Abstract
Background
Modeling studies using large datasets from men with lower urinary tract symptoms/benign prostate enlargement (LUTS/BPE) can predict changes in International Prostate Symptom Score (IPSS) and risk of acute urinary retention/surgery under different treatment regimens and according to predictors (baseline characteristics) that commonly define risk of progression. We assessed the impact of treatments on different symptom types (storage, voiding, and nocturia), quality of life (QoL; IPSS Q8), and BPH Impact Index [BII]).
Methods
Generalized least squares models were used to predict each outcome. Data from the CombAT study were used to predict outcomes for active treatments (dutasteride, tamsulosin, combination therapy). Predictors included: age; IPSS total, storage, voiding, nocturia and QoL (IPSS Q8) scores; BII; prostate volume; maximum urine flow rate (Qmax), prostate-specific antigen, postvoid residual urine (PVR); alpha-blocker usage within 12 months. Data from phase III dutasteride monotherapy studies were used to predict placebo outcomes. Results were visualized using an interactive web-based tool (www.bphtool.com).
Results
Combination therapy provided greater predicted benefit than either monotherapy for all five outcomes for most patient profiles within the CombAT inclusion criteria. PVR and corresponding subscores were significant predictors of change in both storage and voiding subscores. Alpha-blocker use within 12 months, age (storage subscore), and Qmax (voiding subscore) were also significant predictors. PVR, age, Qmax, and nocturia score were significant predictors of change in nocturia. PVR, Qmax, previous alpha-blocker use, total IPSS, and QoL (IPSS Q8) score were significant predictors of change in QoL (IPSS Q8) score. For BII, significant predictors were PVR, age, total IPSS, and BII score. The multivariable effect of covariates and treatments is best visualized through the interactive web-based tool.
Conclusions
This predictive modeling study informs our understanding of how risk factors for disease progression interact and affect treatment impact on different symptom types and QoL scores.
Similar content being viewed by others
Introduction
Clinical guidelines provide clear recommendations for assessing men with lower urinary tract symptoms (LUTS) as a result of benign prostatic enlargement (BPE), and have two main objectives: to establish a differential diagnosis (since the origin of LUTS in men is multifactorial) and to define the clinical profile (including risk of disease progression, e.g., higher prostate volume [PV], higher serum prostate-specific antigen [PSA] concentration, advanced age, higher post-void residual volume [PVR], and lower urinary flow) of men with LUTS in order to provide personalized and appropriate care [1, 2].
Men with LUTS/BPE can be affected by voiding, storage, and post-micturition symptoms [3]. Voiding symptoms are thought to arise from urethral obstruction, often as a result of BPE [4, 5]. Storage symptoms (including nocturia) are often seen in men with overactive bladder (OAB) and BPE, and result from altered smooth muscle structure and function in the bladder and prostate [5, 6]. Voiding and storage symptoms cause bother and impair quality of life (QoL) [7,8,9]. Nocturia is among the most frequently reported and bothersome symptom [10, 11] and the major cause of physician consultations in men with LUTS/BPE [12]. LUTS/BPE can progress to worsening of symptoms and complications, such as acute urinary retention (AUR) and BPE-related surgery. Therefore, a treatment approach that targets the underlying disease mechanism and improves different symptom types, as well as reducing the risk of AUR/surgery, would be advantageous.
The wealth and complexity of clinical trial data make it difficult to understand how evidence can optimally inform personalized treatment decisions, since results are typically presented as mean values for a defined population. Insights from the application of predictive analytics to large clinical cohorts can support physicians in understanding the key characteristics and relationships behind responses to individual treatments. This knowledge can help to tailor the treatment approach in patients with LUTS/BPE at different levels of progression risk. Visualizing individual risks, and how they may change in the future depending on treatment choice (active or placebo), may support healthcare professionals and patients in making more personalized, data-driven decisions based on easily accessible baseline parameters and risk factors.
A predictive analytics solution, using large datasets of patients receiving placebo, dutasteride, tamsulosin, or dutasteride/tamsulosin combination therapy (CT), was developed to project the change from baseline in total IPSS and risk of AUR or surgery under these different treatment regimens, according to baseline characteristics that commonly define patients at risk of disease progression, such as age ≥50 years, moderate-to-severe LUTS, PV ≥ 30 mL, and PSA ≥ 1.5 ng/mL [13]. The study showed that the vast majority of patients benefit more from dutasteride or dutasteride/tamsulosin CT compared with tamsulosin alone, highlighting the prognostic importance of baseline covariates to predict treatment response in individual profiles [13]. An educational, interactive web-based tool was developed to facilitate visualization and understanding of predicted outcomes for any individual profile meeting the CombAT study entry criteria, integrating any possible combination of variables (predictors). The tool is available at www.bphtool.com.
The current study aimed to expand on the predictive analytics solution described above to better understand how placebo, dutasteride, tamsulosin, or CT impact different symptom types (IPSS subscores for storage, voiding, and nocturia [IPSS Q7]) over time, as well as QoL (IPSS Q8) and BPH Impact Index (BII), in different profiles of men with BPE at risk of progression as defined by their baseline characteristics. The web-based tool was updated to facilitate visualization and understanding of study results.
Methods
Data sources, endpoints, and variables
Datasets are the same as those used in the initial predictive analytics solution [13]; three placebo-controlled dutasteride trials (ARIA3001, ARIA3002, and ARIB3003) and one trial comparing the active therapies: dutasteride, tamsulosin, and combination (ARI40005; CombAT) [14, 15]. Reasons for not including other studies of dutasteride and finasteride have been previously described [13].
Using clinically relevant baseline characteristics that commonly define patients with LUTS/BPE at risk of disease progression, we aimed to separately predict longitudinal change from baseline in (i) IPSS voiding subscore, (ii) IPSS storage subscore, (iii) IPSS nocturia subscore (Q7), (iv) QoL (IPSS Q8), and (v) BII score. Definitions of the disease outcomes explored, and duration of follow-up, are detailed in the Supplementary information (Table S1). The covariates used to predict treatment effect on LUTS/BPE outcomes in these models are shown in Table 1.
Predictive modeling strategy
Patient-level data from the CombAT study [15] were used in a model to predict outcomes with active treatments (dutasteride, tamsulosin, and CT). Patient-level data from three phase III dutasteride monotherapy studies [14] were used in a model to predict outcomes with placebo.
A generalized least squares model was used to predict each of the five disease outcomes, assuming all outcomes to be continuous. Models were validated using a 10-fold cross-validation method, and performed equally well in the training and test sets. Model evaluation was compared before and after excluding non-relevant predictors and nugatory predictors, based on estimated parameters with associated p values > 0.05 and insignificant improvement of model when its presence was excluded. After exclusion, the change in parameter estimates for the remaining predictors was evaluated; those with a relative change in estimate >30% were considered possible confounders and adjusted for in the final model. The analyses adhere to the Transparent Reporting of a multivariable prediction model for Individual Prognosis Or Diagnosis statement [16].
Table 2 shows summary statistics of baseline characteristics from the CombAT and phase III dutasteride studies that were considered for model development and validation. Additional information on datasets (Table S2), endpoints, variable selection, handling of missing data, modeling strategy, and model performance is provided in the Supplementary material.
Results
Descriptive analysis of baseline variables
A total of 9166 subjects with LUTS/BPE at risk of progression who were included in the CombAT study and placebo-controlled dutasteride monotherapy studies were considered. There were no significant differences in baseline covariates between groups in CombAT or the placebo-controlled dutasteride studies (Tables S3 and S4). Table 3 presents the relevant covariates with significant estimates (p < 0.05) for each of the outcomes.
IPSS storage subscore
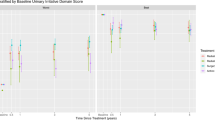
The benefit of treatment (reduction in storage subscore) is predicted to be greater with dutasteride plus tamsulosin than with either monotherapy for most patient profiles within the CombAT study inclusion criteria. Figure 1a shows the change from baseline in IPSS storage subscore for an example patient profile, based on mean values of the relevant covariates considered in this model, as visualized on the updated interactive tool (www.bphtool.com).
a storage subscore, b voiding subscore, c nocturia subscore. Obtained from www.bphtool.com. Estimates for placebo are made using a model trained on monotherapies data only (2-year study duration). These examples consider mean values of covariates considered to estimate the trajectories for both treatments and placebo for the intended outcomes: (1) Common predictors for all outcomes: age, 66 years; PV, 55 mL; PVR, 68 mL; Qmax, 11 mL/s; PSA, 4 ng/mL; alpha-blocker use, no. (2) Additional outcome-specific predictors: IPSS storage subscore, 7; IPSS voiding subscore, 9; IPSS nocturia (Q7) score, 2.
The baseline covariates of PVR, previous alpha-blocker use, age, and baseline storage subscore were significant predictors of the change in storage subscore in the CombAT model (Table 3, Table S6). The positive sign of the coefficient indicates that higher baseline values of PVR and age, and previous alpha-blocker use, predict an increase in the subscore and, therefore, a worsening of symptoms. For the placebo model, age, PSA, and previous alpha-blocker use were significant predictors of change in storage subscore (Table 3, Table S9).
Baseline IPSS storage subscore was a significant predictor of improvement in storage subscore for each of the active treatments (coefficient of –0.603; p < 0.001). Improvements in storage subscore were greater with CT than with either monotherapy across all baseline IPSS storage values; the improvement was greater with higher baseline storage subscores. Older age (coefficient of 0.019; p < 0.001), higher baseline PVR (coefficient of 0.001; p = 0.004), or previous alpha-blocker use (coefficient of 0.259; p = 0.001) predicted a significant worsening of storage symptoms.
While baseline PSA was not a significant predictor of change in storage subscore, the best model fitting the data is represented by the combination of the significant covariates at baseline and interaction between PSA and baseline storage subscore with treatments (Table S5). CT was predicted to improve IPSS storage subscores compared with tamsulosin across all baseline PSA values, with greater improvement with lower baseline PSA. The effect of dutasteride was similar to that of CT.
IPSS voiding subscore
The predicted treatment benefit (reduction in voiding subscore) is greater with CT than with either monotherapy for most patient profiles within the CombAT inclusion criteria. The change from baseline in IPSS voiding subscore for an example patient profile in this model is shown in Fig. 1b.
The baseline covariates of Qmax, PVR, and baseline voiding subscore are significant predictors of the change in voiding subscore in the CombAT model (Table 3, Table S10). Overall, patient profiles with higher baseline voiding subscores benefit from each of the active treatments (coefficient of −0.652; p < 0.001), and improvement is greater with CT compared with dutasteride (coefficient of 0.085; p = 0.001) and tamsulosin (coefficient of 0.062; p = 0.012). Higher baseline PVR (coefficient of 0.003; p < 0.001) and lower Qmax (coefficient of −0.042; p < 0.001) at baseline predicted a significant worsening in voiding symptoms. For the placebo model, PSA and previous alpha-blocker use were significant predictors of change in voiding subscore (Table 3, Table S12).
Significant interaction effects were detected between baseline PV, PSA, and voiding subscores with treatment (Table 3). Patient profiles with lower PSA values were predicted to have significantly greater voiding symptom improvement with CT compared with either monotherapy. Higher baseline PSA values resulted in a comparable predicted treatment effect for dutasteride and CT.
Nocturia (IPSS Q7)
The change from baseline in nocturia for an example patient profile is shown in Fig. 1c. The predicted treatment benefit for most patient profiles within the CombAT inclusion criteria was greater with CT compared with either monotherapy.
The baseline covariates of Qmax, PVR, nocturia severity, and age were significant predictors of the change in nocturia score in the CombAT model (Table 3, Table S14). Overall, patients with more severe nocturia at baseline benefited from all treatments (coefficient of –0.595; p < 0.001). Higher baseline PVR (coefficient of 0.001; p = 0.001) and lower baseline Qmax (coefficient of –0.008; p = 0.006) predicted a significant worsening in nocturia symptoms. For the placebo model, age, PSA, and baseline nocturia score were significant predictors of change in nocturia score (Table 3, Table S16).
A significant interaction between alpha-blocker use and treatment was observed. While previous alpha-blocker use predicted greater improvement in nocturia with CT or dutasteride, a significant worsening was predicted with tamsulosin (coefficient of 0.172; p = 0.009). Baseline nocturia score, age, and PVR also interacted significantly with treatment. Higher values of baseline nocturia score predicted greater improvements with CT compared with either monotherapy.
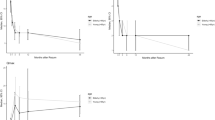
QoL (IPSS Q8)
Figure 2a shows the change from baseline in QoL (IPSS Q8) for the example patient profile. Predictions for placebo were not possible since data for QoL (IPSS Q8) were not available in the dutasteride phase III studies. Once more, the predicted benefit for most profiles within CombAT inclusion criteria is greater with CT than with either monotherapy. The baseline covariates of total IPSS, IPSS Q8 score, Qmax, PVR, and previous alpha-blocker use were significant predictors of change in Q8 score (Table 3, Table S18).
a IPSS Q8 score, b BII score. Obtained from www.bphtool.com. Estimates for placebo are made using a model trained on monotherapies data only (2-year study duration). These examples consider mean values of covariates considered to estimate the trajectories for both treatments and placebo for the intended outcomes: (1) Common predictors for both outcomes: age, 66 years; PV, 55 mL; PVR, 68 mL; Qmax, 11 mL/s; PSA, 4 ng/mL; alpha-blocker use, no. (2) Additional outcome-specific predictors: IPSS QoL (Q8) score, 3; BII score, 5.
Significant interactions were detected between baseline covariates of QoL (IPSS Q8) score, PV, age, Qmax, and treatment (Table 3). Higher scores at baseline were predictive of greater improvement in QoL (IPSS Q8) with CT compared with either monotherapy. For PV, the predicted difference of tamsulosin over CT was greater with higher baseline values.
BII
The change from baseline in BII for an example patient profile is shown in Fig. 2b. CT provides greater predicted benefit compared with either monotherapy for most profiles within the CombAT inclusion criteria. Baseline age, PVR, BII score, and total IPSS were significant predictors of change in BII score (Table 3, Table S20). For the placebo model, total IPSS, PSA, and previous alpha-blocker use were significant predictors of change in BII score (Table 3, Table S22). A significant interaction between alpha-blocker use and treatment was observed (Table 3). Alpha-blocker use in the previous 12 months was predicted to provide greater benefit than no previous use for treatment with tamsulosin; however, both dutasteride and CT were predicted to provide greater benefit than tamsulosin alone.
Discussion
We have previously developed multivariable predictive models using the largest available datasets of patients with LUTS/BPE at risk of disease progression to predict the change in IPSS total score and the risk of AUR and BPE-related surgery with different treatment regimens (placebo, dutasteride, tamsulosin, or CT) for up to 48 months, with baseline characteristics commonly used to define the risk of disease progression [13]. The current study extends this work by developing similar models to predict changes in IPSS storage subscore, IPSS voiding subscore, nocturia (IPSS Q7), QoL (IPSS Q8), and BII (bother). Consistent with results from post hoc analyses of average CombAT patient profiles [17, 18], in general, the predicted benefit over time of treatment with dutasteride/tamsulosin CT is greater than with either monotherapy for most patient risk profiles. Our results reinforce the benefit of a treatment approach that targets the underlying disease mechanism (5α-reductase inhibitors [5ARI]) in the short and long term in men with LUTS/BPE at risk of disease progression. They also provide insight on the impact of the studied treatments on different types of symptoms and QoL measures for individual patient profiles, which is typically not available from clinical trials (that address average treatment effects across a study population). In addition, the results allow greater understanding of the contribution of individual baseline characteristics that commonly define risk of LUTS/BPE disease progression.
Prior alpha-blocker use is a significant predictive factor of most outcomes. In addition, the models predict that the placebo effect is lower in men with a history of alpha-blocker use than in men without. This likely reflects differences in perceived benefit of active study treatment, which is likely to have been lower in men with alpha-blocker use in the previous 12 months than in men with no prior alpha-blocker use.
The predicted long-term effects of 5ARI-based treatment on storage symptoms and nocturia are also noteworthy. PVR is thought to be a multifactorial condition, with involvement of both bladder outlet obstruction (BOO) and bladder dysfunction (e.g., detrusor underactivity) [19]. Previous studies have suggested a role for 5ARIs in counteracting the molecular changes that lead to development and worsening of storage symptoms, probably as a result of PV reduction and improvement in BOO over time [20,21,22,23]. Several studies have also reported that 5ARI-based therapy can improve nocturia [18, 24]. Nocturia is associated with incomplete bladder emptying, OAB symptoms, and nocturnal polyuria, with the latter known to be highly prevalent in men with BPE [25].
While LUTS/BPE is rarely life-threatening, symptoms such as nocturia have been linked to increased mortality risk in men with the condition [26, 27]. The impact on QoL is also significant and should not be underestimated. This study allows visualization of the estimated change in total IPSS from baseline and corresponding QoL in individual profiles, to better understand the relevance of changes that ultimately will help guide treatment decisions [28].
As with our previous study [13], we found that each baseline covariate contributes differently to the predicted improvements. In addition, we identified significant interaction effects between covariates and treatment for each disease outcome, which should be interpreted in conjunction with the observed main effect of the covariate and treatment. This wealth of complexity poses a challenge in how to effectively present many and diverse results in an informative manner. For example, visualizing the effect of medical treatment in distinct patient profiles would require numerous nomograms or heatmaps. The educational interactive web-based tool (www.bphtool.com) was developed to facilitate visualization and understanding of the predicted outcomes for various combinations of baseline values within the eligibility criteria for the CombAT study [13]. The tool has been updated to enable visualization of change from baseline (absolute or percentage) in IPSS voiding and storage subscores, as well as nocturia score (IPSS Q7), QoL (IPSS Q8) score, and BII. It is, though, important to note that the tool is not intended on its own to substitute for medical advice nor to drive treatment decisions in real-world clinical practice. All such decisions should also consider a range of additional factors such as presence of comorbidities, risk of adverse events, and patient preferences and needs.
Potential limitations of our study should be acknowledged. The main limitation is that the modeling data and predictions may not be generalizable to the broader population of men with LUTS/BPE, as no information is provided for variables outside of the inclusion criteria used in the dutasteride source datasets (e.g., age <50 years, IPSS < 12, PV < 30 mL, PSA < 1.5 ng/mL). Also, placebo predictions were made using a model trained on 2-year monotherapy data only, since there was no placebo arm in CombAT; consequently, comparison of placebo with active therapies requires a strong assumption of exchangeability. In addition, it was not possible to validate model performance using data from trials with 2-year follow-up on active therapy, given the absence of such studies. Moreover, the models have not been assessed in the healthcare setting so are not, therefore, validated for clinical use. The models also did not evaluate adverse events, which are an important consideration when deciding on a personalized treatment approach. A further limitation is that the IPSS questionnaire does not allow assessment of incontinence, post-micturition symptoms, or bother due to different symptom types. Finally, due to the absence of suitable data from the source datasets, our models do not take account of other variables that might contribute to disease and treatment outcomes for men with LUTS/BPE (such as presence of comorbidities, intravesical prostatic protrusion, etc); this would be an interesting area of future research, along with extending the analyses to other available treatments and patient populations.
In conclusion, this predictive modeling study based on large datasets enhances our understanding of how risk factors for disease progression interact and affect the impact of treatment on different symptom types and QoL, reinforcing the importance of an individualized approach to LUTS/BPE management.
Data availability
Anonymized individual participant data and study documents from the studies mentioned within this paper can be requested for further research from www.clinicalstudydatarequest.com/Default.aspx. All the codes used to generate the outputs from this study are stored in a GSK-owned repository and can be requested for further research with permission from the owner.
References
Cornu JN, Gacci M, Hashim H, Hermann TRW, Malde S, Netsch C, et al. EAU Guidelines on Management of Non-Neurogenic Male Lower Urinary Tract Symptoms (LUTS), incl. benign prostatic obstruction (BPO). Arnhem: European Association of Urology Guidelines Office; 2023. https://uroweb.org/guidelines/management-of-non-neurogenic-male-luts. Accessed 25 Jul 2023.
Gravas S, Gacci M, Gratzke C, Herrmann TRW, Karavitakis M, Kyriazis I, et al. Summary paper on the 2023 European Association of Urology Guidelines on the Management of Non-neurogenic Male Lower Urinary Tract Symptoms. Eur Urol. 2023;84:207–22.
Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the international continence society. Urology. 2003;61:37–49.
Roehrborn CG. Combination medical therapy for lower urinary tract symptoms and benign prostatic hyperplasia. Rev Urol. 2005;7:S43–51.
Rosenberg MT, Staskin DR, Kaplan SA, MacDiarmid SA, Newman DK, Ohl DA. A practical guide to the evaluation and treatment of male lower urinary tract symptoms in the primary care setting. Int J Clin Pract. 2007;61:1535–46.
Mirone V, Imbimbo C, Longo N, Fusco F. The detrusor muscle: an innocent victim of bladder outlet obstruction. Eur Urol. 2007;51:57–66.
Martin SA, Haren MT, Marshall VR, Lange K, Wittert GA. Prevalence and factors associated with uncomplicated storage and voiding lower urinary tract symptoms in community-dwelling Australian men. World J Urol. 2011;29:179–84.
Kupelian V, Wei JT, O’Leary MP, Kusek JW, Litman HJ, Link CL, et al. Prevalence of lower urinary tract symptoms and effect on quality of life in a racially and ethnically diverse random sample: the Boston Area Community Health (BACH) survey. Arch Intern Med. 2006;166:2381–7.
Agarwal A, Eryuzlu LN, Cartwright R, Thorlund T, Tammela TLJ, Guyatt GH, et al. What is the most bothersome lower urinary tract symptom? Individual- and population-level perspectives for both men and women. Eur Urol. 2014;65:1211–7.
Rohrman S, Katzke V, Kaaks R. Prevalence and progression of lower urinary tract symptoms in an aging population. Urology. 2016;95:158–63.
Coyne KS, Wein AJ, Tubaro A, Sexton CC, Thompson CL, Kopp ZS, et al. The burden of lower urinary tract symptoms: evaluating the effect of LUTS on health-related quality of life, anxiety and depression: EpiLUTS. BJU Int. 2009;103 Suppl 3:4–11.
Oelke M, Wiese B, Berges R. Nocturia and its impact on health-related quality of life and health care seeking behaviour in German community-dwelling men aged 50 years or older. World J Urol. 2014;32:1155–62.
Gravas S, Palacios-Moreno JM, Thompson D, Concas F, Kamola PJ, Roehrborn CG, et al. Understanding treatment response in individual profiles of men with prostatic enlargement at risk of progression. Eur Urol Focus. 2023;9:178–87.
Roehrborn CG, Boyle P, Nickel JC, Hoefner K, Andriole G. Efficacy and safety of a dual inhibitor of 5-alpha-reductase types 1 and 2 (dutasteride) in men with benign prostatic hyperplasia. Urology. 2002;60:434–41.
Roehrborn CG, Siami P, Barkin J, Damiao R, Major-Walker K, Nandy I, et al. The effects of combination therapy with dutasteride and tamsulosin on clinical outcomes in men with symptomatic benign prostatic hyperplasia: 4-year results from the CombAT study. Eur Urol. 2010;57:123–31.
Collins GS, Reitsma JB, Altman DG, Moons KGM. Transparent reporting of a multivariate prediction model for Individual Prognosis or Diagnosis (TRIPOD): the TRIPOD statement. Ann Intern Med. 2015;162:55–63.
Montorsi F, Roehrborn C, Garcia-Penit J, Borre M, Roeleveld TA, Alimi JC, et al. The effects of dutasteride or tamsulosin alone and in combination on storage and voiding symptoms in men with lower urinary tract symptoms (LUTS) and benign prostatic hyperplasia (BPH): 4-year data from the Combination of Avodart and Tamsulosin (CombAT) study. BJU Int. 2011;107:1426–31.
Oelke M, Roehrborn CG, D’Ancona C, Wilson TH, Castro R, Manyak M. Nocturia improvement in the combination of Avodart® and tamsulosin (CombAT) study. World J Urol. 2014;32:1133–40.
Stoffel JT, Peterson AC, Sandhu JS, Suskind AM, Wei JT, Lightner DJ. AUA white paper on nonneurogenic chronic urinary retention: consensus definition, treatment algorithm, and outcome end points. J Urol. 2017;198:153–60.
Matsuka Y, Gotoh M, Kato M, Funahashi Y, Narita M, Mitsui K. Effects of dutasteride on storage and voiding symptoms in male patients with lower urinary tract symptoms as a result of benign prostatic obstruction: the 1-year outcomes from a prospective urodynamic study. Int J Urol. 2014;21:826–30.
Wada N, Kita M, Hashizume K, Matsumoto S, Kakizaki H. Urodynamic effects of dutasteride add-on therapy to alpha-adrenergic antagonist for patients with benign prostatic enlargement: prospective pressure-flow study. Neurourol Urodyn. 2013;32:1123–7.
Wada N, Matsumoto S, Kita M, Hashizume K, Kakizaki H. Decreased urinary nerve growth factor reflects prostatic volume reduction and relief of outlet obstruction in patients with benign prostatic enlargement treated with dutasteride. Int J Urol. 2014;21:1258–62.
Wada N, Matsumoto S, Kita M, Hashizume K, Kakizaki H. Improvement of overactive bladder symptoms and bladder ischemia with dutasteride in patients with benign prostatic enlargement. Low Urin Trac Symptoms. 2015;7:37–41.
Kuhlmann PG, Fischer SC, Howard LE, Moreira DM, Andriole GL, Hopp ML, et al. Dutasteride improves nocturia but does not lead to better sleep: results from the REDUCE clinical trial. J Urol. 2021;205:1733–9.
Yoong HF, Sundaram MB, Aida Z. Prevalence of nocturnal polyuria in patients with benign prostatic hyperplasia. Med J Malays. 2005;60:294–6.
Bliwise DL, Howard LE, Moreira DM, Andriole GL, Hopp ML, Freedland SJ. Nocturia and associated mortality: observational data from the REDUCE trial. Prostate Cancer Prostatic Dis. 2019;22:77–83.
Moon S, Kim YJ, Chung HS, Yu JM, Park II, Park SG, et al. The relationship between nocturia and mortality: data from the National Health and Nutrition Examination Survey. Int Neurourol J. 2022;26:144–52.
Lerner LB, McVary KT, Barry MJ, Bixler BR, Dahm P, Das AK, et al. Management of lower urinary tract symptoms attributed to benign prostatic hyperplasia: AUA Guideline Part I—initial work-up and medical management. J Urol. 2021;206:806–17.
Acknowledgements
Editorial support in the form of writing assistance, including preparation of the draft manuscript under the direction and guidance of the authors, collating and incorporating authors’ comments for each draft, assembling tables and figures, grammatical editing, and referencing, was provided by Tony Reardon, of Luna, OPEN Health Communications, in accordance with Good Publication Practice (GPP) guidelines (www.ismpp.org/gpp-2022). Support was funded by GSK.
Funding
This research was funded by GSK (study number 219073). GSK has developed the web app tool to support visualization of study results and holds copyrights. The sponsor played a role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, and approval of the manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to data analysis and interpretation, drafting of the manuscript, and final approval of the manuscript. SG, JMP, CC, CGR, MO, MAA, AB, LMG, and VC contributed to conception and design; JMP, CC, AB, and VC contributed to provision of study material or patients; and AB and LMG contributed to collection and/or assembly of data.
Corresponding author
Ethics declarations
Competing interests
SG received research grants and/or honoraria from Astellas, GSK, Lilly, and Pierre Fabre Medicament. CGR received honoraria from and acted as a consultant for GSK. MO has been a speaker, consultant, and/or trial participant for Apogepha, Astellas, Duchesnay, Ferring, GSK, Lilly, Pierre Fabre, Pfizer, and SAJA Pharma, and received research grants from Astellas and Pfizer. MAA is an internal expert for GSK. JMP, VC, CC, AB, and KM are employees of and hold stocks/shares in GSK. LMG is an employee of Parexel; Parexel received funding from GSK to support the conduct of this study.
Ethical approval and informed consent
No direct subject contact or primary collection of individual human subject data has occurred. Study results are in tabular form and presented as aggregate analyses that omit subject identification; therefore, informed consent, ethics committee, or institutional review board approval were not required.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gravas, S., Manuel-Palacios, J., Chavan, C. et al. Modeling study of the effect of placebo and medical therapy on storage and voiding symptoms, nocturia, and quality of life in men with prostate enlargement at risk for progression. Prostate Cancer Prostatic Dis (2023). https://doi.org/10.1038/s41391-023-00731-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41391-023-00731-w
This article is cited by
-
Impact of medical treatment on storage and voiding LUTS, nocturia, and quality of life in men at risk for progression
Prostate Cancer and Prostatic Diseases (2023)