Role of Gastrointestinal Hormones in the Proliferation of Normal and ...
Role of Gastrointestinal Hormones in the Proliferation of Normal and ...
Role of Gastrointestinal Hormones in the Proliferation of Normal and ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
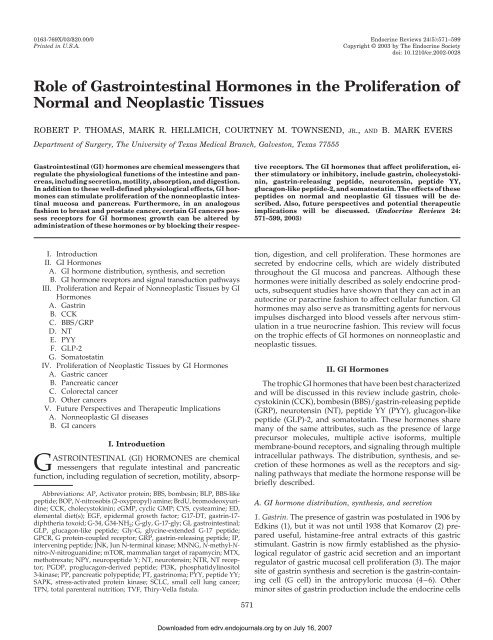
0163-769X/03/$20.00/0 Endocr<strong>in</strong>e Reviews 24(5):571–599Pr<strong>in</strong>ted <strong>in</strong> U.S.A.Copyright © 2003 by The Endocr<strong>in</strong>e Societydoi: 10.1210/er.2002-0028<strong>Role</strong> <strong>of</strong> <strong>Gastro<strong>in</strong>test<strong>in</strong>al</strong> <strong>Hormones</strong> <strong>in</strong> <strong>the</strong> <strong>Proliferation</strong> <strong>of</strong><strong>Normal</strong> <strong>and</strong> Neoplastic TissuesROBERT P. THOMAS, MARK R. HELLMICH, COURTNEY M. TOWNSEND, JR., AND B. MARK EVERSDepartment <strong>of</strong> Surgery, The University <strong>of</strong> Texas Medical Branch, Galveston, Texas 77555<strong>Gastro<strong>in</strong>test<strong>in</strong>al</strong> (GI) hormones are chemical messengers thatregulate <strong>the</strong> physiological functions <strong>of</strong> <strong>the</strong> <strong>in</strong>test<strong>in</strong>e <strong>and</strong> pancreas,<strong>in</strong>clud<strong>in</strong>g secretion, motility, absorption, <strong>and</strong> digestion.In addition to <strong>the</strong>se well-def<strong>in</strong>ed physiological effects, GI hormonescan stimulate proliferation <strong>of</strong> <strong>the</strong> nonneoplastic <strong>in</strong>test<strong>in</strong>almucosa <strong>and</strong> pancreas. Fur<strong>the</strong>rmore, <strong>in</strong> an analogousfashion to breast <strong>and</strong> prostate cancer, certa<strong>in</strong> GI cancers possessreceptors for GI hormones; growth can be altered byadm<strong>in</strong>istration <strong>of</strong> <strong>the</strong>se hormones or by block<strong>in</strong>g <strong>the</strong>ir respectivereceptors. The GI hormones that affect proliferation, ei<strong>the</strong>rstimulatory or <strong>in</strong>hibitory, <strong>in</strong>clude gastr<strong>in</strong>, cholecystok<strong>in</strong><strong>in</strong>,gastr<strong>in</strong>-releas<strong>in</strong>g peptide, neurotens<strong>in</strong>, peptide YY,glucagon-like peptide-2, <strong>and</strong> somatostat<strong>in</strong>. The effects <strong>of</strong> <strong>the</strong>sepeptides on normal <strong>and</strong> neoplastic GI tissues will be described.Also, future perspectives <strong>and</strong> potential <strong>the</strong>rapeuticimplications will be discussed. (Endocr<strong>in</strong>e Reviews 24:571–599, 2003)I. IntroductionII. GI <strong>Hormones</strong>A. GI hormone distribution, syn<strong>the</strong>sis, <strong>and</strong> secretionB. GI hormone receptors <strong>and</strong> signal transduction pathwaysIII. <strong>Proliferation</strong> <strong>and</strong> Repair <strong>of</strong> Nonneoplastic Tissues by GI<strong>Hormones</strong>A. Gastr<strong>in</strong>B. CCKC. BBS/GRPD. NTE. PYYF. GLP-2G. Somatostat<strong>in</strong>IV. <strong>Proliferation</strong> <strong>of</strong> Neoplastic Tissues by GI <strong>Hormones</strong>A. Gastric cancerB. Pancreatic cancerC. Colorectal cancerD. O<strong>the</strong>r cancersV. Future Perspectives <strong>and</strong> Therapeutic ImplicationsA. Nonneoplastic GI diseasesB. GI cancersAbbreviations: AP, Activator prote<strong>in</strong>; BBS, bombes<strong>in</strong>; BLP, BBS-likepeptide; BOP, N-nitrosobis (2-oxypropyl) am<strong>in</strong>e; BrdU, bromodeoxyurid<strong>in</strong>e;CCK, cholecystok<strong>in</strong><strong>in</strong>; cGMP, cyclic GMP; CYS, cysteam<strong>in</strong>e; ED,elemental diet(s); EGF, epidermal growth factor; G17-DT, gastr<strong>in</strong>-17-diph<strong>the</strong>ria toxoid; G-34, G34-NH 2 ; G-gly, G-17-gly; GI, gastro<strong>in</strong>test<strong>in</strong>al;GLP, glucagon-like peptide; Gly-G, glyc<strong>in</strong>e-extended G-17 peptide;GPCR, G prote<strong>in</strong>-coupled receptor; GRP, gastr<strong>in</strong>-releas<strong>in</strong>g peptide; IP,<strong>in</strong>terven<strong>in</strong>g peptide; JNK, Jun N-term<strong>in</strong>al k<strong>in</strong>ase; MNNG, N-methyl-Nnitro-N-nitroguanid<strong>in</strong>e;mTOR, mammalian target <strong>of</strong> rapamyc<strong>in</strong>; MTX,methotrexate; NPY, neuropeptide Y; NT, neurotens<strong>in</strong>; NTR, NT receptor;PGDP, proglucagon-derived peptide; PI3K, phosphatidyl<strong>in</strong>ositol3-k<strong>in</strong>ase; PP, pancreatic polypeptide; PT, gastr<strong>in</strong>oma; PYY, peptide YY;SAPK, stress-activated prote<strong>in</strong> k<strong>in</strong>ase; SCLC, small cell lung cancer;TPN, total parenteral nutrition; TVF, Thiry-Vella fistula.I. IntroductionGASTROINTESTINAL (GI) HORMONES are chemicalmessengers that regulate <strong>in</strong>test<strong>in</strong>al <strong>and</strong> pancreaticfunction, <strong>in</strong>clud<strong>in</strong>g regulation <strong>of</strong> secretion, motility, absorption,digestion, <strong>and</strong> cell proliferation. These hormones aresecreted by endocr<strong>in</strong>e cells, which are widely distributedthroughout <strong>the</strong> GI mucosa <strong>and</strong> pancreas. Although <strong>the</strong>sehormones were <strong>in</strong>itially described as solely endocr<strong>in</strong>e products,subsequent studies have shown that <strong>the</strong>y can act <strong>in</strong> anautocr<strong>in</strong>e or paracr<strong>in</strong>e fashion to affect cellular function. GIhormones may also serve as transmitt<strong>in</strong>g agents for nervousimpulses discharged <strong>in</strong>to blood vessels after nervous stimulation<strong>in</strong> a true neurocr<strong>in</strong>e fashion. This review will focuson <strong>the</strong> trophic effects <strong>of</strong> GI hormones on nonneoplastic <strong>and</strong>neoplastic tissues.II. GI <strong>Hormones</strong>The trophic GI hormones that have been best characterized<strong>and</strong> will be discussed <strong>in</strong> this review <strong>in</strong>clude gastr<strong>in</strong>, cholecystok<strong>in</strong><strong>in</strong>(CCK), bombes<strong>in</strong> (BBS)/gastr<strong>in</strong>-releas<strong>in</strong>g peptide(GRP), neurotens<strong>in</strong> (NT), peptide YY (PYY), glucagon-likepeptide (GLP)-2, <strong>and</strong> somatostat<strong>in</strong>. These hormones sharemany <strong>of</strong> <strong>the</strong> same attributes, such as <strong>the</strong> presence <strong>of</strong> largeprecursor molecules, multiple active is<strong>of</strong>orms, multiplemembrane-bound receptors, <strong>and</strong> signal<strong>in</strong>g through multiple<strong>in</strong>tracellular pathways. The distribution, syn<strong>the</strong>sis, <strong>and</strong> secretion<strong>of</strong> <strong>the</strong>se hormones as well as <strong>the</strong> receptors <strong>and</strong> signal<strong>in</strong>gpathways that mediate <strong>the</strong> hormone response will bebriefly described.A. GI hormone distribution, syn<strong>the</strong>sis, <strong>and</strong> secretion1. Gastr<strong>in</strong>. The presence <strong>of</strong> gastr<strong>in</strong> was postulated <strong>in</strong> 1906 byEdk<strong>in</strong>s (1), but it was not until 1938 that Komarov (2) prepareduseful, histam<strong>in</strong>e-free antral extracts <strong>of</strong> this gastricstimulant. Gastr<strong>in</strong> is now firmly established as <strong>the</strong> physiologicalregulator <strong>of</strong> gastric acid secretion <strong>and</strong> an importantregulator <strong>of</strong> gastric mucosal cell proliferation (3). The majorsite <strong>of</strong> gastr<strong>in</strong> syn<strong>the</strong>sis <strong>and</strong> secretion is <strong>the</strong> gastr<strong>in</strong>-conta<strong>in</strong><strong>in</strong>gcell (G cell) <strong>in</strong> <strong>the</strong> antropyloric mucosa (4–6). O<strong>the</strong>rm<strong>in</strong>or sites <strong>of</strong> gastr<strong>in</strong> production <strong>in</strong>clude <strong>the</strong> endocr<strong>in</strong>e cells571Downloaded from edrv.endojournals.org by on July 16, 2007
572 Endocr<strong>in</strong>e Reviews, October 2003, 24(5):571–599 Thomas et al. • <strong>Gastro<strong>in</strong>test<strong>in</strong>al</strong> <strong>Hormones</strong> <strong>and</strong> <strong>Proliferation</strong><strong>of</strong> <strong>the</strong> pancreas (7), pituitary (8), <strong>and</strong> extraantral G cells (9).Gastr<strong>in</strong> release is stimulated by food components, particularlyaromatic am<strong>in</strong>o acids <strong>and</strong> am<strong>in</strong>e derivatives <strong>of</strong> am<strong>in</strong>oacids, <strong>and</strong> is <strong>in</strong>hibited by lum<strong>in</strong>al acid (10).Human progastr<strong>in</strong>, <strong>the</strong> precursor <strong>of</strong> gastr<strong>in</strong>, consists <strong>of</strong> a21-am<strong>in</strong>o-acid signal peptide, a 37-am<strong>in</strong>o-acid N-term<strong>in</strong>alextension, <strong>the</strong> gastr<strong>in</strong>-34 sequence, <strong>and</strong> a 9-am<strong>in</strong>o-acid C-term<strong>in</strong>al extension (3, 10). In antral G cells, progastr<strong>in</strong> isstored <strong>and</strong> processed <strong>in</strong>to secretory granules, <strong>and</strong> N-term<strong>in</strong>al<strong>and</strong> C-term<strong>in</strong>al extensions are removed by prohormone convertases.The C-term<strong>in</strong>al basic am<strong>in</strong>o acids are sequentiallyremoved by a carboxypeptidase, which results <strong>in</strong> <strong>the</strong> formation<strong>of</strong> glyc<strong>in</strong>e-extended G34 (G34-gly). G34-gly is amidatedby peptidyl glyc<strong>in</strong>e -amidat<strong>in</strong>g monooxygenase t<strong>of</strong>orm G34-NH 2 (G-34) or cleaved at <strong>in</strong>ternal lys<strong>in</strong>e/lys<strong>in</strong>eresidues to form G-17-gly (referred to as G-gly) (10). Recentstudies have demonstrated that <strong>the</strong> majority <strong>of</strong> G-17-NH 2(also known as gastr<strong>in</strong> or G-17) arises from <strong>the</strong> conversion <strong>of</strong>G34-NH 2 to G-17-NH 2 , ra<strong>the</strong>r than by amidation <strong>of</strong> G-gly,suggest<strong>in</strong>g that <strong>the</strong> conversion <strong>of</strong> G-gly to amidated G-17 isblocked <strong>and</strong> that G-gly is a term<strong>in</strong>al, secondary end-product<strong>of</strong> progastr<strong>in</strong> process<strong>in</strong>g <strong>in</strong> normal antral G cells (10, 11). Thisis contrasted by evidence <strong>in</strong> colon cancer cells that gastr<strong>in</strong>bypasses <strong>the</strong> process<strong>in</strong>g mach<strong>in</strong>ery <strong>and</strong> is expressed <strong>in</strong>larger, unprocessed forms that are transported <strong>in</strong> secretoryvesicles <strong>and</strong> cont<strong>in</strong>uously fused with <strong>the</strong> plasma membrane<strong>and</strong> released (11).2. CCK. CCK was described <strong>in</strong> 1928 by Ivy <strong>and</strong> Oldberg (12)as a contam<strong>in</strong>ant <strong>in</strong> impure secret<strong>in</strong> preparations. These impuritieswere noted to produce gallbladder contraction <strong>in</strong>dogs <strong>and</strong> cats. In 1943, Harper <strong>and</strong> Raper (13) identified as<strong>in</strong>gle agent extracted from <strong>in</strong>test<strong>in</strong>al samples that possessedpancreatic-stimulat<strong>in</strong>g activity. After complete purification<strong>and</strong> sequenc<strong>in</strong>g, it was determ<strong>in</strong>ed that this s<strong>in</strong>gle compound,CCK, was responsible for gallbladder contraction<strong>and</strong> pancreatic enzyme secretion (14). O<strong>the</strong>r actions <strong>of</strong> CCK<strong>in</strong>clude <strong>in</strong>hibition <strong>of</strong> gastric empty<strong>in</strong>g, stimulation <strong>of</strong> bowelmotility, potentiation <strong>of</strong> <strong>in</strong>sul<strong>in</strong> secretion, <strong>and</strong> trophic effectson <strong>the</strong> pancreas <strong>and</strong> GI mucosa (3). CCK release is stimulatedby fats, prote<strong>in</strong>s, <strong>and</strong> am<strong>in</strong>o acids.CCK is produced by endocr<strong>in</strong>e cells <strong>of</strong> <strong>the</strong> gut (primarilyduodenum <strong>and</strong> jejunum), <strong>the</strong> neurons <strong>of</strong> <strong>the</strong> bra<strong>in</strong>, <strong>and</strong> <strong>the</strong>peripheral nervous system <strong>of</strong> <strong>the</strong> GI tract (15–18). Ultrastructuralstudies demonstrate that <strong>the</strong> cells are identical to I cells<strong>of</strong> <strong>the</strong> human <strong>in</strong>test<strong>in</strong>e (19). CCK neurons are found <strong>in</strong> <strong>the</strong>myenteric plexus, submucosal plexus, <strong>and</strong> circular musclelayers <strong>of</strong> <strong>the</strong> distal <strong>in</strong>test<strong>in</strong>e <strong>and</strong> colon (9). PostganglionicCCK nerve fibers are found <strong>in</strong> <strong>the</strong> pancreas surround<strong>in</strong>g <strong>the</strong>islets <strong>of</strong> Langerhans (20). Fur<strong>the</strong>rmore, although CCK hasnot been found <strong>in</strong> <strong>the</strong> <strong>in</strong>tr<strong>in</strong>sic neurons <strong>of</strong> <strong>the</strong> stomach <strong>and</strong>duodenum, CCK cells are <strong>in</strong> <strong>the</strong> celiac plexus <strong>and</strong> can befound <strong>in</strong> <strong>the</strong> vagus nerve, especially after <strong>in</strong>jury (21, 22).The molecular forms <strong>of</strong> CCK are diverse <strong>and</strong> appear to betissue-specific (23, 24). The most abundant form <strong>in</strong> <strong>the</strong> bra<strong>in</strong>appears to be CCK-8, although significant amounts <strong>of</strong> largercarboxy-amidated forms like CCK-33, CCK-58, <strong>and</strong> CCK-83have been isolated.3. BBS/GRP. BBS, a tetradecapeptide orig<strong>in</strong>ally isolated from<strong>the</strong> sk<strong>in</strong> <strong>of</strong> <strong>the</strong> frog Bomb<strong>in</strong>a bomb<strong>in</strong>a, is analogous to mammalianGRP (24). In general, BBS/GRP may be thought <strong>of</strong> asa universal on-switch with predom<strong>in</strong>antly stimulatory effects.BBS/GRP stimulates <strong>the</strong> release <strong>of</strong> all GI hormones,<strong>in</strong>test<strong>in</strong>al <strong>and</strong> pancreatic secretion, <strong>and</strong> motility (24). Themost important functions <strong>of</strong> BBS/GRP are antral gastr<strong>in</strong>release <strong>and</strong> stimulation <strong>of</strong> gastric acid secretion (25, 26). Thispeptide also stimulates growth <strong>of</strong> <strong>the</strong> GI mucosa <strong>and</strong> pancreas(24).BBS/GRP-like immunoreactivity is widely distributedthroughout <strong>the</strong> GI tract <strong>of</strong> rats, gu<strong>in</strong>ea pigs, dogs, <strong>and</strong> humans(27–31), predom<strong>in</strong>antly <strong>in</strong> <strong>the</strong> neuronal populations <strong>of</strong><strong>the</strong> gut. GRP is most abundant <strong>in</strong> <strong>the</strong> stomach, with GRPpositivecells <strong>and</strong> fibers <strong>in</strong>nervat<strong>in</strong>g <strong>the</strong> oxyntic <strong>and</strong> antralmucosa <strong>and</strong> circular muscle.4. NT. NT, a tridecapeptide orig<strong>in</strong>ally isolated from bov<strong>in</strong>ehypothalamus (32), is localized ma<strong>in</strong>ly <strong>in</strong> <strong>the</strong> central nervoussystem (predom<strong>in</strong>antly hypothalamus <strong>and</strong> pituitary) <strong>and</strong> <strong>in</strong>endocr<strong>in</strong>e cells (N cells) <strong>of</strong> <strong>the</strong> jejunal <strong>and</strong> ileal mucosa (33,34). NT is released <strong>in</strong> response to <strong>in</strong>creased <strong>in</strong>tralum<strong>in</strong>al fats(35, 36) <strong>and</strong> has numerous functions <strong>in</strong> <strong>the</strong> GI tract, <strong>in</strong>clud<strong>in</strong>gstimulation <strong>of</strong> pancreatic secretion (37), <strong>in</strong>hibition <strong>of</strong> gastric<strong>and</strong> small bowel motility (38), facilitation <strong>of</strong> fatty acid translocationfrom <strong>the</strong> <strong>in</strong>test<strong>in</strong>al lumen (39), <strong>and</strong> growth stimulation<strong>of</strong> various GI tissues (34, 40–43).NT is produced from a s<strong>in</strong>gle precursor, preproneurotens<strong>in</strong>,that conta<strong>in</strong>s both NT 1–13 <strong>and</strong> <strong>the</strong> related peptide,neuromed<strong>in</strong> N. Neuromed<strong>in</strong> N comprises <strong>the</strong> C-term<strong>in</strong>alportion <strong>of</strong> <strong>the</strong> proneurotens<strong>in</strong> peptide after NT is removed.NT 1–13, <strong>the</strong> major product <strong>of</strong> proneurotens<strong>in</strong> <strong>in</strong> <strong>the</strong> ileum<strong>and</strong> bra<strong>in</strong> (44), is cleaved at or soon after secretion at <strong>the</strong>dibasic arg 8 -arg 9 residues, result<strong>in</strong>g <strong>in</strong> <strong>the</strong> <strong>in</strong>active degradationproduct NT 1–8 <strong>and</strong> <strong>the</strong> biologically active NT 9–13.Substance P, muscar<strong>in</strong>ic agonists (carbachol), catecholam<strong>in</strong>es,<strong>and</strong> BBS/GRP stimulate NT release, suggest<strong>in</strong>g that a complex<strong>in</strong>terplay <strong>of</strong> neural, endocr<strong>in</strong>e, <strong>and</strong> lum<strong>in</strong>al mechanisms is responsiblefor NT release <strong>and</strong> physiological function<strong>in</strong>g (45–47).5. PYY. PYY, a 36-am<strong>in</strong>o-acid peptide, is homologous to twoo<strong>the</strong>r regulatory peptides, pancreatic polypeptide (PP) <strong>and</strong>neuropeptide Y (NPY) (3). Both <strong>the</strong> rat <strong>and</strong> human PYY geneshave been isolated <strong>and</strong> characterized (48, 49). The conservedstructural organization <strong>of</strong> <strong>the</strong> genes encod<strong>in</strong>g PYY, NPY, <strong>and</strong>PP suggests that each gene is derived from duplication <strong>of</strong> acommon ancestral gene. The biological actions <strong>of</strong> PYY <strong>in</strong>clude<strong>in</strong>hibition <strong>of</strong> pancreatic bicarbonate secretion <strong>and</strong> contraction<strong>of</strong> <strong>the</strong> gallbladder (50). In addition, PYY <strong>in</strong>hibitsgastric empty<strong>in</strong>g <strong>and</strong> <strong>in</strong>test<strong>in</strong>al transit <strong>and</strong> has been postulatedas an agent that contributes to <strong>the</strong> ileal brake phenomenon,a negative-feedback mechanism that promotes <strong>in</strong>test<strong>in</strong>alabsorption (3). PYY can also stimulate growth <strong>of</strong> <strong>the</strong> GImucosa (51).PYY, NPY, <strong>and</strong> PP are syn<strong>the</strong>sized as prepropeptides consist<strong>in</strong>g<strong>of</strong> a signal peptide followed by <strong>the</strong> 36-residue activepeptide, a cleavage-sequence Gly-Lys-Arg, <strong>and</strong> a carboxyterm<strong>in</strong>alflank<strong>in</strong>g peptide (52, 53). Dur<strong>in</strong>g process<strong>in</strong>g, <strong>the</strong>precursor is cleaved at <strong>the</strong> carboxy term<strong>in</strong>al by a specificprohormone convertase. The Lys-Arg sequences are <strong>the</strong>nlysed by a carboxypeptidase, <strong>and</strong> <strong>the</strong> carboxy-term<strong>in</strong>al tyros<strong>in</strong>eis amidated. Typical enteroendocr<strong>in</strong>e cells, with longDownloaded from edrv.endojournals.org by on July 16, 2007
Thomas et al. • <strong>Gastro<strong>in</strong>test<strong>in</strong>al</strong> <strong>Hormones</strong> <strong>and</strong> <strong>Proliferation</strong> Endocr<strong>in</strong>e Reviews, October 2003, 24(5):571–599 573basal processes, are visualized by immunohistochemistry <strong>in</strong><strong>the</strong> mucosa <strong>of</strong> <strong>the</strong> ileum, colon, <strong>and</strong> rectum (54).6. GLP. GLPs are a group <strong>of</strong> peptides known as <strong>the</strong> enteroglucagons.The enteroglucagons are products <strong>of</strong> <strong>the</strong> samegene that produces glucagon <strong>in</strong> <strong>the</strong> pancreatic -cell (3). The<strong>in</strong>test<strong>in</strong>al L cell produces two elongated glucagons, glicent<strong>in</strong><strong>and</strong> oxyntomodul<strong>in</strong>, <strong>and</strong> both <strong>of</strong> <strong>the</strong> enteroglucagons, GLP-1<strong>and</strong> GLP-2 (55). Both GLP-1 <strong>and</strong> GLP-2 have effects on nutrientabsorption <strong>and</strong> GI tract physiology; however, <strong>the</strong>setwo peptides have dist<strong>in</strong>ct roles. GLP-1 has a significanteffect on blood glucose levels, lower<strong>in</strong>g blood glucose levelsvia stimulation <strong>of</strong> <strong>in</strong>sul<strong>in</strong> secretion (55), thus suggest<strong>in</strong>g thatGLP-1 may provide some <strong>the</strong>rapeutic benefit to patients withdiabetes. GLP-2 displays m<strong>in</strong>imal effects on glucose levels,but demonstrates potent trophic effects on <strong>in</strong>test<strong>in</strong>al epi<strong>the</strong>lia(55).Both GLP-1 <strong>and</strong> GLP-2 are released when <strong>the</strong> L cell isexposed lum<strong>in</strong>ally to <strong>the</strong> products <strong>of</strong> a mixed meal (carbohydrateor fat) (55). L cells are most abundant <strong>in</strong> <strong>the</strong> mucosa<strong>of</strong> <strong>the</strong> ileum <strong>and</strong> colon; <strong>the</strong>y are <strong>the</strong> second most numerouspopulation <strong>of</strong> endocr<strong>in</strong>e cells <strong>in</strong> <strong>the</strong> human <strong>in</strong>test<strong>in</strong>e, afterenterochromaff<strong>in</strong> cells (56). Both GLP-1 <strong>and</strong> GLP-2 are rapidlycleaved by <strong>the</strong> exopeptidase dipeptidyl peptidase IV(55). Current concepts <strong>of</strong> L cell regulation <strong>in</strong>volve <strong>in</strong>tegration<strong>of</strong> hormonal messages from peptides, such as GRP <strong>and</strong> glucose-dependent<strong>in</strong>sul<strong>in</strong>otropic polypeptide, <strong>and</strong> neuronalcontrol (55).7. Somatostat<strong>in</strong>. Somatostat<strong>in</strong> was isolated <strong>and</strong> characterizedfrom ov<strong>in</strong>e hypothalamic tissue dur<strong>in</strong>g a search for a GHreleas<strong>in</strong>gfactor (57). S<strong>in</strong>ce <strong>the</strong> identification <strong>and</strong> purification<strong>of</strong> somatostation-14, precursor forms <strong>of</strong> greater molecularweight, <strong>in</strong>clud<strong>in</strong>g somatostat<strong>in</strong>-28, with somatostat<strong>in</strong>-14mak<strong>in</strong>g up <strong>the</strong> C term<strong>in</strong>us, <strong>and</strong> larger precursor forms <strong>of</strong> 120or more am<strong>in</strong>o acids have been identified (58). All <strong>of</strong> <strong>the</strong>sepeptides exert biological activity but differ <strong>in</strong> <strong>the</strong>ir relativepotency.Somatostat<strong>in</strong> has been detected <strong>in</strong> <strong>the</strong> nerves <strong>and</strong> cellbodies <strong>of</strong> <strong>the</strong> central <strong>and</strong> peripheral nervous systems, <strong>in</strong>clud<strong>in</strong>g<strong>the</strong> autonomic nervous system <strong>of</strong> <strong>the</strong> GI tract <strong>and</strong> <strong>the</strong>endocr<strong>in</strong>e-like D cells <strong>of</strong> <strong>the</strong> pancreatic islets <strong>and</strong> mucosa <strong>of</strong><strong>the</strong> stomach <strong>and</strong> <strong>in</strong>test<strong>in</strong>e (3). More than 90% <strong>of</strong> <strong>the</strong> somatostat<strong>in</strong>immunoreactivity <strong>in</strong> <strong>the</strong> human gut is located with<strong>in</strong><strong>the</strong> mucosal endocr<strong>in</strong>e D cells (58). In addition, somatostat<strong>in</strong>is located <strong>in</strong> <strong>the</strong> nerves <strong>of</strong> <strong>the</strong> myenteric plexus. Somatostat<strong>in</strong><strong>in</strong> <strong>the</strong> pancreas is located <strong>in</strong> <strong>the</strong> D cells at <strong>the</strong> periphery <strong>of</strong> <strong>the</strong>islets closely associated with <strong>the</strong> -cells (59).Somatostat<strong>in</strong> is a regulatory-<strong>in</strong>hibitory peptide, which, <strong>in</strong>contrast to BBS/GRP, may be considered as <strong>the</strong> universalendocr<strong>in</strong>e <strong>of</strong>f-switch. Somatostat<strong>in</strong> <strong>in</strong>hibits <strong>the</strong> release <strong>of</strong> GH<strong>and</strong> somatomed<strong>in</strong> C <strong>and</strong> all known GI hormones (3). Somatostat<strong>in</strong>also <strong>in</strong>hibits gastric acid secretion <strong>and</strong> motility, <strong>in</strong>test<strong>in</strong>alabsorption, <strong>and</strong> pancreatic bicarbonate <strong>and</strong> enzymesecretion, <strong>and</strong> selectively decreases splanchnic <strong>and</strong> portalblood flow (60). In addition, somatostat<strong>in</strong> can <strong>in</strong>hibit <strong>the</strong>growth <strong>of</strong> normal <strong>and</strong> neoplastic tissues (61–67).B. GI hormone receptors <strong>and</strong> signal transduction pathways1. Receptors. GI hormone-stimulated signal transduction occurswith <strong>the</strong> b<strong>in</strong>d<strong>in</strong>g <strong>of</strong> hormones to <strong>the</strong>ir cognate cell surfacereceptor, <strong>the</strong> G prote<strong>in</strong>-coupled receptor (GPCR) (68).The GI hormone-GPCRs have <strong>the</strong> typical structural features<strong>of</strong> G prote<strong>in</strong> b<strong>in</strong>d<strong>in</strong>g seven-transmembrane receptors (Fig. 1).The receptors for gastr<strong>in</strong>, CCK, BBS/GRP, NT, PYY, GLP-2,<strong>and</strong> somatostat<strong>in</strong>, which are respectively, <strong>the</strong> gastr<strong>in</strong>/CCK-Breceptor, CCK-A receptor, GRP receptor, <strong>the</strong> NT receptor(NTR), NPY receptor, GLP-2 receptor, <strong>and</strong> <strong>the</strong> somatostat<strong>in</strong>receptor (five subtypes), are all GPCRs (3, 55). GPCRs regulatea number <strong>of</strong> physiological processes, <strong>in</strong>clud<strong>in</strong>g proliferation,growth, <strong>and</strong> development (68). It was orig<strong>in</strong>allythought that, <strong>in</strong> order for GPCR signal<strong>in</strong>g to occur, specific<strong>in</strong>teractions between <strong>the</strong> GI hormone <strong>and</strong> <strong>the</strong> receptor werenecessary to produce conformational changes <strong>in</strong> <strong>the</strong> receptor<strong>and</strong> stimulate <strong>in</strong>tracellular signal transduction networks.However, recent studies suggest a more complex regulation<strong>of</strong> <strong>the</strong> GPCRs through: 1) dimerization with <strong>the</strong>mselves <strong>and</strong>o<strong>the</strong>r receptors; 2) activation <strong>of</strong> differ<strong>in</strong>g G prote<strong>in</strong>s; 3) <strong>in</strong>ternalization<strong>and</strong> desensitization; <strong>and</strong> 4) ability to change <strong>in</strong>conformation <strong>and</strong> <strong>in</strong>teractions with empty, or <strong>in</strong>active, receptors(69). It is suggested that this complicated mechanism<strong>of</strong> regulation allows peptides to <strong>in</strong>teract with GPCRs to stimulatediverse <strong>in</strong>tracellular signal<strong>in</strong>g pathways <strong>and</strong> ultimatelyaffect multiple physiological functions, depend<strong>in</strong>g on celltype.2. Signal transduction pathways. The seven transmembranespann<strong>in</strong>g-helical doma<strong>in</strong>s function as lig<strong>and</strong>-regulatedguan<strong>in</strong>e nucleotide exchange factors for <strong>the</strong> <strong>in</strong>tracellular heterotrimericG prote<strong>in</strong>s (68). Heterotrimeric G prote<strong>in</strong>s arecomposed <strong>of</strong> <strong>the</strong> products <strong>of</strong> three gene families encod<strong>in</strong>g -,-, <strong>and</strong> -subunits (68). The agonist-activated GPCR catalyzes<strong>the</strong> exchange <strong>of</strong> GTP for GDP bound to <strong>the</strong> G-subunit,as well as <strong>the</strong> dissociation <strong>of</strong> <strong>the</strong> GTP-G from its cognateG dimer (Fig. 2A) (68). The activated GTP-G- <strong>and</strong> Gsubunits,<strong>in</strong> turn, regulate <strong>the</strong> activity <strong>of</strong> various <strong>in</strong>tracellulareffector prote<strong>in</strong>s such as phospholipases, adenylyl cyclases,prote<strong>in</strong> k<strong>in</strong>ases, membrane ion channels, <strong>and</strong> members <strong>of</strong> <strong>the</strong>Ras family <strong>of</strong> GTP-b<strong>in</strong>d<strong>in</strong>g prote<strong>in</strong>s (68). In addition, basedon structural similarities, <strong>the</strong> 20 identified G-subunits havebeen divided <strong>in</strong>to four subfamilies <strong>and</strong> assigned an effectorpathway based on current evidence. The four are: 1) <strong>the</strong>cholera tox<strong>in</strong>-sensitive () subunits that stimulate adenylcyclase <strong>and</strong> <strong>in</strong>crease cAMP levels; 2) <strong>the</strong> pertussis tox<strong>in</strong>sensitive( i/o ) subunits that <strong>in</strong>hibit adenylyl cyclase activity;3) <strong>the</strong> pertussis tox<strong>in</strong>-<strong>in</strong>sensitive ( q/11/14 ) subunits that stimulatemembrane phospholipases; <strong>and</strong> 4) <strong>the</strong> 12/13 subfamilythat l<strong>in</strong>ks GPCR to <strong>the</strong> Ras-related GTP-b<strong>in</strong>d<strong>in</strong>g prote<strong>in</strong>, Rho(68). Additionally, 12 G- <strong>and</strong> 6-G subunits have been identified;<strong>the</strong>se -dimers have been l<strong>in</strong>ked to <strong>the</strong> signal<strong>in</strong>gmolecules phosphatidyl<strong>in</strong>ositol 3-k<strong>in</strong>ase (PI3K) <strong>and</strong> selectforms <strong>of</strong> adenylyl cyclase <strong>and</strong> receptor k<strong>in</strong>ases (68).Among <strong>the</strong> multiple <strong>in</strong>tracellular signal<strong>in</strong>g pathways thatmediate <strong>the</strong> proliferative effects <strong>of</strong> GPCRs, a family <strong>of</strong> relatedser<strong>in</strong>e-threon<strong>in</strong>e k<strong>in</strong>ases, collectively known as ERKs orMAPKs, appear to play a central role (70). After phosphorylationby <strong>the</strong>ir immediate upstream MAPK k<strong>in</strong>ase, members<strong>of</strong> <strong>the</strong> MAPK family translocate to <strong>the</strong> nucleus, where<strong>the</strong>y phosphorylate transcription factors, thus regulat<strong>in</strong>g <strong>the</strong>expression <strong>of</strong> genes that control growth (71). <strong>Hormones</strong> actas lig<strong>and</strong>s to eventually activate p42 <strong>and</strong> p44 MAPK (Fig. 2B)Downloaded from edrv.endojournals.org by on July 16, 2007
574 Endocr<strong>in</strong>e Reviews, October 2003, 24(5):571–599 Thomas et al. • <strong>Gastro<strong>in</strong>test<strong>in</strong>al</strong> <strong>Hormones</strong> <strong>and</strong> <strong>Proliferation</strong>FIG. 1. GPCR: am<strong>in</strong>o acid sequence for <strong>the</strong> structure <strong>of</strong> typical GPCR <strong>in</strong>clud<strong>in</strong>g <strong>the</strong> seven-transmembrane doma<strong>in</strong>s. Am<strong>in</strong>o acid sequences<strong>of</strong> CCK-B (A) <strong>and</strong> CCK-A (B) receptors <strong>in</strong>dicat<strong>in</strong>g similar seven-transmembrane structure <strong>and</strong> about 50% am<strong>in</strong>o acid identity. Identical am<strong>in</strong>oacids are shaded. The NH 2 portion is extracellular, <strong>and</strong> <strong>the</strong> COOH portion is <strong>in</strong>tracellular. [From J. H. Walsh: Physiology <strong>of</strong> <strong>the</strong> <strong>Gastro<strong>in</strong>test<strong>in</strong>al</strong>Tract, Vol 1, pp 1–128, 1994 (3). © Lipp<strong>in</strong>cott Williams & Wilkens.](72). The mechanism by which this occurs <strong>in</strong>volves a complex<strong>in</strong>terplay <strong>of</strong> several known nonreceptor k<strong>in</strong>ases <strong>and</strong> receptork<strong>in</strong>ases. The ability <strong>of</strong> tyros<strong>in</strong>e k<strong>in</strong>ase <strong>in</strong>hibitors to reduce <strong>the</strong>activation <strong>of</strong> MAPK by GPCR (73) <strong>and</strong> <strong>the</strong> rapid tyros<strong>in</strong>ephosphorylation <strong>of</strong> Shc (Src homology <strong>and</strong> collagen) afterGPCR stimulation with <strong>the</strong> consequent formation <strong>of</strong> Shc-Downloaded from edrv.endojournals.org by on July 16, 2007
Thomas et al. • <strong>Gastro<strong>in</strong>test<strong>in</strong>al</strong> <strong>Hormones</strong> <strong>and</strong> <strong>Proliferation</strong> Endocr<strong>in</strong>e Reviews, October 2003, 24(5):571–599 575FIG. 2. Diversity <strong>of</strong> GPCRs. A, <strong>Hormones</strong> use GPCRs to stimulate cytoplasmic <strong>and</strong> nuclear targets through heterotrimeric G prote<strong>in</strong>-dependent<strong>and</strong> -<strong>in</strong>dependent pathways. B, Multiple pathways l<strong>in</strong>k GPCRs to MAPK. Activated MAPK translocates to <strong>the</strong> nucleus <strong>and</strong> phosphorylatesnuclear prote<strong>in</strong>s, <strong>in</strong>clud<strong>in</strong>g transcription factors, <strong>the</strong>reby regulat<strong>in</strong>g gene expression. C, Novel signal<strong>in</strong>g pathways that connect GPCRs to JNK,p38 is<strong>of</strong>orms, <strong>and</strong> big mitogen-activated k<strong>in</strong>ase 1 (ERK5): molecules that l<strong>in</strong>k GPCRs to <strong>the</strong> different members <strong>of</strong> <strong>the</strong> MAPK family. EPAC,Exchange prote<strong>in</strong> activated by cAMP; FAK, focal adhesion k<strong>in</strong>ase; GAP, GTPase-activat<strong>in</strong>g prote<strong>in</strong>; GEF, guan<strong>in</strong>e nucleotide exchange factor;GRF, guan<strong>in</strong>e-nucleotide releas<strong>in</strong>g factor; MEK <strong>and</strong> MKK, MAPK k<strong>in</strong>ase; MEKK, MAPK k<strong>in</strong>ase k<strong>in</strong>ase; MLK, mixed l<strong>in</strong>eage k<strong>in</strong>ase; PKA,prote<strong>in</strong> k<strong>in</strong>ase A; PLC, phospholipase C; PYK2, prol<strong>in</strong>e-rich tyros<strong>in</strong>e k<strong>in</strong>ase 2; RGS, regulator <strong>of</strong> G prote<strong>in</strong> signal<strong>in</strong>g; RTK, receptor tyros<strong>in</strong>ek<strong>in</strong>ase. [Adapted with permission from M. J. Mar<strong>in</strong>issen <strong>and</strong> J. S. Gutk<strong>in</strong>d: Trends Pharmacol Sci 22:368–376, 2001 (68). ©Elsevier Science.]Downloaded from edrv.endojournals.org by on July 16, 2007
576 Endocr<strong>in</strong>e Reviews, October 2003, 24(5):571–599 Thomas et al. • <strong>Gastro<strong>in</strong>test<strong>in</strong>al</strong> <strong>Hormones</strong> <strong>and</strong> <strong>Proliferation</strong>Grb2 (growth factor receptor-bound 2) complexes (74) provideevidence that tyros<strong>in</strong>e k<strong>in</strong>ases l<strong>in</strong>k GPCRs to <strong>the</strong> Ras-MAPK pathway.Additionally, GPCRs l<strong>in</strong>k to <strong>the</strong> Jun N-term<strong>in</strong>al k<strong>in</strong>ase(JNK), p38 MAPK, <strong>and</strong> <strong>the</strong> big mitogen-activated k<strong>in</strong>ase 1 orERK5 pathways (Fig. 2C) (68). JNK, also termed stress-activatedprote<strong>in</strong> k<strong>in</strong>ase (SAPK), is structurally related toMAPK, but <strong>the</strong> pathways used by GPCRs to activate <strong>the</strong>sek<strong>in</strong>ases are different. Activated Rac <strong>and</strong> Cdc42 affect JNKactivation through stimulation from free -dimers <strong>and</strong> G 12<strong>and</strong> G 13 .Four p38 MAPKs have been described, p38 (CSBP-1), p38, p38 (ERK6 or SAPK3), <strong>and</strong> p38 (SAPK4) (75). Yamauchiet al. (76) demonstrated that G q <strong>and</strong> dimers activatep38. Two nonreceptor tyros<strong>in</strong>e k<strong>in</strong>ases, Btk <strong>and</strong> Src (77, 78),have been associated with this process. ERK5 can be activatedby oxidative stress <strong>and</strong> plays a role <strong>in</strong> early geneexpression (79). GPCRs can potently stimulate ERK5 througha mechanism that <strong>in</strong>volves G q <strong>and</strong> G 13 , <strong>in</strong>dependent <strong>of</strong>Rho, Rac1, <strong>and</strong> Cdc42 (80, 81). Fur<strong>the</strong>rmore, ERK5 regulatesearly gene expression through <strong>the</strong> phosphorylation <strong>of</strong> <strong>the</strong>transcription factor, myocyte enhancer factor 2 (80).The molecular mechanisms through which GPCRs transducesignals are complex <strong>and</strong> likely <strong>in</strong>volve multiple signalpathways. In addition, <strong>the</strong> signal<strong>in</strong>g pathways are likelycell-specific, which may expla<strong>in</strong> <strong>the</strong> diverse physiologicalfunctions controlled by GI hormones rang<strong>in</strong>g from regulation<strong>of</strong> secretion, mobility, <strong>and</strong>, <strong>in</strong> some <strong>in</strong>stances, growthdepend<strong>in</strong>g upon <strong>the</strong> target tissue.III. <strong>Proliferation</strong> <strong>and</strong> Repair <strong>of</strong> NonneoplasticTissues by GI <strong>Hormones</strong>GI hormones can alter proliferation <strong>of</strong> <strong>the</strong> normal gut <strong>and</strong>pancreas. In this section, we will review <strong>the</strong> effects <strong>of</strong> <strong>the</strong>stimulatory hormones gastr<strong>in</strong>, CCK, BBS/GRP, NT, PYY,<strong>and</strong> GLP-2 <strong>and</strong> <strong>the</strong> <strong>in</strong>hibitory hormone, somatostat<strong>in</strong>, on <strong>the</strong>growth <strong>of</strong> <strong>the</strong> pancreas <strong>and</strong> mucosa <strong>of</strong> <strong>the</strong> GI tract.A. Gastr<strong>in</strong>Gastr<strong>in</strong> is <strong>the</strong> GI hormone that has been best characterizedfor its trophic effects. In addition to stimulat<strong>in</strong>g acid secretionfrom gastric parietal cells, gastr<strong>in</strong> is <strong>the</strong> s<strong>in</strong>gle most importanttrophic hormone <strong>of</strong> <strong>the</strong> stomach (82).1. Stomach. The trophic effect <strong>of</strong> gastr<strong>in</strong> was <strong>in</strong>itially describedmore than 30 yr ago <strong>in</strong> two separate reports. Johnsonet al. (83) <strong>and</strong> Crean et al. (84) demonstrated that pentagastr<strong>in</strong>,a syn<strong>the</strong>tic gastr<strong>in</strong> analog conta<strong>in</strong><strong>in</strong>g <strong>the</strong> active carboxylterm<strong>in</strong>altetrapeptide, <strong>in</strong>creased prote<strong>in</strong> syn<strong>the</strong>sis <strong>and</strong> parietalcell mass <strong>in</strong> rats. These results were fur<strong>the</strong>r confirmedus<strong>in</strong>g <strong>the</strong> natural amidated gastr<strong>in</strong>s, G-17 <strong>and</strong> G-34. G-17 <strong>and</strong>G-34 produced maximal stimulation <strong>of</strong> DNA syn<strong>the</strong>sis <strong>in</strong> <strong>the</strong>oxyntic mucosa, duodenum, <strong>and</strong> colon at doses <strong>of</strong> 13.5 <strong>and</strong>6.75 nmol/kg, respectively.In <strong>the</strong> stomach, <strong>the</strong> oxyntic, acid-secret<strong>in</strong>g mucosa <strong>and</strong>enterochromaff<strong>in</strong>-like cells (cells that produce histam<strong>in</strong>escritical to parietal cell acid production) are particularly sensitiveto <strong>the</strong> trophic actions <strong>of</strong> gastr<strong>in</strong> (85). The removal <strong>of</strong>endogenous gastr<strong>in</strong>, by antral resection, results <strong>in</strong> mucosalatrophy that can be prevented by adm<strong>in</strong>ister<strong>in</strong>g exogenousgastr<strong>in</strong>.Overexpression <strong>of</strong> ei<strong>the</strong>r unprocessed gastr<strong>in</strong>s or <strong>the</strong> amidatedgastr<strong>in</strong>s (G-17 <strong>and</strong> G-34) <strong>in</strong> transgenic mice results <strong>in</strong>a 2-fold elevation <strong>in</strong> serum-amidated gastr<strong>in</strong> <strong>and</strong> producesmarked thicken<strong>in</strong>g <strong>of</strong> <strong>the</strong> oxyntic mucosa with <strong>in</strong>creasedbromodeoxyurid<strong>in</strong>e (BrdU) label<strong>in</strong>g, represent<strong>in</strong>g an 85%<strong>in</strong>crease <strong>in</strong> cells undergo<strong>in</strong>g proliferation (86, 87). These f<strong>in</strong>d<strong>in</strong>gsare fur<strong>the</strong>r supported by results <strong>in</strong> athymic nude micebear<strong>in</strong>g xenografts <strong>of</strong> a transplanted human gastr<strong>in</strong>oma (PT)demonstrat<strong>in</strong>g gastric <strong>and</strong> duodenal mucosal hyperplasia(Fig. 3) (Ref. 88).In gastr<strong>in</strong>-deficient mice (89, 90), a 35% decrease <strong>in</strong> parietalcell mass with no decrease <strong>in</strong> basal fundic proliferation ratesis noted, compared with wild-type control mice, suggest<strong>in</strong>gthat, although gastr<strong>in</strong> can stimulate proliferation, it is notnecessarily required for basal proliferation. Taken toge<strong>the</strong>r,<strong>the</strong>se experimental results, us<strong>in</strong>g different <strong>in</strong> vivo models,<strong>in</strong>dicate that amidated gastr<strong>in</strong> can stimulate proliferation <strong>of</strong><strong>the</strong> oxyntic mucosa, result<strong>in</strong>g <strong>in</strong> <strong>in</strong>creased parietal <strong>and</strong> enterochromaff<strong>in</strong>-likecell production.2. Small <strong>in</strong>test<strong>in</strong>e. The role <strong>of</strong> gastr<strong>in</strong> as a stimulant for smallbowel mucosal growth is less clear. Johnson et al. (83) showedthat [ 3 H]thymid<strong>in</strong>e <strong>in</strong>corporation <strong>and</strong> DNA syn<strong>the</strong>sis <strong>of</strong> ratduodenal tissues were significantly <strong>in</strong>creased by pentagas-FIG. 3. Human PT xenografts produce gastr<strong>in</strong>, result<strong>in</strong>g<strong>in</strong> gastric <strong>and</strong> duodenal mucosal growth. A, Stomachsopened along greater curvature from mice with PTtumors (top) <strong>and</strong> controls (bottom). B, Effects <strong>of</strong> PT on<strong>the</strong> mouse gastric fundus (n 5 PT mice; n 10 controlmice; *, P 0.05). [Adapted with permission from J. R.Upp Jr. et al.: Surgery 104:1037–1045, 1988 (88). ©Mosby, Inc.]Downloaded from edrv.endojournals.org by on July 16, 2007
Thomas et al. • <strong>Gastro<strong>in</strong>test<strong>in</strong>al</strong> <strong>Hormones</strong> <strong>and</strong> <strong>Proliferation</strong> Endocr<strong>in</strong>e Reviews, October 2003, 24(5):571–599 577tr<strong>in</strong>, G-17, <strong>and</strong> G-34 adm<strong>in</strong>istration. Schwartz <strong>and</strong> Storozuk(91) found that exogenous gastr<strong>in</strong> (13.5 nmol/kgd) enhancedgrowth <strong>of</strong> jejunoileal segments obta<strong>in</strong>ed from 19- to20-d gestation fetal rats transplanted sc <strong>in</strong> adult rats. Inaddition, adm<strong>in</strong>istration <strong>of</strong> gastr<strong>in</strong> enhanced <strong>the</strong> absorption<strong>of</strong> galactose <strong>and</strong> glyc<strong>in</strong>e, suggest<strong>in</strong>g that gastr<strong>in</strong> <strong>in</strong>creasesfunctional activity as well as growth. Subsequent studies,however, us<strong>in</strong>g both pentagastr<strong>in</strong> <strong>and</strong> natural G-17 havefailed to demonstrate significant trophic effects <strong>of</strong> gastr<strong>in</strong> <strong>in</strong><strong>the</strong> small bowel (jejunum <strong>and</strong> ileum) mucosa <strong>of</strong> <strong>the</strong> adult ratas measured by v<strong>in</strong>crist<strong>in</strong>e-arrested metaphase (92). An explanationfor <strong>the</strong>se differ<strong>in</strong>g results is not entirely clear butmay perta<strong>in</strong> to different experimental measures <strong>of</strong> proliferation.Therefore, although <strong>the</strong> trophic effects <strong>in</strong> <strong>the</strong> oxyntic<strong>and</strong> duodenal mucosa are well established, <strong>the</strong> trophic effect<strong>of</strong> gastr<strong>in</strong> <strong>in</strong> <strong>the</strong> rema<strong>in</strong><strong>in</strong>g small <strong>in</strong>test<strong>in</strong>e is currently consideredm<strong>in</strong>imal, at best.3. Colon. Similar to <strong>the</strong> small bowel, evidence for a trophiceffect <strong>of</strong> gastr<strong>in</strong> <strong>in</strong> <strong>the</strong> colon is limited. In earlier studies byJohnson (93), adm<strong>in</strong>istration <strong>of</strong> natural porc<strong>in</strong>e gastr<strong>in</strong>s stimulatedDNA syn<strong>the</strong>sis <strong>in</strong> <strong>the</strong> colon. In contrast, hypergastremia,<strong>in</strong>duced through acid blockade by ei<strong>the</strong>r omeprazoleadm<strong>in</strong>istration (94) or fundectomy (95), failed to produceproliferation <strong>of</strong> ei<strong>the</strong>r normal colon or <strong>the</strong> colon carc<strong>in</strong>omacells transplanted from an orig<strong>in</strong>al 1,2-dimethylhydraz<strong>in</strong>e<strong>in</strong>ducedadenocarc<strong>in</strong>oma.As opposed to results us<strong>in</strong>g amidated gastr<strong>in</strong>, recent experimentsus<strong>in</strong>g G-gly demonstrate colonic proliferation,spark<strong>in</strong>g renewed <strong>in</strong>terest <strong>in</strong> a role for gastr<strong>in</strong> precursorproducts <strong>in</strong> colonic growth. Koh et al. (96) generated micethat overexpress progastr<strong>in</strong> truncated at glyc<strong>in</strong>e-72 (MTI/G-GLY), which demonstrates elevated serum <strong>and</strong> mucosallevels <strong>of</strong> G-gly compared with wild-type mice. MTI/G-GLYmice display a 43% <strong>in</strong>crease <strong>in</strong> colonic mucosal thickness <strong>and</strong>a 41% <strong>in</strong>crease <strong>in</strong> <strong>the</strong> percentage <strong>of</strong> goblet cells per crypt.Fur<strong>the</strong>rmore, adm<strong>in</strong>istration <strong>of</strong> G-gly to gastr<strong>in</strong>-deficientmice resulted <strong>in</strong> a 10% <strong>in</strong>crease <strong>in</strong> colonic mucosal thickness<strong>and</strong> an 81% <strong>in</strong>crease <strong>in</strong> colonic proliferation (as measured byBrdU) when compared with control mice. Thus, <strong>the</strong>se data,us<strong>in</strong>g exogenous adm<strong>in</strong>istration <strong>and</strong> genetic mouse models,demonstrate that G-gly is a potent stimulator <strong>of</strong> colonicproliferation.4. Pancreas. The role <strong>of</strong> gastr<strong>in</strong> <strong>in</strong> normal pancreatic growthis also believed to be stimulatory. In two separate studies,<strong>in</strong>vestigators <strong>in</strong> our laboratory have demonstrated small,albeit significant, <strong>in</strong>creases <strong>in</strong> pancreatic growth. In <strong>the</strong> firststudy, young adult rats were given pentagastr<strong>in</strong>, NT, or BBS<strong>in</strong> comb<strong>in</strong>ation with an elemental diet (ED) (33). Pentagastr<strong>in</strong>at a maximal dose, 250 g/kg, <strong>in</strong>creased pancreatic weightcompared with control rats. In <strong>the</strong> second study, pentagastr<strong>in</strong>(100 g/kg) was given to young (3-month-old), adult(12-month-old), <strong>and</strong> aged (24-month-old) rats (97). In youngrats, pentagastr<strong>in</strong> <strong>in</strong>creased pancreatic weight, DNA, RNA,<strong>and</strong> prote<strong>in</strong> content. In adult rats, however, pentagastr<strong>in</strong>only produced <strong>in</strong>creases <strong>in</strong> RNA content, whereas aged ratsshowed no trophic effect. These results suggest that <strong>the</strong> effects<strong>of</strong> gastr<strong>in</strong> on pancreatic growth are dependent uponage. Fur<strong>the</strong>r support for a stimulatory effect <strong>of</strong> gastr<strong>in</strong> onpancreatic cells is provided by <strong>in</strong> vitro studies us<strong>in</strong>g <strong>the</strong> ratpancreatic ac<strong>in</strong>ar cancer cell l<strong>in</strong>e, AR42J, demonstrat<strong>in</strong>g thatgastr<strong>in</strong>s can <strong>in</strong>duce cellular proliferation through stimulation<strong>of</strong> <strong>the</strong> c-fos transcription factor via prote<strong>in</strong> k<strong>in</strong>ase C-dependent <strong>and</strong> <strong>in</strong>dependent mechanisms (98).In contrast, Chen et al. (99) <strong>in</strong>duced hypergastr<strong>in</strong>emia <strong>in</strong>male Sprague-Dawley rats by cont<strong>in</strong>uous <strong>in</strong>fusion <strong>of</strong> humanLeu 15-gastr<strong>in</strong>-17, by fundectomy, or by treatment with omeprazole.Gastr<strong>in</strong> <strong>in</strong>fusion or omeprazole treatment did notaffect pancreatic weight <strong>and</strong> DNA content, whereas fundectomy<strong>in</strong>creased pancreatic weight <strong>and</strong> DNA content. Thesef<strong>in</strong>d<strong>in</strong>gs suggest that endogenous gastr<strong>in</strong> level variations donot directly play a role <strong>in</strong> pancreatic growth. Fur<strong>the</strong>r studiesare needed to conclusively establish <strong>the</strong> differences <strong>in</strong>gastr<strong>in</strong>-related hormonal signal<strong>in</strong>g affect<strong>in</strong>g <strong>the</strong> growth <strong>of</strong><strong>the</strong> pancreas.B. CCKCCK, act<strong>in</strong>g through CCK-A receptors, is one <strong>of</strong> <strong>the</strong> mostpotent secretagogues regulat<strong>in</strong>g pancreatic ac<strong>in</strong>ar cells (100).Additionally, CCK stimulates <strong>the</strong> growth <strong>of</strong> <strong>the</strong> pancreas <strong>in</strong>experimental studies (101, 102). However, evidence for CCKplay<strong>in</strong>g a major role <strong>in</strong> <strong>the</strong> growth <strong>of</strong> <strong>the</strong> GI mucosa (stomach,small bowel, <strong>and</strong> colon) is limited.1. GI mucosa. Adm<strong>in</strong>istration <strong>of</strong> CCK <strong>and</strong> secret<strong>in</strong> preventedatrophy <strong>in</strong> <strong>the</strong> jejunum <strong>and</strong> ileum <strong>of</strong> dogs given total parenteralnutrition (TPN) as a sole nutrient source (103). Inaddition, adm<strong>in</strong>istration <strong>of</strong> <strong>the</strong>se peptides <strong>in</strong>creased galactoseabsorption, suggest<strong>in</strong>g that CCK is a positive enterotrophicfactor for <strong>the</strong> gut. Weser et al. (104) provided additionalevidence that CCK alone, or <strong>in</strong> comb<strong>in</strong>ation withsecret<strong>in</strong>, could prevent TPN-associated jejunal <strong>and</strong> ileal atrophy<strong>in</strong> rats. In subsequent studies, F<strong>in</strong>e et al. (105), us<strong>in</strong>g<strong>in</strong>test<strong>in</strong>al bypass models, demonstrated that <strong>the</strong> trophic responsenoted by CCK <strong>and</strong> secret<strong>in</strong> <strong>in</strong> <strong>the</strong> small bowel was <strong>the</strong><strong>in</strong>direct result <strong>of</strong> <strong>in</strong>creased pancreatobiliary secretion, as opposedto a direct stimulatory effect <strong>of</strong> <strong>the</strong>se peptides on <strong>the</strong>gut mucosa. Confirmation <strong>of</strong> <strong>the</strong> lack <strong>of</strong> a direct effect <strong>of</strong> CCKon small bowel growth was provided by Stange et al. (106)us<strong>in</strong>g cultured rabbit jejunum <strong>and</strong> ileum preparations.2. Pancreas. In contrast, <strong>the</strong> trophic effects <strong>of</strong> CCK on <strong>the</strong>pancreas have been demonstrated by a number <strong>of</strong> experimentalmodels (107–113). In one study, <strong>the</strong> effects <strong>of</strong> camostate(400 mg/kg), a potent <strong>in</strong>hibitor <strong>of</strong> tryps<strong>in</strong> (which blocksser<strong>in</strong>e proteases), were compared with <strong>the</strong> effects <strong>of</strong> chronicexogenous adm<strong>in</strong>istration <strong>of</strong> CCK-8 with or without adm<strong>in</strong>istration<strong>of</strong> <strong>the</strong> CCK-receptor antagonist, CR 1409 (114).Chronic (10-d) camostate feed<strong>in</strong>g <strong>in</strong>creased pancreaticweight, prote<strong>in</strong>, <strong>and</strong> DNA content, which was associatedwith <strong>in</strong>creased CCK plasma levels. The adm<strong>in</strong>istration <strong>of</strong>exogenous CCK produced similar <strong>in</strong>creases <strong>in</strong> pancreaticgrowth. The comb<strong>in</strong>ation <strong>of</strong> camostate <strong>and</strong> CCK-8 producedan additive stimulatory effect on <strong>the</strong> pancreas. The CCKreceptorantagonist, CR 1409, completely abolished <strong>the</strong> trophiceffects <strong>of</strong> exogenous CCK-8 <strong>and</strong> <strong>in</strong>hibited <strong>the</strong> effects <strong>of</strong>chronic camostate feed<strong>in</strong>g. Fur<strong>the</strong>rmore, CR 1409 alone decreasedpancreatic weight, DNA, <strong>and</strong> prote<strong>in</strong> content <strong>of</strong> rats.Additionally, o<strong>the</strong>r studies have substantiated <strong>and</strong> con-Downloaded from edrv.endojournals.org by on July 16, 2007
578 Endocr<strong>in</strong>e Reviews, October 2003, 24(5):571–599 Thomas et al. • <strong>Gastro<strong>in</strong>test<strong>in</strong>al</strong> <strong>Hormones</strong> <strong>and</strong> <strong>Proliferation</strong>firmed a stimulatory effect <strong>of</strong> CCK on <strong>the</strong> pancreas (110–113).Taken toge<strong>the</strong>r, <strong>the</strong>se studies provide clear evidence thatCCK is a potent stimulant for pancreatic growth.Recently, <strong>the</strong> cellular mechanisms regulat<strong>in</strong>g <strong>the</strong> proliferativeeffect <strong>of</strong> CCK have been exam<strong>in</strong>ed. Similar to gastr<strong>in</strong>,CCK activates <strong>the</strong> MAPK cascade, lead<strong>in</strong>g to <strong>the</strong> activation<strong>of</strong> ERK, JNK, <strong>and</strong> p38 MAPK <strong>in</strong> <strong>the</strong> pancreas (115). In addition,<strong>the</strong>re is evidence that o<strong>the</strong>r signal<strong>in</strong>g pathways, suchas <strong>the</strong> PI3K-mTOR (mammalian target <strong>of</strong> rapamyc<strong>in</strong>)-p70 s6kpathway, are <strong>in</strong>volved <strong>in</strong> CCK-stimulated mitogenesis <strong>and</strong>cellular proliferation (115). p70 s6k is physiologically importantfor phosphorylat<strong>in</strong>g <strong>the</strong> small ribosomal subunit prote<strong>in</strong>S6, which was <strong>the</strong> first regulated phosphoprote<strong>in</strong> identified<strong>in</strong> pancreatic ac<strong>in</strong>ar cells (115), <strong>the</strong>reby facilitat<strong>in</strong>g <strong>the</strong> syn<strong>the</strong>sis<strong>of</strong> RNA. Bragado et al. (116) demonstrated <strong>the</strong> phosphorylation<strong>and</strong> activation <strong>of</strong> p70 s6k <strong>in</strong> rat pancreatic ac<strong>in</strong>i byCCK, carbachol, <strong>and</strong> BBS, but not by cAMP, phorbol ester, orcalcium ionophore. This activation was blocked by rapamyc<strong>in</strong>,which <strong>in</strong>hibits mTOR, <strong>and</strong> by wortmann<strong>in</strong> (a PI3K <strong>in</strong>hibitor).In addition, <strong>the</strong> PI3K-mTOR pathway is known toplay a role <strong>in</strong> activat<strong>in</strong>g prote<strong>in</strong> syn<strong>the</strong>sis by phosphorylat<strong>in</strong>g<strong>the</strong> b<strong>in</strong>d<strong>in</strong>g prote<strong>in</strong> eIF4E, <strong>the</strong> translation <strong>in</strong>itiation factorthat b<strong>in</strong>ds to <strong>the</strong> 7-methyl guanos<strong>in</strong>e cap at <strong>the</strong> 5 end <strong>of</strong> mosteukaryotic mRNA molecules (117). This b<strong>in</strong>d<strong>in</strong>g prote<strong>in</strong>,known as eIF4E-BP or PHAS-I, possesses multiple phosphorylatedsites <strong>and</strong>, when sufficiently phosphorylated, dissociatesfrom eIF4E, which can <strong>the</strong>n <strong>in</strong>teract with eIF4G (a scaffoldprote<strong>in</strong>) toge<strong>the</strong>r with eIF4A (a RNA helicase) to forma complex, known as eIF4F, <strong>and</strong> stimulate prote<strong>in</strong> syn<strong>the</strong>sis.CCK stimulation <strong>of</strong> rat pancreatic ac<strong>in</strong>i leads to PHAS-Iphosphorylation <strong>and</strong> <strong>in</strong>itiation <strong>of</strong> a complex formation (118).C. BBS/GRPBBS/GRP stimulates pancreatic, gastric, <strong>and</strong> <strong>in</strong>test<strong>in</strong>al secretion,<strong>and</strong> gut motility, smooth muscle contraction, <strong>and</strong>release <strong>of</strong> all gut hormones (29). In addition, BBS/GRP is apotent trophic factor for <strong>the</strong> GI tract <strong>and</strong> pancreas.1. Stomach. Lehy <strong>and</strong> colleagues (119, 120) reported that BBS,given orally or sc, stimulated <strong>the</strong> growth <strong>of</strong> gut mucosa <strong>and</strong>pancreas <strong>in</strong> neonatal rats. In this study, 7-d-old rats were<strong>in</strong>jected sc with BBS (20 g/kg) twice daily for 6 d. Gastricweight, fundic <strong>and</strong> antral mucosal height, <strong>and</strong> <strong>the</strong> density <strong>of</strong>parietal cells were <strong>in</strong>creased <strong>in</strong> BBS-treated pups comparedwith sal<strong>in</strong>e-treated controls.Demb<strong>in</strong>ski et al. (121, 122) demonstrated that BBS, adm<strong>in</strong>isteredto rats for 7 successive days, significantly <strong>in</strong>creased<strong>the</strong> weight <strong>and</strong> RNA <strong>and</strong> DNA contents <strong>of</strong> <strong>the</strong> oxyntic mucosa<strong>of</strong> <strong>the</strong> stomach <strong>and</strong> <strong>the</strong> duodenal mucosa; somatostat<strong>in</strong>attenuated <strong>the</strong> proliferative effect <strong>of</strong> BBS. Antrectomy, whichremoves <strong>the</strong> gastr<strong>in</strong>-secret<strong>in</strong>g cells, <strong>and</strong> <strong>the</strong> CCK receptor<strong>in</strong>hibitor, L-364,718, partly reduced but did not abolish <strong>the</strong>proliferative effects <strong>of</strong> BSS, suggest<strong>in</strong>g that <strong>the</strong> grow<strong>the</strong>nhanc<strong>in</strong>gmechanisms <strong>of</strong> BBS <strong>in</strong>volved gastr<strong>in</strong> <strong>and</strong> CCKstimulation. More importantly, <strong>the</strong>se studies confirmed thatBBS had direct effects on <strong>the</strong> gastroduodenal mucosa.Later, Demb<strong>in</strong>ski et al. (122) extended <strong>the</strong>ir <strong>in</strong>itial f<strong>in</strong>d<strong>in</strong>gsby assess<strong>in</strong>g <strong>the</strong> effects <strong>of</strong> <strong>the</strong> BBS/GRP receptor antagonist,RC-3095, on BBS-mediated growth. BBS (10 g/kg) adm<strong>in</strong>isteredthree times daily for 2d<strong>in</strong>fasted rats significantly<strong>in</strong>creased <strong>the</strong> rate <strong>of</strong> DNA syn<strong>the</strong>sis <strong>in</strong> <strong>the</strong> gastroduodenalmucosa <strong>and</strong> pancreas as measured by <strong>the</strong> <strong>in</strong>corporation <strong>of</strong>[ 3 H]thymid<strong>in</strong>e; this proliferative effect was abolished by RC-3095. These results provide fur<strong>the</strong>r evidence that BBS/GRPstimulates <strong>the</strong> growth <strong>of</strong> <strong>the</strong> stomach <strong>and</strong> duodenum <strong>and</strong>that <strong>the</strong>se effects are due predom<strong>in</strong>antly to a direct effect <strong>of</strong>BBS/GRP stimulation.2. Small <strong>in</strong>test<strong>in</strong>e. BBS also stimulates growth <strong>of</strong> <strong>the</strong> rema<strong>in</strong>der<strong>of</strong> <strong>the</strong> small bowel mucosa. We exam<strong>in</strong>ed <strong>the</strong> effects <strong>of</strong> BBS<strong>in</strong> <strong>the</strong> prevention <strong>of</strong> gut mucosal atrophy <strong>in</strong> Sprague-Dawleyrats given liquid ED (33). Four groups <strong>of</strong> rats were given anED <strong>and</strong> <strong>in</strong>jected with sal<strong>in</strong>e (control), pentagastr<strong>in</strong> (250 g/kg), NT (300 g/kg), or BBS (10 g/kg) sc every 8 h. A fifthgroup was fed a regular chow diet. Atrophy <strong>of</strong> <strong>the</strong> ilealmucosa was apparent on d 6 <strong>and</strong> 11, <strong>and</strong> atrophy <strong>of</strong> <strong>the</strong>jejunal mucosa was present by d 11. BBS prevented jejunalmucosal atrophy <strong>and</strong> significantly <strong>in</strong>creased ileal mucosalgrowth (mucosal weight, RNA, DNA, prote<strong>in</strong> content) comparedwith control.Chu et al. (123) determ<strong>in</strong>ed whe<strong>the</strong>r <strong>the</strong> trophic actions <strong>of</strong>BBS on <strong>the</strong> small bowel were mediated by nonlum<strong>in</strong>al orlum<strong>in</strong>al (i.e., pancreaticobiliary secretion) factors by construction<strong>of</strong> isolated small bowel loops [i.e., Thiry-Vella fistulas(TVFs)]. BBS <strong>in</strong>creased mucosal weight, DNA, <strong>and</strong> prote<strong>in</strong>content <strong>in</strong> both jejunal <strong>and</strong> ileal TVF compared withcontrol animals, suggest<strong>in</strong>g that BBS-mediated stimulation<strong>of</strong> small bowel mucosal growth is mediated by factors thatare <strong>in</strong>dependent <strong>of</strong> lum<strong>in</strong>al contents <strong>and</strong> pancreaticobiliarysecretion.In addition to its effects on gut mucosal growth, BBS exhibitsprotective effects <strong>in</strong> <strong>the</strong> gut after <strong>in</strong>jury. Us<strong>in</strong>g a lethalenterocolitis model <strong>in</strong> rats <strong>in</strong>duced by <strong>the</strong> chemo<strong>the</strong>rapeuticagent methotrexate (MTX), BBS enhanced gut mucosalgrowth <strong>and</strong> significantly <strong>in</strong>hibited mortality <strong>in</strong> rats (124). Thebeneficial effect <strong>of</strong> BBS on survival was noted when BBS wasgiven before or at <strong>the</strong> same time as MTX, which suggestedthat BBS may act through additional mechanisms o<strong>the</strong>r thangut mucosal growth alone. One possibility is that BBS mayproduce its beneficial effects through enhancement <strong>of</strong> <strong>the</strong>immune system, which is a known action <strong>of</strong> BBS (125).3. Colon. Studies assess<strong>in</strong>g <strong>the</strong> effects <strong>of</strong> BBS/GRP on <strong>the</strong>colonic mucosa are limited but, similar to <strong>the</strong> small bowel,appear to support a trophic effect <strong>of</strong> this agent <strong>in</strong> <strong>the</strong> colon.Johnson <strong>and</strong> Guthrie (126) demonstrated that BBS (20 g/kg,three times daily for 7 d) stimulated colonic mucosal growth.Puccio <strong>and</strong> Lehy (119) found that adm<strong>in</strong>istration <strong>of</strong> BBSorally <strong>in</strong> <strong>the</strong> neonatal period stimulated colonic growth. Incontrast, we have not detected a proliferative effect <strong>of</strong> BBS <strong>in</strong><strong>the</strong> colon <strong>of</strong> chow-fed rats after 7 or 14 d (127). In rats givenan ED, BBS produced a proliferative effect only <strong>in</strong> <strong>the</strong> proximalcolon. Therefore, although BBS appears to exert a trophiceffect on <strong>the</strong> colonic mucosa, <strong>the</strong> effects are less pronouncedthan <strong>in</strong> <strong>the</strong> stomach or small bowel.4. Pancreas. A number <strong>of</strong> studies have shown that BBS stimulates<strong>the</strong> growth <strong>of</strong> <strong>the</strong> pancreas (97, 119, 120, 128). Forexample, Lehy <strong>and</strong> colleagues (119, 120) demonstrated atrophic response for BBS <strong>in</strong> <strong>the</strong> pancreas as well as o<strong>the</strong>r GIDownloaded from edrv.endojournals.org by on July 16, 2007
Thomas et al. • <strong>Gastro<strong>in</strong>test<strong>in</strong>al</strong> <strong>Hormones</strong> <strong>and</strong> <strong>Proliferation</strong> Endocr<strong>in</strong>e Reviews, October 2003, 24(5):571–599 579tissues. In addition, electron morphometric analysis <strong>in</strong>dicatedthat <strong>the</strong> <strong>in</strong>crease <strong>in</strong> pancreatic weight was due to hypertrophy<strong>of</strong> <strong>the</strong> ac<strong>in</strong>ar cells. Increases <strong>in</strong> pancreatic chymotryps<strong>in</strong><strong>and</strong> tryps<strong>in</strong>ogen content were noted, with little effecton lipase or colipase <strong>and</strong> amylase levels. Similar to its effectson <strong>the</strong> pancreatic ac<strong>in</strong>i, BBS stimulates endocr<strong>in</strong>e cells <strong>of</strong> <strong>the</strong>pancreas (129).Liehr et al. (130) assessed <strong>the</strong> role <strong>of</strong> CCK <strong>in</strong> BBS-<strong>in</strong>ducedgrowth <strong>in</strong> rats. Sprague-Dawley rats received sc <strong>in</strong>jections <strong>of</strong>BBS every 8 h for 5 d, alone or <strong>in</strong> comb<strong>in</strong>ation with <strong>the</strong> CCKreceptor antagonist, L-364,718. BBS produced a dose-dependent<strong>in</strong>crease <strong>in</strong> pancreatic weight, DNA <strong>and</strong> prote<strong>in</strong> content,as well as amylase <strong>and</strong> chymotryps<strong>in</strong>ogen levels. L-364,718significantly <strong>in</strong>hibited pancreatic growth <strong>in</strong>duced by a highconcentration (5 nmol/kg) <strong>of</strong> BBS but had m<strong>in</strong>imal effects ongrowth <strong>in</strong>duced by lower dosages <strong>of</strong> BBS. These results suggestthat low doses <strong>of</strong> BBS stimulate pancreatic growth <strong>in</strong> adirect manner, <strong>in</strong>dependent <strong>of</strong> CCK, whereas high doses <strong>of</strong>BBS act <strong>in</strong> part through CCK release.More recently, Fiorucci et al. (131) found that chronic BBSadm<strong>in</strong>istration stimulated pancreatic regeneration after pancreatectomy<strong>in</strong> pigs. Fur<strong>the</strong>rmore, <strong>the</strong>se studies exam<strong>in</strong>ed<strong>the</strong> cellular processes that may be regulated by BBS. Threegroups <strong>of</strong> pigs underwent sham operation, subtotal distalpancreatectomy, or subtotal pancreatectomy comb<strong>in</strong>ed withBBS for 4 wk. After treatment, <strong>the</strong> pancreas was removed,weighed, <strong>and</strong> assayed for p42 <strong>and</strong> p44 MAPK, p46 Shc ,p52 Shc , p66 Shc , <strong>and</strong> Grb2. BBS adm<strong>in</strong>istration resulted <strong>in</strong> a100% <strong>in</strong>crease <strong>in</strong> residual pancreatic tissue when comparedwith control animals <strong>and</strong> approximately a 3-fold <strong>in</strong>crease <strong>in</strong><strong>the</strong> rate <strong>of</strong> pancreatic ac<strong>in</strong>ar cell proliferation. Also, BBSadm<strong>in</strong>istration significantly <strong>in</strong>creased p46 Shc /p52 Shc <strong>and</strong>MAPK expression <strong>and</strong>/or activity <strong>in</strong> whole pancreas extracts.These results fur<strong>the</strong>r demonstrate a proliferative effect<strong>of</strong> BBS <strong>in</strong> a large animal model <strong>and</strong> provide evidence that BBScan stimulate cell proliferation via <strong>the</strong> MAPK pathway.Upp et al. (128) demonstrated that BBS had both direct <strong>and</strong><strong>in</strong>direct actions <strong>in</strong> <strong>the</strong> pancreas. Polyam<strong>in</strong>e syn<strong>the</strong>sis, anessential part <strong>of</strong> DNA syn<strong>the</strong>sis, was assessed with BBS adm<strong>in</strong>istrationover a time course. BBS produced significantpancreatic hyperplasia (<strong>in</strong>creased pancreatic weight, prote<strong>in</strong>,<strong>and</strong> DNA content) after 14 d <strong>of</strong> treatment. CR1409, <strong>the</strong> CCKreceptor antagonist, <strong>in</strong>hibited only BBS-mediated <strong>in</strong>creases<strong>in</strong> DNA content. BBS stimulated polyam<strong>in</strong>e biosyn<strong>the</strong>sis asearly as 2 h after adm<strong>in</strong>istration; CR1409 did not <strong>in</strong>hibit this<strong>in</strong>crease <strong>in</strong> polyam<strong>in</strong>es. These results suggested that <strong>the</strong> trophicactions <strong>of</strong> BBS are both direct <strong>and</strong> <strong>in</strong>direct <strong>and</strong> that <strong>the</strong>direct effects are mediated by polyam<strong>in</strong>e syn<strong>the</strong>sis.D. NTThe physiological functions <strong>of</strong> NT <strong>in</strong> <strong>the</strong> GI tract <strong>in</strong>cludestimulation <strong>of</strong> pancreatic <strong>and</strong> biliary secretions (37) <strong>and</strong> <strong>in</strong>hibition<strong>of</strong> small bowel <strong>and</strong> gastric motility (38). In addition,NT stimulates growth <strong>of</strong> <strong>the</strong> gastric antrum, small bowel (33,34, 42), colon (132), <strong>and</strong> pancreas (40, 133).1. Stomach. Feurle et al. (40) demonstrated that sc adm<strong>in</strong>istration<strong>of</strong> high dosages <strong>of</strong> NT for 2 wk <strong>in</strong>creased prote<strong>in</strong>concentration <strong>and</strong> thickness <strong>of</strong> <strong>the</strong> gastric antrum <strong>in</strong> Wistarrats, whereas DNA content <strong>and</strong> weight were not affected. Incontrast, Hoang et al. (134) noted that NT alone had no effecton <strong>the</strong> oxyntic gl<strong>and</strong> area or <strong>the</strong> antrum, but it <strong>in</strong>hibited<strong>in</strong>creases <strong>in</strong> antral weight, DNA, <strong>and</strong> prote<strong>in</strong> <strong>in</strong>duced bysecret<strong>in</strong>. The effects <strong>of</strong> NT on antral growth are, <strong>the</strong>refore,m<strong>in</strong>imal at best <strong>and</strong> may occur with prolonged, high dosages<strong>of</strong> NT.2. Small bowel. In contrast to <strong>the</strong> stomach, <strong>the</strong> trophic effects<strong>of</strong> NT <strong>in</strong> <strong>the</strong> small bowel are more pronounced. Wood et al.(42) first noted that NT stimulated <strong>the</strong> small bowel mucosa<strong>of</strong> rats fed a normal chow diet. We have shown that adm<strong>in</strong>istration<strong>of</strong> NT prevents gut mucosal atrophy <strong>in</strong>duced byfeed<strong>in</strong>g rats an ED (Fig. 4) (Ref. 34) <strong>and</strong> stimulates mucosalgrowth <strong>in</strong> defunctionalized self-empty<strong>in</strong>g jejunoileal loopsor isolated TVFs, thus support<strong>in</strong>g a direct role for NT <strong>in</strong> <strong>the</strong>stimulation <strong>of</strong> gut mucosal growth. These f<strong>in</strong>d<strong>in</strong>gs demonstratethat NT is an important trophic hormone that canma<strong>in</strong>ta<strong>in</strong> <strong>and</strong> even augment gut mucosal structure by an<strong>in</strong>crease <strong>in</strong> overall mucosal cellularity. Consistent with ourf<strong>in</strong>d<strong>in</strong>gs, Vagianos et al. (135) reported that NT restores gutFIG. 4. NT prevents small bowel mucosal atrophy associatedwith ED. Histology <strong>of</strong> Sprague-Dawley ratsmall bowel after ED, ED <strong>and</strong> NT (<strong>in</strong>jected sc 300 g/kgthree times a day), <strong>and</strong> chow (control) for 5 d.Downloaded from edrv.endojournals.org by on July 16, 2007
580 Endocr<strong>in</strong>e Reviews, October 2003, 24(5):571–599 Thomas et al. • <strong>Gastro<strong>in</strong>test<strong>in</strong>al</strong> <strong>Hormones</strong> <strong>and</strong> <strong>Proliferation</strong>mucosal <strong>in</strong>tegrity <strong>in</strong> rats <strong>and</strong> prevents <strong>the</strong> translocation <strong>of</strong><strong>in</strong>digenous bacteria after radiation-<strong>in</strong>duced mucosal <strong>in</strong>jury.We have extended <strong>the</strong> observation that NT <strong>in</strong>creases proliferation<strong>of</strong> small bowel mucosa by evaluat<strong>in</strong>g <strong>the</strong> effects <strong>of</strong> NT<strong>in</strong> rats <strong>of</strong> different age groups <strong>and</strong> found that <strong>in</strong>creases <strong>of</strong>growth measurements (DNA, RNA, <strong>and</strong> prote<strong>in</strong>) were <strong>the</strong>greatest <strong>in</strong> <strong>the</strong> small bowel mucosa <strong>of</strong> aged rats. These f<strong>in</strong>d<strong>in</strong>gsdemonstrate that, with ag<strong>in</strong>g, <strong>the</strong> ability <strong>of</strong> <strong>the</strong> smallbowel mucosa to respond to <strong>the</strong> trophic stimulus <strong>of</strong> NT isreta<strong>in</strong>ed <strong>and</strong> may, <strong>in</strong> fact, be greater when compared with <strong>the</strong>proliferative response <strong>in</strong> young rats given NT.Izukura et al. (136) demonstrated that adm<strong>in</strong>istration <strong>of</strong> NTaugments <strong>the</strong> normal adaptive hyperplasia <strong>of</strong> gut mucosathat is associated with massive (i.e., 70%) small bowel resection.Consistent with our results, de Miguel et al. (137) usedan 80% bowel resection model <strong>and</strong> demonstrated that exogenousNT significantly <strong>in</strong>creased villus length <strong>in</strong> both <strong>the</strong>jejunum <strong>and</strong> ileum compared with <strong>the</strong> resected group notreceiv<strong>in</strong>g NT, suggest<strong>in</strong>g that adm<strong>in</strong>istration <strong>of</strong> exogenousNT potentiated <strong>the</strong> growth <strong>of</strong> <strong>the</strong> <strong>in</strong>test<strong>in</strong>al villi <strong>and</strong> accelerated<strong>the</strong> trophic response after massive small bowel resection.These <strong>in</strong>vestigators also noted <strong>in</strong>creased circulat<strong>in</strong>glevels <strong>of</strong> enteroglucagon after NT adm<strong>in</strong>istration <strong>and</strong> postulatedthat this may have contributed to <strong>the</strong> proliferativeeffect noted with NT. Ryan et al. (138) demonstrated <strong>in</strong> arabbit model <strong>of</strong> midgut bowel resection that ei<strong>the</strong>r epidermalgrowth factor (EGF) or NT resulted <strong>in</strong> significantly <strong>in</strong>creasedmicrovillus height <strong>and</strong> brush-border surface areas after adm<strong>in</strong>istration.After bowel resection, both EGF <strong>and</strong> NT <strong>in</strong>ducedenterocyte microvillus hypertrophy <strong>and</strong> <strong>in</strong>creased absorptivesurface area <strong>in</strong> <strong>the</strong> remnant bowel. It was suggestedthat <strong>the</strong>se peptides might be useful <strong>in</strong> accelerat<strong>in</strong>g smallbowel adaptation <strong>and</strong> prevent<strong>in</strong>g <strong>the</strong> development <strong>of</strong> shortbowel syndrome. The effects <strong>of</strong> NT on <strong>in</strong>test<strong>in</strong>al adaptationhave also been studied <strong>in</strong> a colectomy model (139). After acolon resection, jejunal proliferation <strong>in</strong>creased significantly<strong>in</strong> rats treated with NT, with less pronounced effects noted<strong>in</strong> <strong>the</strong> rema<strong>in</strong><strong>in</strong>g colon <strong>and</strong> ileum. This study provides additionalsupport that NT augments <strong>the</strong> adaptive response <strong>of</strong>ei<strong>the</strong>r <strong>the</strong> small bowel or colon after bowel resection.3. Colon. We have shown that NT (300 g/kg three timesdaily) stimulates proliferation <strong>of</strong> colonic mucosa <strong>in</strong> young<strong>and</strong> aged rats <strong>in</strong> a differential fashion (41). Colonic proliferation<strong>in</strong> young (2-month-old) rats was characterized by<strong>in</strong>creases <strong>in</strong> cell number, whereas <strong>in</strong> aged (2-yr-old) rats,<strong>in</strong>dices <strong>of</strong> hypertrophy were elevated significantly without aconcomitant <strong>in</strong>crease <strong>in</strong> cell number. This study shows thatNT is not only important for small bowel growth <strong>and</strong> mucosal<strong>in</strong>tegrity, but also functions as an important hormoneregulat<strong>in</strong>g colonic mucosal proliferation. Fur<strong>the</strong>rmore,Hoang et al. (134) demonstrated that NT (100 g/kg) significantly<strong>in</strong>creased prote<strong>in</strong> content <strong>in</strong> <strong>the</strong> colon but did notaffect weight or DNA content <strong>in</strong> F344 rats. The decreasedeffect noted <strong>in</strong> <strong>the</strong>ir study relates to <strong>the</strong> decreased dosage <strong>of</strong>NT compared with our previous study. It is clear that, althoughnot as pronounced as <strong>the</strong> small bowel, NT can stimulateproliferation <strong>of</strong> colonic mucosa.4. Pancreas. Feurle et al. (40) demonstrated that adm<strong>in</strong>istration<strong>of</strong> NT <strong>in</strong>creased pancreatic weight, DNA, RNA, <strong>and</strong>prote<strong>in</strong> contents as well as lipase <strong>and</strong> amylase concentrations.A proliferative effect for NT on <strong>the</strong> pancreas was likewisedemonstrated by Wood et al. (133) by chronic adm<strong>in</strong>istration<strong>of</strong> NT, which produced small but statisticallysignificant trophic effects <strong>in</strong> <strong>the</strong> pancreas, with <strong>the</strong> highestdose <strong>of</strong> NT (300 g/kg) <strong>in</strong>creas<strong>in</strong>g pancreatic weight by 16%,DNA content by 12%, <strong>and</strong> prote<strong>in</strong> content by 17%. When NTwas given <strong>in</strong> comb<strong>in</strong>ation with ei<strong>the</strong>r cerule<strong>in</strong> or secret<strong>in</strong>, ithad m<strong>in</strong>imal additive effects on <strong>the</strong> responses <strong>of</strong> <strong>the</strong>se twopeptides (134). Therefore, from <strong>the</strong>se studies it can be concludedthat NT stimulates pancreatic growth but not to <strong>the</strong>same extent as CCK or BBS/GRP.E. PYYPYY <strong>in</strong>hibits blood flow to <strong>the</strong> GI tract (140, 141), <strong>in</strong>hibitssmall bowel fluid <strong>and</strong> electrolyte secretion (142–144), <strong>and</strong>regulates GI motility. In addition, adm<strong>in</strong>istration <strong>of</strong> PYY canstimulate proliferation <strong>of</strong> small bowel <strong>and</strong> colonic mucosa.The effects <strong>of</strong> PYY on <strong>the</strong> stomach <strong>and</strong> pancreas are notknown.1. Small bowel <strong>and</strong> colon. Gomez et al. (51) first demonstrateda trophic effect for PYY (150–200 nmol/kg, three times daily)on <strong>the</strong> small bowel <strong>and</strong> colonic mucosa <strong>of</strong> both rat <strong>and</strong>mouse. Consistent with <strong>the</strong>se f<strong>in</strong>d<strong>in</strong>gs, Chance et al. (145)found that PYY treatment (1 nmol/kgh) <strong>in</strong> Sprague-Dawleyrats given TPN produced significant <strong>in</strong>creases <strong>in</strong> jejunal,ileal, <strong>and</strong> colonic prote<strong>in</strong> contents.The trophic effects noted for PYY were <strong>in</strong> contrast to workby Guan et al. (146) demonstrat<strong>in</strong>g that PYY, adm<strong>in</strong>istered at400 pmol/kgh (cont<strong>in</strong>uous <strong>in</strong>fusion) for 4 d, failed to affectduodenal weight, prote<strong>in</strong>, or DNA/RNA contents <strong>in</strong> maleWistar rats. In addition, us<strong>in</strong>g ei<strong>the</strong>r a small bowel resectionmodel (147) or a gut atrophy model <strong>in</strong>duced by TPN (148),adm<strong>in</strong>istration <strong>of</strong> PYY failed to elicit a trophic effect on smallbowel mucosa. These negative results were attributable to<strong>the</strong> smaller doses <strong>and</strong> different experimental designs.F. GLP-2A trophic effect for proglucagon-derived peptides(PGDPs) on <strong>the</strong> <strong>in</strong>test<strong>in</strong>al mucosa has been postulated s<strong>in</strong>ce<strong>the</strong> description <strong>of</strong> a glucagon-secret<strong>in</strong>g tumor <strong>of</strong> <strong>the</strong> kidneyassociated with small bowel mucosal hypertrophy. Druckeret al. (149) were <strong>the</strong> first to demonstrate that <strong>the</strong> <strong>in</strong>test<strong>in</strong>otrophicfactor was GLP-2.1. Small <strong>in</strong>test<strong>in</strong>e. To assess <strong>the</strong> potential consequences <strong>of</strong><strong>in</strong>creased proglucagon gene expression on <strong>in</strong>test<strong>in</strong>al growth,Brubaker et al. (150) created glucagon-SV40 T-antigen transgenicmice that developed proglucagon-produc<strong>in</strong>g tumors<strong>and</strong> elevated levels <strong>of</strong> <strong>the</strong> PGDPs. Small bowel mucosal hypertrophywas noted <strong>in</strong> <strong>the</strong> transgenic mice; however, it wasnot possible to ascerta<strong>in</strong> which <strong>of</strong> <strong>the</strong> PGDPs was responsiblefor small bowel growth. To better ascerta<strong>in</strong> which <strong>of</strong> <strong>the</strong>PGDPs stimulated gut growth, nude mice with three differentsc proglucagon-produc<strong>in</strong>g tumor xenografts (InR1-G9,RIN1056A, <strong>and</strong> STC-1 cells) were analyzed (149). Fur<strong>the</strong>rmore,CD1 mice were treated with GLP-1, GLP-2, glicent<strong>in</strong>,<strong>and</strong> <strong>in</strong>terven<strong>in</strong>g peptide (IP)-1 (all are produced from <strong>the</strong>Downloaded from edrv.endojournals.org by on July 16, 2007
Thomas et al. • <strong>Gastro<strong>in</strong>test<strong>in</strong>al</strong> <strong>Hormones</strong> <strong>and</strong> <strong>Proliferation</strong> Endocr<strong>in</strong>e Reviews, October 2003, 24(5):571–599 581proglucagon gene). Mice with all three xenograft types demonstratedan <strong>in</strong>crease <strong>in</strong> small bowel weight, crypt-villusheight, <strong>and</strong> percentage <strong>of</strong> BrdU-positive cells; glicent<strong>in</strong> (43.75g) adm<strong>in</strong>istered twice daily for 10 d produced modest <strong>in</strong>creases<strong>in</strong> total small bowel weight. Nei<strong>the</strong>r GLP-1 nor IP-1had an effect on <strong>the</strong> gut mucosa, whereas GLP-2 produceda 50% <strong>in</strong>crease <strong>in</strong> small bowel weight. Fur<strong>the</strong>rmore, onlyGLP-2 produced a significant <strong>in</strong>crease <strong>in</strong> mucosal thickness,with <strong>the</strong> <strong>in</strong>crease attributable to <strong>in</strong>creased villus height (149).Similarly, Ghatei et al. (151) demonstrated prom<strong>in</strong>ent trophiceffects <strong>of</strong> GLP-2 <strong>in</strong> Wistar rats. Us<strong>in</strong>g vary<strong>in</strong>g doses <strong>of</strong> enteroglucagon,GLP-1, oxyntomodul<strong>in</strong>, <strong>and</strong> GLP-2, onlyGLP-2 produced a dose-dependent <strong>in</strong>crease <strong>in</strong> <strong>the</strong> weight <strong>of</strong>stomach, small <strong>in</strong>test<strong>in</strong>e, <strong>and</strong> colon <strong>of</strong> parenterally fed rats.Therefore, <strong>the</strong>se studies confirmed that, <strong>of</strong> <strong>the</strong> PGDPs, GLP-2was <strong>the</strong> major mediator <strong>of</strong> <strong>in</strong>test<strong>in</strong>al epi<strong>the</strong>lial proliferation.Litvak et al. (152, 153) demonstrated that GLP-2 (1.75g/kg twice a day) significantly <strong>in</strong>creased <strong>the</strong> weight <strong>of</strong>jejunum, ileum, <strong>and</strong> colon <strong>of</strong> athymic nude mice comparedwith both control mice <strong>and</strong> mice treated with NT (600 g/kgthree times a day). These studies confirmed <strong>the</strong> previousf<strong>in</strong>d<strong>in</strong>gs <strong>of</strong> a trophic effect for GLP-2 <strong>and</strong> demonstrated that<strong>the</strong> proliferative effects were equal to or greater than those<strong>of</strong> NT. In ano<strong>the</strong>r study, GLP-2-produc<strong>in</strong>g tumor cells (STC-1cells) were implanted <strong>in</strong> athymic mice <strong>and</strong> <strong>the</strong>n r<strong>and</strong>omizedto receive ei<strong>the</strong>r NT or sal<strong>in</strong>e (152, 153). The mice treated withNT <strong>and</strong> GLP-2 (from STC-1) displayed significant <strong>in</strong>creases<strong>in</strong> jejunal <strong>and</strong> ileal weight <strong>and</strong> prote<strong>in</strong> content over ei<strong>the</strong>r NTor GLP-2 alone. The adm<strong>in</strong>istration <strong>of</strong> NT appeared to enhance<strong>the</strong> enterotrophic effects <strong>of</strong> GLP-2, suggest<strong>in</strong>g that <strong>the</strong>comb<strong>in</strong>ation may be useful to enhance <strong>in</strong>test<strong>in</strong>al growth <strong>in</strong>patients with short bowel syndrome.In addition to <strong>the</strong> effects <strong>of</strong> GLP-2 on normal mucosa, <strong>the</strong>effects <strong>of</strong> this agent dur<strong>in</strong>g periods <strong>of</strong> gut <strong>in</strong>jury or atrophyhave also been assessed. Mice treated with <strong>the</strong> nonsteroidalagent <strong>in</strong>domethac<strong>in</strong> develop small bowel enteritis associatedwith significant mortality at 48–72 h after adm<strong>in</strong>istration;treatment with human [Gly 2 ]GLP-2 before, dur<strong>in</strong>g, or after<strong>in</strong>domethac<strong>in</strong> adm<strong>in</strong>istration resulted <strong>in</strong> reduced mortality<strong>and</strong> decreased mucosal <strong>in</strong>jury (154). The protective effectswere attributed to significantly <strong>in</strong>creased crypt cell proliferation<strong>and</strong> decreased crypt compartment apoptosis. Theeffect <strong>of</strong> GLP-2 on chemo<strong>the</strong>rapy-<strong>in</strong>duced <strong>in</strong>test<strong>in</strong>al mucositishas also been assessed. Pretreatment <strong>of</strong> mice with human[Gly 2 ]GLP-2 before adm<strong>in</strong>istration <strong>of</strong> <strong>the</strong> topoisomerase <strong>in</strong>hibitorir<strong>in</strong>otecan resulted <strong>in</strong> reduced bacterial <strong>in</strong>fection, <strong>in</strong>test<strong>in</strong>aldamage, <strong>and</strong> mortality (155). Histological <strong>and</strong> biochemicalanalyses revealed significant reductions <strong>in</strong> cryptcompartment apoptosis <strong>and</strong> reduced caspase-8 activation.Consistent with <strong>the</strong>se reports, Tavakkolizadeh et al. (156)noted decreased <strong>in</strong>test<strong>in</strong>al damage <strong>in</strong> rats given GLP-2 <strong>in</strong>comb<strong>in</strong>ation with <strong>the</strong> chemo<strong>the</strong>rapeutic agent 5-fluorouracil.F<strong>in</strong>ally, repeated cyclical adm<strong>in</strong>istration <strong>of</strong> both human[Gly 2 ]GLP-2 <strong>and</strong> ir<strong>in</strong>otecan resulted <strong>in</strong> decreased mortality<strong>in</strong> groups <strong>of</strong> BALB/C mice implanted with sc CT-26 coloncarc<strong>in</strong>omas. These data suggest that GLP-2 may have <strong>the</strong>rapeuticadvantages for cancer patients by support<strong>in</strong>g bowel<strong>in</strong>tegrity without dim<strong>in</strong>ish<strong>in</strong>g <strong>the</strong> effectiveness <strong>of</strong> <strong>the</strong>chemo<strong>the</strong>rapy.2. Colon. Although <strong>the</strong> small bowel is significantly moresensitive to <strong>the</strong> effects <strong>of</strong> GLP-2, studies have shown thatGLP-2 <strong>and</strong> GLP-2 analogs can stimulate <strong>the</strong> growth <strong>of</strong> colonicmucosa. As previously noted, Litvak et al. (152) demonstrateda trophic effect <strong>of</strong> GLP-2 on <strong>the</strong> colonic mucosa <strong>of</strong>athymic nude mice. Drucker et al. (157) demonstrated an<strong>in</strong>crease <strong>in</strong> colonic growth us<strong>in</strong>g dipeptidyl peptidase IVresistantGLP-2 analog, human [Gly 2 ]GLP-2 <strong>in</strong> CD1 mice.Fur<strong>the</strong>rmore, <strong>the</strong> comb<strong>in</strong>ation <strong>of</strong> this agent with IGF-I, GH,or long [Arg3]IGF-I produced a greater <strong>in</strong>crease <strong>in</strong> largebowel mass than mice treated with [Gly 2 ]GLP-2 alone.Treatment with GLP-2 has also been shown to reducecolonic mucosal <strong>in</strong>jury, similar to <strong>the</strong> f<strong>in</strong>d<strong>in</strong>gs <strong>in</strong> <strong>the</strong> smallbowel (51). In a dextran sulfate-<strong>in</strong>duced colitis model, concomitantadm<strong>in</strong>istration <strong>of</strong> sc human [Gly 2 ]GLP-2 <strong>and</strong> oraldextran sulfate for 10 d resulted <strong>in</strong> markedly reduced colonicdamage <strong>and</strong> decreased weight loss <strong>in</strong> CD1 <strong>and</strong> BALB/Cmice. Treatment with [Gly 2 ]GLP-2 preserved colonic length,decreased <strong>in</strong>test<strong>in</strong>al histological damage, reduced IL-1 expression,<strong>and</strong> <strong>in</strong>creased crypt cell proliferation.G. Somatostat<strong>in</strong>Somatostat<strong>in</strong> has predom<strong>in</strong>antly <strong>in</strong>hibitory effects, whichhave been used to advantage <strong>in</strong> certa<strong>in</strong> cl<strong>in</strong>ical scenarios.Somatostat<strong>in</strong> <strong>in</strong>hibits pancreatic <strong>and</strong> GI secretion <strong>and</strong> GImotility <strong>and</strong> <strong>in</strong>hibits <strong>the</strong> release <strong>of</strong> GH <strong>and</strong> all known GIhormones (3). The active peptide analog <strong>of</strong> somatostat<strong>in</strong>(octreotide) has been effectively used as an agent to amelioratesymptoms associated with endocr<strong>in</strong>e-overproduc<strong>in</strong>gtumors, pancreatic fistulas, <strong>and</strong> enterocutaneous fistulas(158, 159). In experimental studies, somatostat<strong>in</strong> has alsobeen shown to <strong>in</strong>hibit <strong>the</strong> growth <strong>of</strong> <strong>the</strong> GI mucosa <strong>and</strong>normal pancreas (158, 159). These effects may be throughei<strong>the</strong>r an <strong>in</strong>direct mechanism such as <strong>in</strong>hibition <strong>of</strong> o<strong>the</strong>rtrophic hormones or a direct effect through <strong>in</strong>teraction with<strong>the</strong> somatostat<strong>in</strong> receptor subtype 2 (160, 161). This somatostat<strong>in</strong>receptor subtype associates <strong>and</strong> stimulates tyros<strong>in</strong>ephosphatase src homology 2-conta<strong>in</strong><strong>in</strong>g tryos<strong>in</strong>e phosphatase1 activity, which <strong>in</strong> turn arrests cells <strong>in</strong> <strong>the</strong> G o /G 1 phase<strong>of</strong> <strong>the</strong> cell cycle associated with up-regulation <strong>of</strong> <strong>the</strong>cycl<strong>in</strong>-dependent k<strong>in</strong>ase <strong>in</strong>hibitor p27 kip1 <strong>and</strong> an <strong>in</strong>crease <strong>in</strong>hypophosphorylated ret<strong>in</strong>oblastoma prote<strong>in</strong> levels (160,161). Although <strong>the</strong> major portion <strong>of</strong> this review has focusedon <strong>the</strong> stimulatory effects <strong>of</strong> various GI hormones, it is importantto discuss <strong>the</strong> <strong>in</strong>hibition <strong>of</strong> growth us<strong>in</strong>g somatostat<strong>in</strong><strong>and</strong> its analogs.1. Stomach. The effects <strong>of</strong> somatostat<strong>in</strong> on gastric mucosalgrowth have been assessed. Treatment <strong>of</strong> Wistar rats withsomatostat<strong>in</strong> (50 g/kgh) reduced nuclear uptake <strong>of</strong>[ 3 H]thymid<strong>in</strong>e <strong>and</strong> cell division <strong>in</strong> both fundic <strong>and</strong> antralprogenitor cells (162). Fur<strong>the</strong>rmore, <strong>the</strong> comb<strong>in</strong>ation <strong>of</strong> somatostat<strong>in</strong><strong>and</strong> gastr<strong>in</strong> reduced gastr<strong>in</strong>-stimulated DNA syn<strong>the</strong>sis<strong>in</strong> <strong>the</strong> gastric mucosa. In contrast, <strong>in</strong> <strong>the</strong> duodenum<strong>and</strong> jejunum, <strong>the</strong> effects <strong>of</strong> somatostat<strong>in</strong> were less consistent,with nocturnal somatostat<strong>in</strong> produc<strong>in</strong>g slight decreases <strong>in</strong>DNA syn<strong>the</strong>sis. These f<strong>in</strong>d<strong>in</strong>gs suggested that somatostat<strong>in</strong>could <strong>in</strong>hibit cell proliferation <strong>in</strong> <strong>the</strong> mucosa <strong>of</strong> <strong>the</strong> normalGI tract <strong>and</strong>, fur<strong>the</strong>rmore, could antagonize <strong>the</strong> trophic ac-Downloaded from edrv.endojournals.org by on July 16, 2007
582 Endocr<strong>in</strong>e Reviews, October 2003, 24(5):571–599 Thomas et al. • <strong>Gastro<strong>in</strong>test<strong>in</strong>al</strong> <strong>Hormones</strong> <strong>and</strong> <strong>Proliferation</strong>tivity <strong>of</strong> gastr<strong>in</strong>, particularly <strong>in</strong> <strong>the</strong> fundus <strong>and</strong> antrum <strong>of</strong> <strong>the</strong>stomach. Similar results were noted by Rivard et al. (61),demonstrat<strong>in</strong>g <strong>in</strong>hibitory effects on rat mucosal growth <strong>of</strong><strong>the</strong> duodenum us<strong>in</strong>g <strong>the</strong> somatostat<strong>in</strong> analog, S<strong>and</strong>ostat<strong>in</strong>.The adm<strong>in</strong>istration <strong>of</strong> S<strong>and</strong>ostat<strong>in</strong> <strong>in</strong> this model was associatedwith a decrease <strong>in</strong> plasma CCK <strong>and</strong> IGF-I levels (61),suggest<strong>in</strong>g an <strong>in</strong>duced effect <strong>of</strong> somatostat<strong>in</strong>.2. Small <strong>in</strong>test<strong>in</strong>e. There is also evidence to support an <strong>in</strong>hibitoryeffect <strong>of</strong> somatostat<strong>in</strong> <strong>in</strong> <strong>the</strong> jejunum <strong>and</strong> ileum. Bass etal. (62) demonstrated that <strong>the</strong> normal adaptive hyperplasianoted <strong>in</strong> rats after 40% small bowel resection could be attenuatedby adm<strong>in</strong>istration <strong>of</strong> octreotide, as noted by assessment<strong>of</strong> villus height <strong>and</strong> residual bowel weight. Us<strong>in</strong>g arabbit model <strong>of</strong> an ileal mucosal defect, Thompson et al. (163)demonstrated that octreotide <strong>in</strong>hibited normal but not EGFstimulatedcell migration. In addition, octreotide decreasedEGF-stimulated proliferation. In contrast, V<strong>and</strong>erho<strong>of</strong> <strong>and</strong>Kollman (164) failed to show significant differences <strong>in</strong> mucosalweight, prote<strong>in</strong>, <strong>and</strong> sucrase levels <strong>in</strong> rats treated withoctreotide after an 80% small bowel resection. The differencesnoted <strong>in</strong> this study, compared with that <strong>of</strong> Bass et al.(62), may simply represent <strong>the</strong> fact that a more extensiveresection model was used, which may have provided anenhanced stimulation <strong>of</strong> mucosal regeneration that could notbe <strong>in</strong>hibited by adm<strong>in</strong>istration <strong>of</strong> somatostat<strong>in</strong>.The question rema<strong>in</strong>s, however, as to <strong>the</strong> role endogenoussomatostat<strong>in</strong> plays <strong>in</strong> <strong>the</strong> <strong>in</strong>hibition <strong>of</strong> normal <strong>in</strong>test<strong>in</strong>algrowth <strong>and</strong> proliferation. Parekh et al. (63) demonstrated thatsomatostat<strong>in</strong> appears to function as an endogenous <strong>in</strong>hibitoryfactor. Male F344 rats were given cysteam<strong>in</strong>e (CYS; anagent known to deplete endogenous somatostat<strong>in</strong>). The adm<strong>in</strong>istration<strong>of</strong> CYS stimulated growth <strong>of</strong> <strong>the</strong> proximal <strong>and</strong>distal small <strong>in</strong>test<strong>in</strong>e as assessed by <strong>in</strong>creases <strong>in</strong> weight,DNA, <strong>and</strong> RNA content; this effect was assumed to be secondaryto a depletion <strong>of</strong> endogenous somatostat<strong>in</strong>, althougho<strong>the</strong>r <strong>in</strong>direct effects cannot be entirely ruled out.3. Pancreas. The effects <strong>of</strong> somatostat<strong>in</strong> on <strong>the</strong> normal pancreashave been extensively analyzed. The f<strong>in</strong>d<strong>in</strong>g <strong>of</strong> Dcells <strong>in</strong> <strong>the</strong> normal pancreas suggested a role for this peptide<strong>in</strong> not only physiological functions <strong>of</strong> <strong>the</strong> pancreas,but also growth <strong>of</strong> <strong>the</strong> normal pancreas. Rivard et al. (61)demonstrated that S<strong>and</strong>ostat<strong>in</strong> significantly decreasedpancreatic weight, DNA, RNA, <strong>and</strong> prote<strong>in</strong> content. Fur<strong>the</strong>rmore,results <strong>of</strong> Parekh et al. (63) demonstrated thatsomatostat<strong>in</strong> depletion with CYS stimulated pancreaticweight by 127% <strong>and</strong> DNA content by 141% compared withcontrol animals. In addition, CYS augmented <strong>the</strong> trophiceffect <strong>of</strong> BBS on <strong>the</strong> pancreas, thus suggest<strong>in</strong>g that somatostat<strong>in</strong>may serve to limit normal pancreatic growth.Block<strong>in</strong>g endogenous somatostat<strong>in</strong> may release <strong>the</strong>se <strong>in</strong>hibitoryconstra<strong>in</strong>ts <strong>and</strong> allow for <strong>in</strong>creased proliferation<strong>of</strong> <strong>the</strong> normal pancreas. The specific mechanisms, however,as to how somatostat<strong>in</strong> acts <strong>in</strong> vivo are still unknown.The effects may be direct, act<strong>in</strong>g through <strong>the</strong> somatostat<strong>in</strong>receptor subtype 2 receptor, or <strong>in</strong>direct through <strong>the</strong> <strong>in</strong>hibition<strong>of</strong> o<strong>the</strong>r proliferative agents.IV. <strong>Proliferation</strong> <strong>of</strong> Neoplastic Tissues byGI <strong>Hormones</strong>Endocr<strong>in</strong>e control <strong>of</strong> cancer growth was first demonstratedby <strong>the</strong> Scottish surgeon Beatson (165), who successfullytreated a patient with breast cancer by perform<strong>in</strong>g bilateraloophorectomy. In 1941, Hugg<strong>in</strong>s <strong>and</strong> Hodges (166)described orchiectomy <strong>and</strong> estrogen <strong>the</strong>rapy for patientswith prostate cancer, <strong>and</strong> <strong>the</strong>n, <strong>in</strong> 1952, Hugg<strong>in</strong>s <strong>and</strong> Bergenstal(167) performed bilateral adrenalectomy, whichcaused regression <strong>of</strong> breast <strong>and</strong> prostate cancers <strong>in</strong> certa<strong>in</strong>patients. In 1971, Jensen et al. (168) reported that <strong>the</strong> presence<strong>of</strong> estrogen receptors predicted response to adrenalectomyfor patients with breast cancer. Therefore, <strong>the</strong> response <strong>of</strong>breast <strong>and</strong> prostate cancers to endocr<strong>in</strong>e <strong>the</strong>rapy is wellestablished <strong>and</strong> forms <strong>the</strong> basis <strong>of</strong> many <strong>of</strong> <strong>the</strong> current <strong>the</strong>rapeuticoptions described for <strong>the</strong> treatment <strong>of</strong> <strong>the</strong>se cancers.In a manner analogous to breast <strong>and</strong> prostate cancers, <strong>the</strong>hypo<strong>the</strong>sis was formulated that GI cancers may also possessreceptors <strong>and</strong> likewise be responsive to various GI hormones.In this regard, receptors for various GI hormoneshave been identified <strong>in</strong> gastric, pancreatic, <strong>and</strong> colorectalcancers; <strong>the</strong>se cancers are responsive to <strong>the</strong> effects <strong>of</strong> GIhormone treatment (169).A. Gastric cancerAlthough <strong>the</strong> <strong>in</strong>cidence <strong>of</strong> gastric cancer has been decreas<strong>in</strong>g<strong>in</strong> <strong>the</strong> United States, it is still estimated to be one <strong>of</strong> <strong>the</strong>more common cancers worldwide <strong>and</strong> is endemic <strong>in</strong> certa<strong>in</strong>areas <strong>of</strong> <strong>the</strong> world such as Japan, Eastern Europe, <strong>and</strong> SouthAmerica (170). The <strong>the</strong>rapeutic options are limited, becauseradiation <strong>and</strong> chemo<strong>the</strong>rapy are, for <strong>the</strong> most part, <strong>in</strong>effective<strong>in</strong> <strong>in</strong>creas<strong>in</strong>g survival <strong>in</strong> patients with metastatic disease(170).Certa<strong>in</strong> gastric cancers possess both low- <strong>and</strong> high-aff<strong>in</strong>itygastr<strong>in</strong>/CCK-B receptors (171, 172). The growth <strong>of</strong> <strong>the</strong>secancers is stimulated by pharmacological <strong>and</strong>, <strong>in</strong> certa<strong>in</strong> <strong>in</strong>stances,physiological concentrations <strong>of</strong> gastr<strong>in</strong> or gastr<strong>in</strong>analogs <strong>in</strong> vitro <strong>and</strong> <strong>in</strong> vivo (173–178). Sumiyoshi et al. (174)identified gastr<strong>in</strong> receptors <strong>in</strong> <strong>the</strong> human gastric cancer, SC-6-JCK; treatment <strong>of</strong> this poorly differentiated adenocarc<strong>in</strong>omawith gastr<strong>in</strong> resulted <strong>in</strong> <strong>in</strong>creased tumor weight, size,<strong>and</strong> label<strong>in</strong>g <strong>in</strong>dex <strong>of</strong> [ 3 H]thymid<strong>in</strong>e. Gastr<strong>in</strong> receptor antagonistsblocked <strong>the</strong>se trophic effects, demonstrat<strong>in</strong>g a directeffect through <strong>the</strong> gastr<strong>in</strong>/CCK-B receptor (174, 179).O<strong>the</strong>r <strong>the</strong>rapeutic strategies that decrease gastr<strong>in</strong> receptorpositivegastric cancer growth <strong>in</strong>clude <strong>in</strong>hibition <strong>of</strong> gastr<strong>in</strong>release by agents such as enprostil, a prostagl<strong>and</strong><strong>in</strong> derivativethat lowers serum gastr<strong>in</strong> levels <strong>in</strong> fasted <strong>and</strong> fed humans<strong>and</strong> mice. Adm<strong>in</strong>istration <strong>of</strong> enprostil to mice bear<strong>in</strong>ggastr<strong>in</strong> receptor-positive gastric cancers <strong>in</strong>hibited <strong>the</strong> growth<strong>of</strong> <strong>the</strong>se cancers; however, <strong>the</strong> growth <strong>of</strong> gastr<strong>in</strong> receptornegativecancers was not affected (180). Therefore, <strong>the</strong>se f<strong>in</strong>d<strong>in</strong>gs<strong>in</strong>dicate that certa<strong>in</strong> gastric cancers possess gastr<strong>in</strong> receptors,<strong>and</strong> growth may be modulated by ei<strong>the</strong>r block<strong>in</strong>g<strong>the</strong> receptors or <strong>in</strong>hibit<strong>in</strong>g gastr<strong>in</strong> release.The glyc<strong>in</strong>e-extended G-17 peptide, Gly-G, which is colocalizedwith amidated gastr<strong>in</strong> <strong>in</strong> antral G cells <strong>and</strong> cosecretedwith G-17, was <strong>in</strong>itially thought to be biologicallyDownloaded from edrv.endojournals.org by on July 16, 2007
Thomas et al. • <strong>Gastro<strong>in</strong>test<strong>in</strong>al</strong> <strong>Hormones</strong> <strong>and</strong> <strong>Proliferation</strong> Endocr<strong>in</strong>e Reviews, October 2003, 24(5):571–599 583<strong>in</strong>active. However, Iwase et al. (181) have shown that Gly-Gstimulated <strong>the</strong> growth <strong>of</strong> <strong>the</strong> human gastric cancers, AGS <strong>and</strong>SIIA. This <strong>in</strong>creased growth was not blocked by ei<strong>the</strong>r <strong>the</strong>CCK-B or <strong>the</strong> CCK-A receptor antagonists, suggest<strong>in</strong>g <strong>the</strong>presence <strong>of</strong> a novel receptor that is different from <strong>the</strong> classicCCK-A or CCK-B receptor. In contrast, G-17 stimulated <strong>the</strong>growth <strong>of</strong> both AGS <strong>and</strong> SIIA cells. Consistent with <strong>the</strong>sef<strong>in</strong>d<strong>in</strong>gs, Szabo et al. (182) demonstrated stimulation <strong>of</strong> AGScell growth with both G-17 <strong>and</strong> pentagastr<strong>in</strong>. Pentagastr<strong>in</strong>was found to be 10 times less potent as a stimulator <strong>of</strong> AGSproliferation when compared with G-17, suggest<strong>in</strong>g a specific,active CCK-B/gastr<strong>in</strong> receptor <strong>in</strong> <strong>the</strong>se cells.Although <strong>the</strong> effects <strong>of</strong> gastr<strong>in</strong> appear well established <strong>in</strong>tumor models, <strong>the</strong> effects <strong>of</strong> gastr<strong>in</strong> on carc<strong>in</strong>ogen-<strong>in</strong>ducedgastric cancers have produced conflict<strong>in</strong>g results. Tahara <strong>and</strong>Haizuka (183) noted that gastr<strong>in</strong> <strong>in</strong>creases <strong>the</strong> <strong>in</strong>cidence <strong>of</strong>N-methyl-N-nitro-N-nitroguanid<strong>in</strong>e (MNNG)-<strong>in</strong>duced cancers<strong>in</strong> rats, whereas Tasuta et al. (184) found that gastr<strong>in</strong><strong>in</strong>hibits <strong>the</strong> <strong>in</strong>cidence <strong>of</strong> stomach cancers <strong>in</strong>duced by <strong>the</strong>same carc<strong>in</strong>ogen. The tim<strong>in</strong>g <strong>and</strong> adm<strong>in</strong>istration <strong>of</strong> gastr<strong>in</strong>appears critical <strong>in</strong> <strong>the</strong>se two studies <strong>and</strong> may account for <strong>the</strong>conflict<strong>in</strong>g results. For example, it was noted that gastr<strong>in</strong>adm<strong>in</strong>istered dur<strong>in</strong>g exposure to MNNG <strong>in</strong>creased gastriccancer development, but late adm<strong>in</strong>istration did not display<strong>the</strong> same growth-enhanc<strong>in</strong>g effect. Therefore, <strong>the</strong> effects <strong>of</strong>gastr<strong>in</strong> may be more pronounced <strong>in</strong> <strong>the</strong> early stages <strong>of</strong> tumordevelopment ra<strong>the</strong>r than <strong>in</strong> <strong>the</strong> later stages <strong>of</strong> growth <strong>in</strong>which o<strong>the</strong>r peptide factors may play a more prom<strong>in</strong>ent role.Recent f<strong>in</strong>d<strong>in</strong>gs by Hagiwara et al. (185) fur<strong>the</strong>r support a rolefor gastr<strong>in</strong> <strong>in</strong> carc<strong>in</strong>ogen-<strong>in</strong>duced stomach cancers. In thisstudy, carbachol-<strong>in</strong>duced gl<strong>and</strong>ular carc<strong>in</strong>omas <strong>in</strong> F344 ratswere associated with <strong>in</strong>creased endogenous gastr<strong>in</strong> levels.In addition to experimental studies, cl<strong>in</strong>ical studies fur<strong>the</strong>rl<strong>in</strong>k gastr<strong>in</strong> to <strong>the</strong> development <strong>and</strong> growth <strong>of</strong> gastric cancers.Recently, gastr<strong>in</strong> has been l<strong>in</strong>ked to Helicobacter pylori<strong>in</strong>fection, a known risk factor for gastric cancer (186). Moreover,significantly higher plasma <strong>and</strong> lum<strong>in</strong>al gastr<strong>in</strong> levelshave been measured <strong>in</strong> gastric cancer patients comparedwith control patients (186). Watson <strong>and</strong> colleagues (173, 187)evaluated 90 archival samples <strong>of</strong> atrophic gastritis; <strong>in</strong>test<strong>in</strong>almetaplasia; mild, moderate <strong>and</strong> severe gastric epi<strong>the</strong>lial dysplasia;<strong>and</strong> <strong>in</strong>test<strong>in</strong>al-type gastric adenocarc<strong>in</strong>oma. Increasedexpression <strong>of</strong> gastr<strong>in</strong> <strong>and</strong> <strong>the</strong> CCK-B/gastr<strong>in</strong> receptor wasassociated with <strong>the</strong> progression <strong>of</strong> atrophic dysplasia to adenocarc<strong>in</strong>oma(173). Toge<strong>the</strong>r, <strong>the</strong>se cl<strong>in</strong>ical studies providefur<strong>the</strong>r support, albeit circumstantial, for <strong>the</strong> role <strong>of</strong> gastr<strong>in</strong><strong>in</strong> gastric carc<strong>in</strong>ogenesis.In addition to gastr<strong>in</strong>, GRP is thought to contribute togastric cancer growth. Preston et al. (188) identified highaff<strong>in</strong>ityGRP receptors <strong>in</strong> a s<strong>in</strong>gle gastric cancer cell l<strong>in</strong>e, St42,<strong>and</strong> Kim et al. (189) identified expression <strong>of</strong> GRP receptors <strong>in</strong>two <strong>in</strong> vitro gastric cancer cell l<strong>in</strong>es (SIIA <strong>and</strong> MKN-45) <strong>and</strong><strong>in</strong> three <strong>of</strong> five human gastric cancer xenografts. The presence<strong>of</strong> GRP receptors <strong>in</strong> gastric cancer appears to play afunctional role <strong>in</strong> <strong>the</strong> growth <strong>of</strong> <strong>the</strong>se tumors, as noted by Q<strong>in</strong>et al. (190) who demonstrated that <strong>the</strong> GRP receptor antagonist,RC-3095, blocked <strong>the</strong> growth <strong>of</strong> <strong>the</strong> human gastriccancer, Hs746T, both <strong>in</strong> vitro <strong>and</strong> when placed as xenografts<strong>in</strong> nude mice. P<strong>in</strong>ski et al. (191) also found that RC-3095significantly <strong>in</strong>hibited MKN-45 xenograft tumor weight <strong>and</strong>volume. As an assessment <strong>of</strong> signal<strong>in</strong>g pathways regulat<strong>in</strong>g<strong>the</strong> mitogenic effect <strong>of</strong> GRP, Kim et al. (189) from our laboratoryhave shown that treatment <strong>of</strong> <strong>the</strong> gastric cancer celll<strong>in</strong>e, SIIA, with BBS stimulates release <strong>of</strong> <strong>in</strong>tracellular calcium<strong>and</strong> <strong>in</strong>creases <strong>the</strong> expression <strong>of</strong> <strong>the</strong> activator prote<strong>in</strong>(AP)-1-related prote<strong>in</strong>s, c-Jun <strong>and</strong> c-Fos, that have beenshown to play a role <strong>in</strong> cellular proliferation; this effect wasblocked by specific GRP receptor antagonists. Cl<strong>in</strong>ical studies<strong>in</strong>dicate that as many as 50% <strong>of</strong> gastric cancers displayhigh-aff<strong>in</strong>ity b<strong>in</strong>d<strong>in</strong>g for GRP (192). Similarly, Carroll et al.(193) identified expression <strong>of</strong> GRP receptor mRNA <strong>in</strong> eight<strong>of</strong> 20 (40%) nonantral gastric cancers. Of <strong>the</strong>se eight, six <strong>of</strong> <strong>the</strong>GRP receptors were mutated; some <strong>of</strong> <strong>the</strong> mutations resulted<strong>in</strong> nonfunctional GRP receptors. Survival <strong>of</strong> patients whosetumors expressed functional GRP receptors was not statisticallydifferent from those that did not; however, this mayrepresent <strong>the</strong> fact that only a small number <strong>of</strong> patients wereanalyzed. Future studies, assess<strong>in</strong>g a larger patient population,are required before a def<strong>in</strong>itive assessment can be maderegard<strong>in</strong>g <strong>the</strong> association <strong>of</strong> GRP receptors with gastriccancers.F<strong>in</strong>ally, <strong>in</strong> limited studies, <strong>the</strong> hormone NT has beenshown to contribute to carc<strong>in</strong>ogen-<strong>in</strong>duced gastric cancer.Tatsuta et al. (194) found that prolonged alternate-day adm<strong>in</strong>istration<strong>of</strong> NT significantly <strong>in</strong>creased <strong>the</strong> <strong>in</strong>cidence <strong>of</strong>MNNG-<strong>in</strong>duced gastric cancer <strong>in</strong> Wistar rats compared withrats given MNNG alone. The effect <strong>of</strong> NT on human gastriccancers, however, has not been assessed.B. Pancreatic cancerCarc<strong>in</strong>oma <strong>of</strong> <strong>the</strong> pancreas is <strong>the</strong> fifth lead<strong>in</strong>g cause <strong>of</strong>cancer deaths <strong>in</strong> <strong>the</strong> United States (195). The prognosis fromthis disease rema<strong>in</strong>s dismal, with a mean survival time afterdiagnosis <strong>of</strong> about 4–6 months. The effects <strong>of</strong> both stimulatory<strong>and</strong> <strong>in</strong>hibitory hormones on pancreatic cancer growthhave been assessed, <strong>and</strong> <strong>the</strong> signal<strong>in</strong>g mechanisms regulat<strong>in</strong>ghormone-<strong>in</strong>duced pancreatic cancer proliferation are currentlybe<strong>in</strong>g analyzed.Experimental studies have demonstrated a role for CCK<strong>and</strong> gastr<strong>in</strong> <strong>in</strong> pancreatic cancers. CCK receptors have beenidentified <strong>in</strong> hamster <strong>and</strong> human pancreatic cancer cell l<strong>in</strong>es.In vitro studies have demonstrated that CCK <strong>and</strong> its analog,JMV-180, can stimulate <strong>the</strong> growth <strong>of</strong> human pancreatic cancercell l<strong>in</strong>es, <strong>in</strong>clud<strong>in</strong>g MIA PaCa-2 (196–199), PANC-1 (197,199, 200), BxPC-3 (198, 199), Capan-2 (199), RWP-2 (199),SW-1990 (199, 201, 202), <strong>and</strong> MD PANC-3 (203). Similarly, <strong>the</strong>presence <strong>of</strong> CCK receptors can predict <strong>the</strong> responsiveness <strong>of</strong>human pancreatic cancer cells to CCK treatment (180, 204,205). In addition to effects on pancreatic cancer proliferation,Hirata et al. (206) reported that CCK-8 <strong>in</strong>creases <strong>the</strong> production<strong>of</strong> metalloprote<strong>in</strong>ase-9 <strong>in</strong> pancreatic cancer cells via <strong>in</strong>duction<strong>of</strong> prote<strong>in</strong> k<strong>in</strong>ase C, suggest<strong>in</strong>g a role for CCK <strong>in</strong>pancreatic cancer <strong>in</strong>vasiveness <strong>and</strong> possibly metastasis.Cerule<strong>in</strong>, a CCK analog, significantly stimulates <strong>the</strong>growth <strong>of</strong> <strong>the</strong> CCK receptor-positive pancreatic cell l<strong>in</strong>e SKI(207); however, cerule<strong>in</strong> has no effect on <strong>the</strong> CAV pancreaticcancer cell l<strong>in</strong>e, which does not possess CCK receptors.Fur<strong>the</strong>rmore, Asperl<strong>in</strong>, a competitive, nonpeptide CCK receptorantagonist, <strong>in</strong>hibits growth <strong>of</strong> SKI xenografts (208).Downloaded from edrv.endojournals.org by on July 16, 2007
584 Endocr<strong>in</strong>e Reviews, October 2003, 24(5):571–599 Thomas et al. • <strong>Gastro<strong>in</strong>test<strong>in</strong>al</strong> <strong>Hormones</strong> <strong>and</strong> <strong>Proliferation</strong>Townsend et al. (209) demonstrated that growth <strong>of</strong> <strong>the</strong> hamsterpancreatic cancer cell l<strong>in</strong>e, H2T, was stimulated by cerule<strong>in</strong><strong>and</strong> that growth could be fur<strong>the</strong>r enhanced by concomitanttreatment with secret<strong>in</strong>. Both gastr<strong>in</strong> <strong>and</strong> Gly-G canstimulate <strong>the</strong> proliferation <strong>of</strong> AR42J rat pancreatic tumorcells (210, 211); <strong>the</strong>se growth-promot<strong>in</strong>g effects can beblocked by L-365,260, a CCK-B receptor antagonist (210–212). Therefore, <strong>the</strong>se studies provide strong support for amodulatory effect <strong>of</strong> CCK, secret<strong>in</strong>, <strong>and</strong> gastr<strong>in</strong> on certa<strong>in</strong>pancreatic cancers. In contrast, Liehr et al. (213) found thatCCK, at dosages <strong>of</strong> 10 12 to 10 6 m, had no effect on <strong>the</strong>growth <strong>of</strong> ei<strong>the</strong>r MIA PaCa-2 or PANC-1 cells. Moreover,stable transfection <strong>of</strong> MIA PaCa-2 <strong>and</strong> PANC-1 cells withCCK-A or CCK-B receptors resulted <strong>in</strong> growth-<strong>in</strong>hibitoryresponses after activation <strong>of</strong> both receptor subtypes by <strong>the</strong>irlig<strong>and</strong>s. The reason for <strong>the</strong>se discrepant results is not readilyapparent.In vivo studies support a role for CCK <strong>in</strong> <strong>the</strong> stimulation<strong>of</strong> pancreatic cancer growth. Pancreatic tumors <strong>in</strong> rats can be<strong>in</strong>duced by endogenous CCK us<strong>in</strong>g CCK-releas<strong>in</strong>g agents,such as tryps<strong>in</strong> <strong>in</strong>hibitors, by biliary diversion or us<strong>in</strong>g bilesalt-b<strong>in</strong>d<strong>in</strong>g drugs (214–216). For example, feed<strong>in</strong>g rats asoybean diet, a natural tryps<strong>in</strong> <strong>in</strong>hibitor, <strong>in</strong>duced <strong>the</strong> formation<strong>of</strong> preneoplastic lesions <strong>in</strong> <strong>the</strong> pancreas <strong>and</strong>, whentreatment was prolonged for years, pancreatic cancer developed(217–219).Evidence exists that CCK can enhance chemical carc<strong>in</strong>ogen-<strong>in</strong>ducedpancreatic cancers, as well. When comb<strong>in</strong>edwith azaser<strong>in</strong>e (a carc<strong>in</strong>ogenic DNA alkylat<strong>in</strong>g agent), <strong>the</strong>long-term adm<strong>in</strong>istration <strong>of</strong> exogenous CCK or elevation <strong>of</strong>endogenous CCK levels (220–222) enhanced <strong>the</strong> developmentor shortened <strong>the</strong> latency period <strong>of</strong> <strong>the</strong> preneoplasticac<strong>in</strong>ar lesions. These effects could be blocked by CCK-Areceptor antagonists (223–225). Consistent with <strong>the</strong>se results,Satake et al. (107) found that adm<strong>in</strong>istration <strong>of</strong> cerule<strong>in</strong>enhanced <strong>the</strong> carc<strong>in</strong>ogenic effect <strong>of</strong> N-nitrosobis (2-hydroxypropyl) am<strong>in</strong>e <strong>in</strong> hamsters. Fur<strong>the</strong>rmore, Howatson<strong>and</strong> Carter (226) found that both CCK <strong>and</strong> secret<strong>in</strong> enhancedpancreatic carc<strong>in</strong>ogenesis <strong>in</strong>duced by N-nitrosobis (2-oxypropyl) am<strong>in</strong>e (BOP) <strong>in</strong> hamsters. In contrast, Johnsonet al. (227) reported that CCK-8 <strong>in</strong>hibited development <strong>of</strong>nitrosam<strong>in</strong>e-<strong>in</strong>duced pancreatic cancer <strong>in</strong> hamsters. The differencesnoted <strong>in</strong> <strong>the</strong>se studies may relate to differences <strong>in</strong> <strong>the</strong>animal models. With <strong>the</strong> exception <strong>of</strong> this study, <strong>the</strong> majority<strong>of</strong> studies suggest that agents capable <strong>of</strong> <strong>in</strong>creas<strong>in</strong>g endogenousCCK <strong>and</strong> stimulat<strong>in</strong>g <strong>the</strong> growth <strong>of</strong> normal pancreascan also stimulate pancreatic carc<strong>in</strong>ogenesis.Similar to CCK, BBS/GRP, ano<strong>the</strong>r pancreatic trophic factor,has been associated with pancreatic carc<strong>in</strong>ogenesis.Douglas et al. (223) demonstrated that rats treated with azaser<strong>in</strong>e(30 mg/kg) <strong>and</strong> BBS (10 mg/kg) for 16 wk developedpreneoplastic lesions at a higher rate than rats treated withazaser<strong>in</strong>e alone. Similar results were noted by Meijers et al.(228) <strong>and</strong> Lhoste <strong>and</strong> Longhecker (208). This effect was notmediated solely by <strong>in</strong>duction <strong>of</strong> CCK because <strong>the</strong> development<strong>of</strong> preneoplastic lesions was not blocked by <strong>the</strong> CCKreceptor antagonist CR-1409 (223). In contrast, ano<strong>the</strong>r studydemonstrated that adm<strong>in</strong>istration <strong>of</strong> BBS was accompaniedby a decrease <strong>in</strong> <strong>the</strong> number <strong>of</strong> preneoplastic lesions <strong>in</strong> BOPtreatedhamsters. The differential effects <strong>of</strong> BBS <strong>in</strong> <strong>the</strong>sestudies may be attributed to species differences <strong>and</strong> also to<strong>the</strong> differences <strong>in</strong> <strong>the</strong> carc<strong>in</strong>ogenic agents.In ano<strong>the</strong>r study, Szepeshazi et al. (229) demonstratedthat adm<strong>in</strong>istration <strong>of</strong> <strong>the</strong> BBS receptor antagonist, RC-3095, decreased BOP-<strong>in</strong>duced pancreatic cancers <strong>in</strong> hamsters.RC-3095 significantly decreased EGF b<strong>in</strong>d<strong>in</strong>g capacity,suggest<strong>in</strong>g that <strong>in</strong>direct effects might be largelyresponsible for <strong>the</strong> reduction identified <strong>in</strong> BOP-associatedhamster cancer. In a subsequent study (230), <strong>the</strong>se <strong>in</strong>vestigatorsshowed that <strong>the</strong> comb<strong>in</strong>ation <strong>of</strong> GRP or BBS withRC-3095 was not able to overcome <strong>the</strong> effects <strong>of</strong> RC-3095but, conversely, augmented <strong>the</strong> <strong>in</strong>hibitory effects <strong>of</strong> RC-3095. These data are more consistent with <strong>the</strong> observations<strong>of</strong> Meijer <strong>and</strong> Baak (231) <strong>in</strong> hamsters <strong>and</strong> show <strong>the</strong> complexity<strong>of</strong> BBS/GRP regulation <strong>in</strong> pancreatic cancer, whichmay be highly species-dependent.More recently, <strong>the</strong> effects <strong>of</strong> a potent <strong>and</strong> specific GRPreceptor antagonist, BIM 26226 [[d-F5 Phe 6, d-Ala 11] BBS(6–13) OMe], were evaluated <strong>in</strong> pancreatic cancers <strong>in</strong> vivo<strong>and</strong> <strong>in</strong> vitro (232). Chronic BIM 26226 adm<strong>in</strong>istration significantlyreduced tumor volume, prote<strong>in</strong>, RNA, amylase, <strong>and</strong>chymotryps<strong>in</strong> content <strong>in</strong> both GRP-responsive <strong>and</strong> GRPunresponsivepancreatic cancers. These f<strong>in</strong>d<strong>in</strong>gs suggest thatGRP receptor antagonists may work through ei<strong>the</strong>r a director <strong>in</strong>direct effect to <strong>in</strong>hibit tumor growth. Fur<strong>the</strong>rmore, arecent study by Burghardt et al. (233) demonstrated that BBS<strong>in</strong>creases expression <strong>of</strong> three transcription factors (c-fos,c-myc, <strong>and</strong> high-mobility group prote<strong>in</strong> IY) that are associatedwith proliferation <strong>in</strong> <strong>the</strong> human pancreatic cell l<strong>in</strong>eHPAF. These results provide potential novel mechanisms fortarget<strong>in</strong>g <strong>the</strong> trophic effects <strong>of</strong> BBS/GRP <strong>in</strong> pancreaticcancers.Similar to CCK, NT also stimulates pancreatic cancer proliferation.Our laboratory has shown that <strong>the</strong> human pancreaticcancer cell l<strong>in</strong>e MIA PaCa-2 possesses NTRs <strong>and</strong> mobilizes<strong>in</strong>tracellular calcium (234). Iwase et al. (181) haveshown that <strong>the</strong> NTR antagonist SR48692 <strong>in</strong>hibits <strong>in</strong>tracellularcalcium mobilization, IP-3 turnover, <strong>and</strong> MIA PaCa-2 <strong>in</strong> vitrocell growth <strong>in</strong>duced by NT <strong>in</strong> a dose-dependent fashion.Fur<strong>the</strong>rmore, <strong>in</strong> vivo experiments demonstrated that NT significantly<strong>in</strong>creased <strong>the</strong> size, weight, <strong>and</strong> DNA <strong>and</strong> prote<strong>in</strong>contents <strong>of</strong> xenografted MIA PaCa-2 tumors; SR48692blocked this effect. Recent f<strong>in</strong>d<strong>in</strong>gs by Reubi et al. (235) haveshown that approximately 75% <strong>of</strong> pancreatic adenocarc<strong>in</strong>omasexpress NTRs. Consistent with <strong>the</strong>se reports, Ehlers et al.(236) have shown NTR expression <strong>in</strong> approximately 90% <strong>of</strong>resected pancreatic cancers.The signal<strong>in</strong>g mechanisms regulat<strong>in</strong>g NT-mediated proliferation<strong>in</strong> NTR-positive cancers have been assessed. NTstimulates ERK <strong>and</strong> JNK activity <strong>in</strong> MIA PaCa-2 cells <strong>and</strong><strong>in</strong>creases AP-1 b<strong>in</strong>d<strong>in</strong>g activity (237). Consistent with <strong>the</strong>seresults, Ryder et al. (238) reported that NT stimulated Ca 2mobilization <strong>and</strong> activated ERK1 <strong>and</strong> ERK2 <strong>and</strong> DNA syn<strong>the</strong>sis<strong>in</strong> <strong>the</strong> human pancreatic cancer cell l<strong>in</strong>e, PANC-1.Recently, Guha et al. (239) reported that NT <strong>in</strong>duced a rapidactivation <strong>of</strong> <strong>the</strong> PKC is<strong>of</strong>orm, PKD, <strong>in</strong> PANC-1 cells, whichwas l<strong>in</strong>ked to <strong>the</strong> mitogenic effect <strong>of</strong> NT.The effects <strong>of</strong> PYY on pancreatic cancer growth have beenexam<strong>in</strong>ed. Treatment <strong>of</strong> <strong>the</strong> human pancreatic cancer celll<strong>in</strong>es, MIA PaCa-2 <strong>and</strong> PANC-1, with <strong>the</strong> syn<strong>the</strong>tic analog <strong>of</strong>Downloaded from edrv.endojournals.org by on July 16, 2007
Thomas et al. • <strong>Gastro<strong>in</strong>test<strong>in</strong>al</strong> <strong>Hormones</strong> <strong>and</strong> <strong>Proliferation</strong> Endocr<strong>in</strong>e Reviews, October 2003, 24(5):571–599 585PYY, PYY 22–36, <strong>in</strong>hibited <strong>the</strong> growth <strong>of</strong> <strong>the</strong>se cells <strong>in</strong> vitro(240). A significant decrease <strong>in</strong> <strong>the</strong> growth <strong>of</strong> human pancreaticcancer xenografts was demonstrated <strong>in</strong> nude micegiven PYY 22–36 for 2 wk (241). Similarly, <strong>the</strong>re was a decrease<strong>in</strong> cyclic adenos<strong>in</strong>e monophosphatase expression <strong>and</strong>augmentation <strong>of</strong> <strong>the</strong> tumor-suppress<strong>in</strong>g capability <strong>of</strong> 5-fluorouracil <strong>and</strong> leucovor<strong>in</strong> (241, 242). More recently, Liuet al. (243) reported that a biot<strong>in</strong>ylated PYY analog 14–36,l<strong>in</strong>ked to a fluorescent dye attached to streptavid<strong>in</strong>, significantlybound to human pancreatic cancer cells MIA PaCa-2<strong>and</strong> PANC-1 <strong>and</strong> <strong>in</strong>hibited <strong>the</strong> growth <strong>of</strong> <strong>the</strong>se pancreaticcancer cells. It was postulated that biot<strong>in</strong>ylated PYY 14–36could be used to selectively deliver toxic agents to <strong>the</strong> cancersor, conversely, as a diagnostic tool tagged with a fluorescentagent to identify <strong>the</strong> extent <strong>of</strong> disease. The results <strong>of</strong> <strong>the</strong>sestudies suggest that PYY can <strong>in</strong>hibit pancreatic cancergrowth. However, it has not been determ<strong>in</strong>ed whe<strong>the</strong>r amajority <strong>of</strong> pancreatic cancers express receptors for PYY.Also, <strong>the</strong> cellular mechanisms for <strong>the</strong> <strong>in</strong>hibitory effect <strong>of</strong> PYYneed to be better del<strong>in</strong>eated.Similar to PYY, somatostat<strong>in</strong> <strong>and</strong> its analogs have beenevaluated as antiproliferative agents <strong>in</strong> <strong>the</strong> treatment <strong>of</strong> pancreaticcancer. Many pancreatic cancers have high-aff<strong>in</strong>ityb<strong>in</strong>d<strong>in</strong>g sites for somatostat<strong>in</strong> (244, 245); however, <strong>the</strong> precisemechanisms regulat<strong>in</strong>g <strong>the</strong> antiproliferative effect <strong>of</strong> somatostat<strong>in</strong>have not been entirely elucidated. Potential mechanisms<strong>in</strong>clude a direct receptor-mediated effect <strong>and</strong> possiblyan <strong>in</strong>direct effect that could <strong>in</strong>clude <strong>in</strong>hibition <strong>of</strong>angiogenesis <strong>and</strong>/or <strong>the</strong> suppression <strong>of</strong> GH <strong>and</strong> IGF secretion(244, 245). Redd<strong>in</strong>g <strong>and</strong> Schally (246) reported significantreductions <strong>in</strong> tumor weight <strong>and</strong> volume <strong>in</strong> Wistar-Lewisrats bear<strong>in</strong>g <strong>the</strong> pancreatic ac<strong>in</strong>ar tumor DNC-322 after a21-d adm<strong>in</strong>istration <strong>of</strong> somatostat<strong>in</strong> analog [l-5-Br-Trp 8 ]somatostat<strong>in</strong>-14.Upp et al. (64) demonstrated <strong>in</strong>hibition <strong>of</strong> twohuman pancreatic cancer xenografts (SKI <strong>and</strong> CAV) <strong>in</strong> nudemice by <strong>the</strong> adm<strong>in</strong>istration <strong>of</strong> <strong>the</strong> long-act<strong>in</strong>g somatostat<strong>in</strong>analog SMS 201-995 (octreotide). O<strong>the</strong>r growth factors (e.g.,EGF) may modulate <strong>the</strong> growth <strong>of</strong> pancreatic cancers. In vitrostudies by Hierowski et al. (247) <strong>and</strong> Liebow et al. (248)demonstrated receptors for EGF <strong>and</strong> somatostat<strong>in</strong> <strong>in</strong> <strong>the</strong> MIAPaCa-2 cancer cell l<strong>in</strong>e. The effects <strong>of</strong> somatostat<strong>in</strong> may bethrough its actions on o<strong>the</strong>r growth factors <strong>and</strong> <strong>the</strong>ir receptors.For example, <strong>the</strong> long-act<strong>in</strong>g analog RC-160 <strong>in</strong>hibitsproliferation <strong>of</strong> <strong>the</strong> pancreatic cancer cell l<strong>in</strong>e MIA PaCa-2,possibly by activat<strong>in</strong>g dephosphorylation <strong>of</strong> <strong>the</strong> EGF receptor(247, 248).Colorectal cancer is a significant health problem worldwide,with <strong>the</strong> death rate rema<strong>in</strong><strong>in</strong>g third to lung <strong>and</strong> prostatecancer <strong>in</strong> men <strong>and</strong> lung <strong>and</strong> breast cancer <strong>in</strong> women(249). Approximately 57,000 deaths are expected to occur thisyear <strong>in</strong> <strong>the</strong> United States (249). Current chemo<strong>the</strong>rapeuticregimens are relatively <strong>in</strong>effective for metastatic disease. Theeffects <strong>of</strong> GI hormones, particularly gastr<strong>in</strong>, have been welldescribed <strong>and</strong> characterized <strong>in</strong> various colon cancer models.Gastr<strong>in</strong> stimulates <strong>the</strong> growth <strong>of</strong> colorectal cancers thatpossess high-aff<strong>in</strong>ity gastr<strong>in</strong> receptors, <strong>in</strong>clud<strong>in</strong>g <strong>the</strong> mousecolon cancer cell l<strong>in</strong>e MC-26. The adm<strong>in</strong>istration <strong>of</strong> <strong>the</strong> gastr<strong>in</strong>receptor antagonist, proglumide, <strong>in</strong>hibited <strong>the</strong> growth <strong>of</strong>MC-26 tumors <strong>in</strong> vivo <strong>and</strong> prolonged survival <strong>of</strong> tumorbear<strong>in</strong>gmice (Fig. 5) (250). Ishizuka et al. (251) have shownthat gastr<strong>in</strong> stimulates <strong>the</strong> growth <strong>of</strong> two human colon cancercell l<strong>in</strong>es, LoVo <strong>and</strong> HT29, but <strong>in</strong>hibits <strong>the</strong> growth <strong>of</strong> a thirdcolon cancer cell l<strong>in</strong>e, HCT-116, suggest<strong>in</strong>g that differentgastr<strong>in</strong> receptor subtypes or o<strong>the</strong>r signal transduction pathwaysregulate <strong>the</strong> trophic effects <strong>of</strong> gastr<strong>in</strong>. As an alternateapproach, we have assessed <strong>the</strong> effect <strong>of</strong> suppress<strong>in</strong>g endogenousgastr<strong>in</strong> with <strong>the</strong> prostagl<strong>and</strong><strong>in</strong> analog enprostil onMC-26 tumor growth <strong>and</strong> found that, similar to our results<strong>in</strong> gastric cancers, enprostil significantly <strong>in</strong>hibited MC-26tumor growth <strong>in</strong> vivo (252, 253).In addition to <strong>the</strong> experimental evidence for <strong>the</strong> effect <strong>of</strong>gastr<strong>in</strong> on colon cancers, cl<strong>in</strong>ical studies have assessed <strong>the</strong>potential role <strong>of</strong> gastr<strong>in</strong> <strong>and</strong> gastr<strong>in</strong> receptor expression <strong>in</strong>colorectal tumors. Upp et al. (254) analyzed 67 primary colorectalcancers for gastr<strong>in</strong> receptors <strong>and</strong> found a spectrum <strong>of</strong>receptor expression, suggest<strong>in</strong>g a correlation between tumorstage <strong>and</strong> <strong>the</strong> presence <strong>of</strong> gastr<strong>in</strong> receptors. A significantlygreater percentage <strong>of</strong> patients (52%) with early cancers(Dukes’ A <strong>and</strong> B) had gastr<strong>in</strong> receptor contents greater than10 fmol/mg when compared with patients with more advancedcolorectal cancers (Fig. 6). In contrast, five <strong>of</strong> 19Dukes’ C patients <strong>and</strong> eight <strong>of</strong> 16 Dukes’ D patients withgastr<strong>in</strong> receptors less than 10 fmol/mg prote<strong>in</strong> developedtumor recurrence or died. This study was <strong>the</strong> first to suggestthat assessment <strong>of</strong> gastr<strong>in</strong> receptor expression <strong>in</strong> colorectalcancers may predict tumor stage as well as overall survival.Fur<strong>the</strong>r studies are needed to correlate <strong>the</strong> receptor expressionwith long-term cl<strong>in</strong>ical parameters.Hoose<strong>in</strong> et al. (255, 256) demonstrated that gastr<strong>in</strong> stimulatescolorectal cancer cell growth <strong>and</strong> that this stimulationwas possibly attributable to an autocr<strong>in</strong>e mechanism. Thegrowth <strong>of</strong> six colon cancer cell l<strong>in</strong>es was assessed after treatmentwith two gastr<strong>in</strong> receptor antagonists, proglumide <strong>and</strong>benzotript, or antibodies to gastr<strong>in</strong> (255). Both <strong>in</strong>hibitorssuppressed monolayer cell growth <strong>in</strong> all <strong>of</strong> <strong>the</strong> colon cancerl<strong>in</strong>es. Fur<strong>the</strong>rmore, <strong>in</strong> HCT-116 cells, <strong>the</strong> addition <strong>of</strong> antigastr<strong>in</strong>antisera resulted <strong>in</strong> a concentration-dependent <strong>in</strong>hi-C. Colorectal cancerFIG. 5. Survival <strong>of</strong> MC-26 tumor-bear<strong>in</strong>g mice after treatment withnormal sal<strong>in</strong>e (solid l<strong>in</strong>e), proglumide beg<strong>in</strong>n<strong>in</strong>g on <strong>the</strong> day <strong>of</strong> tumor<strong>in</strong>oculation (long-dash l<strong>in</strong>e), or proglumide beg<strong>in</strong>n<strong>in</strong>g 7 d after <strong>in</strong>oculation(short-dash l<strong>in</strong>e). [From R. D. Beauchamp et al.: Ann Surg202:303–309, 1985 (250).]Downloaded from edrv.endojournals.org by on July 16, 2007
586 Endocr<strong>in</strong>e Reviews, October 2003, 24(5):571–599 Thomas et al. • <strong>Gastro<strong>in</strong>test<strong>in</strong>al</strong> <strong>Hormones</strong> <strong>and</strong> <strong>Proliferation</strong>FIG. 6. Gastr<strong>in</strong> receptor (GR) content by stage <strong>of</strong> disease. A, Number<strong>of</strong> patients with tumors highly positive for gastr<strong>in</strong> receptors (10fmol/mg prote<strong>in</strong>) <strong>and</strong> ei<strong>the</strong>r negative or poorly positive (10 fmol/mgprote<strong>in</strong>) for receptors, by stage <strong>of</strong> disease. B, Percentage <strong>of</strong> patientswith tumors demonstrat<strong>in</strong>g more than 10 fmol gastr<strong>in</strong> receptors (GRper milligram prote<strong>in</strong>) by stage <strong>of</strong> disease. *, P 0.05. [Reproducedwith permission from J. R. Upp Jr. et al.: Cancer Res 49:488–492,1989 (254).]bition <strong>of</strong> cellular proliferation <strong>in</strong> serum-free media. Next,proliferation <strong>of</strong> <strong>the</strong> colon cancer cell l<strong>in</strong>es HCT-116 <strong>and</strong> CBSwas assessed us<strong>in</strong>g dibutyryl cyclic GMP (cGMP), a gastr<strong>in</strong>receptor antagonist (256). Dibutyryl cGMP <strong>in</strong>hibited proliferation<strong>and</strong> <strong>in</strong>duced morphological change <strong>in</strong> both cell l<strong>in</strong>es.In b<strong>in</strong>d<strong>in</strong>g studies, dibutyryl cGMP competed with 125 I-labeled gastr<strong>in</strong> for b<strong>in</strong>d<strong>in</strong>g to HCT-116 cells (IC 50 , 1.8 mm).RIA <strong>of</strong> conditioned media from both cell l<strong>in</strong>es demonstrated<strong>the</strong> presence <strong>of</strong> gastr<strong>in</strong>. Additionally, Nor<strong>the</strong>rn blot analysisdetected expression <strong>of</strong> gastr<strong>in</strong> mRNA.Additional studies provide support for <strong>the</strong> potential autocr<strong>in</strong>erole <strong>of</strong> gastr<strong>in</strong> <strong>in</strong> colorectal cancer growth. Smith <strong>and</strong>Watson (257) found no expression <strong>of</strong> gastr<strong>in</strong> or gastr<strong>in</strong>/CCK-B receptors <strong>in</strong> normal colonic mucosa although demonstrat<strong>in</strong>g78 <strong>and</strong> 81% expression, respectively, <strong>in</strong> colonicpolyps. Immunohistochemical analysis identified progastr<strong>in</strong><strong>in</strong> 91% <strong>of</strong> polyps, Gly-G <strong>in</strong> 80%, <strong>and</strong> G-17 <strong>in</strong> only 47%. Thisstudy was <strong>the</strong> first to demonstrate widespread expression <strong>of</strong>both gastr<strong>in</strong> <strong>and</strong> its receptor <strong>in</strong> preneoplastic colorectal polyps,suggest<strong>in</strong>g that gastr<strong>in</strong> may promote tumor progressionthrough <strong>the</strong> adenoma-carc<strong>in</strong>oma sequence <strong>in</strong> <strong>the</strong> colon. Becausea majority <strong>of</strong> human colon cancers express <strong>the</strong> gastr<strong>in</strong>gene (258), it was suggested that expression <strong>of</strong> gastr<strong>in</strong> maybe critically l<strong>in</strong>ked to gastr<strong>in</strong>-controlled growth <strong>of</strong> cancercells. This supposition was fur<strong>the</strong>r supported by <strong>the</strong> demonstrationthat antisense RNA to <strong>the</strong> gastr<strong>in</strong> gene <strong>in</strong>hibited<strong>the</strong> growth <strong>of</strong> Colo-320 <strong>and</strong> HCT-116 colon cancer cells,which express gastr<strong>in</strong>, whereas <strong>the</strong> growth <strong>of</strong> Colo-205Acells, which do not express gastr<strong>in</strong>, was not affected by antisensetreatment (66).Although <strong>the</strong> proliferative effects <strong>of</strong> exogenous gastr<strong>in</strong> ongastr<strong>in</strong>-receptor positive colorectal cancers have been demonstrated<strong>in</strong> numerous <strong>in</strong> vitro <strong>and</strong> <strong>in</strong> vivo models, <strong>the</strong> roles<strong>of</strong> endogenous hypergastr<strong>in</strong>emia <strong>and</strong> colon carc<strong>in</strong>ogenesisare controversial. McGregor et al. (259) found that antralexclusion, which produces a pr<strong>of</strong>ound hypergastr<strong>in</strong>emia,<strong>in</strong>creased DNA syn<strong>the</strong>sis <strong>and</strong> carc<strong>in</strong>ogen-<strong>in</strong>duced colon tumorsbut did not alter <strong>the</strong> <strong>in</strong>cidence <strong>of</strong> tumor formation. Incontrast, Oscarson et al. (260) demonstrated that endogenoushypergastr<strong>in</strong>emia, <strong>in</strong>duced by fundectomy, did not potentiatedimethylhydraz<strong>in</strong>e (DNH)-<strong>in</strong>duced colon carc<strong>in</strong>ogenesis.The discrepancies between <strong>the</strong>se studies may be relatedto <strong>the</strong> tim<strong>in</strong>g <strong>and</strong> adm<strong>in</strong>istration <strong>of</strong> <strong>the</strong> carc<strong>in</strong>ogen as well as<strong>the</strong> method <strong>of</strong> produc<strong>in</strong>g hypergastr<strong>in</strong>emia.In addition, <strong>the</strong>re rema<strong>in</strong>s considerable confusion regard<strong>in</strong>g<strong>the</strong> forms <strong>of</strong> gastr<strong>in</strong> that are responsible for <strong>the</strong> regulation<strong>of</strong> human colorectal cancer growth. For example, Kameyamaet al. (261) reported that <strong>the</strong> <strong>in</strong>cidence <strong>of</strong> liver metastasis <strong>in</strong>colorectal cancer was significantly higher <strong>in</strong> patients wi<strong>the</strong>levated serum gastr<strong>in</strong> levels. Thorburn et al. (262) conducteda case control study among 128,992 subscribers to a healthma<strong>in</strong>tenance program <strong>and</strong> found that median gastr<strong>in</strong> levelswere similar <strong>in</strong> patients with colorectal cancers <strong>and</strong> matchedcontrols (41.7 vs. 40.7 pg/ml). However, elevated gastr<strong>in</strong>levels were associated with <strong>in</strong>creased risk <strong>of</strong> colorectal malignancy(odds ratio, 3.9). These authors concluded that thisrelationship was causal, with 8.6% <strong>of</strong> colorectal cancers thatcould be attributed to hypergastr<strong>in</strong>emia. O<strong>the</strong>r studies havedemonstrated <strong>in</strong>creased circulat<strong>in</strong>g levels <strong>of</strong> gastr<strong>in</strong> <strong>in</strong> somepatients with colorectal cancer but little or no change <strong>in</strong>o<strong>the</strong>rs (263–265).There is <strong>in</strong>creas<strong>in</strong>g evidence that Gly-G <strong>and</strong> <strong>the</strong> lessprocessedprogastr<strong>in</strong> peptides, <strong>the</strong> so-called nonamidatedgastr<strong>in</strong>s, may be <strong>the</strong> critical regulator <strong>of</strong> colorectal cancergrowth. Siddheshwar et al. (266) found elevated levels <strong>of</strong>Gly-G, but not G-17, <strong>in</strong> patients with colorectal cancer <strong>and</strong>dysplastic polyps. Stepan et al. (267) found that G-17 failedto b<strong>in</strong>d or stimulate <strong>the</strong> growth <strong>of</strong> LoVo, HT29, HCT-116,Colo 320DM, or T84 cells. In contrast, LoVo <strong>and</strong> HT29 cellsdisplayed saturable b<strong>in</strong>d<strong>in</strong>g <strong>of</strong> Gly-G. Treatment with Gly-G<strong>in</strong>creased proliferation <strong>of</strong> LoVo <strong>and</strong> HT29 cells as measuredby [ 3 H]thymid<strong>in</strong>e uptake; <strong>the</strong>se effects were not blocked byG-17 or <strong>the</strong> gastr<strong>in</strong>/CCK-B receptor antagonist, PD134308.These data suggest that Gly-G, b<strong>in</strong>d<strong>in</strong>g to a novel receptor,plays a critical role <strong>in</strong> <strong>the</strong> growth <strong>of</strong> certa<strong>in</strong> colon cancer cells.Similarly, Litvak et al. (268) found that Gly-G stimulatedgrowth <strong>of</strong> DLD-1 cancer xenografts <strong>in</strong> nude mice. Moreover,a novel gastr<strong>in</strong>-receptor antagonist, JMV1155, blocked <strong>the</strong>stimulatory effects <strong>of</strong> Gly-G.Additional support for a role <strong>of</strong> gastr<strong>in</strong>s, o<strong>the</strong>r than <strong>the</strong> amidatedG-17 <strong>and</strong> G-34 gastr<strong>in</strong>s, <strong>in</strong> colorectal cancer growth isprovided by f<strong>in</strong>d<strong>in</strong>gs <strong>in</strong> transgenic mice. S<strong>in</strong>gh et al. (269, 270)evaluated <strong>the</strong> mitogenic <strong>in</strong>duction <strong>and</strong> adenoma/adenocarc<strong>in</strong>omaformation after azoxymethane treatment <strong>in</strong> miceDownloaded from edrv.endojournals.org by on July 16, 2007
Thomas et al. • <strong>Gastro<strong>in</strong>test<strong>in</strong>al</strong> <strong>Hormones</strong> <strong>and</strong> <strong>Proliferation</strong> Endocr<strong>in</strong>e Reviews, October 2003, 24(5):571–599 587overexpress<strong>in</strong>g progastr<strong>in</strong> compared with wild-type mice <strong>and</strong>mice overexpress<strong>in</strong>g G-17. Progastr<strong>in</strong>-overexpress<strong>in</strong>g mice displayed<strong>in</strong>creased tumor formation <strong>and</strong> mitogenic <strong>in</strong>dices comparedwith both wild-type <strong>and</strong> G-17-overexpress<strong>in</strong>g mice.Recently, Siddheshwar et al. (266) found that progastr<strong>in</strong>, <strong>and</strong> notG-17, was elevated <strong>in</strong> patients with colorectal cancer <strong>and</strong> dysplasticpolyps, thus provid<strong>in</strong>g cl<strong>in</strong>ical support for <strong>the</strong> importance<strong>of</strong> nonamidated gastr<strong>in</strong>s.Most recently, <strong>the</strong> identification <strong>of</strong> a constitutively activevariant <strong>of</strong> <strong>the</strong> gastr<strong>in</strong>/CCK-B receptor is provid<strong>in</strong>g novel<strong>in</strong>sight <strong>in</strong>to fur<strong>the</strong>r effects <strong>of</strong> gastr<strong>in</strong> <strong>in</strong> <strong>the</strong> proliferation <strong>of</strong>colorectal cancers. Hellmich et al. (271) identified a CCK-Breceptor splice variant that is expressed only <strong>in</strong> colorectalcancers but not <strong>in</strong> normal colonic mucosa adjacent to <strong>the</strong>cancer. This splice variant exhibits constitutive (lig<strong>and</strong><strong>in</strong>dependent)activation <strong>of</strong> pathways regulat<strong>in</strong>g <strong>in</strong>tracellular-freecalcium <strong>and</strong> cell growth. Primary cultures <strong>of</strong> cellsisolated from resected colorectal cancers exhibited spontaneous,lig<strong>and</strong>-<strong>in</strong>dependent oscillatory <strong>in</strong>creases <strong>in</strong> <strong>in</strong>tracellularcalcium, with an <strong>in</strong>crease <strong>in</strong> <strong>in</strong>tracellular calcium notedwith <strong>the</strong> addition <strong>of</strong> G-17. Selective CCK-B receptor antagonistsblocked <strong>the</strong> G-17-stimulated calcium stimulation butnot <strong>the</strong> spontaneous <strong>in</strong>tracellular calcium oscillations. Cellsexpress<strong>in</strong>g <strong>the</strong> CCK-B receptor splice variant exhibited an<strong>in</strong>creased growth rate <strong>in</strong> <strong>the</strong> absence <strong>of</strong> G-17 compared withcells stably transfected with <strong>the</strong> wild-type CCK-B receptor.The selective pattern <strong>of</strong> expression, <strong>the</strong> constitutive activity<strong>and</strong> trophic action associated with this CCK-B receptor splicevariant suggested that this novel variant may regulate colorectalcancer cell proliferation through a gastr<strong>in</strong>-<strong>in</strong>dependentmechanism. This splice variant has recently been identified<strong>in</strong> pancreatic cancers, suggest<strong>in</strong>g that expression may not belimited to colorectal cancer (272).In addition to gastr<strong>in</strong>, NT stimulates growth <strong>of</strong> certa<strong>in</strong>human colon cancer cell l<strong>in</strong>es both <strong>in</strong> vitro <strong>and</strong> <strong>in</strong> vivo (273,274). Yosh<strong>in</strong>aga et al. (273) demonstrated that adm<strong>in</strong>istration<strong>of</strong> NT (ei<strong>the</strong>r 300 or 600 g/kg, three times daily for 21 d)significantly stimulated mean tumor area, weight, <strong>and</strong> DNA,RNA, <strong>and</strong> prote<strong>in</strong> content <strong>of</strong> <strong>the</strong> mur<strong>in</strong>e colon cancer, MC-26.In addition, <strong>the</strong> survival rate <strong>of</strong> mice bear<strong>in</strong>g MC-26 tumors<strong>and</strong> treated with NT was significantly decreased comparedwith <strong>the</strong> control group. Similarly, NT stimulated growth <strong>of</strong><strong>the</strong> human colon cancer, LoVo. We have shown that approximately25% <strong>of</strong> colon cancers analyzed express NT mRNA(274). An autocr<strong>in</strong>e effect for NT <strong>in</strong> certa<strong>in</strong> colorectal cancersis postulated on <strong>the</strong> basis <strong>of</strong> NT expression <strong>in</strong> four colorectalcancer cell l<strong>in</strong>es (LoVo, HT29, HCT-116, <strong>and</strong> CBS), one <strong>of</strong>n<strong>in</strong>e cancer xenografts, <strong>and</strong> two <strong>of</strong> six freshly resected coloncancers; NT expression was not identified <strong>in</strong> <strong>the</strong> adjacentnormal colonic tissue. NT peptide was detected <strong>in</strong> LoVo,HT29, <strong>and</strong> HCT-116 extracts; <strong>and</strong> NTR expression was demonstrated<strong>in</strong> HT29 <strong>and</strong> HCT-116 cells. In a study by Rovereet al. (275), all 13 human colon cancer cell l<strong>in</strong>es displayed lowto moderate levels <strong>of</strong> pro-NT/neuromed<strong>in</strong> N prote<strong>in</strong> expression.Only six <strong>of</strong> <strong>the</strong>se 13 tumors, however, processed <strong>the</strong>precursor to produce NT <strong>and</strong> larger precursor fragmentsend<strong>in</strong>g with <strong>the</strong> NT or neuromed<strong>in</strong> N sequence. Similar to<strong>the</strong> signal<strong>in</strong>g pathways mediat<strong>in</strong>g <strong>the</strong> effects <strong>of</strong> NT <strong>in</strong> pancreaticcancers, Ehlers et al. (276) have shown that NT treatment<strong>of</strong> <strong>the</strong> human colon cancer cell l<strong>in</strong>e KM20, whichexpresses high levels <strong>of</strong> <strong>the</strong> NTR, results <strong>in</strong> calcium mobilizationas well as activation <strong>of</strong> <strong>the</strong> ERK pathway. Thesef<strong>in</strong>d<strong>in</strong>gs suggest that <strong>the</strong> proliferative effect <strong>of</strong> NT may bethrough <strong>the</strong> ERK stimulatory pathway <strong>and</strong> that, similar togastr<strong>in</strong>, NT may be an autocr<strong>in</strong>e growth factor <strong>in</strong> certa<strong>in</strong>colon cancers. The fact that <strong>in</strong>tralum<strong>in</strong>al fats are <strong>the</strong> mostpotent stimulus for NT release suggests an association between<strong>the</strong> known stimulatory effects <strong>of</strong> fats on colon carc<strong>in</strong>ogenesis<strong>and</strong> hormones, such as NT, which <strong>in</strong>crease coloncancer proliferation.Additionally, NT appears to promote carc<strong>in</strong>ogenesis <strong>in</strong> <strong>the</strong>colon <strong>of</strong> rats. Tatsuta et al. (184) reported that rats given10 weekly <strong>in</strong>jections <strong>of</strong> azoxymethane (7.4 mg/kg), as well asNT (200 g/kg every o<strong>the</strong>r day for 40 wk), displayed significant<strong>in</strong>creases <strong>in</strong> <strong>the</strong> number <strong>and</strong> size <strong>of</strong> colon tumors,with a higher degree <strong>of</strong> submucosal penetration. This wascontrasted by <strong>the</strong> fact that NT alone did not <strong>in</strong>crease <strong>the</strong>overall <strong>in</strong>cidence <strong>of</strong> colonic tumors <strong>in</strong> rats. NT caused asignificant <strong>in</strong>crease <strong>in</strong> tumor cell modification above that <strong>of</strong>normal colonic mucosa.Similar to f<strong>in</strong>d<strong>in</strong>gs <strong>in</strong> gastric <strong>and</strong> pancreatic cancers, somatostat<strong>in</strong>has been shown to <strong>in</strong>hibit growth <strong>of</strong> certa<strong>in</strong> humancolon cancers (65–67). Our laboratory has found that <strong>the</strong>somatostat<strong>in</strong> analog, MK-678, significantly <strong>in</strong>hibited growth<strong>of</strong> human colon cancer xenografts (RIP <strong>and</strong> DRUM) (277).One mechanism may be due to <strong>in</strong>hibition <strong>of</strong> gastr<strong>in</strong> release,which is fur<strong>the</strong>r supported by <strong>the</strong> demonstration that adm<strong>in</strong>istration<strong>of</strong> octreotide blocked gastr<strong>in</strong>-<strong>in</strong>duced stimulation<strong>of</strong> <strong>the</strong> MC-26 colon cancer cell l<strong>in</strong>e (65). Melen-Muchaet al. (278) have demonstrated that octreotide <strong>in</strong>hibits proliferation,as measured by BrdU, <strong>and</strong> <strong>in</strong>creases apoptosis, asassessed by <strong>in</strong>creased nuclear DNA fragmentation. Octreotidedecreases <strong>the</strong> proliferation/apoptosis ratio <strong>in</strong> favor <strong>of</strong>cell death <strong>in</strong> Colon 38 transplanted tumors <strong>in</strong> mice. Inhibition<strong>of</strong> colorectal cancer growth with somatostat<strong>in</strong> analogs hasnot been demonstrated <strong>in</strong> all cancer cell l<strong>in</strong>es. di Paolo et al.(67) found that <strong>the</strong> somatostat<strong>in</strong> analog, SMS 201-995, <strong>in</strong>hibitedgrowth <strong>of</strong> SW480 colon cancer cells, but failed to alter<strong>the</strong> growth <strong>of</strong> SW620 cells. However, SW620 cells were sensitiveto SMS 201-995 when used <strong>in</strong> comb<strong>in</strong>ation with IL-1 or<strong>in</strong>terferon-. These results suggest <strong>the</strong> existence <strong>of</strong> differentsomatostat<strong>in</strong> receptor subtypes, which may account for differentialeffects <strong>of</strong> somatostat<strong>in</strong> analogs <strong>in</strong> colorectal cancercells. A recent study has found that l<strong>in</strong>k<strong>in</strong>g toxic chemo<strong>the</strong>rapeuticagents to somatostat<strong>in</strong> analogs that selectively b<strong>in</strong>dto somatostat<strong>in</strong> receptor subtypes can direct chemo<strong>the</strong>rapeuticagents <strong>and</strong> provide more efficient delivery <strong>of</strong> cytotoxicagents to colorectal tumors (279).D. O<strong>the</strong>r cancersGI hormones have been shown to play trophic roles <strong>in</strong> neoplasmsoutside <strong>the</strong> GI tract as well. Notable examples <strong>in</strong>cludebreast, lung, <strong>and</strong> prostate cancers <strong>and</strong> neuroblastomas.1. Breast cancer. In 2002, <strong>of</strong> <strong>the</strong> 647,000 new cases <strong>of</strong> canceraffect<strong>in</strong>g women <strong>in</strong> <strong>the</strong> United States, almost one third werebreast cancers, mak<strong>in</strong>g breast cancer <strong>the</strong> most prevalent canceramong women (249). Hormonal <strong>the</strong>rapy, with antiestrogenagents such as tamoxifen, is an important adjuvant agentDownloaded from edrv.endojournals.org by on July 16, 2007
588 Endocr<strong>in</strong>e Reviews, October 2003, 24(5):571–599 Thomas et al. • <strong>Gastro<strong>in</strong>test<strong>in</strong>al</strong> <strong>Hormones</strong> <strong>and</strong> <strong>Proliferation</strong><strong>in</strong> patients with estrogen receptor-positive cancers <strong>and</strong> maybe useful <strong>in</strong> prevention as well (280). Fur<strong>the</strong>rmore, Hercept<strong>in</strong>,a monoclonal antibody growth factor receptor that blocks<strong>the</strong> Her-2/neu (c-erb-B2) growth factor receptor, a member<strong>of</strong> <strong>the</strong> EGF receptor family, has recently been shown to be <strong>of</strong>potential benefit to patients with breast cancers that are positivefor Her-2/neu (280). Certa<strong>in</strong> GI hormones have alsobeen shown to affect breast cancer growth.Goettler et al. (281) noted <strong>in</strong>creased postpr<strong>and</strong>ial levels <strong>of</strong>gastr<strong>in</strong> <strong>in</strong> women with stage I <strong>and</strong> II breast cancer. In contrast,levels <strong>of</strong> NT <strong>and</strong> CCK were not altered. This <strong>in</strong>crease<strong>in</strong> gastr<strong>in</strong> was found to be <strong>in</strong>dependent <strong>of</strong> diet <strong>and</strong> suggestedthat hypergastr<strong>in</strong>emia may contribute to breast carc<strong>in</strong>ogenesis.These f<strong>in</strong>d<strong>in</strong>gs are fur<strong>the</strong>r supported by <strong>the</strong> occasionalexpression <strong>of</strong> gastr<strong>in</strong> <strong>in</strong> breast carc<strong>in</strong>omas (282). Nesl<strong>and</strong>et al. (283) screened 38 <strong>in</strong>filtrat<strong>in</strong>g ductal carc<strong>in</strong>omas forgastr<strong>in</strong> <strong>and</strong> found scattered positive-sta<strong>in</strong><strong>in</strong>g cells for gastr<strong>in</strong><strong>in</strong> five <strong>of</strong> 38 cases. An <strong>in</strong>direct mechanism for <strong>the</strong> effect <strong>of</strong>gastr<strong>in</strong> has been postulated <strong>in</strong> breast cancers. Gastr<strong>in</strong>enhancedproteolysis leads to <strong>in</strong>creased availability <strong>of</strong> tryptophan-derivedseroton<strong>in</strong> that, <strong>in</strong> turn, stimulates pituitaryrelease <strong>of</strong> prolact<strong>in</strong> (a central activator <strong>of</strong> breast development)<strong>and</strong> may contribute to breast cancer growth (281).Although limited <strong>and</strong> relatively circumstantial, <strong>the</strong>se datasuggest that gastr<strong>in</strong> may play some role <strong>in</strong> breast cancerdevelopment or growth. More studies are warranted to betterascerta<strong>in</strong> whe<strong>the</strong>r any association exists.The potential effects <strong>of</strong> BBS/GRP on breast cancers appearbetter established than <strong>the</strong> effects <strong>of</strong> gastr<strong>in</strong>. Breast milkconta<strong>in</strong>s GRP, <strong>and</strong> receptors for GRP have been noted <strong>in</strong> amajority <strong>of</strong> breast cancers (284). A recent report by Reubi et al.(284) found that high-density GRP receptors were detected<strong>in</strong> neoplastic mammary cells us<strong>in</strong>g <strong>in</strong> vitro autoradiography:29 <strong>of</strong> 46 <strong>in</strong>vasive ductal carc<strong>in</strong>omas, 11 <strong>of</strong> 17 ductal carc<strong>in</strong>omas<strong>in</strong> situ, one <strong>of</strong> four <strong>in</strong>vasive lobular carc<strong>in</strong>omas, one<strong>of</strong> two lobular carc<strong>in</strong>omas <strong>in</strong> situ, <strong>and</strong> one muc<strong>in</strong>ous <strong>and</strong> onetubular carc<strong>in</strong>oma. A heterogeneous GRP receptor distributionwas found <strong>in</strong> 32 <strong>of</strong> 52 <strong>in</strong>vasive carc<strong>in</strong>omas <strong>and</strong> 12 <strong>of</strong> 19cases <strong>of</strong> carc<strong>in</strong>oma <strong>in</strong> situ. GRP receptors were also present<strong>in</strong> normal breast tissue to some degree <strong>and</strong> displayed nocorrelation with <strong>the</strong> amount <strong>of</strong> receptors found <strong>in</strong> neoplastictissues. These data suggest that GRP may contribute to bothneoplastic <strong>and</strong> nonneoplastic breast tissue growth <strong>and</strong> <strong>the</strong>potential <strong>of</strong> GRP-target<strong>in</strong>g <strong>of</strong> breast tissue for sc<strong>in</strong>tigraphy<strong>and</strong> directed chemo<strong>the</strong>rapies. In this regard, a recent reportby Bajo et al. (285) demonstrated <strong>the</strong> potential utility <strong>of</strong> specificBBS antagonists on <strong>the</strong> <strong>in</strong>hibition <strong>of</strong> breast cancergrowth. The BBS/GRP <strong>in</strong>hibitors RC-3095 <strong>and</strong> RC-3940 IIgiven for 6 wk produced a 40 <strong>and</strong> 50% reduction <strong>in</strong> <strong>the</strong>volume <strong>of</strong> MDA-MB-435 human breast cancer cell xenografts,respectively. The mechanism <strong>of</strong> action may bethrough both direct <strong>and</strong> <strong>in</strong>direct effects because BBS wasnoted to decrease <strong>the</strong> expression <strong>of</strong> <strong>the</strong> Her-2/neu oncoprote<strong>in</strong><strong>and</strong>, fur<strong>the</strong>rmore, decrease expression <strong>of</strong> AP-1 transcriptionfactors (c-jun <strong>and</strong> c-fos). These data suggest that specificBBS/GRP antagonists may be useful as adjuvant <strong>the</strong>rapy forbreast cancer patients <strong>in</strong> a similar fashion to tamoxifen <strong>and</strong>Hercept<strong>in</strong> be<strong>in</strong>g commonly used <strong>in</strong> <strong>the</strong> treatment regimen.Fur<strong>the</strong>r work is required to establish which patients maybenefit from BBS/GRP receptor antagonists.2. Lung cancer. Lung cancer is <strong>the</strong> lead<strong>in</strong>g cause <strong>of</strong> cancerrelateddeaths <strong>in</strong> <strong>the</strong> United States. Frequently, lung cancershave spread beyond surgical resection at <strong>the</strong> time <strong>of</strong> diagnosis.Therapeutic attempts to limit this disease are <strong>the</strong>nconf<strong>in</strong>ed to adjuvant <strong>the</strong>rapies; <strong>the</strong>refore, to realize improvement<strong>in</strong> <strong>the</strong> mortality from lung cancers, improved chemo<strong>the</strong>rapeuticstrategies are needed.There have been a number <strong>of</strong> studies l<strong>in</strong>k<strong>in</strong>g GRP <strong>and</strong>BBS-like peptides (BLPs; a group <strong>in</strong>clud<strong>in</strong>g GRP <strong>and</strong> neuromed<strong>in</strong>B) <strong>in</strong> <strong>the</strong> regulation <strong>of</strong> small cell lung cancer (SCLC),suggest<strong>in</strong>g that <strong>the</strong>se BLPs act <strong>in</strong> an autocr<strong>in</strong>e or paracr<strong>in</strong>efashion to stimulate growth (286–288). Human BLPs, specificallyGRP, are produced <strong>and</strong> secreted by SCLC cells, <strong>and</strong>a number <strong>of</strong> <strong>the</strong>se cells express <strong>the</strong> GRP receptor <strong>and</strong> neuromed<strong>in</strong>-B-preferr<strong>in</strong>gBBS receptor (289). Thomas et al. (286)demonstrated that potent BLP antagonists, BIM 26182 <strong>and</strong>BIM 26189, <strong>in</strong>hibited <strong>the</strong> proliferation <strong>of</strong> SCLC 41 cells, whichexpress GRP receptor <strong>and</strong> prepro-GRP. Fur<strong>the</strong>rmore, <strong>the</strong>seBIM compounds <strong>in</strong>hibited growth <strong>of</strong> SCLC 41 <strong>and</strong> SCLC 75tumor growth <strong>in</strong> vivo. However, <strong>the</strong>se compounds had noeffect on two o<strong>the</strong>r SCLC cell l<strong>in</strong>es, SCLC 6 <strong>and</strong> SCLC 74R,which do not express GLP receptor. Cuttitta et al. (287) noted<strong>in</strong>hibition <strong>of</strong> SCLC xenografts <strong>in</strong> athymic nude mice us<strong>in</strong>g anantibody that b<strong>in</strong>ds to <strong>the</strong> C term<strong>in</strong>al <strong>of</strong> BLPs (<strong>in</strong>clud<strong>in</strong>gGRP). Antibody adm<strong>in</strong>istration given three times daily for4 wk resulted <strong>in</strong> a greater than 90% <strong>in</strong>hibition <strong>in</strong> tumorgrowth compared with control animals receiv<strong>in</strong>g nonspecificantibody. Phase I trials with <strong>the</strong> C-term<strong>in</strong>al b<strong>in</strong>d<strong>in</strong>g antibody(2A11) reported no toxicity; however, <strong>the</strong> cl<strong>in</strong>ical efficacy hasyet to be established (288).Recent studies (290, 291) have analyzed prepro-GRP expressionas a potential tumor marker to aid <strong>in</strong> <strong>the</strong> diagnosis<strong>of</strong> SCLC <strong>and</strong> demonstrate sensitivities <strong>of</strong> only 50–65%. Althoughexpression <strong>of</strong> prepro-GRP <strong>in</strong> SCLC cells may be useful<strong>in</strong> <strong>the</strong> determ<strong>in</strong>ation <strong>of</strong> <strong>the</strong> specific diagnosis, it is likelythat o<strong>the</strong>r markers, <strong>in</strong> comb<strong>in</strong>ation with GRP expression, willprovide more sensitive data. In addition to SCLC, Siegfriedet al. (292) demonstrated that GRP was produced <strong>in</strong> <strong>the</strong>bronchiolo-alveolar cancer cell l<strong>in</strong>e A549. GRP produced by<strong>the</strong>se cells was fur<strong>the</strong>r demonstrated to be trophic for asquamous carc<strong>in</strong>oma cell l<strong>in</strong>e <strong>in</strong> vitro, suggest<strong>in</strong>g that GRPmay be a potential stimulant <strong>of</strong> non-small cell lung carc<strong>in</strong>omaas it has been established for SCLC. These studiesprovide compell<strong>in</strong>g data to suggest that BLPs may play asignificant role as ei<strong>the</strong>r an autocr<strong>in</strong>e or paracr<strong>in</strong>e agent <strong>in</strong>SCLC, as well as non-SCLC. Therefore, BLP antagonists orantibodies may provide useful <strong>the</strong>rapy <strong>in</strong> <strong>the</strong>se patients.NT has been shown also to play a role <strong>in</strong> lung carc<strong>in</strong>omas.Most recently, Moody et al. (293) demonstrated that NT waspresent <strong>in</strong> measurable amounts (0.06–5.1 pmol/mg prote<strong>in</strong>)<strong>in</strong> half <strong>of</strong> <strong>the</strong> classical SCLC cell l<strong>in</strong>es. The effects <strong>of</strong> NTRantagonist, SR48692, were <strong>in</strong>vestigated <strong>in</strong> <strong>the</strong> lung cancer celll<strong>in</strong>es NCI-H209 <strong>and</strong> H345 (294). SR48692 <strong>in</strong>hibited NTmediatedCa 2 mobilization <strong>in</strong> NCI-H209 cells <strong>and</strong> c-fosmRNA <strong>in</strong>duction <strong>and</strong> proliferation <strong>of</strong> both cells <strong>in</strong> a dosedependentfashion. Fur<strong>the</strong>rmore, SR48692 <strong>in</strong>hibited <strong>in</strong> vivogrowth <strong>of</strong> NCI-H209 xenografts.3. Prostate cancer. Cancer <strong>of</strong> <strong>the</strong> prostate is <strong>the</strong> most commoncancer <strong>in</strong> men <strong>in</strong> <strong>the</strong> United States <strong>and</strong> <strong>the</strong> second lead<strong>in</strong>gDownloaded from edrv.endojournals.org by on July 16, 2007
Thomas et al. • <strong>Gastro<strong>in</strong>test<strong>in</strong>al</strong> <strong>Hormones</strong> <strong>and</strong> <strong>Proliferation</strong> Endocr<strong>in</strong>e Reviews, October 2003, 24(5):571–599 589cause <strong>of</strong> cancer deaths, account<strong>in</strong>g for 30% <strong>of</strong> new cancerdiagnoses <strong>in</strong> men (288). Prostate cancer progression can belimited with <strong>and</strong>rogen (testosterone) withdrawal; however,<strong>the</strong>re is <strong>in</strong>creas<strong>in</strong>g <strong>in</strong>terest <strong>in</strong> <strong>the</strong> effects <strong>of</strong> o<strong>the</strong>r hormoneson this disease.A subset <strong>of</strong> prostate cancers was noted to be <strong>in</strong>sensitiveto <strong>the</strong> effects <strong>of</strong> <strong>and</strong>rogen withdrawal (i.e., <strong>the</strong> removal <strong>of</strong>testosterone failed to promote tumor regression) (295–297).Interest<strong>in</strong>gly, clusters <strong>of</strong> neuroendocr<strong>in</strong>e cells were <strong>of</strong>tenfound <strong>in</strong> this subset <strong>of</strong> cancers. Sehgal et al. (296) demonstratedthat <strong>the</strong> <strong>and</strong>rogen-sensitive LNCap human prostatecancer cell l<strong>in</strong>e produced <strong>and</strong> secreted NT after <strong>and</strong>rogenwithdrawal. Fur<strong>the</strong>rmore, LNCap cells expressed a functionalNTR <strong>and</strong> were stimulated to proliferate with exogenousNT adm<strong>in</strong>istration after withdrawal <strong>of</strong> <strong>and</strong>rogen. Thesedata suggested that NT stimulates proliferation <strong>of</strong> prostatecancer cells dur<strong>in</strong>g conditions <strong>of</strong> prostate cancer <strong>and</strong>rogen<strong>in</strong>sensitivity, which provides support for <strong>the</strong> potential use <strong>of</strong>NTR antagonists as potential <strong>the</strong>rapy for a subset <strong>of</strong> prostatecancers that cont<strong>in</strong>ue to grow after <strong>and</strong>rogen withdrawal.Seethalakshmi et al. (297) noted similar effects us<strong>in</strong>g NT <strong>in</strong><strong>the</strong> <strong>and</strong>rogen-<strong>in</strong>sensitive PC3 prostate cancer cell l<strong>in</strong>e. Recently,Dal Farra et al. (298) noted expression <strong>of</strong> <strong>the</strong> NTRsubtype, NTR 3, uniformly <strong>in</strong> human prostate cancer cells.Transfection <strong>of</strong> <strong>the</strong> Ch<strong>in</strong>ese hamster ovary cells with NTRrendered <strong>the</strong>se cells sensitive to <strong>the</strong> growth-promot<strong>in</strong>g effects<strong>of</strong> NT. Therefore, extrapolation <strong>of</strong> <strong>the</strong>se results to prostatecancers suggests that NT, act<strong>in</strong>g through <strong>the</strong> NTR subtype,NTR 3, may be responsible for promot<strong>in</strong>g growth <strong>in</strong>prostate cancer cells. Block<strong>in</strong>g this receptor subtype providesano<strong>the</strong>r potential avenue for <strong>the</strong> adjuvant treatment <strong>of</strong> prostatecancers.Evidence suggests that BBS/GRP may affect prostatecancer growth. P<strong>in</strong>ski et al. (299) tested <strong>the</strong> effects <strong>of</strong> <strong>the</strong>somatostat<strong>in</strong> analog, RC-160, <strong>and</strong> <strong>the</strong> BBS/GRP antagonist,RC-3095, <strong>in</strong> Copenhagen rats bear<strong>in</strong>g <strong>the</strong> anaplastic,<strong>and</strong>rogen-<strong>in</strong>dependent Dunn<strong>in</strong>g R3327-AT-1 prostatic cancertumors. A significant reduction <strong>in</strong> tumor volumes <strong>and</strong>weights was noted with RC-160 (60 g/d for 332 d) as comparedwith control. RC-3095, at 100 g/d, reduced tumorvolume after 7 d, but after 18 d <strong>the</strong> <strong>in</strong>hibition was no longerapparent. Although <strong>the</strong> somatostat<strong>in</strong> <strong>in</strong>hibitor appeared tosuppress Dunn<strong>in</strong>g R3327-AT-1 cell growth <strong>in</strong> vivo, <strong>in</strong> vitrostudies failed to demonstrate a high-aff<strong>in</strong>ity receptor forsomatostat<strong>in</strong>, although <strong>the</strong> receptor for GRP was detected.Fur<strong>the</strong>rmore, only RC-3095 was capable <strong>of</strong> <strong>in</strong> vitro <strong>in</strong>hibition<strong>of</strong> R3327-AT-1 cells. These f<strong>in</strong>d<strong>in</strong>gs <strong>in</strong>dicated that BBS/GRPmay play a more direct role <strong>in</strong> prostate cancer proliferation.Consistent with <strong>the</strong>se results, Jungwirth et al. (300) demonstratedthat two new BBS/GRP antagonists, RC-3940-II <strong>and</strong>RC-3950-II, significantly decreased DU-145 xenograft tumorvolume when compared with control.4. Neuroblastomas. Neuroblastoma is <strong>the</strong> most common extracranialsolid malignancy <strong>of</strong> childhood <strong>and</strong> has a mortalityrate exceed<strong>in</strong>g 50%, particularly <strong>in</strong> older children (301). Thecl<strong>in</strong>ical behavior <strong>of</strong> neuroblastoma is varied <strong>and</strong> unpredictable<strong>and</strong> can range from spontaneous tumor regression, maturationfrom a malignant to a benign lesion or progression(302, 303). This unpredictable feature <strong>of</strong> neuroblastoma suggeststhat malignant transformation <strong>of</strong> cells may result, <strong>in</strong>part, from a failure to respond to normal signals regulat<strong>in</strong>gdifferentiation <strong>and</strong> proliferation. The GI hormones that havebeen most closely associated with effects on neuroblastomagrowth are somatostat<strong>in</strong> <strong>and</strong> GRP.Borgstrom et al. (304) demonstrated that somatostat<strong>in</strong>treatment <strong>in</strong>hibited <strong>the</strong> growth <strong>of</strong> <strong>the</strong> somatostat<strong>in</strong> receptorpositivehuman neuroblastoma cell l<strong>in</strong>e SH-SY5Y whenimplanted as xenografts <strong>in</strong> athymic nude rats. Moreover,Cattaneo et al. (305) demonstrated that <strong>the</strong> somatostat<strong>in</strong>analog lanreotide (BIM 23014) <strong>in</strong>hibited MAPK activity <strong>and</strong>platelet-derived growth factor-<strong>in</strong>duced Ras prote<strong>in</strong> activation<strong>in</strong> SY5Y neuroblastoma cells. The <strong>in</strong>hibition <strong>of</strong> bothMAPK <strong>and</strong> Ras has been implicated <strong>in</strong> <strong>the</strong> <strong>in</strong>hibition <strong>of</strong>tumor cell proliferation <strong>and</strong> provides strong evidence thatsomatostat<strong>in</strong> <strong>and</strong> its receptors can regulate neuroblastomagrowth. Most recently, two separate studies have shown that<strong>the</strong> absence <strong>of</strong> a functional somatostat<strong>in</strong> receptor, more specifically<strong>the</strong> subtype 2, was strongly correlated with a lessfavorable prognosis <strong>in</strong> patients with neuroblastomas (306,307). Therefore, detection <strong>of</strong> somatostat<strong>in</strong> receptors <strong>in</strong> neuroblastomasmay provide for an assessment <strong>of</strong> overall prognosis,as well as potentially provid<strong>in</strong>g a mechanism for <strong>in</strong>hibit<strong>in</strong>gneuroblastoma growth <strong>in</strong> patients with somatostat<strong>in</strong>receptor-positive tumors.Recent studies have implicated GRP <strong>and</strong> its receptor as apotential autocr<strong>in</strong>e or paracr<strong>in</strong>e factor <strong>in</strong> neuroblastoma cellgrowth. Sebesta et al. (308) assessed 19 resected neuroblastomaspecimens <strong>and</strong> identified expression <strong>of</strong> GRP <strong>and</strong> GRPreceptor mRNA <strong>in</strong> all 19. Kim et al. (309) assessed <strong>the</strong> immunosta<strong>in</strong><strong>in</strong>gpatterns <strong>of</strong> GRP <strong>and</strong> GRP receptor <strong>in</strong> a number<strong>of</strong> resected neuroblastoma specimens <strong>of</strong> vary<strong>in</strong>g grade.Immunohistochemical analysis <strong>of</strong> 33 paraff<strong>in</strong>-embeddedneuroblastomas from patients demonstrated an <strong>in</strong>creasedexpression <strong>of</strong> GRP receptor <strong>in</strong> a higher percentage <strong>of</strong> undifferentiatedtumors when compared with more benign <strong>and</strong>differentiated tissue. GRP receptor mRNA was detected <strong>in</strong><strong>the</strong> neuroblastoma cell l<strong>in</strong>es SK-N-SN, IMR-32, SN-SYSY,<strong>and</strong> LAN-1. Fur<strong>the</strong>rmore, GRP treatment was shown to mobilize[Ca 2 ] i <strong>in</strong> two neuroblastoma cell l<strong>in</strong>es <strong>and</strong>, more importantly,stimulated growth <strong>in</strong> all four cell l<strong>in</strong>es. These datademonstrate <strong>the</strong> synchronous relationship between GRP <strong>and</strong>GRP receptor <strong>in</strong> neuroblastomas, with expression <strong>of</strong> GRPreceptor correlat<strong>in</strong>g with more aggressive tumors. Additionally,<strong>the</strong> demonstration <strong>of</strong> <strong>in</strong>creased proliferation <strong>in</strong> neuroblastomacells <strong>in</strong> vitro after GRP treatment suggests that GRPmay act as an autocr<strong>in</strong>e <strong>and</strong>/or paracr<strong>in</strong>e growth factor forneuroblastomas.V. Future Perspectives <strong>and</strong> Therapeutic ImplicationsGI hormones have been used cl<strong>in</strong>ically as both diagnostic<strong>and</strong> <strong>the</strong>rapeutic agents. For example, adm<strong>in</strong>istration <strong>of</strong>CCK-8 can help establish <strong>the</strong> diagnosis <strong>of</strong> biliary colic, adm<strong>in</strong>istration<strong>of</strong> secret<strong>in</strong> has been useful <strong>in</strong> <strong>the</strong> diagnosis <strong>of</strong>equivocal patients with <strong>the</strong> Zoll<strong>in</strong>ger-Ellison syndrome, <strong>and</strong>adm<strong>in</strong>istration <strong>of</strong> gastr<strong>in</strong> has been useful to assess maximalacid output <strong>in</strong> patients <strong>in</strong> whom <strong>the</strong> diagnosis <strong>of</strong> Zoll<strong>in</strong>ger-Ellison syndrome is be<strong>in</strong>g considered (310). Somatostat<strong>in</strong> isDownloaded from edrv.endojournals.org by on July 16, 2007
590 Endocr<strong>in</strong>e Reviews, October 2003, 24(5):571–599 Thomas et al. • <strong>Gastro<strong>in</strong>test<strong>in</strong>al</strong> <strong>Hormones</strong> <strong>and</strong> <strong>Proliferation</strong><strong>the</strong> GI peptide that has been used most extensively. Somatostat<strong>in</strong>analogs have been used to decrease pancreatic <strong>and</strong>GI secretions associated with fistulas (311). In addition,somatostat<strong>in</strong> <strong>the</strong>rapy provides symptomatic relief fromhormone overproduction secondary to carc<strong>in</strong>oid tumorsor o<strong>the</strong>r endocr<strong>in</strong>e-produc<strong>in</strong>g tumors (312). Fur<strong>the</strong>rmore,octreotide radionucleotide scans provide useful diagnostictools to identify endocr<strong>in</strong>e tumors (158).GI hormones may have direct cl<strong>in</strong>ical applicability to diseases<strong>of</strong> <strong>the</strong> nonneoplastic GI tract <strong>and</strong> pancreas. Agents thatblock hormone receptors or hormone release may be usefulas a potential adjuvant <strong>the</strong>rapy <strong>in</strong> patients with GI malignancies.As more specific <strong>and</strong> longer-act<strong>in</strong>g agents are developed,it is anticipated that <strong>the</strong> use <strong>of</strong> GI hormones orantagonists, depend<strong>in</strong>g on <strong>the</strong> cl<strong>in</strong>ical scenario, may providenovel <strong>the</strong>rapies for various GI diseases.A. Nonneoplastic GI diseases1. Ulcer heal<strong>in</strong>g. The potential utility <strong>of</strong> GI hormones <strong>in</strong> certa<strong>in</strong><strong>in</strong>flammatory <strong>and</strong> atrophic diseases <strong>of</strong> <strong>the</strong> GI tract has beenpostulated on <strong>the</strong> basis <strong>of</strong> experimental animal models. Inpeptic ulcer disease, Schmassmann <strong>and</strong> Reubi (313) demonstrated<strong>in</strong>creased ulcer heal<strong>in</strong>g rates <strong>in</strong> <strong>the</strong> rat stomach us<strong>in</strong>ga potent CCK-B/gastr<strong>in</strong> receptor antagonist, YF-476, dur<strong>in</strong>g<strong>the</strong> early phase <strong>of</strong> ulcer heal<strong>in</strong>g (d 0–8), <strong>and</strong> us<strong>in</strong>g G-17 <strong>in</strong><strong>the</strong> later phases <strong>of</strong> heal<strong>in</strong>g. These results clearly demonstrate<strong>the</strong> improved wound-heal<strong>in</strong>g ability <strong>of</strong> <strong>in</strong>hibit<strong>in</strong>g gastr<strong>in</strong>b<strong>in</strong>d<strong>in</strong>g (dur<strong>in</strong>g <strong>the</strong> early phase) <strong>and</strong> <strong>the</strong>n modulat<strong>in</strong>g gastr<strong>in</strong>levels (<strong>in</strong> <strong>the</strong> later phase) to enhance heal<strong>in</strong>g rates forpeptic ulcer disease.2. Gut disuse or atrophy. The potential use <strong>of</strong> trophic agents hasreceived a considerable amount <strong>of</strong> attention <strong>in</strong> diseases <strong>of</strong> gutdisuse or atrophy. Trophic peptides that can ma<strong>in</strong>ta<strong>in</strong> oraugment GI mucosa dur<strong>in</strong>g periods <strong>of</strong> gut disuse <strong>in</strong>clude NT,BBS/GRP, <strong>and</strong> GLP-2 (33, 34, 42, 123, 149). In particular, <strong>the</strong>seagents may be <strong>of</strong> use <strong>in</strong> critically ill patients who are unableto take enteral nutrition, a situation that results <strong>in</strong> a pr<strong>of</strong>ound<strong>in</strong>test<strong>in</strong>al mucosal atrophy. Moreover, <strong>the</strong> use <strong>of</strong> GI hormonesmay be <strong>of</strong> potential utility <strong>in</strong> patients with short bowelsyndrome, a condition <strong>in</strong> which it would be important to<strong>in</strong>crease <strong>the</strong> adaptive mucosal hyperplasia so that <strong>the</strong>se patientsare able to survive without long-term parenteral nutrition.Cl<strong>in</strong>ical studies have shown a potential advantageus<strong>in</strong>g a comb<strong>in</strong>ation <strong>of</strong> glutam<strong>in</strong>e with GH, suggest<strong>in</strong>g thatthis may be a useful <strong>the</strong>rapy for patients with short bowelsyndrome (314). The use <strong>of</strong> GI hormones would <strong>of</strong>fer morespecific agents to selectively stimulate gut mucosal growth.In this regard, we have shown that NT can augment <strong>the</strong>adaptive hyperplasia associated with small bowel resection<strong>in</strong> rats (136). Consistent with our f<strong>in</strong>d<strong>in</strong>gs, o<strong>the</strong>rs have notedsimilar effects <strong>of</strong> NT on gut growth us<strong>in</strong>g various resectionmodels (137, 138, 315). Similar f<strong>in</strong>d<strong>in</strong>gs have been noted forGLP-2 <strong>and</strong>, <strong>in</strong> a limited cl<strong>in</strong>ical trial assess<strong>in</strong>g eight patientswith short bowel syndrome, patients were treated withGLP-2 for 35 d, which resulted <strong>in</strong> improved <strong>in</strong>test<strong>in</strong>al energyabsorption, decreased energy excretion, <strong>in</strong>creased bodyweight <strong>and</strong> lean body mass, decreased fat mass, <strong>and</strong> enhancedur<strong>in</strong>ary creat<strong>in</strong><strong>in</strong>e excretion (316). These results areencourag<strong>in</strong>g but are nei<strong>the</strong>r def<strong>in</strong>itive nor mechanisticallyunderstood. Confirmation <strong>of</strong> <strong>the</strong>se results with a larger prospective,r<strong>and</strong>omized trial is needed before any def<strong>in</strong>itiveconclusions can be made. However, it seems likely that GIhormones, such as GLP-2, NT, or BBS/GRP, alone or <strong>in</strong>comb<strong>in</strong>ation, may prove to be useful <strong>the</strong>rapy <strong>in</strong> patients withdiseases or conditions <strong>in</strong> which gut mucosal growth wouldbe advantageous.3. Inflammatory conditions. GI hormones may also provide aprotective effect for <strong>the</strong> GI mucosa dur<strong>in</strong>g periods <strong>of</strong> <strong>in</strong>flammation.For example, some chemo<strong>the</strong>rapeutic agents are associatedwith a severe enterocolitis, which can greatly limit<strong>the</strong> use <strong>of</strong> <strong>the</strong>se drugs. In experimental studies, Chu et al.(124) demonstrated that <strong>the</strong> adm<strong>in</strong>istration <strong>of</strong> BBS greatlyameliorated <strong>the</strong> effects <strong>of</strong> MTX on <strong>the</strong> <strong>in</strong>test<strong>in</strong>al mucosa <strong>and</strong><strong>in</strong>creased survival <strong>of</strong> rats given MTX. GLP-2 has likewisebeen shown to provide a protective effect for <strong>the</strong> GI mucosadur<strong>in</strong>g episodes <strong>of</strong> chemo<strong>the</strong>rapy-<strong>in</strong>duced enterocolitis(155). Cl<strong>in</strong>ical trials have yet to be performed to assess <strong>the</strong> use<strong>of</strong> GI hormones <strong>in</strong> this sett<strong>in</strong>g. However, given <strong>the</strong> experimentalresults, it appears clear that, <strong>in</strong> certa<strong>in</strong> sett<strong>in</strong>gs, adm<strong>in</strong>istration<strong>of</strong> GI hormones can provide a short-term protectiveeffect for <strong>the</strong> <strong>in</strong>test<strong>in</strong>al mucosa.B. GI cancersThe use <strong>of</strong> agents that block hormone receptors, as well as<strong>the</strong> antitrophic hormone somatostat<strong>in</strong>, have been assessed <strong>in</strong>limited cl<strong>in</strong>ical trials <strong>in</strong> cancer patients. In a recent phase I/IItrial by Smith et al. (317), gastr<strong>in</strong>-17-diph<strong>the</strong>ria toxoid (G17-DT; Gastrimmune), an immunogen capable <strong>of</strong> produc<strong>in</strong>ghigh-aff<strong>in</strong>ity neutraliz<strong>in</strong>g antibodies directed aga<strong>in</strong>st G-17,was assessed <strong>in</strong> 50 patients with advanced colorectal cancer.Eight percent <strong>of</strong> patients had measurable antibody formation,<strong>and</strong> no systemic side effects were noted (317). Theantibody levels were sufficient to compete with G-17 b<strong>in</strong>d<strong>in</strong>g<strong>and</strong> neutralize postpr<strong>and</strong>ial <strong>in</strong>creases <strong>in</strong> gastr<strong>in</strong>. One <strong>of</strong> <strong>the</strong>centers <strong>in</strong> this multicenter trial noted that two patients haddisease stabilization with adm<strong>in</strong>istration <strong>of</strong> G17-DT. Thesedata demonstrate that this agent is not toxic to humans <strong>and</strong>can produce <strong>in</strong>creased levels <strong>of</strong> gastr<strong>in</strong> antibody. However,its potential utility <strong>in</strong> patients with advanced colorectal cancerrema<strong>in</strong>s to be assessed <strong>in</strong> larger cl<strong>in</strong>ical trials. In ano<strong>the</strong>rstudy, Watson et al. (318) assessed <strong>the</strong> effect <strong>of</strong> G17-DT <strong>in</strong> <strong>the</strong>treatment <strong>of</strong> patients with gastric cancers. Limited data fromone center demonstrated tumor stabilization or response <strong>of</strong><strong>the</strong> disease to treatment <strong>in</strong> 80% <strong>of</strong> <strong>the</strong> patients treated withG17-DT (318). These studies provide evidence that agentsthat block gastr<strong>in</strong> may be <strong>of</strong> potential utility <strong>in</strong> patients withgastric cancers <strong>in</strong> whom surgical <strong>the</strong>rapy alone is usually notcurative.In ano<strong>the</strong>r study, Abbruzzese et al. (319) assessed <strong>the</strong> effects<strong>of</strong> a CCK receptor antagonist, MK-329, <strong>in</strong> 18 patientswith advanced pancreatic cancer. Unfortunately, this receptorantagonist had no effect on tumor progression or overallsurvival. However, <strong>the</strong>re was no <strong>in</strong>formation on <strong>the</strong> status <strong>of</strong>CCK receptors <strong>in</strong> <strong>the</strong> tumors <strong>of</strong> <strong>the</strong>se patients. In addition,<strong>the</strong>se patients had advanced disease <strong>in</strong> which o<strong>the</strong>r <strong>the</strong>rapieshad already been attempted. In a more recent prospective,Downloaded from edrv.endojournals.org by on July 16, 2007
Thomas et al. • <strong>Gastro<strong>in</strong>test<strong>in</strong>al</strong> <strong>Hormones</strong> <strong>and</strong> <strong>Proliferation</strong> Endocr<strong>in</strong>e Reviews, October 2003, 24(5):571–599 591double-bl<strong>in</strong>d study assess<strong>in</strong>g loxiglumide, a CCK-A receptorantagonist, <strong>in</strong> 64 pancreatic cancer patients, no appreciableeffect on survival or tumor size progression was noted (320).Once aga<strong>in</strong>, though, <strong>the</strong> status <strong>of</strong> CCK receptors <strong>in</strong> <strong>the</strong>secancers was not evaluated. With <strong>the</strong> production <strong>of</strong> morespecific <strong>and</strong> longer act<strong>in</strong>g antagonists, future cl<strong>in</strong>ical trialsshould be designed for pancreatic cancer patients with CCKreceptor-positive cancers. In this way, <strong>the</strong>rapy could be betterdesigned to <strong>the</strong> particular cancer. In addition, <strong>the</strong> use <strong>of</strong><strong>the</strong>se receptor antagonists may have more utility comb<strong>in</strong>edwith more conventional <strong>the</strong>rapeutic agents, much as tamoxifenis <strong>of</strong>ten used as part <strong>of</strong> a regimen for breast cancertreatment.Cl<strong>in</strong>ical trials have been performed to assess somatostat<strong>in</strong><strong>in</strong> <strong>the</strong> growth <strong>of</strong> various endocr<strong>in</strong>e <strong>and</strong> nonendocr<strong>in</strong>e cancers(321). The results have been equivocal. Somatostat<strong>in</strong> analogshave been used primarily for symptomatic control <strong>in</strong> patientswith advanced endocr<strong>in</strong>e tumors, usually with extensiveliver metastases. The reported effects <strong>of</strong> <strong>the</strong>se analogs ontumor regression have <strong>of</strong>ten been based on a small experience<strong>and</strong> usually rely on serial computed tomography orliver scan. Interpretation <strong>of</strong> an antiproliferative effect is fur<strong>the</strong>rcomplicated by <strong>the</strong> use <strong>of</strong> multiple <strong>the</strong>rapeutic <strong>in</strong>terventions,<strong>in</strong>clud<strong>in</strong>g chemo<strong>the</strong>rapy <strong>and</strong> embolization for endocr<strong>in</strong>etumors. Kraenzl<strong>in</strong> et al. (322) first reported thatoctreotide produced shr<strong>in</strong>kage <strong>of</strong> a hepatic metastasis <strong>in</strong> apatient with a VIPoma. In a later study with long-term follow-up<strong>in</strong> four patients with VIPomas, Williams et al. (323)could not demonstrate tumor regression us<strong>in</strong>g octreotide.Study<strong>in</strong>g <strong>the</strong> effects <strong>of</strong> octreotide <strong>in</strong> patients with endocr<strong>in</strong>etumors is fur<strong>the</strong>r complicated by <strong>the</strong> fact that <strong>the</strong>se tumorsare relatively rare <strong>and</strong> tumor growth is usually slow <strong>and</strong>unpredictable. Therefore, because <strong>the</strong>se tumors are so <strong>in</strong>frequent,this makes successful evaluation <strong>of</strong> <strong>the</strong> role <strong>of</strong> <strong>the</strong>seanalogs extraord<strong>in</strong>arily difficult.Somatostat<strong>in</strong> analogs have also been assessed for pancreatic<strong>and</strong> colorectal cancers (279, 324, 325). A prelim<strong>in</strong>ary trialfound that octreotide (500 g/d for 6 months) conferredsome survival advantage <strong>and</strong> improved quality <strong>of</strong> life <strong>in</strong> fourpatients with advanced pancreatic cancer (326). In ano<strong>the</strong>rstudy, Goldberg et al. (325) reported <strong>in</strong> a phase III r<strong>and</strong>omized,double-bl<strong>in</strong>d study <strong>of</strong> 260 patients with colorectal cancerthat octreotide failed to reduce tumor progression <strong>and</strong>improve patient survival. With <strong>the</strong> syn<strong>the</strong>sis <strong>of</strong> more specific<strong>and</strong> longer act<strong>in</strong>g analogs, <strong>the</strong> utility <strong>of</strong> <strong>the</strong>se agents for solidtumors <strong>of</strong> <strong>the</strong> GI tract should be reassessed. In this regard,Szepeshazi et al. (279) recently described a novel compound,AN-238, which conta<strong>in</strong>s a cytostatic somatostat<strong>in</strong> analogl<strong>in</strong>ked to 2-pyrrol<strong>in</strong>odoxorubic<strong>in</strong>. This directed <strong>the</strong>rapy resulted<strong>in</strong> enhanced tumor <strong>in</strong>hibition <strong>of</strong> <strong>the</strong> human colorectalcancer cells HCT-15 <strong>and</strong> HT29. Taken toge<strong>the</strong>r, <strong>the</strong>se datashow that somatostat<strong>in</strong>-targeted <strong>the</strong>rapies may providemore benefit compared with current somatostat<strong>in</strong> analogs. In<strong>the</strong> future, one can envision tailor<strong>in</strong>g <strong>the</strong>rapy for patientswith GI malignancies on <strong>the</strong> basis <strong>of</strong> <strong>the</strong> receptor status <strong>of</strong><strong>the</strong>se tumors. For example, patients with GI cancers thatpossess somatostat<strong>in</strong> receptors may be potential c<strong>and</strong>idatesto receive somatostat<strong>in</strong>-directed <strong>the</strong>rapy. Alternatively, patientswith GI cancers with CCK, gastr<strong>in</strong>, or NT receptorsmay be c<strong>and</strong>idates for agents that ei<strong>the</strong>r block <strong>the</strong> receptoror <strong>in</strong>hibit hormone release as a part <strong>of</strong> an overall cancerchemo<strong>the</strong>rapy regimen.AcknowledgmentsWe thank Liz Cook, Eileen Figueroa, <strong>and</strong> Karen Mart<strong>in</strong> for manuscriptpreparation.Address all correspondence <strong>and</strong> requests for repr<strong>in</strong>ts to: B. MarkEvers, M.D., Department <strong>of</strong> Surgery, The University <strong>of</strong> Texas MedicalBranch, 301 University Boulevard, Galveston, Texas 77555-0536. E-mail:mevers@utmb.eduResults from our laboratories were supported by National Institutes<strong>of</strong> Health Grants R01-DK58119 (to M.R.H.), P01-DK35608 <strong>and</strong> R01-DK48345 (to C.M.T.), <strong>and</strong> R37-AG10885 <strong>and</strong> T32-DK07639 (to B.M.E.).R.P.T. is <strong>the</strong> recipient <strong>of</strong> a Jeane B. Kempner Scholars Award.References1. Edk<strong>in</strong>s JS 1906 The chemical mechanism <strong>of</strong> gastric secretion.J Physiol 34:1332. Komarov SA 1938 Gastr<strong>in</strong>. Proc Soc Exp Biol Med 38:5143. Walsh JH 1994 <strong>Gastro<strong>in</strong>test<strong>in</strong>al</strong> hormones. In: Johnson LR, AlpersDH, Christensen J, Jacobson ED, Walsh JH, eds. Physiology <strong>of</strong> <strong>the</strong>gastro<strong>in</strong>test<strong>in</strong>al tract. 3rd ed. New York: Raven Press; 1–1284. Modl<strong>in</strong> IM, Tang LH 1993 A new look at an old hormone: gastr<strong>in</strong>.Trends Endocr<strong>in</strong>ol Metab 4:51–575. Gardner JD, Jensen RT 1990 <strong>Role</strong>s <strong>of</strong> receptors <strong>in</strong> expression <strong>of</strong>gastro<strong>in</strong>test<strong>in</strong>al hormone function. In: <strong>Gastro<strong>in</strong>test<strong>in</strong>al</strong> endocr<strong>in</strong>ology.Orl<strong>and</strong>o, FL: Academic Press Inc; 1–126. Larsson LI 1980 <strong>Gastro<strong>in</strong>test<strong>in</strong>al</strong> cells produc<strong>in</strong>g endocr<strong>in</strong>e, neurocr<strong>in</strong>e<strong>and</strong> paracr<strong>in</strong>e messengers. Cl<strong>in</strong> Gastroenterol 9:485–5167. Bardram L, Hilsted L, Rehfeld JF 1990 Progastr<strong>in</strong> expression <strong>in</strong>mammalian pancreas. Proc Natl Acad Sci USA 87:298–3028. Rehfeld JF 1988 The expression <strong>of</strong> progastr<strong>in</strong>, procholecystok<strong>in</strong><strong>in</strong><strong>and</strong> <strong>the</strong>ir hormonal products <strong>in</strong> pituitary cells. J Mol Endocr<strong>in</strong>ol1:87–949. Larsson L, Rehfeld JF 1979 A peptide resembl<strong>in</strong>g COOH-term<strong>in</strong>altetrapeptide amide <strong>of</strong> gastr<strong>in</strong> from a new gastro<strong>in</strong>test<strong>in</strong>al endocr<strong>in</strong>ecell type. Nature 277:575–57810. Walsh JH 1994 Gastr<strong>in</strong>. In: Walsh JH, Dockray GJ, eds. Gut peptides:biochemistry <strong>and</strong> physiology. New York: Raven Press;75–12111. Dick<strong>in</strong>son CJ 1996 Relationship <strong>of</strong> gastr<strong>in</strong> process<strong>in</strong>g to coloncancer. Gastroenterology 109:1384–138812. Ivy AC, Oldberg E 1928 A hormone mechanism for gallbladdercontraction <strong>and</strong> evacuation. Am J Physiol 76:599–61313. Harper AA, Raper HS 1943 Pancreozym<strong>in</strong>, a stimulant <strong>of</strong> secretion<strong>of</strong> pancreatic enzymes <strong>in</strong> extracts <strong>of</strong> <strong>the</strong> small <strong>in</strong>test<strong>in</strong>e. J Physiol102:115–12514. Mutt V, Jorpes JE 1968 Structure <strong>of</strong> porc<strong>in</strong>e cholecystok<strong>in</strong><strong>in</strong>pancreozym<strong>in</strong>.1. Cleavage with thromb<strong>in</strong> <strong>and</strong> with tryps<strong>in</strong>. EurJ Biochem 6:156–16215. Buffa R, Solcia E, Go VLW 1976 Immunohistochemical identification<strong>of</strong> <strong>the</strong> cholecystok<strong>in</strong><strong>in</strong> cell <strong>in</strong> <strong>the</strong> <strong>in</strong>test<strong>in</strong>al mucosa. Gastroenterology70:528–53216. Larsson LI, Rehfeld JF 1978 Distribution <strong>of</strong> gastr<strong>in</strong> <strong>and</strong> CCK cells<strong>in</strong> <strong>the</strong> rat gastro<strong>in</strong>test<strong>in</strong>al tract. Evidence for <strong>the</strong> occurrence <strong>of</strong> threedist<strong>in</strong>ct cell types stor<strong>in</strong>g COOH-term<strong>in</strong>al gastr<strong>in</strong> immunoreactivity.Histochemistry 58:23–3117. Polak JM, Pearse AG, Grimelius L, Bloom SR 1975 Growthhormonerelease-<strong>in</strong>hibit<strong>in</strong>g hormone <strong>in</strong> gastro<strong>in</strong>test<strong>in</strong>al <strong>and</strong> pancreaticD cells. Lancet 1:1220–122218. Rehfeld JF 1978 Immunochemical studies on cholecystok<strong>in</strong><strong>in</strong>. II.Distribution <strong>and</strong> molecular heterogeneity <strong>in</strong> <strong>the</strong> central nervoussystem <strong>and</strong> small <strong>in</strong>test<strong>in</strong>e <strong>of</strong> man <strong>and</strong> hog. J Biol Chem 253:4022–403019. Buchan AMJ, Polak JM, Solcia E, Capella C, Hudson D, PearseAGE 1978 Electron immunohistochemical evidence for <strong>the</strong> human<strong>in</strong>test<strong>in</strong>al I cell as <strong>the</strong> source <strong>of</strong> CCK. Gut 19:403–40720. Rehfeld JF, Larsson LI, Goltermann NR, Schwartz TW, Holst JJ,Jensen SL, Morley JS 1980 Neural regulation <strong>of</strong> pancreatic hor-Downloaded from edrv.endojournals.org by on July 16, 2007
592 Endocr<strong>in</strong>e Reviews, October 2003, 24(5):571–599 Thomas et al. • <strong>Gastro<strong>in</strong>test<strong>in</strong>al</strong> <strong>Hormones</strong> <strong>and</strong> <strong>Proliferation</strong>mone secretion by <strong>the</strong> C-term<strong>in</strong>al tetrapeptide <strong>of</strong> CCK. Nature284:33–3821. Dockray GJ, Gregory RA, Tracy HJ, Zhu WY 1981 Transport <strong>of</strong>cholecystok<strong>in</strong><strong>in</strong>-octapeptide-like immunoreactivity toward <strong>the</strong> gut<strong>in</strong> afferent vagal fibres <strong>in</strong> cat <strong>and</strong> dog. J Physiol 314:501–51122. Rehfeld JF, Lundberg JM 1983 Cholecystok<strong>in</strong><strong>in</strong> <strong>in</strong> fel<strong>in</strong>e vagal <strong>and</strong>sciatic nerves: concentration, molecular form <strong>and</strong> transport velocity.Bra<strong>in</strong> Res 275:341–34723. Be<strong>in</strong>feld MC 1999 Biosyn<strong>the</strong>sis <strong>and</strong> process<strong>in</strong>g <strong>of</strong> gastro<strong>in</strong>test<strong>in</strong>alpeptide hormones. In: Greeley Jr GH, ed. <strong>Gastro<strong>in</strong>test<strong>in</strong>al</strong> endocr<strong>in</strong>ology.Totowa, NJ: Humana Press; 33–6324. Guo Y-S, Townsend Jr CM 1999 <strong>Gastro<strong>in</strong>test<strong>in</strong>al</strong> hormones <strong>and</strong>gastro<strong>in</strong>test<strong>in</strong>al cancer growth. In: Greeley Jr GH, ed. <strong>Gastro<strong>in</strong>test<strong>in</strong>al</strong>endocr<strong>in</strong>ology. Totowa, NJ: Humana Press Inc.; 189–21425. Varner AA, Modl<strong>in</strong> IM, Walsh JH 1981 High potency <strong>of</strong> bombes<strong>in</strong>for stimulation <strong>of</strong> human gastr<strong>in</strong> release <strong>and</strong> gastric acid secretion.Regul Pept 1:289–29626. Hirschowitz BI, Mol<strong>in</strong>a E 1983 Relation <strong>of</strong> gastric acid <strong>and</strong> peps<strong>in</strong>secretion to serum gastr<strong>in</strong> levels <strong>in</strong> dogs given bombes<strong>in</strong> <strong>and</strong> gastr<strong>in</strong>-17.Am J Physiol 244:G546–G55127. Greeley Jr GH, Newman J 1987 Enteric bombes<strong>in</strong>-like peptides. In:Thompson JC, Greeley Jr GH, Rayford PL, Townsend Jr CM, eds.<strong>Gastro<strong>in</strong>test<strong>in</strong>al</strong> endocr<strong>in</strong>ology. New York: McGraw-Hill Book Co.;322–32928. Moran TH, Moody TW, Hostetler AM, Rob<strong>in</strong>son PH, Goldrich M,McHugh PR 1988 Distribution <strong>of</strong> bombes<strong>in</strong> b<strong>in</strong>d<strong>in</strong>g sites <strong>in</strong> <strong>the</strong> ratgastro<strong>in</strong>test<strong>in</strong>al tract. Peptides 9:643–64929. Dockray GJ, Vaillant C, Walsh JH 1979 The neuronal orig<strong>in</strong> <strong>of</strong>bombes<strong>in</strong>-like immunoreactivity <strong>in</strong> <strong>the</strong> rat gastro<strong>in</strong>test<strong>in</strong>al tract.Neuroscience 4:1561–156830. Mantyh PW, Catton MD, Boehmer CG, Welton ML, Passaro Jr EP,Maggio JE, Vigna SR 1989 Receptors for sensory neuropeptides <strong>in</strong>human <strong>in</strong>flammatory diseases: implications for <strong>the</strong> effector role <strong>of</strong>sensory neurons. Peptides 10:627–64531. Evans GS 1989 The distribution <strong>of</strong> endocr<strong>in</strong>e cells along <strong>the</strong> mousesmall <strong>in</strong>test<strong>in</strong>e. Bombes<strong>in</strong> <strong>and</strong> somatostat<strong>in</strong> produc<strong>in</strong>g cells. VirchowsArch B Cell Pathol Incl Mol Pathol 58:165–17232. Carraway R, Leeman SE 1975 The am<strong>in</strong>o acid sequence <strong>of</strong> a hypothalamicpeptide, neurotens<strong>in</strong>. J Biol Chem 250:1907–191133. Evers BM, Izukura M, Townsend Jr CM, Uchida T, Thompson JC1990 Differential effects <strong>of</strong> gut hormones on pancreatic <strong>and</strong> <strong>in</strong>test<strong>in</strong>algrowth dur<strong>in</strong>g adm<strong>in</strong>istration <strong>of</strong> an elemental diet. Ann Surg211:630–63834. Evers BM, Izukura M, Townsend Jr CM, Uchida T, Thompson JC1992 Neurotens<strong>in</strong> prevents <strong>in</strong>test<strong>in</strong>al mucosal hypoplasia <strong>in</strong> ratsfed an elemental diet. Dig Dis Sci 37:426–43135. Re<strong>in</strong>ecke M 1985 Neurotens<strong>in</strong>. Immunohistochemical localization<strong>in</strong> central <strong>and</strong> peripheral nervous system <strong>and</strong> <strong>in</strong> endocr<strong>in</strong>e cells <strong>and</strong>its functional role as neurotransmitter <strong>and</strong> endocr<strong>in</strong>e hormone.Prog Histochem Cytochem 16:1–17236. Ferris CF, Carraway RE, Hammer RA, Leeman SE 1985 Release<strong>and</strong> degradation <strong>of</strong> neurotens<strong>in</strong> dur<strong>in</strong>g perfusion <strong>of</strong> rat small <strong>in</strong>test<strong>in</strong>ewith lipid. Regul Pept 12:101–11137. Baca I, Feurle GE, Schwab A, Mittmann U, Knauf W, Lehnert T1982 Effect <strong>of</strong> neurotens<strong>in</strong> on exocr<strong>in</strong>e pancreatic secretion <strong>in</strong> dogs.Digestion 23:174–18338. Andersson S, Rosell S, Hjelmquist U, Chang D, Folkers K 1977Inhibition <strong>of</strong> gastric <strong>and</strong> <strong>in</strong>test<strong>in</strong>al motor activity <strong>in</strong> dogs by (Gln4)neurotens<strong>in</strong>. Acta Physiol Sc<strong>and</strong> 100:231–23539. Armstrong MJ, Parker MC, Ferris CF, Leeman SE 1986 Neurotens<strong>in</strong>stimulates [ 3 H]oleic acid translocation across rat small <strong>in</strong>test<strong>in</strong>e.Am J Physiol 251:G823–G82940. Feurle GE, Muller B, Rix E 1987 Neurotens<strong>in</strong> <strong>in</strong>duces hyperplasia<strong>of</strong> <strong>the</strong> pancreas <strong>and</strong> growth <strong>of</strong> <strong>the</strong> gastric antrum <strong>in</strong> rats. Gut28(Suppl):19–2341. Evers BM, Izukura M, Chung DH, Parekh D, Yosh<strong>in</strong>aga K, GreeleyJr GH, Uchida T, Townsend Jr CM, Thompson JC 1992 Neurotens<strong>in</strong>stimulates growth <strong>of</strong> colonic mucosa <strong>in</strong> young <strong>and</strong> agedrats. Gastroenterology 103:86–9142. Wood JG, Hoang HD, Bussjaeger LJ, Solomon TE 1988 Neurotens<strong>in</strong>stimulates growth <strong>of</strong> small <strong>in</strong>test<strong>in</strong>e <strong>in</strong> rats. Am J Physiol255:G813–G81743. Chung DH, Evers BM, Shimoda I, Townsend Jr CM, RajaramanS, Thompson JC 1992 Effect <strong>of</strong> neurotens<strong>in</strong> on gut mucosal growth<strong>in</strong> rats with jejunal <strong>and</strong> ileal Thiry-Vella fistulas. Gastroenterology103:1254–125944. Carraway RE, Mitra SP 1990 Differential process<strong>in</strong>g <strong>of</strong> neurotens<strong>in</strong>/neuromed<strong>in</strong>N precursor(s) <strong>in</strong> can<strong>in</strong>e bra<strong>in</strong> <strong>and</strong> <strong>in</strong>test<strong>in</strong>e. J BiolChem 265:8627–863145. Gill SS, Lee YC, Ghatei MA, Ghiglione M, Uttenthal LO, BloomSR 1984 The use <strong>of</strong> a rat isolated ileal preparation to <strong>in</strong>vestigate <strong>the</strong>release <strong>of</strong> neurotens<strong>in</strong>. Cl<strong>in</strong> Exp Pharmacol Physiol 11:457–46546. Holst Pedersen J, Knuthsen S, Bernabei M, Orskov C, Holst JJ1988 Secretion <strong>of</strong> neurotens<strong>in</strong> from isolated perfused porc<strong>in</strong>e ileum.Regul Pept 21:13–1947. Herrmann C, Cuber JC, Abello J, Dakka T, Bernard C, ChayvialleJA 1991 Release <strong>of</strong> ileal neurotens<strong>in</strong> <strong>in</strong> <strong>the</strong> rat by neurotransmitters<strong>and</strong> neuropeptides. Regul Pept 32:181–19248. Kras<strong>in</strong>ski SD, Wheeler MB, Leiter AB 1991 Isolation, characterization,<strong>and</strong> developmental expression <strong>of</strong> <strong>the</strong> rat peptide-YY gene.Mol Endocr<strong>in</strong>ol 5:433–44049. Kohri K, Nata K, Yonekura H, Nagai A, Konno K, Okamoto H1993 Clon<strong>in</strong>g <strong>and</strong> structural determ<strong>in</strong>ation <strong>of</strong> human peptide YYcDNA <strong>and</strong> gene. Biochim Biophys Acta 1173:345–34950. Tatemoto K, Mutt V 1980 Isolation <strong>of</strong> two novel c<strong>and</strong>idate hormonesus<strong>in</strong>g a chemical method for f<strong>in</strong>d<strong>in</strong>g naturally occurr<strong>in</strong>gpolypeptides. Nature 285:417–41851. Gomez G, Zhang T, Rajaraman S, Thakore KN, Yanaihara N,Townsend Jr CM, Thompson JC, Greeley GH 1995 Intest<strong>in</strong>alpeptide YY: ontogeny <strong>of</strong> gene expression <strong>in</strong> rat bowel <strong>and</strong> trophicactions on rat <strong>and</strong> mouse bowel. Am J Physiol 268:G71–G8152. Leiter AB, Toder A, Wolfe HJ, Taylor IL, Cooperman S, M<strong>and</strong>elG, Goodman RH 1987 Peptide YY. Structure <strong>of</strong> <strong>the</strong> precursor <strong>and</strong>expression <strong>in</strong> exocr<strong>in</strong>e pancreas. J Biol Chem 262:12984–1298853. M<strong>in</strong>th CD, Andrews PC, Dixon JE 1986 Characterization, sequence,<strong>and</strong> expression <strong>of</strong> <strong>the</strong> cloned human neuropeptide Y gene.J Biol Chem 261:11974–1197954. Gomez G, Udupi V, Greeley Jr GH 1999 Peptide YY. In: GreeleyJr GH, ed. <strong>Gastro<strong>in</strong>test<strong>in</strong>al</strong> endocr<strong>in</strong>ology. Totowa, NJ: HumanaPress; 551–57655. Drucker DJ 2002 Biological actions <strong>and</strong> <strong>the</strong>rapeutic potential <strong>of</strong> <strong>the</strong>glucagon-like peptides. Gastroenterology 122:531–54456. Sjolund K, S<strong>and</strong>en G, Hakanson R, Sundler F 1983 Endocr<strong>in</strong>e cells<strong>in</strong> human <strong>in</strong>test<strong>in</strong>e: an immunocytochemical study. Gastroenterology85:1120–113057. Brazeau P, Vale W, Burgus R, L<strong>in</strong>g N, Butcher M, Rivier J, Guillem<strong>in</strong>R 1973 Hypothalamic polypeptide that <strong>in</strong>hibits <strong>the</strong> secretion<strong>of</strong> immunoreactive pituitary growth hormone. Science 179:77–7958. Reis<strong>in</strong>e T 1995 Somatostat<strong>in</strong>. Cell Mol Neurobiol 15:597–61459. Orci L, Unger RH 1975 Functional subdivision <strong>of</strong> islets <strong>of</strong> Langerhans<strong>and</strong> possible role <strong>of</strong> D cells. Lancet 2:1243–124460. Evers BM 2001 Small bowel. In: Townsend Jr CM, Beauchamp RD,Evers BM, Mattox KL, eds. Sabiston textbook <strong>of</strong> surgery: <strong>the</strong> biologicalbasis <strong>of</strong> modern surgical practice. 16th ed. Philadelphia:W. B. Saunders Company; 873–91661. Rivard N, Guan D, Turkelson CM, Petitclerc D, Solomon TE,Morisset J 1991 Negative control by S<strong>and</strong>ostat<strong>in</strong> on pancreatic <strong>and</strong>duodenal growth: a possible implication <strong>of</strong> <strong>in</strong>sul<strong>in</strong>-like growthfactor I. Regul Pept 34:13–2362. Bass BL, Fischer BA, Richardson C, Harmon JW 1991 Somatostat<strong>in</strong>analogue treatment <strong>in</strong>hibits post-resectional adaptation <strong>of</strong> <strong>the</strong>small bowel <strong>in</strong> rats. Am J Surg 161:107–11263. Parekh D, Izukura M, Yosh<strong>in</strong>aga K, Townsend Jr CM, ThompsonJC 1990 Endogenous somatostat<strong>in</strong> is an antitrophic factor for <strong>the</strong>gut <strong>and</strong> pancreas. Digestion 46:8464. Upp Jr JR, Olson D, Poston GJ, Alex<strong>and</strong>er RW, Townsend Jr CM,Thompson JC 1988 Inhibition <strong>of</strong> growth <strong>of</strong> two human pancreaticadenocarc<strong>in</strong>omas <strong>in</strong> vivo by somatostat<strong>in</strong> analog SMS 201-995. Am JSurg 155:29–3565. S<strong>in</strong>gh P, Le S, Townsend Jr CM, Beauchamp RD, Laridjani A,Thompson JC 1986 A long act<strong>in</strong>g somatostat<strong>in</strong> analog (SRIF) (201-995) <strong>and</strong> proglumide (PGL) <strong>in</strong>hibit <strong>the</strong> trophic <strong>and</strong> gastr<strong>in</strong> receptor(GR) regulatory effects <strong>of</strong> pentagastr<strong>in</strong> (PG) on mouse colon cancer(MC-26) cells <strong>in</strong> vivo. Gastroenterology 90:163666. S<strong>in</strong>gh P, Owlia A, Varro A, Dai B, Rajaraman S, Wood T 1996Downloaded from edrv.endojournals.org by on July 16, 2007
Thomas et al. • <strong>Gastro<strong>in</strong>test<strong>in</strong>al</strong> <strong>Hormones</strong> <strong>and</strong> <strong>Proliferation</strong> Endocr<strong>in</strong>e Reviews, October 2003, 24(5):571–599 593Gastr<strong>in</strong> gene expression is required for <strong>the</strong> proliferation <strong>and</strong> tumorigenicity<strong>of</strong> human colon cancer cells. Cancer Res 56:4111–411567. di Paolo A, Bocci G, Innocenti F, Agen C, Nard<strong>in</strong>i D, Danesi R,del Tacca M 1995 Inhibitory effect <strong>of</strong> <strong>the</strong> somatostat<strong>in</strong> analogueSMS 201-995 <strong>and</strong> cytok<strong>in</strong>es on <strong>the</strong> proliferation <strong>of</strong> human colonadenocarc<strong>in</strong>oma cell l<strong>in</strong>es. Pharmacol Res 32:135–13968. Mar<strong>in</strong>issen MJ, Gutk<strong>in</strong>d JS 2001 G-prote<strong>in</strong>-coupled receptors <strong>and</strong>signal<strong>in</strong>g networks: emerg<strong>in</strong>g paradigms. Trends Pharmacol Sci22:368–37669. Wilkie TM 2001 Treasures throughout <strong>the</strong> life-cycle <strong>of</strong> G-prote<strong>in</strong>coupledreceptors. Trends Pharmacol Sci 22:396–39770. Benali N, Cordelier P, Calise D, Pages P, Rochaix P, Nagy A,Esteve JP, Pour PM, Schally AV, Vaysse N, Sus<strong>in</strong>i C, Buscail L2000 Inhibition <strong>of</strong> growth <strong>and</strong> metastatic progression <strong>of</strong> pancreaticcarc<strong>in</strong>oma <strong>in</strong> hamster after somatostat<strong>in</strong> receptor subtype 2 (sst2)gene expression <strong>and</strong> adm<strong>in</strong>istration <strong>of</strong> cytotoxic somatostat<strong>in</strong> analogAN-238. Proc Natl Acad Sci USA 97:9180–918571. Davis RJ 1995 Transcriptional regulation by MAP k<strong>in</strong>ases. MolReprod Dev 42:459–46772. Gutk<strong>in</strong>d JS 1998 The pathways connect<strong>in</strong>g G prote<strong>in</strong>-coupled receptorsto <strong>the</strong> nucleus through divergent mitogen-activated prote<strong>in</strong>k<strong>in</strong>ase cascades. J Biol Chem 273:1839–184273. Hordijk PL, Verlaan I, van Corven EJ, Moolenaar WH 1994 Prote<strong>in</strong>tyros<strong>in</strong>e phosphorylation <strong>in</strong>duced by lysophosphatidic acid <strong>in</strong>Rat-1 fibroblasts. Evidence that phosphorylation <strong>of</strong> MAP k<strong>in</strong>ase ismediated by <strong>the</strong> Gi-p21ras pathway. J Biol Chem 269:645–65174. van Biesen T, Hawes BE, Luttrell DK, Krueger KM, Touhara K,Porfiri E, Sakaue M, Luttrell LM, Lefkowitz RJ 1995 Receptortyros<strong>in</strong>e-k<strong>in</strong>ase-<strong>and</strong> G-mediated MAP k<strong>in</strong>ase activation by acommon signall<strong>in</strong>g pathway. Nature 376:781–78475. Ono K, Han J 2000 The p38 signal transduction pathway: activation<strong>and</strong> function. Cell Signal 12:1–1376. Yamauchi J, Nagao M, Kaziro Y, Itoh H 1997 Activation <strong>of</strong> p38mitogen-activated prote<strong>in</strong> k<strong>in</strong>ase by signal<strong>in</strong>g through G prote<strong>in</strong>coupledreceptors. Involvement <strong>of</strong> G <strong>and</strong> Gq/11 subunits.J Biol Chem 272:27771–2777777. Bence K, Ma W, Kozasa T, Huang XY 1997 Direct stimulation <strong>of</strong>Bruton’s tyros<strong>in</strong>e k<strong>in</strong>ase by G(q)-prote<strong>in</strong> -subunit. Nature 389:296–29978. Nagao M, Yamauchi J, Kaziro Y, Itoh H 1998 Involvement <strong>of</strong>prote<strong>in</strong> k<strong>in</strong>ase C <strong>and</strong> Src family tyros<strong>in</strong>e k<strong>in</strong>ase <strong>in</strong> Gq/11-<strong>in</strong>ducedactivation <strong>of</strong> c-Jun N-term<strong>in</strong>al k<strong>in</strong>ase <strong>and</strong> p38 mitogen-activatedprote<strong>in</strong> k<strong>in</strong>ase. J Biol Chem 273:22892–2289879. Kato Y, Tapp<strong>in</strong>g RI, Huang S, Watson MH, Ulevitch RJ, Lee JD1998 Bmk1/Erk5 is required for cell proliferation <strong>in</strong>duced by epidermalgrowth factor. Nature 395:713–71680. Mar<strong>in</strong>issen MJ, Chiariello M, Pallante M, Gutk<strong>in</strong>d JS 1999 Anetwork <strong>of</strong> mitogen-activated prote<strong>in</strong> k<strong>in</strong>ases l<strong>in</strong>ks G prote<strong>in</strong>coupledreceptors to <strong>the</strong> c-jun promoter: a role for c-Jun NH2-term<strong>in</strong>al k<strong>in</strong>ase, p38 s, <strong>and</strong> extracellular signal-regulated k<strong>in</strong>ase 5.Mol Cell Biol 19:4289–430181. Fukuhara S, Mar<strong>in</strong>issen MJ, Chiariello M, Gutk<strong>in</strong>d JS 2000 Signal<strong>in</strong>gfrom G prote<strong>in</strong>-coupled receptors to ERK5/Big MAPK 1<strong>in</strong>volves G q <strong>and</strong> G 12/13 families <strong>of</strong> heterotrimeric G prote<strong>in</strong>s.Evidence for <strong>the</strong> existence <strong>of</strong> a novel Ras AND Rho-<strong>in</strong>dependentpathway. J Biol Chem 275:21730–2173682. Mulholl<strong>and</strong> M 1997 Gastric anatomy <strong>and</strong> physiology. In: GreenfieldLJ, Mulholl<strong>and</strong> M, Oldham KT, Zelenock GB, Lillemoe KD,eds. Surgery: scientific pr<strong>in</strong>ciples <strong>and</strong> practice. 2nd ed. Philadelphia:Lipp<strong>in</strong>cott-Raven; 745–75883. Johnson LR, Aures D, Hakanson R 1969 Effect <strong>of</strong> gastr<strong>in</strong> on <strong>the</strong> <strong>in</strong>vivo <strong>in</strong>corporation <strong>of</strong> 14C-leuc<strong>in</strong>e <strong>in</strong>to prote<strong>in</strong> <strong>of</strong> <strong>the</strong> digestive tract.Proc Soc Exp Biol Med 132:996–99884. Crean GP, Marshall MW, Rumsey RD 1969 Parietal cell hyperplasia<strong>in</strong>duced by <strong>the</strong> adm<strong>in</strong>istration <strong>of</strong> pentagastr<strong>in</strong> (ICI 50,123) torats. Gastroenterology 57:147–15585. Johnson LR 1976 The trophic action <strong>of</strong> gastro<strong>in</strong>test<strong>in</strong>al hormones.Gastroenterology 70:278–28886. Wang TC, Koh TJ, Varro A, Cahill RJ, Dangler CA, Fox JG,Dockray GJ 1996 Process<strong>in</strong>g <strong>and</strong> proliferative effects <strong>of</strong> humanprogastr<strong>in</strong> <strong>in</strong> transgenic mice. J Cl<strong>in</strong> Invest 98:1918–192987. Wang TC, Dangler CA, Chen D, Goldenr<strong>in</strong>g JR, Koh T,Raychowdhury R, C<strong>of</strong>fey RJ, Ito S, Varro A, Dockray GJ, Fox JG2000 Synergistic <strong>in</strong>teraction between hypergastr<strong>in</strong>emia <strong>and</strong> Helicobacter<strong>in</strong>fection <strong>in</strong> a mouse model <strong>of</strong> gastric cancer. Gastroenterology118:36–4788. Upp Jr JR, Trudel JL, Townsend Jr CM, Alex<strong>and</strong>er RW,Rajaraman S, Nealon WH, Greeley Jr GH, Thompson JC 1988Establishment <strong>of</strong> a human gastr<strong>in</strong>oma <strong>in</strong> nude mice. Surgery 104:1037–104589. Friis-Hansen L, Sundler F, Li Y, Gillespie PJ, Saunders TL,Greenson JK, Owyang C, Rehfeld JF, Samuelson LC 1998 Impairedgastric acid secretion <strong>in</strong> gastr<strong>in</strong>-deficient mice. Am J Physiol274:G561–G56890. Nagata A, Ito M, Iwata N, Kuno J, Takano H, M<strong>in</strong>owa O, ChiharaK, Matsui T, Noda T 1996 G prote<strong>in</strong>-coupled cholecystok<strong>in</strong><strong>in</strong>-B/gastr<strong>in</strong> receptors are responsible for physiological cell growth <strong>of</strong><strong>the</strong> stomach mucosa <strong>in</strong> vivo. Proc Natl Acad Sci USA 93:11825–1183091. Schwartz MZ, Storozuk RB 1985 Enhancement <strong>of</strong> small <strong>in</strong>test<strong>in</strong>efunction by gastr<strong>in</strong>. J Surg Res 38:613–61792. Ekundayo AA, Lee CY, Goodlad RA 1995 Gastr<strong>in</strong> <strong>and</strong> <strong>the</strong> growth<strong>of</strong> <strong>the</strong> gastro<strong>in</strong>test<strong>in</strong>al tract. Gut 36:203–20893. Johnson LR 1977 New aspects <strong>of</strong> <strong>the</strong> trophic action <strong>of</strong> gastro<strong>in</strong>test<strong>in</strong>alhormones. Gastroenterology 72:788–79294. Häkanson R, Blom H, Carlsson E, Larsson H, Ryberg B, SundlerF 1986 Hypergastr<strong>in</strong>aemia produces trophic effects <strong>in</strong> stomach butnot <strong>in</strong> pancreas <strong>and</strong> <strong>in</strong>test<strong>in</strong>es. Regul Pept 13:225–23395. Chen D, Destree M, Hakanson R, Willems G 1998 Endogenoushypergastr<strong>in</strong>aemia does not promote growth <strong>of</strong> colonic mucosa or<strong>of</strong> a transplanted colon adenocarc<strong>in</strong>oma <strong>in</strong> rats. Eur J GastroenterolHepatol 10:293–29996. Koh TJ, Dockray GJ, Varro A, Cahill RJ, Dangler CA, Fox JG,Wang TC 1999 Overexpression <strong>of</strong> glyc<strong>in</strong>e-extended gastr<strong>in</strong> <strong>in</strong>transgenic mice results <strong>in</strong> <strong>in</strong>creased colonic proliferation. J Cl<strong>in</strong>Invest 103:1119–112697. Poston GJ, Saydjari R, Lawrence JP, Chung D, Townsend Jr CM,Thompson JC 1991 Ag<strong>in</strong>g <strong>and</strong> <strong>the</strong> trophic effects <strong>of</strong> cholecystok<strong>in</strong><strong>in</strong>,bombes<strong>in</strong> <strong>and</strong> pentagastr<strong>in</strong> on <strong>the</strong> rat pancreas. Pancreas6:407–41198. Todisco A, Takeuchi Y, Urumov A, Yamada J, Stepan VM,Yamada T 1997 Molecular mechanisms for <strong>the</strong> growth factor action<strong>of</strong> gastr<strong>in</strong>. Am J Physiol 273:G891–G89899. Chen D, Nyl<strong>and</strong>er AG, Norlen P, Hakanson R 1996 Gastr<strong>in</strong> doesnot stimulate growth <strong>of</strong> <strong>the</strong> rat pancreas. Sc<strong>and</strong> J Gastroenterol31:404–410100. Tarasova N 1999 Cellular <strong>and</strong> molecular targets <strong>of</strong> gastr<strong>in</strong>. In:Greeley Jr GH, ed. <strong>Gastro<strong>in</strong>test<strong>in</strong>al</strong> endocr<strong>in</strong>ology. Totowa, NJ:Humana Press; 101–123101. Brants F, Morisset J 1976 Tropic effect <strong>of</strong> cholecystok<strong>in</strong><strong>in</strong>-pancreozym<strong>in</strong>on pancreatic ac<strong>in</strong>ar cells from rats <strong>of</strong> different ages. ProcSoc Exp Biol Med 153:523–527102. Fölsch UR, W<strong>in</strong>ckler K, Wormsley KG 1978 Influence <strong>of</strong> repeatedadm<strong>in</strong>istration <strong>of</strong> cholecystok<strong>in</strong><strong>in</strong> <strong>and</strong> secret<strong>in</strong> on <strong>the</strong> pancreas <strong>of</strong><strong>the</strong> rat. Sc<strong>and</strong> J Gastroenterol 13:663–671103. Hughes CA, Bates T, Dowl<strong>in</strong>g RH 1978 Cholecystok<strong>in</strong><strong>in</strong> <strong>and</strong> secret<strong>in</strong>prevent <strong>the</strong> <strong>in</strong>test<strong>in</strong>al mucosal hypoplasia <strong>of</strong> total parenteralnutrition <strong>in</strong> <strong>the</strong> dog. Gastroenterology 75:34–41104. Weser E, Bell D, Tawil T 1981 Effects <strong>of</strong> octapeptide-cholecystok<strong>in</strong><strong>in</strong>,secret<strong>in</strong>, <strong>and</strong> glucagon on <strong>in</strong>test<strong>in</strong>al mucosal growth <strong>in</strong> parenterallynourished rats. Dig Dis Sci 26:409–416105. F<strong>in</strong>e H, Lev<strong>in</strong>e GM, Shiau YF 1983 Effects <strong>of</strong> cholecystok<strong>in</strong><strong>in</strong> <strong>and</strong>secret<strong>in</strong> on <strong>in</strong>test<strong>in</strong>al structure <strong>and</strong> function. Am J Physiol 245:G358–G363106. Stange EF, Schneider A, Seiffer E, Ditschuneit H 1986 Effect <strong>of</strong>pentagastr<strong>in</strong>, secret<strong>in</strong> <strong>and</strong> cholecystok<strong>in</strong><strong>in</strong> on growth <strong>and</strong> differentiation<strong>in</strong> organ cultured rabbit small <strong>in</strong>test<strong>in</strong>e. Horm Metab Res18:303–307107. Satake K, Mukai R, Kato Y, Umeyama K 1986 Effects <strong>of</strong> cerule<strong>in</strong>on <strong>the</strong> normal pancreas <strong>and</strong> on experimental pancreatic carc<strong>in</strong>oma<strong>in</strong> <strong>the</strong> Syrian golden hamster. Pancreas 1:246–253108. Petersen H, Solomon T, Grossman MI 1978 Effect <strong>of</strong> chronic pentagastr<strong>in</strong>,cholecystok<strong>in</strong><strong>in</strong>, <strong>and</strong> secret<strong>in</strong> on pancreas <strong>of</strong> rats. Am JPhysiol 234:E286–E293109. Solomon TE, Petersen H, Elash<strong>of</strong>f J, Grossman MI 1978 Interac-Downloaded from edrv.endojournals.org by on July 16, 2007
594 Endocr<strong>in</strong>e Reviews, October 2003, 24(5):571–599 Thomas et al. • <strong>Gastro<strong>in</strong>test<strong>in</strong>al</strong> <strong>Hormones</strong> <strong>and</strong> <strong>Proliferation</strong>tion <strong>of</strong> caerule<strong>in</strong> <strong>and</strong> secret<strong>in</strong> on pancreatic size <strong>and</strong> composition<strong>in</strong> rat. Am J Physiol 235:E714–E719110. Johnson FE, Hudd C, LaReg<strong>in</strong>a MC, Dev<strong>in</strong>e JE 1989 Effect <strong>of</strong>chronically adm<strong>in</strong>istered cholecystok<strong>in</strong><strong>in</strong> on <strong>the</strong> nude mouse.J Surg Res 46:177–183111. Trulsson LM, Svanvik J, Permert J, Gassl<strong>and</strong>er T 2001 Cholecystok<strong>in</strong><strong>in</strong>octapeptide <strong>in</strong>duces both proliferation <strong>and</strong> apoptosis <strong>in</strong> <strong>the</strong>rat pancreas. Regul Pept 98:41–48112. Nagy I, Takacs T, Mohacsi G 1997 One-year treatment withcholecystok<strong>in</strong><strong>in</strong>-octapeptide <strong>and</strong> secret<strong>in</strong>: effects on pancreatic trophism<strong>in</strong> <strong>the</strong> rat. Pharmacol Res 36:77–85113. Zucker KA, Adrian TE, Bilchik AJ, Modl<strong>in</strong> IM 1989 Effects <strong>of</strong> <strong>the</strong>CCK receptor antagonist L364,718 on pancreatic growth <strong>in</strong> adult<strong>and</strong> develop<strong>in</strong>g animals. Am J Physiol 257:G511–G516114. Niederau C, Liddle RA, Williams JA, Grendell JH 1987 Pancreaticgrowth: <strong>in</strong>teraction <strong>of</strong> exogenous cholecystok<strong>in</strong><strong>in</strong>, a protease <strong>in</strong>hibitor,<strong>and</strong> a cholecystok<strong>in</strong><strong>in</strong> receptor antagonist <strong>in</strong> mice. Gut28(Suppl):63–69115. Williams JA 2001 Intracellular signal<strong>in</strong>g mechanisms activated bycholecystok<strong>in</strong><strong>in</strong>-regulat<strong>in</strong>g syn<strong>the</strong>sis <strong>and</strong> secretion <strong>of</strong> digestive enzymes<strong>in</strong> pancreatic ac<strong>in</strong>ar cells. Annu Rev Physiol 63:77–97116. Bragado MJ, Groblewski GE, Williams JA 1997 p70s6k Is activatedby CCK <strong>in</strong> rat pancreatic ac<strong>in</strong>i. Am J Physiol 273:C101–C109117. Proud CG, Denton RM 1997 Molecular mechanisms for <strong>the</strong> control<strong>of</strong> translation by <strong>in</strong>sul<strong>in</strong>. Biochem J 328:329–341118. Bragado MJ, Groblewski GE, Williams JA 1998 Regulation <strong>of</strong>prote<strong>in</strong> syn<strong>the</strong>sis by cholecystok<strong>in</strong><strong>in</strong> <strong>in</strong> rat pancreatic ac<strong>in</strong>i <strong>in</strong>volvesPHAS-I <strong>and</strong> <strong>the</strong> p70 S6 k<strong>in</strong>ase pathway. Gastroenterology 115:733–742119. Puccio F, Lehy T 1989 Bombes<strong>in</strong> <strong>in</strong>gestion stimulates epi<strong>the</strong>lialdigestive cell proliferation <strong>in</strong> suckl<strong>in</strong>g rats. Am J Physiol 256:G328–G334120. Lehy T, Puccio F, Chariot J, Labeille D 1986 Stimulat<strong>in</strong>g effect <strong>of</strong>bombes<strong>in</strong> on <strong>the</strong> growth <strong>of</strong> gastro<strong>in</strong>test<strong>in</strong>al tract <strong>and</strong> pancreas <strong>in</strong>suckl<strong>in</strong>g rats. Gastroenterology 90:1942–1949121. Demb<strong>in</strong>ski A, Konturek PK, Konturek SJ 1990 <strong>Role</strong> <strong>of</strong> gastr<strong>in</strong> <strong>and</strong>cholecystok<strong>in</strong><strong>in</strong> <strong>in</strong> <strong>the</strong> growth-promot<strong>in</strong>g action <strong>of</strong> bombes<strong>in</strong> on <strong>the</strong>gastroduodenal mucosa <strong>and</strong> <strong>the</strong> pancreas. Regul Pept 27:343–354122. Demb<strong>in</strong>ski A, Warzecha Z, Konturek SJ, Banas M, Cai RZ,Schally AV 1991 The effect <strong>of</strong> antagonist <strong>of</strong> receptors for gastr<strong>in</strong>,cholecystok<strong>in</strong><strong>in</strong> <strong>and</strong> bombes<strong>in</strong> on growth <strong>of</strong> gastroduodenal mucosa<strong>and</strong> pancreas. J Physiol Pharmacol 42:263–277123. Chu KU, Higashide S, Evers BM, Ishizuka J, Townsend Jr CM,Thompson JC 1995 Bombes<strong>in</strong> stimulates mucosal growth <strong>in</strong> jejunal<strong>and</strong> ileal Thiry-Vella fistulas. Ann Surg 221:602–611124. Chu KU, Higashide S, Evers BM, Rajaraman S, Ishizuka J,Townsend Jr CM, Thompson JC 1994 Bombes<strong>in</strong> improves survivalfrom methotrexate-<strong>in</strong>duced enterocolitis. Ann Surg 220:570–577125. Zarzaur BL, Wu Y, Fukatsu K, Johnson CD, Kudsk KA 2002 Theneuropeptide bombes<strong>in</strong> improves IgA-mediated mucosal immunitywith preservation <strong>of</strong> gut <strong>in</strong>terleuk<strong>in</strong>-4 <strong>in</strong> total parenteral nutrition-fedmice. Surgery 131:59–65126. Johnson LR, Guthrie PD 1983 Regulation <strong>of</strong> antral gastr<strong>in</strong> content.Am J Physiol 245:G725–G729127. Chu KU, Evers BM, Ishizuka J, Townsend Jr CM, Thompson JC1995 <strong>Role</strong> <strong>of</strong> bombes<strong>in</strong> on gut mucosal growth. Ann Surg 222:94–100128. Upp Jr JR, Poston GJ, MacLellan DG, Townsend Jr CM, BarrancoSC, Thompson JC 1988 Mechanisms <strong>of</strong> <strong>the</strong> trophic actions <strong>of</strong> bombes<strong>in</strong>on <strong>the</strong> pancreas. Pancreas 3:193–198129. Lehy T, Puccio F 1990 Promot<strong>in</strong>g effect <strong>of</strong> bombes<strong>in</strong> on <strong>the</strong> cellproliferation <strong>in</strong> <strong>the</strong> rat endocr<strong>in</strong>e pancreas dur<strong>in</strong>g <strong>the</strong> early postnatalperiod. Regul Pept 27:87–96130. Liehr RM, Reidelberger RD, Rosewicz S, Bussjaeger LJ, SolomonTE 1992 Dose-related <strong>in</strong>volvement <strong>of</strong> CCK <strong>in</strong> bombes<strong>in</strong>-<strong>in</strong>ducedpancreatic growth. Regul Pept 38:207–219131. Fiorucci S, Bufalari A, Distrutti E, Lanfrancone L, Servoli A, SarpiL, Federici B, Bartoli A, Morelli A, Moggi L 1998 Bombes<strong>in</strong><strong>in</strong>ducedpancreatic regeneration <strong>in</strong> pigs is mediated by p46Shc/p52Shc <strong>and</strong> p42/p44 mitogen-activated prote<strong>in</strong> k<strong>in</strong>ase upregulation.Sc<strong>and</strong> J Gastroenterol 33:1310–1320132. Izukura M, Parekh D, Evers BM, Yosh<strong>in</strong>aga K, Greeley Jr GH,Townsend Jr CM, Thompson JC 1990 Neurotens<strong>in</strong> stimulates colongrowth <strong>in</strong> rats. Gastroenterology 98:A416133. Wood JG, Hoang HD, Bussjaeger LJ, Solomon TE 1988 Effect <strong>of</strong>neurotens<strong>in</strong> on pancreatic <strong>and</strong> gastric secretion <strong>and</strong> growth <strong>in</strong> rats.Pancreas 3:332–339134. Hoang HD, Wood JG, Bussjaeger LJ, Solomon TE 1988 Interaction<strong>of</strong> neurotens<strong>in</strong> with caerule<strong>in</strong> or secret<strong>in</strong> on digestive tract growth<strong>in</strong> rats. Regul Pept 22:275–284135. Vagianos C, Karatzas T, Scopa CD, Panagopoulos C, Tsoni I,Spiliopoulou I, Kalfarentzos F 1992 Neurotens<strong>in</strong> reduces microbialtranslocation <strong>and</strong> improves <strong>in</strong>test<strong>in</strong>al mucosa <strong>in</strong>tegrity afterabdom<strong>in</strong>al radiation. Eur Surg Res 24:77–83136. Izukura M, Evers BM, Parekh D, Yosh<strong>in</strong>aga K, Uchida T,Townsend Jr CM, Thompson JC 1992 Neurotens<strong>in</strong> augments <strong>in</strong>test<strong>in</strong>alregeneration after small bowel resection <strong>in</strong> rats. Ann Surg215:520–527137. de Miguel E, Gomez de Segura IA, Bonet H, Rodriguez MontesJA, Mata A 1994 Trophic effects <strong>of</strong> neurotens<strong>in</strong> <strong>in</strong> massive bowelresection <strong>in</strong> <strong>the</strong> rat. Dig Dis Sci 39:59–64138. Ryan CK, Miller JH, Seydel AS, Jensen KM, Sax HC 1997 Epidermalgrowth factor <strong>and</strong> neurotens<strong>in</strong> <strong>in</strong>duce microvillus hypertrophyfollow<strong>in</strong>g massive enterectomy. J Gastro<strong>in</strong>test Surg 1:467–473139. Mata A, Gomez de Segura IA, Largo C, Codesal J, De Miguel E1997 Neurotens<strong>in</strong> <strong>in</strong>creases <strong>in</strong>test<strong>in</strong>al adaptation <strong>and</strong> reduces enteroglucagon-likeimmunoreactivity after large bowel resection <strong>in</strong>rats. Eur J Surg 163:387–393140. Lundberg JM, Tatemoto K, Terenius L, Hellstrom PM, Mutt V,Hokfelt T, Hamberger B 1982 Localization <strong>of</strong> peptide YY (PYY) <strong>in</strong>gastro<strong>in</strong>test<strong>in</strong>al endocr<strong>in</strong>e cells <strong>and</strong> effects on <strong>in</strong>test<strong>in</strong>al blood flow<strong>and</strong> motility. Proc Natl Acad Sci USA 79:4471–4475141. Buell MG, Hard<strong>in</strong>g RK 1989 Effects <strong>of</strong> peptide YY on <strong>in</strong>test<strong>in</strong>alblood flow distribution <strong>and</strong> motility <strong>in</strong> <strong>the</strong> dog. Regul Pept 24:195–208142. Saria A, Beubler E 1985 Neuropeptide Y (NPY) <strong>and</strong> peptide YY(PYY) <strong>in</strong>hibit prostagl<strong>and</strong><strong>in</strong> E2-<strong>in</strong>duced <strong>in</strong>test<strong>in</strong>al fluid <strong>and</strong> electrolytesecretion <strong>in</strong> <strong>the</strong> rat jejunum <strong>in</strong> vivo. Eur J Pharmacol 119:47–52143. Gadbois DM, Crissman HA, Nastasi A, Habbersett R, Wang SK,Chen D, Lehnert BE 1996 Alterations <strong>in</strong> <strong>the</strong> progression <strong>of</strong> cellsthrough <strong>the</strong> cell cycle after exposure to particles or rays. RadiatRes 146:414–424144. Cox HM, Cuthbert AW, Hakanson R, Wahlestedt C 1988 The effect<strong>of</strong> neuropeptide Y <strong>and</strong> peptide YY on electrogenic ion transport <strong>in</strong>rat <strong>in</strong>test<strong>in</strong>al epi<strong>the</strong>lia. J Physiol 398:65–80145. Chance WT, Zhang X, Balasubramaniam A, Fischer JE 1996 Preservation<strong>of</strong> <strong>in</strong>test<strong>in</strong>e prote<strong>in</strong> by peptide YY dur<strong>in</strong>g total parenteralnutrition. Life Sci 58:1785–1794146. Guan D, Rivard N, Morisset J, Greeley Jr GH 1993 Effects <strong>of</strong>peptide YY on <strong>the</strong> growth <strong>of</strong> <strong>the</strong> pancreas <strong>and</strong> <strong>in</strong>test<strong>in</strong>e. Endocr<strong>in</strong>ology132:219–223147. Liu CD, H<strong>in</strong>es OJ, Whang EE, Laird EC, Skotzko MJ, Z<strong>in</strong>ner MJ,Ashley SW, McFadden DW 1995 Pancreatic peptide YY mRNAlevels <strong>in</strong>crease dur<strong>in</strong>g adaptation after small <strong>in</strong>test<strong>in</strong>al resection.J Surg Res 58:6–11148. Goodlad RA, Ghatei MA, Dom<strong>in</strong> J, Bloom SR, Wright NA 1990Is peptide YY trophic to <strong>the</strong> <strong>in</strong>test<strong>in</strong>al epi<strong>the</strong>lium <strong>of</strong> parenterally fedrats? Digestion 46(Suppl 2):177–181149. Drucker DJ, Erlich P, Asa SL, Brubaker PL 1996 Induction <strong>of</strong><strong>in</strong>test<strong>in</strong>al epi<strong>the</strong>lial proliferation by glucagon-like peptide 2. ProcNatl Acad Sci USA 93:7911–7916150. Brubaker PL, Lee YC, Drucker DJ 1992 Alterations <strong>in</strong> proglucagonprocess<strong>in</strong>g <strong>and</strong> <strong>in</strong>hibition <strong>of</strong> proglucagon gene expression <strong>in</strong> transgenicmice which conta<strong>in</strong> a chimeric proglucagon-SV40 T antigengene. J Biol Chem 267:20728–20733151. Ghatei MA, Goodlad RA, Taheri S, Taheri, S, M<strong>and</strong>ir N, BrynesAE, Jord<strong>in</strong>son M, Bloom SR 2001 Proglucagon-derived peptides <strong>in</strong><strong>in</strong>test<strong>in</strong>al epi<strong>the</strong>lial proliferation: glucagon-like peptide-2 is a majormediator <strong>of</strong> <strong>in</strong>test<strong>in</strong>al epi<strong>the</strong>lial proliferation <strong>in</strong> rats. Dig Dis Sci46:1255–1263152. Litvak DA, Hellmich MR, Evers BM, Banker NA, Townsend JrCM 1998 Glucagon-like peptide 2 is a potent growth factor for small<strong>in</strong>test<strong>in</strong>e <strong>and</strong> colon. J Gastro<strong>in</strong>test Surg 2:146–150Downloaded from edrv.endojournals.org by on July 16, 2007
Thomas et al. • <strong>Gastro<strong>in</strong>test<strong>in</strong>al</strong> <strong>Hormones</strong> <strong>and</strong> <strong>Proliferation</strong> Endocr<strong>in</strong>e Reviews, October 2003, 24(5):571–599 595153. Litvak DA, Evers BM, Hellmich MR, Townsend Jr CM 1999Enterotrophic effects <strong>of</strong> glucagon-like peptide 2 are enhanced byneurotens<strong>in</strong>. J Gastro<strong>in</strong>test Surg 3:432–440154. Boushey RP, Yusta B, Drucker DJ 1999 Glucagon-like peptide 2decreases mortality <strong>and</strong> reduces <strong>the</strong> severity <strong>of</strong> <strong>in</strong>domethac<strong>in</strong><strong>in</strong>ducedmur<strong>in</strong>e enteritis. Am J Physiol 277:E937–E947155. Boushey RP, Yusta B, Drucker DJ 2001 Glucagon-like peptide(GLP)-2 reduces chemo<strong>the</strong>rapy-associated mortality <strong>and</strong> enhancescell survival <strong>in</strong> cells express<strong>in</strong>g a transfected GLP-2 receptor. CancerRes 61:687–693156. Tavakkolizadeh A, Shen R, Abraham P, Kormi N, Seifert P,Edelman ER, Jacobs DO, Z<strong>in</strong>ner MJ, Ashley SW, Whang EE 2000Glucagon-like peptide 2: a new treatment for chemo<strong>the</strong>rapy<strong>in</strong>ducedenteritis. J Surg Res 91:77–82157. Drucker DJ, DeForest L, Brubaker PL 1997 Intest<strong>in</strong>al response togrowth factors adm<strong>in</strong>istered alone or <strong>in</strong> comb<strong>in</strong>ation with human[Gly2]glucagon-like peptide 2. Am J Physiol 273:G1252–G1262158. de Herder WW, Lamberts SW 2002 Somatostat<strong>in</strong> <strong>and</strong> somatostat<strong>in</strong>analogues: diagnostic <strong>and</strong> <strong>the</strong>rapeutic uses. Curr Op<strong>in</strong> Oncol 14:53–57159. Tulassay Z 1998 Somatostat<strong>in</strong> <strong>and</strong> <strong>the</strong> gastro<strong>in</strong>test<strong>in</strong>al tract. Sc<strong>and</strong>J Gastroenterol Suppl 228:115–121160. Pages P, Benali N, Sa<strong>in</strong>t-Laurent N, Esteve JP, Schally AV,Tkaczuk J, Vaysse N, Sus<strong>in</strong>i C, Buscail L 1999 sst2 Somatostat<strong>in</strong>receptor mediates cell cycle arrest <strong>and</strong> <strong>in</strong>duction <strong>of</strong> p27(Kip1).Evidence for <strong>the</strong> role <strong>of</strong> SHP-1. J Biol Chem 274:15186–15193161. Lopez F, Ferjoux G, Cordelier P, Sa<strong>in</strong>t-Laurent N, Esteve JP,Vaysse N, Buscail L, Sus<strong>in</strong>i C 2001 Neuronal nitric oxide synthase:a substrate for SHP-1 <strong>in</strong>volved <strong>in</strong> sst2 somatostat<strong>in</strong> receptor growth<strong>in</strong>hibitory signal<strong>in</strong>g. FASEB J 15:2300–2302162. Lehy T, Dubrasquet M, Bonfils S 1979 Effect <strong>of</strong> somatostat<strong>in</strong> onnormal <strong>and</strong> gastric-stimulated cell proliferation <strong>in</strong> <strong>the</strong> gastric <strong>and</strong><strong>in</strong>test<strong>in</strong>al mucosae <strong>of</strong> <strong>the</strong> rat. Digestion 19:99–109163. Thompson JS, Nguyen BL, Harty RF 1993 Somatostat<strong>in</strong> analogue<strong>in</strong>hibits <strong>in</strong>test<strong>in</strong>al regeneration. Arch Surg 128:385–389164. V<strong>and</strong>erho<strong>of</strong> JA, Kollman KA 1998 Lack <strong>of</strong> <strong>in</strong>hibitory effect <strong>of</strong>octreotide on <strong>in</strong>test<strong>in</strong>al adaptation <strong>in</strong> short bowel syndrome <strong>in</strong> <strong>the</strong>rat. J Pediatr Gastroenterol Nutr 26:241–244165. Beatson GT 1896 On <strong>the</strong> treatment <strong>of</strong> <strong>in</strong>operable cases <strong>of</strong> carc<strong>in</strong>oma<strong>of</strong> <strong>the</strong> mammal. Suggestions for a new method <strong>of</strong> treatment, withillustrative cases. Lancet 2:204–207166. Hugg<strong>in</strong>s CB, Hodges CV 1941 Studies on prostatic cancer. Part I:<strong>the</strong> effect <strong>of</strong> castration, <strong>of</strong> estrogen, <strong>and</strong> <strong>of</strong> <strong>and</strong>rogen <strong>in</strong>jection onserum phosphatases <strong>in</strong> metastatic carc<strong>in</strong>oma <strong>of</strong> <strong>the</strong> prostate. CancerRes 1:293–297167. Hugg<strong>in</strong>s C, Bergenstal DM 1952 Inhibition <strong>of</strong> human mammary<strong>and</strong> prostatic cancers by adrenalectomy. Cancer Res 12:134–141168. Jensen EV, Block GE, Smith S, Kyser K, DeSombre ER 1971Estrogen receptors <strong>and</strong> breast cancer response to adrenalectomy.Natl Cancer Inst Monogr 34:55–70169. Evers BM, Townsend Jr CM 1999 Growth factors, hormones <strong>and</strong>receptors <strong>in</strong> GI cancers. In: Evers BM, ed. Molecular mechanisms<strong>in</strong> gastro<strong>in</strong>test<strong>in</strong>al cancer. Aust<strong>in</strong>, TX: R. G. L<strong>and</strong>es Company; 1–19170. Cheung LY, Delcore R 2001 Stomach. In: Townsend Jr CM,Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston textbook <strong>of</strong>surgery: <strong>the</strong> biological basis <strong>of</strong> modern surgical practice. 16th ed.Philadelphia: W. B. Saunders Company; 837–872171. S<strong>in</strong>gh P, Rae-Venter B, Townsend Jr CM, Khalil T, Thompson JC1985 Gastr<strong>in</strong> receptors <strong>in</strong> normal <strong>and</strong> malignant gastro<strong>in</strong>test<strong>in</strong>almucosa: age-associated changes. Am J Physiol 249:G761–G769172. We<strong>in</strong>stock J, Baldw<strong>in</strong> GS 1988 B<strong>in</strong>d<strong>in</strong>g <strong>of</strong> gastr<strong>in</strong>(17) to humangastric carc<strong>in</strong>oma cell l<strong>in</strong>es. Cancer Res 48:932–937173. Henwood M, Clarke PA, Smith AM, Watson SA 2001 Expression<strong>of</strong> gastr<strong>in</strong> <strong>in</strong> develop<strong>in</strong>g gastric adenocarc<strong>in</strong>oma. Br J Surg 88:564–568174. Sumiyoshi H, Yasui W, Ochiai A, Tahara E 1984 Effects <strong>of</strong> gastr<strong>in</strong>on tumor growth <strong>and</strong> cyclic nucleotide metabolism <strong>in</strong> xenotransplantablehuman gastric <strong>and</strong> colonic carc<strong>in</strong>omas <strong>in</strong> nude mice.Cancer Res 44:4276–4280175. Watson SA, Durrant LG, Morris DL 1988 Growth-promot<strong>in</strong>g action<strong>of</strong> gastr<strong>in</strong> on human colonic <strong>and</strong> gastric tumour cells cultured<strong>in</strong> vitro. Br J Surg 75:342–345176. Kelly A, Holl<strong>and</strong>e F, Shulkes A, Baldw<strong>in</strong> GS 1998 Expression <strong>of</strong>progastr<strong>in</strong>-derived peptides <strong>and</strong> gastr<strong>in</strong> receptors <strong>in</strong> a panel <strong>of</strong>gastro<strong>in</strong>test<strong>in</strong>al carc<strong>in</strong>oma cell l<strong>in</strong>es. J Gastroenterol Hepatol 13:208–214177. Watson SA, Durrant LG, Crosbie JD, Morris DL 1989 The <strong>in</strong> vitrogrowth response <strong>of</strong> primary human colorectal <strong>and</strong> gastric cancercells to gastr<strong>in</strong>. Int J Cancer 43:692–696178. Baldw<strong>in</strong> GS 1995 The role <strong>of</strong> gastr<strong>in</strong> <strong>and</strong> cholecystok<strong>in</strong><strong>in</strong> <strong>in</strong> normal<strong>and</strong> neoplastic gastro<strong>in</strong>test<strong>in</strong>al growth. J Gastroenterol Hepatol10:215–232179. Tanaka J, Yamaguchi T, Takahashi T, Ogata N, B<strong>and</strong>o K, KoyamaK 1986 Regulatory effects <strong>of</strong> gastr<strong>in</strong> <strong>and</strong> secret<strong>in</strong> on carc<strong>in</strong>omas <strong>of</strong><strong>the</strong> stomach <strong>and</strong> colon. Tohoku J Exp Med 148:459–460180. Townsend Jr CM, S<strong>in</strong>gh P, Evers BM, Gomez G, Alex<strong>and</strong>er RW,Thompson JC 1990 Effect <strong>of</strong> gastro<strong>in</strong>test<strong>in</strong>al hormones on neoplasticgrowth. In: Thompson JC, Cooper CW, Greeley Jr GH,Rayford PL, S<strong>in</strong>gh P, Townsend Jr CM, eds. <strong>Gastro<strong>in</strong>test<strong>in</strong>al</strong> endocr<strong>in</strong>ology:receptors <strong>and</strong> post-receptor mechanisms. San Diego:Academic Press; 273–284181. Iwase K, Evers BM, Hellmich MR, Kim HJ, Higashide S, GullyD, Thompson JC, Townsend Jr CM 1997 Inhibition <strong>of</strong> neurotens<strong>in</strong><strong>in</strong>ducedpancreatic carc<strong>in</strong>oma growth by a nonpeptide neurotens<strong>in</strong>receptor antagonist, SR48692. Cancer 79:1787–1793182. Szabo I, Rumi G, Bodis B, Nemeth P, Mozsik G 2000 Gastr<strong>in</strong> <strong>and</strong>pentagastr<strong>in</strong> enhance <strong>the</strong> tumour proliferation <strong>of</strong> human stablecultured gastric adenocarc<strong>in</strong>oma cells. J Physiol Paris 94:71–74183. Tahara E, Haizuka S 1975 Effect <strong>of</strong> gastro-entero-pancreatic endocr<strong>in</strong>ehormones on <strong>the</strong> histogenesis <strong>of</strong> gastric cancer <strong>in</strong> rats<strong>in</strong>duced by N-methyl-N-nitro-N-nitrosoguanid<strong>in</strong>e; with specialreference to development <strong>of</strong> scirrhous gastric cancer. Gann 66:421–426184. Tasuta M, Iishi H, Baba M, Taniguchi H 1990 Enhancement byneurotens<strong>in</strong> <strong>of</strong> experimental carc<strong>in</strong>ogenesis <strong>in</strong>duced <strong>in</strong> rat colon byazoxymethane. Br J Cancer 62:368–371185. Hagiwara A, Takesada Y, Tanaka H, Tamano S, Hirose M, Ito N,Shirai T 2001 Dose-dependent <strong>in</strong>duction <strong>of</strong> gl<strong>and</strong>ular stomachpreneoplastic <strong>and</strong> neoplastic lesions <strong>in</strong> male F344 rats treated withcatechol chronically. Toxicol Pathol 29:180–186186. Konturek PC, Konturek SJ, Sulekova Z, Meixner H, Bielanski W,Starzynska T, Karczewska E, Marlicz K, Stachura J, Hahn EG 2001Expression <strong>of</strong> hepatocyte growth factor, transform<strong>in</strong>g growth factor, apoptosis related prote<strong>in</strong>s Bax <strong>and</strong> Bcl-2, <strong>and</strong> gastr<strong>in</strong> <strong>in</strong>human gastric cancer. Aliment Pharmacol Ther 15:989–999187. Watson SA, Gilliam AD 2001 G17DT–a new weapon <strong>in</strong> <strong>the</strong> <strong>the</strong>rapeuticarmoury for gastro<strong>in</strong>test<strong>in</strong>al malignancy. Expert Op<strong>in</strong> BiolTher 1:309–317188. Preston SR, Woodhouse LF, Gokhale J, Miller GV, Primrose JN1994 Characterization <strong>of</strong> a bombes<strong>in</strong>/gastr<strong>in</strong>-releas<strong>in</strong>g peptide receptoron a human gastric-cancer cell l<strong>in</strong>e. Int J Cancer 57:734–741189. Kim HJ, Evers BM, Guo Y, Banker NA, Hellmich MR, TownsendJr CM 1996 Bombes<strong>in</strong>-mediated AP-1 activation <strong>in</strong> a human gastriccancer (SIIA). Surgery 120:130–137190. Q<strong>in</strong> Y, Halmos G, Cai RZ, Szoke B, Ertl T, Schally AV 1994Bombes<strong>in</strong> antagonists <strong>in</strong>hibit <strong>in</strong> vitro <strong>and</strong> <strong>in</strong> vivo growth <strong>of</strong> humangastric cancer <strong>and</strong> b<strong>in</strong>d<strong>in</strong>g <strong>of</strong> bombes<strong>in</strong> to its receptors. J Cancer ResCl<strong>in</strong> Oncol 120:519–528191. P<strong>in</strong>ski J, Halmos G, Yano T, Szepeshazi K, Q<strong>in</strong> Y, Ertl T, SchallyAV 1994 Inhibition <strong>of</strong> growth <strong>of</strong> MKN45 human gastric-carc<strong>in</strong>omaxenografts <strong>in</strong> nude mice by treatment with bombes<strong>in</strong>/gastr<strong>in</strong>releas<strong>in</strong>g-peptideantagonist (RC-3095) <strong>and</strong> somatostat<strong>in</strong> analogueRC-160. Int J Cancer 57:574–580192. Preston SR, Woodhouse LF, Jones-Blackett S, Wyatt JI, PrimroseJN 1993 High aff<strong>in</strong>ity b<strong>in</strong>d<strong>in</strong>g sites for gastr<strong>in</strong> releas<strong>in</strong>g peptide onhuman gastric cancer <strong>and</strong> Menetrier’s mucosa. Cancer Res 53:5090–5092193. Carroll RE, Carroll R, Benya RV 1999 Characterization <strong>of</strong> gastr<strong>in</strong>releas<strong>in</strong>gpeptide receptors aberrantly expressed by non-antral gastricadenocarc<strong>in</strong>omas. Peptides 20:229–237194. Tatsuta M, Iishi H, Baba M, Taniguchi H 1989 Promotion byneurotens<strong>in</strong> <strong>of</strong> gastric carc<strong>in</strong>ogenesis <strong>in</strong>duced by N-methyl-Nnitro-N-nitrosoguanid<strong>in</strong>e<strong>in</strong> Wistar rats. Cancer Res 49:843–846195. Parker SL, Tong T, Bolden S, W<strong>in</strong>go PA 1997 Cancer statistics,1997. CA Cancer J Cl<strong>in</strong> 47:5–27196. Kaufmann R, Schafberg H, Rudr<strong>of</strong>f C, Henkle<strong>in</strong> P, Nowak G 1997Downloaded from edrv.endojournals.org by on July 16, 2007
596 Endocr<strong>in</strong>e Reviews, October 2003, 24(5):571–599 Thomas et al. • <strong>Gastro<strong>in</strong>test<strong>in</strong>al</strong> <strong>Hormones</strong> <strong>and</strong> <strong>Proliferation</strong>Cholecystok<strong>in</strong><strong>in</strong> B-type receptor signal<strong>in</strong>g is <strong>in</strong>volved <strong>in</strong> humanpancreatic cancer cell growth. Neuropeptides 31:573–583197. Swift IR, Smith JP 1994 Cholecystok<strong>in</strong><strong>in</strong> analog, JMV-180, stimulatesgrowth <strong>of</strong> human pancreatic cancer. Dig Dis Sci 39:1007–1013198. Heald EB, Kramer ST, Smith JP 1992 Trophic effects <strong>of</strong> unsulfatedcholecystok<strong>in</strong><strong>in</strong> on mouse pancreas <strong>and</strong> human pancreatic cancer.Pancreas 7:530–535199. Smith JP, Kramer ST, Solomon TE 1991 CCK stimulates growth<strong>of</strong> six human pancreatic cancer cell l<strong>in</strong>es <strong>in</strong> serum-free medium.Regul Pept 32:341–349200. Smith JP, Rickabaugh CA, McLaughl<strong>in</strong> PJ, Zagon IS 1993 Cholecystok<strong>in</strong><strong>in</strong>receptors <strong>and</strong> PANC-1 human pancreatic cancer cells.Am J Physiol 265:G149–G155201. Smith JP, Solomon TE, Bagheri S, Kramer S 1990 Cholecystok<strong>in</strong><strong>in</strong>stimulates growth <strong>of</strong> human pancreatic adenocarc<strong>in</strong>oma SW-1990.Dig Dis Sci 35:1377–1384202. Smith JP, Kramer S, Bagheri S 1990 Effects <strong>of</strong> a high-fat diet <strong>and</strong>L364,718 on growth <strong>of</strong> human pancreas cancer. Dig Dis Sci 35:726–732203. Frazier ML, Pathak S, Wang ZW, Cleary K, S<strong>in</strong>gletary SE, OliveM, Mackay B, Steck PA, Lev<strong>in</strong> B 1990 Establishment <strong>of</strong> a newhuman pancreatic adenocarc<strong>in</strong>oma cell l<strong>in</strong>e, MDAPanc-3. Pancreas5:8–16204. Townsend Jr CM, S<strong>in</strong>gh P, Thompson JC 1986 <strong>Gastro<strong>in</strong>test<strong>in</strong>al</strong>hormones <strong>and</strong> gastro<strong>in</strong>test<strong>in</strong>al <strong>and</strong> pancreatic carc<strong>in</strong>omas. Gastroenterology91:1002–1006205. S<strong>in</strong>gh P, Townsend Jr CM, Poston GJ, Reubi JC 1991 Specificb<strong>in</strong>d<strong>in</strong>g <strong>of</strong> cholecystok<strong>in</strong><strong>in</strong>, estradiol <strong>and</strong> somatostat<strong>in</strong> to humanpancreatic cancer xenografts. J Steroid Biochem Mol Biol 39:759–767206. Hirata M, Tsuchida A, Iwao T, Sasak T, Matsubara K, YamamotoS, Mor<strong>in</strong>aka K, Kawasaki Y, Fujimoto Y, Inoue H, Kariya K,Kajiyama G 1999 Cholecystok<strong>in</strong><strong>in</strong> regulates <strong>the</strong> <strong>in</strong>vasiveness <strong>of</strong>human pancreatic cancer cell l<strong>in</strong>es via prote<strong>in</strong> k<strong>in</strong>ase C pathway.Int J Oncol 14:1129–1135207. Upp Jr JR, S<strong>in</strong>gh P, Townsend Jr CM, Thompson JC 1987 Predict<strong>in</strong>gresponse to endocr<strong>in</strong>e <strong>the</strong>rapy <strong>in</strong> human pancreatic cancerwith cholecystok<strong>in</strong><strong>in</strong> receptors. Gastroenterology 92:1677208. Lhoste EF, Longnecker DS 1987 Effect <strong>of</strong> bombes<strong>in</strong> <strong>and</strong> caerule<strong>in</strong>on early stages <strong>of</strong> carc<strong>in</strong>ogenesis <strong>in</strong>duced by azaser<strong>in</strong>e <strong>in</strong> <strong>the</strong> ratpancreas. Cancer Res 47:3273–3277209. Townsend Jr CM, Frankl<strong>in</strong> RB, Watson LC, Glass EJ, ThompsonJC 1981 Stimulation <strong>of</strong> pancreatic cancer growth by caerule<strong>in</strong> <strong>and</strong>secret<strong>in</strong>. Surg Forum 32:228–229210. Seva C, Dick<strong>in</strong>son CJ, Yamada T 1994 Growth-promot<strong>in</strong>g effects<strong>of</strong> glyc<strong>in</strong>e-extended progastr<strong>in</strong>. Science 265:410–412211. Blackmore M, Hirst BH 1992 Autocr<strong>in</strong>e stimulation <strong>of</strong> growth <strong>of</strong>AR4–2J rat pancreatic tumour cells by gastr<strong>in</strong>. Br J Cancer 66:32–38212. Smith JP, Fantaskey AP, Liu G, Zagon IS 1995 Identification <strong>of</strong>gastr<strong>in</strong> as a growth peptide <strong>in</strong> human pancreatic cancer. Am JPhysiol 268:R135–R141213. Liehr RM, Melnykovych G, Solomon TE 1990 Growth effects <strong>of</strong>regulatory peptides on human pancreatic cancer l<strong>in</strong>es PANC-1 <strong>and</strong>MIA PaCa-2. Gastroenterology 98:1666–1674214. Lamers CB, Jansen JB, Woutersen RA 1990 Cholecystok<strong>in</strong><strong>in</strong> <strong>and</strong>gastro<strong>in</strong>test<strong>in</strong>al cancer. J Steroid Biochem Mol Biol 37:1069–1072215. Beardshall K, Frost G, Morarji Y, Dom<strong>in</strong> J, Bloom SR, Calam J1989 Saturation <strong>of</strong> fat <strong>and</strong> cholecystok<strong>in</strong><strong>in</strong> release: implications forpancreatic carc<strong>in</strong>ogenesis. Lancet 2:1008–1010216. Miazza BM, Widgren S, Chayvialle JA, Nicolet T, Loizeau E 1987Exocr<strong>in</strong>e pancreatic nodules after long-term pancreaticobiliary diversion<strong>in</strong> rats. An effect <strong>of</strong> raised CCK plasma concentrations. Gut28(Suppl):269–273217. McGu<strong>in</strong>ness EE, Morgan RG, Levison DA, Frape DL, HopwoodD, Wormsley KG 1980 The effects <strong>of</strong> long-term feed<strong>in</strong>g <strong>of</strong> soyaflour on <strong>the</strong> rat pancreas. Sc<strong>and</strong> J Gastroenterol 15:497–502218. McGu<strong>in</strong>ness EE, Morgan RG, Wormsley KG 1987 Fate <strong>of</strong> pancreaticnodules <strong>in</strong>duced by raw soya flour <strong>in</strong> rats. Gut 28(Suppl):207–212219. McGu<strong>in</strong>ness EE, Morgan RG, Wormsley KG 1984 Effects <strong>of</strong> soybeanflour on <strong>the</strong> pancreas <strong>of</strong> rats. Environ Health Perspect 56:205–212220. Watanapa P, Flaks B, Oztas H, Deprez PH, Calam J, WilliamsonRC 1993 Inhibitory effect <strong>of</strong> a cholecystok<strong>in</strong><strong>in</strong> antagonist on pancreaticcarc<strong>in</strong>ogenesis after pancreatobiliary diversion. Br J Cancer67:663–667221. Watanapa P, Flaks B, Oztas H, Deprez PH, Calam J, WilliamsonRC 1992 Duodenogastric reflux enhances growth <strong>and</strong> carc<strong>in</strong>ogenesis<strong>in</strong> <strong>the</strong> rat pancreas. Br J Surg 79:791–794222. Watanapa P, Flaks B, Oztas H, Deprez PH, Calam J, WilliamsonRC 1992 Enhanc<strong>in</strong>g effect <strong>of</strong> partial gastrectomy on pancreaticcarc<strong>in</strong>ogenesis. Br J Cancer 65:383–387223. Douglas BR, Woutersen RA, Jansen JB, de Jong AJ, Rovati LC,Lamers CB 1989 Influence <strong>of</strong> cholecystok<strong>in</strong><strong>in</strong> antagonist on <strong>the</strong>effects <strong>of</strong> cholecystok<strong>in</strong><strong>in</strong> <strong>and</strong> bombes<strong>in</strong> on azaser<strong>in</strong>e-<strong>in</strong>duced lesions<strong>in</strong> rat pancreas. Gastroenterology 96:462–469224. Douglas BR, Woutersen RA, Jansen JB, de Jong AJ, Rovati LC,Lamers CB 1989 Modulation by CR-1409 (lorglumide), a cholecystok<strong>in</strong><strong>in</strong>receptor antagonist, <strong>of</strong> tryps<strong>in</strong> <strong>in</strong>hibitor-enhanced growth<strong>of</strong> azaser<strong>in</strong>e-<strong>in</strong>duced putative preneoplastic lesions <strong>in</strong> rat pancreas.Cancer Res 49:2438–2441225. Povoski SP, Zhou W, Longnecker DS, Roebuck BD, Bell Jr RH1994 Growth <strong>of</strong> azaser<strong>in</strong>e-<strong>in</strong>duced putative preneoplastic nodules<strong>in</strong> <strong>the</strong> rat pancreas is mediated specifically by way <strong>of</strong> cholecystok<strong>in</strong><strong>in</strong>-Areceptors. Ann N Y Acad Sci 713:439–441226. Howatson AG, Carter DC 1985 Pancreatic carc<strong>in</strong>ogenesis-enhancementby cholecystok<strong>in</strong><strong>in</strong> <strong>in</strong> <strong>the</strong> hamster-nitrosam<strong>in</strong>e model. Br JCancer 51:107–114227. Johnson FE, LaReg<strong>in</strong>a MC, Mart<strong>in</strong> SA, Bashiti HM 1983 Cholecystok<strong>in</strong><strong>in</strong><strong>in</strong>hibits pancreatic <strong>and</strong> hepatic carc<strong>in</strong>ogenesis. CancerDetect Prev 6:389–402228. Meijers M, van Garderen-Hoetmer A, Lamers CB, Rovati LC,Jansen JB, Woutersen RA 1991 Effects <strong>of</strong> bombes<strong>in</strong> on <strong>the</strong> development<strong>of</strong> N-nitrosobis(2-oxopropyl)am<strong>in</strong>e-<strong>in</strong>duced pancreatic lesions<strong>in</strong> hamsters. Cancer Lett 59:45–50229. Szepeshazi K, Schally AV, Cai RZ, Radulovic S, Milovanovic S,Szoke B 1991 Inhibitory effect <strong>of</strong> bombes<strong>in</strong>/gastr<strong>in</strong>-releas<strong>in</strong>g peptideantagonist RC-3095 <strong>and</strong> high dose <strong>of</strong> somatostat<strong>in</strong> analogueRC-160 on nitrosam<strong>in</strong>e-<strong>in</strong>duced pancreatic cancers <strong>in</strong> hamsters.Cancer Res 51:5980–5986230. Szepeshazi K, Schally AV, Groot K, Halmos G 1993 Effect <strong>of</strong>bombes<strong>in</strong>, gastr<strong>in</strong>-releas<strong>in</strong>g peptide (GRP)(14–27) <strong>and</strong> bombes<strong>in</strong>/GRP receptor antagonist RC-3095 on growth <strong>of</strong> nitrosam<strong>in</strong>e<strong>in</strong>ducedpancreatic cancers <strong>in</strong> hamsters. Int J Cancer 54:282–289231. Meijer GA, Baak JP 1992 [Oncogenes, tumor suppressor genes <strong>and</strong><strong>the</strong> medical genetics <strong>of</strong> cancer]. Ned Tijdschr Geneeskd 136:1525–1526232. Damge C, Hajri A 1998 Effect <strong>of</strong> <strong>the</strong> gastr<strong>in</strong>-releas<strong>in</strong>g peptideantagonist BIM 26226 <strong>and</strong> lanreotide on an ac<strong>in</strong>ar pancreatic carc<strong>in</strong>oma.Eur J Pharmacol 347:77–86233. Burghardt B, Wenger C, Barabas K, Racz G, Olah A, Flautner L,Coy DH, Gress TM, Varga G 2001 GRP-receptor-mediated signaltransduction, gene expression <strong>and</strong> DNA syn<strong>the</strong>sis <strong>in</strong> <strong>the</strong> humanpancreatic adenocarc<strong>in</strong>oma cell l<strong>in</strong>e HPAF. Peptides 22:1119–1128234. Sumi S, Evers BM, Townsend Jr CM, Yosh<strong>in</strong>aga K, Uchida T,Murakami M, Sato K, Ishizuka J, Thompson JC 1993 Comparativeeffects <strong>of</strong> neurotens<strong>in</strong> <strong>and</strong> neuromed<strong>in</strong> N on growth <strong>of</strong> humanpancreatic cancer, MIA PaCa-2. Surg Oncol 2:267–272235. Reubi JC, Waser B, Friess H, Buchler M, Laissue J 1998 Neurotens<strong>in</strong>receptors: a new marker for human ductal pancreatic adenocarc<strong>in</strong>oma.Gut 42:546–550236. Ehlers RA, Kim S, Zhang Y, Ethridge RT, Murrilo C, HellmichMR, Evans DB, Townsend Jr CM, Evers BM 2000 Gut peptidereceptor expression <strong>in</strong> human pancreatic cancers. Ann Surg 231:838–848237. Ehlers RA, Zhang Y, Hellmich MR, Evers BM 2000 Neurotens<strong>in</strong>mediatedactivation <strong>of</strong> MAPK pathways <strong>and</strong> AP-1 b<strong>in</strong>d<strong>in</strong>g <strong>in</strong> <strong>the</strong>human pancreatic cancer cell l<strong>in</strong>e, MIA PaCa-2. Biochem BiophysRes Commun 269:704–708238. Ryder NM, Guha S, H<strong>in</strong>es OJ, Reber HA, Rozengurt E 2001 Gprote<strong>in</strong>-coupled receptor signal<strong>in</strong>g <strong>in</strong> human ductal pancreatic cancercells: neurotens<strong>in</strong> responsiveness <strong>and</strong> mitogenic stimulation.J Cell Physiol 186:53–64239. Guha S, Rey O, Rozengurt E 2002 Neurotens<strong>in</strong> <strong>in</strong>duces prote<strong>in</strong>k<strong>in</strong>ase C-dependent prote<strong>in</strong> k<strong>in</strong>ase D activation <strong>and</strong> DNA syn<strong>the</strong>-Downloaded from edrv.endojournals.org by on July 16, 2007
Thomas et al. • <strong>Gastro<strong>in</strong>test<strong>in</strong>al</strong> <strong>Hormones</strong> <strong>and</strong> <strong>Proliferation</strong> Endocr<strong>in</strong>e Reviews, October 2003, 24(5):571–599 597sis <strong>in</strong> human pancreatic carc<strong>in</strong>oma cell l<strong>in</strong>e PANC-1. Cancer Res62:1632–1640240. Liu CD, Balasubramaniam A, Saxton RE, Paiva M, McFaddenDW 1995 Human pancreatic cancer growth is <strong>in</strong>hibited by peptideYY <strong>and</strong> BIM-43004-1. J Surg Res 58:707–712241. Liu CD, Slice LW, Balasubramaniam A, Walsh JH, Newton TR,Saxton RE, McFadden DW 1995 Y2 receptors decrease humanpancreatic cancer growth <strong>and</strong> <strong>in</strong>tracellular cyclic adenos<strong>in</strong>e monophosphatelevels. Surgery 118:229–236242. Liu CD, Rongione AJ, Garvey L, Balasubramaniam A, McFaddenDW 1996 Adjuvant hormonal treatment with peptide YY or itsanalog decreases human pancreatic carc<strong>in</strong>oma growth. Am J Surg171:192–196243. Liu CD, Kwan D, Simon N, McFadden DW 2001 Syn<strong>the</strong>tic peptideYY analog b<strong>in</strong>ds to a cell membrane receptor <strong>and</strong> delivers fluorescentdye to pancreatic cancer cells. J Gastro<strong>in</strong>test Surg 5:147–152244. Rosenberg L 2001 Pancreatic cancer: does octreotide <strong>of</strong>fer anypromise? Chemo<strong>the</strong>rapy 47(Suppl 2):134–149245. Rosenberg L 2000 Pancreatic cancer: a review <strong>of</strong> emerg<strong>in</strong>g <strong>the</strong>rapies.Drugs 59:1071–1089246. Redd<strong>in</strong>g TW, Schally AV 1984 Inhibition <strong>of</strong> growth <strong>of</strong> pancreaticcarc<strong>in</strong>omas <strong>in</strong> animal models by analogs <strong>of</strong> hypothalamic hormones.Proc Natl Acad Sci USA 81:248–252247. Hierowski MT, Liebow C, du Sap<strong>in</strong> K, Schally AV 1985 Stimulationby somatostat<strong>in</strong> <strong>of</strong> dephosphorylation <strong>of</strong> membrane prote<strong>in</strong>s<strong>in</strong> pancreatic cancer MIA PaCa-2 cell l<strong>in</strong>e. FEBS Lett 179:252–256248. Liebow C, Reilly C, Serrano M, Schally AV 1989 Somatostat<strong>in</strong>analogues <strong>in</strong>hibit growth <strong>of</strong> pancreatic cancer by stimulat<strong>in</strong>g tyros<strong>in</strong>ephosphatase. Proc Natl Acad Sci USA 86:2003–2007249. Jemal A, Thomas A, Murray T, Thun M 2002 Cancer statistics,2002. CA Cancer J Cl<strong>in</strong> 52:23–47250. Beauchamp RD, Townsend Jr CM, S<strong>in</strong>gh P, Glass EJ, ThompsonJC 1985 Proglumide, a gastr<strong>in</strong> receptor antagonist, <strong>in</strong>hibits growth<strong>of</strong> colon cancer <strong>and</strong> enhances survival <strong>in</strong> mice. Ann Surg 202:303–309251. Ishizuka J, Townsend Jr CM, Bold RJ, Mart<strong>in</strong>ez J, Rodriguez M,Thompson JC 1994 Effects <strong>of</strong> gastr<strong>in</strong> on 3,5-cyclic adenos<strong>in</strong>emonophosphate, <strong>in</strong>tracellular calcium, <strong>and</strong> phosphatidyl<strong>in</strong>ositolhydrolysis <strong>in</strong> human colon cancer cells. Cancer Res 54:2129–2135252. Trudel JL, Upp Jr JR, Alex<strong>and</strong>er RW, Poston GJ, Townsend Jr CM,Thompson JC 1988 Enprostil <strong>in</strong>hibits <strong>the</strong> growth <strong>of</strong> a mouse coloncancer (MC-26) that possesses gastr<strong>in</strong> receptors. Gastroenterology94:A197253. Yactayo S, Patrice T, Foultier MT, Berrada A, Xu XN 1991 Effect<strong>of</strong> gastr<strong>in</strong> <strong>and</strong> enprostil, a PGE2 analog, on colonic cancerous cellgrowth. Gastroenterol Cl<strong>in</strong> Biol 15:519–524254. Upp Jr JR, S<strong>in</strong>gh P, Townsend Jr CM, Thompson JC 1989 Cl<strong>in</strong>icalsignificance <strong>of</strong> gastr<strong>in</strong> receptors <strong>in</strong> human colon cancers. CancerRes 49:488–492255. Hoose<strong>in</strong> NM, Kiener PA, Curry RC, Rovati LC, McGilbra DK,Bratta<strong>in</strong> MG 1988 Antiproliferative effects <strong>of</strong> gastr<strong>in</strong> receptor antagonists<strong>and</strong> antibodies to gastr<strong>in</strong> on human colon carc<strong>in</strong>oma celll<strong>in</strong>es. Cancer Res 48:7179–7183256. Hoose<strong>in</strong> NM, Kiener PA, Curry RC, Bratta<strong>in</strong> MG 1990 Evidencefor autocr<strong>in</strong>e growth stimulation <strong>of</strong> cultured colon tumor cells bya gastr<strong>in</strong>/cholecystok<strong>in</strong><strong>in</strong>-like peptide. Exp Cell Res 186:15–21257. Smith AM, Watson SA 2000 Gastr<strong>in</strong> <strong>and</strong> gastr<strong>in</strong> receptor activation:an early event <strong>in</strong> <strong>the</strong> adenoma-carc<strong>in</strong>oma sequence. Gut 47:820–824258. Schmitz F, Otte J-M, Stechele HU, Reimann B, Banasiewicz T,Fölsch UR, Schmidt W, Herzig K-H 2001 CCK-B/gastr<strong>in</strong> receptors<strong>in</strong> human colorectal cancer. [Erratum (2002) 32:69]. Eur J Cl<strong>in</strong> Invest31:812–820259. McGregor DB, Jones RD, Karl<strong>in</strong> DA, Romsdahl MM 1982 Trophiceffects <strong>of</strong> gastr<strong>in</strong> on colorectal neoplasms <strong>in</strong> <strong>the</strong> rat. Ann Surg195:219–223260. Oscarson JE, Veen HF, Ross JS, Malt RA 1982 Dimethylhydraz<strong>in</strong>e<strong>in</strong>ducedcolonic neoplasia: dissociation from endogenous gastr<strong>in</strong>levels. Surgery 91:525–530261. Kameyama M, Fukuda I, Imaoka S, Nakamori S, Iwanaga T 1993Level <strong>of</strong> serum gastr<strong>in</strong> as a predictor <strong>of</strong> liver metastasis fromcolorectal cancer. Dis Colon Rectum 36:497–500262. Thorburn CM, Friedman GD, Dick<strong>in</strong>son CJ, Vogelman JH,Orentreich N, Parsonnet J 1998 Gastr<strong>in</strong> <strong>and</strong> colorectal cancer: aprospective study. Gastroenterology 115:275–280263. Orbuch M, Venzon DJ, Lubensky IA, Weber HC, Gibril F, JensenRT 1996 Prolonged hypergastr<strong>in</strong>emia does not <strong>in</strong>crease <strong>the</strong> frequency<strong>of</strong> colonic neoplasia <strong>in</strong> patients with Zoll<strong>in</strong>ger-Ellison syndrome.Dig Dis Sci 41:604–613264. Mihas AA, Maliakkal RJ, Shueke M, Achord JL 1995 Serum gastr<strong>in</strong>levels <strong>in</strong> patients with colorectal cancer <strong>and</strong> adenomatouspolyps: a prospective study. Res Commun Mol Pathol Pharmacol90:301–304265. Fontanesi BV, Boris B, Delcio M, Manoukian FN 1997 Gastr<strong>in</strong>levels <strong>in</strong> patients with colorectal cancer. Hepatogastroenterology44:1082–1084266. Siddheshwar RK, Gray JC, Kelly SB 2001 Plasma levels <strong>of</strong> progastr<strong>in</strong>but not amidated gastr<strong>in</strong> or glyc<strong>in</strong>e extended gastr<strong>in</strong> areelevated <strong>in</strong> patients with colorectal carc<strong>in</strong>oma. Gut 48:47–52267. Stepan VM, Sawada M, Todisco A, Dick<strong>in</strong>son CJ 1999 Glyc<strong>in</strong>eextendedgastr<strong>in</strong> exerts growth-promot<strong>in</strong>g effects on human coloncancer cells. Mol Med 5:147–159268. Litvak DA, Hellmich MR, Iwase K, Evers BM, Mart<strong>in</strong>ez J, AmblardM, Townsend Jr CM 1999 JMV1155: a novel <strong>in</strong>hibitor <strong>of</strong>glyc<strong>in</strong>e-extended progastr<strong>in</strong>-mediated growth <strong>of</strong> a human coloncancer <strong>in</strong> vivo. Anticancer Res 19:45–49269. S<strong>in</strong>gh P, Velasco M, Given R, Wargovich M, Varro A, Wang TC2000 Mice overexpress<strong>in</strong>g progastr<strong>in</strong> are predisposed for develop<strong>in</strong>gaberrant colonic crypt foci <strong>in</strong> response to AOM. Am J PhysiolGastro<strong>in</strong>test Liver Physiol 278:G390–G399270. S<strong>in</strong>gh P, Velasco M, Given R, Varro A, Wang TC 2000 Progastr<strong>in</strong>expression predisposes mice to colon carc<strong>in</strong>omas <strong>and</strong> adenomas <strong>in</strong>response to a chemical carc<strong>in</strong>ogen. Gastroenterology 119:162–171271. Hellmich MR, Rui XL, Hellmich HL, Flem<strong>in</strong>g RY, Evers BM,Townsend Jr CM 2000 Human colorectal cancers express a constitutivelyactive cholecystok<strong>in</strong><strong>in</strong>-B/gastr<strong>in</strong> receptor that stimulatescell growth. J Biol Chem 275:32122–32128272. D<strong>in</strong>g WQ, Kuntz SM, Miller LJ 2002 A misspliced form <strong>of</strong> <strong>the</strong>cholecystok<strong>in</strong><strong>in</strong>-B/gastr<strong>in</strong> receptor <strong>in</strong> pancreatic carc<strong>in</strong>oma: role <strong>of</strong>reduced sellular U2AF35 <strong>and</strong> a suboptimal 3-splic<strong>in</strong>g site lead<strong>in</strong>gto retention <strong>of</strong> <strong>the</strong> fourth <strong>in</strong>tron. Cancer Res 62:947–952273. Yosh<strong>in</strong>aga K, Evers BM, Izukura M, Parekh D, Uchida T,Townsend Jr CM., Thompson JC 1992 Neurotens<strong>in</strong> stimulatesgrowth <strong>of</strong> colon cancer. Surg Oncol 1:127–134274. Evers BM, Zhou Z, Dohlen V, Rajaraman S, Thompson JC,Townsend Jr CM 1996 Fetal <strong>and</strong> neoplastic expression <strong>of</strong> <strong>the</strong> neurotens<strong>in</strong>gene <strong>in</strong> <strong>the</strong> human colon. Ann Surg 223:464–471275. Rovere C, Barbero P, Maoret JJ, Labur<strong>the</strong> M, Kitabgi P 1998Pro-neurotens<strong>in</strong>/neuromed<strong>in</strong> N expression <strong>and</strong> process<strong>in</strong>g <strong>in</strong> humancolon cancer cell l<strong>in</strong>es. Biochem Biophys Res Commun 246:155–159276. Ehlers 2nd RA, Bonnor RM, Wang X, Hellmich MR, Evers BM1998 Signal transduction mechanisms <strong>in</strong> neurotens<strong>in</strong>-mediated cellularregulation. Surgery 124:239–247277. Milhoan RA, Milhoan LH, Trudel JL, Lawrence JP, Townsend JrCM, Thompson JC 1988 Somatostat<strong>in</strong> <strong>and</strong> -difluoromethylornith<strong>in</strong>e(DFMO) have additive <strong>in</strong>hibitory effects on growth <strong>of</strong> humancolon carc<strong>in</strong>oma (HCC) <strong>in</strong> vivo. Biomed Res 9:30278. Melen-Mucha G, W<strong>in</strong>czyk K, Pawlikowski M 1998 Somatostat<strong>in</strong>analogue octreotide <strong>and</strong> melaton<strong>in</strong> <strong>in</strong>hibit bromodeoxyurid<strong>in</strong>e <strong>in</strong>corporation<strong>in</strong>to cell nuclei <strong>and</strong> enhance apoptosis <strong>in</strong> <strong>the</strong> transplantablemur<strong>in</strong>e colon 38 cancer. Anticancer Res 18:3615–3619279. Szepeshazi K, Schally AV, Halmos G, Armatis P, Hebert F, SunB, Feil A, Kiaris H, Nagy A 2002 Targeted cytotoxic somatostat<strong>in</strong>analogue AN-238 <strong>in</strong>hibits somatostat<strong>in</strong> receptor-positive experimentalcolon cancers <strong>in</strong>dependently <strong>of</strong> <strong>the</strong>ir p53 status. Cancer Res62:781–788280. Iglehart JD, Kael<strong>in</strong> CM 2001 Diseases <strong>of</strong> <strong>the</strong> breast. In: TownsendJr CM, Beauchamp RD, Evers BM, Mattox KL, eds. Sabiston textbook<strong>of</strong> surgery: <strong>the</strong> biological basis <strong>of</strong> modern surgical practice,16th ed. Philadelphia: W. B. Saunders Company; 555–590281. Goettler DM, Lev<strong>in</strong> L, Chey WY 1990 Postpr<strong>and</strong>ial levels <strong>of</strong> prolact<strong>in</strong><strong>and</strong> gut hormones <strong>in</strong> breast cancer patients: association withstage <strong>of</strong> disease, but not dietary fat. J Natl Cancer Inst 82:22–29282. Caniano DA, Starr J, G<strong>in</strong>n-Pease ME 1989 Extensive short-bowelsyndrome <strong>in</strong> neonates: outcome <strong>in</strong> <strong>the</strong> 1980s. Surgery 105:119–124Downloaded from edrv.endojournals.org by on July 16, 2007
598 Endocr<strong>in</strong>e Reviews, October 2003, 24(5):571–599 Thomas et al. • <strong>Gastro<strong>in</strong>test<strong>in</strong>al</strong> <strong>Hormones</strong> <strong>and</strong> <strong>Proliferation</strong>283. Nesl<strong>and</strong> JM, Holm R, Johannessen JV, Gould VE 1986 Neuronespecific enolase immunosta<strong>in</strong><strong>in</strong>g <strong>in</strong> <strong>the</strong> diagnosis <strong>of</strong> breast carc<strong>in</strong>omaswith neuroendocr<strong>in</strong>e differentiation. Its usefulness <strong>and</strong> limitations.J Pathol 148:35–43284. Reubi JC, Schaer JC, Waser B 1997 Cholecystok<strong>in</strong><strong>in</strong>(CCK)-A<strong>and</strong> CCK-B/gastr<strong>in</strong> receptors <strong>in</strong> human tumors. Cancer Res 57:1377–1386285. Bajo AM, Schally AV, Krupa M, Hebert F, Groot K, SzepeshaziK 2002 Bombes<strong>in</strong> antagonists <strong>in</strong>hibit growth <strong>of</strong> MDA-MB-435 estrogen-<strong>in</strong>dependentbreast cancers <strong>and</strong> decrease <strong>the</strong> expression <strong>of</strong><strong>the</strong> ErbB-2/HER-2 oncoprote<strong>in</strong> <strong>and</strong> c-jun <strong>and</strong> c-fos oncogenes. ProcNatl Acad Sci USA 99:3836–3841286. Thomas F, Arvelo F, Anto<strong>in</strong>e E, Jacrot M, Poupon MF 1992 Antitumoralactivity <strong>of</strong> bombes<strong>in</strong> analogues on small cell lung cancerxenografts: relationship with bombes<strong>in</strong> receptor expression. CancerRes 52:4872–4877287. Cuttitta F, Carney DN, Mulsh<strong>in</strong>e J, Moody TW, Fedorko J,Fischler A, M<strong>in</strong>na JD 1985 Bombes<strong>in</strong>-like peptides can function asautocr<strong>in</strong>e growth factors <strong>in</strong> human small-cell lung cancer. Nature316:823–826288. Chaudhry A, Carrasquillo JA, Avis IL, Shuke N, Reynolds JC,Bartholomew R, Larson SM, Cuttitta F, Johnson BE, Mulsh<strong>in</strong>e JL1999 Phase I <strong>and</strong> imag<strong>in</strong>g trial <strong>of</strong> a monoclonal antibody directedaga<strong>in</strong>st gastr<strong>in</strong>-releas<strong>in</strong>g peptide <strong>in</strong> patients with lung cancer. Cl<strong>in</strong>Cancer Res 5:3385–3393289. Giladi E, Nagalla SR, Sp<strong>in</strong>del ER 1993 Molecular clon<strong>in</strong>g <strong>and</strong>characterization <strong>of</strong> receptors for <strong>the</strong> mammalian bombes<strong>in</strong>-likepeptides. J Mol Neurosci 4:41–54290. Lacroix J, Becker HD, Woerner SM, Rittgen W, Dr<strong>in</strong>gs P, vonKnebel Doeberitz M 2001 Sensitive detection <strong>of</strong> rare cancer cells<strong>in</strong> sputum <strong>and</strong> peripheral blood samples <strong>of</strong> patients with lungcancer by preproGRP-specific RT-PCR. Int J Cancer 92:1–8291. Shibayama T, Ueoka H, Nishii K, Kiura K, Tabata M, MiyatakeK, Kitajima T, Harada M 2001 Complementary roles <strong>of</strong> progastr<strong>in</strong>-releas<strong>in</strong>gpeptide (ProGRP) <strong>and</strong> neuron specific enolase(NSE) <strong>in</strong> diagnosis <strong>and</strong> prognosis <strong>of</strong> small-cell lung cancer (SCLC).Lung Cancer 32:61–69292. Siegfried JM, Han YH, DeMichele MA, Hunt JD, Gai<strong>the</strong>r AL,Cuttitta F 1994 Production <strong>of</strong> gastr<strong>in</strong>-releas<strong>in</strong>g peptide by a nonsmallcell lung carc<strong>in</strong>oma cell l<strong>in</strong>e adapted to serum-free <strong>and</strong>growth factor-free conditions. J Biol Chem 269:8596–8603293. Moody TW, Chiles J, Casibang M, Moody E, Chan D, Davis TP2001 SR48692 is a neurotens<strong>in</strong> receptor antagonist which <strong>in</strong>hibits<strong>the</strong> growth <strong>of</strong> small cell lung cancer cells. Peptides 22:109–115294. Moody TW, Carney DN, Korman LY, Gazdar AF, M<strong>in</strong>na JD 1985Neurotens<strong>in</strong> is produced by <strong>and</strong> secreted from classic small celllung cancer cells. Life Sci 36:1727–1732295. Yashi M, Muraishi O, Kobayashi Y, Tokue A, Nanjo H 2002Elevated serum progastr<strong>in</strong>-releas<strong>in</strong>g peptide (31–98) <strong>in</strong> metastatic<strong>and</strong> <strong>and</strong>rogen-<strong>in</strong>dependent prostate cancer patients. Prostate 51:84–97296. Sehgal I, Powers S, Huntley B, Powis G, Pittelkow M, Maihle NJ1994 Neurotens<strong>in</strong> is an autocr<strong>in</strong>e trophic factor stimulated by <strong>and</strong>rogenwithdrawal <strong>in</strong> human prostate cancer. Proc Natl Acad SciUSA 91:4673–4677297. Seethalakshmi L, Mitra SP, Dobner PR, Menon M, Carraway RE1997 Neurotens<strong>in</strong> receptor expression <strong>in</strong> prostate cancer cell l<strong>in</strong>e<strong>and</strong> growth effect <strong>of</strong> NT at physiological concentrations. Prostate31:183–192298. Dal Farra C, Sarret P, Navarro V, Botto JM, Mazella J, V<strong>in</strong>cent JP2001 Involvement <strong>of</strong> <strong>the</strong> neurotens<strong>in</strong> receptor subtype NTR3 <strong>in</strong> <strong>the</strong>growth effect <strong>of</strong> neurotens<strong>in</strong> on cancer cell l<strong>in</strong>es. Int J Cancer92:503–509299. P<strong>in</strong>ski J, Reile H, Halmos G, Groot K, Schally AV 1994 Inhibitoryeffects <strong>of</strong> somatostat<strong>in</strong> analogue RC-160 <strong>and</strong> bombes<strong>in</strong>/gastr<strong>in</strong>releas<strong>in</strong>gpeptide antagonist RC-3095 on <strong>the</strong> growth <strong>of</strong> <strong>the</strong><strong>and</strong>rogen-<strong>in</strong>dependent Dunn<strong>in</strong>g R-3327-AT-1 rat prostate cancer.Cancer Res 54:169–174300. Jungwirth A, P<strong>in</strong>ski J, Galvan G, Halmos G, Szepeshazi K, CaiRZ, Groot K, Vadillo-Buenfil M, Schally AV 1997 Inhibition <strong>of</strong>growth <strong>of</strong> <strong>and</strong>rogen-<strong>in</strong>dependent DU-145 prostate cancer <strong>in</strong> vivo bylute<strong>in</strong>is<strong>in</strong>g hormone-releas<strong>in</strong>g hormone antagonist Cetrorelix <strong>and</strong>bombes<strong>in</strong> antagonists RC-3940-II <strong>and</strong> RC-3950-II. Eur J Cancer33:1141–1148301. Davis S, Rogers MA, Pendergrass TW 1987 The <strong>in</strong>cidence <strong>and</strong>epidemiologic characteristics <strong>of</strong> neuroblastoma <strong>in</strong> <strong>the</strong> UnitedStates. Am J Epidemiol 126:1063–1074302. Joshi VV, Silverman JF 1994 Pathology <strong>of</strong> neuroblastic tumors.Sem<strong>in</strong> Diagn Pathol 11:107–117303. Kelly DR, Joshi VV 1996 Neuroblastoma <strong>and</strong> related tumors. In:Parham DM, ed. Pediatric neoplasia: morphology <strong>and</strong> biology.Philadelphia: Lipp<strong>in</strong>cott-Raven; 105–152304. Borgstrom P, Hassan M, Wassberg E, Refai E, Jonsson C, Larsson,SA, Jacobsson H, Kogner P 1999 The somatostat<strong>in</strong> analogueoctreotide <strong>in</strong>hibits neuroblastoma growth <strong>in</strong> vivo. Pediatr Res 46:328–332305. Cattaneo MG, Scita G, Vicent<strong>in</strong>i LM 1999 Somatostat<strong>in</strong> <strong>in</strong>hibitsPDGF-stimulated Ras activation <strong>in</strong> human neuroblastoma cells.FEBS Lett 459:64–68306. Schill<strong>in</strong>g FH, Ambros PF, Bihl H, Mart<strong>in</strong>sson T, Ambros IM,Borgstrom P, Jacobsson H, Falkmer UG, Treuner J, Kogner P 2001Absence <strong>of</strong> somatostat<strong>in</strong> receptor expression <strong>in</strong> vivo is correlated todi- or tetraploid 1p36-deleted neuroblastomas. Med Pediatr Oncol36:56–60307. Orl<strong>and</strong>o C, Raggi CC, Bagnoni L, Sest<strong>in</strong>i R, Briganti V, La CavaG, Bern<strong>in</strong>i G, Ton<strong>in</strong>i GP, Pazzagli M, Serio M, Maggi M 2001Somatostat<strong>in</strong> receptor type 2 gene expression <strong>in</strong> neuroblastoma,measured by competitive RT-PCR, is related to patient survival <strong>and</strong>to somatostat<strong>in</strong> receptor imag<strong>in</strong>g by <strong>in</strong>dium-111-pentetreotide.Med Pediatr Oncol 36:224–226308. Sebesta JA, Young A, Bullock J, Moore KH, Azarow K, Saw<strong>in</strong> RS2001 Gastr<strong>in</strong>-releas<strong>in</strong>g peptide: a potential growth factor expressed<strong>in</strong> human neuroblastoma tumors(1). Curr Surg 58:86–89309. Kim S, Hu W, Kelly DR, Hellmich MR, Evers BM, Chung DH2002 Gastr<strong>in</strong>-releas<strong>in</strong>g peptide is a growth factor for human neuroblastomas.Ann Surg 235:621–630310. Thompson JC, Townsend Jr CM 2001 Endocr<strong>in</strong>e pancreas. In:Townsend Jr CM, Beauchamp RD, Evers BM, Mattox KL, eds.Sabiston textbook <strong>of</strong> surgery: <strong>the</strong> biological basis <strong>of</strong> modern surgicalpractice. 16th ed. Philadelphia: W. B. Saunders Company;646–661311. Angood PB, G<strong>in</strong>galewski CA, Andersen DK 2001 Surgical complications.In: Townsend Jr CM, Beauchamp RD, Evers BM, MattoxKL, eds. Sabiston textbook <strong>of</strong> surgery: <strong>the</strong> biological basis <strong>of</strong> modernsurgical practice, 16th ed. Philadelphia: W. B. Saunders Company;198–225312. Oberg K 2001 Chemo<strong>the</strong>rapy <strong>and</strong> bio<strong>the</strong>rapy <strong>in</strong> <strong>the</strong> treatment <strong>of</strong>neuroendocr<strong>in</strong>e tumours. Ann Oncol 12(Suppl 2):S111–S114313. Schmassmann A, Reubi JC 2000 Cholecystok<strong>in</strong><strong>in</strong>-B/gastr<strong>in</strong> receptorsenhance wound heal<strong>in</strong>g <strong>in</strong> <strong>the</strong> rat gastric mucosa. J Cl<strong>in</strong>Invest 106:1021–1029314. Scolapio JS 2001 Treatment <strong>of</strong> short-bowel syndrome. Curr Op<strong>in</strong>Cl<strong>in</strong> Nutr Metab Care 4:557–560315. Toledano A, Rodriguez-Arellano JJ, Gomez de Segura IA,De Miguel E, Mart<strong>in</strong>ez-Rodriguez R 1996 Bowel resection <strong>and</strong>neurotens<strong>in</strong> treatment. Histochemical study <strong>of</strong> neurotens<strong>in</strong>-like<strong>and</strong> somatostat<strong>in</strong>-like immunoreactivities <strong>and</strong> receptors. Cell MolBiol (Noisy-le-gr<strong>and</strong>) 42:1145–1158316. Jeppesen PB, Hartmann B, Thulesen J, Graff J, Lohmann J,Hansen BS, T<strong>of</strong>teng F, Poulsen SS, Madsen JL, Holst JJ,Mortensen PB 2001 Glucagon-like peptide 2 improves nutrientabsorption <strong>and</strong> nutritional status <strong>in</strong> short-bowel patients with nocolon. Gastroenterology 120:806–815317. Smith AM, Just<strong>in</strong> T, Michaeli D, Watson SA 2000 Phase I/II study<strong>of</strong> G17-DT, an anti-gastr<strong>in</strong> immunogen, <strong>in</strong> advanced colorectalcancer. Cl<strong>in</strong> Cancer Res 6:4719–4724318. Watson SA, Michaeli D, Morris TM, Clarke P, Varro A, Griff<strong>in</strong>N, Smith A, Just<strong>in</strong> T, Hardcastle JD 1999 Antibodies raised bygastrimmune <strong>in</strong>hibit <strong>the</strong> spontaneous metastasis <strong>of</strong> a human colorectaltumour, AP5LV. Eur J Cancer 35:1286–1291319. Abbruzzese JL, Gholson CF, Daugherty K, Larson E, DuBrow R,Berl<strong>in</strong> R, Lev<strong>in</strong> B 1992 A pilot cl<strong>in</strong>ical trial <strong>of</strong> <strong>the</strong> cholecystok<strong>in</strong><strong>in</strong>receptor antagonist MK-329 <strong>in</strong> patients with advanced pancreaticcancer. Pancreas 7:165–171320. Militello C, Sperti C, Di Prima F, Pedrazzoli S 1997 Cl<strong>in</strong>icalDownloaded from edrv.endojournals.org by on July 16, 2007
Thomas et al. • <strong>Gastro<strong>in</strong>test<strong>in</strong>al</strong> <strong>Hormones</strong> <strong>and</strong> <strong>Proliferation</strong> Endocr<strong>in</strong>e Reviews, October 2003, 24(5):571–599 599evaluation <strong>and</strong> safety <strong>of</strong> loxiglumide (CCK-A receptor antagonist)<strong>in</strong> nonresectable pancreatic cancer patients. Italian Pancreatic CancerStudy Group. Pancreas 14:222–228321. Hejna M, Schmid<strong>in</strong>ger M, Raderer M 2002 The cl<strong>in</strong>ical role <strong>of</strong>somatostat<strong>in</strong> analogues as ant<strong>in</strong>eoplastic agents: much ado aboutnoth<strong>in</strong>g? Ann Oncol 13:653–668322. Kraenzl<strong>in</strong> ME, Ch’ng JL, Wood SM, Carr DH, Bloom SR 1985Long-term treatment <strong>of</strong> a VIPoma with somatostat<strong>in</strong> analogue result<strong>in</strong>g<strong>in</strong> remission <strong>of</strong> symptoms <strong>and</strong> possible shr<strong>in</strong>kage <strong>of</strong> metastases.Gastroenterology 88:185–187323. Williams G, Anderson JV, Williams SJ, Bloom SR 1987 Cl<strong>in</strong>icalevaluation <strong>of</strong> SMS 201-995. Long-term treatment <strong>in</strong> gut neuroendocr<strong>in</strong>etumours, efficacy <strong>of</strong> oral adm<strong>in</strong>istration, <strong>and</strong> possible use<strong>in</strong> non-tumoural <strong>in</strong>appropriate TSH hypersecretion. Acta Endocr<strong>in</strong>olSuppl (Copenh) 286:26–36324. Ebert M, Friess H, Beger HG, Buchler MW 1994 <strong>Role</strong> <strong>of</strong> octreotide<strong>in</strong> <strong>the</strong> treatment <strong>of</strong> pancreatic cancer. Digestion 55(Suppl 1):48–51325. Goldberg RM, Moertel CG, Wie<strong>and</strong> HS, Krook JE, Schutt AJ,Veeder MH, Mailliard JA, Dalton RJ 1995 A phase III evaluation<strong>of</strong> a somatostat<strong>in</strong> analogue (octreotide) <strong>in</strong> <strong>the</strong> treatment <strong>of</strong>patients with asymptomatic advanced colon carc<strong>in</strong>oma. NorthCentral Cancer Treatment Group <strong>and</strong> <strong>the</strong> Mayo Cl<strong>in</strong>ic. Cancer76:961–966326. Cirillo F, Bott<strong>in</strong>i A, Brunelli A, Zuffada S, Bassi M, Filipp<strong>in</strong>i L,Alquati P 1998 Octreotide <strong>in</strong> <strong>the</strong> treatment <strong>of</strong> advanced pancreatictumor. Prelim<strong>in</strong>ary study. M<strong>in</strong>erva Chir 53:979–9853rd European Congress <strong>of</strong> Andrology/16th Congress <strong>of</strong> <strong>the</strong> German Society <strong>of</strong> AndrologySeptember 11–14, 2004Münster, GermanyThe 3rd ECA will be <strong>the</strong> premier event <strong>in</strong> Andrology <strong>in</strong> 2004 <strong>in</strong> Europe, sponsored by <strong>the</strong> European Academy<strong>of</strong> Andrology (EAA) <strong>and</strong> <strong>the</strong> German Society <strong>of</strong> Andrology (DGA). It br<strong>in</strong>gs toge<strong>the</strong>r cl<strong>in</strong>icians <strong>and</strong> basicscientists active <strong>in</strong> <strong>and</strong>rology <strong>and</strong> will cover all aspects <strong>of</strong> <strong>and</strong>rology with emphasis on control <strong>of</strong> spermatogenesis,spermatogonial stem cells, <strong>the</strong>rapeutic use <strong>of</strong> <strong>and</strong>rogens, erectile dysfunction, male <strong>in</strong>fertility,assisted reproduction, paternally mediated teratogenicity, prostate cancer, testicular tumors, environment<strong>and</strong> reproduction, <strong>and</strong> f<strong>in</strong>ally male contraception.Fur<strong>the</strong>r <strong>in</strong>formation, registration <strong>and</strong> abstract submission through <strong>the</strong> web site: www.3rd-eca.deFur<strong>the</strong>r contact: Pr<strong>of</strong>. Dr. E. Nieschlag, Institute <strong>of</strong> Reproductive Medic<strong>in</strong>e <strong>of</strong> <strong>the</strong> University, D-48129Muenster, Germany, Tel: 49 0251/83 56096, Fax: 49 0251/8356093, E-mail: nieschl@uni-muenster.deIOF World Congress on OsteoporosisThe International Osteoporosis Foundation is pleased to <strong>in</strong>vite you to participate <strong>in</strong> <strong>the</strong> IOF World Congresson Osteoporosis to be held <strong>in</strong> Rio de Janerio (Brazil), May 14–18, 2004. This event is your chance to hear—<strong>and</strong>meet—<strong>the</strong> lead<strong>in</strong>g experts <strong>in</strong> <strong>the</strong> field <strong>and</strong> learn <strong>the</strong> latest developments <strong>in</strong> basic research <strong>and</strong> cl<strong>in</strong>ical <strong>and</strong><strong>the</strong>rapeutic advances. Onl<strong>in</strong>e abstract submission <strong>and</strong> registration can be found at www.oste<strong>of</strong>ound.orgContact: IOF–Congress Secretariat, 71 cours Albert Thomas, 69447 Lyon, France, Tel: 33472914177,Fax: 33 4 72 36 90 52, E-mail: <strong>in</strong>fo@oste<strong>of</strong>ound.orgDownloaded from edrv.endojournals.org by on July 16, 2007