodotoxin (TTX). To determine thesodium current, they then subtracted the potassium current from the total current.[Today, the selective blocking agent tetraethylammonium or (TEA) may be used to isolatethe sodium current.] Based on their experiments, Hodkin and Huxley came up withan empirical model of an excitable membrane. A Matlab program (HODKINHUX-LEY.M, available in the book’s ftp site) can simulate the behavior of the axon membranebased on their model and can be used to play neurophysiologist without acquiring thesquid-slicing skills of a sushi chef.Figure 7.2 shows what happens when the simulated axon setup of Figure 7.1 is stimulatedwith weak (1 µA/cm 2 ) and strong (10 µA/cm 2 ) depolarizing ( electrode inside the cell) andhyperpolarizing ( electrode inside the cell) stimuli. The change in membrane voltageevoked by the weak stimuli is related primarily to the change in charge across the membrane’s
STIMULATION <strong>OF</strong> EXCITABLE TISSUES 307Figure 7.2 Simulation results from the stimulation of a giant squid axon with weak (1 µA/cm 2 ) and strong (10 µA/cm 2 ) depolarizing (positiveelectrode inside the cell) and hyperpolarizing (negative electrode inside the cell) stimuli. (a) and (b) The change in membrane voltageevoked by the weak stimuli is related primarily to the change in charge across the membrane’s capacitance. (c) A strong depolarizing stimulus(10 µA/cm 2 ) takes the membrane voltage over the threshold, causing action potentials for the duration of the stimulus. (d) A stronghyperpolarizing stimulus (10 µA/cm 2 ) yields an action potential at the trailing edge of the pulse through rebound excitation.capacitance. However, the strong depolarizing stimulus (10 µA/cm 2 ) takes the membranevoltage over threshold, causing action potentials for the duration of the stimulus.The strong hyperpolarizing stimulus (10 µA/cm 2 ) also yields an action potential, butonly at the trailing edge of the hyperpolarizing pulse. This is what Hodgkin and Huxleyreferred to as anode break excitation or rebound excitation. The hyperpolarizing pulsedecreases the potassium conductance and removes sodium inactivation. The former leadsto less hyperpolarizing current and the latter to more depolarizing current. Since the kineticsof the potassium channels are slower than that for the sodium channel gate, a transientdepolarization takes place after a prolonged hyperpolarizing voltage, which if largeenough can generate an action potential.What we would like you to remember as we move to discuss the clinical uses of electricalstimulation is that anodic currents are usually responsible for the activation ofexcitable tissue when the current is delivered through an intracellular electrode. In addition,we would ask you to remember that hyperpolarizing currents can also lead to activationof excitable tissue via the rebound excitation mechanism.
308 STIMULATION <strong>OF</strong> EXCITABLE TISSUESEXTRACELLULAR STIMULATIONIn clinical practice, the stimulation methods used to elucidate the electrical properties ofexcitable cells are simply not suitable. To start with, clinically useful stimulation requiresstimulating much more than a single nerve or muscle cell, making it impractical to buildelectrode arrays that can impale a large number of cells simultaneously. Next, even if asufficient number of cells could be impaled with microelectrodes, it is next to impossible tokeep them in place in a living, moving being. Because of this, in vivo stimulation almostalways involves delivering the stimulating currents between a pair of electrodes placed near(but not inside) the target cells. Consider the simple model of Figure 7.3. Here the vectorcurrent flux is indicated by arrows and transmembrane current is assumed to flow only atthe anode and cathode (in reality it flows at all parts of the cell) when the switch closes. Asshown in Figure 7.3b, the current through the membrane will hyperpolarize the intracellularmembrane region under the anode and depolarize the intracellular region under the cathode.Stimulation will occur when the transmembrane potential at the cathode crosses the(a)+ -I stimAnodeI outCathodeCellI inIntracellularFluidExtracellularFluid(b)Istim+ -IoutR outCM_Anode++++++++++++++- - - - - - - - - - - - -CM_ Cathode- - - - - - - - - - - - -++++++++++++++Outside of CellInside of CellI inRFigure 7.3 Simplified model of electrical stimulation of a cell by a current applied through extracellular electrodes. (a) A transmembranecurrent is assumed to flow only at the anode and cathode. The vector current flux is indicated by arrows. (b) The current through the membranehyperpolarizes the intracellular membrane region under the anode and depolarizes the intracellular region under the cathode.Stimulation occurs when the transmembrane potential at the cathode crosses the membrane’s threshold voltage.
EXTRACELLULAR STIMULATION 309membrane’s threshold voltage. Note that this is the reverse of what happens with intracellularstimulation, where excitation occurs at the anode.Depending on the arrangement of the electrodes, three stimulation modes can be distinguished:1. Bipolar. Both electrodes are close to the target tissue.2. Monopolar (also called unipolar). One electrode, normally the cathode, is close tothe target tissue, and the other (anode) is remote from the target tissue, making itssize and exact placement irrelevant.3. Field stimulation. Both electrodes are remote from the target tissue.The efficiency of bipolar and monopolar stimulation is similar. However, the currentdelivered in the monopolar mode often crosses through nontarget tissue on its way to theanode (yes, the conventional direction for current is in the opposite direction, but you knowwhat we mean) and is sometimes capable of stimulating these nontarget excitable cellsundesirably. Field stimulation is the most inefficient method but is very commonly the preferredmode of current delivery in nonchronic applications since it allows tissues to bestimulated using noninvasive skin-surface electrodes.A stimulus must be of adequate intensity and duration to evoke a response. If it is tooshort, even a strong pulse will not be effective. The stimulation threshold is defined as theminimum strength of stimulus (expressed either in volts or in milliamperes) required foractivation of a target tissue for a given stimulus duration. When thresholds for several durationsare put together on the same graph, a strength–duration curve is formed. The nicething about the strength–duration curve is that with one quick look one can determinewhether or not a stimulus will be effective. Any stimulus that falls above the curve willexcite the target tissue.As shown in the stylized strength–duration curve of Figure 7.4, stimulus current andduration can be mutually traded off over a certain range. For a short pulse, the effectivenessof a stimulus is characterized by the product of current I and duration t, where deliveredcharge Q It. Hence if the amount of charge required to activate the target tissue isQ threshold and the stimulus duration is t, the current I threshold required to achieve activationwill be I threshold Q threshold /t.It would seem from this relationship that the strength–duration curve should show adecline to near zero as stimulus duration is increased. However, the strength–durationcurve of real excitable tissue flattens out with long stimulus durations, reaching an asymptotecalled the rheobase. The root rheo means current and base means foundation; thus,the rheobase is the foundation, or minimum, current (stimulus strength) that will producea response. When the stimulus strength is below the rheobase, stimulation is ineffectiveeven when stimulus duration is very long.The reason for the difference between the actual behavior and that predicted byI threshold Q threshold /t is that the latter assumes that the membrane is an ideal capacitor. Thisis not the case, and the leakage resistance shows its effect during prolonged stimulation(large values of t). The equation fails to predict the charge transfer across the cell membranebecause under these conditions, more membrane current is carried by the leakageresistance and less is used to charge the membrane capacitance. Membrane potential thusrises exponentially to a plateau during prolonged stimulation instead of increasing linearlywith time.The strength–duration curve was characterized by Lapicque [1909] by the value of therheobase (in volts or milliamperes) and a second number called the chronaxie. The rootchron means time and axie means axis. The chronaxie is measured along the time axis andis defined as the stimulus duration (in milliseconds) that yields excitation of the tissue whenstimulated at twice the rheobase strength. In the strength–duration curve of Figure 7.4, the
310 STIMULATION <strong>OF</strong> EXCITABLE TISSUESFigure 7.4 It is possible to see from this stylized strength–duration curve that stimulus current and duration can be mutually traded off overa certain range. The strength–duration curve was characterized by Lapicque by the value of the rheobase (in volts or milliamperes) and thechronaxie, which is measured along the time axis and defined as the stimulus duration (in milliseconds) that yields excitation of the tissuewhen stimulated at twice the rheobase strength. In this example, rheobase 3.5 mA and chronaxie 0.22 ms.rheobase is the minimum stimulus strength that will produce a response, which is the pointat which the curve asymptotes, about 3.5 mA. To determine the chronaxie, simply look forthe stimulus duration that yields a response when the stimulus strength is set to exactlytwice rheobase, or 7 mA. In this example, the chronaxie is 0.22 ms.The strength–duration curve is highly dependent on the type of tissue being stimulated.For example, the chronaxie of human motor nerve is approximately 0.01 ms, about 0.25 msfor pain receptors, and approximately 2 ms for mammalian cardiac muscle. That is whythere is rarely a need for pulses longer than 2 ms in nerve stimulation, whereas a pulsewidth as long as 10 ms is often necessary for direct stimulation of certain smooth muscles.The empirical equations for the threshold current, charge, and energy for a rectangularstimulation pulse areI threshold rheobase 1 chron axietQ threshold rheobase t 1 chron axiet
CLINICAL USES <strong>OF</strong> ELECTRICAL STIMULATION 311Figure 7.5 The strength–duration relationship can be expressed in terms of threshold current, threshold charge, or threshold energy neededto excite a tissue. For a rectangular current stimulus of duration t delivered to a load of resistance r, these relationships are given by I threshold rheobase (1 chronaxie/t), Q threshold rheobase t (1 chronaxie/t), and E threshold rheobase 2 r t (1 chronaxie/t) 2 .2E threshold (rheobase) 2 r t 1 chron axietwhere t is the stimulus duration and r is the resistance of the path through which the currentflows (resistance of the wires, ionic resistance of the medium, and electrode–tissue interfaceimpedance). Figure 7.5 presents the three strength–duration curves in a single graph.In practice, stimulation parameters close to those of the strength–duration curve are seldomused. Owing to small fluctuations of excitability, the target tissue may not always be excitedif the stimulus is only slightly above threshold. For this reason, the stimulus parameters areusually set to at least twice the threshold in applications that require reliable stimulation.CLINICAL USES <strong>OF</strong> ELECTRICAL STIMULATIONClinical electrical stimulation is simply the application of electrical currents to a body, be itfor function or therapy. As we just discussed, the current of electrons passing through the wiresis converted into a current of ions moved within the tissue, which are in turn capable of transportingelectrical charge across the membranes of excitable tissues. The purpose of theseapplied currents is to cause the targeted depolarization of nerve and/or muscle to threshold.
312 STIMULATION <strong>OF</strong> EXCITABLE TISSUESThe most common clinical applications of electrical stimulation are:1. Cardiac pacing. Electrical stimulation of the heart’s chambers relieves or eliminatesthe symptoms of bradycardia (a heart rate that is too slow). Rhythmic stimulation (pacing)increases the heart rate to meet the oxygen needs of the body. Cardiac pacing is discussedin detail in Chapter 8.2. Cardiac defibrillation. High-energy stimulation of the heart (in the form of an electricalshock) interrupts a rapid heart rhythm (tachycardia) so that a more normal rhythmcan be restored. Cardiac defibrillation is discussed in detail in Chapter 8.3. Cardiomyoplasty. A skeletal muscle (e.g., the latissimus dorsi, which attaches at oneend to the upper part of the upper arm bone and spreads out like a fan to attach to the spineand ribs) is dissected free from its normal attachments and then wrapped around the heart. Themuscle is then stimulated to contract in synchronism with the heart. Since skeletal muscle isprone to fatigue, it must first be trained by converting its fibers to fatigue-resistant type 1 musclefibers. Training is done with a low stimulation rate with only one pulse in a burst and overa period of six weeks increasing the repetition rate and the number of pulses in the burst.4. Electroventilation. Electrical stimulation of the phrenic nerve or the diaphragmaticmuscles is used to support ventilation. Candidates for breathing pacing include patientswho require chronic ventilatory support because of spinal cord injury, decreased day ornight ventilatory drive (e.g., sleep apnea), intractable hiccups (chronic hiccups often leadto severe weight loss and fatigue and can have fatal consequences), and damaged phrenicnerve(s). The physiological respiratory function provided by these devices is far superiorto that provided by mechanical ventilators since the air inhaled is drawn into the lungs bythe musculature rather than being forced into the chest under mechanical pressure.5. Diagnostic stimulation of nerves and muscles. Nerve conduction studies are performedroutinely to assess peripheral nerve function. Electrical stimulation is applied to anerve and the nearby EMG signal is measured. This is done to determine the speed of transmissionalong the nerve. It also helps to determine if there is a blockage in the nerve orwhere the nerve connects to the muscle. In a similar way, electrical stimuli delivered at thewrist or behind the knee are used to evoke brain responses to sensory inputs. Thesomatosensory-evoked potentials are detected by coherent averaging of the EEG. Fromthis information, the evaluator may determine whether there is a delay in conduction to thebrain, a blockage at any point, or abnormally low or high activity in the brain. Anothercommon diagnostic use of nerve stimulation is monitoring the depth of neurologicalblocks present in a patient following the administration of muscle relaxant drugs (e.g.,prior to surgery, and after surgery following the administration of antagonist drugs).6. Diagnostic stimulation of the brain. Very brief high-voltage pulses or pulse bursts tostimulate percutaneously human motor cortex, visual cortex, or spinal cord are used forintraoperative monitoring as well as for diagnosis of neurological diseases.7. Pain relief. The technique of applying electric currents to the spinal cord or a peripheralnerve to relieve pain is known as electroanalgesia. Its use with both permanentlyimplanted and nonsurgically applied devices is common practice in the treatment ofpatients suffering from chronic pain.8. Control of epileptic seizures. Electrical stimulation of the vagus nerve [also knownas vagus nerve stimulation (VNS)] involves periodic mild electrical stimulation of thevagus nerve in the neck by a surgically implanted device. VNS has been found effective incontrolling some epilepsies when antiepileptic drugs have been inadequate, their sideeffects intolerable, or neurosurgery has not been an option. In some cases VNS has alsobeen effective in stopping seizures. It carries minimal side effects (e.g., mild tingling sensationsand voice hoarseness during stimulation), but unlike many medications, there seemto be no significant intellectual, cognitive, behavioral, or emotional side effects to VNStherapy. VNS is now the second most common treatment for epilepsy in the United States,and the improvement in seizure control is comparable to that of new antiepileptic drugs.
9. Control of Parkinsonian tremor. Electrical stimulation of neuron clusters deep insidethe brain [also known as deep brain stimulation (DBS)] is now used to inactivate the subthalamicnucleus, which is overactive in Parkinson’s disease. A multielectrode lead isimplanted into the ventrointermediate nucleus of the thalamus. The lead is connected to apulse generator that is surgically implanted under the skin in the upper chest. When thepatient passes a magnet over the pulse generator, the device delivers high-frequency pulsetrains to the subthalamic nucleus to block the tremor.10. Gastric “pacing.” Electrical stimulation of the stomach is currently being used toreduce symptoms of nausea and vomiting for patients suffering from gastroparesis (a stomachdisorder in which food moves through the stomach more slowly than normal).11. Restoration of lost sight. Electrical stimulation of the retina, the optical nerve, andthe visual cortex is now developed to the point at which implants for functionally restoringsights to blind patients will soon be available commercially. Functional sight may begiven to patients blinded by retinitis pigmentosa by using integrated circuits embedded incontact with the retina. The ICs contain an array of photovoltaic cells that directly poweran array of microstimulators and electrodes to convert the image into a directly mappedelectrical image, bypassing degenerated photoreceptors and directly stimulating theremaining nerve cells in the retina. For patients with blindness caused farther down theoptical nerve, the possibility exists of stimulating the visual cortex directly using microelectrodearrays to generate coherent images from phosphenes (sensation of a spot of light)elicited by the electrical stimulation.12. Restoration of lost hearing. Cochlear implants stimulate spinal ganglion cells of theauditory nerves, bypassing nonfunctional hair cells to restore limited hearing in some typesof deafness. The cochlear implant system really consists of an implanted stimulator connectedto an electrode array inserted in the cochlea and an external speech processor thatcodes the speech into stimulation patterns that can be translated back into sounds by thebrain. The external speech processor also powers the implant via an inductive energy transferlink. Cochlear implants are now common and provide substantial benefits to many profoundlydeafened children and adults. Benefits vary by person and range from increasedperception of environmental sounds to the ability to use a telephone.13. Restoration of lost or impaired neuromuscular function. Functional electrical stimulation(FES), also known as functional neuromuscular stimulation (FNS), is a rehabilitationstrategy that applies electrical currents to the nerves that control paralyzed muscles inorder to stimulate functional movements such as standing or stepping. FNS systems includeeither skin-surface or implanted electrodes, a control unit which often also receives motioninformation back from sensors, and a stimulus generator. A number of FNS units are noweither available commercially or under clinical investigation. Typical applications of FNSinclude controlling foot drop, enabling lower-limb paraplegics to stand or sit, and restoringhand function to the paralyzed upper limb.14. Maintenance or increase in range of movement. Electrical muscle stimulation(EMS) is used to strengthen muscle and facilitate voluntary motor function. AlthoughEMS devices are often advertised for muscle toning and weight reduction, they are authorizedby the FDA only as prescription devices for maintaining or increasing range ofmotion, relaxation of muscle spasm, prevention or retardation of disuse atrophy, musclereeducation, increasing local blood circulation, and postsurgical stimulation of calf musclesto prevent the formation of blood clots.15. Electroconvulsive therapy (ECT). This is a relatively painless procedure that iseffective in treating major depression. A short, controlled set of electrical pulses isgiven for about a minute through scalp electrodes to produce generalized seizures.Biological changes that result from the seizure are believed to result in a change inbrain chemistry which is believed to be the key to restoring normal function. Becausepatients are under anesthesia and have taken muscle relaxants, they neither convulsenor feel the current.CLINICAL USES <strong>OF</strong> ELECTRICAL STIMULATION 313
314 STIMULATION <strong>OF</strong> EXCITABLE TISSUESTABLE 7.1Typical Parameters Used in Various Clinical Applications Involving the Stimulation of Tissues with Electrical CurrentsClinical Typical Method of Typical Typical CurrentApplication Current Delivery Waveform or VoltageCardiac pacing Implanted electrodes in contact with 0.1- to 2-ms capacitor-discharge 0.1 to 8 V peak deliveredheart; electrode impedance pulse with charge-balancing from 5- to 10-µF250 Ω to 1 kΩ phase capacitorGelled skin-surface electrodes placed Balanced biphasic current pulse 50 to 200 mA with 30-Von chest; electrode impedance 50 Ω 20 to 40 ms in duration complianceCardiac defibrillation Implanted electrodes in contact with Biphasic capacitor discharge 2 to 10 A with capacitorheart; electrode impedance 30 to 60 Ω 5 to 10 ms in duration bank charged to 1kVGelled skin surface electrodes placed Monophasic or biphasic 30 to 40 A with capacitoron chest; electrode impedance capacitor-discharge pulse bank charged to 3kV50 to 100 Ω 5 to 10 ms in durationCardiomyoplasty Platinum–iridium wire electrodes Burst of capacitive discharge pulses 0.1 to 8 V peak deliveredsewn across skeletal muscle a few with charge-balancing phase, from 5- to 10-µFcentimeters apart, looped under the 0.06 to 1.0 ms in duration; 1 to capacitornerve branches that run along the 16 pulses per burst, at a pulsesurface of the muscle; electrodeimpedance 50 to 100 Ωrepetition rate of 10 to 60 Hz;burst delivered in synchrony withcardiac activity at a burst-to-beatratio of 1 : 1 to 1 : 16Electroventilation Temporary electroventilation with 0.8-s bursts of balanced monophasic 200 mA to 1.5 A with up togelled anterior axillary skin-surface pulses 10 µs in duration at 35 Hz 1500-V complianceelectrodes; impedance 250 Ω to 1 kΩImplanted electrodes in contact with 0.8-s bursts of balanced biphasic 1 to 10 mA withphrenic nerve or innervation point current pulses 1 to 10 ms in 12-V complianceof diaphragmatic musclesduration or (phrenic nerve) 25 to100 ms in duration (muscles);repetition rate 30 HzDiagnostic stimulation Bipolar pair of 2- to 5-mm-diameter Monophasic current pulses 50 µs 0 to 100 mA with up toof peripheral nerves spherical dry electrodes with to 2 ms in duration 400-V complianceinterelectrode distance of 2 to 5 mmapplied to skin over target nerveDiagnostic stimulation Bipolar pair gelled electrodes 50-µs-wide transformer-isolated 100 to 1000 V with aof brain (cortex) and (or corkscrew electrodes for square wave maximum current ofspinal cord intraoperative monitoring) 1.5 A (at a rate ofwith interelectrode distancecurrent rise of 0.1 A/µs)of 7 cm applied to skinPain relief Implanted electrodes in contact Monophasic or biphasic pulses 0.1 to 12 V peakwith spinal cord or targeted210 µs in duration deliveredperipheral nerve to block theat 30 to 80 Hzsensation of painGelled skin-surface electrodes Monophasic or biphasic pulses 10 to 150 mA with(impedance 200 Ω to 1 kΩ) placed 50 to 150 µs in duration 150-V complianceon painful region; often knowndelivered at 10 to 150 Hzas transcutaneous electrical nervestimulation (TENS)Vagus nerve Implanted electrodes in contact Monophasic current pulses 0.25 to 35 mA withstimulation (VNS) with vagus nerve; electrode (with charge-balancing phase) 12-V complianceimpedance 1 to 7 kΩ130 to 1000 µs in durationdelivered at 30 Hz for 30 severy 5 minutes
TABLE 7.1(Continued)CLINICAL USES <strong>OF</strong> ELECTRICAL STIMULATION 315Clinical Typical Method of Typical Typical CurrentApplication Current Delivery Waveform or VoltageDeep brain Thin electrode implanted deep 60- to 450-µs charge-balanced 0.1 to 10.5 V peakstimulation (DBS) into parts of the brain that are capacitor-discharge pulsesinvolved in control of movement; delivered at 2 to 185 Hz; burstelectrode impedance 600 Ω to 2 kΩ on/off times depend on patientneedsGastric pacing Implanted electrodes stitched to the Monophasic or biphasic pulses 0.1 to 12 V peakstomach muscle wall of the antrum 210 µs in duration delivered10 cm proximal to the pylorus; at 30 to 80 Hzelectrode impedance 200 Ω to1kΩRestoration of lost Implanted electrode array in contact Balanced biphasic current pulse 10 to 600 µA with 6-Vsight with retina; typical electrode 100 µs to 5 ms in duration; complianceimpedance 1 to 10 kΩrepetition rate 60 to 500 HzImplanted electrode array in contact Balanced biphasic current pulse 1 to 60 µA with 6-Vwith brain’s visual cortex; typical 100 µs to 2 ms in duration; complianceelectrode impedance 10 torepetition rate 10 to 250 Hz100 kΩCochlear stimulation Implanted electrode array in contact Balanced biphasic current 30 µA to 2 mA with 12-Vwith cochlea; typical electrode pulse 20 µs to 1.2 ms in complianceimpedance 1 to 10 kΩduration; repetition rate upto 2 kHzFunctional Implanted electrodes in contact with Balanced biphasic current 1 to 10 mA with 20-Vneuromuscular muscle; electrode impedance pulse 25 to 500 ms in compliancestimulation (FNS) 200 Ω to 2 kΩ duration; repetition rate upto 100 HzGelled skin-surface electrodes placed 1-ms pulse (typically around 10 to 150 mA withover target muscle 300 µs) with a frequency 150-V compliance100 Hz (due to the absoluterefractory period of normalmuscle)Biphasic 10- to 15-ms waveforms10 Hz for denervated muscleElectrical muscle Gelled skin-surface electrodes 1-ms pulse (typically around 10 to 150 mA withstimulation (EMS) placed over target muscles 300 µs) with a frequency of 150-V compliance100 Hz (due to the absoluterefractory period of normalmuscle)Biphasic 10- to 15-ms waveforms10 Hz for denervated muscleInterferential mode: at least two Sinusoidal current; one channel at a 0 to 100 mA RMS withpairs of skin surface electrodes frequency of 4 kHz, second 150-V p-p compliancedelivering high-frequency signals channel at 4 kHz selectablethat interfere at the target muscles; beat frequencygelled skin-surface electrodeswith impedance 100 Ω to 1.5 kΩat 4 kHzElectroconvulsive Gelled skin-surface electrodes applied 10-s burst of 0.25-ms pulses Up to 1 A with 2.5-kVtherapy (ECT) to the forehead; impedance 250 Ω delivered at 10 to 100 Hz voltage complianceto 1.5 kΩ
316 STIMULATION <strong>OF</strong> EXCITABLE TISSUESThe primary factors determining whether sufficient current flows to yield a desired clinicaleffect are impedance of the body tissues in the path of the current, electrode size andposition, stimulation parameters, and the electrical characteristics of the tissue to beexcited. These parameters are usually interrelated, as shown in Table 7.1 for the variousclinical areas in which electrical stimulation is used.The most commonly used stimulation signal waveshapes are those shown in Figure 7.6.The charge-balanced pulses of Figure 7.6a ensure that no net charge is introduced to theFigure 7.6 These are the most common stimulation signal waveshapes and the generic circuits used to produce them. (a) Charge-balancedpulses ensure that no net charge is introduced to the body. In the balanced bidirectional pulse pair, each stimulus pulse has two phases ofidentical duration and identical current magnitude, but of opposite polarity. (b) True monophasic waveforms are seldom, if ever, used to stimulatetissue because they introduce net charge through the tissue that can cause tissue damage. They are produced only when the energysource is switched along the way to the tissue and there is no way for the electrode–tissue interface capacitance to discharge. (c) Monophasicwaveforms really tend to be asymmetric biphasic, as the net charge built up in the electrode–tissue interface or in a dedicated dc-blockingcapacitor discharges. Not all stimulators deliver a constant-current stimulus. Some generate the stimulus current by discharging a capacitorinto the tissue (d) or by using an impulse transformer to step-up the voltage (e).
DIRECT STIMULATION <strong>OF</strong> NERVE <strong>AND</strong> MUSCLE 317body. Current is driven into the tissue first in one direction and then, after a brief interval,in the other. Thus, ions moving in the tissue would first be pushed one way and thenquickly the other way, stimulating the tissue and leaving the ions in their former positionswithin the electrodes, interstitial fluids, and cells. This waveform is known as a balancedbidirectional pulse pair. Neurons are especially sensitive to poisoning by metallic ionsreleased from the electrodes as well as by the products of electrolytic decomposition ofsalts and water. Microscopic studies of brains stimulated with this balanced pulse pair atlow current densities showed that it causes no electrolytic damage to the neurons.As shown in Figure 7.6b, true monophasic pulses are produced only when the energysource is switched along the way to the tissue and there is no way for the electrode–tissueinterface capacitance to discharge. True monophasic waveforms are seldom, if ever, usedto stimulate tissue because they introduce net charge through the tissue that can cause electrolysisand tissue damage. Monophasic waveforms really tend to be asymmetric biphasic,as the net charge built up in the electrode–tissue interface or in a dedicated dc-blockingcapacitor discharges as shown in Figure 7.6c–e.DIRECT STIMULATION <strong>OF</strong> NERVE <strong>AND</strong> MUSCLEImplantable cardiac pacemakers have been around since the late 1950s. More recently, thesame basic techniques have been applied to stimulate the vagus nerve for the control ofepilepsy, to stimulate the sacral roots to control the bladder and correct erectile dysfunction,and to stimulate nerves in the spine for the control of pain and angina. In addition, interest infunctional electrical stimulation (FES) has grown rapidly during recent years, due primarilyto progress made in miniaturized hardware that makes multichannel stimulators possible.New surgical techniques enable the use of chronically implanted stimulators to stimulatespecific nerves and brain sections directly within the body, making it possible to restore functionlost due to disease or trauma. Advances are being made rapidly in the development ofimplants for restoring limbs, sight (e.g., through artificial retinas or by direct stimulation ofthe visual cortex), and hearing (e.g., through cochlear implants) [Loeb, 1989].As shown in Table 7.1, and with the exception of cardiac defibrillation, all other applicationsin which the electrodes are placed in close contact with target tissue require the deliveryof relatively narrow pulses (2 ms) of low voltage (12 V) at low current (35 mA).These can easily be produced with miniature circuits that use standard bipolar or MOSFETtransistors (discrete transistors or as part of an IC), tantalum capacitors, and implantablegradelithium batteries. Implantable stimulators typically use either a constant-current sourceor a capacitor discharge circuit as output stages to generate stimulation pulses.Capacitor-Discharge StimulatorsIn a capacitor-discharge output stage, an energy-storage capacitor, usually called a tankcapacitor, is charged to the desired peak voltage and then delivered to the target tissue.Figure 7.7 shows the circuit of a simple capacitor-discharge pulse generator circuit thatcan generate stimulation pulses with an amplitude of either 3 or 6 V from a 3-V source(e.g., a single lithium battery). When inactive, the control logic for the stimulator sets theHIGH AMPLITUDE STIMULUS line low, which charges tank capacitor C2 to VDD.The STIMULUS signal is maintained low to keep transistor Q2 open, and line ACTIVEDISCHARGE is maintained low to keep switch Q1 open. Coupling capacitor C1 slowlydischarges by way of resistor R1 (100 kΩ) through the tissue and electrodes connected toterminals V and V.When a stimulus is to be generated, and if the amplitude selected is 6 V, the HIGHAMPLITUDE STIMULUS line is set high, which closes Q4 and opens Q3. This causes
318 STIMULATION <strong>OF</strong> EXCITABLE TISSUESVDDACTIVE DISCHARGEQ1BSS84ANODER2100 OhmsR1100kC110uF+OUTPUTCATHODESTIMULUSVDDQ2BSS138HIGH AMPLITUDE STIMULUSQ3BSS84C215uF+VDDQ4BSS138R315kD1HSMS28243VHIGHAMPLITUDESTIMULUSACTIVE DISCHARGESTIMULUSOUTPUTVOLTAGE INTOTISSUE6V10-50ms3V10-50ms
DIRECT STIMULATION <strong>OF</strong> NERVE <strong>AND</strong> MUSCLE 31912VB1-B4Duracell DL2032 x 4C110nF754628CVRSTTHRTRGVCCIC1NE555DSCHGGND1OUT3D11N4148R115MD21N4148R239K+ C222uFR32KR41K+ C41uFC310nFIC2ICM75555CONTV OUT374DISCHRESET2TRIG6THOLD8V+GND1R512KQ1BC337R622KC50.22uF1Electrodes1J1J2Figure 7.8 A variation on the capacitor-discharge circuit is the capacitor-coupled stimulator. In this circuit for the stimulation of denervatedmuscles, C5 differentiates the rectangular square waveform at the output of Q1 to yield a net-zero charge transfer across the tissue.by delivering the energy stored in this capacitor through the tissue. A zero net current flowthrough the tissue results from passing the same amount of charge (albeit not within thesame amount of time) through the tissue during the discharge phase as was delivered duringthe stimulus pulse, but in the opposite direction. Not doing so would cause electrochemicalimbalance, which can result in electrode corrosion and tissue damage. Taking theACTIVE DISCHARGE line low closes Q1, allowing the charge in coupling capacitor C1to flow through the tissue via resistors R2 and R1 (100 Ω in parallel with 100 kΩ). Anyremaining charge after the fast discharge time is delivered at a slower rate through R1(100 kΩ). With the component values shown, this circuit is suitable for delivering stimuluspulses with durations of up to 2 ms into implanted electrodes that present a load impedanceof approximately 500 Ω.A variation on the capacitor-discharge circuit is the capacitor-coupled stimulator.Figure 7.8 shows a stimulator based on the circuit configuration proposed by Sebille et al.[1988] for the stimulation of denervated muscles. In this circuit, timer IC2 generates asquare wave that drives transistor Q1. The common-collector connection allows the outputvoltage to remain independent of the impedance presented by the tissue being stimulated.C5 differentiates the rectangular square wave to yield a zero net charge transfer across thetissue. Timer IC1 cycles IC2’s power on and off, making it possible to vary the stimulationduty cycle by changing the values of R1 and R2.Current-Source StimulatorsHochmair [1980] described a CMOS low-power current source suitable for implantabledevices. It uses a standard CMOS 4007 integrated circuit, which contains six enhancementMOSFETs, three n-channel and three p-channel. The n-channel bodies (p-silicon) are connectedto pin 7 and must be kept at the most negative voltage used in the circuit. Thep-channel bodies (n-silicon) are connected to pin 14 and must be kept at the most positivevoltage used in the IC. The transistor elements are accessible through the package terminals.
320 STIMULATION <strong>OF</strong> EXCITABLE TISSUESThe CD4007 is usually characterized as a CMOS digital IC, but it is perfectly useful as aFET for analog circuits.In the current-source circuit of Figure 7.9, the control voltage V in is delivered to thegates of the CMOS pair formed by transistors Q1 and Q2. The output capacitor C2 ischarged by the n-channel transistor Q4. The thresholds of Q3 and Q4 are adjusted toapproximately the same level of V in , about 4 V. Q4 conducts above this level and Q3 conductsbelow it. When the current source is not active, either Q3 or Q4 is off completely,and the power consumption is under 400 µW.Q1 and Q2 together with zener diode D1 act as source followers to increase thethresholds of the current-source output transistors. D1 is selected to compensate forR2D1100K(a)IC1CD400767.5V7Q314R4Reference Electrode18136K3Q2Q1+15V452110Q49 11C1100pFR1100KR38.5KVIN1112C2Stimulating Electrode50nFI(b)Vin0IQBalance=QStim0QStimIStim = F(Vin)Figure 7.9 A MOS circuit based on a standard 4007 can be used as a low-power current-source stimulator capable of delivering chargebalancedpulses of up to 700 µA with a compliance of up to 10 V for a maximum delivered charge per pulse of 0.5 µC.
DIRECT STIMULATION <strong>OF</strong> NERVE <strong>AND</strong> MUSCLE 321parameter variations of the 4007 IC such that the thresholds of Q3 and Q4 are adjustedto be almost identical. For a 15-V power supply, a 7.5-V zener is required to bring thethreshold of Q4 up to 4 V. Figure 7.10 shows the transfer characteristics of the currentsource. The circuit can be implemented as a thin-film hybrid using bare-die 4007, thinfilmresistors, and surface-mounted diodes and capacitors. Hochmair reported using thiscircuit as part of an eight-channel auditory nerve stimulator capable of deliveringcharge-balanced pulses of up to 700 µA with a compliance of up to 10 V for a maximumdelivered charge per pulse of 0.5 µC.True symmetrical biphasic current waveforms are often generated through a voltage-tocurrentconverter driven by the voltage representation of the current waveform desired.Figure 7.11a and b show the basic configurations for floating-load op-amp voltage-tocurrentconverters. Floating-load circuits provide the best possible performance of any ofthe current output circuits, but require the load to float, which makes them unsuitable formany applications. In these circuits, the load current I out develops a proportional voltage inR sense , which is fed back for comparison to applied input. As long as voltage across R senseis lower than the input voltage, the magnitude of the output voltage increases. The invertingcircuit has the advantage of being able scale the transfer function up or down by selectingthe proper ratio R F /R in .The improved Howland current pump provides a topology for voltage-to-current convertersthat require the load to have one end ground referenced. The circuits of Figure 7.11cand d act as differential amplifiers with a differential input and a differential output. V in isgained up by the ratio of R F /R in and impressed differentially across R sense . I out is thus thevoltage across R sense divided by the value of R sense . Since the input is also differential, movingV in to the opposite input simply reverses the relationship of I out to V in . The dominanterror source in the Howland pump topology is ratio matching of the R F /R in resistors. Theratio of R F /R in for the negative feedback path should closely match the ratio of R F /R in in thenegative feedback path.I out700[µA]600500400300200ISD n-channelISD p-channel1001 2 3 4 5 6 7 8 9 10 11 12 13 14 15V in [V]Figure 7.10of 15 V.Transfer characteristics of the current source of Figure 7.9 for a supply voltage
322 STIMULATION <strong>OF</strong> EXCITABLE TISSUES(a)+V(b)-V327+-6IoutRin234-+6IoutVin4Vin7-V+VLOADLOADRfIout =______ VinRSenseRSenseIout =-Vin Rf_________RSense RinRSense(c)RinRf(d)RinRfRin23-V4-+6RSenseIoutVinRin23-V4-+6RSenseIoutVin7+VRfLOAD7+VRfLOADVin RfIout = -_________Vin RfRSense Rin___________Iout =RSense RinFigure 7.11 Symmetrical biphasic current waveforms are often generated through voltage-to-current converters: (a) floating-load noninvertingconfiguration; (b) floating-load inverting configuration; (c) grounded-load noninverting improved Howland current pump; (d) invertingconfiguration of the Howland pump.As an example, Figure 7.12 presents the output stage of a backpack stimulator based onthe one developed by Livnat et al. [1981] for animal experiments involving chronic stimulationof the central nervous system with implanted electrodes. Pulses are generated byIC1 at a frequency set by R3 and R4 (e.g., 160 Hz). IC2A, IC3A, IC4A, IC4B, and IC5reshape the output of timer IC1 into a symmetric bipolar square-pulse train. The voltagewaveform at the output of IC5 is converted into a constant-current waveform by the invertingHowland pump built around IC6. The stimulation current can be selected by the settingof R1. In Livnat’s stimulator, power for the output stage was turned on and off througha set of CMOS switches driven by a low-frequency sequencer that selected the burst durationand frequency at which bursts were delivered to the animal. The stimulator output wasdesigned to deliver up to 1 mA into electrodes with impedances of up to 10 kΩ.Another way of producing biphasic current pulses is to use a unipolar current source thatis switched through an H-bridge so that the polarity presented to the tissue can be reversed.Take, for example, the optically isolated bipolar current source of Figure 7.13. This veryneat circuit configuration was proposed by Woodward [1998] as a laboratory stimulator forneurophysiology research. In this circuit, the four optocoupler transistors of the H-bridge(IC2) are used not only to switch the polarity of the current source, they are themselves the
ELECTRODE 1ELECTRODE 2I_OUTR3+15V_SWITCHED1M +15V_SWITCHEDR21MR125kR41MC30.01uFC40.01uF74268C60.01uF+5V_SWITCHEDIC1ICM7555/TO5 3CONTVO UTDISCHRESETTRIGTHOLDV+1+5V416132JKCLKCLRPREIC2A74C76IC3AQQ1 274C04151412R5100kR7100kR11100kIC5UPC4250C70.01uF3245IC4A74C08IC4B74C08367+-4 86R91MC20.01uF-15V_ SWITCHEDR62MR102MC11uF+C51uF+327+-4 8R81MGND-15V_SWITCHEDR12IC6UPC42506+5V_SWITCHEDR131M+15V+15V_SWITCHED100k-15V-15V_SWITCHED+5V+5V_SWITCHED30s to 4min30s to 4min30min to 20hoursFigure 7.12 In this symmetric biphasic current stimulator, pulses generated by timer IC1 are reshaped by IC2A, IC3A, IC4A, IC4B, andIC5 into a symmetric bipolar square-pulse train. The resulting voltage waveform is converted into a constant-current waveform by the invertingHowland current pump built around IC6. Livnat et al. [1981] used implanted electrodes and this output stage for chronic stimulation ofthe central nervous system.323
FAULT:COMPLIANCELIMITD1RED LEDIC2BPS2501- 4I_OUTELECTRODE 1IC2DPS2501-4ELECTRODE 2+15V<strong>OF</strong>FSET NULLR1100kR350kR649.9kR422M32+-+15V84-15V1IC1ALT1013R21kC1330pFR5120Q12N4403D24 X 1N4148 BRIDGE14+-2+15V31287IC3APS2501-2IC3BPS2501-256+15VBT19 to 60V43125616151211IC2APS2501-4IC2CPS2501-434781413901GAINTRIM2kR8R94.02k56R105.1k+-847C20.1uFIC1BLT1013R75.1kQ22N3904-15VC30.1uFFigure 7.13 In this circuit for neurophysiology research, the four optocoupler transistors of the H-bridge are used to switch the polarity ofthe current source and to regulate the current delivered to the electrodes. The current delivered to the bridge is sensed by optocoupler IC3B.The current-control loop is closed via IC1A, which receives setpoint and feedback currents through IC3A and IC3B, respectively.J1V_IN 12324
DIRECT STIMULATION <strong>OF</strong> NERVE <strong>AND</strong> MUSCLE 325current-regulating elements of the current source. In a nutshell, the circuit works as follows:IC1B and Q2 will drive current through either the LEDs of IC2A and IC2D or those ofIC2B and IC2C, depending on the polarity of the input signal. This will cause current fromthe battery to be driven into the load connected to the electrodes by the H-bridge transistorsof multichannel optocoupler IC2. The current delivered to the bridge is sensed by optocouplerIC3B. The current-control loop is closed via IC1A, which receives setpoint and feedbackcurrents through IC3A and IC3B, respectively. Q1 and LED D1 turn on when IC1Adrives excessive current through the bridge, providing an indication that the voltage complianceof the source has been reached.Op-Amp Bridge StimulatorsAnother stimulator output stage configuration that is worth exploring is the op-amp bridge.The bridge connection of two op-amps provides output voltage swings twice that of one opamp.This makes it possible to reach higher stimulation or compliance voltages in applicationswith low supply voltages or applications that operate amplifiers near their maximumvoltage ratings in which a single amplifier could not provide sufficient drive. 2 In addition,the bridge configuration is the only way to obtain bipolar dc-coupled drive in single-supplyapplications.Figure 7.14a shows a generic voltage-output bridge connection of two op-amps. AmplifierA1 is commonly referred to as the master and A2 as the slave. The master amplifieraccepts the input signal and provides the gain necessary to develop full output swing fromthe input signal. The total gain across the load is thus twice the gain of the master amplifier.The master amplifier can be set up as any op-amp circuit: inverting or noninverting, differentialamplifier, or as a current source such as a Howland current pump. In the latter, onlythe master amplifier is configured as a current source. As shown in Figure 7.14b, the slaveremains as an inverting voltage amplifier.This is, however, not the only current-source circuit that can be built in bridgeconfiguration. In fact, U.S. patent 4,856,525 to van den Honert [1989] shows how to usetwo current sources per channel of a multichannel stimulator to minimize the crosscouplingof stimulating currents between channels. As shown in Figure 7.15a, eachchannel of a multichannel stimulator may have a current source that drives currentbetween one electrode and a common ground electrode. However, a single currentsource for each channel requires only that the current in the loop containing the electrodeand electrical ground be equal to the value of the current source and not necessarilythat the current passing to ground go through any particular one of electrodescoupled to electrical ground. If the electrical power supplies of the channels of the electricalstimulator are not isolated electrically, a cross current from one electrode pair toanother electrode pair could occur while maintaining the loop current requirements ofeach channel’s single current source. Van den Honert invented a multichannel currentsource configuration with improved channel isolation that does not require electricallyisolated power supplies.As shown in Figure 7.15b, each channel of the electrical stimulator has a pair of currentsources that work in concert. One current source is coupled to each electrode of eachchannel’s electrode pair. The current sources operate harmoniously. When one currentsource is sourcing (or sinking) a certain current, its complementary current source is sinking(or sourcing) an almost identical current. As such, the current passing between the2Op-amp bridge current sources are not only limited to low-voltage applications in direct stimulation of tissues.There are a number of op-amps that will operate with very high supply voltages, making it possible to use the sametechniques in the design of high-voltage external stimulators. For example, the PA89 by Apex Microtechnology israted for a total supply voltage of 1200 V.
326 STIMULATION <strong>OF</strong> EXCITABLE TISSUES(a)RfRSlave-VSupply-VSupplyVinRin42 -3 +7+VSupply6A1Master____ RfGain =RinLOADA2SlaveVLoad Max = +/- 2VSupply647- 2+ 3+VSupplyGain = 1RSlave(b)RfRSlave-VSupply-VSupplyRinRin42 -3 +76RSenseVin+VSupply+VSupplyRfSlaveMasterVCompliance = +/- 2VSupplyFigure 7.14 The bridge connection of two op-amps provides output voltage swings twice that of one op-amp, making it possible to reachhigher stimulation or compliance voltages in applications that operate amplifiers near their maximum voltage ratings. (a) Generic voltageoutputbridge connection of two op-amps. (b) The master amplifier can be set up as any op-amp circuit: for example, as a Howland currentpump.LOAD647- 2+ 3RSlaveelectrode pair is equal to the amount of current desired. Current leak between electrodepairs is minimized and channel isolation is improved significantly. Figure 7.15c showshow the circuit could be built with Howland current pumps.Charge Injection through Implanted ElectrodesElectrodes used for stimulation behave radically different than electrodes that are usedonly for sensing biopotentials. This is because much stronger currents need to be producedthrough the tissue by converting electron flow in the leads to ion movement in theaqueous solution. Safe electrical stimulation of the nerves and muscle through directcontactelectrodes requires this conversion to happen only through reversible chargeinjectionprocesses. Irreversible reactions such as electrolysis result in the evolution ofgases and acid or alkali solutions that can destroy the tissues. Other harmful irreversiblefaradic reactions include saline oxidation, metal dissolution, and oxidation of organicmolecules.
DIRECT STIMULATION <strong>OF</strong> NERVE <strong>AND</strong> MUSCLE 327(a)Channel 1TissueUndesiredCurrents(b)Control 1Channel 1TissueControl 1Desired CurrentsChannel 2Channel 2Control 2Control 2Constant CurrentStimulatorsElectrodes(C)Vin 1I out 1Vin 2Iout 2Figure 7.15 Van den Honert [1989] showed how to use two current sources per channel of a multichannel stimulator to minimize the crosscouplingof stimulating currents between channels. (a) A cross current from one electrode pair to another electrode pair can occur whilemaintaining the loop current requirements of each channel’s single current source when isolated power supplies are not used. (b) Using twocurrent sources per channel improves channel isolation without requiring electrically isolated power supplies. (c) The improved circuit couldbe built with Howland current pumps.A simple fully reversible reaction is the charging and discharging of the capacitancebetween the conductive electrode and body fluids. However, the limit of reversibility isreached when the charge accumulated on the electrode–tissue interface capacitance yieldsa potential difference above the working voltage for the electrolysis of water (approximately0.8 V). As such, the amount of charge that can be passed by this double-layerinterface depends on the equivalent capacitance of the electrode–tissue interface. Just as ina conventional capacitor, the capacitance of the electrode–tissue interface depends on thesurface area of the electrode and the thickness of the effective dielectric boundary of theinterface.Two safety demands are then obvious for implantable stimulating electrodes. The firstis that the electrode material must be compatible with the body so that the formation ofconnective tissue layers whose thickness is greater than 100 µm is suppressed such that the
328 STIMULATION <strong>OF</strong> EXCITABLE TISSUESstimulation threshold remains largely constant. Second, a high double-layer capacitanceshould develop at the phase boundary between the electrode and the body fluids so that thepolarization rise during the stimulation pulses remains under the limit of irreversible electrochemicalreactions.The classical materials for invasive stimulating electrodes have been stainless steel andplatinum. These materials have a limited range for reversible charge injection by surfacefaradic processes in the in vivo saline environment before the onset of water electrolysis(approximately 0.5 mC/cm 2 for platinum and platinum alloys) or catastrophic corrosion(approximately 0.04 mC/cm 2 for stainless steel). These charge injection limits restrict theirusefulness as stimulation electrodes to applications requiring only low charge-injectiondensities. However, even low charge-injection densities are known to produce corrosion ofthe metal, thereby releasing trace quantities of dissolved metal into the surrounding environment.In the case of platinum, dissolution products may be toxic to the tissue in whichthe electrodes are implanted. In the case of stainless steel electrodes, dissolution or corrosionof the electrode may result in electrode failure due to corrosion-induced fracture. Infact, dissolution often results in disappearance of the entire electrode.Another metal in use today for stimulating electrodes is iridium. Pure iridium is extremelystiff and has a much lower impedance than that of any other noble metal. It is extremely inertand very resistant to corrosion. The de facto standard, however, is an alloy of platinum–iridium that has a lower concomitant impedance value than that of either tungsten or stainlesssteel for the same exposure, making electrodes less likely to erode during intense stimulationprotocols. This alloy is excellent for chronic implants because it is very biocompatible.Table 7.2 shows the material properties of some of the most common metals used for the fabricationof electrodes. You can buy high-purity materials to make chronically implantableelectrodes from a number of suppliers, including Alfa Aesar (high-purity raw materials),Noble-Met (drawn wire as thin as 0.001 in. in diameter), and Xylem Company (wires andmetallic parts).In the 1970s, the promise of electrical stimulation as a cure for pain, paralysis, deafness,and blindness seemed close at hand. Development in these areas prompted the search fornew electrode materials to increase safe charge-injection densities. Significant developmentswere made in the 1980s with the introduction of metallic oxide layers. Electrodeswith a large microscopic surface area were fabricated by anodizing titanium and tantalumelectrodes. The anodized electrodes operate by charging and discharging the double-layercapacitance at the electrode–electrolyte interface. They provide an intrinsically safe meansof charge injection because they form a dc-blocking capacitor right at the electrode–tissueinterface that ensures charge balancing. Unfortunately, these anodized electrodes have limitedcharge densities (lower than those of platinum) and can be used for injecting anodiccharge only, unless appropriately biased, whereas the physiological preference is forcathodic charge.Later, coatings such as titanium nitride (TiN) [Konrad et al., 1984] and iridium oxide(IROX) [Robblee et al., 1986] were developed to overcome the shortcomings of anodizedelectrodes. IROX works by delivering charge to tissues through reversible reduction–TABLE 7.2Desirable Material Properties for Some Metals Commonly Used in Stimulating ElectrodesMP35NStainless BiocompatiblePlatinum Iridium Gold Silver Tantalum Titanium Steel SuperalloyCorrosion resistance ✓ ✓ ✓ ✓ ✓ ✓ ✓Biocompatibility ✓ ✓ ✓ ✓ ✓ ✓ ✓Electrical conductivity ✓ ✓
DIRECT STIMULATION <strong>OF</strong> NERVE <strong>AND</strong> MUSCLE 329oxidation reactions occurring within the oxide film. The iridium oxide layer becomes thecharge transfer interface and enables charge injection densities up to 10 mC/cm 2 for eithercathodic or anodic polarities without water electrolysis or other faradic reactions involvedin corrosion of the underlying metallic electrode.Thin films of hydrated iridium oxide have been used as low-impedance coatings forneural stimulation and recording electrodes. The iridium oxide provides a way of injectingcharge into tissue while minimizing electrochemically irreversible processes at theelectrode–tissue interface, where reduction and oxidation reactions occur to mediatebetween electron flow in the external circuit and ion flow in the tissue. Electrodes coatedwith iridium oxide are very good for long-term stimulation of nerves in the spinal cord[Woodford et al., 1996], in the ear’s cochlea [Anderson et al., 1989], and in the brain cortex[Bak et al., 1990; Hambrecht, 1995].The idea behind using IROX as an electrode material is that iridium can store charge bygoing through valence changes that cause reversible redox reactions. The fact that thesereactions are reversible is important for biocompatibility. Reversibility means that no newsubstance is formed and hence no reactants are released into tissue. The state of the iridiumwill depend on the potential applied across the metal–electrolyte junction.Since tissue-contact stimulation is usually accomplished with a constant-current source,the voltage applied is dependent on the charge storage of the oxide. As the oxide absorbsmore charge (positive current), the potential across the interface will increase, which willresult in the oxide reacting with the electrolyte. Initially, with no applied voltage, the iridiumoxide is in the Ir(OH) 3 state. As potential is increased, the iridium oxide increasesvalence by ejecting protons into the solution. The following reaction summarizes thesequential change in the oxide as potential increases:IrO x1 (OH) 4x ⇌ IrO x (OH) 3x (x 1)(H e )where x 1, 2, 3 and increases with potential. The IrO 3 state (x 3) is unstable and itsdegradation will result in oxygen evolution. This reaction defines the water window on thepositive voltage side. Subsequently, as charge is removed from the oxide (negative current),the reactions reverse. Do you see where the name IrOx comes from?Iridium oxide coatings are usually formed on electrodes by three different processes:1. Activated iridium oxide film (AIR<strong>OF</strong>): formed from iridium metal in an aqueouselectrolyte by an activation process in which the electrochemical potential of themetal is cycled or pulsed between negative and positive potential limits close tothose for electrolysis of water2. Sputtered iridium oxide film (SIR<strong>OF</strong>): formed by reactive sputtering of iridiummedium in an oxidizing atmosphere3. Thermal iridium oxide film (TIR<strong>OF</strong>): formed by the decomposition of iridium saltsto form an iridium oxide film on top of a metallic substrate electrodeThe AIR<strong>OF</strong> method is the simplest to use to home-brew IROX-coated electrodes bystarting with electrode substrates made of pure iridium metal. Iridium grows a hydrous oxidelayer on its surface when it is activated electrochemically in an electrolyte (0.3 M sodiumphosphate dibasic, Na 2 HPO 4 ). A standard three-electrode scheme is used to perform cyclicvoltammetry using the setup shown in Figure 7.16. Cyclic voltammetry is an analyticaltechnique that involves application of a time-varying potential to an electrochemical celland simultaneous measurement of the resulting current. 3 This measurement can be used toprovide oxidation–reduction information about the system being studied. However, in thisapplication, the technique is used as a manufacturing process.
CURRENTTOOSCILLOSCOPECHANNEL 2"Y" INPUT FORVOLTAMMETRYJ2SIGNAL GENERATORAPPLIED VOLTAGETOOSCILLOSCOPECHANNEL 1"X" INPUT FORVOLTAMMETRY+15VR310k32+-+15V411-15VIC2ATL084112BWVIN+15V53VOUTIC1BUF6344+ C1R11010uF+15V12BWVIN5VOUTIC3BUF6344+ C410uFV- V+V- V+C60.01uFJ156+-411IC2BTL0847R210kC30.01uFC90.01uF-15VC20.1uF+ C8C70.01uF10C10 10uF0.1uF -9+411IC2CTL0848+15VC50.1uFR410R5C113-15VC130.01uF10050pF-15VC140.01uF-15VC150.1uF+ C1210uFSATURATEDCALOMELREFERENCEELECTRODELARGEPLATINUMCOUNTERELECTRODER6100k"WORKING" ELECTRODE:IRIDIUM ELECTRODE TOBE COATED WITH IROX0.3M Na2HPO4ELECTROLYTEPYREX CONTAINERFigure 7.16 Iridium oxide coatings can be grown on iridium-metal electrodes by electrochemical activation in a Na 2 HPO 4 solution.Electrochemical activation should be done using a standard three-electrode cyclic voltammetry setup. The potentiostat circuit (IC1, IC2A,and IC2B) tries to maintain the voltage applied between the working and reference electrodes with negligible current passing through thereference electrode. IC2C, IC3, R4, and R6 act as a current-to-voltage converter such that the counter electrode acts as a source or sink ofelectrons to balance the redox reaction occurring at the working electrode.330
DIRECT STIMULATION <strong>OF</strong> NERVE <strong>AND</strong> MUSCLE 331In this circuit, IC1, IC2A, and IC2B form a potentiostat, which tries to maintain the voltageapplied between the working and reference electrodes and allows negligible currentthrough the reference electrode (IC2B is configured as a unity-gain buffer, presenting virtuallyinfinite input impedance to the reference electrode). In voltammetric measurements, thecurrent is measured as a function of this applied potential. The counter electrode acts as asource or sink of electrons to balance the redox reaction occurring at the working electrode.IC2C, IC3, R4, and R6 act as a current-to-voltage converter. Therefore, the potential appliedbetween the counter and working electrodes must be sufficient both to drive the appropriateelectron transfer reaction at the counter electrode and to compensate for the potential drop dueto the solution resistance between the counter and reference electrodes (this potential drop isgiven by Ohm’s law, V iR solution , where i is the current generated by the electrochemical reactionand R solution is the solution resistance between the electrodes). The compliance voltage isthen the maximum potential that can be supplied between the working and counter electrodes.The voltage waveform is applied to a counter electrode (a large platinum electrode) inthe electrolyte. The iridium electrode to be activated is the working electrode and providesa return current path. A saturated calomel electrode (SCE) provides a reference (FisherScientific 13-620-52). The voltage on the counter electrode is cycled between anodic andcathodic potentials while the iridium electrode is exposed to an electrolyte.During the anodic sweep, an inner oxide (IrO 2 ) is formed from pure iridium. As thepotential increases, the inner oxide changes to a hydrous outer layer [Ir(OH) 3 ]. The factthat this layer is hydrated (water molecules are attached) limits formation to a monolayer.The cathodic sweep causes reduction of the inner oxide back to iridium but does not golow enough to reduce the outer layer. The outer layer remains. Since the oxide is porous,the metal maintains contact with the electrolyte. Therefore, on the next potential sweep theprocess will repeat. In this way, a hydrous porous layer of iridium oxide is created. Thepotential limits depend on the electrolyte but should not exceed the potential that results inoxygen or hydrogen evolution.The University of Michigan Center for Neural Communication Technology recommendsthe following method for the formation of high-quality IROX films:1. Initially, hold sites at potentials of 3.0 and 2.5 V for approximately 3 minutes eachto remove any oxide that has formed, essentially cleaning the metal.2. Cycle the activation potential between 0.85 and 0.75 V. These limits are usuallywide enough to grow an oxide but narrow enough to remain within the water window(the potential range that does not result in oxygen or hydrogen evolution). As a rule,the voltage limits should be set approximately 100 mV inside the water window.3. Use a square wave (0.5 to 1 Hz) to activate. This allows the metal to remain at thecritical levels for hydrous oxide formation (0.75 V) and inner oxide reduction(0.85 V) for a longer time than a ramp wave would. Holding the potential at theselevels allows more complete oxide formation and reduction and also reduces thenumber of potential cycles (500 to 1000 cycles) needed to grow the oxide.4. Activate to a limit of 30 mC/cm 2 . Although studies have shown 100 mC/cm 2 to be themaximum usable storage capacity for activated iridium, 30 mC/cm 2 allows the oxideto better maintain electrical characteristics and should suffice for most neural stim-3You can still use this circuit as a classical cyclic voltammeter. Just change the output of the function generatorto a triangular wave and connect the voltage- and current-monitoring outputs to a two-channel oscilloscope capableof working in the x–y mode. For a detailed discussion of the cyclic voltammetry technique, we recommendD. K. Grosser, Cyclic Voltammetry Simulation and Analysis of Reaction Mechanisms, Wiley-VCH, Weinheim,Germany, 1993. In addition, the accompanying CD-ROM includes a cyclic voltammetry simulator (VirtualCVv1.0 freeware for Windows 9x by Andre Laouenan) to help you understand how the technique works and how toanalyze results.
332 STIMULATION <strong>OF</strong> EXCITABLE TISSUESulation applications. In vitro pulse tests of the oxide grown using this method showthat coating maintains its electrical characteristics over at least 100 million pulses.The TIR<strong>OF</strong> method is more difficult for home-based coating, but it can be used todeposit IROX on any common metallic substrate. Robblee’s patent, “Iridium Oxide CoatedElectrodes for Neural Stimulation” [1987], describes exactly how to coat platinum,platinum–iridium, stainless steel, titanium, or tantalum with a TIR<strong>OF</strong> 4 :1. An acid–alcohol solution containing dissolved iridium complexes is prepared by heatingIrCl 3 3H 2 O [Ir(III)trichloride] in 5.5 M HCl (4% wt/vol) until 75 to 80% of the solutionis evaporated. Heating the Ir(III) trichloride in the acid results in conversion of theIr(III)trichloride to a hexachloroiridate ion, (IrCl 6 ) 2− . The solution is restored to its initialvolume with the addition of alcohol. Either isopropyl alcohol or ethyl alcohol canbe used. This acid–alcohol solution is then aged for a period of time (e.g., 1 to 2 weeks),during which time the hexachloroiridate ion is slowly converted to a chloroiridate–-alcohol complex of Ir(IV). A way of avoiding boiling iridium chloride in HCl is simplyto buy chloroiridic acid [Hydrogen hexachloroiridate(IV) hydrate] from Alfa-Aesar(item 11031) and stir it with isopropyl alcohol to achieve the correct acid–alcohol ratio.The solution must then be left to age for 1 to 2 weeks in a tightly sealed jar.2. The surface of the metallic electrode is pretreated prior to deposition of the iridiumsolution to enhance adhesion of the iridium oxide film formed. Such pretreatmentsinclude chemical or electrochemical etching and vary depending on the metallicelectrode being coated. Common ways of preparing surfaces for coating includeetching with HCl and sandblasting using a fine abrasive powder.3. The metallic electrode is soaked in the aged acid–alcohol solution for a prolongedperiod of time, typically 16 hours, after which it is dried for 1 hour at room temperature(22°C) and annealed in air at 320°C for 80 to 90 minutes. Prolonged soaking of themetallic electrode allows intimate association of chloroiridate–alcohol complexes insolution with the surface of the metallic electrode so that the metallic surface becomescompletely covered with iridium complexes. Shorter soaking times lead to incompletecoverage of the metallic surface so that areas of uncoated metal remain exposed.4. Successive layers are added by soaking the electrode in the acid–alcohol solutionof iridium again and again for 16 to 24 hours, followed by 3 to 6 hours annealingat 320°C after each period of soaking. Typically, two to four layers are applied. Thehigh-temperature annealing converts the chloroiridate–alcohol complexes depositedon the surface of the electrode to an oxide of iridium [probably a combination ofIrO 2 , IrO 2 H 2 O, and Ir(OH) 4 ]. The annealing temperature of 320°C was reported byRobblee to be optimal for obtaining electrodes of the highest charge-injectioncapacity. The long annealing times are required for complete conversion of thechloroiridate–alcohol complexes to iridium oxide and the elimination of chloridefrom the film.5. Chloro complexes of iridium that may remain on the surface due to insufficientannealing are susceptible to passive leaching and dissolution from the film. Moreover,insufficiently annealed films that contain a high chloride content have a very lowcharge injection capacity, due to the smaller proportion of Ir(IV) oxide species, whichare responsible for the surface faradic charge injection reactions desired. As such,4Patents issued before June 5, 1995 had a 17-year term from the date of issue. Patents filed after that date have a20-year term measured from the filing date. Patents filed before that date, and pending or issued on that date, havethe longer of the two terms. Once a patent has expired the invention is in the public domain, and you are free touse it.
DIRECT STIMULATION <strong>OF</strong> NERVE <strong>AND</strong> MUSCLE 333repeated neutralization with deionized water in an ultrasonic cleaner and thoroughcleaning (e.g., with alcohol) are needed to ensure that the tissues are not poisoned bythe chemical precursors of the IROX film.IROX-coated electrodes acquire the electrochemical properties of the IROX and losethose of the underlying metallic electrode. For example, the voltage change across theIROX interface in response to a constant-current pulse is significantly less than the voltagechange across an uncoated metallic electrode interface in response to a current pulseof the same magnitude. The corrosion resistance conferred upon the metallic electrode byan IROX coating is also enormous. In agreement with our own experience, Robblee foundthat no dissolution of the underlying metallic electrode occurred when using IROX-coatedplatinum–iridium electrodes stimulated with biphasic regulated current pulses, whereasthe same electrodes with no coating lost between 2 and 8 µg of platinum during only 24hours of in vitro stimulation under the same conditions.The coating process is dependent on the purity and concentration of the chloriridic acid,the exact ratio of chloroiridate–alcohol complexes, and the preparation and cleanliness ofthe base metal. You’ll end up going through a lot of chloroiridic acid (and sweat) beforeyou achieve a repeatable coating process.As for titanium nitride, the preferred process is to apply the porous nitride layer to thecarrier material serving as substrate by means of reactive ion plating. If you are part of auniversity, you can probably ask around the material sciences department to see if theyhave the setup necessary for physical vapor deposition. If you really want to home-brewtitanium nitride–coated electrodes, we recommend that you read the very practical articleson amateur sputtering by Steve Hansen that appeared in The Bell Jar (volume 8, numbers3–4, pages 14–16, 1999; volume 9, number 1, pages 2–4, 2000; and volume 9, number 2,pages 10–12, 2000). 5An alternative to doing your own coating is to contact one of the specialized vendors thatcan coat electrodes for you. The two best known in the implantable devices industry areHittman Materials (now Wilson Greatbatch Technologies, Inc.) and W.C. Heraus. Bothcompanies are providers of precious metals and special material processing for implantabledevices. If you approach vendors other than Hittman or Heraeus, be aware that “desirablecharacteristics” vary depending on the application. For example, one form of titaniumnitride coating (a shiny golden finish) generates a very hard, smooth surface and is used onmetal mold surfaces and surgical tools. But the form of titanium nitride preferred forWarning! Chloroiridic acid, iridium trichloride, and hydrochloric acid are relativelydangerous materials. Do not breathe dust or mist and do not get in eyes, on skin, or onclothing. Sodium phosphate dibasic is an eye and skin irritant. When working withthese materials, approved safety goggles or glasses must be worn. Contact lenses arenot protective devices: Appropriate eye and face protection must be worn instead of, orin conjunction with, contact lenses. Wear disposable protective clothing to preventexposure. Protective clothing to prevent skin contact includes a lab coat and apron,flame- and chemical-resistant coveralls, gloves, and boots. Follow good hygiene andhousekeeping practices when working with these materials. Do not eat, drink, or smokewhile working with them. Wash hands before eating, drinking, smoking, or applyingcosmetics.5The Bell Jar (ISSN 1071-4219) is a short magazine on vacuum technique and related topics for the amateurinvestigator. It is edited and published by Steve Hansen, who can be contacted through the Bell Jar’s Web site atwww.belljar.net, or by mail at 35 Windsor Drive, Amherst, NH 03031.
334 STIMULATION <strong>OF</strong> EXCITABLE TISSUESelectrodes (a dull charcoal color) is a microporous structure that has a very rough texturerather than a smooth one.Our experience with electrodes coated with titanium nitride and IROX is that they performsimilarly. Typical capacitances are in the range 10 to 20 µF/mm 2 . Platinum black andactivated glassy carbon are other electrode materials that have high capacitance and exhibitexcellent biocompatibility. Other interesting possibilities are to coat the electrode with layersof microspheres to increase the wetted surface or to create porous metallic electrodesand then “plug” the pores with carbon.Neuromuscular Electrical StimulationNeuromuscular electrical stimulation (NMES) is the use of electrical stimulation of theintact peripheral nervous system to contract a muscle, either through direct activation ofthe motor neurons in the mixed peripheral nerve, or indirectly through reflex recruitment.When the stimuli are used to activate muscles directly, without activation of the peripheralnerve, the modality is known as electrical muscle stimulation (EMS).NMES may be used for therapeutic or functional purposes. Therapeutic use is directedtoward lessening impairments, prevention of secondary complications, or halting progressionof a disabling condition. Therapeutic NMES includes strengthening muscles, lesseningof spasticity, preventing muscle atrophy, and improving regional blood flow.Functional NMES is more commonly known as functional neuromuscular stimulation(FNS), which is a replacement for lost or impaired motor control. Today, transcutaneousFNS is widely used in the rehabilitation of paralyzed patients in whom natural nervouscontrol of muscular contraction has been lost due to a spinal cord injury or a central nervoussystem disorder. In its best known applications, FNS has been used to restore functionto affected limbs by providing artificial electrical stimulation patterns that enable the subject,for instance, to use upper extremity functions, to stand up, or to walk [Kralj and Bajd,1989].One or more pairs of surface electrodes along with conductive creams or gels are usedto activate the excitable tissues. Surface electrical stimulation typically consists of a trainof regular monophasic or biphasic pulses. The rate at which the nerve fibers fire dependson the frequency of pulse repetition. A single pulse produces a short-lived muscle twitchof not more than 250 ms. If pulses are repeated more frequently than this, the muscle doesnot have time to relax between stimuli, and at some point tetanic (continuous) contractionoccurs.Regardless of what mechanism is used to evoke muscle contractions, nerve and musclestimulators are FDA class II prescription devices. The international standard that specificallycovers the design, performance, and testing of these devices is IEC-60601-2-10, MedicalElectrical Equipment—Part 2: Particular Requirements for the Safety of Nerve and MuscleStimulators.Transcutaneous NMES devices are relatively simple. Figures 7.17 and 7.18 show thecircuit diagram of a battery-powered stimulator that can be used in NMES therapy and asan output channel for transcutaneous FNS. Whenever a stimulus is required, Q1 dischargesC1 into step-up transformer T1, which yields a high-voltage pulse on its secondary. Thetransformers that we have used successfully are the type built for the small invertersdesigned for fluorescent lamp lanterns. The high-voltage pulse (150 V peak) chargescapacitor C2 to a voltage regulated by zener D1. The setting of R5 selects the current thatflows through the electrodes. With switch SW1 open, the pulse output is monophasic(although the capacitance of the electrodes will generate a discharge phase through R7).With the switch open, the charge accumulated in the coupling capacitor (C2 and C3 backto-backin series 5µF nonpolar) flows through the electrodes after the stimulus to yieldnet-zero charge transfer through the tissue.
WAVEFORM:CLOSED = MONOPHASICOPEN = ASYMMETRIC BIPHASICSW2+ C12200uF+9VR310T1INVERTER TRANSFORMERR447kR510k LINEAR TAPER"HIGH ELECTRODEIMPEDANCE" WARNINGD2RED LEDD4ECG5055AQ2ECG287D31N4007+C210uF, 100VR7100kC3+10uF, 100VJ11J21ANODETO ELECTRODESCATHODER110012Q1IRF510/TOC10.01uFD11N4737AR6100R2100k3SW1OUTPUT CURRENTCONTROL: 0-60mAC50.1uF+ C4100uFBT19V ALKALINEFigure 7.17 Output stage of a simple neuromuscular electrical stimulation (NMES) device that can be used for transcutaneous electricalstimulation of muscle contractions either through direct activation of the muscle fibers or through excitation of the motor neurons in themixed peripheral nerve and/or through reflex recruitment.PULSE335
PULSER9250kR148.2kEXTERNAL TRIGGERSIGNAL ISOLATOR+9VR3510IC11 624N2654R247kR410kR5100k231R110kQ12N2222CYCLE FREQUENCYCONTINUOUSSTIM PULSE RATE:10 to 100Hz+9VEXTERNAL25TRCV4IC4NE555QDISTHR3RR153.9kCYCLICD1GREEN LEDC30.01uF25TRCV4IC3NE555QDISTHRR7270k376C40.01uFPULSEWIDTH: 10to 300 usRC20.01uF25TRCV4IC2NE555QDISTHR376R8250kR123.9kSW3TRIGGERMODESELECTORR11110R133.9kC11000pFR1010kR"STIM"INDICATORR6250kR163.9k76C51uFC61uFC71000pFSTIMULATION TRAINREPETITION-RATEGENERATORSTIMULUS PULSEREPETITION-RATEGENERATORSTIMULUS PULSE-WIDTHMONOSTABLE GENERATORFigure 7.18 This circuit drives the output stage of Figure 7.17 to produce output pulses 10 to 300 µs in duration at a frequency of 10 to 100 Hz.J1BNC12336
DIRECT STIMULATION <strong>OF</strong> NERVE <strong>AND</strong> MUSCLE 337The circuit of Figure 7.18 drives the output stage to produce output pulses 10 to 300 µsin duration (based on the setting of potentiometer R9) at a frequency of 10 to 100 Hz(depending on the setting of potentiometer R6). Pulse-rate generator timer IC3 is eitherconstantly enabled or turned on and off, depending on the setting of switch SW3. In thecyclic setting, the burst duration and frequency is defined by IC2 to the setting of R8. Inthe external mode, the trigger time and duration of the stimulus burst are set to the timethat an external controller (e.g., a microcontroller in a FNS system) energizes the LED inoptocoupler IC1.There is clinical evidence showing that appropriate electrical stimulation can cause adenervated muscle to contract, which in turn may help limit edema and venous stasiswithin a muscle and therefore delay muscle fiber degeneration and fibrosis. Studies seemto indicate that proper use of EMS shortens recovery time following denervation.EMS is not necessarily a benign therapy, however. Some studies indicate that contractionof a denervated muscle may disrupt regenerating neuromuscular junctions and subsequently,delay reinnervation. In addition, denervated muscle is more sensitive to traumathan is innervated muscle, and electrical stimulation may further traumatize the denervatedmuscle. Moreover, prolonged electrical stimulation until reinnervation occurs is often notworth the costs or time involved.Television has popularized the cosmetic use of EMS devices. Late-night infomercialsclaim that muscle stimulators can help in losing weight and increasing muscle definitionthrough “no-work” or “passive” exercising. Despite the “guaranteed results” offered bythese advertisements, don’t count on looking like Venus or Adonis by slapping on somegelled electrodes to twitch your beer belly. There is no clinical evidence that electricalmuscle stimulation would provide any benefit toward weight loss and body toning.In fact, the FDA has seen no evidence that these devices are safe and effective for homeuse or for applications touted in health spas and beauty salons. FDA considers electricalmuscle stimulation to be misbranded and fraudulent when promoted for weight loss orbody shaping. There are currently no acceptable uses for these devices when labeled forover-the-counter use. When labeled for medical use by a licensed practitioner, the followinguses are generally recognized as acceptable:• Relaxation of muscle spasm• Prevention or retardation of disuse atrophy• Muscle reeducation (e.g., rehabilitation of muscle function after a stroke)• Increasing local blood circulation• Immediate postsurgical stimulation of calf muscles to prevent venous thrombosis(formation of blood clots)• Maintaining or increasing range of motionThe bottom line on the cosmetic use of electrical muscle stimulators: If you want tolook like the models in muscle stimulation commercials, do not buy the stimulator, but doget on a diet and join a health club.Transcutaneous Electric Nerve StimulationTranscutaneous electrical nerve stimulation (TENS) provides symptomatic relief fromsome forms of chronic or acute pain, including postsurgical and posttraumatic pain. TENSdevices require FDA approval as class II medical devices and need physician prescriptionto be dispensed to or used on patients. Electrodes are placed at specific sites on the bodyfor treatment with TENS. The current travels through electrodes and into the skin, stimulatingnerve pathways to produce a tingling or massaging sensation that reduces the
338 STIMULATION <strong>OF</strong> EXCITABLE TISSUESperception of pain. When used as directed, TENS is a safe, noninvasive, drug-free methodof pain management. TENS has no curative value; it is a symptomatic treatment that suppressespain sensation that would otherwise serve as a protective mechanism on the outcomeof the clinical process. As such, it is used only to offer a better quality of life forpeople with pain when the source of the pain cannot be treated. It must be noted, however,that none of the studies have proven conclusive, and there is still quite a bit of debate aboutthe degree to which TENS is more effective than placebo in reducing pain. Generally,TENS provides initial relief of pain in about 70% of patients, but the success rate decreasesafter a few months to around 25%.The most accepted theories of how TENS may work are:• Gate control theory: suggests that by electrically stimulating sensory nerve receptors,a gate mechanism is closed in a segment of the spinal cord, preventing pain-carryingmessages from reaching the brain and blocking the perception of pain.• Endorphin release theory: suggests that electrical impulses stimulate the productionof endorphins and enkaphalins in the body. These natural, morphinelike substancesblock pain messages from reaching the brain, in a manner similar to conventionaldrug therapy but without the danger of dependence or other side effects.• Descending inhibitory pathway theory: suggests that noxious stimuli excite the smallerpain fibers, leading to activation of the brainstem reticular formation. This releases serotonin(a neurotransmitter related to the feeling of well-being), which in turn inhibitspain at the spinal cord level. Putting it shortly, “pain inhibits pain.”The practitioners of quack treatments credit TENS with restoring “energy lines” andstimulating “acupuncture points.” Don’t waste your time considering such claims.The circuit for a battery-powered two-channel TENS unit is shown in Figure 7.19. Inthis circuit, timer IC1 produces a pulse every time the stimulation channels need to be triggered.The rate at which the trigger pulses are generated is set via R1. With the componentvalues shown in the circuit, trigger frequency can be varied between 3 and 100 Hz. Constantpulsing at a set frequency is known in TENS jargon as the conventional mode.What is commonly known as conventional TENS is to stimulate at a relatively high frequency(40 to 150 Hz) and low current (10 to 30 mA), barely above the threshold of sensation.The reported onset of analgesia with these parameters is virtually immediate. Painrelief lasts while the stimulus is turned on, but it usually returns when the stimulation isturned off. Patients often leave the electrodes in place all day and turn stimulation on for30 to 60 minutes whenever they need it. In the low-frequency conventional mode, theTENS unit is set to deliver pulses at 1 to 10 Hz, but the stimulus intensity is increased closeto the patient’s tolerance limit. The belief is that this will increase the time of analgesiaafter therapy because of the release of natural morphinelike substances. This stimulationmode is uncomfortable, and not many patients can tolerate it.Burst TENS uses low-intensity stimuli firing in high-frequency bursts. Each burst deliverssome 5 to 10 pulses at a rate of 100 Hz, with rests between bursts. Patients usuallyreport that each burst is felt as a single pulse, making it more comfortable than single-pulsesensation. No particular advantage has otherwise been established for the burst methodover the conventional TENS method. The TENS circuit of Figure 7.19 implements thelow-frequency burst mode when SW2 connects the reset line of timer IC3. This IC3 periodicallyinhibits IC1 from oscillating. The fundamental burst frequency is approximately2 Hz, which allows approximately seven trigger pulses to be issued by IC1 per burst cycle.Ramped modulation is a feature that is often encountered in TENS units to cause a gradualrise and decline of amplitude and frequency, resulting in a comfortable stimulation sensation.It is very similar to the conventional mode, but a modulation in pulse rate andamplitude is thought to avoid nerve adaptation and accommodation, which diminishes the
BT1 BT2 BT3 BT41.5V1.5V1.5V1.5VSW1POT SWITCHCHANNEL 1IC2LM555DSCHGCVRSTTHRTRGVCC1OUT3R1468kR833kNORMALSW3D2FDH300R43.6kR108.2k785462CVRSTIC1LM5551+ C12.2uFOUT3D11N4148R17100R2220R333+C3180uFR13330GNDGNDC415uf+LOWMODULATIONSW2POT SWITCHRATECONTROLR1470kR1691D41N4148R510kC50.1uFDSCHGTHRTRGVCCC20.033uFR620kR1191kQ2MPSA63INTENSITYCONTROLR910kR125.6kQ1ZTX653/TOD31N414814T1ELECTRODE 15681A1AELECTRODE 2R19560kR2191k75462IC3LM5553R2018kQ42N3904D6R1833YELLOW LEDELECTRODE 1GNDC91u F+C1080.1uFDSCHGCVRSTTHRTRGVCC1Q32N4403OUTC81uF+STIMULATIONONBATTERY IN5V OUTD51N4759Q5ZTX653/TOHV OUT 1CHANNEL 21ATRIGGER INHV OUT 21AELECTRODE 2Figure 7.19 Circuit of a battery-powered, two-channel TENS unit. IC1 produces a pulse every time the stimulation channels need to betriggered. The trigger frequency can be varied between 3 and 100 Hz. Burst TENS is activated when SW2 connects the reset line of timerIC3 periodically to inhibit IC1 from oscillating. Modulated TENS is enabled by closing SW3, which allows a triangle wave generated byIC2 to modulate the frequency of IC1. The electrodes are driven by step-up transformer T1. Stimulation current is controlled via R9, whichsets the current that Q1 allows across the primary of the step-up transformer. The peak current of a pulse into a purely resistive load of 500 Ωcan be varied between 0 and 150 mA.754628C70.1u FR71kR15330k+C62.2uF339
340 STIMULATION <strong>OF</strong> EXCITABLE TISSUESeffectiveness of conventional TENS. When the circuit is operating in the conventionalmode, modulation can be employed by closing SW3. This allows a triangle wave generatedby timer IC2 to be fed to the control voltage input of IC1. The modulating signal frequencyis approximately 1 Hz, which induces a 40% change in the selected conventional-modefrequency. Note that when modulation is enabled, the timing characteristics of the triggerpulses generated by IC1 change such that pulse amplitude is modulated to 25% on eachmodulation cycle.The electrodes are driven by step-up transformer T1. A stimulation pulse is generatedevery time Q5 is driven into conduction by the Darlington pair Q2 connected to the outputof IC1 via ac-coupling capacitor C2. LED D6 flashes each time that a stimulation pulse isdelivered. The constant-current amplitude is set via R9, which controls the current that Q1allows across the primary of the step-up transformer. The peak current of a pulse into apurely resistive load of 500 Ω can be varied between 0 and 150 mA. The shape of the pulsedelivered to the skin electrodes is shown in Figure 7.20. The load used to simulate the bodyimpedance is the one specified in the American National Standard for TranscutaneousElectrical Nerve Stimulators (ANSI/AAMI NS4-1985). The preferred waveform is biphasic,to avoid the electrolytic and iontophoretic (whereby ions and charged molecules canbe driven through the skin by an electrical current) effects of a unidirectional current.Power for the stimulator is controlled independently via the potentiometer switchesSW1 of each channel. When either channel is on, current supplied by the four alkaline batteriesin series is delivered to the timer ICs via diode D1 of the active stimulation channel.Each output channel is isolated from the other, which allows two distinct areas of pain tobe stimulated independently.TENS electrodes are usually placed initially on the skin over the painful area, but otherlocations, such as over cutaneous nerves, may give comparable or even better pain relief.TENS should not be applied over the carotid sinuses, due to the risk of acute hypotension(because of stimulation of the vagus nerve), over the anterior neck because of possiblespasm of the larynx, or over an area of sensory impairment where the current could burnthe skin without the patient becoming aware of it. Of course, TENS should not be used inpatients with any active implantable medical device (e.g., pacemakers and implantabledefibrillators) because of the risk of interfering with or damaging the implantable device.In addition, TENS should not be used during pregnancy because it may induce prematurelabor.A relatively new TENS-like modality is percutaneous electrical nerve stimulation(PENS), which is often incorrectly called electroacupuncture. Rather than using surfaceelectrodes, PENS uses needle probes as electrodes, placed just under the outer layers ofthe skin in the region where the patient feels pain. The only advantage of PENS over TENSis that it bypasses local skin resistance and delivers electrical stimuli at the precise leveldesired, in close proximity to the nerve endings.Interferential StimulationStimulating deep tissues using surface stimulation electrodes requires that very strong currentsbe delivered to the skin to yield sufficiently high currents to depolarize target tissue.Strong pulses are often painful, limiting their clinical applicability, especially when electricalstimulation is used for therapeutic purposes (e.g., TENS, or for the stimulation ofdeep muscles such as those of the pelvic floor). As shown in Figure 7.21, interferential currenttherapy (IFC) is based on the summation of two ac signals of slightly differentfrequency that are delivered using two pairs of electrodes. Each of the few-kilohertz “carriers”on their own do not cause skin sensations or stimulation of the underlying tissues.However, the tissue causes the signals to mix or interfere with each other, resulting in alow-frequency current that consists of cyclical modulation of amplitude, based on the
DIRECT STIMULATION <strong>OF</strong> NERVE <strong>AND</strong> MUSCLE 3411VoltageCurrent1CH1GNDGNDCH2OSCILLOSCOPETENS UNIT5.1ELECTRODE 164ELECTRODE 28.STEPUP TRANSFORMER200, 500, 1k12.7k0.1uF1/10 ATENS CURRENT WAVEFORM300us60usTENS TEST LOADper ANSI/AAMI NS4 - 1985A = 0 to 150mA20us1/2 AFigure 7.20 Stimulation pulse delivered to the skin electrodes by the TENS generator of Figure 7.19. The American National Standard forTranscutaneous Electrical Nerve Stimulators (ANSI/AAMI NS4-1985) specifies the load used to simulate the body impedance.difference in frequency between the two carrier signals. When the signals are in phase, thelow-frequency components sum to an amplitude that is sufficient to stimulate, but no stimulationoccurs when they are out of phase. The beat frequency of IFC is equal to thedifference in the frequencies of the two carrier signals. For example, the beat frequency,and hence the stimulation rate of an interferential unit with signals set at 4 and 4.1 kHz, is100 Hz.The interferential method is used most often for the therapeutic stimulation of nervesand muscles in the treatment of acute pain, edema reduction, and muscle rehabilitation. Itis not a common modality for functional neuromotor stimulation because it requiresgreater energy consumption and a larger number of electrodes. Scientists in the formerSoviet Union also use interferential currents delivered through scalp electrodes to producenarcosis (electronarcosis) and anesthesia (electroanesthesia). This last application, whichdoes not involve causing convulsions as with ECT, is very controversial and seldom usedin Western psychiatry.IFC stimulators commonly use carrier frequencies around 4 to 5 kHz, with sinusoidalwaveforms that can reach peak-to-peak voltages of 150 V and force currents of up to 100 mA
342 STIMULATION <strong>OF</strong> EXCITABLE TISSUESElectrodesChannel 1 Channel 25kHz4.92kHzLimbTargetTissueStimulation Current is “beat tone” at 80 HzFigure 7.21 Interferential current therapy (IFC) is based on the summation of two ac signals ofslightly different frequency that are delivered using two pairs of electrodes. Each of the few-kilohertz“carriers” on their own do not cause skin sensations or stimulation of the underlying tissues. However,the tissue causes the signals to mix or interfere with each other, resulting in a low-frequency beat currentcapable of stimulating the tissue.RMS. The most common beat-frequency therapy ranges are 1 to 10 Hz for edema, 1 to150 Hz for rehabilitation of muscle, and 80 to 150 Hz for the control of pain. Figure 7.22shows a simple circuit that can generate interferential audio-frequency currents. The poweramplifier sections are based around the ST Microelectronics TDA2005 10 W 10 W audioamplifier IC. This IC is intended specifically for use in bridge amplifier designs in car audiosystems. It is a class B dual audio power amplifier with a high output current capability ofup to 3.5 A, ac and dc output short-circuit protection (one wire to ground only), and thermalshutdown protection, and is capable of driving very inductive loads. Although it can be usedas a dual amplifier by operating each half of the device separately, in this application it isconfigured for operation as a bridge amplifier. With this mode, the current and voltage swingsin and around the IC are twice that of a single amplifier, which results in a power output fourtimes greater than that of a single amplifier with the same load connected to the output pins.Two audio-output transformers are used in reverse to step up the amplifier’s output voltageall the way up to the 150 V pp necessary to push up to 100 mA RMS through the body.We used Hammond 1615 audio-output transformers in reverse; that is, the 8-Ω speakeroutputs were connected to the outputs of the power amplifiers, and the 5-kΩ inputs wereconnected to the electrodes. As with all bridge amplifier designs powered from a singlesupply, both output terminals of the TDA2005 are held at half the supply voltage, whicheliminates the need for the usually large-value dc blocking capacitor in series with the outputtransformers. The power amplifiers are driven through audio isolation transformers. Thecomplete circuit should be powered from an IEC601-compliant power supply ratedfor 12 V at 5 A or more, for example using a Condor model MD12-6.8-A medical-gradelinear supply.
ELECTRODE 3BODY PARTTO BESTIMULATED+12V_ISOELECTRODE 2FROM PCSOUNDCARDJ1PHONEJACK STEREOT1AUDIO ISOLATION12 3 1 5BLK/YEL24 875846YELLOW19 3111 510BLK/YELT2AUDIO ISOLATION4 8C42.2 uFC17++2.2uFC10.1uFC72.2 uF+C14C110.1uF+2.2 uF1IC1TDA20059* HEATSINK5* HEATSINK3+12V_ISOIC2TD A20056R1120K+1110C12+C22.2 uFC9 +220uFR8120K2.2uF8427C19220uF+++C3100uF+ C8220uFR410C13100uF+ C18220uFR1110+R31KR610+R101KR1310C16100uFC6100u FR52.2KR122.2 KC50.1u FC100.1uFC150.1uFR21 O hmR71 O hmR91 O hmC200.1uFR141 O hmT3Hammond 1615YELLOW14T4Hammond 161514568568BLUEBROWNBLUEBROWNELECTRODE 1TARGETTISSUEELECTRODE 4Figure 7.22 An experimental interferential-mode stimulator uses two audio-output transformers as step-up transformers. The primaries aredriven by bridged audio amplifiers at carrier frequencies around 4 kHz with peak-to-peak voltages of 150 V and force currents of up to100 mA RMS. Audio signals are generated by the PC sound card running a beat-tone generator program. The most common beat-frequencytherapy ranges are 1 to 10 Hz for edema, 1 to 150 Hz for rehabilitation of muscle, and 80 to 150 Hz for the control of pain.343
344 STIMULATION <strong>OF</strong> EXCITABLE TISSUESThe exact frequency difference and phase relationship between the carrier signals has atremendous effect on the site inside the body at which the differential stimulation will takeplace. For this reason, the majority of audio signal generators used in modern IFC stimulatorsare based on direct-digital synthesizers (see Chapter 6). The simplest way to drivethe experimental IFC stimulator circuit of Figure 7.22 is to use the PC sound card and softwarethat is freely available for download from the Web, such as the beat-tone generator(BEATINBRAIN.EXE, freeware for Windows 9x, 2000, NT) by the Physics Lab of RutgersUniversity, a copy of which is supplied for your convenience in the book’s ftp site.Although this program is not designed specifically for IFC stimulation, 6 it generates twosine waves of different frequencies through the left and right sound card channels thatcan be used to drive the isolated high-voltage output stages. If you are a Matlab user, youcan devise complex frequency and phase shifts between the carriers. The data streams canthen be played using the sound(y, Fs) command, where y is an N 2 matrix thatcontains the sine-wave data to be played through each one of the sound card channels andFs is the sampling frequency.The risks associated with interferential stimulators is much larger than those fordevices that deliver narrow stimulation pulses. The reason is that the carrier signals areconstantly on and convey quite a bit of power through the tissue. IFC stimulators, especiallythose that do not have electrode impedance monitoring with automatic turn-off,require special attention to electrode selection, placement, and maintenance. If you everuse or build an IFC stimulator, first connect a 2-kΩ 1 -W resistor between one of the electrodepairs. Crank the power up until the resistor bursts into flames. This is exactly what4will happen to skin if electrode contact is poor. As such, when placing electrodes for IFC,it is imperative that they are not touching and will not touch each other, since burns onthe edges of the electrodes as well as on the skin will occur if electrodes are touching duringstimulation. Even though the electrodes may appear to be far enough apart, rememberthat when a muscle comes into contraction, it can bring the electrodes together. Inaddition, if you use carbon-loaded silicone electrodes, always remember to apply andmaintain a sufficient amount of an appropriate conductive medium, such as water-soakedsponges or especially formulated electrotherapy gel to prevent burns during stimulation.Finally, never even consider passing IFC currents through the brain. Remember the “thisis your brain on drugs” advertising? Well, misapplication of IFC takes the fried-egg analogyone notch up on the realism scale.General Safety Precautions and Contraindications forTranscutaneous Electrical Stimulation TherapiesAll transcutaneous electrical stimulation devices (e.g., TENS, EMS, IFC, as well as iontophoresisunits) are classified by the FDA as either class II or class III medical devices 7and require physician prescription to be dispensed to or used on patients. The fact thatsome of these devices are sold without a prescription by unscrupulous online vendors maymake a lot of people believe that they cannot do any damage. However, most electricalstimulation therapies carry significant risks with them. The following should be consideredbefore using any form of transcutaneous electrical stimulator:6The brain is able to combine two pure tones, each sent to a separate ear, to produce a beat tone at the differencefrequency. Some researchers believe that this binaural beat effect can be exploited to affect brain states positivelyusing difference frequencies related to those of the alpha, beta, and theta brainwaves. Even if it would be demonstratedthat the brain can be trained to generate specific frequencies, whether or not altering the brainwaves hasany effect on mind, body, or mood is subject to considerable debate.7For the FDA’s definition of class II and class III medical device, see the Epilogue.
• Cardiac demand pacemakers that detect a user’s heart rate and turn on a pacemakerwhen the heart rate falls below a predetermined level can in certain circumstances beaffected by stimulation. This is because the pulses from the stimulator may be confusedwith the heart’s intrinsic signals and fool the pacemaker into thinking that theheart is beating faster than it is. A pacemaker or implantable defibrillator should beconsidered to be an absolute contraindication to upper limb and shoulder stimulation.Electrical stimulators can sometimes be used with caution for lower limb applicationsin these patients as long as the action of the pacemaker/defibrillator and heart ischecked by a cardiologist while the stimulator is in use.• Electrical stimulation should be used with extreme care in patients with any othertype of active implantable medical device, such as a spinal cord stimulator or intrathecalpump. This is because electrical stimulation currents can interfere with the operationor even damage the circuitry of an implanted device. In addition, electricalstimulators should not be used over metal implants, whether active (pacemakers,spinal cord stimulators, etc.) or passive (orthopedic nails, metal plates, prostheticjoints, etc.) because these will distort the flow of current through the body and maycause internal hot spots with high current density that can destroy adjacent tissues.• Electrical stimulation should not be applied over the eyes or the carotid sinuses (sideof neck), due to the risk of acute hypotension through a vasovagal reflex.• Electrical stimulation electrodes should not be placed over the anterior neck becauseof possible laryngospasm due to laryngeal muscle contraction.• Electronic equipment such as ECG monitors, ECG alarms, sleep apnea monitors, andso on, may not operate properly when electrical stimulators are in use.• Electrical stimulation should not be used during pregnancy because it may inducepremature labor.• With the exception of electrical stimulation that is specifically intended for the stimulationof the brain, electrodes should never be placed to cause current to flow transcerebrally(through the head), as this may induce seizures and have other undesirableneurological consequences.• With the exception of electrical stimulation that is specifically intended for stimulationof the heart, electrodes should never be placed to cause current to flow across thechest (e.g., both arms simultaneously) because electrical stimulation currents maycause or lead to arrhythmic events. For the same reason, patients should be warnednever to handle the electrodes while a stimulator is on since a current path throughthe heart could be created by accident.• There are rare anecdotal reports that people who have poorly controlled epilepsy havehad symptoms increased after using electrical stimulation. There is no known mechanismfor this effect, but our advice is that electrical stimulators should not be usedin patients with epilepsy that is not well controlled by drugs.• Because electrical stimulation (especially EMS and IFC) will increase local bloodcirculation, it is possible that stimulation in the area of a malignant tumor mightincrease the rate of metastasizing and therefore the spread of the cancer. Electrodesshould never be placed over the area of a known tumor.• Long-term stimulation at the same electrode site may cause skin irritation throughpossible allergic reaction to tape or gel. Poor skin condition can be a problem whenself-adhesive skin electrodes are used. This is because there is a greater chance ofskin irritation. Electrodes should never be placed over broken skin or over rashes,blisters, spots, and so on.• Electrical currents used in some modes of electrical stimulation (e.g., IFC) are largeenough that they may cause skin burns under the electrodes. For this reason, theelectrodes should not be placed in an area of sensory impairment (e.g., in cases ofDIRECT STIMULATION <strong>OF</strong> NERVE <strong>AND</strong> MUSCLE 345
346 STIMULATION <strong>OF</strong> EXCITABLE TISSUESnerve lesions, neuropathies) where the possibility exists that the patient would not feelthat the skin is being burned.• People who have a spinal cord injury may be subject to episodes of autonomicdysreflexia. This is characterized by a rise in blood pressure elicited by a noxious stimulussuch as electrical stimulation (e.g., FNS) applied below the level of the lesion.• Electrical stimulators should not be used while driving or operating dangerousmachinery.MAGNETIC STIMULATIONExcitable tissue can be stimulated by strong, time-varying magnetic fields. As shown inFigure 7.23, a coil is placed over the tissue to be stimulated and a capacitor bank is dischargedinto the coil. Because of Faraday’s law of induction, the time-varying current inthe coil generates a time-varying magnetic field, which induces eddy currents in the tissue,causing stimulation. Note that we are not talking about some nonmedical therapy involvingweak magnets alleged to promote health. We are talking about producing eddy currentsthat are strong enough to actually depolarize cell membranes and hence activate excitabletissue. This is electrodeless electrical stimulation, where the magnetic field is only themedium used to transfer electrical energy from the coil to the tissue. The magnetic fieldstrengths need to reach a peak of several tesla (comparable to the static magnetic field ofMRI machines, some 40,000 times the Earth’s magnetic field), which is usually achievedby driving the stimulating coil with brief current pulses of several kiloamperes.Plain electrical brain stimulation is possible noninvasively using scalp electrodes. However,transcranial electrical stimulation (TCES) is very painful because of activation of painfibers in the scalp and hence is of limited clinical value. On the other hand, magnetic stimulationof the brain and peripheral nerves is painless. The reason for this difference is thatin direct electrode stimulation, the stimulus current decays as a function of the impedanceof the tissue between the electrodes and the target tissue. On its way to the brain, the currentmust pass through the highly resistive scalp and skull. Hence, to deliver sufficient electriccurrent to neural tissue within the brain requires much higher currents to be delivered to thescalp. The narrow (e.g., 50 to 100 µs in duration) high-voltage pulses (800 V) producevery high current densities close to the electrodes, which activate the pain receptors. In con-BICoilELocaldepolarizationEAxon membraneFigure 7.23 Excitable tissue can be stimulated by strong, time-varying magnetic fields. A coil isplaced over the tissue to be stimulated and a capacitor bank is discharged into the coil. Because ofFaraday’s law of induction, the time-varying current I(t) in the coil generates a time-varying magneticfield B which induces eddy currents in the tissue, causing an electric field E that leads to stimulation.
MAGNETIC STIMULATION 347trast, a magnetic field penetrates all body tissues without alteration, falling off in magnitudeonly as the inverse square of the distance. As such, much lower currents are generated atscalp level to induce the same amount of current at the target brain structure.The idea of magnetically stimulating excitable tissue is not new. The first experimentswith magnetic stimulation were conducted by d’Arsonval in 1896. He reported phosphenes(visual sensations) and vertigo when placing a subject’s head inside an induction coil.Magnetic stimulation of human peripheral nerves stimulation was accomplished byBickford and Fremming [1965] using an oscillatory magnetic field that lasted 40 ms.Modern magnetic stimulation is based on research by Polson et al. [1982], who constructeda pulsed magnetic stimulator for peripheral nerve stimulation. They used a pulseof 2 ms duration, which allowed them to record motor-evoked potentials (MEPs) by stimulatingthe median nerve.Electric Field Induced by Magnetic StimulationThe large time-varying magnetic field B required to induce an electric field E in theexcitable tissue is obtained by passing a pulsed current I(t) through a coil placed close tothe target tissue. The relationship between the electric field induced and the magnetic fieldis obtained from Faraday’s law:∇ ⊗ E ∂B∂twhere the magnetic field produced by the coil is given by the Biot–Savart law:B(r, t) µ 0I (t)4π dl(r ) ⊗( r r)C |r 3r|where the integration is performed with the vector dl along the coil windings C, r is theposition in the tissue, and r is a point in the coil. The permeability of free spaceµ 0 4π 10 7 H/m can be assumed, since the permeability of tissue is nearly equal to thatof free space, and the conductivity is approximately 1/Ωm. The electric field E causesmovement of charges in both the intra- and extracellular spaces. Any part of the cell membraneinterrupting this charge flow becomes depolarized or hyperpolarized. Once themembrane threshold potential is exceeded, an action potential occurs.The shape of the electric field induced in the tissue depends on the shape of the inductioncoil, the location and orientation of the coil with respect to the tissue, and the electricalconductivity structure of the tissue. We refer you to Ruohonen’s Ph.D. thesis [1998] fora detailed model of the currents induced in the tissue.Design of Magnetic StimulatorsFrom a device engineering point of view, these models are more than an academic exercisesince they yield estimates of the threshold magnetic field needed to cause activationof excitable tissues. Since the cell membrane of excitable tissues behaves as a leaky integrator,the most effective induced current will have a duration in the same range as that ofthe membrane’s time constant. The approximate value for the membrane of neurons isaround 150 µs, and typical magnetic stimulators for use in neurology produce magneticpulses that last anywhere between 100 and 600 µs. Coils usually consist of 10 to 20 turnsof heavy copper tubing or wire. Typical peak currents driven through the coil are in therange 5 to 15 kA to generate peak magnetic field strengths in the range 1 to 5 T.Figure 7.24 shows the circuit diagram for an experimental magnetic stimulator basedon a design proposed by Merton and Morton [1980]. The high-voltage output of transformerT1 is rectified by D2–D4 and charges a 2100-µF capacitor bank through resistor
348 STIMULATION <strong>OF</strong> EXCITABLE TISSUESWarning! This is an extremely dangerous device! It produces high voltages backed bysufficient energy to cause lethal electrical shocks. This is definitely a project that shouldnot be attempted by anyone who is not experienced with high-voltage/high-energydevices. Just consider that TNT releases approximately 2 kJ/g. As such, a short acrossthe capacitor bank would definitely blow up the weakest link in the chain with the forceof a small explosive charge. Needless to say, any remains will turn into shrapnel thatcan cause further injury or death. Consider that 2 kJ is the equivalent energy of droppinga 100-kg anvil on your foot from a height of 2 m.R2. The capacitor bank consists of nine Cornell Doubilier type 400X212U450BF8 2100-µF 450-V dc electrolytic capacitors in series–parallel arrangement. However, because ofits photoflash rating, the PF212V500BF2B would be a better choice. Resistors R4–R6,R9–R11, and R14–R16 equalize the voltage drop among all capacitors. These resistorsalso bleed any remaining charge on the capacitors after the device is used. The capacitorbank can be charged to a maximum of 1350 V, resulting in the storage of up to CV 2 /2 1.93 kJ. A blinking LED and a Mallory Sonalert II alarm module warn the user when thecapacitor bank is charged.The desired capacitor charge voltage is selected by the user by pressing on the chargeswitch. A keylock switch and an interlock switch also need to be closed to complete thecircuit to energize the charge relay K1, which in turn energizes the primary of high-voltagetransformer T1. The complete high-voltage circuit of the stimulator is contained withina 1 -in.-thick polycarbonate enclosure that acts as a blast shield in case of component failure.Interlock switch SW2 automatically disables charging whenever this polycarbonate2enclosure is opened to access the circuit.The switching element is an International Rectifier type ST330S16P0 high-powerthyristor (SCR). This specific device is rated for a maximum repetitive peak and off-statevoltage of 1600 V. It can handle a 9-kA peak current with a maximum dI/dt value of1 kA/µs. SCR triggering is done through a MOC3010 triac-output optocoupler. Wheneverpushbutton switch SW5 is depressed, the optocoupler allows C4 to discharge between themain gate and the center amplifying gate of SCR1. Diodes D5–D8 prevent the voltage onthe capacitor bank from reversing after the discharge.Suitable coil inductances can be evaluated using the simplified PSpice model shown inFigure 7.25. The capacitors are each modeled as an ideal 2100-µF capacitor with a 40-mΩresistor in series to simulate their high-frequency ESR. The heavy wire carrying the currentto the coil and the coil’s resistance are modeled by a 100-mΩ resistor (R_COIL).Since International Rectifier does not have a PSpice model available for the thyristor, wemodified the instance model for a C228A SCR (which is totally different from aST330S16P0) by setting the model parameters as follows:• VDRM: max. nonrepetitive peak voltage1700 V• VRRM: max. off-state voltage1600 V• IH: max. holding current600 mA• VTM: max. on-state voltage1.66 V• ITM: max. one-peak nonrepetitive surge current8380 A• dV dt: max. critical rate voltage rise400 10 6 V/s• IGT: dc gate current required to trigger200 mA• VGT: dc gate voltage required to trigger2.5 V• TON: typical turn-on time 1 µs
SCR1ST330S16P0L1COILEXTREME DANGER!!! HIGH VOLTAGE / HIGH ENERGYR1400KPOWER SUPPLY+12V+12VAC HOTAC NEULED1Blinking LEDPWR GNDGNDLS1AlarmD15.1VD3T1110VAC/2.5kVACPOWERD4D2K154SW131DIODE R2DIODEDIODER3680kC32100uF 450VC22100uF 450V10k 25W HV6+C12100uF 450V5867+128SW3+4R72.7D540HF100R6330k 1W HVR5330k 1W HVR4330k 1W HVR8RDS1CHARGINGC410uFD740HF100C72100uF 450VC62100uF 450V+C52100uF 450V+++6 4R11330k 1W HVR10330k 1W HVR9330k 1W HVR19D69.1VD840HF10080MIC1MOC3010R13POT1 2C102100uF 450V++R16330k 1W HVC8C92100uF 450V R14330k 1W HV 2100uF 450VR15330k 1W HV+HV Resistor DividerR2030kR18620DVM+12VSW5SW4FIRECHARGECHARGE ENABLEINREFV+GNDV-CONTROL BOX+12VFigure 7.24 Schematic diagram of the experimental magnetic stimulator. A 2100-µF capacitor bank that can be charged to a maximum of1350 V, resulting in the storage of up to 1.93 kJ. The switching element is an International Rectifier type ST330S16P0 high-power SCR ratedfor a maximum repetitive peak and off-state voltage of 1600 V. It can handle a 9-kA peak current with a maximum dI/dt of 1 kA/µs. SCRtriggering is done through a triac-output optocoupler.J1110VACF12FUSE31SW2INTERLOCK SWITCH349
I1TR280IR_TISSUE100k+ –d/dt d/dt10uPOTR24IC =1350V+C22100uFR740mC32100uFR840mR6330kR10330kVCAPACITOR BANKC92100uFR1240mC52100uFR1340mR18330kR10330kC102100uFR1540mC72100uFR1640mR19330kD14Dbreak-XD13Dbreak-XR17330kD9Dbreak-X+-V20 0R_COIL100 mHX2C228AITX11TR40C42100uFR940mR11330kC62100uFR2040mR21330kR2240mC82100uFR2240mR23330k0Figure 7.25 Suitable coil inductances for the magnetic stimulator can be evaluated using this simplified PSpice model. Since InternationalRectifier does not have a PSpice model available for the thyristor, we modified the instance model for a C228A SCR (which is totallydifferent from a ST330S16P0) to model the parameters of the ST330S16P0. Similarly, a breakaway diode model (DBREAK) was modifiedto simulate the behavior of the 40HF100 diodes. The simulation is used to to find an inductance that keeps the peak current within the SCR’scurrent-handling capability (8.3 kA) while conforming to the SCR’s switch-on capability (dI/dt 400 V/µs).V30+–5000350
MAGNETIC STIMULATION 351• T<strong>OF</strong>F: typical turn-off time 100 µs• IDRM: max. off-state leakage current50 mAIn a similar way, a breakaway diode model (DBREAK) is modified to simulate thebehavior of the 40HF100 diodes:• VRRM: max. peak reverse voltage• IRRM• IF(AV): max. average forward current• IF(RMS): max. RMS forward current• IFSM: max. peak surge current• VF(TO)1: low-level value of threshold voltage• VF(TO)2: high-level value of threshold voltage• RF1: low-level value of forward slope resistance• RF2: high-level value of forward slope resistance• VFM: max. forward voltage drop1000 V9 mA40 A62 A570 A0.65 V0.70 V4.29 mΩ3.98 mΩ1.30 VNow the trick is to find an inductance that keeps the peak current within the SCR’s current-handlingcapability (8.3 kA) while conforming to the SCR’s switch-on capability(dI/dt 400 V/µs). The PSpice simulation results of Figure 7.26 show that the peak currentthrough the coil is approximately 8 kA and dI/dt is 270 A/µs, which are both withinthe ST330S16P0’s ratings. The stimulating phase of the pulse lasts for approximately100 µs. The other 900 µs of the current pulse duration doesn’t do much as far as stimulatingthe tissue but causes considerable heat dissipation in the coil.The energy delivered to the coil by the stimulator is really divided into Joulean energyand magnetic field energy. The Joulean energy is from the current flow through the system’sresistance, and is lost as heat. However, some stimulator designs are capable ofrecovering the energy stored in the magnetic field (given by E magnetic LI 2 max/2). For example,Figure 7.27 shows a magnetic stimulator that uses a nonpolar capacitor bank. As shownin the PSpice simulation results of Figure 7.28, when the SCR is triggered, the capacitordischarges through the coil. Selecting L and C to yield an underdamped response, as thecapacitor voltage reaches zero, the coil current and magnetic field are at their maximum. Asthe magnetic field collapses, the coil current continues to flow in the same direction untilit charges the capacitor to the opposite polarity. A diode placed antiparallel to the SCR allowsthe charge to flow back through the coil in the opposite direction, charging the capacitorto its initial polarity. At this point the current stops because the SCR has turned off. If theloss to Joulean heating is low, most of the energy ends up back in the capacitor bank, andonly a small amount of additional power is needed to restore the capacitor voltage.Magnetic Stimulator Coil DesignIn magnetic stimulation, the design of the coil is in many ways far more important than thedesign of the energy source. This is because the coil is placed in very close proximity tothe subject, posing risks of electrocution, burning, and/or mechanical impact to both thesubject and the operator. The following consideration must be made when designing stimulatorcoils:1. The voltage across the coil is typically a few kilovolts. Depending on the coil’s construction,the voltage across adjacent turns will typically be in the range 200 to1000 V. For this reason, insulator materials must be selected such that they can pass
I(R_COIL)V(dIdt)V(CAPACITOR_BANK)I(R_TISSUE)0.2ms 0.4ms 0.6ms 0.8ms 1.0msTimeFigure 7.26 PSpice simulation results for the experimental magnetic simulator show that the peak current through the coil is approximately8 kA and dI/dt is 270 A/µs, which are both within the ST330S16P0’s ratings. The stimulating phase of the pulse lasts for approximately 100 µs.10K0A400V–400V2.0KV0V-10uASEL>>-10uA352
MAGNETIC STIMULATION 353+ –d/dtCOIL_dldtV33.3uR_DUMMY21T0R_CHARGE100k+IC =1600VVITX1I+–V11600VR_CAP10mC1100uFCAPACITORVTRIGGERSCRC228A30mR_COIL7uHCoilR_BODY100kR_DUMMY1T+-V_TRIGGERDbreakD_BACK_EMF00 0 0 00Figure 7.27A magnetic stimulator that uses nonpolar capacitors is capable of recovering the energy stored in the magnetic field.hiPot testing (see Chapter 3) for reinforced insulation. You may remember that partscarrying voltages U between 1 and 10 kV require their reinforced insulation to betested at a voltage of 2(U 2500) for 60 s.2. The intense pulsed currents driven for stimulation cause very strong expanding andcompressing forces in the coil. This is because when magnetic flux lines are packedtogether, they create magnetic pressure. The force of the expanding coil is proportionalto the energy delivered to the coil and related inversely to the coil size. Typicalpressures for circular coils are in the range 500 to 1500 lb/in 2 , making it necessaryto enclose the coil in a potting material (e.g., epoxy) to prevent the coil windingsfrom flying apart when the stimulation pulse is delivered. A detailed analysis ofmagnetic stimulator coil forces was published by Mouchawar et al. [1991].3. Joulean heating of the coil must also be considered, since according to the medicaldevice standards, the surface temperature of the coil must not exceed 41°C. Themain contributor to Joulean heating is the coil conductor’s resistance, which is determinedby the wire material, gauge, and coil geometry. Copper is used almost universallybecause of its relatively high conductivity and good mechanical properties.When the wire cross section exceeds 1 mm 2 , the skin and proximity effects changethe current distribution in the wire, increasing the dc resistance significantly. Striped,foil, or isolated multistrand (litz) wire is often used to reduce the skin and proximityeffects.The term litz wire is derived from the German word litzendraht meaning woven wire.This wire is constructed of individual film-insulated wires bunched or braided together ina uniform pattern. The multistrand configuration minimizes the power losses otherwise
354 STIMULATION <strong>OF</strong> EXCITABLE TISSUESFigure 7.28 When the SCR of Figure 7.27 is triggered, the capacitor discharges through the coil. As the capacitor voltage reaches zero,the coil current and magnetic field are at their maximum. When the magnetic field collapses, the coil current continues to flow in the samedirection until it charges the capacitor to the opposite polarity. A diode placed antiparallel to the SCR allows the charge to flow backthrough the coil in the opposite direction, charging the capacitor to its initial polarity. At this point, the current stops because the SCR hasturned off.encountered in a solid conductor due to the skin effect or tendency of radio-frequencycurrent to be concentrated at the surface of a conductor. A good supplier of litz wire isWireTronic. You can download a free Windows utility from their Web site (WTSETUP.EXE is also provided for your convenience in the book’s ftp site) that will give you dimensionaldata for a wide range of wire sizes, insulation specifications, current-handlingcapacities, resistance calculation, break strength calculation, and ordering information.The coil for our experimental magnetic stimulator was constructed with WireTronic litzwire type 85/26HPN-DN in a flat pancake configuration. The inductance of an air-corepancake coil can be calculated using Wheeler’s formula:rL(µH) 2 2n 8r 11wwhere r is the radius to the center of the winding (in inches), n the number of turns, and wthe width of the winding (in inches). Our prototype coil was wound on the inside of a PVC
MAGNETIC STIMULATION 355tube cap. A hole cut on the side of the cap was fitted with a PVC tube which acts as thecoil handle and wire exit. 24-hour epoxy was used to pot the coil inside the cap. One mustkeep in mind that some glues can damage enamel on coil wire.Coil geometry directly affects the depth and focality (precision of targeting) of the tissueto be stimulated. Standard stimulating coils are circular, with a diameter ranging from50 to 150 mm. Coils designed for focal stimulation, that is, capable of stimulating onegiven area without stimulating a nearby area, usually consist of two adjacent coils withcurrent flowing in opposite directions. Induced currents add at the center of these figureeightcoils, yielding twice the stimulus produced at the edges of the individual coils. Fourleafcoils have been constructed to produce a concentrated dot stimulus useful forperipheral nerve stimulation. Another design that is now being used is the half-toroid coil(as in a Slinky), which is wound with the turns in different angles while maintaining thetangency along one edge to drastically reduce the current induced away from the targetstimulation site.Mouchawar et al.’s paper [1991] provides a thorough analysis of the effect of coil geometryon stimulation. Despite this, designing coils for magnetic stimulators is more an art thanan exact science. To play different “what if” scenarios, we recommend a free finite elementanalysis program called FEMM (Finite Element Methods Magnetics) by David Meeker (suppliedfor your convenience in the book’s ftp site). FEMM is a suite of programs for solvingstatic and low-frequency problems in magnetics. The programs currently address problemson two-dimensional planar and axisymmetric domains. FEMM comprises:• A preprocessor: a CAD-like program for laying out the geometry of the problem tobe solved and defining material properties and boundary conditions• A solver: a device that takes a set of data files that describe a problem and solves therelevant Maxwell’s equations to obtain values for the magnetic field through the solutiondomain• A postprocessor: a graphical program that displays the resulting fields in the form ofcontour and density plotsInterestingly, many theoretical studies have demonstrated that today’s coils are far fromoptimal. These studies also show that power consumption can be reduced drastically, openingmany opportunities for individual innovators in coming up with new ideas that canbecome platforms for completely unexplored applications.Commercial Magnetic Stimulators and Their ApplicationsCommercial magnetic stimulators are not much different than the simple prototype devicediscussed above. The three main commercial players in the magnetic stimulation field areCadwell Laboratories, Inc. (Kennewick, Washington), Magstim Company, Ltd. (Whitland,UK) and Medtronic Dantec NeuroMuscular (Skovlunde, Denmark). One of the newestmagnetic stimulation modalities is repetitive transcranial magnetic stimulation (rTMS),capable of delivering trains of stimuli at 1 to 50 Hz. rTMS was first produced by CadwellLaboratories in 1988. Dantec and Magstim have add-on modules for their single-pulsedevices that can be used to drive one coil with two to four pulses separated by 1 ms to 1 s.As you can imagine, the duration of sustained operation is limited by coil heating, andCadwell solves this problem with continuous water cooling.Single-stimulus magnetic stimulators are used routinely by neurologists as diagnostictools to measure nerve-conduction time. In addition, transcranial magnetic stimulation(TMS) over the primary motor cortex evokes movement in the contralateral limb and has providedinformation on the anatomical organization and functional characteristics of the motor
356 STIMULATION <strong>OF</strong> EXCITABLE TISSUESsystem. TMS can be used to map motor cortex representations precisely. Magnetic stimulationis now used for operating-room monitoring to directly assess the central motor pathways.Recently, rTMS has shown therapeutic potential in the control of depression [Georgeet al., 1996; Pascual-Leone et al., 1996]. Many groups of investigators have demonstratedthat mood can be altered by rTMS in healthy subjects and improve mood even in patientswith medication-resistant depression [George et al., 1995, 1997]. Much more clinical workis still required to turn rTMS into a clinical alternative to current antidepressant treatments.However, its promise is significant. An open trial reported comparable antidepressantefficacy for TMS and the most powerful of all antidepressant treatments, electroconvulsivetherapy (ECT). However, unlike ECT, rTMS does not require sedation or cause cognitiveimpairment and can be administered in an outpatient setting.At the time of this writing, commercially available magnetic stimulators are approvedby the FDA for peripheral nerve and spinal cord stimulation only, but the FDA is allowinglow-repetition-rate devices (1 Hz) to be used by investigators for human cortical stimulationwithout the need for an Investigational Device Exemption (IDE; see the Epilogue).However, the FDA believes that TMS at frequencies of 1 Hz carries significant risk andthus requires an IDE for studies involving rTMS of the human cortex.A different emerging area for the therapeutic use of repetitive magnetic stimulation is theexcitation of peripheral nerves for painless treatment of neurological and neuromusculardisorders. For example, Neotonus Inc. (Marietta, Georgia) has focused its attention on thetreatment of urinary incontinence. In June 1998, the FDA approved use of their magnetic stimulatorto enhance peripheral nerve innervation in treating urinary incontinence in women.Some groups, such as that of Loughborough University [Young et al., 2001], are pursuinga much more ambitious goal. They are working on pulsed power energized from a pairof parallel-connected 200-µF at 22 kV capacitors. The 118-µH double coil induces pulsesof 500 µs in duration and 400 V/m at 5 cm from the coil. This has the potential to activatestructures deep inside the body, such as the heart, bowel, bladder, spinal cord, and kidney.The aim of this group’s program is to be able to stimulate the kidneys to restart or enhanceperistaltic pumping to evacuate stone fragments left behind after extracorporeal shock wavelithotripsy. Threshold for peristalsis with a “low-power” (by Loughborough’s standards)4.2-kJ magnetic stimulator applied directly to the kidney during surgery was reported to bebetween 470 and 720 V/m, with an induced pulse width of 270 µs. They expect that the 500-µs pulse delivered by their 80-kJ stimulator will activate the unmyelinated nerve fibers inthe kidney from outside the body. This is certainly a new field with plenty of potential. It’seasy to see that as in many other areas of biomedical engineering, progress will be madewith magnetic stimulation as ingenious solutions tackle today’s engineering challenges.Safety in Magnetic StimulationGuidelines for safe use of magnetic stimulation have not been established conclusively. Itis obvious that magnetic stimulation should not be applied to subjects with implanted metallicor magnetic objects. The magnetic field of the stimulator attracts ferromagnetic objectsand repels nonmagnetic conductors with a force that can harm surrounding tissues. It shouldalso be obvious to practitioners of magnetic stimulation that an enormous magnetic pulsecan destroy any implanted electronic devices (e.g., pacemakers, implantable defibrillators).On the less obvious side of possible side effects, the experimenter should take into accountpossible induction of seizures by transcranial magnetic stimulation. Also, magnetic stimulatorcoils usually produce loud clicks when their windings try to expand during a pulse. The peaksound pressure is often in the range 120 to 130 dB at a distance of 10 cm from the coil. Mostsound energy is in the frequency range 2 to 7 kHz, where the human ear is the most sensitive,and this noise may exceed criteria limits for sensorineural hearing loss. For this reason, hearingprotection aids are recommended for both the experimenter and the subject.
OTHER CLINICAL APPLICATIONS <strong>OF</strong> ELECTRICAL CURRENT DELIVERY TO TISSUES 357OTHER CLINICAL APPLICATIONS <strong>OF</strong> ELECTRICALCURRENT DELIVERY TO TISSUESThere are many clinical applications for the delivery of electrical currents to the body thatdo not involve the activation of excitable tissue. Unfortunately, the marketplace is also litteredwith all sorts of “energy medicine” contraptions and procedures that claim to “balancethe flow of vital energy in the body” using currents delivered to the body. Needlessto say, the latter are all either extremely controversial or totally unproven. Some, such aselectroacupuncture, are simply old “alternative” treatments with an electrical twist. Othersare without doubt the electrical equivalents of snake oil. Let’s take a look at what is realand what is quack.Electrosurgery and RF AblationThe use of alternating currents for surgical techniques was attempted by D’Arsonval in1891. However, the technique did not become practical until 1928, when physicist WilliamT. Bovie developed an RF electrosurgical unit (ESU) for use in the operative environment.Developments in solid-state circuitry and advances in the methodology of RF signal modulationas well as inventions related to the precise control of tip temperature have enabledall sorts of interventional applications for RF-based surgical tools (Table 7.3).Depending on how RF is applied, as well as the crest factor (the ratio of peak voltageto root mean square voltage), the waveform (damped or unmodulated sinusoid), and thepower output, three different electrosurgical effects can be achieved:1. Electrosurgical cutting: electric sparking to tissue with a cutting effect2. Electrosurgical fulguration: electric sparking to tissue without significant cutting, alsoknown as noncontact coagulation or spray mode; used to control diffuse bleeding3. Electrosurgical desiccation 8 : low-power coagulation without sparking, also knownas contact coagulation mode; used to control local bleeding and enables point coagulationof tissuesThe RF current flows from a tip electrode into the tissue, producing ionic agitation inthe tissue about the electrode tip as the ions attempt to follow the changes in directionof the alternating current. This agitation drives water from the cells, leading to desiccationand coagulation (which occurs at a temperature of approximately 48°C). Further increasesin temperature due to ionic frictional heating in the tissue surrounding the electrode areresponsible for cutting and fulguration.Today, RF energy delivered via catheters to the heart is being used to treat cardiacarrhythmias. RF ablation (selective destruction) has replaced traditional surgical proceduresin the treatment of refractory supraventricular arrhythmias and ventricular tachycardia bydelivering energy to selectively destroy the accessory conduction pathways responsible forthe arrhythmia.IontophoresisIontophoresis is an accepted method of drug delivery similar to the passive transdermalmedication patches now on the market for smoking cessation and hormone therapy.However, iontophoresis uses low-level electrical current to speed up delivery of the drugions into the skin and surrounding tissues (Table 7.4). Iontophoretic drug delivery systems8Not to be confused with electrocautery, which is the coagulation of blood or tissue by means of an electricallyheated wire, where the current heats only the wire and does not pass through the patient’s body.
358 STIMULATION <strong>OF</strong> EXCITABLE TISSUESTABLE 7.3Typical Parameters Used in Various Electrosurgery and RF Ablation InstrumentsMethod of Typical Typical CurrentClinical Application Current Delivery Waveform or VoltageElectrosurgical cutting Contact electrodes with various surface Continuous-wave sine wave 300 Up to 1 kV peak to yield upareas, depending on desired coarseness to 800 kHz causes quick, clean to 350 Wof cut; either unipolar (referenced cutting effects with little or noagainst large surface-dissipative hemostasis; this pure-cutelectrode) or bipolar pair on “scalpel”; waveform causes cells to swellelectrode impedance 100 to 300 Ω and explode into steam andsmokeElectrosurgical Noncontact electrode allowed to spark Modulated 300 to 800 kHz; Up to 6 kV peak to yield upfulguration against tissue; reference electrode is coagulation occurs when the to 50 Wusually a large dissipative platecell fluid is allowed to coolbetween heating. The waveformconsists of a dampened cutwave with an ON time (heating),then an <strong>OF</strong>F time (cooling);most ESUs offer a “blend”mode that combines cut andcoagulation currentsElectrosurgical Contact electrodes with various Up to 500 V peak to yield updesiccation a surface areas, depending on to 60 Wdesired width of dessication;either unipolar (referenced againstlarge surface dissipative electrode)or bipolar pair on dessication tool;electrode impedance 100 to 500 ΩSelective ablation Electrode inserted into the heart via Sine wave 300 to 800 kHz Up to 50 Wof myocardiaca temporary catheter; electrodetissue to terminate impedance 100 to 300 Ωarrhythmic fociPerforation of soft Fine-tip electrode inserted to desired Sine wave 300 to 800 kHz Up to 25 Wtissue for the creation perforation site via a temporaryof atrial septal defects, catheter; electrode impedancetreatment of pulmonary 2 to 4 kΩatresia, hypoplastic leftheart syndrome, SVCocclusion andesophageal atresiaaHowever, not all forms of coagulation have to be performed with a “coagulation current”. Endoscopic procedures, particularly coagulation, should be performedusing non-modulated current (“cutting current”) delivered through an electrode with larger surface area so that contact coagulation can be done at alower voltage with reduced arcing.use a low-level dc current of under 4 mA to push water-soluble ionized medication throughthe skin’s outermost layer (stratum corneum), which is the main barrier to drug transport.Once the drug passes through the skin barrier, natural diffusion and circulation are requiredto shuttle the drug to its proper location.The drug delivery electrode that contains the medication is placed over the area to betreated or where the procedure is to be done. For example, the drug delivery electrode loadedwith a suitable local anesthetic (e.g., lidocaine) is placed over a vein in the bend of the elbowfor a routine blood draw or intravenous start. The other electrode, the grounding (dispersive)electrode, is placed approximately 4 to 6 in. away from the drug delivery electrode.Topical anesthetic agents are often delivered through iontophoresis prior to cut-downfor dialysis, insertion of tracheotomy tubes, and insertion of catheters. Iontophoresis has
OTHER CLINICAL APPLICATIONS <strong>OF</strong> ELECTRICAL CURRENT DELIVERY TO TISSUES 359TABLE 7.4 Typical Parameters Used in Iontophoresis InstrumentsClinical Method of Typical Typical CurrentApplication Current Delivery Waveform or VoltageDelivery of water-soluble Current delivered between drug-delivery Dc 0 to 4 mA with limitedionized medication and “dispersive” surface electrodes; 60-V compliance;through the skin typical electrode impedance at electrode current densitybeginning of treatment in themaintained underrange 20 to 100 kΩ; impedance at the 500 mA/cm 2end of treatment in the range 1 to 20 kΩDrawing glucose Current delivered between extraction Dc applied for 3 to 5 minutes, 200 µA to 1 mA to yieldthrough skin by surface electrodes then glucose is analyzed for current density ofelectroosmosis 7 to 10 minutes, followed by 0.3 mA/cm 2 at theanother extraction using dc cathodein opposite direction for3 to 5 minutesalso been investigated with some success as a way of delivering anti-inflammatory agents(dexamethasone sodium phosphate lidocaine) to treat musculoskeletal disorders,hyaluronidase to reduce edema, as well as medication for many localized skin disorders,such as nail diseases, herpes lesions (e.g., delivery of acyclovir), psoriasis, eczema, andcutaneous T-cell lymphoma.An iontophoresis dose is expressed ascharge delivered (mA/min) current (mA) treatment time (minutes)A typical iontophoretic drug delivery dose is 40 mA/min but can vary from 0 to 80 mA/min.Most people feel little or no sensation at all during an iontophoretic treatment. Some peoplefeel a tingling or warm sensation under one or both of the electrodes. This is caused bysmall blood vessels in the skin expanding due to the presence of direct current, or becausemast cells are responding to the current by releasing histamine.It has also been demonstrated that electroosmosis can be taken advantage of inreverse iontophoresis. Here, imposing an electric current across the skin extracts a substanceof interest from within or beneath the skin to the surface. Sodium and chlorideions from beneath the skin migrate toward the electrodes. Uncharged molecules, includingglucose, are also carried along with the ions by convective transport (electroosmosis).This technique is now being used to monitor the subdermal concentration variationof glucose, allowing diabetic patients to track their blood sugar without painful fingerpricks.Modulation of Cardiac ContractilityA major determinant of contractile strength of cardiac muscle cells is the amount ofcalcium reaching the contractile proteins during a beat. Reduced calcium transients arebelieved to contribute to contractile dysfunction in heart failure. Shlomo Ben-Haim, thefounder of Impulse Dynamics (Haifa, Israel), discovered that extracellularly appliedelectric fields delivered during the absolute refractory period can modulate myocardialcontractility [Ben-Haim et al., 2002] (Table 7.5). Experimental evidence in situ as wellas in vivo (healthy dogs and pigs, heart failure dogs, and heart failure human patients)indicates that electrical signals do modulate cardiac contractility [Burkhoff et al.,2001].
360 STIMULATION <strong>OF</strong> EXCITABLE TISSUESTABLE 7.5 Typical Parameters Used in Cardiac Contractility Modulation InstrumentsClinical Method of Typical Typical CurrentApplication Current Delivery Waveform or VoltageEnhancement of High-capacitance implantable Charge-balanced biphasic controlled-current 5 to 15 mA with 20-Vcardiac electrodes in contact with or capacitor-discharge pulse burst 5 to compliance or up to 8Vcontractility cardiac muscle; typical 10 ms in duration per phase; one to three from 660-µF capacitorelectrode impedancepulses per burst delivered 30 to 60 ms into200 to 500 Ω the ventricular absolute refractory periodImpule Dynamics’ implantable cardiac contractility modulation devices [Prutchi et al.,1999] are currently undergoing clinical investigations to determine their safety and effectivenessas tools in the treatment of heart failure. Inside the implantable pulse generator’stitanium can, sense amplifiers detect the heart’s electrical activity through standard pacingleads. Specialized circuitry is used to generate and deliver the cardiac contractility modulation(CCM) signals to the heart muscle during the ventricular absolute refractory period[Mika et al., 2001]. An implantable-grade battery powers the device.In principle, the same techniques can be applied to controlling other tissues that use calciumas their main signaling mechanism. In gastroenterology, for example, application ofelectric impulses is being researched by Impulse Dynamics to treat morbidly obese patient.The hope is that application of these nonexcitatory signals to these organs will alter cellularfunction in a predictable and reproducible way while avoiding the systemic side effectsof pharmacological agents.Bone Growth StimulatorsElectrical bone growth stimulators have been proven to hasten the healing process for certaintypes of fractures and bone fusions. Noninvasive, semi-invasive, and invasive methodsof electrical bone growth stimulation are available (Table 7.6). There are twononinvasive bone growth stimulation techniques. The first, pulsed electromagnetic fields(PEMF), involves the use of paired coils that are placed on either side of a fracture site.It is believed that this triggers calcification of the fibrous cartilage tissue within the fracturegap. Ten hours of treatment per day are usually necessary. Because of the relativelystrong fields that need to be generated, these units run on mains power and are notportable, which forces the patient to spend a substantial part of the day next to a wallpower outlet.The second type of noninvasive bone growth stimulator, the capacitively coupled stimulator,involves the use of skin-surface gelled electrodes through which a constant current60-Hz sine-wave signal is delivered at 5 to 10 mA to produce an electrical fieldstrength at the desired fusion site of some 2.0 V/m with a current density of approximately300 mA/cm 2 . The probable mechanism of operation of this method is throughtranslocation of calcium into the cells at the fracture site through voltage-gated calciumchannels.Semi-invasive and invasive bone growth stimulators utilize a dc source to generate aweak electrical current in the underlying tissue. Semi-invasive or percutaneous bonegrowth stimulators use an external power supply and electrodes (cathodes) that are insertedthrough the skin and into the bone segment where growth is desired, while a self-adhesivegelled anode electrode is placed directly on the skin. The electrodes are then connected toa power pack that delivers 20 µA dc and is embedded within the cast. These units are typicallydesigned to be applied for 12 weeks.
OTHER CLINICAL APPLICATIONS <strong>OF</strong> ELECTRICAL CURRENT DELIVERY TO TISSUES 361TABLE 7.6 Typical Parameters Used in Bone Growth Stimulation InstrumentsClinical Method of Typical Typical CurrentApplication Current Delivery Waveform or VoltageAccelerate bone Noninvasive capacitive coupling: Ac constant-current, 60-Hz 5 to 10 mA to producefracture healing ac signal delivered between gelled sine-wave signal electrical field strength ator bone fusion skin surface electrodes the desired fusion site of2.0 V/m with a currentdensity of 300 µA/cm 2Noninvasive electromagnetic: Inductively coupled field 15-Hz Maximum magnetic fieldac magnetic field applied through burst, 20 pulses per burst, amplitude at the fusioncoils over desired bone fusion site and a pulse frequency of 4.3 kHz site 25 G to induce anelectrical field of 0.2 V/mSemi-invasive: cathode electrode is Dc 20 µAimplanted within the fragments ofbone graft at the fusion site; anodeis a skin surface electrodeFully implanted: cathode electrode Dc 20 µAis implanted within the fragmentsof bone graft at the fusion site;anode is the enclosure of theimplanted dc power sourceInvasive bone growth stimulators require surgical implantation of a current generator ina subcutaneous pocket. A cathode electrode is implanted within the fragments of bonegraft at the fusion site. The generator is often no more than a battery and a 20 µA constantcurrentdiode to the cathode electrode via a silicone-coated lead. The device’s metallicenclosure acts as the anode electrode. The implant delivers dc continuously for six to ninemonths and is then removed by a simple procedure and is done most often under localanesthesia.The precise mechanism of how dc speeds bone healing is not clearly understood.However, it is believed that the localized increase in pH and lowered oxygen tension at thecathode favor the activity of bone-forming cells and inhibit bone-absorbing cells. Bonegrowth takes place with a current between 5 and 20 µA. Currents below 5 µA do notenhance growth, and levels above 20 µA cause cell necrosis and bone death.Electrical Stimulation for the Treatment of Chronic WoundsElectrical stimulation has been studied as a possible therapy for accelerating wound healing(Table 7.7). In vitro as well as in vivo animal studies have shown that externallyapplied electrical currents can increase ATP concentrations in tissues, increase DNAsynthesis, promote healing of soft tissue or ulcers, cause epithelial and fibroblasts tomigrate into wound sites, accelerate the recovery of damaged neural tissue, reduce edema,and inhibit the growth of some pathogens.Research has been done to evaluate the effectiveness of dc, pulsed, and ac currents inpromoting the healing of wounds. However, a technology assessment study conducted bythe Emergency Care Research Institute (ECRI) [1996] concluded that whereas electricalstimulation does facilitate the complete healing of chronic ulcers compared to the use ofplain dressings, it is no better than conventional wound care involving debridement, cleaningagents, antibiotics (systemic or local), and bandages.
362 STIMULATION <strong>OF</strong> EXCITABLE TISSUESTABLE 7.7Typical Parameters Used in Chronic Wound Treatment Instruments aClinical Method of Typical Typical CurrentApplication Current Delivery Waveform or VoltagePromoting healing Cathode wrapped in saturated (saline) Dc applied two or three times per 20 to 100 µA with aof wounds and gauze and placed directly over day for 2 hours at a time compliance of 8Vskin ulcers the wound site, gelled skin surface Low-voltage monophasic current 30 to 40 mA with up toanode placed near the wound pulses, 50% duty cycle delivered 12-V complianceat up to 150 HzHigh-voltage monophasic pulses, 100 to 250 V50% duty cycle delivered at upto 150 HzBiphasic 40-Hz square-wave current 15 to 25 mA with 100-VcomplianceTENS device generating charge-balanced 10 to 50 mA “stimulation”current-controlled pulses, 0.1 to 0.2 ms phase with 150-Vduration at 80 to 90 HzcomplianceAc magnetic field applied through Inductively coupled field 10 to 150 Hz Maximum magnetic fieldcoils over wound dressings burst, 10 to 100 pulses per burst and amplitude at the wounda pulse frequency of 2 to 10 kHz site 50 G to induce anelectrical field of 0.1 to0.5 V/mNonthermal high-frequency RF 60 to 100 µs of high-peak-power RF Peak pulse power of 200 Wapplied with small capacitive bursts of 27 MHz, repeated at to 1 kW“antenna” over wound80 to 600 HzdressingsaIt should be noted that in 1996 the ECRI found no evidence that dc stimulation improves the healing rate of chronic, decubitus, or diabetic ulcers. All otherforms of stimulation seem to improve the normalized healing rate of decubitus ulcers but not of chronic venous or diabetic ulcers.Electrochemotherapy or Electroporation TherapyBrief, intense electric pulses have been in use since the 1970s to create temporary pores incells without causing permanent damage. This process, known as electroporation, happenswhen the electrical pulse causes a transmembrane potential of 0.5 to 1.5 V. Under this fieldintensity, the lipid bilayer of cells is temporarily rearranged, forming aqueous channels inthe cell membrane. These “pores” make the cell membrane permeable to a large variety ofhydrophilic molecules that are otherwise unable to enter into the cell. Once formed, thesepores remain open for a duration of seconds to minutes.Genetronics, Inc. (San Diego, California) introduced the use of electroporation for invivo delivery of high doses of chemotherapeutic drugs to cancerous tumors [Hofmannet al., 1996] (Table 7.8). Electroporation therapy (EPT) makes it possible to introduce intocells potent anticancer drugs such as bleomycin, which normally cannot penetrate themembranes of certain cancer cells. Treatment is carried out by injecting bleomycin directlyinto the tumor and applying electroporation pulses through an array of needle electrodes.The field strength must be adjusted reasonably accurately so that electroporation of thecells of the tumor occurs without damage, or at least minimal damage, to any normal orhealthy cells. Treatment with this therapy avoids the toxic effects associated with the systemicadministration of anticancer agents, making it possible to kill selectively the cancerouscells while avoiding surrounding healthy tissue. As such, a patient should require amuch lower dose of chemotherapy than is usually necessary to kill the tumor, drasticallyreducing nasty side effects such as hair loss, nausea, and vomiting that are associated withconventional chemotherapy.
OTHER CLINICAL APPLICATIONS <strong>OF</strong> ELECTRICAL CURRENT DELIVERY TO TISSUES 363TABLE 7.8 Typical Parameters Used in Electrochemotherapy (Electroporation) InstrumentsClinical Method of Typical Typical CurrentApplication Current Delivery Waveform or VoltageDeliver high doses of Genetronics: six needle electrodes Genetronics: voltage pulses, 100 µs Maximum pulse amplitudechemotherapeutic in a circle in contact with tumor in duration, delivered at a frequency of 3 kV to yield fielddrugs to cancerous driven in opposing pairs at any of 1 to 100 Hz intensity of 600 totumors one time 1200 V/cmDaskalov et al. [1999]: pair of Daskalov et al. [1999]: burst of eight Maximum pulse amplitudestainless-steel wires 0.8 mm in biphasic voltage pulses of 50 µs of 1.25 kV to yield fielddiameter and 14 mm in length duration per phase at a frequency intensity of 330 tospaced 5 to 30 mm of 1 kHz 1250 V/cmElectroporation therapy can be delivered to external tumors by placing electrodes onopposite sides of a tumor so that the electric field is between the electrodes. However,when large or internal tumors are to be treated, it is not easy to locate electrodes properlyand measure the distance between them. For this type of tumors, needles are the preferredtype of electrodes. Since the use of only two needles creates an inhomogeneous field,Genetronics uses an array of six needles to optimize the uniformity of the pore formationaround the cell [Hofmann, 2001]. Genetronics drives the needle electrodes in opposingpairs because the resulting field is more homogeneous than that between opposing singleneedles. After each electroporation pulse the polarity of the needles is reversed immediatelyand the needle pair is pulsed again. After each of these paired pulsings, the sequencefor the next electric field is rotated 60 degrees. A fairly uniform distribution, which maximizespore formation in the cells over a circular section of the tissue, is generated by rotatingthe field three times.Electrochemical TherapyElectrochemical therapy (EChT), also known as electrochemical tumor therapy or cancergalvanotherapy consists of placing a platinum wire anode electrode into a tumor and anumber of similar cathode electrodes in the tumor’s periphery. 100 mA dc is passedbetween the electrodes until the delivered charge reaches some 50 to 100 C/mL of tumor(Table 7.9). The flow of direct current through tumor tissue triggers electrolytic processesat the electrodes. Positively charged ions (e.g., H ,Na ) migrate to the cathode, resultingin the formation of an extremely alkaline environment (pH 12.9). At the same time, negativelycharged ions (e.g., Cl ) migrate to the anode, creating an extremely acidic environment(pH 2.1). These local pH levels are well outside the physiologic range and havea destructive effect on tissue.The hypothesis is that the cancerous tissue is more sensitive to than normal tissueextreme pH levels and is thus selectively killed. It is also thought that the change in ionconcentrations permanently depolarizes cancer cell membranes, causing their furtherdestruction. Last, proponents of the technique suggest that the EChT process may alsogenerate heat shock proteins around the cancer cells, inducing the body’s own killer cellsto better target the tumor.The technique has reportedly been applied with success, mostly in China and Japan, forthe treatment of lung, breast, and bladder cancers. The technique has been used primarilyin conjunction with systemic or topical chemotherapy agents (e.g., adriamycin), whichbecause of their polar nature may be attracted by the electrodes and concentrate at thetumor site. Yuling [2000] reviewed the experience at 108 hospitals of treating 7642 patientsof malignant tumors with EChT between 1978 and 1998. Yuling reported complete remissionin 33.2% of the cases and partial remission in 42.8% of the cases, concluding that the
364 STIMULATION <strong>OF</strong> EXCITABLE TISSUESTABLE 7.9 Typical Parameters Used in Electrochemical Therapy InstrumentsClinical Method of Typical Typical CurrentApplication Current Delivery Waveform or VoltageElectrochemical Two or more platinum needle Dc 5 to 100 mA with a voltagedestruction of electrodes positioned under local compliance of up to 20 Vtumors anesthesia in or at the site of the to deliver a total charge oftumor with an interelectrodedistance of 3 cmapproximately 30 to100 C/mL of tumorvolumeAttract lymphocytes 12-µm-diameter IROX-coated wire Charge-balanced biphasic current 20 µA to yield 500 toto solid tumors or electrodes in the tumor or pulses 400 µs in duration delivered 2000 µC/cm 2infections infection and large platinum at 200 Hz for 10 minutes toreference electrode at remote site 8 hours per sessiontechnique was effective in 76% of cases. The effectiveness rate reported for superficialtumors only was 80.2%. However, because most of the trials were conducted at centers thatare not bound by the strict research methodologies prescribed by the FDA to prove safetyand effectiveness, we must consider these results to be mere anecdotal evidence that EChTmay become a useful tool in the fight against cancer.Unfortunately, EChT is not being given the attention that it deserves to rigorously proveor disprove its clinical efficacy. The problem is that the pioneer of the technique, Swedishphysician Björn E. W. Nordenström, believes that the body has a second circulatory systemof continuous energy circulation that he calls a biologically closed electrical circuit(BCEC). He believes that these currents participate in maintaining homeostasis and in controllingthe healing process in living organisms, and presents EChT as a direct applicationof his BCEC concepts. This not only attracts the attention of a lot of quacks, but also makesthe principle of EChT unpalatable to most mainstream oncologists.In a somewhat related application, U.S. patent 6,038,478 to Yuen et al. [2000] describesthe use of low-current biphasic pulses to attract lymphocytes to sites that can be accessedthrough surgery to place an array of electrodes. The technique is said to be useful in thetreatment of solid tumors or in the treatment of certain infections, especially in poorly vascularized(e.g., brain) or inaccessible areas where surgical intervention is unadvised andelectrode placement is feasible and less destructive.Induction of Apoptosis via Nanosecond Pulsed Electric FieldsApoptosis is the process by which a cell actively commits suicide, which is essential formaintaining tissue homeostasis. Cancer is believed to result from the failure to regulateapoptosis properly. High-intensity (300 kV/cm), nanosecond (10 to 300 ns) pulsed electricfields (nsPEFs) are now being investigated as a tool to trigger apoptosis in cancerous tissue(Table 7.10). The hypothesized working principle behind nsPEF is cytochrome crelease into the cytoplasm, suggesting that nsPEF targets the mitochondria, which are theinitiators of apoptosis. This technique, pioneered by researchers at Old DominionUniversity in Norfolk, Virginia [Schoenbach et al., 2001], is still in its infancy, and its clinicalefficacy, if any, is yet to be demonstrated.Embolic TherapyThe traditional treatment for a ruptured intracranial aneurysm to prevent rebleeding isthrough microsurgery. The method comprises a step of clipping the neck of the aneurysm,
OTHER CLINICAL APPLICATIONS <strong>OF</strong> ELECTRICAL CURRENT DELIVERY TO TISSUES 365TABLE 7.10 Typical Parameters Used in Nanosecond Pulse Field Therapy InstrumentsClinical Method of Typical Typical CurrentApplication Current Delivery Waveform or VoltageInduction of apoptosis RF applicator in contact 1 to 10 narrow high-voltage Sufficient to yield fieldvia nanosecond pulsed with tumor? nanosecond-rise-time pulses, intensities of 50 toelectric fields (nsPEFs) 10 to 300 ns in duration 300 kV/cmTABLE 7.11 Typical Parameters Used in Embolic Therapy InstrumentsClinical Method of Typical Typical CurrentApplication Current Delivery Waveform or VoltageDetachment of embolic device Between guide wire (anode) and Dc delivered until embolic 0.1 to 1 mA with complianceand initiation of platelet and gelled surface electrode (cathode); device separates from of 10 VRBC aggregation typical impedance 1 to 4 kΩ guide wireperforming a suture ligation of the neck, or wrapping the entire aneurysm. General anesthesia,craniotomy, brain retraction, and placement of a clip around the neck of theaneurysm are required in these surgical procedures. The surgical procedure is oftendelayed while waiting for the patient to stabilize, leading to the death of many patientsfrom the underlying disease or defect prior to surgery.A minimally invasive alternative to surgery involves reaching the interior of theaneurysm through a catheter introduced through a remote artery. Once the catheter is positioned,a long platinum microcoil that is fused to a guide wire is fed into the aneurism.Detachment of the coil from the guide wire is then achieved by the passage of low-voltagedc through the guide wire to hydrolyze a sacrificial link between the guide wire and coil(Table 7.11). The current along the coil also initiates platelet and RBC aggregation, promotingthrombosis. Within a short period of time after the filling of the aneurysm with theembolic coil, a thrombus forms in the aneurysm and is shortly thereafter complementedwith a collagenous material that significantly lessens the potential for aneurysm rupture.Microcurrent Stimulation and Other Energy TherapiesMicrocurrent stimulators have been around since the 1960s. Proponents of the techniquebelieve that delivering charge-balanced square waves of some 10 to 600 µA at frequenciesbetween 0.5 and 100 Hz across the head “normalizes the activity of the nervous system”and is thus claimed to treat depression, anxiety, and insomnia. In 1976, when Congresschartered the FDA with enforcing the Federal Food, Drug, and Cosmetic (FD&C) Act,these devices were classified as cranial electrotherapy stimulation and their commercialapproval was obtained through a grandfather provision of the FD&C Act. This is why thesedevices, although far from being proven effective by today’s standards, are promoted bytheir manufacturers as “FDA Approved.”The alleged mechanism of operation of these devices certainly groups them along withthe quackery promoted by homeopaths and chiropractors. Just look at what ElectromedicalProducts International, probably the largest microcurrent stimulator manufacturer, claimsabout their devices: [The Alpha-Stim devices are] “based on the concept that the biophysicsunderlying the body’s biochemistry also plays a significant role in regulating all of life’sprocesses. . . . Alpha-Stim’s proprietary waveform works by moving electrons through thebody and brain at a variety of frequencies, collectively known as harmonic resonance. Thisnormalizes the electrical activity of the nervous system and brain as measured by an electroencephalogram(EEG).” Controlled studies reported in reputable journals [Tan et al.,
366 STIMULATION <strong>OF</strong> EXCITABLE TISSUES2000] found that microcurrent stimulators do no better than placebo in treating depression,anxiety, and insomnia. When confronted, microcurrent stimulator manufacturers quicklytell you all about conspiracies against them and cite their own studies [Kirsch, 1999]. Thedebate for their effectiveness continues. We remain among the skeptics.All other forms of energy therapy are either untested or unverified. Electroacupunctureand auricular acupuncture (acupuncture limited to the ear) claim to deliver currents tovarious “acupuncture points” to relieve pain and cure disease by correcting “imbalances”in the flow of “life energy.” MORA units purportedly select, amplify, and reintroduce intothe body the patient’s own “good electromagnetic oscillations” filtering out the “pathologicaloscillations.” Other unproven contraptions (e.g., Bioresonance, Rife, Zapper, andRadionic devices) claim to use sound and radio waves supposedly “tuned to the resonantfrequency” of various pathogens to kill cancer cells, viruses, bacteria, and fungi. Again,we are skeptics.REFERENCESAnderson, D. J., K. Najafi, S. J. Tanghe, D. A. Evans, K. L. Levy, J. F. Hetke, X. Xue, J. J. Zappia,and K. D. Wise, Batch-Fabricated Thin-Film Electrodes for Stimulation of the Central AuditorySystem, IEEE Transactions on Biomedical Engineering, 36, 693–704, 1989.Bak, M., J. P. Girvin, F. T. Hambrecht, C. V. Kufts, G. E. Loeb, and E. M. Schmidt, Visual SensationsProduced by Intracortical Microstimulation of the Human Occipital Cortex, Medical andBiological Engineering, 257–259, 1990.Ben-Haim, S., N. Darvish, M. Fenster, and Y. Mika, Electrical Muscle Controller, U.S. patent6,363,279, 2002.Bickford, R. G., and B. D. Fremming, Neural Stimulation by Pulsed Magnetic Fields in Animals andMan, Digest of the 6th International Conference on Medical Electronics and BiologicalEngineering (Tokyo), Abstract 7-6, 1965.Brighton, C. T., W. Wang, R. Seldes, G. Zhang, and S. R. Pollack, Signal Transduction in ElectricallyStimulated Bone Cells, Journal of Bone and Joint Surgery, 83-A, 1514–1523, 2001.Burkhoff, D., I. Shemer, B. Felzen, J. Shimizu, Y. Mika, M. Dickstein, D. Prutchi, N. Darvish, andS. Ben-Haim, Electric Currents Applied during the Refractory Period Can Modulate CardiacContractility In Vitro and In Vivo, Heart Failure Review, 6(1), 27–34, 2001.Daskalov, I., N. Mudrov, and E. Peycheva, Exploring New Instrumentation Parameters for Electrochemotherapy,IEEE Engineering in Medicine and Biology, 62–66, January–February 1999.Emergency Care Research Institute (ECRI), Health Technology Assessment Information Service,Electrical Stimulation for the Treatment of Chronic Wounds, 1996.George, M. S., E. M. Wassermann, W. A. Williams, A. Callahan, T. A. Ketter, and P. Basser, DailyRepetitive Transcranial Magnetic Stimulation (rTMS) Improves Mood in Depression,Neuroreport, 6, 1853–1856, 1995.George, M. S., E. M. Wassermann, W. A. Williams, J. Steppel, A. Pascual-Leone, and P. Basser,Changes in Mood and Hormone Levels after Rapid-Rate Transcranial Magnetic Stimulation(rTMS) of the Prefrontal Cortex, Journal of Neuropsychiatry and Clinical Neuroscience, 8,172–180, 1996.George, M. S., E. Wassermann, T. Kimbrell, J. Little, W. Williams, and A. Danielson, MoodImprovement Following Daily Left Prefrontal Repetitive Transcranial Magnetic Stimulation inPatients with Depression: A Placebo-Controlled Crossover Trial, American Journal of Psychiatry,154, 1752–1756, 1997.Hambrecht, F. T., Visual Prostheses Based on Direct Interfaces to the Visual System, Bullieres’sClinical Neurology, 4, 147–165, 1995.Hochmair, E. S., An Implantable Current Source for Electrical Nerve Stimulation, IEEE Transactionson Biomedical Engineering, 27, 278–280, 1980.
Hodgkin, A. L., and A. F. Huxley, A Quantative Description of Membrane Current and Its Applicationto Conduction and Excitation in Nerve, Journal of Physiology, 117, 500–544, 1952.Hofmann, G. A., S. B. Dev, and G. S. Nanda, Electrochemotherapy: Transition from Laboratory tothe Clinic, IEEE Engineering in Medicine and Biology, 124–132, November–December 1996.Hofmann, G. A., Apparatus for Electroporation Mediated Delivery of Drugs and Genes, U.S. patent6,241,701, 2001.Kirsch, D. L., The Science behind Cranial Electrotherapy Stimulation, Medical Scope Publishing,Edmonton, Alberta, Canada, 1999.Konrad, M., H. Freller, and H. Friedrich, Electrode for Medical Applications, U.S. patent 4,603,704,1984.Kralj, A. R., and T. Bajd, Functional Electrical Stimulation: Standing and Walking after Spinal CordInjury, CRC Press, Boca Raton, FL, 1989.Lapicque, L., Définition Expérimentale de l’Excitabilité, Comptes Rendus de l’Academic desSciences, 67, 280–283, 1909.Livnat, A., R. P. Johnson, and J. E. Zehr, Programmable Miniature Backpack Stimulator for ChronicBiomedical Studies, IEEE Transactions on Biomedical Engineering, 28, 359–362, 1981.Loeb, G. E., Neural Prosthetic Interfaces with the Nervous System, Trends in Neurosciences, 12,195–201, 1989.Merton, P. A., and H. B. Morton, Stimulation of the Cerebral Cortex in the Intact Human Subject,Nature, 285, 227, 1980.Mika, Y., D. Prutchi, and Z. Belsky, Apparatus and Method for Timing the Delivery of Non-excitatoryETC Signals to a Heart, U.S. patent 6,263,242, 2001.Mouchawar, G. A., J. A. Nyenhuis, J. D. Bourland, and L. A. Geddes, Guidelines for Energy-Efficient Coils: Coils Designed for Magnetic Stimulation of the Heart, Magnetic Motor Stimulation:Basic Principles and Clinical Experience (EEG Supplement), 43, 255–267, 1991.Pascual-Leone, A., M. D. Catala, and P. A. Pascual-Leone, Lateralized Effect of Rapid-RateTranscranial Magnetic Stimulation of the Prefrontal Cortex on Mood, Neurology, 46, 499–502,1996.Polson, M. J. R., A. T. Barker, and I. L. Freeston, Stimulation of Nerve Trunks with Time-VaryingMagnetic Fields, Medical and Biological Engineering and Computing, 20, 243–244, 1982.Prutchi, D., Y. Mika, Y. Snir, J. Ben-Arie, N. Darvish, Y. Kimchy, and S. Ben-Haim, An ImplantableDevice to Enhance Cardiac Contractility through Non-excitatory Signals, Circulation, 100(Supplement 1), 1, 122, 1999.Robblee, L. S., Iridium Oxide Coated Electrodes for Neural Stimulation, U.S. patent 4,677,989,1987.Ruohonen, J., Transcranial Magnetic Stimulation: Modelling and New Techniques, Ph.D. dissertation,Helsinki University of Technology, Espoo, Finland, 1998.Robblee, L. S., M. M. Mangaudis, E. D. Lasinsky, A. G. Kimball, and S. B. Brummer, ChargeInjection Properties of Thermally-Prepared Iridium Oxide Films, Materials Research SocietySymposium Proceedings, 55, 303–310, 1986.Schoenbach, K. H., S. J. Beebe, and E. S. Buescher, Intracellular Effect of Ultrashort ElectricalPulses, Bioelectromagnetics, 22, 440–448, 2001.Sebille, A., P. Fontagnes, J. Legagneus, J. C. Mira, and M. Pecot-Dechavassine, Portable Stimulatorfor Direct Electrical Stimulation of Denervated Muscles in Laboratory Animals, Journal ofBiomedical Engineering, 10, 371–372, 1988.Tan, G., T. Monga, and J. Thornby, Efficacy of Microcurrent Electrical Stimulation on Pain Severity,Psychological Distress, and Disability, American Journal of Pain Management, 10, 35–44, 2000.Van den Honert, C., Multichannel Electrical Stimulator with Improved Channel Isolation, U.S.patent 4,856,525, 1989.Woodford, B. J., R. R. Carter, D. McCreery, L. A. Bullara, and W. F. Agnew, Histopathologic andPhysiologic Effects of Chronic Implantation of Microelectrodes in Sacral Spinal Cord in the Cat,Journal of Neuropathology and Experimental Neurology, 55, 982–991, 1996.REFERENCES 367
368 STIMULATION <strong>OF</strong> EXCITABLE TISSUESWoodward, W. S., Optically Isolated Precision Bipolar Current Source, Electronic Design, 130–132,April 20, 1998.Young, A. J., B. M. Novac, I. R. Smith, B. Lynn, and R. A. Miller, Two-Dimensional Modelling ofa Double-Spiral Coil System for High Electric Field Generation for Biological Applications, IEESymposium on Pulsed Power 2001, London, 19/1–19/4, 2001.Yuen, T. G. H., W. F. Agnew, D. B. McCreery, L. A. Bullara, and M. Ingram, Lymphocyte Attractionby Electrical Stimulation, U.S. patent 6,038,478, 2000.Yuling, X., Clinical Results of 7642 Cases of Malignant Tumors Treated with ElectrochemicalTherapy (ECT), Abstracts of HIGH CARE 2000, Audimax Ruhr-University, Bochum, Germany,February 2000.
8CARDIAC PACING <strong>AND</strong> DEFIBRILLATIONWITH CONTRIBUTIONS BY FERN<strong>AND</strong>O BRUM, JULIO ARZUAGA,PEDRO ARZUAGA, <strong>AND</strong> OSCAR SANZThe heart is a pump that normally beats approximately 72 times every minute. This addsup to an impressive 38 million beats every year. The walls of the heart are made of muscletissue. When they contract, the blood is ejected from the heart into the arteries of thebody. As shown in Figure 8.1, the heart has four chambers, two on the left side and two onthe right side. Each side is divided further into a receiving chamber (atrium) and a pumpingchamber (ventricle). The atria and ventricles are separated by one-way valves that keepthe blood flowing in the proper direction. The right side of the heart pumps blood to thelungs (via the pulmonary artery) and the left side of the heart pumps blood to the rest ofthe organs (via the aorta). The amount of blood the left ventricle pumps into the aorta everyminute, known as cardiac output, is expressed in liters per minute. If cardiac outputdecreases in a significant manner, the body’s organs are starved for oxygen. In the case ofthe brain, a very low cardiac output can cause lightheadedness, weakness, loss of consciousnessand even death.The heart contains two specialized types of cardiac muscle cells. The majority (around99%) are contractile cells responsible for the mechanical work of pumping the heart. Thesecond type of cardiac cells are the autorhythmic cells. Their function is to initiate andconduct action potentials that are responsible for the contraction of the working cells.Autorhythmic cells have pacemaker activity as opposed to a nerve or skeletal muscle cellwhich maintains a constant membrane potential until stimulated. Cells that display pacemakeractivity have membranes that slowly depolarize between action potentials untilthreshold is reached, at which time the cell undergoes active depolarization, initiating anaction potential. These action potentials, generated by the autorhythmic cardiac musclecells, will then spread throughout the heart, triggering rhythmic beating without any nervousstimulation.The coordinated contraction of the various chambers of the heart is mediated throughan organized electrical conduction system within the heart. Disturbances within the electricalconduction system are the cause of all arrhythmias (rhythm disturbances). The electricalsignal that initiates each normal heartbeat arises from a small structure located at thetop of the right atrium called the sinus node or sinoatrial node. In a normal heart, the sinusDesign and Development of Medical Electronic Instrumentation By David Prutchi and Michael NorrisISBN 0-471-67623-3 Copyright © 2005 John Wiley & Sons, Inc.369
370 CARDIAC PACING <strong>AND</strong> DEFIBRILLATIONSinoatrial(SA) NodeAortaLeftAtriumLeft BundleBranchRightAtriumLeftVentricleRightVentriclePurkinje FiberAtrioventricular(AV)NodeRight BundleBranchFigure 8.1 The human heart has four chambers, two on the left side and two on the right side. Each side is further divided into a receivingchamber (atrium) and a pumping chamber (ventricle). One-way valves separate the atria from the ventricles. The right side of the heartpumps blood to the lungs (via the pulmonary artery), and the left side pumps blood to the rest of the organs (via the aorta).node acts as a natural pacemaker, setting the rate at which the heart beats. At rest, the sinusnode fires 60 to 80 times per minute. When metabolic demand increases, for example dueto physical activity or emotional stress, the sinus node accelerates to make the heart beatfaster and increase cardiac output.The depolarization of the sinus node creates a depolarization wave that spreads rapidlyacross the right atrium and the left atrium, causing them to contract. The atria are insulatedelectrically from the ventricles by the atrioventricular (AV) groove that runs around theoutside of the heart. Electrical activity from the atria is transferred to the ventricles via asecond electrical structure of the heart called the atrioventricular node or AV node, locateddeep in the center of the heart. The AV node is connected to the bundle of His, a bundle ofspecialized cells in the heart that can rapidly conduct the electrical signal to the musclecells of the ventricles. The bundle of His branches downstream into a right bundle branch(to the right ventricle) and a left bundle branch (to the left ventricle). The fibers eventuallybranch out to the distant ventricular tissues and are at that point referred to as Purkinjefibers.When the complete conduction system works properly, the atria contract about 200 to300 ms ahead of ventricular contraction. This allows extra filling of the ventricles beforethey pump the blood through the lungs and peripheral circulation. Another important functionof this system is that it allows all portions of the ventricles to contract almost simultaneously,which is essential for effective pressure generation in the ventricular chambers.As such, the heart must maintain a more or less steady rhythm in order to pump properly.Excessively slow heart rhythms make the cardiac output insufficient, causing symptoms offatigue, weakness, lightheadedness, and loss of consciousness. On the other hand, if theheart beats too quickly, it does not get enough time in between beats to fill up with blood.
BRADYARRHYTHMIAS 371As a result, only a small amount of blood gets ejected with each beat, and cardiac outputdrops significantly.Arrhythmias result from disturbances to the normal pacing and/or conduction systems ofthe heart. Sometimes the signal gets blocked along the way and the heart or a portion thereofdoes not beat when it is supposed to since the cells do not receive a stimulus to contract. Thiscan cause slow heart rhythms, also known as bradycardia (from the Greek brady slow cardia heart). Sometimes the electrophysiological parallel of a short circuit is formed,causing the depolarization wave to take an abnormal route or to get stuck in a reentrant circularpathway. This can cause the heart to beat rapidly, in a condition known as tachycardia(from the Greek, tachy fast). Sometimes, a stimulus signal will arise from somewhere inthe heart besides the sinus node and cause the heart to contract prematurely in what is knownas a premature atrial contraction (PAC) or a premature ventricular contraction (PVC).BRADYARRHYTHMIASThe first obvious reason for bradycardia is that the natural pacing signal is generated bythe sinus node at a low rate. Sinus bradycardia happens when the sinus node fires at lessthan 60 times per minute. However, sinus bradycardia is not necessarily abnormal. Healthypeople often have heart rates below 60 beats/minute during rest or sleep. Athletes will usuallyhave rates below 60 beats/minute at even moderate levels of activity because theirtraining has made their hearts become very efficient at pumping. Sinus bradycardia is oftenseen in the elderly as a result of medications taken for high blood pressure, angina, ortachycardia. If there are no symptoms due to a sinus bradycardia, nothing needs to be doneabout it. However, a medical condition by the name of sick sinus syndrome arises whensinus bradycardia is associated with severe symptoms.Sometimes the sinus node stops firing temporarily, and long pauses in the heart rhythmmay result. This condition may occur because of aging, ischemia, neurological imbalances,and certain drugs. It causes symptoms of fatigue, lightheadedness, shortness of breath, andsyncope. Sick sinus syndrome is usually treated with a permanent pacemaker which suppliesa weak electrical signal to the atria that replaces the stimulus generated by the cyclicdepolarizations of the sinus node.Another common condition that causes bradycardia is the AV node failing to conductatrial signals properly to the ventricles. This condition is known as AV block or heart block.The severity of AV block varies from mild to life-threatening:•A first-degree AV block is an excessive delay (greater than 0.2 s) in the conduction ofthe depolarization signal from the atria to the ventricles, but all the action potentialsare conducted. This benign condition is usually caused by disease in the AV node orby certain cardiac medications (Ca -channel blockers and β-blockers). No treatmentis usually required at this stage.• In second-degree AV block, some of the atrial signals fail to pass through the AVnode. Depending on how often atrial impulses are blocked, second-degree AV blockcan cause symptoms that require a pacemaker implant.• In third-degree AV block none of the atrial impulses can get through the AV nodebecause of severe disease in cardiac conduction system. Under these conditions, ventricularcontractions are initiated by autorhythmical (pacemaker) cells, whose pacemakerbehavior is usually inhibited by the higher rate of the SA node, as shown in Table 8.1.• Complete AV block usually results in severe bradycardia, and occasionally, the ventriclescan stop beating, resulting in severe symptoms that may lead to death. The veryfirst pacemakers were designed to treat patients with complete heart block.
372 CARDIAC PACING <strong>AND</strong> DEFIBRILLATIONTABLE 8.1 The Function of Autorhythmic (Pacemaker)Cells Is to Initiate and Conduct Action Potentials That AreResponsible for the Contraction of the Heart Muscle Cells aTissueAction Potentialsper MinuteSA node 60–80AV node 40–60Bundle of His 20–40Purkinje fibers 20–40aSince the sinoatrial node is capable of depolarizing at the highest rate,its activity usually controls the rate of the entire heart.THE FIRST PACEMAKERSIn 1932, Alfred S. Hyman developed the first device used in the United States to stimulatethe heart electronically. He called his creation an artificial pacemaker. His invention wasused to resuscitate people who had suffered from shock or hypothermia by utilizing briefelectrical currents. The Hyman device used mechanical induction of current to deliverstimuli of approximately 3 mA directly to the heart via a needle electrode at rates of 30, 60or 120 impulses per minute. His device had to be rewound every 6 minutes. In 1952, PaulZoll developed the first temporary external pacemaker. His device was large and limitedthe patient’s mobility to areas where it could be wheeled and plugged to an electrical outlet.Electric shocks were coupled to the heart through electrodes placed on the skin, oftencausing pain and skin burns. Later, Earl Bakken modified the circuit of a transistorizedmetronome that he found in a back issue of Popular Electronics to operate as a portablepacemaker.It was not until 1958, after low-leakage transistors became available, that an implantablepacemaker was constructed for human use. On October 8, 1958, Swedish physician ÅkeSenning implanted the first pacemaker in a human patient. Arne Larsson became the firstrecipient of the device developed by Rune Elmqvist of Elema-Schönander. The pacemakerwas a hockey-puck-sized device that comprised a handful of electronic components, includingtwo silicon transistors and a nickel–cadmium battery encapsulated in epoxy resin. Thepulse generator delivered pulses of approximately 2 V in amplitude and 2 ms in duration.Batteries were charged noninvasively by RF induction of energy from a line-connectedvacuum-tube radio-frequency generator driving a coil at 150 kHz. The first unit worked foronly a few hours before it failed. On the next morning, a second unit was implanted andlasted for approximately six weeks.The first successful long-term human implant of a pacemaker was achieved in Uruguayon February 2, 1960 by Orestes Fiandra and Roberto Rubio. The pacemaker was manufacturedby Elmqvist and was implanted in Uruguay in a 34-year-old patient with AVblock. Battery charging was done through the same RF link as that used in the first implant.One charging session, which was done overnight, was enough to power the pacemaker forabout a month. This unit worked successfully for nine and a half months, until the patientdied of sepsis from an infection. Other successful implants of the Swedish pacemakerfollowed in London. Soon after, William Chardack conducted the first human implant ofa pacemaker in the United States. The device powered by 10 mercury–zinc cells wasdesigned by Wilson Greatbatch.In 1969, Fiandra began the Centro de Construcción de Cardioestimuladores del Uruguay(CCC) with the purpose of producing pacemakers for use in Latin America at prices wellunder those of U.S. devices. During the 1970s and 1980s CCC assembled pacemakers
THE FIRST PACEMAKERS 373designed in the United States by Cordis. In the early 1990s, however, CCC formed an inhousedesign team. Today, CCC offers highly reliable pacemakers to markets that cannotafford the prices of devices manufactured in the United States or Europe.In addition, CCC caters its design and manufacturing capabilities to companies interestedin developing medical devices. Their field of expertise is in the design, prototyping, and manufactureof low-power circuitry for implantable and other critical-use medical devices.In the sections that follow we describe the basic logic and circuitry of pacemakers.These were kindly contributed by CCC’s engineering team: Fernando Brum designed thesoftware architecture, hardware was developed by Pedro Arzuaga and Julio Arzuaga, andOscar Sanz was responsible for the firmware.Pacemaker State MachinesThe first pacemakers were simple devices that generated a pacing pulse at a constant interval.Figure 8.2 shows a finite-state machine that represents the operation of such a pacemaker.This state machine has a single state [S]; [Time Out] is the event that causes thestate machine to evolve; and [Pace] is the action that occurs as the state transition occurs.An arrowed line indicates the direction of a state transition and separates the event fromactions taken during the transition.In a simple pacemaker, the implementation of such state machine would consist of atimer with a fixed period. Every time that a length of time [Time Out] elapses, the statemachine exits state [S], generates a pacing pulse (as described by the action [Pace]), andreturns to state [S]. In early pacemakers, the timer’s period, as well as the pacing pulsecharacteristics (amplitude, waveshape, and duration) were solely a function of the circuit.Take for example the circuit of Figure 8.3, which has been set up for PSpice simulation.The circuit is a replica of a 1960s design by Wilson Greatbatch. The story goes that around1956, Greatbatch was designing a transistorized 1-kHz marker oscillator circuit to helprecord fast heart sounds. By mistake, he grabbed the wrong resistor from a box andplugged it into the circuit that he was making. Instead of producing the tone he expected,the circuit pulsed for 1.8 ms, stopped for 1 s, then repeated the cycle. Greatbatch recognizedthe “lub-dub” rhythm and the potential of the circuit for driving a sick human heart.On May 7, 1958, Greatbatch brought what would become the world’s first implantable cardiacpacemaker to William Chardack and Andrew Gage. The three connected the oscillatorcircuit to the exposed heart of a dog. The device took control of the rate.The blocking oscillator of the circuit is conceptually similar to that used in Greatbatch’sfirst pacemaker. The circuit is self-starting and its output waveshape (pulse width and intervalbetween pulses) remains almost constant despite drops in battery voltage. The circuitconsumes almost no power between pulses. The original pacemaker used 10 zinc–mercuryTime outSPaceFigure 8.2 This finite-state machine represents the operation of an early pacemaker that generatedpacing pulses at a constant interval. This state machine has a single state [S], [Time Out] is the eventthat causes the state machine to evolve, and [Pace] is the action that occurs as the state transitionoccurs. An arrowed line indicates the direction of a state transition and separates the event fromactions taken during the transition.
374 CARDIAC PACING <strong>AND</strong> DEFIBRILLATIONOscillatorVoltage DoublerR14.7MC10.47uFQ22N3906R610kR910kV12.8VD11N4148D21N4148R21.8kQ1MPS2924R320kR410kR550kQ3MPS2924+ C222uFR710kR850kQ4MPS2924+ C222uFCathodeElectrodeAnodeElectrodeR_HEART1kFigure 8.3 Early pacemakers had a period and pacing pulse characteristics (amplitude, waveshape, and duration) that were solely a functionof their circuit. In this replica of a 1960s design by Wilson Greatbatch, a self-staring blocking oscillator drives a voltage doubler to producepacing pulses with waveshape parameters (pulse width and interval between pulses) that remains almost constant despite drops inbattery voltage.batteries of 1.35 V and leads connecting the unit to the ventricle. The output was a 2-ms pulseof 5 to 8 V in amplitude every 1 s. Later, Greatbatch adopted the lithium–iodide batterychemistry, powering his circuits from a single 2.8-V cell. In the circuit of Figure 8.3, the outputof the blocking oscillator drives a voltage doubler, making the pacing pulses delivered tothe heart achieve sufficiently high amplitudes (approximately 5 V, as shown in the simulationresults of Figure 8.4) for the pacing electrodes of the time to “capture” the heart.Early pacemakers did not consider that the patient’s heart could have spontaneous electricalactivity. An important development in the field of cardiac pacing was the inclusionof circuitry that could detect the patient’s intrinsic heart activity and pace only when theheart’s rate fell below a predefined rate. Figure 8.5 shows that the logic needed to accountfor the patient’s intrinsic activity simply requires the addition of a sense event to the statemachine. When the pacemaker detects an intrinsic cardiac event, the timer in charge ofissuing [Time Out] is retriggered.In reality, however, the implementation of such a state machine is not all that simple,since it requires the inclusion of an amplifier and associated circuitry capable of detectingthe heart’s intrinsic activity. Since pacemaker sensing circuits usually limit their complexityto a low-power biopotential amplifier followed by a threshold detector, they detectintrinsic cardiac events based on the presence of a signal that surpasses the threshold voltage.This means that as the depolarization waveform sweeps past the pacing electrodes, thesense amplifier does not yield a single sharp transition that can be translated into a clear[Sense] event. Rather, it behaves as a very “bouncy” switch that generates a pulse trainwith unpredictable transitions and lasts as long as the cardiac signal remains within therange of the threshold comparator. In a similar way, the pacemaker’s logic must be able todiscriminate between an intrinsic beat and potentials resulting from pacing (the pacing
Figure 8.4 The output of a PSpice simulation on the circuit of Figure 8.3 shows that the circuit consumes almost no power between pulses.This simulation assumes use of a single lithium–iodide 2.8-V cell. The amplitude of the pacing pulses (approximately 5 V) was sufficientto “capture” the heart using 1960s electrodes. Today’s electrodes allow pacing to capture the heart reliably with sub-1-V pacing pulsesthat last 0.5 ms.375
376 CARDIAC PACING <strong>AND</strong> DEFIBRILLATIONSenseTime outSTime outPaceFigure 8.5 An important development was the inclusion of circuitry that could detect a patient’sintrinsic heart activity and pace only when the heart’s rate fell below a predefined rate. To do sorequires the addition of a sense event to the state machine. In its simplest form, when the pacemakerdetects an intrinsic cardiac event, the timer in charge of issuing [Time Out] is retriggered.SenseAR ToutRA ToutPaceFigure 8.6 The practical implementation of the state machine of Figure 8.5 requires the inclusionof a refractory period to “debounce” the sense event detected by a simple threshold comparator thatis generally used in the sense amplifier circuit. In this state machine, [A] is the “alert” state in whichthe pacemaker attempts to detect the heart’s intrinsic electrical activity, while [R] is the refractorystate in which the pacemaker ignores any external signal. The stimulus period is the sum of the timeoutperiods ([A Time Out] [R Time Out]).artifact and evoked potentials). To do so, the state machine is redesigned to incorporate theconcept of a refractory period. In the state machine of Figure 8.6, [A] is the “alert” statein which the pacemaker attempts to detect the heart’s intrinsic electrical activity, while [R]is the refractory state in which the pacemaker ignores any external signal. The stimulusperiod is now defined by the sum of two time-out periods [A Time Out] [R Time Out].An additional problem of using a simple signal detection scheme is the possibility thatinterfering signals, either from a source internal to the patient’s body (e.g., potentials fromthe arm and chest muscles) or an external source (e.g., electromagnetic interference) willfalsely trip the sense amplifier. One possible solution to this problem is considered later inthe chapter.Most pacemakers of the type described so far were used to stimulate the heart’s ventriclesin patients in whom intrinsic atrial signals would not propagate to the ventricles, most commonlydue to a block in the atrioventricular conduction system. An obvious limitation ofthese pacemakers is their inability to make use of atrial function to enhance hemodynamicperformance (the heart’s capability to pump blood to the body) when the ventricles are paced.Improved physiological response of the pacemaker can be achieved by expanding the statemachine to synchronize the activation of the ventricles to atrial activity. Figure 8.7 displaysthe state diagram of a dual-chamber pacemaker.
THE FIRST PACEMAKERS 377V SenseA SenseV SenseA V RA ToutA PaceAV ToutV PaceR ToutFigure 8.7 Dual-chamber pacemakers synchronize the activation of the ventricles to atrial activity. This simplified DDD pacemaker statemachine can pace both atria ([A Pace]) and ventricles ([V Pace]). It has the following possible states: [A], atrial and ventricular alert, duringwhich the pacemaker may sense signals from either or both chambers; [V], ventricular alert, during which sensing of intrinsic events isenabled only for the ventricle; and [R], refractory state. Possible events that cause transition between states are: [A Sense], sensing of anintrinsic atrial event; [V Sense], sensing of an intrinsic ventricular event; [A Time Out], maximum time that the state machine waits for anatrial sense event after exiting from the refractory period; [AV Time Out], maximum time that the state machine waits for a ventricular senseevent after an atrial event; and [R Time Out], refractory period.Possible events that cause transition between states are:• [A Sense]• [V Sense]• [A Time Out]• [AV Time Out]• [R Time Out]Sensing of an intrinsic atrial eventSensing of an intrinsic ventricular eventMaximum time that the state machine waits for an atrial sense eventafter exiting from the refractory periodMaximum time that the state machine waits for a ventricular senseevent after an atrial eventRefractory periodPossible actions taken by the state machine are:• [A Pace]• [V Pace]Pacing pulse delivered to the atriumPacing pulse delivered to the ventricleThe states of this pacemaker state machine are:• [A]• [V]• [R]Atrial and ventricular alert, during which the pacemaker may sense signalsfrom either or both chambersVentricular alert, during which sensing of intrinsic events is enabled only forthe ventricleRefractory stateIf intrinsic events are not detected from the heart, the state machine’s period is given bythe following sequence:1. Pacing pulse delivered to the atrium2. AV delay ([AV Time Out])3. Pacing pulse delivered to ventricle
378 CARDIAC PACING <strong>AND</strong> DEFIBRILLATION4. Refractory period ([R Time Out])5. Completely alert period ([A Time Out])6. Go to 1.This is an oversimplification of a real pacemaker’s state machine because it does notconsider the following situations that occur in clinical practice:• Atrial tachycardia: an inappropriately high atrial rate caused by such a simplifiedstate machine• Noise detected by the sense amplifiers• Need for atrial refractory of duration different from that of the ventricular refractoryAs such, this state machine is presented for illustration purposes only. The descriptionof the complete state machine of a modern pacemaker is outside the scope of this book.PROGRAMMABLE PACEMAKERSModern pacemakers make it possible to program the various timeouts and pacing pulseparameters. This allows therapy to be tuned to the specific requirements of the patient.Possible programmable parameters for a microprocessor implementation of the simplifieddual-chamber state machine described above are:Timeouts• [A Time Out]• [R Time Out]Period during which the device is able to detect the heart’s intrinsicactivityRefractory periodProgrammability of these parameters is accomplished by maintaining the programmed valuesin variables that can be handled by the device’s firmware. Physicians are asked to enterdesired values for the minimal heart rate (in beats per minute) and the refractory period (inmilliseconds). The alert period is then calculated as60,000 (ms/min)[A Time Out](ms) refractory period (ms)heart rate (beats/min)Pacing Stimulus Parameters• Pacing pulse width: duration of the pacing pulse, can be implemented in the sameway as timeouts• Pacing pulse amplitude: initial voltage of the pacing pulse; requires the hardware toenable the firmware to adjust the pacing voltage to the desired levelSensing Parameters• Atrial sensing sensitivity: threshold voltage level (in millivolts) that the atrial electrogramsignal must reach for the sense amplifier to report the occurrence of intrinsicatrial activity as an atrial sense event• Ventricular sensing sensitivity: same as above, but for the ventricle
Pacing Mode This parameter selects the state machine to be used to deliver therapy. Athree-letter code is used in medical nomenclature to specify a pacemaker’s behavior. Thefirst letter represents which chamber can be stimulated by the device (A, atrium; V, ventricle;D, both atrium and ventricle; O, no pacing enabled), the second represents thesensed chamber (A, atrium; V, ventricle; D, both atrium and ventricle; O, no sensing availableor enabled), and the third the behavior of the device upon detecting a sensed event (I,inhibit pacing; T, trigger pacing; D, both inhibit or pace, depending on the current state ofthe state machine; O, disregards sensed events).For example, the first pacemakers were asynchronous ventricular stimulators, alsoknown as VOO pacemakers:COMMUNICATING WITH AN IMPLANTABLE DEVICE 379• V• O• OPacemaker can stimulate the ventricle.No sensing capabilities are present.There is no response to sensed events (since no sensing means are available).The simplified state machine of Figure 8.6 corresponds to the VVI mode:• V• V• IPacemaker can stimulate the ventricle.Pacemaker can sense the ventricle.Ventricular pacing is inhibited whenever the pacemaker detects a timely intrinsicventricular event.The simplified dual-chamber state machine of Figure 8.7 implements a simple DDDpacemaker:• D• D• DBoth atrium and ventricle can be stimulated by the pacemaker.Both atrial and ventricular intrinsic signals can be detected by the pacemaker.Whenever timely intrinsic activity is present in both atrium and ventricle, thedevice inhibits pacing (I). However, when ventricular intrinsic activity does notfollow the atrial activity in a timely manner, the device triggers (T) pacing on theventricle in sequentially after the atrium.Another mode which is commonly included in pacemakers is a ventricular trigger(VVT):• V• V• TPacemaker can stimulate the ventricle.Pacemaker can sense intrinsic activity from the ventricle.Pacemaker stimulates the ventricle immediately following ventricular sensing.COMMUNICATING WITH AN IMPLANTABLE DEVICEFigure 8.8 shows how pacemakers have changed since their inception in the 1960s. Thefirst pacemakers had a predetermined set of operating parameters. Later, the pacing rate ofsome early user-settable pacemakers could be changed using a fine needle screwdriver tochange the setting of a potentiometer embedded within the material (e.g., epoxy and/or siliconerubber) encapsulating the pacemaker’s circuitry. Today, pacemakers are programmablein a noninvasive manner using a bidirectional RF link that permits an externalprogrammer to communicate with the implanted device’s microprocessor. Operatingparameters for external (temporary) pacemakers are usually selected through switches anddials.
380 CARDIAC PACING <strong>AND</strong> DEFIBRILLATIONFigure 8.8 Evolution of implantable pacemakers. Top, left to right: Very early CCC VOO pacemakerpowered by six mercury cells, Intermedics InterLith VVI with CMOS circuitry and poweredby a lithium cell. Bottom: Intermedics “Quantum” programmable VVI/VVT pacemaker, a modernMedtronic Thera DDDR pacemaker.Regardless of the programming method, the most convenient time for the microprocessorto read and update parameter settings is during the refractory period. Within that period, themicroprocessor is free to modify timeouts and/or reconfigure the stimulation and sensing circuits.Obviously, RF communication with an implantable device is more demanding thanpolling a few switches in a temporary external pacemaker. The RF link requires the implementationof a hardware and software communications protocol between the implantabledevice’s microprocessor and the microprocessor of a PC-like computer. In addition, modernprogrammers run graphical user interface (GUI) software to ease the programming of sophisticateddevices by physicians and other medical personnel.Since the circuitry of modern implantable devices is almost always encapsulated withina titanium case, communications is almost always achieved through a magnetically coupledlink operating in the sub-100-kHz spectrum. This is a strong limiting factor to the datathroughput through of the link. However, speed is not usually critical for programmingoperations, since the usual parameter set of an implantable pacemaker does not require theexchange of more than a few bytes per cardiac cycle, and at least 100 ms of the refractoryperiod is available on each beat. Although communications speed is not a major constraint,the reliability of the protocol is of utmost importance. Communications protocols forimplantable devices are usually designed with 100% redundance to ensure that the parametersselected by the physician are received and accepted correctly by the implantabledevice’s microprocessor.
EXTERNAL VVI PACEMAKER 381EXTERNAL VVI PACEMAKERFigure 8.9 shows a simple implementation of a VVI pacemaker which will be presented asan example of the techniques involved in the design of pacemakers. The device is representativeof a simple external pacemaker and is switch-programmable as follows:• Mode: VVI, VOO• Rate: 40, 50, 55, 60, 65, 70, 80, 90, 100, 110, 120, 140 beats/min• Refractory period: 250, 350 ms• Pacing pulse amplitude: battery voltage (e.g., 3 V) and two times battery voltage(e.g., 6 V)• Pacing pulse width: 0.125 to 1.5 ms in 0.125-ms steps• Ventricular sensing sensitivity: 1.0 to 6.0 mV in 1.0-mV stepsAlthough functional, the design is given only to illustrate the basic implementation ofa pacemaker’s circuits and state machines. The design does not include a number of importantfeatures found in modern temporary pacemakers, such as:• Low battery detection• “Runaway” detection (which provides protection against clock speedup which canresult in pacing rates beyond 180 ppm)• Regulated power supply• Protection against EMI, electrosurgery, and defibrillationAs shown in Figure 8.10, the state machines that make up this pacemaker’s logic run ona Microchip PIC16C76 microcontroller. This device spends the vast majority of time in the“sleep” mode and is awaken only after timeout of its counters or when a ventricular senseevent is communicated via a high logic state on the circuit’s input line, RB0. The timer isdriven through a crystal-based oscillator running at 32.768 kHz. However, a 4-MHz RCclock is used to run the CPU (not the timer) once the microcontroller wakes up. The RCoscillator is preferable over a crystal oscillator because the former starts oscillation andstabilizes much more quickly once the microcontroller is awaken.V+MicroprocessorV+V-SensingPIC16C76StimulusGeneratorV-SensitivityOtherParametersFigure 8.9 Block diagram of a simple external (temporary) VVI pacemaker circuit. Operatingparameters are programmed through switches.
VDDR211MVDDR20750KC6RefractoryPeriodR221MSW6ACTIVE_DISCHARGEPACINGSENSING INC7 15PF VDDVDDY1R234.7KR24R25R2747033KC8 HIGH AMPLITUDE PACING 1K15PFR28R29C91K1K22PFR30R311K1KR32R331K1KR35R361KSW21KR38PIC16C76R37 1KVDD1KREADING ENABLER394.7KR40470R421 KVDDVDDR43R441K1KR26R45R46R411M1K 1K1MR47R481K 1KR49R50SW4SW51KSW31KR53R52 1KPacing Mode R341K1M32.768KHZ25161718RB42820 1IC4RC3/SCKRC2/CC1RB0/INTRA0/AN0RA4/TOCKRA5/SS/AN41211 RC1/T1OSCI/CCP2RC0/T1OSO/T1CKIRB110 RB39 OSC2/CLKOUTC1/CLKIN5RA3/AN3/VREFRC4/SDI/SDA4RB53 RA2/AN2RB6RA1/AN18 191413RB7VDDMCLRRC5/SD0RC6/TX/CKRC7/RX/DT47NFRB221723262224152627R511MREADING ENABLEVSSVSSPacing PulseWidthSelectionPacingAmplitudeSelectionBaseFrequencySelectionSelectionFigure 8.10 A Microchip PIC16C76 microcontroller runs the pacemaker’s state machines. It spends the vast majority of time in the “sleep”mode and is awakened only after timeout of its counters or when a ventricular sense event is detected through RB0. The timer is driventhrough a crystal-based oscillator running at 32.768 kHz. A 4-MHz RC clock is used to run the CPU once the microcontroller wakes up.382
Figure 8.11 presents the schematic diagram of the sense amplifier circuit. The ventricularelectrogram signal detected through the electrodes attached to the ventricle is attenuatedby the voltage divider formed by resistor R7 and one of the resistors among R15, R16, R17,R18, or R19. Selection is performed via five-position switch SW1, which sets the sensitivityof the sense amplifier. Past the variable attenuator, the electrogram signal is amplified byop-amp IC1. The bandpass of this amplifier is 88 to 100 Hz. The high-pass cutoff is set bythe RC filter formed by R8 and C5. The low-pass characteristics are given by the bandwidthof the µPC4250 op-amp, which is a function of its bias set through resistor R12.Comparators IC2 and IC3 detect whether or not the amplified and bandpassed signalhas an amplitude with absolute value above 15 mV. The comparison range is defined by thedivider formed by resistors R4, R6, R9, and R11. At rest, the outputs of both comparatorsremain at logic low. If the signal exceeds the positive threshold, the output of IC2 goeshigh. If the negative threshold is crossed, the output of IC3 goes high. The comparator outputsare ORed via the two diodes inside D1. A high signal at the output of the wired-ORis interpreted by microcontroller IC4 as a sensed event.Figure 8.12 presents the schematic diagram of the of the pacing pulse generator circuit.This circuit is able to generate pacing pulses with an amplitude of 3 or 6 V, depending onthe state of the pacing amplitude selector switch. When inactive, the microcontrollersets the HIGH AMPLITUDE PACING line low, which charges “tank” capacitor C2 toVDD. The PACING signal is maintained low to keep transistor Q2 open, and lineACTIVE_DISCHARGE is maintained high to keep switch Q1 open. Coupling capacitorC1 slowly discharges by way of resistor R1 (100 kΩ) through the heart’s tissues and electrodesconnected to terminals V and V.When a stimulus is to be generated, and if the amplitude selected is 6 V, IC4 sets HIGHAMPLITUDE PACING line high, which closes Q4 and opens Q3. This causes the positiveterminal of capacitor C2 to be connected with the battery’s negative terminal. When pacingat 3 V is desired, HIGH AMPLITUDE PACING is set low, which connects the C2’spositive terminal to the battery’s positive terminal (VDD). In the first case, the potentialdifference between the negative terminal of C2 and VDD is 6 V, while in the second casethe potential difference is 3 V.To deliver the stimulus to the tissue, microcontroller IC4 sets the PACING line high,which closes Q2 and connects the negative terminal of C2 to C1 (which is discharged). Assuch, the leading-edge voltage of the pulse appearing across electrode terminals V andV is equal to the selected voltage (3 or 6 V). This voltage decays throughout the pacingpulse as C2 discharges and C1 charges. To terminate current delivery to the tissue, IC4places all stimulus-related lines back to their rest condition.Once the pulse has been delivered, coupling capacitor C1 remains charged. The deliveryof a new pacing pulse will require this capacitor to be discharged, a procedure that is doneby delivering the energy stored in this capacitor through the tissue. A net-zero current flowthrough the tissue is accomplished by passing the same amount of charge (albeit not withinthe same amount of time) through the tissue as was delivered during the stimulus pulse, butin the opposite direction. Not doing so would cause electrochemical imbalance, which canresult in electrode corrosion and tissue damage. In this pacemaker, charge balancing isaccomplished during the refractory period by taking line ACTIVE_DISCHARGE low,which closes Q1 allowing the charge in coupling capacitor C1 to flow through the tissue viaresistors R2 and R1 (100 Ω in parallel with 100 kΩ). Any remaining charge after the fastdischarge time is delivered at a slower rate through R1 (100 kΩ).Pacing parameter selection in this demonstration external pacemaker is done throughswitches. As shown in Figure 8.10, parameters with only two possible values (i.e., mode,pacing pulse amplitude, and refractory period) use SPDT switches to deliver a logic highor a logic low directly to an input pin of the microcontroller. The rotary switch used forsensing sensitivity selection acts directly on the sense amplifier circuit. Rate and pacingEXTERNAL VVI PACEMAKER 383
SENSING INVDDR45.1MC347NFD2HSMS2802 1 2VDDR720KR176.8K3R185.1KC4100NFR882KC522NFR193.9KR647KR947K32R115.1M7+6- IC1 UPC42504 8R1215MR510-15M327UPC4250+- IC24 86R1315M327UPC4250+- IC34 8HSMS28246R1415MD3R101MSW11RSW6SENSITIVITYSELECTORFigure 8.11 The sense amplifier circuit detects ventricular electrogram signals through electrodes attached to the ventricle. Signals areattenuated by the voltage divider formed by resistor R7 and one of the resistors among R15, R16, R17, R18, or R19. Selection of the senseamplifier sensitivity is through switch SW1. Signals within band 88 to 100 Hz are then amplified by IC1. Comparators IC2 and IC3 detectthreshold crossings by the signal. Sense events are sent to microcontroller IC4 when either comparator is activated.R1610KV+V-R1520K384
VDDV+AnodeACTI VE_DISCHARGEQ1BSS84R2100R1100KOUTPUTSTIMULUSVDDQ2BSS138C1+10uFV-CathodeHIGH_AMPLITUDE_STIMULUSQ3BSS84Q4BSS138+C215uFR315KD1HSMS2824VDD3VHIGH AMPLITUDE STIMULUSACTIVE DISCHARGESTIMULUSOUTPUT VOLTAGEINTO TISSUE10 - 50 ms3V
386 CARDIAC PACING <strong>AND</strong> DEFIBRILLATIONpulse width selection is accomplished through rotary switches that select a resistor usedwithin a voltage-divider circuit fed from the battery voltage. The output of the resistivedivider is measured by one of IC4’s analog inputs. Different voltages are mapped by themicrocontroller to the various parameter value selections.Power for the circuit is obtained from a single nonrechargeable 3-V lithium battery(e.g., a Panasonic lithium carbon monofluoride battery). Please note that pacing pulseamplitude and sensing sensitivity vary as a function of battery voltage. Although two regularalkaline batteries in series could be used to power the circuit, the lithium carbonmonofluoride chemistry has an almost flat discharge curve which minimizes the shift in thesensing threshold as battery capacity is used.Almost all commercially available implantable pacemakers designed in the last 20 yearsuse lithium–iodide cells (Li/I 2 ). These cells are designed to deliver current drains in themicroampere range, reliably over long periods of time. They are available from Wilson GreatbatchTechnologies, Inc. in a variety of sizes, shapes, and capacities. Lately, implantable-gradelithium carbon monofluoride (Li/CFx) are being used more and more in pacemakers and otherimplantable devices. The internal impedance of the CFx cell is much lower than that of theLi/I 2 cell throughout its entire life, allowing more flexibility in circuit design and performance.Wilson Greatbatch Technologies, Inc. now has Li/CFx batteries, which feature a titaniumcase, making it weigh half of a Li/I 2 cell of the same capacity.Firmware for the VVI PacemakerThe microcontroller runs algorithms that implement the state machine as well as stimulusroutines. Firmware for pacemakers is usually coded in assembly language due to reliabilityconcerns as well as real-time and power consumption issues. For clarity in this example,however, programming was done in C. Despite this, power consumption and real-timeperformance are reasonable, and use of a high-level language could be used to developcode for an implantable device.The basic state machine for a VVI pacemaker was shown in Figure 8.6. However,enhancements are required to enable the logic to discriminate true intrinsic cardiac eventsfrom interference, such that pacing therapy is inhibited only when true ventricular activityoccurs. A possible way of implementing a discrimination mechanism is to use dedicatedhardware to prevent interfering signals from triggering a sense event at the microprocessor’sinput. For example, a retriggerable monostable together with edge-triggered sensing by themicroprocessor would be able to cope with noise. However, this implementation requiresadditional circuitry and does not lend itself to real-time reporting of noise detection. Instead,this pacemaker design incorporates software mechanisms to detect noise and change thedevice’s behavior to prevent noise from inappropriately inhibiting pacing therapy.International standards that define the minimum requirements for pacemakers establishthat devices must consider events detected repeating at more than 10 Hz to be noise. Whensuch a condition is detected, a VVI pacemaker must automatically switch the mode toVOO. The device should remain in this asynchronous mode until normal sensing isresumed. Events detected at a rate below 10 Hz cannot be distinguished by simple circuitryfrom real cardiac events and may occasionally give rise to uncertain responses.The state machine of Figure 8.13 is an enhanced version of the basic VVI state machinecapable of detecting and responding to the presence of noise. Two new states [N] and [W]have been added. These states affect the sense condition, as well as the way in which themachine returns from the [R] state to the [A] state. The refractory period is now split intwo: [R Time Out], which is an absolute refractory, which then proceeds to state [N]–anoise window within which events are sensed but not reported to the VVI state machine.Whenever a sense event occurs within state [N], the moment of occurrence is stored intime stamp variable [TS], but the machine remains in state [N] until a 100-ms timeout
EXTERNAL VVI PACEMAKER 387TimeStampSenseNN ToutR ToutSense and no noiseARA ToutPacePaceSense and noiseWA ToutFigure 8.13 This enhanced version of the basic VVI state machine is capable of detecting andresponding to the presence of noise. The refractory period is now composed of an absolute refractory[R Time Out] and noise window [N]. The presence of noise is assumed if the difference in timebetween sense events within [N] and [A] is equal or smaller than 100 ms, causing the machine tomove to state [W] to complete the programmed period.[Noise Time Out] elapses. By the time the machine enters the alert state [A], the completerefractory period will have elapsed, and variable [TS] will hold the time of the last senseevent detected within the noise window. Under no-noise conditions, [TS] will be zero.If no event is detected within the alert state [A], the device’s behavior does not change.However, if an event is detected within [A], it is evaluated against the time of events thatmay have occurred within the noise window. If the difference between the time of occurrenceof a sense event within the alert window and a time-stamped event is less than100 ms, the presence of noise is assumed (since 1/100 ms 10 Hz), and the state machineis moved to state [W] to complete the programmed period. If, on the other hand, thedifference in time between the event sensed and the time-stamped event is larger than100 ms (or no sensed events occurred within the noise window), the response to the sensedevent will be to inhibit pacing and start a new cycle.Despite the additional complexity introduced by this mechanism to the basic VVI statemachine, its realization is relatively straightforward. An efficient and clear-cut method forimplementing the finite-state machine is to encapsulate the event detection procedure withina routine [GetEvent()] and build an infinite loop that polls a variable that keeps track of themachine’s current state.
388 CARDIAC PACING <strong>AND</strong> DEFIBRILLATIONThe pacemaker state machine can then be implemented using the following code as themain software loop:for( ; ; ) {switch( State ) {case ALERT:Event GetEvent();DisableSense() ;switch( Event ) {case TOUT:Pace();Tout RefractoryTout ;State REFRACTORY;break;case SENSE:if ( (TimeStamp 0) (SenseTime –TimeStamp > T_100ms) ) {Tout RefractoryTout ;State REFRACTORY;}else {Tout AlertTout - Elapsed() ;State WAIT_END_ALERT ;}break;default:State FAILURE;break;}break;case WAIT_END_ALERT:Event GetEvent();switch( Event ) {case TOUT:Pace();Tout RefractoryTout ;State REFRACTORY;break;default:State FAILURE;break;}break;case REFRACTORY:ReadParameters();Event GetEvent();switch( Event ) {case TOUT:EnableSense();TimeStamp 0 ;Tout T_100ms ;State NOISE_WINDOW;break;
EXTERNAL VVI PACEMAKER 389}}default:State FAILURE;break;}break;case NOISE_WINDOW:Event GetEvent();switch( Event ) {case TOUT:Tout AlertTout ;State ALERT ;break;case SENSE:TimeStamp SenseTime ;Tout Tout - Elapsed() ;break;default:State FAILURE;break;}break;case FAILURE:default:break;The variables for this implementation of the state machine are:• Unsigned char State: keeps the current state of the machine. In addition to the variousstates of the machine, this variable can also have the value of FAILURE to terminateoperation of the device in case of failure.• Unsigned char Event: represents the event that occurred.• Unsigned int Tout: global variable used to tell GetEvent() of a desired timeout.• Unsigned int RefractoryTout: keeps the programmed refractory period minus 100 ms.These 100 ms correspond to the time that the machine spends in the noise window.• Unsigned int AlertTout: keeps the programmed period minus the programmed refractoryminus the programmed pacing pulse width.• Unsigned int TimeStamp: keeps the time at which a sense event is detected within thenoise window.• Unsigned int SenseTime: keeps the time at which the last ventricular event is detected.It is used to calculate whether a sensed event that happens within the alert state shouldbe classified as normal or as noise.Auxiliary routines used by the main routine are:• Unsigned char GetEvent(): waits for the occurrence of an event. Its return value correspondsto the event that happened. Please note that the microcontroller will spendmost of its time within this routine.• Void DisableSense(): prevents sense events from being reported by GetEvent(). Thisfunction could be used in an implantable device to turn off sensing circuitry when notneeded in order to reduce power consumption.
390 CARDIAC PACING <strong>AND</strong> DEFIBRILLATION• Void EnableSense(): does the opposite of the previous routine.• Void Pace(): implements pacing pulse generation.• Unsigned int Elapsed(): returns the time elapsed while GetEvent() waited for anevent to occur.• Void ReadParameters(): reads programmable parameters and updates them. Oncethis routine updates parameters, the device assumes the new parameter set at once.The book’s ftp site includes three source code file archives for firmware that can be usedfor this project:1. VVI.zip implements a simple VVI state machine that disregards the VOO mode.This is the program that was discussed above.2. VVI with embedded VOO.zip implements a VVI state machine that can be placed inVOO mode by disregarding sensed events. The state machine is identical to the oneimplemented in VVI.zip, but the EnableSense routine enables or disables sensingdepending on the desired state.3. VVI VOO with VOO state.zip is a VVI state machine in which the VOO state isimplemented through a new state during which there is no sensing.POWER CONSUMPTIONTogether with safety and reliability, power consumption is a major design constraint in thedevelopment of implantable devices. One popular technique is to power-down circuitswhen they are not in use. For example, power to sense amplifiers can be shut down duringthe refractory period. In a similar manner, the telemetry and communications circuit canbe kept off when out of range of a programmer.Interestingly, software in an implantable device is often evaluated in connection withthe power that it consumes. To keep power consumption down, clocks are kept to the lowestpossible frequency, and software is usually designed to maximize the microcontroller’sstandby mode (using the SLEEP command). The [GetEvent()] routine implements thistechnique in the following manner:unsigned char GetEvent(){InitTout( Tout );Sleep();SenseTime ReadTimer();if( INTF && INTE ) //sensing event{INTF 0;return SENSE;}else if ( TMR1IF && TMR1IE ) // timeout{TMR1IF 0;return TOUT;}elsereturn UNKNOWN_EVENT;}
S<strong>OF</strong>TWARE TESTING 391Of course, safety is by far the major concern in a medical device. Modern pacemakersincorporate fault-detection mechanisms such that if a fault condition arises, they will notcause harm to the patient. In some devices, redundancy is incorporated in the design of thepacemaker circuitry to ensure the maintenance of pacing therapy in the event of crystaloscillator, microprocessor, or other failures. When such a safety measure is implemented,the pacemaker may incorporate a backup pacing controller that runs on independent circuitry(either a separate microcontroller or dedicated logic) with conservative parametersthat suffice to provide life-sustaining therapy to most patients.The pacemaker presented in this section does not have redundant pacing capabilities.By way of example, however, the pacemaker’s firmware incorporates some fault-detectionmechanisms. Tripping any of the following fault detectors causes the device’s pacing therapyto be deactivated:• RAM signature. Possible catastrophic RAM failures cause all volatile memory locationsto be written with hex 00 or hex FF. These failures can be detected by initializinga specific volatile memory location with a test value (a “signature”) and havingthe firmware check for the presence of this value on every cardiac cycle.• Parameter shadowing. Programmable devices keep parameters that reside in variablesthat should remain invariant at all times except when a programming operationtakes place. For this reason, it is convenient to keep a duplicate copy of the parameterarea (parameter “shadow”) and check consistency of the main parameter area withits shadow on every cardiac cycle.• Program counter outside program area. Unexpected intrusions of the program counterinto areas outside that used for the device’s program can be detected by filling any freeprogram memory with instructions to jump to a known safe program instruction.S<strong>OF</strong>TWARE TESTINGImplantable pacemakers and defibrillators take care of conditions that could lead to thepatient’s death if left untreated. In addition, inappropriately delivered stimuli can causedangerous and even lethal tachyarrhythmias. For this reason, testing of implantable cardiacstimulators has to be planned and performed with utmost care. Verifying that thehardware of the device works properly is relatively straightforward, since it usuallyinvolves injecting known test signals to the various subcircuits and verifying their operation.In addition, various kinds of hardware-related faults can be simulated readily usingexternal hardware.On the other hand, testing proper operation of the software is more involved and less ofa common area for the uninitiated. Probably the most important tool for software testingstarts with the design of the software itself. The key to simplifying testing is in writingclean, simple code which is as legible as possible and as close as possible to the formallanguage used to describe the operation of the device—in this case using finite-statemachines and timer events.In the example project presented above, testing would not only involve assessing properoperation of the various circuits and the ways in which the microprocessor controls them,but also the operation of the system as a whole, paying special attention to power consumption,operation of the [GetEvent()] routine and tests of the behavior of the device inthe presence of noise. A reasonable approximation could be connecting the sensing inputto a signal generator and verifying that the device enters the noise mode in the presence ofsignals sensed with a frequency over 10 Hz. Besides the clock, the device has a singleexternal signal input, making it relatively easy to probe its behavior in response to differentsignal patterns.
392 CARDIAC PACING <strong>AND</strong> DEFIBRILLATIONRATE RESPONSIVENESSThe pacemakers described so far attempt to maintain the ventricular rate over a minimum,fixed programmed rate. However, most modern pacemakers have sensors that feedalgorithms that attempt to determine what the heart rate should be from moment tomoment. These sensors measure variables that are connected to the patient’s activitylevel and/or emotional state, making it possible to calculate whether a heart rate higherthan the programmed base rate should be maintained to supply the body with blood duringtimes of physical and/or emotional stress. These pacemakers are said to be rateresponsive and are identified by the letter “R” following the operational mode (e.g.,DDD-R).Rate-responsive pacemakers make use of different sensor technologies to determine theoptimal heart rate. The goal is to control the heart rate of a pacemaker patient in a mannersimilar to the intrinsic heart rate of a healthy person with a normally functioning heart,under various conditions of rest and exercise, in a physiologically appropriate manner. Themost common type of sensor used in pacemakers today is one that detects body movement.The more the patient is moving, the faster the heart rate should be. The level of activity ormotion of the patient is picked up by an accelerometer or a piezoelectric crystal “microphone.”Filtering and signal processing are applied to the signals detected by activity sensorsto reduce the effects of disturbances unrelated to exercise which would otherwiseaffect the heart rate.Another widely used method for rate responsiveness involves estimating a respirationparameter called minute ventilation (MV). Minute ventilation is the air volume beingexpired by the patient during 1 minute. Most minute ventilation sensors use the principleof impedance plethysmography, where the electrical impedance of the lung tissues is monitoredand the changes in electrical impedance are interpreted as changes in the volume ofair in the lungs. Higher impedance typically results from more air and less blood in thelungs following inhalation. Conversely, lower impedances result from less air and moreblood in the lungs due to expiration.Despite advances in the technology, activity sensors are inherently limited to detectingphysical activity, leaving the pacemaker unresponsive to emotional stresses, which alsorequire added hemodynamic support. In addition, activity sensors also have to make strongassumptions regarding what the patient’s rate should be after exercise has stopped butwhen the patient still needs high levels of blood flow to let the tissues recover. For this reason,the very latest commercial pacemakers combine an activity sensor with an MV sensorto get the rate response closer to that of a healthy person.There is still place for further developments in sensor technology for pacemakers. Thisis not only because better response to emotional stresses is desirable, but because theheart’s own state should be considered in the calculation of rate. As such, it would be desirableto tune the parameters of a pacemaker to improve it hemodynamic state: namely,forces the heart has to develop to circulate blood through the cardiovascular system. Thehemodynamic state of the heart is represented by the relationship between blood pressureand blood flow.One promising hemodynamic sensor technology that we have worked on is the measurementof intracardiac impedance. In essence, impedance signals derived from electrodesattached to the heart contain information regarding the volume of blood held by the heartas a function of time. Intracardiac impedance measurements have been used to estimate theheart’s stroke volume. The stroke volume of the heart is defined as the volume of bloodexpelled by the ventricle in a single beat. It is equal to the difference between the end diastolicvolume (volume of blood to which the heart is filled when it relaxes) and the end systolicvolume (volume of blood remaining in the heart when it reaches maximum
IMPEDANCE TECHNIQUE 393contraction). In healthy humans, the stroke volume of the heart has been found to remainrelatively constant over a wide range of exertion.Now, cardiac output equals stroke volume multiplied by heart rate. Increases in cardiacoutput required to meet physiologic needs are provided primarily by increased heart rate, butsome of the cardiac output during exertion is also provided by the heart, increasing its strokevolume. The stroke volume cannot increase, however, by a factor more than about 2 to 2 1 2 .Beyond a certain rate, the heart does not fill up sufficiently, and increased heart rate beyondthis point can actually result in decreases of stroke volume and ultimately, cardiac output.The point at which further increase in heart rate does not result in an increase in stroke volumeis typically shifted markedly toward low rates for patients suffering from diseases of theheart muscle. The idea then is to use an impedance sensor to estimate stroke volume, andadjust the pacemaker’s base rate and other parameters to optimize cardiac output.IMPEDANCE TECHNIQUEImpedance plethysmography (also known as impedance rheography) is one of the oldestapplications of impedance measurement on living tissues. It is based on the fact that theimpedance of body segments reflects the filling state of the blood vessels contained. Thisprinciple has been used in such diverse applications as monitoring cardiac hemodynamics(impedance cardiography), monitoring lung function and perfusion (rheopneumography),and monitoring cerebral blood flow (rheoencephalography). Since the conductivity of thebody depends on the fluid content in various intracellular and extracellular compartments,body composition estimates can also be made using impedance measurements by assumingthat bodily fluids subdivide the body mass into fat mass and lean body mass. In addition,impedance measurements are not limited to estimating the volume of bodily cavities.Bioimpedance techniques have also been used at the level of individual cells and smallgroups of cells to discriminate pathological states from changes in their equivalent resistiveand capacitive parameters. For example, such changes have been detected in cancerouscells.In the case of intracardiac impedance measurements, the impedance between two electrodesin the ventricular blood pool decreases as the ventricle is filled (since there are moreconduction pathways for electrical currents), reaching a minimum at end diastole. At endsystole, when the ventricle has expelled as much blood as possible, impedance measurementsreach their highest values. Figure 8.14 depicts the most common methods for measuringthe impedance of tissues. Here a constant-current source injects an ac current ofconstant amplitude into the tissue through two current-injection electrodes. This currentcauses a potential difference to be developed between any two points between the currentinjectionelectrodes. This potential difference is related to the resistivity of the tissuebetween the voltage-sensing electrodes. The equivalent resistance is defined as the ratio ofthe voltage difference between the two voltage electrodes and the current flowing throughthe tissue.Two-terminal measurements introduce some errors because the potential differencesensed between the two electrodes includes nonlinear voltages generated by the currentflowing through the polarization impedance at the electrode–tissue interface. The fourelectrodeconfiguration yields a more precise measurements since the highly nonlineareffects of electrode–tissue contact impedance are reduced, as the sites of current injectionand voltage measurement are physically separated. With a constant-current source, theinjected boundary current becomes essentially independent of the contact impedance.Using voltage amplifiers with sufficiently high input impedance ensures that voltage measurementsare virtually unaffected by the electrode–tissue contact impedance. For example,
394 CARDIAC PACING <strong>AND</strong> DEFIBRILLATION(a)ConstantCurrentSourceFIVAC VoltmeterElectrodeTissue(b)IVVoltageSensingElectrodeCurrent-InjectionElectrodeTissueFigure 8.14 The most common method for measuring the impedance of tissues involves injectingan ac current of constant amplitude into the tissue and measuring the potential difference developedacross two points between the current-injection electrodes. (a) Two-terminal measurement in whichthe impedance of the system at frequency f is given by Ohm’s law R V/i. (b) A four-terminal techniquereduces errors of the two-terminal measurement caused by nonlinear potential differences generatedat the current-injection electrodes by currents flowing through the electrode–tissue interfacepolarization impedance.in an impedance cardiograph (Figure 8.15), one set of surface electrodes (usually, twopairs of gelled disk electrodes or two band electrodes) placed on the upper abdomen andupper neck are used to inject an ac current, providing more or less homogeneous coverageof the thorax with a high-frequency field. The voltage developed by the field is detectedthrough a second set of electrodes located at the level of the root of the neck and thediaphragm.The circuits of Figures 8.16 to 8.20 implement a general-purpose impedance plethysmograph.The circuit of Figure 8.16 is a 50-kHz sinusoidal oscillator that feeds the voltage-controlledcurrent source of Figure 8.17 [AAMI, 1994]. The output of the RCoscillator formed around IC2A is feedback-stabilized by JFET transistor Q1. This transistoris controlled by the error signal between the amplitude setpoint given by R16 and theaverage oscillator output signal envelope calculated by the detector formed by D1 and C4.The output of the oscillator is buffered by IC1A, scaled via potentiometer R30 and accoupledto modulate the current through Q3. IC3, Q2, and Q3 is a class B amplifier that ismade to operate as a constant-current source. The 50-kHz input signal is adjusted via
IMPEDANCE TECHNIQUE 395
396 CARDIAC PACING <strong>AND</strong> DEFIBRILLATIONC1R1R43.5KR23.5KIC3.001uF.001uF342+-11R74.7KIC2ATL0841R347KR524KI6511447K-+R8IC2BTL0847C20.1uFOUTPUTSETTINGR650KHZ50KI47KR122.2KR947K11910R1324K4-+IC2CTL0848R104.7KD11N914C40.1uFR1147KIC5IR14150K-5VisoR1535050 KHzC7+ C6IC2D AMPLITUDEQ110uF .01uFSETTING11 TL084MPf102I IR17D2DR1813R16G3.6V1410K-1247K1WS10K+4IC8R19+24K.01uF IC9C10+5Viso10uF.01uFIII IFigure 8.16 A 50-kHz sinusoidal oscillator used to drive the current source of the general-purpose impedance plethysmograph. The outputof the RC oscillator formed around IC2A is feedback-stabilized by JFET transistor Q1, which is controlled by the error signal betweenthe amplitude set point given by R16 and the average oscillator output signal envelope calculated by the detector formed by D1 and C4.33pF-5Viso15 should be supplied to the circuit from a medical-grade power supply. The isolationamplifier (IC7) generates isolated 15 V, which are regulated via IC10 and IC13 to 5Vused to power the 50-kHz oscillator, constant-current source, and synchronous demodulator.Alternatively, a 9-V battery can be used to power these circuits via the 5-V linearregulator IC10. If a battery is used, 5 V is generated using voltage pumps IC11 and IC12.Measurements of ventricular volume using a “conductance catheter” are done in essentiallythe same way as for impedance cardiography, but using catheter-borne electrodesinstead of surface electrodes. As shown in Figure 8.21, a multielectrode catheter is introducedin the left ventricle. A small (e.g., 10 µA), high-frequency (e.g., 50 kHz) constantcurrent is injected via the two extreme electrodes, and voltages are measured by severalintermediate pairs of electrodes. The idea is to divide the ventricular cavity into a numberof cylindrical segments. The various voltage signals are each proportional to the volumeheld by each segment. The sum yields the total ventricular volume.
IMPEDANCE TECHNIQUE 397C110.1uFR205.6M1%+5Viso+5VisoIR2111K1%R221K+ C1210uFI+ 10uFC15IR2810M1%C13.01uFI7 132+-4 5C16 -5Viso.01uFI R271M1%IC3TL0816R2322K1%R2422K1%R2511K1%1%IQ22N3906Q32N3904R261K1%JP1JUMPERC14.05uFCurrent InjectionElectrode 1J11 Inj1J21VTOI_1Inj2Current InjectionElectrode 250KHZR29100K832+-IC1ATL0821IJP2JUMPER4 C17R3010K.047uFIFigure 8.17 Voltage-controlled current source of the general-purpose impedance plethysmograph. The output of the oscillator is bufferedby IC1A, scaled via potentiometer R30 and ac-coupled to modulate the current through Q3. IC3, Q2, and Q3 is a class B amplifier that ismade to operate as a constant-current source.-5VisoImpedance measurements obtained through the conductance catheter cannot be useddirectly, since important intrinsic errors are generated by the nonhomogeneous distributionof the current lines within the measured volume as well as because of leakage currentsthrough the heart muscle and extracardiac tissues. The first error affects the linear relationshipbetween conductance and volume, while the latter adds a “phantom” parallel volume.Special calibration and signal processing techniques are usually applied to scale andlinearize the impedance measurements against true ventricular volume.Conductance catheters are often used by researchers and physicians to generate a graphof the left-ventricular pressure–volume relationship. This relationship, known as a PVloop, gives important information on the type of cardiomyopathy and possible treatments.Pressure is measured using a miniature sensor that is part of the conductance catheter. PVdiagrams clearly distinguish the four phases of the cardiac cycle (isovolumetric contraction,
DIFFERENTIAL<strong>OF</strong>FSETNULLINGR3510KR3710KCOMMON-MODE<strong>OF</strong>FSETNULLINGC180.1uFR31+5Viso100K-5VisoD3FDH300D4FDH300IC5INA110OUTPUTGAINADJUSTR34100KI234-+8+5VisoIC4ATL0821R32100KIC190.1uFDEMOD_OUT-5Viso+5Viso-5VisoD5FDH300D6FDH300R38100KR42100KX10X100X200X500R39100KIJP3JP4JP5JP6C24.01uFR401KR43100KR44620K+5VisoR411KCMRRADJUSTI369OOA2SENSE21 +IN -IN RG REF1312 *1016*100 11*200OUT*5004IOA15 14 15 10 IOA5OOA1+5Viso +C25.01uFR45II71171614151213IC6CS B/ARINARINBRARBRFCOMPVOUTAD630IC211uFCHA+CHA-CHB+CHB-SELASELBDOADJDOADJCOADJCOADJ+VS-VSI22018191093456118C220.1uFIC230.1uF+ C20I1uF+5Viso-5VisoI-5Viso-5Viso100K+5Viso-5Viso+5Viso +VCCIC1BTL082568+-47IC26.01uFR47100KR49100KIC27.01uF654-+8IC4B7TL082R48I++DECOUPLING CAPS.INA110C2810uFC3210uFC290.1uFC330.1uF-5VisoC30.01uFIPHASESHIFTADJUSTIC34.01uFC31.01uFI+5VisoFigure 8.18 A lock-in amplifier is used to detect 50-kHz voltage signals in the general-purpose impedance plethysmograph. The circuitcomprises a standard linear amplifier (IC5) followed by a synchronous detector (IC6). The reference signal is buffered through IC1B.Demodulation is maximized by correcting the reference signal phase through the phase-shifting circuit built around IC4B. The lock-inamplifier’s output is scaled and low-pass filtered via the circuit built around IC4A.I100K-5Viso-VCCR33100KR731MR36100KR46100KVoltageSensingElectrode 1J3C6510.47uFIVoltageSensingElectrode 2J41REFERENCESIGNALINPUT50KHZ398
DEMOD_OUT+15Viso-15VisoINPUTJ5SMC39.01uFII+ C3822uF+ C4222uFL2330uH85mAL3330uH85mAISOLATION BARRIERMAINTAIN 0.3" AIR CLEARANCE<strong>AND</strong> 0.5" CREEPAGE+15Viso+C4022uF++C3710uFNON-ISOLATEDSIDE10+9113 11 VINV OUT234JP12JUMPERJP16JUMPERIC10LM78L05ACZ2C5810uFR51+VPJP13JUMPERI-VPJP17JUMPER90.9K-5VisoJ81 2X100X1JP14JUMPERJP18JUMPERGAINSETTINGR531.5KD71N5817C46.33uFC48.1uF+C5310uFC6010uFC44.01uFIR5410KC49.01uF-VPR61100KC51.01uFR56100KR58100KC50.01uFR6320K+VP-VPR6530.1KR6230.1KJP8564-VPR60100KNOTCHFREQUENCYSETTING+-11IC8BTL084712134+-11-VPJP912345IC8DTL08414JP1112OUT2GNDGND9V BATTERYPOWER IN +-15Viso+L110uH2 20mAI X101 2 3 4C41+22uFISOLATEDSIDEIC7ISO107A+C560.1uFC590.1uFR50R521M10.5K+5VisoJ61 2J71 2C61.01uFC6210uF+ C36++1uF327 1+-4 5245245IC12C45.01uFIC9LF441AIC11CAP+CAP-VOUTCAP+CAP-VOUT6LVOSCV+GNDLVOSCV+GND67836783OUTPUT<strong>OF</strong>FSETADJUSTIR591KC47.01uF32+VP411+-IC8ATL0841R6420KJP7JUMPERJUMPERC521uF+VP+VPJP1050/60 Hz NOTCH12POWERCM2NCGN1VINCM1SNC-V2+V2ENBC43.01uFJP1532C54.47uFC57.47uF31 3029I1LM79L05ACZIC13201918172 3IN OUTC5510uF4-IC8CTL0848+R55C351uFNC+V1NC-V1CM2VO SYNGN2131415165.36KICL7660CPAICL7660CPAR5710KOUT1IFigure 8.19 The demodulated voltage signal detected by the general-purpose impedance plethysmograph is galvanically isolated fromrecording instruments via isolation amplifier IC7. A notch filter built around IC8 filters power line interference. IC7 also generates isolated15 V, which is regulated to 5 V to power the 50-kHz oscillator, constant-current source, and synchronous demodulator. Alternatively, a9-V battery powers these circuits via 5-V linear regulator IC10. If a battery is used, 5 V is generated using voltage pumps IC11 and IC12.399
400 CARDIAC PACING <strong>AND</strong> DEFIBRILLATIONR6620K 1%R6720K 1%-5VisoR6810K 1%R6920K 1%VTOI_1R70IC14ATL08220K 1% 3+24-C63.01uFI1D81N4148654-+IC14BTL0827Absolute-ValueOutJP1912R7115K8C64D91N4148R726.2K8I+5Viso.01uFIIIFigure 8.20 A precision full-wave rectifier built around IC14A is available for testing the general-purpose impedance plethysmograph. Itprovides the absolute value of the voltage generated by the current source across the current-injection electrodes.ejection, relaxation, and passive filling) and allow estimation of the heart’s contractile state(inotropy). Areas under the PV loop are related to cardiac work, and thus heart efficiencycan also be calculated. Finally, the shape of the PV loop can be analyzed to assess valvularfunction as well as the coupling between the ventricles and the arterial load.INTRACARDIAC IMPEDANCE SENSORImpedance sensors for use as hemodynamic sensors in implantable pacemakers don’t needto be as accurate as those used for the generation of PV loops. Relative rather than absoluteindications of volumes are usually sufficient. As such, impedance sensors used in pacemakersoften make certain assumptions that simplify the volume-estimation problem at theexpense of precision. The circuit represented in Figure 8.22 is a simple, yet highly effectiveimpedance sensor suitable for implantable cardiac stimulators. This technique is known ascompensated capacitor discharge (CCD) impedance sensing [Prutchi, 1996]. It makes useof very small energy probe pulses (orders of magnitude subthreshold) to estimate the resistivecomponent of the lead impedance. The output of the circuit is an analog voltage proportionalto the lead impedance.In its simplest form, the circuit comprises a first capacitor, C a (e.g., 0.01 µF), referredto as the active capacitor. At the beginning of each impedance measurement cycle, C a ischarged to a preselected voltage level V src (e.g., 1 V). At the same time, a capacitor C p(of the same value as C a ), referred to as the passive capacitor or presample capacitor, isdischarged to 0 V. After C a is fully charged to V src and C p is fully discharged, a switch connectsC p to the body, allowing it to sample the potential across the lead system and adc-blocking capacitor C b (e.g., 1 µF) for a brief interval t CCD (e.g., 10 µs). The voltage
INTRACARDIAC IMPEDANCE SENSOR 401Left ventricle
402 CARDIAC PACING <strong>AND</strong> DEFIBRILLATIONVsrcRleadS1CHRHsRHPS3OUTS/H+CaCdc_blockLEADRionicRtissue(Cardiac, etc)-CpS4S5RpassViegmS/HS2HEARTVnoiseS1Switch ClosedSwitch OpenS2Switch ClosedS3S4S5Switch OpenTCCD = 10µsTCCD = 10µsS/HSampleHoldFigure 8.22 The CCD impedance sensor for implantable cardiac stimulators: (a) simplified circuit diagram of the sensor; (b) simplifiedtiming diagram. At the beginning of each measurement cycle, C a is charged to V src while C p is discharged. C p is then connected to the body,allowing it to sample the potential across the lead system for a brief interval t CCD . Immediately thereafter, C a is discharged across the leadsystem for the same amount of time t CCD . The subtraction of V Cp from V Ca is a value proportional to the tissue impedance,t CCDR C a ln{[V Ca (t CCD ) V Cp (t CCD )]/V src }In reality, however, other sources in the circuit (e.g., intrinsic electrical activity of the heart,electrode polarization potentials) have a strong effect on V Ca (t) and make the measurementof R imprecise.By using the voltage sampled in C p , the effects of these sources of error can be canceled.This compensation process is carried out by subtracting V Cp from V Ca before determiningthe resistive component R of the impedance:R tC a ln{[V Ca (t) V Cp (t)]/V src }
INTRACARDIAC IMPEDANCE SENSOR 403At the end of the measurement cycle, a switch is closed for interval t ACTD to discharge thedc-blocking capacitor and the capacitance at the electrode interface. After this switch isopened, a fairly high value resistor, Rpas (e.g., 100 kΩ), completes the “passive” dischargeof these capacitances. The charge movement during both active and passive dischargecauses balancing of the injected charge, resulting in a net-zero charge flow through the tissuefor each measurement cycle.Improved performance over the CCD technique is possible by modifying the impedancemeasurementcircuit configuration as shown in Figure 8.23. Here, a first capacitor C a1 (e.g.,0.01 µF), referred to as the first active capacitor, is charged through switch S1 to a preselected+VsrcS1S3OUTS/H+CaCdc_blockLEAD-Ca2S4S/HS2HEART-VsrcS1S2S3S4S/HFigure 8.23 Improved performance over the CCD technique can be achieved by using two opposing-polarity current injections per measurementcycle: (a) simplified circuit diagram of the sensor; (b) simplified timing diagram. C a1 is charged to V src and C a2 to V src . These capacitorsare then discharged in sequence. The discharge of both capacitors in reverse polarity through the tissue cancels sources of error andyields twice the amount of signal as the circuit of Figure 8.22. The impedance is then given byR t CCDC a ln{[V Ca1 (t CCD ) V Ca2 (t CCD )]/2V src }
404 CARDIAC PACING <strong>AND</strong> DEFIBRILLATIONvoltage level V src (e.g., 1 V). At the same time, a capacitor C a2 (of the same value as C a1 ),referred to as the second active capacitor, is charged through switch S2 to the negative of thevoltage level V src (e.g., 1V).After C a1 is fully charged to V src and C a2 is fully charged to V src , a switch (S3) connectsC a1 to the body, allowing it to discharge through the lead system and a dc-blockingcapacitor C dc block (e.g., 1 µF) for a brief interval t CCD (e.g., 10 µs). Immediately thereafter,C a2 is discharged across the lead system by closing a switch (S4) for the same amount oftime that C a1 was discharged. With no other sources in the circuit, the voltage on eachactive capacitor decays exponentially according toV Ca(i) V src e t/RC a(i)where V Ca(i) is the voltage remaining on active capacitor i after a time t, V src the initial voltageof the active capacitor, R the lumped resistance of the circuit, and C a(i) the capacitanceof the active capacitor i. The resistance of the circuit to the narrow pulse would then bedetermined fromR As explained above, however, other sources in the circuit (e.g., the intracardiac electrogram,electrode polarization potentials) have a strong effect on V Ca(i) (t) and make measurementof R imprecise.By using the discharge of both capacitors, which happens in reverse polarity throughthe tissue, the effects of these sources of error are virtually canceled. This compensationprocess is carried out by subtracting V Ca1 from V Ca2 before determining the resistive componentR of the impedance:R tC a(i) ln[V Ca(i) (t)/V src ]tC a ln{[V Ca1 (t) V Ca2 (t)]/2V src }Since the discharge polarity through the body is reversed for each phase, the subtractionof capacitor voltages results in twice the voltage signal while canceling interferingsignals:V Ca1 (t) V Ca2 (t) voltage decay on a capacitor of size C a due to discharge through theresistive path effect of interference sources on a capacitor of size C a (voltage decay on a capacitor of size C a due to discharge throughthe resistive path effect of interference sources on a capacitor ofsize C a ) 2(voltage decay on a capacitor of size C a due to discharge through theresistive path)Active discharge is not needed at the end of the measurement cycle. The charge injectedby each phase is substantially similar but in the opposite direction. This results in thedesired net-zero charge flow through the tissue for each measurement cycle.Also at the end of the measurement cycle, the voltage difference between the capacitorsis measured and sampled via a sample-and-hold circuit. Figure 8.24 is an actual dualopposing capacitor discharge (DOCD) prototype circuit. The core circuit of the sensor ispresented in Figure 8.25. In it, capacitor C a1 (C39) is charged to 1.2 V through switchIC9D and current-limiting resistor R11. At the same time, C a2 (C47) is charged to 1.2 Vthrough IC9A. The ground path during this process is established through IC9C. All other
INTRACARDIAC IMPEDANCE SENSOR 405Figure 8.24 This sensor circuit generates low-energy capacitive-discharge pulses to measure twoterminalimpedance across electrodes implanted in the heart. An ISO107 isolation amplifier is usedfor galvanic isolation of the applied part from external signal acquisition equipment.switches are open during the charging of C a1 and C a2 . This is the normal state of the statemachine implemented by the microcontroller (IC12) of Figure 8.26.When an impedance measurement is to be performed, the external data acquisition systemgenerates an interrupt that is received through line IMPED_START on the statemachinemicrocontroller IC12. Switches IC9D, IC9C, and IC9A are opened. Almostsimultaneously, IC10C connects the reference terminal of the capacitors to one of theleads. Then, the other lead is connected to C a1 through IC10D and dc-blocking capacitorC48. The discharge of C a1 through the body–lead system is sampled for 10 µs. IC10D isthen opened, and C a2 is allowed to discharge through the lead system for 10 µs by way ofIC10A, C48, and IC10C.After the samples are taken, IC10C is opened to float the lead system in relationship tothe system ground. (Optionally, IC10B is closed to discharge the dc-blocking capacitoractively for 768 µs. This was left in the circuit to make it possible to implement CCDmeasurements.) IC9C is closed and the differential signal corresponding to the compensatedimpedance measurement is developed by IC8A, IC8D (unity-gain buffers, used onlyto preserve the charge on the active capacitors), and instrumentation amplifier IC11. At theend of 768 µs, the sample-and-hold implemented through IC9B, C44, and IC8B holds thevoltage level corresponding to the impedance measurement. This level is then scaled andfiltered through IC8C and its associated components.The circuit of Figure 8.27 isolates sensor signals from recording instruments connectedto the sensor. This circuit also generates isolated power for the applied part of the intracardiacimpedance sensor. With the component values shown, the circuit produces an outputvoltage as a function of impedance (resistance) as shown in the graph of Figure 8.28.It should be noted that other implementations of the same circuit, which are particularlyefficient for use in implantable medical devices, are possible, as shown in Figure 8.29.
406 CARDIAC PACING <strong>AND</strong> DEFIBRILLATIONFigure 8.25 Circuit for the dual opposing capacitor discharge intracardiac impedance sensor core. C a1 (C39) is charged to 1.2 V throughIC9D and C a2 (C47) is charged to 1.2 V through IC9A with ground established through IC9C. IC9D, IC9C, and IC9A then open whileIC10C connects the reference terminal C39 and C47 to one of the intracardiac electrodes. C a1 discharges into the heart through IC10D andC48 for 10 µs. C a2 then discharges for 10 µs by way of IC10A, C48, and IC10C. IC10C is then opened and IC9C is closed. The differentialcompensated impedance measurement is generated by instrumentation amplifier IC11. A sample-and-hold circuit (IC9B, C44, and IC8B)holds the measurement. The impedance signal is scaled and filtered by IC8C.Here most of the active signal-processing circuitry (buffers and differential amplifier) arereplaced by a switched-capacitor differential to a single-ended converter, which also actsas a sample-and-hold circuit.Figure 8.30 shows some impedance signals obtained through an instrument that usesthe sensor circuit of Figure 8.24. These signals were acquired from a human subject usingthe electrode configuration shown in Figure 8.30b. Theoretical and experimental studies[Hoekstein and Inbar, 1994] have shown that the largest contributor to the impedance signaldetected through pacing electrodes is the near-field movement of the cardiac walls inthe largely inhomogeneous field around the distal electrode.
VENTRICULAR TACHYARRHYTHMIAS 407Timer 0 TimeoutMainTake aMeasurementFigure 8.26 Timing of the various events of the intracardiac impedance sensor is performed by astate machine that runs on microcontroller IC12. The interrupt that causes a measurement cycle tostart can be received from an external source (JP9) or from an internal clock programmed at 300 Hz.TRANSCUTANEOUS PACINGCardiac pacing can be achieved by delivering pacing currents through skin-surface electrodes.Transcutaneous external cardiac pacing (TEP) [Bocka, 1989] is used as a temporarylife-support measure in patients with symptomatic bradycardia and a pulse, but has shownlittle benefit in pulseless situations. Common TEP pulse durations are between 20 and40 ms, and pacing currents are in the range 50 to 200 mA. TEP is limited in practice to stimulatingthe ventricles, since higher currents are required to stimulate the atria, making itdifficult (impossible, really, under clinical circumstances) to pace the chambers selectively.Pain and discomfort are the limiting factors to TEP use. A current of 100 mA appliedinto an average impedance of 50 Ω for 20 ms will deliver 0.1 J of energy. This is well belowthe 1 to 2 J required to cause severe pain sensation at the skin using electrode pads with alarge surface area (e.g., 100 cm 2 ). However, the force of skeletal muscle contraction is whatleads to TEP discomfort. Placing electrodes over areas of least skeletal muscle can minimizediscomfort. Placement is generally best in the midline chest and just below the leftscapula. Sedation is often used to control discomfort.You may be thinking about the way in which magnetic stimulation is much less uncomfortablethan electrical stimulation of the brain (see Chapter 7). Pulsed magnetic cardiacpacing has been proposed [Irwin et al., 1970]. Unfortunately, however, much more energyis required to pace the heart than to stimulate a few neurons. The magnetic field energythresholds for cardiac pacing are in the range 30 to 100 kJ. Don’t know about you, but wetake cover before we fire the 2-kJ magnetic stimulator that we presented in Chapter 7.The design of a pulser that can put out 100-kJ fields once a second is certainly not a trivialmatter. All that hassle and the discomfort problem will probably not even go away sinceskeletal muscle will probably be stimulated along the way.VENTRICULAR TACHYARRHYTHMIASVentricular arrhythmias are a major cause of cardiovascular mortality. Therapy forserious ventricular arrhythmias has evolved over the past decade, from treatment with
IMPED_OUTGND PWR+ C3522uF+ C3922uFL2330uH85mAL3330uH85mAGND SIG323130 29201918171 2 3 4 131415 16+C3822uFIC8ISO107AR171.5K+ C3410uFL110uH 220mA-12V_NON_ISOC331uf, tant.+C41 0.33uF+12V_NON_ISO+ C321uf, tant.NON ISO GNDInput Power-12V INGROUND+12V INJP5123NC+V1NC-V1CM2VOSYNGN2NCGN1VINCM1-V2SNC+V2ENBC37+22uFGND PWR+12V_NON_ISOC42.01uFSignal OutputJP612IMPED OUTGROUNDISOLATION BARRIERMAINTAIN 0.3" AIR CLEARANCE<strong>AND</strong> 0.5" CREEPAGER185.36KC430.1uFIC9ATL082A328+-4NON ISO GND1C44.01uFISOLATEDSIDENON-ISOLATEDSIDE-12V_NON_ISONON ISO GNDNON ISO GNDFigure 8.27 Impedance signals detected by the applied part of the intracardiac impedance sensor are galvanically isolated by IC8 from signalacquisition equipment that would be connected to JP6. A medical-grade 12-V power supply powers the sensor. Isolated power for theapplied part is generated by IC8.C36.01uFC40.01uF+12V_ISO-12V_ISO408
1.61.41.2Output Voltage10.80.60.4DVM Reading (V)0.200 500 1000 1500 2000 2500Decade Box Setting (Ω)Figure 8.28 The intracardiac impedance sensor produces an output voltage that follows this graph as a function of impedance (resistive).+VsrcS1OUTS3CouplingCDIFFS5Ca1S6LEADCa2S4HEARTS/HS2-VsrcFigure 8.29 Implementations of the same concept can be done in integrated circuits without the need for operational amplifiers throughthe use of a switched-capacitor differential to single-ended converter, which also acts as a sample-and-hold circuit.409
410Figure 8.30 Intracardiac impedance signals obtained through the sensor circuit of Figure 8.24: (a) these signals were acquired from ahuman subject, (b) impedance signals were collected with a bipolar pacing lead located in the right ventricle. The largest contributor to theimpedance signal detected through pacing electrodes is the near-field movement of the cardiac walls in the largely inhomogeneous fieldaround the distal electrode.
VENTRICULAR TACHYARRHYTHMIAS 411ImpedanceSensorPacemaker LeadDelivered TransvenouslySuperiorVenaCavaRightVentricleLeftVentricleProximal (“ring”)ElectrodeDistal (“tip”) Electrode(b)Figure 8.30 (Continued)antiarrhythmic drugs to implanted devices. Ventricular tachycardia, a condition thatoccurs in approximately 2 out of 10,000 people, is a potentially lethal arrhythmia thatoften causes the heart to become inefficient at pumping blood through the body.Ventricular rates of 160 to 240 beats/minute are usually considered to be the result of anonphysiologic tachycardia (i.e., a high rate that is not the result of the body’s metabolicdemand).Ventricular tachycardia can occur spontaneously. It can also develop as a complicationof a heart attack, cardiomyopathy, mitral valve prolapse, or myocarditis, and afterheart surgery. It may be a result of scar tissue formed after an earlier heart attack or asan undesired effect of antiarrhythmic drugs. It may be triggered by disrupted bloodchemistries (such as a low potassium level), pH (acid–base) changes, or insufficient oxygenation.AV nodal reentry tachycardia (AVNRT) is the most common form of paroxysmalsupraventricular tachycardia (PSVT, a tachycardia not directly of ventricular origin whichcomes in sudden attacks). Patients with this arrhythmia do not usually have other structuralproblems with their heart. PSVT originates in tissues near the AV node, which as we discussedearlier, is the electrical structure that transmits impulses between the atria and theventricles. Susceptible persons have two pathways that can conduct impulses to and from
412 CARDIAC PACING <strong>AND</strong> DEFIBRILLATIONthe AV node. Under certain circumstances, usually following a premature beat, these pathwayscan form an electrical circuit that allows an impulse to reenter the electrical pathwayrepeatedly. Each reentry leads to an impulse propagation to the ventricles, and thus a rapidheart beat.Wolff–Parkinson–White syndrome (WPW) is another tachyarrhythmia that does notoriginate directly in the ventricles. This type of arrhythmia involves an extra electricalpathway from the atria to the ventricles known as the accessory pathway. Under certaincircumstances, electrical impulses may be transmitted rapidly via this additional pathway,causing palpitations and dizziness. Other times, the pathway allows atrial impulses conductedto the ventricles to reenter and restimulate the atria, leading to a rapid arrhythmia.A real ventricular tachycardia (VT) is an arrhythmia that originates in the ventriculartissues. It is usually seen in patients who have damaged ventricular muscle, possibly as theresult of a heart attack or myocardial infarction. Ventricular scar tissue alters many localelectrical properties of the myocardium and sets up conditions favorable to the formationof local reentrant electrical circuits. When the reentrant circuit activates, it is capable ofdelivering rapid stimuli to the ventricles, leading to a rapid arrhythmia.Because the reentry time of the local circuit delivers stimuli faster than the heart’s naturalelectrical activity, it takes over the heart beat for the duration of the arrhythmia. VTmost often results in poor pumping of blood by the heart because the ventricular rate ishigh during the arrhythmia and because the activation sequence of the chamber does notfollow the normal pattern for efficient and effective pumping. VT often causes severe dropsin blood pressure, which leads to unconsciousness. In its most extreme form, ventriculartachycardia can be fatal, requiring immediate medical attention.If a critical number of reentrant loops appear, the arrhythmia degenerates into ventricularfibrillation (VF). Here, the ventricles depolarize repeatedly in an erratic, uncoordinatedmanner. The ECG in ventricular fibrillation shows random, apparently unrelated waves withno recognizable QRS complex. Ventricular fibrillation is often caused by drug toxicity, electrocution,drowning, and myocardial infarction. Ventricular fibrillation is almost invariablyfatal because the uncoordinated contractions of ventricular myocardium result in highlyineffective pumping and little or no blood flow to the body. VF is characterized by a lack ofpulse and pulse pressure and patients rapidly lose consciousness.For a patient to survive, VT and VF require prompt termination which can be accomplishedmost readily by the administration of an electrical shock passed across the chest.A normal rhythm can sometimes be restored through the defibrillation current because itstimulates each myocardial cell of the ventricles to depolarize simultaneously. Followingsynchronous repolarization of all ventricular cells, the SA node can once again assume therole of pacemaker, and the ventricular myocardial cells can resume the essentially simultaneousdepolarization of normal sinus rhythm.DEFIBRILLATIONVirtually all modern defibrillators store energy in capacitors, which are charged to a certainvoltage, depending on the energy needed. The defibrillation waveform is based on thedischarge of this capacitor, either with a wave-shaping inductor (damped sine waveform)or with a switching circuit that truncates the capacitor’s exponential decay (truncatedexponential waveform). Defibrillation waveforms are described by the number of phasesin the defibrillation waveform, the tilt of the defibrillation current, and the duration of thedefibrillation waveform.In a monophasic waveform, the polarity of the electrodes remains the same during theentire pulse, while biphasic waveforms are formed when the polarity of the electrodesreverses at some time during the pulse. Tilt is defined as the fractional reduction in the
DEFIBRILLATION 413stimulus waveform over the pulse duration. It describes how steeply the capacitor dischargesinto the patient’s body and gives an indication of how much of the stored energyis delivered to the tissues. Tilt is dependent on the RC time constant (device capacitancetimes the impedance of the transthoracic discharge pathway). Duration refers to the extentof the defibrillation waveform. Commonly, duration is in the range 8 to 40 ms.Bare-Bones DefibrillatorFigure 8.31 shows a damped sine waveform defibrillator. A transformer T1 steps up thepower line voltage to a high voltage (a few kilovolts). Capacitor C1 is charged throughrectifier D1, current-limiting resistor R1, and charge switch S1 to some voltage V (measuredthrough voltmeter M1) in order to store energy E 1 2 (C1)V 2 . When the defibrillationswitch S2 closes, the defibrillation current I flows through the inductor L1 and the patient,who has a transthoracic impedance of R patient . The discharge waveform depends on thevalues of C1, L1, and total impedance (R inductor R patient ). Note that the critical dampingresistance of the circuit is R critical 2L1/C1. Since defibrillators are commonly designedassuming that a patient impedance of 50 Ω, and if we assume an inductor impedanceR inductor of 10 Ω, a suitable R critical could be 67 Ω. The actual energy delivered to a patientdepends on patient impedance and is given byR entE delivered E C1 RpatientpatiR inductorFor this example, the discharge is underdamped (biphasic, also referred to as a Gurvichwaveform) when the patient resistance is less than about 56 Ω becauseR patient R inductor 56 Ω 10 Ω 66 Ω R critical 67 ΩIn this case, the waveform is underdamped and produces a biphasic (oscillating) waveform.If the patient impedance is higher than 67 Ω, the waveform is overdamped (monophasic,also referred to as an Edmark waveform). In this case the inductor slows the rate of riseD1R1S1DefibrillateL1 S2R. PatientRL1LineAC PowerNeutralT11 54 8C1VFigure 8.31 Simplified block diagram of a damped sine waveform defibrillator. Transformer T1 steps up the power line voltage to chargeC1 through rectifier D1, R1, and charge switch S1 to some voltage V (measured through voltmeter M1) in order to store energy E 1 2 (C1)V 2 .When the defibrillation switch S2 closes, the defibrillation current flows through L1 and the patient.
414 CARDIAC PACING <strong>AND</strong> DEFIBRILLATIONof the discharge current, reduces the maximum voltage applied to the patient, and shapesthe waveform to produce a damped sinusoidal waveform. The current delivered to thepatient gradually rises to a rounded peak and drops back to zero. The discharge currentpulse duration is about 2.5L1/C1, about 2.5 to 3.5 ms for most defibrillators.The circuit would produce an exponential waveform if the inductor L1 is eliminated.However, long-duration exponential-decay waveforms are unreliable for defibrillationbecause the low-amplitude long-duration currents at the end of the defibrillation waveformcould refibrillate the heart. If the exponential decay is truncated, however, defibrillationsuccess is markedly increased, with an efficacy approaching that of a damped sinusoidalwaveform defibrillator. Truncation allows larger-value capacitors to be used, which meansthat the needed energy can be stored at lower voltages. This makes it possible to use solidstatedevices in the switching circuitry.Truncated exponential waveforms are more sensitive to patient impedance changesthan to damped sinusoidal waveforms. In a typical truncated exponential waveformdefibrillator, current drops drops from about 27 A for a patient impedance of 50 Ω to 10 Afor a patient impedance of 150 Ω. For damped sinusoidal waveform defibrillators, the peakcurrent goes from about 60 A for a patient impedance of 50 Ω to 29 A if the patient impedanceincreases to 150 Ω. Considering that about 30 to 40 A is commonly necessary for successfuldefibrillation, both types of defibrillators are suitable for low- and medium-valuepatient impedances. However, damped sinusoidal waveform defibrillators are more effectivein defibrillating high-impedance patients.A simple, practical damped sinusoidal waveform defibrillator circuit is shown inFigure 8.32. This circuit is designed to deliver defibrillation energies of up to 320 J into a50-Ω load through a 5-ms Edmark (monophasic) waveform. When the power switch SW1is on, depressing and holding the charge pushbutton SW2 energizes the primary of highvoltagetransformer T1, a of 110 V to 3 kV current-limiting transformer rated at 150 mA.The high-voltage rectifier network formed by diodes D1–D4 charges capacitor C1through current-limiting resistor R1. Meter M1 measures the voltage across the energystorage capacitor. Its scale should be calibrated so that it provides an estimate of energy(in joules) delivered to the patient, assuming a load impedance of 50 Ω.Once C1 is charged to the desired voltage, defibrillation energy can be delivered tothe patient by pressing on pushbuttons SW3 and SW4 simultaneously. In commercialdefibrillators, the insulating handles for the paddle electrodes usually house one pushbuttoneach. This ensures that the physician administering the defibrillation shock is incontrol of the discharge and that the paddle electrodes do not become energized by accident.The debouncing circuit energized by SW3 and SW4 presents 12 V dc across thecoil terminals of relay K1, which is used to transfer the defibrillation charge from capacitorC1 to the patient. Charge from capacitor C1 is delivered to the patient via pulseshapinginductor L1 and DPDT high-voltage relay K1. A suitable choice for this relayis the Kilovac Products KM-14 DPDT gas-filled “patient” relay (about $600 in lowvolumes).A 5-kΩ resistor formed by R4 and R5 is connected across C1 via DPDT relay K2 duringthe discharge mode. The high value of this resistor has negligible effect when the pulseis being delivered to a patient. However, these resistors discharge the capacitor if thedefibrillation buttons are depressed without a suitable load across the paddle electrodes.The capacitor is also discharged if the defibrillator is powered down because SW1 is turnedoff, the power cord is unplugged, or because safety interlock switch SW5 opens (to protectmaintenance personnel from dangerous voltages when the instrument’s cabinet isopened). The leakage current through the meter circuit slowly dissipates the stored energyif the defibrillation pushbutton switches SW3 and SW4 are not depressed soon after capacitorC1 is charged.
SW5Safety InterlockF12AF20.25ASW1PowerDS1NE215110V3kV48R6100KT1T2110V-24V, 3A4 8Step-UpAC1AC2D1~D3SW2Charge+-SW3D2D4~46K335~R28M, 3W+~D12+C210uF, 30V12+ C2110VACDEFIBRILLATE!R120K, 20WSW4D5,1N4001AD9D11~+-D6,1N4001D10R612 Ohm, 1W~AC1K1KM-14R312 Ohm, 1WR42.5K, 10WR52.5K, 10WDumpK2KM-14L142mH, 5kV, 80ApkC135uF, 5kVHVShieldedWire(Coiled)IsulatingHandleHV ShieldedWire(Coiled)InsulatingHandlePaddleElectrode 1PaddleElectrode 21 5Paddle 1Paddle 2D7,1N4001-D8,1N4001250uF,50VAC1Figure 8.32 Schematic diagram of a damped sinusoidal waveform defibrillator capable of delivering energies of up to 320 J into a 50-Ωpatient load through a 5-ms Edmark (monophasic) waveform. Charge pushbutton SW2 energizes high-voltage transformer T1. C1 is chargedthrough the high-voltage rectifier network D1–D4 and R1. Meter M1 is calibrated to yield an estimate of energy (in joules) delivered to thepatient, assuming a load impedance of 50 Ω. Defibrillation energy is delivered to the patient by simultaneously pressing on pushbuttons SW3and SW4, which energize relay K1, which is used to transfer the defibrillation charge from capacitor C1 to the patient via pulse shapinginductor L1. R4 and R5 discharge C1 if the defibrillation buttons are depressed without a suitable load across the paddle electrodes or thedefibrillator is powered down.BLKWHI21PLUG AC MALEJ1GRN3415
416 CARDIAC PACING <strong>AND</strong> DEFIBRILLATIONImplantable Cardioverter DefibrillatorsThe father of the implantable defibrillator is widely recognized to be Michael Mirowski.His work on an implantable defibrillator began in the late 1960s after his friend and mentor,Harry Heller, died as a result of ventricular arrhythmia. His concept was to develop acompact defibrillator that could provide continuous rhythm monitoring and deliver appropriateelectrical shock therapy when necessary.The first successful human implant of a totally implantable defibrillator occurred in1980. Five years later the FDA approved the release of an implantable defibrillator for usein the United States. These early defibrillators were simple devices that would only deliverhigh-energy shocks to interrupt ventricular tachyarrhythmias. Much progress has beenmade since, and today, the implantable cardioverter–defibrillator (ICD) is the best therapyfor patients who have experienced an episode of ventricular fibrillation not accompaniedby an acute myocardial infarction or other transient or reversible cause. It is also superiortherapy in patients with sustained ventricular tachycardia causing syncope or hemodynamiccompromise.The implantable defibrillator is connected to leads positioned inside the heart or on itssurface. These leads are used to deliver the defibrillation shocks as well as to sense the cardiacrhythm and sometimes pace the heart, as needed. The various leads are tunneled to thedevice, which is implanted in a pouch beneath the skin of the chest or abdomen. They canbe installed through blood vessels, eliminating the need for open chest surgery. Modernimplantable cardioverter defibrillators have a volume of 30 to 40 cm 3 . Microprocessorbasedcircuitry within the device continuously analyzes the patient’s cardiac rhythm. Whenventricular tachycardia or fibrillation is detected, the device shocks the heart to restore normalrhythm. Defibrillators are also able to provide “overdrive pacing” to convert a sustainedventricular tachycardia electrically, and pacing if bradycardia occurs. Implantabledefibrillators are usually powered by internal lithium–silver vanadium oxide (Li/SVO) batteriescapable of delivering ampere-level currents needed when charging the high-voltagecapacitors.Implantable defibrillators usually generate biphasic truncated exponential decay waveforms,where a second phase of opposite polarity follows the first shock phase. Biphasicwaveforms are as effective as monophasic waveforms, but at lower energy and with fewerpostshock complications. The mechanism by which biphasic pulses reduce the thresholdvoltage is probably related to the first phase of a biphasic pulse not having to synchronizeas many cells, since the second phase removes the residual charge caused by the firstphase, which could otherwise reinitiate refibrillation. Besides lower energy requirements,biphasic shocks are not as traumatic to the heart as monophasic shocks.The optimal durations of the two phases are relatively independent of one another.Theoretically, the optimal first phase is identical to the optimal monophasic waveform—about 2.5 ms for a wide range of RC values. The optimal second-phase duration is basedon the membrane time constant (about 3 ms). Despite this, several studies have shown thatthe second phase should be shorter than the first phase. The second phase of some biphasicwaveforms is so short that it cannot reverse the transmembrane potential caused by thefirst phase, yet it greatly increases defibrillation efficacy. In these studies, as the secondphaseduration increased, the pulse defibrillated less and less effectively and had highervoltage requirements, which implies that the second phase should be as short as possible,yet long enough to return the transmembrane potential to a level close to the one thatexisted before the shock.A major difference between transthoracic (external) defibrillators (which apply currentsacross the chest from electrodes placed on the skin) and internal defibrillators (which applythe defibrillation currents directly to the myocardium) is the energy needed to cardiovertor defibrillate. Transthoracic defibrillation at 100 J is successful in half the cases, and
SHOCK BOX PROTOTYPE 417defibrillation on the order of 200 to 300 J is successful in 85% of the cases. A combinationof antiarrhythmic drugs and defibrillation has a 95% success rate. In contrast, internal defibrillationrequires far less energy. Depending on electrode configuration, energy requirementsfor defibrillation can be less than 5 J. Typical implantable defibrillators can delivera maximum of about 30 J per shock. Of course, the electrodes used for internal defibrillation,especially those used with implantable defibrillators, are different than the gelled paddlescommon for external defibrillators.Originally, open-chest surgery was required to implant the large, flat patch electrodesthat were sewn to the outer surface of the heart. However, the advent of the first transvenouslead systems in the early 1990s meant that physicians could maneuver the leads through avein into the heart, eliminating the need to open the chest. Today, most implantabledefibrillators use a single defibrillation lead. The defibrillator’s titanium can is implanted inthe upper chest, and it acts as the return electrode for the defibrillation current.SHOCK BOX PROTOTYPEModern implantable defibrillators are true marvels of microelectronic packaging. Figure 8.33shows the innards of one such device. This level of miniaturization is achieved using packagingtechnologies that are outside of the typical hobbyist’s budget. In fact, many startupcompanies developing implantable devices often chose not to pursue the technologiesrequired for miniaturization (e.g., custom ICs, chip-level packaging, ceramic substrates), andinstead, use off-the-shelf components and inexpensive manufacturing technologies (e.g.,surface-mounted components, low-power commercial ICs, printed circuit boards) so theycan invest their efforts into developing the technologies that differentiate them from the restof the pack. For this reason it is not easy to build an experimental implantable defibrillator.Instead, we chose to present the instrument of Figure 8.34 only as a demonstrator of the internalworkings of an implantable defibrillator. It shows the considerations included in implementationof the various modules of a shock box, the circuitry responsible for generatinghigh-voltage defibrillation pulses. This instrument does not include simulation of the parts ofan automatic defibrillator that are responsible for detecting ventricular arrhythmias.As shown in Figure 8.35, power for the circuit is obtained through a power line–operated medical-grade power supply. The 15-V line is used to power an isolated dc/dcconverter that yields isolated 30 V dc. The 30 V is used to operate a smart gel-cell batterycharger which charges two 12-V, 1.2-Ah gel-cell batteries in series. The battery powers themodule’s microcontroller constantly. Whenever the defibrillation module is enabled, thebattery is made to power a high-voltage power supply which charges the energy-storagecapacitor bank (165 µF) to a programmable level (up to 50 J).The level of charge to be stored in the capacitor bank is selected through a digital-toanalogconverter controlled by the microcontroller. The actual voltage across the capacitorbank is monitored by the microcontroller through an analog-to-digital converter whichsamples the voltage divider internal to the high-voltage power supply. Once charged to thedesired level, the defibrillation pulse is generated by commuting the capacitor bank ontothe defibrillation load through an H-bridge switch matrix. The switches in the H-bridge areunder the control of the microcontroller.Internal discharge of the capacitor bank is possible through a circuit that dumps storedcharge into a dummy load. This makes it possible to discharge capacitor banks after acapacitor reform procedure 1 as well as to disarm the defibrillation module after an aborted1The capacitance of electrolytic capacitors changes as a function of use and other factors. Whenever they are notused for some time, they require “reforming” such that they can be made to store the full desired charge.Reforming is accomplished by periodic charging of the capacitors to their full capacity.
418 CARDIAC PACING <strong>AND</strong> DEFIBRILLATIONFigure 8.33 Modern implantable defibrillators are true marvels of microelectronic packaging. Thelevel of miniaturization is achieved using advanced circuit integration and packaging technologies,such as custom ICs, chip-level packaging, and ceramic substrates.defibrillation. Voltage across the capacitor bank as well as the capacitor charge and dischargecurrents can be monitored using an oscilloscope or other data acquisition system byway of isolation amplifiers. The module is controlled by an onboard microcontroller. Itreceives parameter information and commands through an isolated RS232 line.Defibrillation commands are entered via a control computer.In addition to running the charge and defibrillate sequences, the microcontroller alsoperforms housekeeping functions (e.g., verify clocks, verify stored energy, perform capacitorreform). To ensure that the required energy has been stored in the capacitor bank priorto defibrillation, the microcontroller reads the voltage across the capacitor bank (using asuitable voltage divider) through an analog-to-digital converter. To enable emergency manualcharging and defibrillation (i.e., not through commands from the computer), isolatedpushbutton switches are available on the instrument. Whenever activated in the manualmode, the defibrillation module charges to the full energy selection, displays the chargestatus, and awaits for the manual command to defibrillate. Defibrillation in the manualmode is done at preset waveform parameters.
SHOCK BOX PROTOTYPE 419Figure 8.34 This prototype instrument is a demonstrator of the internal workings of an implantabledefibrillator. This circuit is capable of delivering defibrillation energies of up to 50 J to the heart. Thisenergy level is suitable when at least one of the electrodes is in direct contact with the ventricularmuscle.Lead impedance is estimated prior to delivery of a shock or under command from thecontrol computer. Inappropriate lead impedances cause the defibrillation command to beaborted since delivering high energies into inappropriately low loads can be dangerous,because the developed currents pose fire or explosion risks. The different modules of thecircuit are presented in the following sections. The interconnection between these modulestakes place as depicted in Figure 8.36.Power Supply SectionA Condor medical-grade (low-leakage, redundantly insulated) power supply is used to generate15 V dc for the defibrillation module. The power line is applied to the power supplyinput terminals through a medical-grade connector/switch/fuse/filter/voltage-selector module.The power supply has low leakage and a redundant isolation on the power transformer,and its linear regulator is capable of producing 15 V at 0.4 A.As shown in Figure 8.37, a Power Convertibles HB04U15D15Q (C&D Power Technologies)isolated dc/dc converter powers the battery charger circuitry. The isolation barrierof this converter is rated at 3000 V (continuous) and tested at 8000 V with a maximum60-Hz leakage of 2 µA. This dc/dc isolation rating is the main power line leakage barrierfor the applied part of the circuit. The output of the dc/dc converter is filtered through aMurata BNX002 filter block and a 470-µF capacitor (C22). A TIP42 transistor and a 33-Vzener diode are configured as an “amplified zener diode” to clamp the dc/dc output of thedc/dc converter at approximately 34 V.A single-chip gel-cell charge controller is used to charge two sealed, leakproof gel cellsin series. Charging of the two 12-V batteries is controlled through a Unitrode (now ownedby Texas Instruments) UC3906 IC, which implements an optimal-charge algorithm with
420 CARDIAC PACING <strong>AND</strong> DEFIBRILLATIONFigure 8.35 Block diagram of the 50-J defibrillator. Power is supplied by a medical-grade power supply. A current of 15 V from this supplyoperates a dc/dc converter to charge two 12-V gel-cell batteries. Battery power is supplied to the microcontroller constantly. The batteryis also used to power a high-voltage power supply which charges the energy-storage capacitor bank (165 µF) up to 50 J, as selected through aDAC. A defibrillation pulse is generated by commuting the capacitor bank onto the defibrillation load through an H-bridge switch matrix.Capacitor bank voltage and current can be monitored by way of isolation amplifiers. Parameter information and commands are entered via acontrol computer through isolated RS232 line. The instrument includes circuitry to measure load impedance without delivering shock currents.fast, float, and trickle-charge phases to charge the gel cells safely. Two Yuasa NP1.2-12batteries are connected in series to generate approximately 24 V for the high-voltage powersupply. Each battery has a nominal voltage of 12 V and a capacity of C 1.2 Ah.Lead–acid batteries with a gelled electrolyte are best kept charged and maintained by acharger at a float voltage of 2.25 to 2.3 V per cell. To obtain a full charge, the battery ischarged to about 2.4 V per cell. Therefore, the charger IC switches back to the float levelwhen necessary. Terminal voltages that exceed the float level place the battery in what isknown as the overcharge region. During fast charge, the charger limits the current to a safelevel known as the bulk rate and then tapers off to the overcharge region at about one-tenthof the bulk rate.
Figure 8.36 Interconnection diagram between the various modules of a shock-box instrument.421
Q17IRF9530+24V_SW+15V_NON_ISOGND NON ISO1IC182 3+VIN +VOUT-VINCOMM-VOUTHBO4U15D15 DC-DC Converter4512BPSGIC43BNX002CBCG43D1333V, 5WQ39TIP42R331.0IC19UC3906D12SCHOTTKY16Q19TIP 421512R106100K11R35100K+24_VBATTO BATTERYR104470KBATT_COMMQ18BS170R10510M+24V_ENABLEC22470uF, 50V1+IN2IC20DSA6U48S54+OUT3-IN-OUTSINK243579C/S -C/LC/S ++VINPWR INDOC INDC260.22uF14 1 8 6C270.1uFVOLT. SENSESTATE LEVEL CNTL1310R39100KR36385KR379.09KC2310uFC24.01uFC250.1uFR381MQ20IRF9530+5V+5SWCOMPC/S OUTOC TERMGNDSOURCECHRG ENABLET. BIAS+5V_ENABLEGNDFigure 8.37 An isolated dc/dc rated at 3 kV with a maximum 60-Hz leakage of a 2-µA converter powers the battery charger circuitry. Asingle-chip gel-cell charge controller IC (UC3906) charges two sealed 12-V batteries. Q4 switches power to the high-voltage power supplyfrom the 24-V battery. This switch is turned-on by Q5 upon receipt of the appropriate command from the shock-box microcontroller. IC9produces 5 V to run the microcontroller and associated logic.422
SHOCK BOX PROTOTYPE 423In operation, the UC3906 ensures that power is available from the dc/dc converter andthat the batteries are in a good state. Pin 5 monitors the supply voltage and enables the chipwhen at least 4.5 V is available. Pin 12 senses the battery terminal voltage. If the voltageis too low (indicative of a dead battery or reverse polarity), the charger is disabled.Upon detection of charging power and a good battery, the UC3906 puts two watchdogsto work: One regulates the charge current and the other looks at the battery terminal voltage.The current regulator (which uses Q19 as the power transistor) senses the voltage acrossseries resistor R33 and limits it to 0.25 V by controlling the charging current. Thus, the bulkcharging rate is determined solely by the value of this resistor. As such, the bulk chargingcurrent using a 1-Ω resistor is 250 mA. This current corresponds to a C/4.8 charging rate. Acurrent of 250 mA is also well within the 300-mA output range of the dc/dc converter.Battery terminal voltage sensed at pin 13 is compared to the IC’s internal referencevoltage. The actual terminal voltage is prescaled appropriately through R35 and R37. Theresistor divider values were selected such that when the critical voltage is reached, the voltageat pin 13 equals 2.3 V. At this point, pin 10 is latched and R36 no longer participatesin the circuit. When the terminal voltage rises to a level that is just below float, the voltageregulator takes control away from the bulk-current regulator and goes into the overchargestate. The current then tapers as the voltage continues to rise toward 2.4 V per cell, thepoint at which the float state is started.As the current tapers, the voltage across R33 drops. Another watchdog looks at thisvoltage to determine when it goes below 0.025 V. When 0.025 V is sensed, a latch is toggledand pin 10 ungrounded. Float conditions are established and the battery voltage driftsback to 2.3 V per cell, which is maintained until the battery becomes discharged or thepower is switched off and back on. A MOSFET (Q17) switches power to the high-voltagepower supply from the 24-V battery. This switch is turned on by Q18 upon receipt of theappropriate command from the shock-box microcontroller.High-Voltage Capacitor ChargerImplantable defibrillators typically use flyback converters to charge the energy-storagecapacitor bank. Crude feedback loops are used in these devices to control the charge level.Instead of designing a custom high-voltage converter, the shock-box prototype uses anOEM module designed specifically for charging capacitor banks: the Ultravolt model IC24-P30 programmable high-voltage power supply. The high-voltage charge section is shown inFigure 8.38. This module utilizes a dual-ended forward topology with a nominal switchingfrequency of 100 kHz. A soft-start circuit brings the converter to full power over a 1-msperiod. A constant-frequency PWM regulation system controls a MOSFET push-pull powerstage and HV transformer. The power stage is protected from output current overloads viaa secondary current limit circuit. The current limit is optimized for low-impedance capacitorcharging. HV ac is rectified and multiplied internally. The HV developed by this multipliergenerates feedback voltage which is sent to the control circuit to maintain regulation.The ac feedback network is configured for no overshoot into capacitive loads.The module has high efficiency (up to 92%) and requires 23 to 30 V dc to operate.The module will remain operational (derated performance) down to 9 V. The HV poweroutput is not isolated from the input. The module produces an output that is proportionalto the level presented to its control input. A voltage of 0 to 5 V at the input results in 0to 1 kV (at 30 W) at the output. The module also has a TTL-controlled enable function.When disabled, the module remains on standby mode at 30 mA.The module’s dimensions are 3.7 in. 1.5 in. 0.77 in. Although the specific moduleused in our prototype is encased in plastic, the same module is available in an RF-tight casewith a six-sided mu-metal shield. The module was originally selected by using the followingformula, used to calculate the rise time required to charge an external capacitor
424 CARDIAC PACING <strong>AND</strong> DEFIBRILLATIONJ1112345678UltraVolt, Model No: IC24-P30,Programmable High Voltage PowerSupplyIC371Power ReturnHV Output 211234567Power InI - SenseEnableSignal GndRemote Adj.+5V Ref.HV Output 1HV Return 2HV Return 11098UltraVolt IC24-P30Charge DumpJ13+5V 1GND 2Enable 34Disable2R871001323Q42BS170IC38Anode Out 1+Cathode Out 2-Out 2+PVI1050Out 1-8765R83100 Ohm, 10 WattR8910M1R107100 Ohm, 10 WattGDummyLoadQ35IXGH17NU12C3ER85R884, 1000k in series 4, 1000k in seriesC63250uF, 360VC64250uF, 360VR900.5 OhmR82400KD8LEDLS1AlarmD145.1VR841M, 500VR1081M, 500VR868KJ1512HighVoltageOut4V@1000 VinV_Cap_OutI_Cap_OutR9110023IC39Out 1-Anode Out 1+Cathode Out 2-Out 2+876521D101N4148Q36BS170HV Gnd21Q43BS170PVI1050R92470K33Figure 8.38 Photoflash electrolytic capacitors are the most commonly used capacitors in implantable defibrillators. Two Panasonic TS-HBseries330-µF capacitors at 450 V are used in the shock box for an equivalent capacitance of 165 µF at 900 V. The capacitors are charged in seriesdirectly from a programmable HV power supply. 400-kΩ bleeder resistors equalize the voltage across the capacitors during charging. A blinkingLED and a piezo buzzer are powered directly from the HV line to warn the user of the presence of high voltage in the capacitor bank.load (C L ) to 99% of the desired value:T(ms) V C LCint (µ F)I ( A) where C L 165 µF, C int 0.018 µF, V 820 V (for ~50 J), and I short 30 mA. As such, theworst-case charge time is just over 4 s (as long as the necessary power is available at thesupply input).shortEnergy Storage CapacitorPhotoflash electrolytic capacitors are the most commonly used capacitors in implantabledefibrillators. These capacitors have been tested thoroughly in the photoflash and strobe
SHOCK BOX PROTOTYPE 425markets and are considered to be very reliable. However, their capacitance changes as afunction of use and other factors. For this reason, whenever they are not used for some time,they require reforming such that they can be made to store the full desired charge. Reformingis accomplished by charging the capacitors to their full capacity periodically. Recently, highvoltagetantalum capacitors have been made available for use in defibrillators. These capacitorsdo not require reforming, and their charge acceptance remains more or less constantdespite its use. However, high-voltage tantalum capacitors are very expensive (a few hundreddollars each), and they are not available in the voltage and capacitance ratings necessary forour application.For the prototype, we used two Panasonic TS-HB-series 330-µF capacitors at 450 V inseries for an equivalent capacitance of 165 µF at 900 V. As shown in the Figure 8.38, thecapacitors are charged in series directly from the HV power supply. 400-kΩ bleeder resistorsare used to equalize the voltage across the capacitors during charging. In addition, a0.5-Ω resistor was added in the series connection to enable monitoring of the charge–discharge current. A circuit comprising a blinking LED and a piezo buzzer is powereddirectly from the HV line to warn the user (especially during experimentation with the circuit)that there is energy stored in the capacitor bank.Switching DevicesExternal defibrillators (which deliver up to 400 J) use high-voltage high-current relays toconnect the defibrillation load to the storage capacitor. Although they are simple to control,these devices are bulky and clearly unsuitable for an implantable device. A commonway of delivering stored energy to the load in implantable defibrillators is through insulatedgate bipolar transistors (IGBTs). Noteworthy properties of IGBTs are the ease ofvoltage control and the low losses at high voltages. These characteristics are similar tothose of MOSFETs. However, the effective ON resistance of IGBTs is significantly lowerthan that of MOSFETs.We selected the IXYS IXGH17N100U1 IGBT for the prototype circuit. A very similardevice in bare-die is used in commercially available implantable defibrillators. This devicefeatures a second-generation HDMOS process with very low V_CE(SAT) 3.5 V for minimumON-state conduction losses. The IXGH17N100U1 is rated for a V_CES of 1,000 Vat 34 A (or 64 A for 1 ms).The common practice in implantable devices is to drive the IGBTs (or MOSFETs)using pulse transformers and a driving circuit. For the sake of simplicity, however, this circuituses new photovoltaic optocouplers such as the International Rectifier PVI1050. Thesedevices generate their own dc current at the output, and as such, can be used to implementmuch simpler control circuits. Each PVI1050 has two photovoltaic cells driven from a singleLED source. Each photovoltaic cell produces a maximum of 8 V at 10 µA.As shown in Figure 8.39, the two photovoltaic cells inside each PVI1050 are wired inseries. Two PVI1050s (IC_Enable_1 and IC_Enable_2) are wired in parallel to charge theIGBT gate capacitance to the saturation voltage. R_Gate_Bleed_IGBT is used to passivelybleed charge accumulated at the gate (e.g., through the Miller effect) of the IGBT. Thisensures that the IGBT remains off until turned on by activating the photovoltaic isolators.Current for the LEDs of the photovoltaic isolators is switched under the control of thedefibrillation module microcontroller through a small switching FET. Since charge buildupwith constant light output takes some time, this instrument implements a technique toimprove the response time of the photovoltaic isolators [Prutchi and Norris, 2002]. Thecurrent is switched on through the LED through the Q_ENABLE line and is limited to asafe continuous level through the 39- and 4.7-Ω resistors. For a brief period (100 µs), however,a very strong current is sent through the LED by way of the Q_KICK line to boostthe output and yield an IGBT turn-on time of under 25 µs at full energy (full saturation).
426 CARDIAC PACING <strong>AND</strong> DEFIBRILLATION+5V+HV8765IC_Enable_1Out 1-Out 1+ AnodeOut 2- CathodeOut 2+PVI1050234.72CLoadIGBTG18765IC_Enable_2Out 1-Out 1+Out 2-Out 2+PVI1050AnodeCathode233913Q_Kick2KickE3R_Gate_Bleed_IGBT10M1Q_Disable213Q_Enable2Enable3 R_Gate_Bleed_FETIC_Disable8470kOut 1-72150Out 1+ AnodeDisable6Out 2- Cathode35Out 2+HV GndPVI1050Figure 8.39 Implantable defibrillators commonly use insulated-gate bipolar transistors (IGBTs) to switch defibrillation energy to the heart.In a shock-box circuit, photovoltaic optocouplers are used to control the IGBTs. The two photovoltaic cells inside each PVI1050 are wiredin series to produce up to 16 V. Two PVI1050s (U_Enable_1 and U_Enable_2) are wired in parallel to charge the IGBT gate capacitance tothe saturation voltage. R_Gate_Bleed_IGBT bleeds charge accumulated at the IGBT gate to ensure that it remains off until turned on by activatingthe photovoltaic isolators. Fast IGBT turn-off is accomplished by discharging the IGBT gate through a FET (Q_Disable).There is no need for further protection of the gate since the 10 MΩ loaded output of thephotovoltaic cells in series/parallel is approximately 24 V, and the allowed transientVGEM of the IGBT is 30 V. Fast IGBT turn-off is accomplished by discharging theIGBT gate through a FET (Q_DISABLE). This FET is actuated via a third photovoltaicisolator.As shown in Figure 8.39, a switching stage is available on the prototype to enable fastdump of stored energy into a 50-Ω load. This feature may be used to deliver sequentialshocks with decreasing energy (since the remaining energy of the previous shock may belarger than the energy desired for the succeeding shock) or to return the module to a safestate after aborting the delivery of a shock.As shown in Figure 8.40, an H-bridge switch configuration was used in the prototypeto generate biphasic waveforms onto the defibrillation load. Each switch acts as
Figure 8.40 A H-bridge switch configuration was used in the prototype to generate biphasic waveforms onto the defibrillation load. Eachswitch acts as an independent, floating solid-state relay. A 100-kΩ resistor across the bridge output is used to maintain stability of the bridge’sswitches by establishing a common-mode horizon whenever there is no defibrillation load connected to the output.427
428 CARDIAC PACING <strong>AND</strong> DEFIBRILLATIONFigure 8.41 Oscilloscope display of the voltage across a 50-Ω resistive load connected to the output of the H-bridge. The capacitor bankwas charged to approximately 90 V, and the circuit was made to generate a biphasic pulse with 5-ms-duration phases. The interphase intervalwas chosen arbitrarily to be 50 µs.an independent, floating solid-state relay. A 100 kΩ resistor across the bridge output isused to maintain stability of the bridge’s switches by establishing a common-mode horizonwhenever there is no defibrillation load connected to the output. It must be noted thatthe photovoltaic isolators are not used as part of the applied-part isolation (safety) barrier.Rather, they are used to simplify the driving circuitry for the H-bridge, since they act asfloating sources that establish a potential difference only across the gate–emitter of theirrelated IGBT.Figure 8.41 presents the oscilloscope display of the voltage across a 50-Ω resistiveload connected to the output of the H-bridge. For this figure the capacitor bank wascharged to approximately 90 V, and the circuit was made to generate a biphasic pulse with5-ms-duration phases. The interphase interval was arbitrarily chosen to be 50 µs.Isolation AmplifiersAs shown in Figure 8.42, an AD210AN isolation amplifier (IC29) is used to sample thevoltage across the capacitor bank (using the voltage divider formed by resistors R84 andR86 on the high-voltage capacitor charging circuit). A second AD210AN (IC35) samplesthe instantaneous capacitor charge–discharge current by sampling the voltage developedacross the 0.5-Ω current-measurement resistor (R90 on the high-voltage capacitor chargingcircuit). The output of the AD210s is made available through BNC connectors to makeit possible to sample and analyze the charge–discharge waveforms with an oscilloscope orother data acquisition system.
SHOCK BOX PROTOTYPE 429V_CAP_OUTR56RGR55RF161719181415IC29FB-IN+INICOM+VISS-VISSPWRPWR COMVOUTOUT COM+VOSS-VOSS1234J5BNCAD21030 29+15V_NON_ISOC4710uFC48.01uFDNon Iso GNI_CAP_OUTR103RGR102RF161719181415IC35FB-IN+INICOM+VISS-VISSPWRPWR COMKVOUTOUT COM+VOSS-VOSS1234J14BNCAD21030 29+15V_NON_ISOC6910uFC70.01uFNon Iso GNDFigure 8.42 An AD210AN isolation amplifier is used to sample the voltage across the capacitor bank (using the voltage divider formedby resistors R84 and R86 on the high-voltage capacitor charging circuit). A second AD210AN samples the instantaneous capacitorcharge–discharge current by sampling the voltage developed across the 0.5-Ω current-measurement resistor (R90 on the high-voltagecapacitor charging circuit).Control of the Shock BoxAs shown in Figure 8.43, a Microchip PIC 16C77 microcontroller (IC24) is the mainshock-box controller. A 32-kHz crystal-controlled clock operates the timers, and a 4-MHzcrystal-controlled clock runs processing upon wake-up. Correct clock operation is verifiedthrough an independent RC circuit (R42 and C31). This microcontroller is powered fromone of the module’s batteries through a 5-V regulator (IC20 on the battery-charging circuit)and will thus have constant supply of energy available for housekeeping of the moduleduring system power-downs.The microcontroller communicates with the programming GUI computer through aserial interface. A four-line RS232 protocol (TX/RX,RTS/CTS) protocol is implemented
P1DB9-M+5V+15V_NON_ISO+5V2IC21A74HC141R4010K43IC22C1E1+15V DETECTA1K112R411.5KDual color LEDR451KD5D64MHZY2RED LEDGREEN LEDDUMP_DISABLE+24V_ENABLEDUMP_ENABLECHARGE_ENABLE+5VA/D_CS_1R46R48R47R491KA/D_CS_21K1K1KC32 C33IC25IC28AD/A_CS0.01uF10uF74HC14C284.7uFD7 RED LEDIC28BKICK_1KICK_2ENABLE_1ENABLE_2DISABLE_1DISABLE_2MAN_DEFIBMAN_CHARGE123A1K1A24 5K2 E2PS2501-2C1E1C28763 474HC14TXCTSRXRTS145111012915IC26C1+VCC3 2C1- V+6V-C2+C2-TTL IN1TTL IN2TTL OUT1TTL OUT2GNDMAX232A1IC23LM78L05ACZVIN2RS-231 OUT1RS-232 OUT 2RS-232 IN 1RS-232 IN 216147138VOUT3GNDC3615pFC3715pFR4210MC31100nF32.768KHZY3C3833pFC3933pFR4333KIC24140MCLRRB7239RA0/ANORB6338RA1/AN1RB5437RA2/AN2RB4536RA3/AN3/VrefRB3635RA4/TOCKIRB2734RA5/SS/AN4RB1833RE0/RD/AN5RBO/INT932RE1/WR/AN6VDD21031RE2/CS/AN7VSS21130VDD1RD7/PSP71229VSS1RD6/PSP61328OSC1/CLKINRD5/PSP51427OSC2/CLKOUT RD4/PSP41526RC0/T1OSO/T1CKI RC7/RX/DT1625RC1/T1OS1/CCP2 RC6/TX/CK1724RC2/CCP1RC5/SDO1823RC3/SCK/SCL RC4/SDI/SDA1922RD0/PSP0RD3/PSP320 21RD1/PSP1 RD2/PSP2PIC16C77SCLKSDINSDOUT+5V_ENABLERXRTS64IC21CSWITCH_CHARGESWITCH_RESETTXIC21B74HC14CTS74HC1425R501K313Q21BS1702+5V+12V_BAT13R511KQ22BS1708765PS2501-1IC27C1E1C2E2PS2501-2A1K1A2K2+5V_NON_ISOR521.5K1234+15V_NON_ISOR531.5K131 21Q23BS1702Q24BS1702+15V_NON_ISOC40 0.1uFC42 0.1uFC29.01uFNon Iso Gnd+5V_NON_ISOC430.1uF+5V_NON_ISOC410.1uFC44C300.1uF0.1uFNon Iso GndIMPED_START3Non Iso GndR441K+5VC3510 uF594837261Figure 8.43 A PIC 16C77 is the main shock-box controller. A 32-kHz crystal-controlled clock operates the timers, and a 4-MHz crystalcontrolledclock runs processing upon wake-up. Communications with the computer is done through through an isolated four-line RS232protocol. Proper RS232 levels are generated through a TTL-to-RS232 interface chip. A dual-color LED (D5/D6) indicates the state of thehigh-voltage capacitor charge. LED D7 warns of lead-impedance overrange conditions.C34.01u F430
SHOCK BOX PROTOTYPE 431onboard the PIC. The lines are optically isolated by way of IC25 and IC27. The LEDs inthe optoisolators are driven by FETs Q21, Q22, Q23, and Q24. The optoisolator outputsare buffered and inverted through IC21B, IC21C, IC28A, and IC28B. Proper RS232 levelsare generated through a TTL-to-RS232 interface chip (IC26). The circuit connected tothe programming GUI computer is powered by 5 V derived from the 15-V Condorpower supply through linear regulator IC23.The shock-box controller knows the state of the power line through optoisolator IC22.The LED in this optoisolator is powered from the 15-V output of the Condor power supplythrough resistor R41. The output of the optoisolator is conditioned and inverted byIC21A and fed to the PIC through pin 5. A dual-color LED (D5/D6) controlled from pins3 and 4 of the PIC is used as an indicator of the high-voltage capacitor charge state (red,charging; green, ready to defibrillate; red blinking, charge fault). A red LED (D7) interfacedto pin 7 of the PIC is used to indicate a lead-impedance overrange condition.D/A and A/D ConvertersThe PIC communicates with two D/A converters (one to measure impedance, the other tomeasure the level of high-voltage charge) and a D/A converter (used to determine the setpoint for the high-voltage power supply) through a SPI serial interface (pins 18, 23, and 24).Chip enables to address these converters are generated through pins 8, 9, and 10. As shownin Figure 8.44, a LTC1451 D/A converter (IC33) is interfaced to the shock-box microcontrollervia a three-line serial (SPI) bus ( enable). IC33 is operated with its internal reference.The maximum of 4.096 V output from this D/A limits the voltage output of the HV powersupply to approximately 860 V, preventing accidental overcharge of the capacitor bank.IC33 is powered through the switched 5-V (isolated) line. For this reason, the enableline is controlled through a FET used as an isolation mechanism between the converter ICand the microcontroller. Two MAX187 A/D converters (IC30, IC31) are interfaced to theshock-box microcontroller via serial (SPI) bus ( separate enables) to measure the voltageacross the capacitor bank as well as the analog output of the impedance measurement circuit.The converters use their internal references and are powered through the switched 5-V(isolated) line. For this reason, the enable lines are controlled through FETs (Q25 and Q26),which are used as isolation mechanisms between the converter ICs and the microcontroller.Isolated Manual-Mode PushbuttonsA photovoltaic isolator powered from the module’s battery in a pulsed regime is controlledby the microcontroller to generate an isolated supply to power the LEDs of optoisolatorscontrolled by the manual defibrillation control switches. This is done to maintain full isolationof the manual-control switches from the applied part, yet still be able to operate themodule in manual mode whenever the main power line fails. As shown in the circuit ofFigure 8.45, photovoltaic isolator IC40 charges two 10-µF capacitors in parallel. Whenpower is first applied to the shock-box circuit, charging occurs for 4 s. From that point, thecapacitors are topped off every 10 s through a 1-s pulse. The series diode prevents the capacitorsfrom being discharged through the relatively high dark leakage current of the photovoltaicisolator during the no-charge periods.Whenever one of the switches (SW1 or SW2) is pressed, the energy stored in the capacitorsis used to pulse the LED of the photocoupler (in IC42) associated with the switchdepressed. Activation of the photocoupler is conditioned through the associated inverter/buffer (IC21D or IC21E) and latched by the associated flip-flop (IC41A or IC41B). Uponwake-up, the shock-box microcontroller reads the status of the latches. If a switch closure isfound, the microcontroller begins the behavior requested (i.e., charge to 50 J or defibrillate),recharges the isolated 10-µF capacitors for 4 s, and then resets the latches (IC41A and IC41B).
432 CARDIAC PACING <strong>AND</strong> DEFIBRILLATION+5SWV_CAP_OUTC45.01uFIC301VDD SCLK82AIN CS73SHDN DOUT64REF GND51R54100K2Q25BS170A/D_CS_1C464.7uFMAX1873SDINSCLKV_IMPED_OUTC49.01uFC504.7uFIC311VDD SCLK8234AINSHDNREFCSDOUTGND765MAX18713R57100KQ26BS1702A/D_CS_2SDOUTIC331CLK VCC82DIN VOUT73CS/LD REF64DOUT GND5C57.01uFR101100KHV_ADJUSTLTC14511Q38BS1702D/A_CS3Figure 8.44 The PIC communicates with two A/D converters (one to measure impedance, the other to measure the level of high-voltagecharge) and a D/A converter (used to determine the set point for the high-voltage power supply) through a SPI serial interface. The maximumof 4.096 V output from this D/A limits the voltage output of the HV power supply to approximately 860 V. Two MAX187 A/D convertersmeasure the voltage across the capacitor bank as well as the analog output of the impedance measurement circuit.Lead Impedance Measurement CircuitLead impedance measurements are made with the compensated capacitor discharge techniquedescribed earlier, which uses very small energy probe pulses to estimate the resistivecomponent of the lead system impedance. As explained before, the output of thecircuit is an analog voltage proportional to the lead impedance. Figure 8.46 presents theactual impedance measurement circuit implemented in the shock box. In it, the “active”capacitor C a (C15) is charged to 1.2 V through switch IC15A and current-limiting resistorR29. At the same time, the “passive” capacitor C p (C7) is discharged through IC15D. Theground path during this process is established through IC15C. All other switches are openduring the charging of C a and discharging of C p . This is the normal state of the statemachine.When an impedance measurement is to be performed, the shock-box microcontrollergenerates an interrupt (through line IMPED_START) to the impedance measurement
SHOCK BOX PROTOTYPE 433+12_VBATC7910uFC6810uFD171N41488765IC40Out 1-Out 1+ AnodeOut 2- CathodeOut 2+PVI1050231R94330Q37BS1702SWITCH_CHARGE3+5VFRONT PANELSW1CHARGESW2DEFIB.R97200IC421A123K1A24 5K2E2PS2501-2C1E1C2876R98100KR99100KIC21D9 874HC14IC21E11 1074HC14R95100K539116 IC41AD SQ1CLKR Q21401348 IC41BD S Q13CLKR Q1210 14013MAN_CHARGE*SWITCH_RESETMAN_DEFIBFigure 8.45 Manual control of the defibrillation is made possible through isolated front-panel pushbuttons. A photovoltaic isolator chargestwo 10-µF capacitors in parallel every 10 s through a 1-s pulse. Whenever one of the switches (SW1 or SW2) is pressed, the energy storedin the capacitors is used to pulse the LED of the photocoupler associated with the depressed switch, starting the behavior requested (i.e.,charge to 50 J or defibrillate).circuit’s state-machine microcontroller IC13. IC15D, IC15C, and IC15A are opened.Almost simultaneously, IC16C connects the reference terminal of the capacitors to one ofthe leads. Then the other lead is connected to C p through IC16D and dc-blocking capacitorC16. The effect of the body–lead system on a 0.1-µF capacitor is sampled for 10 µs.IC16D is then opened, and C a is allowed to discharge through the lead system for 10 µs byway of IC16A, C16, and IC16C.After the passive and active samples are taken, IC16C is opened to float the lead systemin relationship to the system ground. IC16B is closed to actively discharge the dc-blockingcapacitor for 768 µs. While active discharge takes place, IC15C is closed and the differentialsignal corresponding to the compensated impedance measurement is developed byIC14A, IC14D, and instrumentation amplifier IC17. At the end of the 768 µs, the sampleand-holdimplemented through IC15B, C12, and IC14B holds the voltage level correspondingto the impedance measurement. This level is then scaled and filtered throughIC14C and its associated components. Finally, the analog level is converted to a digital
434Figure 8.46 A lead impedance sensor measures the load impedance without using a high-voltage shock. This circuit used the “compensatedcapacitor discharge” sensing principle of Figure 8.22.
SHOCK BOX PROTOTYPE 435value by the corresponding A/D associated to the shock-box microcontroller. Impedancelimit values are determined within the shock-box microcontroller through a preloadedlookup table.To conserve power, the impedance-measurement circuit is powered only when necessary.This is done by supplying the circuit through a switch (MOSFET Q20 in the batterychargingcircuit) whenever deemed necessary by the shock-box controller (through the line5V_ENABLE). The input of the impedance measurement circuit is connected to thedefibrillation electrode terminals by way of a self-activated isolation circuit. A solid-stateswitching circuit that reacts to current flow protects both the impedance measurement circuitfrom defibrillation pulses as well as the patient from faults in the impedance measurementcircuit.Referring to the upper half of the circuit of Figure 8.47, the gates of FETs Q29 and Q30are held at a positive voltage in excess of the conduction threshold by the 5-V sourcethrough resistor R63. This allows impedance measurement to take place via these FETsand resistor R70. However, when a defibrillation pulse is applied, current increasesthrough R70 (shunted at the impedance measurement circuit by the back-to-back zenerdiodes), and depending on the polarity of the pulse, one of the bipolar transistors (Q7 orQ28) starts to conduct, placing its associated FET in the high-impedance state.The bipolar transistor remains conductive until the voltage drops below a safe level forthe impedance measurement circuit, at which time the low-impedance path is reestablishedthrough the FET. The lower portion of the circuit in the figure is essentially the same asthat described above. This portion is used to protect the second terminal of the impedancemeasurementcircuit from the high-voltage defibrillation pulses.Firmware for the Shock BoxThe embedded software source code listing includes comments, to make it easy to understandits operation. It is supplied in the book’s ftp site as SHOCKBOX.ZIP. The followingare short descriptions of the modules implemented by this software.GUI Command Processor This module processes commands sent by the programmingGUI computer to the shock-box microcontroller. There are 15 commands that can be sentby the programming GUI computer to the shock box via RS232. These commands are sentin frames with the following format:Command Number Data Count Data LSB Checksum MSB Checksumwhere Command Number is one of 15 possible commands (see the code for a list of commands)Data Count is the number of data bytes in the parameter data message to follow,Data the Parameter data, LSB Checksum the least-significant byte of the 16-bit checksum,and MSB Checksum the most-significant byte of the 16-bit checksum. Every time themodule executes an accepted command, it either echoes back the GUI command (wheneverdata are not expected back as a response for the command), or sends the commandnumber and the data expected with the same format as for GUI to shock-box communication(where the data are not a command parameter but rather, the response).Main Wake-up Module This module wakes the processor up every 250 ms. Upon wakeup,it does the following:1. Checks if front-panel switches (manual charge or manual defibrillate) have beenpressed.
436 CARDIAC PACING <strong>AND</strong> DEFIBRILLATION+5SWR6033KR6133KR6233KR6433KR6533KR6633KR63330KQ272N2222R671KR681KQ402N2222R69 10J71Q41MTP3N100ER7010Q30MTP3N100EJ81R7133KR7233KR7333KR7533KR7633KR7733KR74330KQ312N2222R781KR791KQ322N2222J91Q33MTP3N100ER80 10R8110Q34MTP3N100EFigure 8.47 The input of the impedance measurement circuit of Figure 8.46 is connected to the defibrillation electrode terminals byway of a self-activated isolation circuit. A solid-state switching circuit that reacts to current flow protects both the impedancemeasurement circuit from defibrillation pulses as well as the patient from faults in the impedance measurement circuit. The gates ofQ29 and Q30 are held at a positive voltage in excess of the conduction threshold by the 5-V source through resistor R63. This allowsimpedance measurement to take place via these FETs and resistor R70. However, when a defibrillation pulse is applied, currentincreases through R70, causing one of the bipolar transistors (Q7 or Q28) to conduct and place its associated FET in the high-impedancestate.J1012. If the switches are pressed, takes appropriate action, including:a. Initiates charge.b. Checks for completion of charge cycle.c. Awaits front-panel command to shock.d. Dumps remaining stored energy after shock.e. Informs GUI of charge due to manual request, and defibrillates due to manualrequest.f. Checks for GUI information requests.
CARDIAC FIBRILLATOR 4373. Every 1 s (every fourth 250-ms wake-up) this module performs the following actions:a. If a charge command has been issued, checks that once the desired charge hasbeen reached, charge is not maintained for more than 30 s, and if past, initiatescharge dump.b. Tests the lead impedance and sets the “check lead impedance” LED appropriately.c. Checks if ac power is available and turns peripheral power on constantly (if acpower is not available, peripherals such as the A/Ds, D/A, and impedance measurementcircuit are powered only when needed).4. Every minute, this module increments the reform counter, which keeps track of thetime elapsed since last capacitor reform.Lead Impedance Verification This module initiates lead impedance measurement andruns the A/D that reads the impedance sensor output. This function is initiated either manually(through a GUI request for lead impedance) or before defibrillation is delivered tothe load. A submodule drives the impedance-measurement A/D and takes eight readings(2.048 ms apart) and averages the measurements prior to using them to enable or disabledefibrillation as well as to communicate the impedance measurement to the GUI.Charge Control This software module enables the high-voltage power supply, establishesDAC output proportional to the desired stored energy level, and verifies successfulcompletion of the charge cycle.Deliver This software module runs a sequencer to turn the H-bridge switches on and offaccording to the defibrillation waveform desired. This module also initiates a lead impedancecheck prior to delivery.Assessment of Charge Delivered This module measures the remaining voltage on thecapacitor bank after shock delivery and communicates the measured value to the controlcomputer. Estimation of charge delivery is done by the control computer. A submoduletakes care of controlling the A/D that reads the voltage across the capacitor bank and averageseight readings.Reform This module keep tabs on the time elapsed since the last full-charge MANUALcharge (through front-panel control) or reform. If the time elapsed runs over 30 days, thismodule enables a full charge of the capacitor bank in order to reform. The module thendumps the charge into the dummy load after the reform operation.Verification of Correct Clock Operation This module verifies correct operation of thetiming mechanisms of the microcontroller. If a fault is found, the module deactivates automatically.Read Manual Switches This module takes care of charging the isolated capacitor usedto power the optocouplers that respond to the manual charge and manual defibrillationpushbutton commands.CARDIAC FIBRILLATORNo, it’s not a typo—a cardiac fibrillator is an instrument for electrical arrest of the actionof the heart. Deliberate cardiac arrest is frequently required during cardiac surgery after
438 CARDIAC PACING <strong>AND</strong> DEFIBRILLATIONarrangements are made for cardiopulmonary bypass. Cardiac paralysis allows a surgeonto perform delicate procedures on a quiet, motionless heart. A common way of causingelective cardiac arrest used to be by applying medium-frequency sine-wave stimulationthrough electrodes on the surface of the heart to bring about ventricular fibrillation, but thismethod is seldom used today. Instead, a potassium-salt solution is usually injected to stopthe heart intentionally (cardoplegia). When a patient is placed on the cardiopulmonarybypass machine, the heart and body are cooled to reduce the heart’s metabolic requirementsand oxygen consumption. The cardiplegia solution is then injected to cause cardiacstandstill and further reduce the heart’s oxygen consumption.When the surgery has been completed, the cardioplegic agents are flushed out of theheart with warm blood. The heart resumes contraction, and use of the heart–lung machineis discontinued. If normal contractions do not begin at once, a defibrillation shock is used.Temporary pacing leads (“heart wires”) are sometimes left stitched on the surface of theheart for connection to a temporary pacemaker, since it is not uncommon that the heartremains bradycardic until all pharmacologic agents are flushed out and normal metabolismis resumed. Chemical cardioplegia is preferred to fibrillation because the heart’s quiveringduring fibrillation wastes the heart muscle’s energy resources that are needed once beatingis resumed. Despite this, fibrillators are still used in animal research connected to thespecific mechanisms of fibrillation as well as in the assessment of defibrillation systems.Figure 8.48 shows a battery-powered fibrillator. The circuit uses a 555 timer IC to generatea 50-Hz square wave. This signal drives two sets of six paired CMOS buffers each.This output stage is actually a full bridge which causes doubling of the effective voltageacross the heart. Capacitors C2 and C4 block dc components on the output signal.Resistors R2 and R3 are used to protect the circuit against defibrillation currents. Since acertain current density threshold has to be exceeded to cause fibrillation, the fibrillatingcurrent and electrode surface contact area are proportional. Using pediatric-usedefibrillation paddle electrodes to fibrillate a pig’s heart typically requires 10 to 12 V at50 Hz. Using the outside surface of alligator clips as electrodes (which have a much lowercontact surface area) may take only 3 to 4 V.As simple as this circuit is, an even simpler battery-powered fibrillator is the most commonmethod for inducing fibrillation in the animal lab. Briefly touching the terminals of astandard 9-V battery to the ventricle (e.g., to the right-ventricular outflow tract) almostalways fibrillates the heart. Moral of the story: Don’t lick-test 9-V batteries laying aroundan electrophysiology lab.CONCLUDING REMARKSThere is much more to the design of active implantable medical devices (implants that relyfor their functioning on a source of electrical energy or any source of power other than thatgenerated directly by the human body or by gravity) than the short explanations anddemonstrations presented in this chapter. The European Union has published a directivethat regulates the level of performance and testing applicable to active implantable medicaldevices. This standard is:• EN-45502-1, Active Implantable Medical Devices—Part 1: General Requirementsfor Safety, Marking and Information to Be Provided by the Manufacturer, 1998As a specialized subset of the implantable devices field, cardiac pacemakers anddefibrillators have been around for quite a few years now. Their clinical success haveturned them almost into commodity items with standardized features. Regulators recognizethis fact and are trying to establish specific standards for the performance of thesedevices. Although at the time of this writing the relevant European standards are still in
CONCLUDING REMARKS 439+9VS1R1IC15CONTV OUT37DISCH42RESET6 TRIGTHOLD8V+GNDICM75551C10.47uF30.1K_______ 1f=1.4RC50Hz35181IC2A2CD4050BIC2B4IC3A13 28CD4049IC3B15 4BT19V BATTERY+9VD11N4148D21N4148R2100, 2WC24uF1J1798181CD4050BIC2C6CD4050BIC2D10CD40498IC3C17 6CD40498IC3D19 10C31nF+9VD31N4148D41N4148R3100, 2WC44uF1J21181CD4050BIC2E12CD40498IC3E111 121481CD4050BIC2F15CD40498IC3F114 158CD4050B8CD4049Figure 8.48 Schematic diagram of a battery-powered fibrillator. A 555 timer IC generates a 50-Hz square wave. This signal drives pairedCMOS buffers. This output stage is actually a full bridge which causes doubling of the effective voltage across the heart.draft form, they are very instructive as to the specific methods applied to the design andtesting of implantable pacemakers and defibrillators:• prEN-45502-2-1, Active Implantable Medical Devices—Part 2-1: ParticularRequirements for Active Implantable Medical Devices Intended to TreatBradyarrhythmia (Cardiac Pacemakers), Final Draft, January 2001• prEN-45502-2-2, Active Implantable Medical Devices—Part 2-2: ParticularRequirements for Active Implantable Medical Devices Intended to TreatTachyarrhythmia (Includes Implantable Defibrillators), 1998On the U.S. side, the FDA has not yet adopted a set of standards harmonized withEN-45502. Officially, the FDA still refers manufacturers to a guidance document writtenin the 1970s:• Donald F. Dahms, Implantable Pacemaker Testing Guidance, FDA FOD#383, postedJanuary 12, 1990, available at www.fda.gov/cdrh/ode/doc383.pdf
440 CARDIAC PACING <strong>AND</strong> DEFIBRILLATIONHowever, this document simply outlines the areas in which implantable pacemakersshould be tested (e.g., electrical characterization, interference, biocompatibility, animaltesting) so that they can be considered safe for human implant. This document does notprovide the specific performance requirements or testing methods available in the EN-45502 series of standards. This is not to say that the FDA doesn’t expect to see much, muchmore than what the guidance document sketches. Until a standard is adopted by FDA,however, it is up to the manufacturers to find ways of justifying the performance oftheir devices and to find ways of testing the devices for safety and effectiveness to satisfythe FDA.Nonimplantable pacemakers and defibrillators are also governed by particular standards:• IEC-601-2-31, Particular Requirements for the Safety of External Cardiac Pacemakerswith Internal Power Source, 1994, specifies the particular safety requirements forexternal pacemakers powered by an internal electrical power source. Applies also topatient cables but does not apply to equipment that can be connected directly or indirectlyto a power line.• IEC-601-2-4, Particular Requirements for the Safety of Cardiac Defibrillators andCardiac Defibrillator Monitors, 1983, specifies requirements for the safety of cardiacdefibrillators and cardiac defibrillator monitors incorporating a capacitive energystorage device.• ANSI/AAMI DF2, Cardiac Defibrillator Devices, 1989, provides minimum labeling,performance, and safety requirements for cardiac defibrillator devices. Requirementsfor performance cover energy range, limited energy output, energy accuracy, pulseshape and duration, controls and indicators, energy-level indicator, reduce-chargecapability, paddle electrode contact area, and other characteristics.• AAMI DF39, Automatic External and Remote Control Defibrillators, 1993, coverstesting and reporting performance results of automatic external defibrillators, primarilythrough description of the performance for the arrhythmia detection component.REFERENCESAAMI, AAMI/ANSI Standard HF18: Electrosurgical Devices, Annex B, 1994.Bocka, J. J., External Transcutaneous Pacemakers, Annals of Emergency Medicine, 18(12),1280–1286, 1989.Hoekstein, K. N., and G. F. Inbar, Cardiac Stroke Volume Estimation from Two Electrode ElectricalImpedance Measurements, EE Publication 911, Technion Institute of Technology, Haifa, Israel,1994.Irwin, D. D., S. Rush, R. Evering, E. Lepeschkin, D. B. Montgomery, and R. J. Weggel, Stimulationof Cardiac Muscle by a Time-Varying Magnetic Field, IEEE Transactions on Magnetics, 6(2),321–322, 1970.Prutchi, D., Rate Responsive Cardiac Pacemaker with Filtered Impedance Sensing and Method, U.S.patent 5,431,772, July 2, 1996.Prutchi, D., and M. Norris, Electro-optically Driven Solid State Relay System, U.S. patent6,335,538, January 1, 2002.
EPILOGUEOut of clutter, find simplicityfrom discord, find harmony.In the middle of difficulty lies opportunity.—Albert EinsteinThink you have a great idea for a new medical device? You’re not alone. Every year, manyphysicians and engineers try to develop their ideas and market them commercially. With aprototype in hand, you may be thinking about how to turn it into an actual product that canbe commercialized. As a first step, you may proceed to conduct some preliminary safetyand functional bench testing on your prototype device. Concurrently, you may invest a littletime visiting the library to research for possible patent infringement. Then you mayshow your prototype to a physician, who may help evaluate your idea by testing the devicein animals and human subjects. If all goes well, and testing shows that your idea wouldtruly constitute an advancement to medicine, you may be tempted to start investing in theinfrastructure, tools, and materials required to mass-produce and commercialize yourdevice. Well, don’t, at least not yet.REGULATORY PATHUnlike many other high-tech businesses, the medical devices industry is highly regulated.Especially in the United States the level of regulation is so extreme that compliance concernsoften outweigh all other technical and financial considerations. In fact, even if youcould build your device out of your own garage at a cost that you could afford to coverfrom your own pocket, the extensive clinical trials and lengthy submission process that areneeded to satisfy the Food and Drug Administration’s (FDA) requirements would probablymake the home-based venture completely nonfeasible. To give you an idea of theDesign and Development of Medical Electronic Instrumentation By David Prutchi and Michael NorrisISBN 0-471-67623-3 Copyright © 2005 John Wiley & Sons, Inc.441
442 EPILOGUEmagnitude of the issue, just consider that it is not uncommon for the costs connected to abare-bones clinical trial and submission for even a simple device to reach several milliondollars.The FDA reasons that these regulatory burdens are absolutely necessary to ensure thesafety and efficacy of a new medical device before it is used by the general population. Weagree. Although you may have a different opinion regarding the validity of thejustifications behind FDA’s strict policies, one thing is clear: The extensive clinical trials,complex submission requirements, and lengthy approval process require resources that arebeyond the budget of the average midnight engineer.We don’t mean to discourage you from pursuing your idea, but we want you to be awareof the unique characteristics of the biomedical startup. First, you will probably need to recruitresources from a specialized venture capital firm. There, investors will not only be interestedin the size of the market opportunity or the gross margin potential but will be looking for abusiness plan that includes detailed information regarding the following topics:1. Preliminary animal and clinical data which objectively demonstrate efficacy andcost-effectiveness of the device2. A clearly defined regulatory pathway that will secure regulatory approval ahead ofcompetitive technologies3. A comprehensive assessment of the risks posed by the proposed technology4. A strategic analysis of the market that will identify potential alliances with establishedcompanies that can help bring the product more quickly to market5. A financial plan for sustaining research, development, and day-to-day operations ofthe company for the duration of the clinical trials and submission processFDA CLASSIFICATIONSPrior to 1976, the FDA was limited to reacting to hazardous devices already on the marketand, then, only after patient injuries occurred. However, in 1976, Congress charteredthe FDA with enforcing the Federal Food, Drug, and Cosmetic (FD&C) Act, whichrequires that reasonable assurance of safety and effectiveness be demonstrated for medicaldevices intended for human use before being marketed to the public. Important amendmentsexpanding on the scope of this act were introduced in 1992 and 1997.The users of a device, usually physicians and patients, don’t necessarily have the expertiseand time required to evaluate independently the safety and effectiveness of each devicethey use. Because of this, the FDA requires the manufacturer of the device to demonstratesafety and effectiveness scientifically. At the FDA, “safe” means that the expected benefitsto the patient’s health for the intended use of the device outweigh probable risks of harm orinjury by the device. Effective means that the device has the clinical effect claimed by themanufacturer in a reliable manner.This last definition is especially important for the budding inventor, since the claim ofeffectiveness relates to clinical usefulness. It is not sufficient to demonstrate that the deviceaccomplishes some physiological effect, but it must provide some medical benefit. Once amanufacturer submits technical and scientific data that demonstrate safety andeffectiveness, the FDA conducts an independent review of all the information and makesdecisions about marketing and labeling approvals on the basis of these evaluations.Medical devices are categorized by the FDA depending on the degree of risk they presentto the patient and/or user, and the level of regulatory control that the FDA deems necessaryto provide sufficient assurance of their safety and effectiveness. Device classification dependson the intended use of the device and also upon indications for use. For example, a scalpel’s
PATH THROUGH THE FDA 443intended use is to cut tissue. A subset of intended use arises when a more specialized indicationis added in the device’s labeling, such as “for making incisions in the cornea.”Class I devices are those for which the FDA requires the lowest level of regulatory control.This classification is given to devices for which there is sufficient information to concludethat safety and effectiveness can be ensured by “general controls” alone. Generalcontrols give FDA authority to enforce against misbranding and adulteration. In addition,the FDA requires manufacturers to register and list their devices, notify consumers ofproblems associated with devices, and follow good manufacturing practices (GMPs) intheir manufacturing operations.Class II devices are those for which the FDA does not believe that general controlssuffice, but for which there is sufficient information that the FDA can establish special controlsto ensure their safety and effectiveness. As such, class II devices are not only subjectto general controls but are also subject to compliance with specific standards, guidelines,and patient or special follow-up once in the market.Class III devices are those for which the FDA requires the strictest regulatory control.This class is reserved for devices for which general and special controls cannot providereasonable assurance of safety and effectiveness or those for which there is insufficientinformation to make that assessment. Typically, a class III device is “represented to be fora use in supporting or sustaining human life or for a use which is of substantial importancein preventing impairment of human health, or presents a potential unreasonable risk of illnessor injury.”PATH THROUGH THE FDAThe requirements for medical devices to be used in human patients vary according to theregulatory classification of the device. Regardless of classification, all medical devicesneed to be cleared by the FDA before commercial distribution. Most devices are clearedfor marketing either through approval of a premarket approval (PMA) application orthrough clearance of a premarket notification submission on the basis of section 510(k) ofthe FD&C Act.Class I and class II devices are often subject to section 510(k) of the act, which is usedto determine whether a new device is substantially equivalent to a device in use prior toMay 28, 1976 (a preamendment device), or should be classified as a postamendmentsdevice. Substantial equivalence is based on the device’s intended use, its technical characteristics,as well as safety and effectiveness aspects. A manufacturer submitting a 510(k)application must supply information identifying a medical device that was marketedlegally prior to the amendment. If the device is found to be substantially equivalent, it canbe marketed immediately, whereas a new device that is not substantially equivalentrequires to go through the PMA process. The advantage of the 510(k) route is that it is substantiallyfaster and less costly than the PMA application.Preparing a PMA application is definitely not a trivial pursuit. A PMA application mustinclude:• Full reports of all information known to the manufacturer (regardless of whether it isgood or bad) concerning all research done to demonstrate safety and effectiveness• Detailed description of all components, properties, and principles of operation of thedevice• Detailed manufacturing data• Proposed labeling (which includes any text or informational figures on the device,packaging, and literature)
444 EPILOGUEAll data supplied by the manufacturer is subjected to thorough, independent review byFDA employees and medical advisors, including specialized medical devices advisorypanels composed of scientists and practicing physicians. If the reviewing team makes apositive recommendation for approval, a manufacturing site inspection is conducted by theFDA. A final notification of the FDA decision is mailed to the manufacturer following concludingdiscussions.ExceptionsThere are some exceptions to these rules. Medical devices that have not been approved bythe FDA for marketing can be used with human subjects under a Humanitarian DeviceExemption (HDE), an Investigational Device Exemption (IDE), or a Product DevelopmentProtocol.Humanitarian Use Devices (HUDs) are devices intended to diagnose or treat a conditionthat affects fewer than 4000 U.S. patients per year. The HDE application is similar toa PMA but does not require the manufacturer to demonstrate effectiveness, only safety.This path was provided through the 1990 Safe Medical Devices Act as a way to reduce thefinancial burden of R&D in the development of devices with limited market potential, butwhich may provide benefit to the patients who need them.A clinical trial for a device may be conducted through an investigational exemption tothe restraint on commercial distribution of unapproved medical devices. An IDE applicationrequires sufficient evidence of the device’s safety and a reasonable expectation ofeffectiveness to warrant its testing in humans. The FDA recognizes the investigationalnature of a clinical trial done under an IDE, allowing fewer rigors than in a PMA application.Nevertheless, important safety issues must be addressed through thorough bench andanimal testing before using the device on human subjects. The use of a medical deviceunder an IDE is very restricted:• The device can be made available only to designated investigators.• The device is to be used only under the terms of the approved IDE application.• Designated investigators are responsible for ensuring that the investigation adheres tothe investigational plan as well as any and all conditions imposed by the host hospital’sInstitutional Review Board (IRB) and the FDA.• The rights, safety, and welfare of subjects is maintained according to ethical guidelinesof the World Medical Association Declaration of Helsinki.• Strict control is maintained over the devices under investigation.Finally, section 515(f) of the FD&C Act provides an alternative to the PMA process forclass III devices. A Product Development Protocol (PDP) should be submitted by the manufacturerto the FDA very early in a device’s development cycle. The PDP defines the typesof data and specific safety and performance levels that the device must achieve to receivemarket clearance. The product can be introduced to the market as soon as the FDA verifiesthe manufacturer’s data, showing that it meets the preestablished safety and performancelevels.MARKETING AN IDEADespite the strong skepticism that is commonly encountered by new biomedical technologies,market statistics show that investors are eager to back medical device ventures. Infact, a recent survey by Medical Device and Diagnostic Industry magazine indicated that
the industry is undergoing profound changes which may make it easy for small entrepreneursto enter the health-care marketplace. Supporting this conclusion are data such as adecrease in the percentage of executives who reported that FDA’s policies were havingharmful effects on their business (47% in 1994, 46% in 1995, and 31% in 1996), a similardecrease in the percentage of respondents reporting delays in the premarket approval oftheir products (53% in 1994, 54% in 1995 and 45% in 1996), as well as an increase in themedian sales volume change (10% in 1995 to 20% in 1996). Now, these changes are certainlynot a quantum leap toward a most favorable business climate. However, operatingwith cautious optimism, you can certainly adapt and prosper in this friendlier (or at leastless hostile) environment.A different strategy for medical device startups that has become very popular is to tryto sell the idea or invention directly to a company that would market it and pay royalties.This is a business model that has made at least a few inventors very rich. However, attractingthe interest of a serious company takes much more than a good idea. A common misconceptionis that companies purchase raw ideas for development. Many inventors makethe mistake of believing that a manufacturing company will agree to sign a Non-DisclosureAgreement (NDA) which would allow the inventor to submit an unpatented idea inconfidence. The argument is that the inventor will not have to go through the expensive andtime-consuming processes of proper R&D, patenting and marketing research before theidea can be evaluated by a big-league player.Inventors often try to use NDAs to shortcut the process of patenting. But no NDA confersproperty rights on an idea; only a patent does. In fact, most reputable manufacturingcompanies will not sign NDAs just to listen to unsolicited ideas. Companies are legitimatelyconcerned of external contamination. Companies worry that someone with anundeveloped idea will come to them when they are already working in the same area. Ifthey sign an NDA, there is the possibility that the “inventor” will later sue the company formisappropriation, claiming that they stole the idea for a successful product. Large companieshave learned the lesson, and most will refuse to accept anything in confidence, requiringinventors to sign a waiver before they look at unsolicited ideas. The waiver requires theperson or company making the disclosure of the idea to give up all rights except those protectedunder the patent laws.NDAs have a legitimate use. They may be needed with potential licensees of a technologyto protect trade secrets. However, don’t live under the illusion that someone willpay you a million dollars for an idea that you disclosed to them with or without an NDAin place. There is no replacement for thorough and secret R&D followed by your own marketresearch to prove the workability, patentability, and marketability of the device. Armedwith this information, you can openly court licensees or distributors.Other inventors don’t find easy access to companies or are concerned that a large corporationwill steal their ideas upon disclosure. These people are often lured to use the servicesof an invention or patent promotion firm. These companies promise to evaluate, develop,patent, and market inventions. Beware, however, that in many cases these firms do little ornothing for the thousands of dollars that inventors are required to pay in exchange for services.The stories abound of dishonest promoters who take advantage of an inventor’s enthusiasmfor a new product. They not only urge inventors to patent their ideas, but also makefalse and exaggerated claims about the market potential of the invention. Our advice is thatyou proceed with caution and in assessing the true market potential of your product. At allcosts, avoid falling for the sweet-sounding promises of a fraudulent promotion firm.Finally, a note on the issue of infringing on someone else’s intellectual property. Patentsprotect many circuits and algorithms used in medical devices. The responsibility for avoidinginfringement is yours. However, the responsibility for policing patent rights belongs tothe patent holder. It is your call as to whether you’d rather learn about a “problem” patentby doing research or by waiting for a cease and desist letter. Your choice can be influencedMARKETING AN IDEA 445
446 EPILOGUEby many factors: What does it cost you to set up your business? How quickly can yourecover your investment? What are your costs of closing down quickly likely to be? Howwell do you know the technical field that your product is in? What do you know about howaggressive existing companies in the industry are at policing their patents?We recommend running a thorough search on one of the various Web-based patent searchengines (e.g., www.delphion.com, www.uspto.gov) for patents that may be related tothe device or technique that you are developing. In addition, the U.S. Patent and TrademarkOffice offers free information about patents, trademarks, and copyrights, and every statehas a Patent and Trademark Depository Library that maintains collections of current andpreviously issued patents and patent and trademark reference materials.More than the description of the invention, read the patent’s claims. If your product ormethod is described by a claim, you have a problem. Avoiding a claim is generally a matterof not having one of the features claimed. One way of “getting around a patent” is tostudy the patent in detail and engineer around the patent. In other words, determine howto modify your device to operate outside the scope of the patent claims. For example, in amedical device patent for a specific biopotential signal application, operating outside theinput voltage ranges claimed might be sufficient to avoid infringement. However, animprovement that has all the features claimed and a few additional ones is likely to be coveredby the patent. If you do this, it is recommended that you consult a patent attorney foran infringement opinion that presents the risk factors of whether your modifications wouldbe sufficient to avoid liability.When there’s a question as to whether or not your product infringes, you may want toask a patent attorney for an opinion of noninfringement. Getting that opinion does notmean that you don’t infringe, but it can protect you from having damages trebled in theevent a court finds that you did infringe. Another thing that you can do is get a validityopinion about the risks that a court of law would find the patent valid.Neither the infringement opinion nor the validity opinion come with any guarantees,they merely explain the risks of doing a particular activity. The decision to operate withinor near the scope of a claimed invention is a business decision based on the risks of beingsued and the risks of losing that lawsuit. If you make the wrong business decision, you mayhave to cease production and pay hefty damages. If the court determines that your infringementwas “willful,” your damages may be tripled and you may end up paying the otherside’s attorney fees.One of our favorite methods of avoiding patent infringement is to copy the productdescribed in a patent that expired at the end of its full term. Patents issued before June 5,1995, had a 17-year term measured from the date of issue. Patents filed after that date havea 20-year term measured from the filing date. Patents filed before that date, and pendingor issued on that date, have the longer of the two terms. Once a patent has expired, theinvention is in the public domain, and you are free to use it.Note that the safest way is to look for patents that have expired at the end of their “fullterm,” not just “expired,” because it is possible that a product described in a patent whichexpired early for lack of payment of maintenance fees might infringe the claims of an older“dominating” patent that is still in effect. If a patent expires after its full term, it is likelythat any older patent would have expired first. However, various factors, including termextensions, or perhaps very prolonged periods pending resolution due to appeals, make thisless than 100% certain, but highly likely.So what are you waiting for? Get your soldering pen, help humanity, and make a decentliving along the way.
APPENDIX ASOURCES FOR MATERIALS <strong>AND</strong> COMPONENTSAlfa Aesar (Johnson Matthey)www.alfa.com30 Bond StreetWard Hill, MA 01835(978) 521-6300(978) 521-6350 (fax)Analog Devices, Inc.www.analog.comOne Technology WayNorwood, MA 02062(617) 329-4700(617) 326-8703 (fax)Apex Microtechnology Corporationwww.apexmicrotech.com5980 North Shannon RoadTucson, AZ 85741(520) 690-8600(520) 888-3329 (fax)Axon Instruments, Inc.www.axon.com3280 Whipple RoadUnion City, CA 94587(510) 675-6200(510) 675-6300 (fax)Burr-Brown Corporationwww.burr-brown.com6730 South Tucson BoulevardTucson, AZ 85706(520) 746-1111(502) 889-1510 (fax)Capteur Sensors & Analysers Ltd.www.capteur.co.ukWalton RoadPortsmouth, Hants, PO61SZ, UK44 (0) 1235-75030044 (0) 2392-386 611 (fax)CCC del Uruguaywww.ccc.com.uyGeneral Paz 137111400 Montevideo, Uruguay598-2-600-7629598-2-601-6286 (fax)C&D Technologies’ Power Electronicswww.cdpowerelectronics.com3400 East Britannia DriveTucson, AZ 85706(800) 547-2537(520) 770-9369 (fax)Design and Development of Medical Electronic Instrumentation By David Prutchi and Michael NorrisISBN 0-471-67623-3 Copyright © 2005 John Wiley & Sons, Inc.447
448 APPENDIX AChomericswww.chomerics.com77 Dragon CourtWoburn, MA 01888-4014(781) 935-4850(781) 933-4318 (fax)Cornell Dubilier Electronics, Inc.www.cornell-dubilier.com140 Technology PlaceLiberty, SC 29657(864) 843-2626(864) 843-2402 (fax)Dallas Semiconductor Corporation(part of Maxim Integrated Products, Inc.)www.maxim-ic.com4401 Beltwood Parkway SouthDallas, TX 75244-3292(214) 450-0448(214) 450-0470 (fax)Electronic Design & Research, Inc.www.vsholding.com7331 Intermodal DriveLouisville KY 40258(502) 933-8660(502) 933-3422 (fax)Elpac Electronics, Inc.www.elpac.com1562 Reynolds AvenueIrvine, CA 92614-5612(949) 476-6070(949) 476-6080 (fax)Fair Radio Saleswww.fairradio.com1016 East Eureka StreetLima, OH 45802(419) 227-6573(419) 227-1313 (fax)Fair-Ritewww.fair-rite.com1 Commercial RowWallkill, NY 12589(845) 895-2055(845) 895-2629 (fax)Fischer Scientificwww.fishersci.comOne Liberty LaneHampton, NH 03842(603) 926-5911(603) 929-2215 (fax)Hammond Manufacturing Co., Inc.(Electronics Group)www.hammondmfg.com256 Sonwil DriveCheektowaga, NY 14225(716) 651-0086(716) 651-0726 (fax)Harris Semiconductor(part of Intersil Corporation)www.intersil.com1301 Woody Burke RoadMelbourne, FL 32902(407) 724-3000(407) 724-3937 (fax)Harvard Apparatus, Inc.www.harvardapparatus.com84 October Hill RoadHolliston, MA 01746(508) 893-8999(508) 429-5732 (fax)Heraeus W.C. GmbH & Co.www.wc-heraeus.com/medicaltechnologyKG Heraeusstrasse 12-14 D-63450Hanau, Germany49 (6181) 35383049 (6181) 359448 (fax)Honeywell Solid State Electronics Centerwww.ssec.honeywell.com12001 State Highway 55Plymouth, MN 55441(763) 954-2539(763) 954-2720 (fax)International Rectifierwww.irf.com233 Kansas StreetEl Segundo, CA 90245(310) 322-3331(310) 322-3332 (fax)Intersil Corporationwww.intersil.com7585 Irvine Center DriveSuite 100Irvine, CA 92618(949) 341-7000(949) 341-7123 (fax)
SOURCES FOR MATERIALS <strong>AND</strong> COMPONENTS 449In Vivo Metricwww.invivometric.com910 Waugh LaneUkiah, CA 95482(707) 462-4121(707) 462-4011 (fax)Kilovac Corporationwww.kilovac.comP.O. Box 4422Santa Barbara, CA 93140(805) 684-4560(805) 684-9679 (fax)LEM U.S.A., Inc.www.lem.com6643 West Mill RoadMilwaukee, WI 53218(414) 353-0711(414) 353-0733 (fax)MacDermid Incorporatedwww.macprintedcircuits.com245 Freight StreetWaterbury, CT 06702(203) 575-5700(203) 575-7916 (fax)Magnetic Shield Corporationwww.magnetic-shield.com740 North Thomas DriveBensenville, IL 60106(888) 766-7800(630) 766-2813 (fax)Maxim Integrated Products, Inc.www.maxim-ic.com120 San Gabriel DriveSunnyvale, CA 94086(408) 737-7600(408) 737-7194 (fax)Microchip Technology, Inc.www.microchip.com2355 West Chandler BoulevardChandler, AZ 85224(480) 792-7966(480) 792-4338 (fax)Mini-Circuitswww.minicircuits.comP.O. Box 350166Brooklyn, NY 11235-0003(718) 934-4500(718) 332-4661 (fax)MSI Scantech Limitedwww.msi-scantech.co.ukThe Centre, Reading RoadEversley, Hampshire, RG27 0NB, UK44 (0) 118 973 792644 (0) 118 973 7927 (fax)muRata Electronics (USA)www.murata.com2200 Lake Park DriveSmyrna, GA 30080-7604(770) 436-1300(770) 436-3030 (fax)Noble-Met Ltd.http://www.uticorporation.com/global/noblemet/noblemet.html200 South Yorkshire StreetSalem, VA 24153(540) 389-7860(540) 389-7857 (fax)Ohmic Instruments Co.www.ohmicinstruments.com508 August StreetEaston, MD 21601(410) 820-5111(410) 822-9633 (fax)Panasonic Industrial Co.www.panasonic.comTwo Panasonic Way, 7H-4Secaucus, NJ 07094(201) 348-5232(201) 392-4441PASCO Scientificwww.pasco.comP.O. Box 61901110101 Foothills BoulevardRoseville, CA 95747-9011(916) 786-3800(916) 786-8905 (fax)Philips Semiconductorswww.phillips.semiconductors.com811 East Arques AvenueSunnyvale, CA 94088-3409(800) 234-7381(708) 296-8556 (fax)Pragmatic Instruments, Inc.www.pragmatic.com7313 Carroll RoadSan Diego, CA 92121(800) 772-4628(619) 271-9567 (fax)
450 APPENDIX ARadio Shackwww.radioshack.com200 Taylor Street, Suite 600Fort Worth, TX 76102(800) 843-7422(817) 415-6880 (fax)Sensortechnics, Inc.www.sensortechnics.com1420 Providence Highway, Unit 267Norwood, MA 02062(781) 762-1674(781) 762-2564 (fax)ST Microelectronicswww.st.com1310 Electronics DriveCarrollton, TX 75006(972) 466-6000(972) 466-8130 (fax)Surplus Sales of Nebraskawww.surplussales.com1502 Jones StreetOmaha, NE 68102(402) 346-4750(402) 346-2939 (fax)TDK Corporation of Americawww.component.tdk.com1600 Feehanville DriveMount Prospect, IL 60056(847) 803-6100(847) 803-6296 (fax)Texas Instruments Incorporatedwww.ti.com12500 TI BoulevardDallas, TX 75243(800) 336-5236The MathWorks, Inc.www.mathworks.com3 Apple Hill DriveNatick, MA 01760-2098(508) 647-7000(508) 647-7001 (fax)UFIwww.ufiservingscience.com545 Main C-2Morro Bay, CA 93442(805) 772-1203(805) 772-5056 (fax)UltraVolt, Inc.www.ultravolt.comCS 9002Ronkonkoma, NY 11779(631) 471-4444(631) 471-4696 (fax)VWR Scientific Productswww.vwrsp.com3000 Hadley RoadSouth Plainfield, NJ 07080(908) 757-4045(908) 757-0313 (fax)Wilson Greatbatch Technologies, Inc.www.greatbatch.com10,000 Wehrle DriveClarence, NY 14031(716) 759-6901(716) 759-8579 (fax)WireTronic, Inc.www.wiretron.com19698 State Highway, 88, CPine Grove, CA 95665(209) 296-8460(209) 296-8462 (fax)Xylemwww.xylemcompany.com1480 Lake Drive WestChanhassen, MN 55317(952) 368-9040(952) 368-9041 (fax)Yuasa Battery, Inc.www.yuasabatteries.com2366 Bernville RoadReading, PA 19612(866) 431-4784Thermometrics New Jerseywww.thermometrics.com808 U.S. Highway 1Edison, NJ 08817(732) 287-2870(732) 287-8847 (fax)
APPENDIX BFTP SITE CONTENTftp://ftp.wiley.com/public/sci_tech_med/medical_electronic/DISCLAIMERAll of the files in the book’s ftp site (collectively, the software) are provided to you free ofcharge for your convenience. This software is presented only as examples of engineeringbuilding blocks used in the design of experimental biopotential signal acquisition and processingsystems. The authors do not suggest that the software presented herein can orshould be used by the reader or anyone else to acquire or process signals from human subjectsor experimental animals. Neither do the authors suggest that the software can orshould be used in place of or as an adjunct to professional medical treatment or advice.Sole responsibility for the use of the software or of systems incorporating the software lieswith the reader, who must apply for any and all approvals and certifications that the lawmay require for its use.The authors do not make any representations as to the completeness or the accuracy ofthe software, and disclaim any liability for damages or injuries, whether caused by or arisingfrom the lack of completeness, inaccuracies of the software, misinterpretations of thedirections, misapplication of the software, or otherwise. References to other manufacturers’products made in this software do not constitute an endorsement of these products butare included for the purpose of illustration and clarification. Since some of the softwaremay relate to or be covered by U.S. or other patents, the authors and the publisher disclaimany liability for the infringement of such patents by the making, use, or selling of suchequipment or software, and suggest that anyone interested in such projects seek properlegal counsel.The authors and the publisher are not responsible to the reader or third parties for anyclaim of special or consequential damages. The software in the book’s ftp site is provided“as-is” without any warranty whatsoever. No technical support or application assistanceare available. In no event will the authors or the publisher be liable to you, under any legaltheory, for indirect or consequential damages resulting from loss of use, profits, downtime,goodwill, damage to, or replacement of equipment or property arising out of or in connectionwith the use or performance of the software. In addition, no liability is assumed byDesign and Development of Medical Electronic Instrumentation By David Prutchi and Michael NorrisISBN 0-471-67623-3 Copyright © 2005 John Wiley & Sons, Inc.451
452 APPENDIX Bthe authors or the publisher for loss of data or any costs for recovering, reprogramming, orreproducing any data stored in any machine used in connection with the software.REDISTRIBUTED FREEWAREFor your convenience, the book’s ftp site also contains some of the programs listed in thebook as freeware that can be downloaded from the Web. These programs are included herefree of charge with the understanding that “freeware” refers to software that can be downloadedwithout having to pay money for them. These files may be distributed freely withoutpaying anything in the way of royalties or distribution fees as long as they are notmodified prior to distribution. Note that this also applies to you. If you intend to distributefurther the files listed as freeware, you must make sure that you hand them out in their originalform. You must also distribute things that come in multiple parts as a complete set(e.g., many of the computer programs have extra files; you must distribute them alltogether, the way you retrieved them from the ftp site). The reason is quite simple: Thehard work that went into these products should be distributed in the way that its authorintended, not the way that someone else thinks it should be.CONTENTS <strong>OF</strong> <strong>MEDICAL</strong>_<strong>ELECTRONIC</strong>.ZIPSoftware for IntroductionFolder: Redistributed Freeware• Little Stimulus Maker v2.0 (LSM2_SFX.EXE freeware for Windows 9x) by John Kelly.Software for Chapter 5: Signal Conditioning, Data Acquisition,and Spectral AnalysisFolder: Universal Sensor InterfaceVB5.0• LPT8_DVM.VBP is a VisualBasic (v5.0) application project that shows how todevelop a virtual instrument to acquire analog and digital data as well as to controlthe D/A and digital outputs of the Universal Sensor Interface. INPOUT32.DLL isused to allow input and output operations to be performed on the printer port. If 16-bit operation is required, modify the programs to make use of the 16-bitCUSER2.DLL file.• LPT8_LOGGER.VBP is basically the same as LPT8_DVM.VBP, but a file dialog hasbeen added to make it possible to log acquired data directly to disk.• LPT8_THERM is used to read temperature in °C and °F using a thermistor.QuickBASIC• LPTAN8.BAS is a simple program for driving the Universal Sensor Interface A/D.• LPTAN8.EXE is the compiled (DOS) version of this program.• ACQUIRE8.BAS implements an eight-channel oscilloscope/four-channel logicanalyzer.
FTP SITE CONTENT 453• LPT8FAST.BAS is the same as ACQUIRE8.BAS, but provisions have been made toallow acquired data to be recorded on disk. The compiled version (LPT8FAST.EXE)of this program is intended to be run from a bootable diskette in which CONFIG.SYSfirst initializes a RAM drive.• ATOD_SL8.BAS is similar to LPTAN8.BAS, but acquisition is regulated through theTIMER command. Data frames are acquired at desired intervals in the range 1 to86,400 seconds. ATOD_SL8.EXE is the compiled (DOS) version of this program.• DTOA.BAS is a simple program that implements the serial protocol to writevalues to the D/A converters. DTOA.EXE is the compiled (DOS) version of thisprogram.• THERMOM.BAS is used to read temperature in °C and °F using a thermistor. THER-MOM.EXE is the compiled (DOS) version of this program.• SCALE.BAS implements an auto-zeroing digital scale by controlling the sensor’soutput offset through the Universal Sensor Interface’s D/A. SCALE.EXE is the compiled(DOS) version of this program.Folder: Spectral Analysis• SPECTRUM.BAS is a QuickBASIC 4.5 program that estimates and displays the spectrumof a signal via the zero-padded FFT, an averaged-periodogram method (Welch’sestimator), and a parametric estimator (Marple’s autoregressive method). SPEC-TRUM.EXE is the compiled (DOS) version of this program.• LPT8SPEC8.BAS is essentially the same as SPECTRUM.BAS but drives the UniversalSensor Interface to acquire evenly sampled data. LPT8SPEC.EXE is the compiled(DOS) version of this program.• MARPLE.DAT is a short 64-point complex test data set used to evaluate differentspectral analysis methods.• NOISE.BAS is a QuickBASIC program to generate data useful for evaluating theresolving power of spectral estimators. NOISE.DAT is an ASCII data file generatedthrough this program.Folder: Redistributed FreewareSignal Generators for the PC Sound Card• BIP Electronics Labs Sine Wave Generator v3.0 (SINE30.ZIP, freeware for Windows3.1, but works well in most cases under Windows 9x) by Marcel Veldhuijzen.• Sweep Sine Wave Generator v2.0 (SWPGEN20.ZIP, freeware for Windows 9x) byDavid Taylor.• PC function generator (PLAY.EXE, freeware for Windows 9x, 2000, NT) by thePhysics Lab of Rutgers University.• Sound interference (INTERFERENCE.EXE, freeware for Windows 9x, 2000, NT) bythe Physics Lab of Rutgers University. This program generates sine waves throughboth channels of the sound card. The phase difference between the right and left channelscan be set through software, allowing demonstrations of active noise control andclassical wave interference.• Beat-tone generation (BEATINBRAIN.EXE, freeware for Windows 9x, 2000, NT)by the Physics Lab of Rutgers University. This program generates two sine waves ofdifferent frequencies through the left and right sound card, allowing experiments inthe generation and detection of beat tones.
454 APPENDIX BAudio Oscilloscopes for the PC Sound Card• BIP Electronics Labs Digital Scope v3.0 (SCOPE30.ZIP, freeware for Windows 3.1,but works well in most cases under Windows 9x) by Marcel Veldhuijzen.• Oscilloscope for Windows v2.51 (OSC2511.ZIP, freeware for Windows 9x) byKonstantin Zeldovich.Audio Spectrum Analyzers for the PC Sound Card• Spectrogram v5.0.5, Dual Channel Audio Spectrum Analyzer (GRAM501.ZIP freewarefor Windows 9x) by Richard Horne.• Audio Wavelet Analyzer v1.0 (AUDIOWAVELETANALYZE.ZIP freeware forWindows 9x) by Christoph Lauer.• 16- or 24-bit Sound Card Oscilloscope and FFT Analyzer (16BITFFTSCOPE.EXEand 24BITFFTSCOPE.EXE, freeware for Windows 9x, 2000, NT) by the PhysicsLab of Rutgers University.Transfer Function Analyzer for the PC Sound Card• RightMark Audio Analyzer v2.5 (RMAA25.ZIP freeware, open-source code forWindows 9x, 2000 and NT) by Alexey Lukin and Max Liadov.• WaveTools v1.0 Audio Analysis software (Signal Generator, Spectrum Analyzer,Oscilloscope and Audio Meter) (WAVETOOL.ZIP freeware for Windows 9x) by PaulKellett.Audio Frequency Counter for the PC Sound Card• BIP Electronics Labs Digital Frequency Counter (COUNTER.ZIP, freeware for Windows3.1, but works well in most cases under Windows 9x) by Marcel Veldhuijzen.Software for Chapter 6: Signal Sources for Simulation, Testing, and Calibration• REALECG.MAT is a Matlab file that contains 60 s of real ECG signal digitized at arate of 5 kHz. The digitized data vector is named “ecg.” The time vector associatedwith this ECG signal is named “time.”Folder: Arbitrary Waveform Generator• MAT2ARB.M is a Matlab function that saves two vectors from the Matlab environmentas a file that can be loaded into the two-channel Arbitrary Waveform Generator.• Arb Loader subfolder contains the installation files for the program used to loadwaveforms into the two-channel Arbitrary Waveform Generator through the PC’s parallelprinter port.• Arb Calibration Files subfolder contains signal/marker files that can be used to testthe two-channel Arbitrary Waveform Generator.Folder: Responsive Simulator Firmware• This file contains the PIC firmware for the Responsive Cardiac Simulator (QUICK-VIEW.ZIP).
FTP SITE CONTENT 455Folder: Redistributed Freeware• SoundArb v1.02 (SASETUP.EXE freeware for Windows 9x, NT) by David ShermanEngineering Co.Software for Chapter 7: Stimulation of Excitable TissueFolder: Hodgkin–Huxley• HODGKINHUXLEY.M is a Matlab program that simulates the response of a giantsquid axon to an electrical stimulus. ALPHA_H.M, ALPHA_M.M, ALPHA_ N.M,BETA_H.M, BETA_M.M and BETA_N.M are Matlab functions that calculate therate constants for the Hodgkin–Huxley model.Folder: Redistributed Freeware• Finite Element Methods for Magnetics v3.1 (FEEM_SETUP.EXE freeware forWindows 9x) by David Meeker.• WireTronic wire information software (WTSETUP.EXE freeware for Windows 9x)by WireTronic, Inc.• VirtualCV v1.0 cyclic voltammetry simulator (VTLCV10.ZIP freeware for Windows9x) by Andre Laouenan.• Beat-tone generation (BEATINBRAIN.EXE, freeware for Windows 9x, 2000, NT)by the Physics Lab of Rutgers University. This program generates two sine waves ofdifferent frequencies through the left and right sound card. Can be used with isolatedhigh-voltage output stages for interferential muscle stimulation.Software for Chapter 8: Cardiac Pacemakers and DefibrillatorsFolder: VVI• VVI.ZIP implements a simple VVI state machine that disregards the VOO mode. Thisis the program that was discussed above.• VVI WITH EMBEDDED VOO.ZIP implements a VVI state machine that can beplaced in VOO mode by disregarding sensed events. The state machine is identical tothe one implemented in VVI.ZIP, but the EnableSense routine enables or disablessensing depending on the desired state.• VVI VOO WITH VOO STATE.ZIP is a VVI state machine in which the VOO state isimplemented through a new state during which there is no sensing.Folder: DOCD• This file contains the PIC firmware for the DOCD Impedance Sensor (DOCD.ASM).Folder: Shock-Box Firmware and Control Software• This file contains the firmware for the defibrillation shock-box PICs and the VBControl software for the defibrillation shock box (SHOCKBOX.ZIP).
INDEXAAMI, see Association for the Advancement ofMedical InstrumentationAblation, see ElectrosurgeryAction current, 305Action potential, 305transmembrane recording of, 42Aliasing, 76, 224, 236, 242American National Standards Institute (ANSI),98, 440Amplifier, 1AC-coupled, 46, 49array, 8, 15, 22, 38, 123, 249blanking, 88, 93bootstrapped, 49buffer,7,38CMR of, 1, 2, 24, 25, 29, 33, 46CMRR of, 2, 26, 29, 49DC-coupled, 41, 44differential, 23drift of, 3follower, 7frequency response of, 1, 29, 32, 41, 108gain of, 1, 6, 17, 23, 25, 28, 39, 108ICIA, 29, 49input impedance of, 3, 8instrumentation, 27, 29, 33inverting, 6isolation, 87, 104, 106, 108, 428lock-in, 395noise of, 3, 18, 32operational, 6, 23, 27, 325recovery of, 3saturation, 3sense, see Pacemaker, sense amplifiersensor, 213single-ended, 6switched-capacitor, 33synchronous, 395wideband, 41Analog-to-digital converter, 118, 206, 226, 417,431Aneurysm, see Embolic therapyANSI, see American National Standards InstituteAntennaapplicator, 361biconical, 177dipole, 156loop, 156measurement, 154ridged-horn, 177TEM horn, 179Association for the Advancement of MedicalInstrumentation (AAMI), 5, 81load, 129, 131, 341standards, 5, 98, 290, 340, 394, 440Atrio-ventricular node, 370, 371Atrium, 369Autoregressive model (AR), 239Autoregressive moving average model(ARMA), 239AV block, 371, 376BandwidthFM, 230, 274, 276telemetry, 230telephone, 230, 276Barrieragainst fire, 98, 145dielectric, 99, 109, 139testing of, 139Batterycharger, 419implantable, 317, 359, 372, 386, 416powered equipment, 125, 141, 386,417Biocompatibility, 145, 328Bioimpedance, see Sensor, impedanceBiopotential signals, 1frequency range of, 41model of, 3, 4Bipole source, 293, 297Blumlein generator, 179Body potential driving, 18, 85Bovie, see ElectrosurgeryBradycardia, 312, 371Bundle of His, 370Cancer treatment, 362, 363Cardiacablation, see Electrosurgeryarrhythmia, 357, 369, 407conduction system, 369contractility modulation, 359defibrillation, see Defibrillatordefibrillator, see Defibrillatorelectrophysiology, 42fibrillation, 102, 412, 437fibrillator, 437output, 369, 393pacemaker, see Pacemakerpacing, see Pacemakerstroke volume, 392Cardiomyoplasty, 312CENELEC, see Comité Européen deNormalisation ElectrotechniqueDesign and Development of Medical Electronic Instrumentation By David Prutchi and Michael NorrisISBN 0-471-67623-3 Copyright © 2004 John Wiley & Sons, Inc.457
458 INDEXCentro de Construccion de Cardioestimuladoresdel Uruguay (CCC), 372Channel skew, 225Chloroiridic acid, 332Chronaxie, 309Clearance, 99, 104, 139Cochlear implant, 313Coil design, 351Comité Européen de NormalisationElectrotechnique (CENELEC), 278, 292Common-modeinterference, 3, 18, 23rejection, see Amplifier, CMRrejection ratio, see Amplifier, CMRRsignal, 3, 23, 27, 33Conductance catheter, 396Constant-current source, 127, 206, 217, 293,322, 393Constant-voltage source, 293Control systems, 221Creepage, 99, 104, 139Currentauxiliary, 101electrocution risk, 97enclosure leakage, 101, 129ground leakage, 101, 129loop, 213measuring device, 129, 131patient leakage, 101, 106, 129source, see Constant-current sourceCyclic voltammetry, 329, 455DC rejection, 44Deep brain stimulation (DBS), 313Defibrillation-proof, 16, 42, 102, 126, 192,435Defibrillator(s)batteries for, 416capacitors for, 414, 417, 424cardiac, 312, 412external, 413implantable, 289, 416shock box, 417, 455standards, 439switching devices for, 414, 425waveforms, 412, 416Depolarization, 305Depression, 355Digital signal processing (DSP), 233, 247Digital-to-analog converter, 206, 214, 255, 264,417, 431Double-layer interface, 327Driven right-leg, see Body potential drivingE-field probe, 158, 161Electrical fast transients (EFT), 172, 181Electrical muscle stimulation (EMS), 297, 313,334, 344Electroacupuncture, see Quack therapiesElectroanalgesia, see Pain reliefElectroanesthesia, 341Electrocardiography (ECG), 11amplifier for, 15, 23, 83, 102body potential mapping, 15, 40, 123, 226,292electrode polarization potentials in, 5inverse solution, 292leads, 85signals, 15, 42, 71, 81, 230, 233, 252, 269,276, 278transtelephonic monitoring, 230Electrocautery, 357Electrochemical therapy (EChT), 363Electrochemotherapy, see Electroporation therapyElectroconvulsive therapy (ECT), 313, 342Electrocution, see Shock, hazardElectrodearray, 10, 14, 22, 362capacitance, 327capacitive, 12catheter, 396charge injection through, 326coatings, 12, 328corrosion, 319, 328electrode-tissue interface, 3, 327electroporation, 362half-cell potential of, 3impedance, 20, 293implantable, 314, 326, 360, 417iontophoresis, 357iridium oxide (IROX), 329, 363materials, 328pasteless, 11pipette, 305platinum/iridium, 328polarization, 3, 25silver/silver chloride, 5stimulation, 314, 326titanium-nitride, 329, 333transtelephonic monitoring, 232Electroencephalography (EEG)amplifier for, 29, 111international 10-20 system, 14signals, 10, 11, 15, 42, 233topographic brain mapping, 40, 123, 226,249Electrogastrogram (EGG), 42Electrogram, see Intracardiac, electrogramElectrolyte paste, 6Electromagnetic compatibility (EMC)design for, 189standards, 147, 171, 290Electromagnetic emissionsconducted, 149, 166from digital circuits, 149radiated, 149, 152sniffing, 158standards, 149, 169Electromagnetic interference (EMI), 145, 147,291comb generator, 165filter, see Filter, EMIwideband generator, 179Electromagneticfield, 155probe, 159signals, 155Electromagnetic susceptibilityconducted, 172, 180radiated, 172, 177, 290standards, 171Electromyography (EMG), 11, 42, 54array, 10, 38, 225, 243, 245motor unit action potentials, 38, 42, 245single fiber electromyogram, 42surface EMG, 10, 11, 38, 42, 245Electronarcosis, 341Electroneurography (ENG), 42Electro-oculography (EOG), 42Electro-osmosis, 359Electroporation therapy (EPT), 362Electroretinography (ERG), 42Electrostatic discharge (ESD)coupling plane, 177model, 173protection from, 10, 12, 15, 20, 42, 191simulator, 174susceptibility to, 172Electrosurgery, 52, 105, 148, 192, 357Electroventilation, 312Embolic therapy, 364Enclosureground, 127leakage current, see Current, leakageshielding characteristics, 190, 201Energy therapies, see Quack therapiesEpileptic seizures, 312Errorpicket-fence, 236quantization, 257scalloping, 236Evoked potentialsamplifier for, 29auditory evoked potential (AEP), 42motor evoked potential (MEP), 347somatosensory evoked potential (SSEP), 42visual evoked potential (VEP), 42Excitable tissue, 305Fault condition, 101, 131, 391FCC, 147Fibrillation, see Cardiac, fibrillationFilteractive, 56adaptive, 73antialiasing, 78, 224, 236artifact, 81autoregressive (AR), 239autoregressive moving average (ARMA), 239band-pass, 60Bessel, 59, 76, 78Butterworth, 59, 76, 78, 79, 93Chebyshev, 59click and pop, 88comb, 71
INDEX 459connector, 201DC-correct, 77, 274elliptic, 76, 257EMI, 152ferrite, 152, 200frequency-domain characteristics, 59gyrator, 70harmonic eliminator, see Filter, combhigh-pass, 52, 60, 80, 88impedance-converter, 70implementation, 59interpolating, 225, 261low-pass, 29, 36, 50, 60, 77, 88, 108, 109,224, 252, 257, 274moving average, 239multiple-feedback, 60N-path, 73noise introduced by, 76notch, 15, 54, 65passive, 49programmable, 65, 76, 79reconstruction, 225, 252response, 59RF, 52, 106, 191, 201rumble, 88Sallen-Key, 60slew-rate limiter, 80state-variable, 60, 71switched-capacitor, 36, 76time-domain characteristics, 59topology, 60tunable, 61twin-T, 65voltage-controlled voltage-source, see Filter,Sallen-KeyFlammability, 145Food and Drug Administration (FDA), seeRegulatory agenciesFourier transformdiscrete Fourier transform (DFT), 235, 243fast Fourier transform (FFT), 233Frequency response of amplifier, see Amplifier,frequency responseFrequency-to-voltage converter (FVC), 114, 274Frequency-wavenumber, 243Functional electrical stimulation (FES), seeElectrical muscle stimulationFunctional neuromuscular stimulation (FNS),see Electrical muscle stimulationGalvanic skin response (GSR), 42Galvanostat, 293, 297Gastroparesis, 313Giant squid axon, 305Gravitational loss of consciousness (GLOC), 11Greatbatch, Wilson, 373Ground integrity, 127H-field probe, 158Heartanatomy, 369block, 371, 376perfused isolated model, 302physiology, 369High voltage, 139, 174, 179, 314, 347, 364,414, 417, 423HiPot, 139Hilbert transform, 230Hodgkin–Huxley, 305Howland pump, 321Humidity preconditioning, 131, 141Hyperbaric chamber, 213Hyperpolarization, 305Ionic currents, 305Impedancecardiography, see Sensor, impedanceof skin, 3, 233, 297plethysmography, see Sensor, impedancerheography, see Sensor, impedanceInsulationbasic, 99, 141double, 99, 141ratings, 99, 141reinforced, 99, 104, 123, 141supplementary, 99, 141Integrated circuit instrumentation amplifier(ICIA), see Amplier, ICIAInterferenceelectromagnetic, see Electromagneticinterference (EMI)from electronic article surveillance systems,289from fluorescent lamps, 1, 18, 71powerline, 1, 18, 65, 71radio frequency (RFI), 171with pacemakers, see Pacemaker, interferencewithInternational Electrotechnical Commission(IEC), 98, 149, 334, 440Inter-Range Instrumentation Group of theRange Commanders Council (IRIG),230Intracardiacelectrogram, 42, 93, 191, 383impedance, see Sensor, impedanceIontophoresis, 357Iridium, 328, 329IsolationA/D converter, 118, 230amplifier, see Amplifier, isolationDC/DC converter, 56, 104, 152, 417multiplexer, 122optical, 54, 109, 111, 118, 221, 322, 425power supply, 123requirements, 99, 141switch, 125three-port, 108Kelvin probe, 127Langendorff perfusion, 302Lapicque, 309Laplace equation, 296Line-impedance stabilization network (LISN),166Litz wire, 353Magnetic fieldgenerator, 187, 347susceptibility, 172, 187Marple’s algorithm, 239Matlab ® , 227, 228, 268, 272, 273, 306, 344,454Medallion, 10, 119Medical deviceclassification, 442effectiveness, 442humanitarian, 444indications, 442investigational, 444postamendment, 443preamendment, 443safety, 442Microcurrent stimulation, see Quack therapiesModulationfrequency, 228, 273pulse-code, 230Monophasic action potential (MAP), 42, 44Moving average (MA), 239MP35N, 328Nanosecond pulsed electric field (nsPEF)therapy, 364Network analyzer, 199Neuromuscular electrical stimulation (NMES),see Electrical muscle stimulationNondisclosure agreement (NDA), 445Nyquist theorem, 224, 236, 252Offset cancellation, 43, 213, 220, 238Op-amp, see Amplifier, operationalOpen field test site, 154Optocoupler, see Isolation, opticalOptoisolator, see Isolation, opticalOscilloscope, 226, 218, 235, 268, 293, 454Oversampling, 224Pacemaker(s)artifact augmentation, 81, 83batteries for, 374cardiac, 277, 312, 314, 345communication system for, 379dual chamber, 376external, 297, 314, 372, 379, 381gastric, 313Greatbatch, Wilson, 373history of, 372interference with, 191, 289, 345, 356, 376,386magnetic, 407modes, 379, 386parameters, 314, 378power consumption in, 390programmable, 378, 381pulse detection, 83
460 INDEXPacemaker(s) (Continued)pulse generator, 374, 383rate-responsive, 392refractory period, 376sense amplifier, 36, 93, 374, 383sensors for, 278software for, 386, 455standards, 438state machine of, 373, 376, 386, 407testing of, 277, 391transcutaneous, 407transtelephonic monitoring of, 232Pain relief, 312, 337Parkinsonian tremor, 313Partaccessible, 98applied, 99, 119, 145cardiac connection, 99floating, 99live, 99signal I/O, 99Patent(s)claims, 446databases, 446infringement of, 441, 445term of, 332, 446Periodogram, 238Phase locked loop (PLL), 274Platinum, 328, 363Potassium channel, 306Potentiostat, 293, 297, 331Powerlinecontrol, 221sensing, 223surges, 172transients, 172, 184voltage variations, 172, 186Power spectral density (PSD), 235, 243Pressure-volume relationship, 397Printed circuit board (PCB)crosstalk in, 198layout, 193line termination, 195resonances in, 200track length, 196transmission line properties, 193PSpice, 61, 130, 348, 375Pulse width modulation, 111Purkinje fibers, 370Quack treatments, 338, 356, 364, 365Radiation, 145Rectifier, 54Regulatory agencies, 98, 146, 171, 334, 440,441Regulatory path, 441Regulatory review, 442Rheobase, 309Rheoencephalography, see Sensor, impedanceRheopneumography, see Sensor, impedanceRight-leg driving, see Body potential drivingRosell’s method, 297Safetyextra low voltage, 124hazard, 171of electrical stimulation, see Stimulation, safetystandards, 97, 125, 127, 129, 139, 334, 340,438test, 127, 129, 139Saline solution, 292, 297Sample-and-hold, 33, 43, 226, 406Sampling, 224burst, 226SensorAC/DC, 223acceleration, 205, 392CO 2 , 215current, 205flow, 205gas, 205hemodynamic, 278, 392humidity, 205, 215impedance, 205, 278, 392, 400, 455interface, 206magnetic field, 205minute ventilation, 392oxygen, 215pressure, 205, 215, 397respiration, 206signal conditioning, 213strain gauge, 220temperature, 205, 215, 220weight, 205, 220Shieldagainst EMI, 190, 201magnetic, 202room, 154Shockhazard, 98, 131protection from, 99, 125Signal generatorarbitrary, 251, 255, 259, 271, 273, 454, 455audio, 226, 344, 453direct digital synthesis (DDS), 256precision, 249sound card software, 226, 271, 344, 453waveforms for, 268Simulator2-D, 293biological realism of, 289, 300cardiac, 255, 276, 293, 454cosmetic use of, 337functional neuromuscular stimulation, 297, 334Hodgkin–Huxley experiment, 306, 455neuromuscular, 334perfused heart, 300skin, 297tissue, 290torso, 290, 297Sinus node, 369, 371Skin conductance, 3, 233, 297, 357Sodium channel, 306Sound card, 226, 271, 273, 344, 453Space clamp, 306Spectral analysis2-D, 233array, 243classical, 238, 453high-resolution, 239, 453multidimensional, 246Spectrum analyzeraudio, 227, 454RF, 154, 162, 166Steel, 328Stimulationanode-break, 308anodic, 307artifact rejection, 36, 81asymmetric, 316balanced, 316, 383bipolar, 309biphasic, 316, 322cathodic, 309clinical uses of, 311diagnostic uses of, 312extracellular, 308field, 309interferential, 315, 340, 455intracellular, 306magnetic, 346monophasic, 316monopolar, 309of bladder, 356of bone-growth, 360of brain, 312, 345, 346of cell apoptosis, 364of heart, see Pacemaker, cardiacof kidneys, 356of muscles, 312, 317, 334of nerves, 312, 317, 321, 347of tissues, 305of visual cortex, 313of wound healing, 360parameters, 309, 314rebound, 307safety of, 334, 337, 340, 344, 356threshold, 307, 309transcranial, 346Stimulatorbridge, 325capacitor-coupled, 319capacitor-discharge, 316, 317, 374, 383,412constant-current, 316, 319, 322constant-voltage, 325implantable, 312, 319, 345, 359interferential, 342magnetic, 347multichannel, 325TENS, 338transformer-coupled, 316, 339
INDEX 461Strength-duration curve, 309Supersampling, 224Tachycardia, 312, 371, 407reentry, 411supraventricular, 411ventricular, 412Teledeltos paper, 293Telemetry, 379Testing, see Safety, testTime-domain reflectometer (TDR), 199Titanium, 328, 380Transcranial magnetic stimulation (TMS), 346Transcutaneous electrical nerve stimulation(TENS), 314, 337, 344Tumor, see Cancer treatmentUnderwriters’ Laboratories (UL), 98Vagus nerve stimulation (VNS), 312Ventricle, 369Venture capital, 442, 444Ventricular late potentials, 71Volume conductor, 292Voltage clamp, 305Voltage-controlled oscillator (VCO), 165,228Voltage-to-frequency converter (VFC), 114Voltage-to-impedance converter, 278Wave file format, 271Welch’s method, 238, 242Wilson central terminal, 84WindowHamming, 237, 242Hanning, 237rectangular, 237sampling, 236triangular, 237Zero-padding, 238