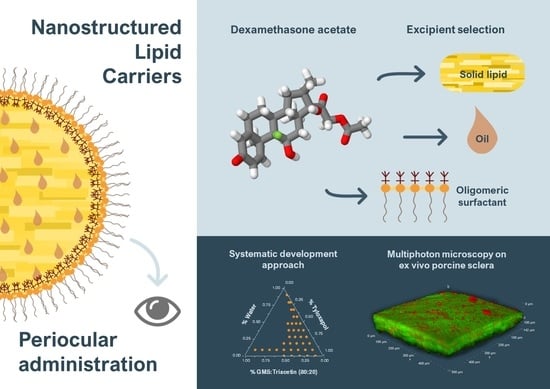
Nanostructured Lipid Carriers for Enhanced Transscleral Delivery of Dexamethasone Acetate: Development, Ex Vivo Characterization and Multiphoton Microscopy Studies
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Lipid Solubility Screening
2.3. Oil-Solid Lipid Mixture Characterization by Differential Scanning Calorimetry
2.4. Surfactant Screening
2.5. Hot-Stage Polarized Light Microscopy
2.6. NLC Preparation and Characterization
2.6.1. Dynamic Light Scattering (DLS)
2.6.2. Nile Red-Loaded NLC
2.6.3. Spectroscopy Studies
2.7. Ex Vivo Swine Ocular Tissues
2.8. Validation of an DexAc-Dex Extraction Method from Porcine Sclera and Choroid
2.9. Permeation and Retention Experiments
2.10. Multiphoton Microscopy Studies
2.11. HPLC Analysis
2.12. Data Processing
2.13. Statistical Analysis
3. Results and Discussion
3.1. Lipid Solubility Screening
3.2. Liquid–Solid Lipid Mixture Characterization by Differential Scanning Calorimetry
3.3. Surfactant Screening
3.4. Hot Stage Polarized Light Microscopy
3.5. NLC Preparation and Characterization
NR Loaded NLC
3.6. Validation of a DexAc Extraction Method from Porcine Sclera and Choroid
3.7. Ex Vivo Ocular Tissues: Permeation and Retention Experiments
3.8. Tissue Distribution of NR through MPM Studies
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fung, A.T.; Tran, T.; Lim, L.L.; Samarawickrama, C.; Arnold, J.; Gillies, M.; Catt, C.; Mitchell, L.; Symons, A.; Buttery, R.; et al. Local delivery of corticosteroids in clinical ophthalmology: A review. Clin. Exp. Ophthalmol. 2020, 48, 366–401. [Google Scholar] [CrossRef] [PubMed]
- Gaballa, S.A.; Kompella, U.B.; Elgarhy, O.; Alqahtani, A.M.; Pierscionek, B.; Alany, R.G.; Abdelkader, H. Corticosteroids in ophthalmology: Drug delivery innovations, pharmacology, clinical applications, and future perspectives. Drug Deliv. Transl. Res. 2021, 11, 866–893. [Google Scholar] [CrossRef] [PubMed]
- Villanueva, J.R.; Villanueva, L.R.; Navarro, M.G. Pharmaceutical technology can turn a traditional drug, dexamethasone into a first-line ocular medicine. A global perspective and future trends. Int. J. Pharm. 2017, 516, 342–351. [Google Scholar] [CrossRef] [PubMed]
- Usayapant, A.; Karana, A.H.; Narurkar, M.M. Effect of 2-hydroxypropyl-β-cyclodextrin on the ocular absorption of dexamethasone and dexamethasone acetate. Pharm. Res. 1991, 8, 1495–1499. [Google Scholar] [CrossRef]
- Leibowitz, H.M.; Kupferman, A.; Stewart, R.H.; Kimbrough, R.L. Evaluation of Dexamethasone Acetate as a Topical Ophthalmic Formulation. Am. J. Ophthalmol. 1978, 86, 418–423. [Google Scholar] [CrossRef]
- Sherif, Z.; Pleyer, U. Corticosteroids in Ophthalmology: Past—Present—Future. Ophthalmologica 2002, 216, 305–315. [Google Scholar] [CrossRef]
- Arakawa, Y.; Hashida, N.; Ohguro, N.; Yamazaki, N.; Onda, M.; Matsumoto, S.; Ohishi, M.; Yamabe, K. Eye-concentrated distribution of dexamethasone carried by sugar-chain modified liposome in experimental autoimmune uveoretinitis mice. Biomed. Res. 2007, 28, 331–334. [Google Scholar] [CrossRef] [Green Version]
- Lee, J.; Goh, U.; Park, J.H.; Park, S.W.; Heo, H. Effective Delivery of Exogenous Compounds to the Optic Nerve by Intravitreal Injection of Liposome. Korean J. Ophthalmol. 2018, 32, 417–423. [Google Scholar] [CrossRef]
- Pescina, S.; Leticia Grolli, L.; Govoni, P.; Padula, C.; Del Favero, E.; Cantù, L.; Santi, P.; Nicoli, S. Ex Vivo Conjunctival Retention and Transconjunctival Transport of Poorly Soluble Drugs Using Polymeric Micelles. Pharmaceutics 2019, 11, 476. [Google Scholar] [CrossRef] [Green Version]
- Di Prima, G.; Licciardi, M.; Bongiovì, F.; Pitarresi, G.; Giammona, G. Inulin-Based Polymeric Micelles Functionalized with Ocular Permeation Enhancers: Improvement of Dexamethasone Permeation/Penetration through Bovine Corneas. Pharmaceutics 2021, 13, 1431. [Google Scholar] [CrossRef]
- Kiss, E.L.; Berkó, S.; Gácsi, A.; Kovács, A.; Katona, G.; Soós, J.; Csányi, E.; Gróf, I.; Harazin, A.; Deli, M.A.; et al. Design and Optimization of Nanostructured Lipid Carrier Containing Dexamethasone for Ophthalmic Use. Pharmaceutics 2019, 11, 679. [Google Scholar] [CrossRef] [Green Version]
- Kumari, S.; Dandamudi, M.; Rani, S.; Behaeghel, E.; Behl, G.; Kent, D.; O’Reilly, N.J.; O’Donovan, O.; McLoughlin, P.; Fitzhenry, L. Dexamethasone-Loaded Nanostructured Lipid Carriers for the Treatment of Dry Eye Disease. Pharmaceutics 2021, 13, 905. [Google Scholar] [CrossRef]
- Coursey, T.G.; Henriksson, J.T.; Marcano, D.C.; Shin, C.S.; Isenhart, L.C.; Ahmed, F.; De Paiva, C.S.; Pflugfelder, S.C.; Acharya, G. Dexamethasone nanowafer as an effective therapy for dry eye disease. J. Control. Release 2015, 213, 168–174. [Google Scholar] [CrossRef] [Green Version]
- Shin, C.S.; Marcano, D.C.; Park, K.; Acharya, G. Application of Hydrogel Template Strategy in Ocular Drug Delivery; Biomedical Nanotechnology; Springer: New York, NY, USA, 2017; Volume 1570, pp. 279–285. ISBN 1493968386. [Google Scholar]
- Rodríguez Villanueva, J.; Bravo Osuna, I.; Herrero Vanrell, R.; Molina Martínez, I.T.; Guzmán Navarro, M. Optimising the controlled release of dexamethasone from a new generation of PLGA-based microspheres intended for intravitreal administration. Eur. J. Pharm. Sci. 2016, 92, 287–297. [Google Scholar] [CrossRef]
- Xu, J.; Wang, Y.; Li, Y.; Yang, X.; Zhang, P.; Hou, H.; Shi, Y.; Song, C. Inhibitory Efficacy of Intravitreal Dexamethasone Acetate-Loaded PLGA Nanoparticles on Choroidal Neovascularization in a Laser-Induced Rat Model. J. Ocul. Pharmacol. Ther. 2007, 23, 527–539. [Google Scholar] [CrossRef]
- Gómez-Gaete, C.; Fattal, E.; Silva, L.; Besnard, M.; Tsapis, N. Dexamethasone acetate encapsulation into Trojan particles. J. Control. Release 2008, 128, 41–49. [Google Scholar] [CrossRef]
- Li, X.; Müller, R.H.; Keck, C.M.; Bou-Chacra, N.A. Mucoadhesive dexamethasone acetate-polymyxin B sulfate cationic ocular nanoemulsion—Novel combinatorial formulation concept. Pharmazie 2016, 71, 327–333. [Google Scholar] [CrossRef]
- Da Silva, G.R.; Lima, T.H.; Fernandes-Cunha, G.M.; Oréfice, R.L.; Da Silva-Cunha, A.; Zhao, M.; Behar-Cohen, F. Ocular biocompatibility of dexamethasone acetate loaded poly(ɛ-caprolactone) nanofibers. Eur. J. Pharm. Biopharm. 2019, 142, 20–30. [Google Scholar] [CrossRef]
- Rocha, E.D.; Ferreira, M.R.S.; dos Santos Neto, E.; Barbosa, E.J.; Löbenberg, R.; Lourenço, F.R.; Bou-Chacra, N. Enhanced In Vitro Antimicrobial Activity of Polymyxin B–Coated Nanostructured Lipid Carrier Containing Dexamethasone Acetate. J. Pharm. Innov. 2021, 16, 125–135. [Google Scholar] [CrossRef]
- Khiev, D.; Mohamed, Z.A.; Vichare, R.; Paulson, R.; Bhatia, S.; Mohapatra, S.; Lobo, G.P.; Valapala, M.; Kerur, N.; Passaglia, C.L.; et al. Emerging Nano-Formulations and Nanomedicines Applications for Ocular Drug Delivery. Nanomaterials 2021, 11, 173. [Google Scholar] [CrossRef]
- Alvarez-Trabado, J.; Diebold, Y.; Sanchez, A. Designing lipid nanoparticles for topical ocular drug delivery. Int. J. Pharm. 2017, 532, 204–217. [Google Scholar] [CrossRef] [PubMed]
- González-Fernández, F.M.; Bianchera, A.; Gasco, P.; Nicoli, S.; Pescina, S. Lipid-Based Nanocarriers for Ophthalmic Administration: Towards Experimental Design Implementation. Pharmaceutics 2021, 13, 447. [Google Scholar] [CrossRef] [PubMed]
- Bonilla, L.; Espina, M.; Severino, P.; Cano, A.; Ettcheto, M.; Camins, A.; García, M.L.; Souto, E.B.; Sánchez-López, E. Lipid Nanoparticles for the Posterior Eye Segment. Pharmaceutics 2021, 14, 90. [Google Scholar] [CrossRef] [PubMed]
- Müller, R.H.; Radtke, M.; Wissing, S.A. Solid lipid nanoparticles (SLN) and nanostructured lipid carriers (NLC) in cosmetic and dermatological preparations. Adv. Drug Deliv. Rev. 2002, 54, S131–S155. [Google Scholar] [CrossRef]
- Sánchez-López, E.; Espina, M.; Doktorovova, S.; Souto, E.B.; García, M.L. Lipid nanoparticles (SLN, NLC): Overcoming the anatomical and physiological barriers of the eye—Part II—Ocular drug-loaded lipid nanoparticles. Eur. J. Pharm. Biopharm. 2017, 110, 58–69. [Google Scholar] [CrossRef]
- Chemical Abstracts Service Scifinder-n: Dexamethasone Acetate CAS Registry Number: 1177-87-3. Available online: https://scifinder-n.cas.org/searchDetail/substance/63ce9c5aa8718f29bd45c6b4/substanceDetails (accessed on 30 November 2022).
- National Center for Biotechnology Information PubChem Compound Summary for CID 5743, Dexamethasone. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/Dexamethasone (accessed on 28 October 2022).
- Rathod, V.R.; Shah, D.A.; Dave, R.H. Systematic implementation of quality-by-design (QbD) to develop NSAID-loaded nanostructured lipid carriers for ocular application: Preformulation screening studies and statistical hybrid-design for optimization of variables. Drug Dev. Ind. Pharm. 2020, 46, 443–455. [Google Scholar] [CrossRef]
- Cavalli, R.; Caputo, O.; Gasco, M.R. Preparation and characterization of solid lipid nanospheres containing paclitaxel. Eur. J. Pharm. Sci. 2000, 10, 305–309. [Google Scholar] [CrossRef]
- Sandri, G.; Motta, S.; Bonferoni, M.C.; Brocca, P.; Rossi, S.; Ferrari, F.; Rondelli, V.; Cantù, L.; Caramella, C.; Del Favero, E. Chitosan-coupled solid lipid nanoparticles: Tuning nanostructure and mucoadhesion. Eur. J. Pharm. Biopharm. 2017, 110, 13–18. [Google Scholar] [CrossRef]
- Jarvinen, T.; Jarvinen, K. Prodrugs for improved ocular drug delivery. Adv. Drug Deliv. Reviews. 1996, 19, 203–224. [Google Scholar] [CrossRef]
- Dai, W.; Dong, L.C.; Li, S.; Pollock-Dove, C.; Chen, J.; Mansky, P.; Eichenbaum, G. Parallel screening approach to identify solubility-enhancing formulations for improved bioavailability of a poorly water-soluble compound using milligram quantities of material. Int. J. Pharm. 2007, 336, 1–11. [Google Scholar] [CrossRef]
- Kovačević, A.B.; Müller, R.H.; Keck, C.M. Formulation development of lipid nanoparticles: Improved lipid screening and development of tacrolimus loaded nanostructured lipid carriers (NLC). Int. J. Pharm. 2020, 576, 118918. [Google Scholar] [CrossRef]
- IOI Oleo GmbH O/W Emusifiers: Imwitor® 491. Available online: https://www.ioioleo.de/produkte/pharma/imwitor-491/ (accessed on 3 November 2022).
- IOI Oleo GmbH O/W Emusifiers: Imwitor® 900 K. Available online: https://www.ioioleo.de/produkte/pharma/imwitor-900-k/ (accessed on 3 November 2022).
- Krog, N.J.; Sparsø, F.V. Food Emulsifiers: Their Chemical and Physical Properties; Friberg, S., Larsson, K., Eds.; Food Emulsions 3rd ed., rev. and expanded; Marcel Dekker: New York, NY, USA, 1997; p. 582. [Google Scholar]
- Fiume, M.Z. Final Report on the Safety Assessment of Triacetin. Int. J. Toxicol. 2003, 22, 1–10. [Google Scholar] [CrossRef]
- Himawan, C.; Starov, V.M.; Stapley, A.G.F. Thermodynamic and kinetic aspects of fat crystallization. Adv. Colloid Interface Sci. 2006, 122, 3–33. [Google Scholar] [CrossRef]
- Salminen, H.; Helgason, T.; Aulbach, S.; Kristinsson, B.; Kristbergsson, K.; Weiss, J. Influence of co-surfactants on crystallization and stability of solid lipid nanoparticles. J. Colloid Interface Sci. 2014, 426, 256–263. [Google Scholar] [CrossRef]
- Jenning, V.; Schäfer-Korting, M.; Gohla, S. Vitamin A-loaded solid lipid nanoparticles for topical use: Drug release properties. J. Control. Release 2000, 66, 115–126. [Google Scholar] [CrossRef]
- Windbergs, M.; Strachan, C.J.; Kleinebudde, P. Understanding the solid-state behaviour of triglyceride solid lipid extrudates and its influence on dissolution. Eur. J. Pharm. Biopharm. 2009, 71, 80–87. [Google Scholar] [CrossRef]
- Windbergs, M.; Strachan, C.J.; Kleinebudde, P. Investigating the Principles of Recrystallization from Glyceride Melts. AAPS PharmSciTech 2009, 10, 1224–1233. [Google Scholar] [CrossRef] [Green Version]
- Ali, H.; Singh, S.K.; Verma, P.R.P. Preformulation and physicochemical interaction study of furosemide with different solid lipids. J. Pharm. Investig. 2015, 45, 385–398. [Google Scholar] [CrossRef]
- Goto, M.; Kozawa, K.; Uchida, T. The Crystal Structure of the β′1 Form of Optically Active α-Monostearin. Bull. Chem. Soc. Jpn. 1988, 61, 1434–1436. [Google Scholar] [CrossRef] [Green Version]
- Yajima, T.; Itai, S.; Takeuchi, H.; Kawashima, Y. Determination of Optimum Processing Temperature for Transformation of Glyceryl Monostearate. Chem. Pharm. Bull. 2002, 50, 1430–1433. [Google Scholar] [CrossRef] [Green Version]
- Bertoni, S.; Passerini, N.; Albertini, B. Liquid Lipids Act as Polymorphic Modifiers of Tristearin-Based Formulations Produced by Melting Technologies. Pharmaceutics 2021, 13, 1089. [Google Scholar] [CrossRef] [PubMed]
- Pattarino, F.; Bettini, R.; Foglio Bonda, A.; Della Bella, A.; Giovannelli, L. Polymorphism and kinetic behavior of binary mixtures of triglycerides. Int. J. Pharm. 2014, 473, 87–94. [Google Scholar] [CrossRef] [PubMed]
- Teeranachaideekul, V.; Boonme, P.; Souto, E.B.; Müller, R.H.; Junyaprasert, V.B. Influence of oil content on physicochemical properties and skin distribution of Nile red-loaded NLC. J. Control. Release 2008, 128, 134–141. [Google Scholar] [CrossRef] [PubMed]
- Gasco, M.R. Method for Producing Solid Lipid Microspheres Having A Narrow Size Distribution. U.S. Patent 5250236A, 5 October 1993. [Google Scholar]
- Haider, M.; Abdin, S.M.; Kamal, L.; Orive, G. Nanostructured Lipid Carriers for Delivery of Chemotherapeutics: A Review. Pharmaceutics 2020, 12, 288. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Regev, O.; Zana, R. Aggregation Behavior of Tyloxapol, a Nonionic Surfactant Oligomer, in Aqueous Solution. J. Colloid Interface Sci. 1999, 210, 8–17. [Google Scholar] [CrossRef]
- Zana, R. Dimeric and oligomeric surfactants. Behavior at interfaces and in aqueous solution: A review. Adv. Colloid Interface Sci. 2002, 97, 205–253. [Google Scholar] [CrossRef]
- Jiao, J. Polyoxyethylated nonionic surfactants and their applications in topical ocular drug delivery. Adv. Drug Deliv. Rev. 2008, 60, 1663–1673. [Google Scholar] [CrossRef]
- Juretić, M.; Cetina-Čižmek, B.; Filipović-Grčić, J.; Hafner, A.; Lovrić, J.; Pepić, I. Biopharmaceutical evaluation of surface active ophthalmic excipients using in vitro and ex vivo corneal models. Eur. J. Pharm. Sci. 2018, 120, 133–141. [Google Scholar] [CrossRef]
- Cerqueira, M.A.; Fasolin, L.H.; Picone, C.S.F.; Pastrana, L.M.; Cunha, R.L.; Vicente, A.A. Structural and mechanical properties of organogels: Role of oil and gelator molecular structure. Food Res. Int. 2017, 96, 161–170. [Google Scholar] [CrossRef] [Green Version]
- McClements, D.J. Nanoemulsions versus microemulsions: Terminology, differences, and similarities. Soft Matter 2012, 8, 1719–1729. [Google Scholar] [CrossRef]
- Zetzl, A.; Ollivon, M.; Marangoni, A. A Coupled Differential Scanning Calorimetry and X-ray Study of the Mesomorphic Phases of Monostearin and Stearic Acid in Water. Cryst. Growth Des. 2009, 9, 3928–3933. [Google Scholar] [CrossRef]
- Morley, W.G.; Tiddy, G.J.T. Phase behaviour of monoglyceride/water systems. Faraday Trans. 1993, 89, 2823–2831. [Google Scholar] [CrossRef]
- Kucherak, O.A.; Oncul, S.; Darwich, Z.; Yushchenko, D.A.; Arntz, Y.; Didier, P.; Mély, Y.; Klymchenko, A.S. Switchable Nile Red-Based Probe for Cholesterol and Lipid Order at the Outer Leaflet of Biomembranes. J. Am. Chem. Soc. 2010, 132, 4907–4916. [Google Scholar] [CrossRef]
- Greenspan, P.; Fowler, S.D. Spectrofluorometric studies of the lipid probe, nile red. J. Lipid Res. 1985, 26, 781–789. [Google Scholar] [CrossRef]
- Boldrini, B.; Cavalli, E.; Painelli, A.; Terenziani, F. Polar Dyes in Solution: A Joint Experimental and Theoretical Study of Absorption and Emission Band Shapes. J. Phys. Chem. A 2002, 106, 6286–6294. [Google Scholar] [CrossRef]
- Nakano, M.; Lockhart, C.M.; Kelly, E.J.; Rettie, A.E. Ocular cytochrome P450s and transporters: Roles in disease and endobiotic and xenobiotic disposition. Drug Metab. Rev. 2014, 46, 247–260. [Google Scholar] [CrossRef] [Green Version]
- Heikkinen, E.M.; Del Amo, E.M.; Ranta, V.; Urtti, A.; Vellonen, K.; Ruponen, M. Esterase activity in porcine and albino rabbit ocular tissues. Eur. J. Pharm. Sci. 2018, 123, 106–110. [Google Scholar] [CrossRef]
- Loch, C.; Zakelj, S.; Kristl, A.; Nagel, S.; Guthoff, R.; Weitschies, W.; Seidlitz, A. Determination of permeability coefficients of ophthalmic drugs through different layers of porcine, rabbit and bovine eyes. Eur. J. Pharm. Sci. 2012, 47, 131–138. [Google Scholar] [CrossRef]
- Pescina, S.; Govoni, P.; Antopolsky, M.; Murtomaki, L.; Padula, C.; Santi, P.; Nicoli, S. Permeation of Proteins, Oligonucleotide and Dextrans Across Ocular Tissues: Experimental Studies and a Literature Update. J. Pharm. Sci. 2015, 104, 2190–2202. [Google Scholar] [CrossRef]
- Pescina, S.; Padula, C.; Santi, P.; Nicoli, S. Effect of formulation factors on the trans-scleral iontophoretic and post-iontophoretic transports of a 40 kDa dextran in vitro. Eur. J. Pharm. Sci. 2011, 42, 503–508. [Google Scholar] [CrossRef]
- Grimaudo, M.A.; Pescina, S.; Padula, C.; Santi, P.; Concheiro, A.; Alvarez-Lorenzo, C.; Nicoli, S. Poloxamer 407/TPGS Mixed Micelles as Promising Carriers for Cyclosporine Ocular Delivery. Mol. Pharm. 2018, 15, 571–584. [Google Scholar] [CrossRef] [PubMed]
- Ghezzi, M.; Ferraboschi, I.; Delledonne, A.; Pescina, S.; Padula, C.; Santi, P.; Sissa, C.; Terenziani, F.; Nicoli, S. Cyclosporine-loaded micelles for ocular delivery: Investigating the penetration mechanisms. J. Control. Release 2022, 349, 744–755. [Google Scholar] [CrossRef] [PubMed]
- Webb, W.W.; Zipfel, W.R.; Williams, R.M. Nonlinear magic: Multiphoton microscopy in the biosciences. Nat. Biotechnol. 2003, 21, 1369–1377. [Google Scholar] [CrossRef]
- Nicoli, S.; Ferrari, G.; Quarta, M.; Macaluso, C.; Govoni, P.; Dallatana, D.; Santi, P. Porcine sclera as a model of human sclera for in vitro transport experiments: Histology, SEM, and comparative permeability. Mol. Vis. 2009, 15, 259–266. [Google Scholar]
- Murtomäki, L.; Vainikka, T.; Pescina, S.; Nicoli, S. Drug Adsorption on Bovine and Porcine Sclera Studied with Streaming Potential. J. Pharm. Sci. 2013, 102, 2264–2272. [Google Scholar] [CrossRef]
- Ray, A.; Das, S.; Chattopadhyay, N. Aggregation of Nile Red in Water: Prevention through Encapsulation in β-Cyclodextrin. ACS Omega 2019, 4, 15–24. [Google Scholar] [CrossRef] [Green Version]
- Golini, C.M.; Williams, B.W.; Foresman, J.B. Further solvatochromic, thermochromic, and theoretical studies on Nile Red. J. Fluoresc. 1998, 8, 395–404. [Google Scholar] [CrossRef]
- Terenziani, F.; Painelli, A.; Comoretto, D. Solvation Effects and Inhomogeneous Broadening in Optical Spectra of Phenol Blue. J. Phys. Chem. A 2000, 104, 11049–11054. [Google Scholar] [CrossRef]










| Phase Diagram Region | Code | Lipid Mix % (GMS: Triacetin 60:40) | Surfactant % (Tyloxapol) | Water % | Warm Microemulsion | Redispersed 1:20 Product | |
|---|---|---|---|---|---|---|---|
| Transparent | Isotropic | ||||||
| Low water | L1 | 37.3 | 24.8 | 37.9 | Y | N | >1 mm pellets |
| L2 | 12.4 | 49.7 | 37.9 | Y | Y | >1 mm pellets | |
| Isotropic | Iso1 | 11.1 | 23.2 | 65.7 | Y | Y | Slightly bluish, milky |
| Iso2 | 10.1 | 29.9 | 60 | Y | Y | Slightly bluish, milky | |
| Iso3 | 12 | 30.3 | 57.7 | Y | Y | Slightly bluish, milky | |
| High water | H1 | 5 | 5 | 90 | N | Y | Slightly bluish, milky |
| DexAc-NLC (230 μg/mL = 529.3 μM) (n = 8) | Dex-NLC (141 μg/mL = 359.9 μM) (n = 4) | ||
|---|---|---|---|
| Sample | Tissue | DexAc+Dex (nmol/g tissue) | Dex (nmol/g tissue) |
| S | S | 139.9 ± 35.6 | Not studied |
| S | 98.9 ± 19.9 | 83.4 ± 8.1 | |
| SCh | Ch | 30.9 ± 9.3 | 80.7 ± 12.6 |
| SCh | 92.8 ± 19.0 | 83.3 ± 8.3 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
González-Fernández, F.M.; Delledonne, A.; Nicoli, S.; Gasco, P.; Padula, C.; Santi, P.; Sissa, C.; Pescina, S. Nanostructured Lipid Carriers for Enhanced Transscleral Delivery of Dexamethasone Acetate: Development, Ex Vivo Characterization and Multiphoton Microscopy Studies. Pharmaceutics 2023, 15, 407. https://doi.org/10.3390/pharmaceutics15020407
González-Fernández FM, Delledonne A, Nicoli S, Gasco P, Padula C, Santi P, Sissa C, Pescina S. Nanostructured Lipid Carriers for Enhanced Transscleral Delivery of Dexamethasone Acetate: Development, Ex Vivo Characterization and Multiphoton Microscopy Studies. Pharmaceutics. 2023; 15(2):407. https://doi.org/10.3390/pharmaceutics15020407
Chicago/Turabian StyleGonzález-Fernández, Felipe M., Andrea Delledonne, Sara Nicoli, Paolo Gasco, Cristina Padula, Patrizia Santi, Cristina Sissa, and Silvia Pescina. 2023. "Nanostructured Lipid Carriers for Enhanced Transscleral Delivery of Dexamethasone Acetate: Development, Ex Vivo Characterization and Multiphoton Microscopy Studies" Pharmaceutics 15, no. 2: 407. https://doi.org/10.3390/pharmaceutics15020407