The Role of Parental Concerns in the Recognition of Sepsis in Children: A Literature Review
- 1Paediatric Critical Care Research Group, Child Health Research Centre and Faculty of Medicine, The University of Queensland, Brisbane, QLD, Australia
- 2Paediatric Intensive Care Unit, Queensland Children's Hospital, Children's Health Queensland, Brisbane, QLD, Australia
- 3School of Nursing, The University of Queensland, Brisbane, QLD, Australia
- 4Faculty of Health and Human Sciences, School of Nursing and Midwifery, University of Plymouth, Plymouth, United Kingdom
- 5Department of Paediatrics, Bern University Hospital, Inselspital, University of Bern, Bern, Switzerland
Background: Sepsis is a time critical disease and outcomes strongly depend on time to initiation of appropriate treatment in hospital. A range of studies have assessed sepsis recognition in hospital settings, whereas little is known about sepsis recognition in the community. The decision-making of parents in seeking medical care may substantially impact survival of children with sepsis. An improved understanding of the parental perspective in recognizing sepsis is urgently needed to inform the design of education campaigns and consideration of using parental concerns as a trigger in sepsis screening tools.
Aim: To review the literature on parental concerns in the diagnosis of sepsis in children.
Methods: A literature review on parental concerns in pediatric sepsis was performed accessing publications in PubMed, CINAHL and Medline published between 1990 and 2018. In addition, we compared guidelines and online institutional sepsis recognition tools and assessed whether parental concerns were used for screening.
Results: Out of 188 articles reviewed, 11 met the criteria. One article was found prospectively assessing the diagnostic performance of parental concern in children evaluated for infection, indicating high positive (16.4) and negative likelihood ratio (0.23) for sepsis/meningitis in presence of parental concerns. The role of parental concern was listed as a sign assisting recognition of sepsis in four studies reporting original data, and six reviews commented on parental concern listed as a factor upon diagnosis of sepsis. When comparing selected examples of institutional sepsis pathways available online, parental concern was variably listed as a criterion to prompt evaluation for sepsis.
Conclusions: Despite some guidelines emphasizing the role of parental concern in recognizing sepsis, there is a paucity of data in the field. An improved understanding of whether parental concerns adds diagnostic value to sepsis recognition at acceptable sensitivity and specificity is urgently needed. Future prospective studies should assess whether including parental concerns in sepsis screening tools benefits the assessment resulting in early diagnosis and treatment of children with sepsis.
Introduction
Sepsis represents a leading cause of global childhood mortality (1–3). In response to the recent resolution by the World Health Organization recognizing sepsis as a priority in healthcare(4, 5), several national and regional healthcare systems have implemented sepsis pathways to improve recognition and early treatment of sepsis in hospital settings (6). Sepsis in children remains a time critical disease and the majority of deaths and multi-organ dysfunction occur within the first 48 h of admission (7–10), highlighting the relevance of timely intervention. While interventional trials in children and adults have failed to result in reduced mortality (11–13), observational studies have consistently indicated that time to sepsis treatment strongly impacts on sepsis survival (14–18).
Physiologic criteria, early warning tools, and electronic health-record based trigger tools have been reported to improve the recognition of children with severe bacterial infections, and sepsis (19–23). Currently used sepsis recognition tools yield high sensitivity but mostly at the expense of poor specificity, given that most infectious illnesses in children manifest with fever, tachycardia, and tachypnea (24, 25). Inaccurate sepsis diagnosis may lead to unnecessary antibiotic therapy, hospitalization, and missed alternative diagnoses. The importance of balancing the need for rapid sepsis recognition vs. potential adverse effects on patients, healthcare resource use and antimicrobial resistance related to overtreatment is becoming increasingly recognized (26, 27) implicating an urgent need for rigorous studies on sepsis recognition.
Importantly, sepsis starts most commonly in the community and the decision and timing of parents in seeking medical care for children is likely to contribute to severity upon presentation and sepsis-related outcomes. Root cause analyses after fatal sepsis outcomes in children often report on recurrent presentations to hospital (16) and anecdotal data reveals parents in such cases often indicated concerns that “this disease is different” suggesting parents may have sensed the potential severity of the disease prior to the recognition of sepsis by clinicians. Increasing parental education has been demonstrated to reduce infant mortality due to infections in low income settings (28, 29). Yet the potential value of including parental assessment in discriminating children with mild infections from sepsis has received little attention. The capacity of parents to assess whether a disease presents differently to previous common febrile illnesses could potentially result in improved diagnostic accuracy of sepsis assessment.
We therefore aimed to review the literature on parental concerns in recognizing sepsis in children, with particular focus on studies reporting on diagnostic accuracy. In addition, we searched whether online available institutional sepsis screening tools include parental concern as a trigger for recognition or escalation.
Methods
Objectives
To review the literature on parental concern in the diagnosis of sepsis in children.
Eligibility Criteria
The Population-Intervention-Control-Outcome-Study design (PICOS) approach was applied and guided the literature review focusing on: (P) pediatric age groups of <18 years of age; with (I) parental concern utilized as an assessment tool; (C) control consisting of standard diagnostic approach without including parental concern as a diagnostic tool; (O) diagnosis of sepsis and diagnostic accuracy of sepsis diagnosis as outcomes; and (S) both quantitative and qualitative original research, case reports, editorials/viewpoints, guidelines, and reviews included.
Search Strategy
Three strategies for data collection were utilized: First, a comprehensive search for published literature through international databases was performed. Second, we manually searched reference lists from articles identified through the database search. Third, we considered additional articles identified as relevant by the authors. Publications were accessed in three literature databases: MEDLINE, CINAHL and PUBMED. Search terms used included: “Concern” OR “worry” OR “fear,” AND “infant” OR “pediatric” OR “pediatric” OR “child” OR “neonate” OR “childhood,” AND “sepsis” OR “septic” OR “severe sepsis” OR “septic shock” OR “bacteremia” OR ”severe infection” OR “systemic inflammatory response syndrome,” AND “parent” OR “family” OR “caregiver” OR “mother” OR “father” (Supplementary Table 1).
Studies were considered if they were published as full text in the English language between January 1st 1990 and September 1st 2018. Duplicate references were removed manually. Original research, case reports, editorials/viewpoints, guidelines, and reviews were considered. The initial title and abstract screen for further review was conducted by two authors (AH, LS). Articles for full text review were selected by applying the search terms to the titles and abstracts of articles.
We then performed a two-stage review of full text articles. In the first stage, we searched articles that provided original data on parental concerns in pediatric sepsis. We considered publications that defined sepsis, including septic shock and severe sepsis, according to the 2005 International Pediatric Sepsis Definition Conference (30), the American College of Chest Physicians (31), or adaptations from the recent Sepsis-3 criteria (24, 32). We included articles which reported on parental concern for children below 18 years as part of diagnostic assessment for patients presenting with sepsis or severe infection. Given the low yield of only one article meeting the PICOS criteria, we included studies reporting on severe infections, and bacteraemia. In the second stage, we searched full-text articles that reported on the use or importance of parental concerns in pediatric sepsis without providing original data.
Articles were excluded if full text was unavailable in English was unavailable. All full text articles identified underwent review by two independent investigators (AH, LJS). Clarification for inclusion was resolved by discussion. Due to the paucity of data reporting on diagnostic accuracy, sensitivity, specificity, and negative and positive predictive value in relation to parental concern, a meta-analysis could not be performed.
Inclusion of Parental Concerns in Pediatric Sepsis Pathways
In order to compare examples of pediatric sepsis pathways in relation to utilization of parental concern, we selected published or online accessible pediatric sepsis pathways available in English language which were published in the past 5 years (date of updated search September 1st 2018). We limited the search to published international pediatric sepsis guidelines, and to pathways of jurisdictions which had previously reported on state- or nationwide sepsis campaigns (14, 33–35). This resulted in examples of pathways from three continents (North America, Europe and Oceania). These examples were selected to show different approaches to the recognition of sepsis in children. Pathways were then searched for the presence of a field listing parental concern as a risk factor or warning sign for sepsis. We considered terms such as “concern” (OR “worry” OR “fear”), and “parent” (OR “family” OR “caregiver” OR “mother/maternal” OR “father/paternal”).
Results
Study Selection
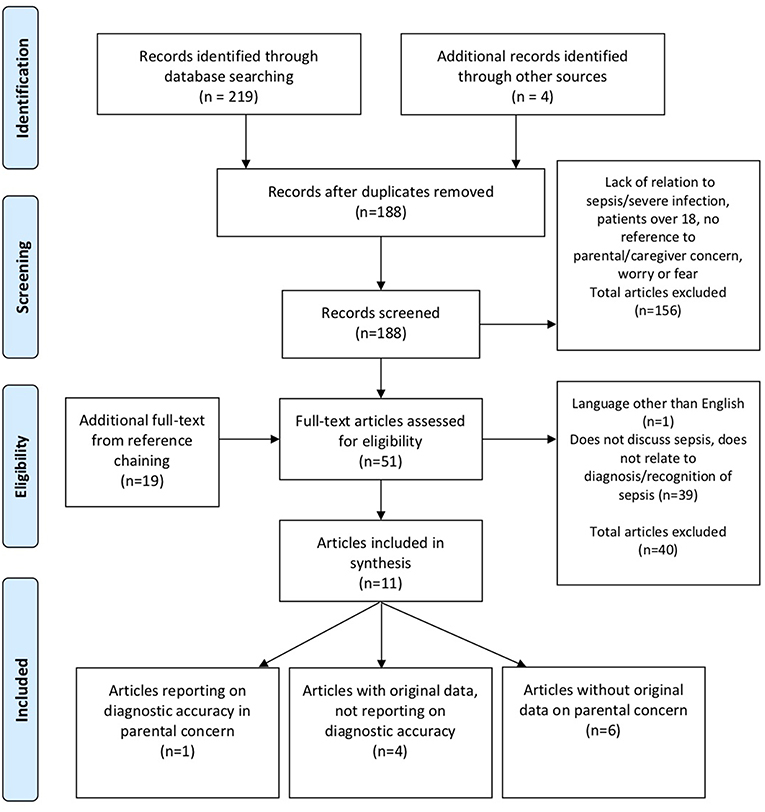
The search of the databases yielded 219 results and an additional four articles through other sources. After exclusion of duplicates and records in languages other than English, 188 remained (Figure 1). Abstract review by two assessors excluded 156 articles as the records were not reporting on sepsis diagnosis pertinent to parental concerns and children. Reference chaining identified a further 19 articles. In total, 51 Articles were selected for full-text review by two assessors. Of these, a further 40 were excluded because of one study in non-English language (36), and 39 because they did not report on parental concern in relation to recognition of sepsis. We included 11 articles in the review, of which five reported original data, out of which one only reported on diagnostic accuracy. Six articles were reviews reporting on parental concern without original data.
Study Characteristics
Only one study reported original data on diagnostic accuracy of parental assessment in relation to sepsis (Table 1). Van den Bruel performed a prospective multicenter study in primary care settings including 3981 children which presented to 121 physicians (General practitioners, pediatricians, and emergency physicians) (37). The study was designed to assess diagnostic accuracy of several clinical features including physiological variables, clinician perception that “something is wrong,” and parental concern. Parental concern was defined as the parental perception or statement that the “disease is different.” Classification and regression tree analysis was performed to define the best performing criteria and criteria combination for clinical practice. Out of the 3981 included children (mean age 5.0 years, range = 0.02–16.9 years), 31 (0.78%) had a serious bacterial infection and 9 (0.22%) were diagnosed with sepsis and/or meningitis. Presence of parental concern that the disease is different was associated with an odds ratio (OR) of 70.5 (95%-CI 14.5 to 341.4) for sepsis/meningitis in the decision tree model, and a sensitivity of 77.8%, specificity of 95.1%, positive predictive value (PPV) of 3.6%, negative predictive value (NPV) of 100%, positive likelihood ratio (PLR) of 16.4, and negative likelihood ratio (NLR) of 0.23. In comparison, the assessment by the treating physician that “something is wrong” was associated with sepsis with an OR of 268 (33–2,163) and a sensitivity of 88.9% and specificity of 97.1%. The sensitivity of parental concern to capture any serious bacterial infection was 46.4%, and the according specificity was 96.8%, PPV 9.5%, NPV 99.6%, PLR 14.35 and NLR 0.55, respectively.
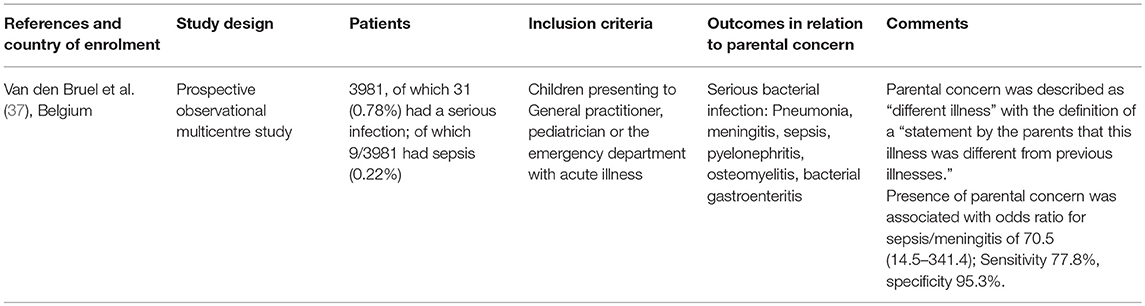
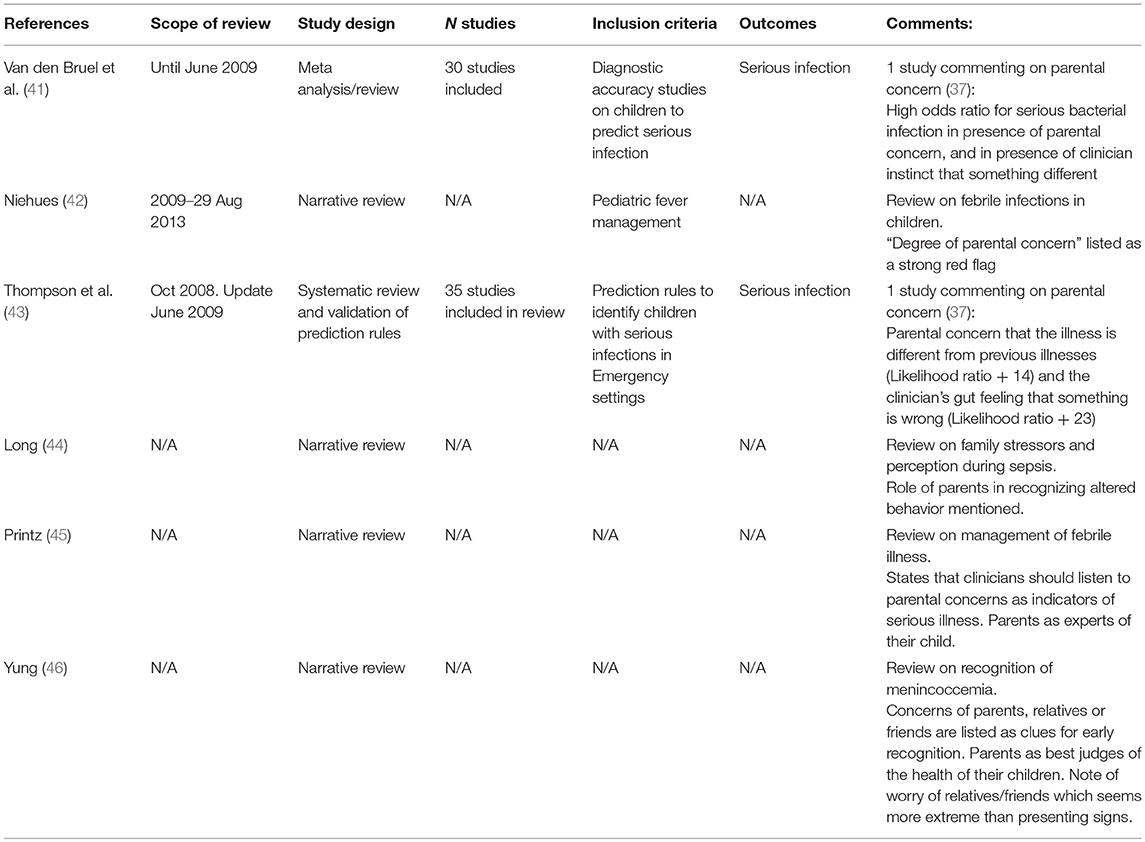
Table 1. Original studies reporting on diagnostic accuracy of parental concern in diagnosis of severe infection and sepsis.
Four further studies reported original data, however none of these reported on diagnostic accuracy (Table 2). A secondary analysis of the 2007 Van den Bruel study investigated the role of clinician‘s gut feeling that something is wrong in the patients. Parental concern was identified as the strongest factor increasing the likelihood of clinician‘s gut feeling that something is wrong (univariate OR 26.93; 9.02 to 80.41, multivariate OR 36.26; 12.28 to 107.07) (38). However, the secondary analysis did not comment on the predictive accuracy of parental concern in relation to serious bacterial infection. Another study by Van den Bruel et al. (39) performed qualitative interviews with families and practitioners of 18 children hospitalized for severe bacterial infection with a mean age of 2.5 years (range 14 days to 11 years). Parents reported findings such as “The moment he was sitting on my lap and suddenly collapsed, I was really frightened and came here immediately. At that moment I just knew it was more than just a cold.” Van den Bruel et al. (39) referring to a 2-year-old child with sepsis. The authors concluded that parents have a high accuracy in describing the behavior of their children and to assess how the current behavior compares with normal behavior, and with behavior during previous illnesses. Another study performed qualitative interviews with General Practitioners to assess their attitudes in relation to recognizing children with meningitis and meningococcal septicemia (40). No patient data was assessed. Parental concern, and maternal “instinct” that the child was not right were mentioned as sometimes representing the only clues to a severe disease. Another study interviewed 95 parents from primary care inner city settings and performed focus groups to explore parental concerns about acute pediatric illness (41). Fever, cough and risk of meningitis emerged as key areas of concern. Sepsis was not specifically mentioned, however parents reported their fear that they may fail to recognize a life-threatening condition.
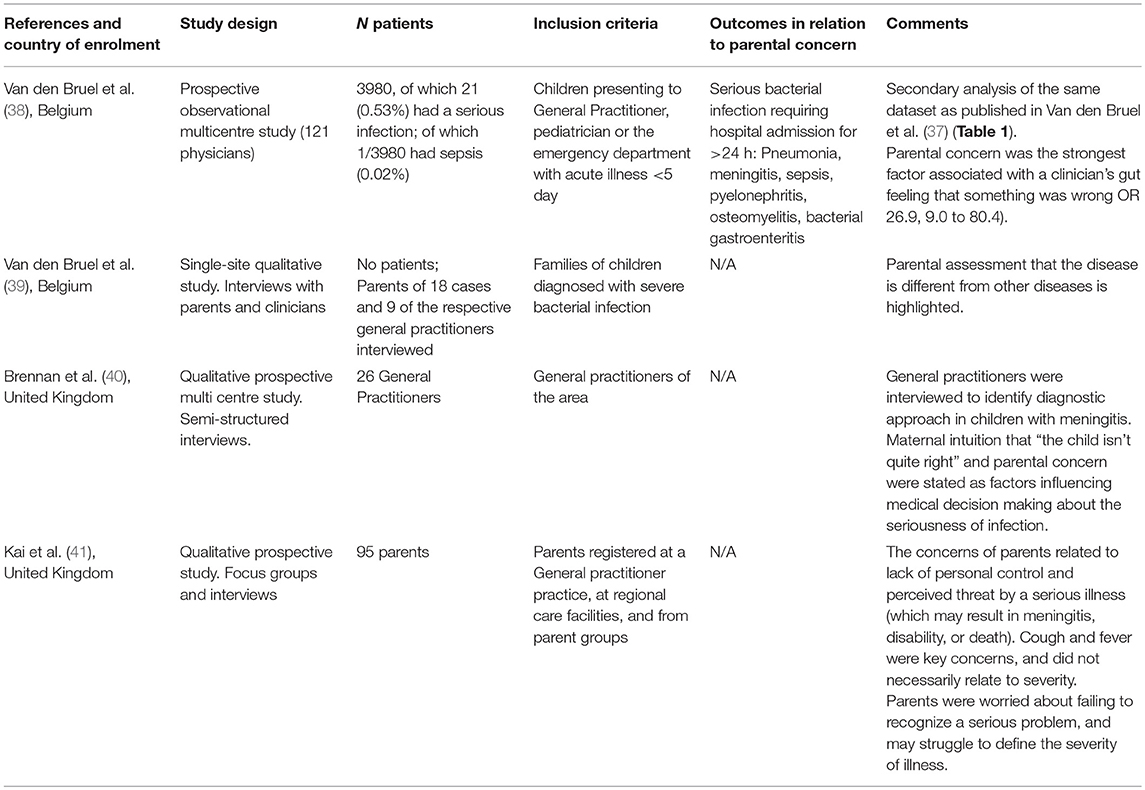
Table 2. Original studies reporting on parental concern as diagnostic measure of sepsis, not reporting on diagnostic accuracy of parental concern.
Six review articles were included which reported on parental concern in diagnosis of sepsis (Table 3). Two systematic reviews analyzed the findings from 36, and 35 articles, respectively, including 30 articles reporting on clinical features in relation to diagnosis of serious infection in children in developed countries (43, 47). The original study of Van den Bruel was the only study in both reviews which reported on parental concern to assist in the diagnosis of serious infection in children (37). While clinician‘s gut feeling that something was wrong performed better than parental concerns, the diagnostic accuracy of both parental concern and clinician‘s gut feeling outperformed most routinely used physiological or observational data in other studies. Four further non-systematic reviews and narratives were identified which listed parental concerns as a feature of children presenting with life-threatening infections or sepsis (42, 44–46). These articles did not use any original data to justify this but rather commented on the value of parental concern in the perspective by the authors.
Examples of Use of Parental Concern in Guidelines and Institutional Pathways
We assessed published and online available international pediatric sepsis guidelines pathways and guidelines in relation to the role of parental concern in the recognition of sepsis. In addition, we selected examples of published and online available institutional pathways designed for the recognition of sepsis in children (Table 4). The selection was limited to jurisdictions which has previously published on the state- or nation-wide implementation of sepsis bundles, specifically the United Kingdom, New York State in the United States, and New South Wales in Australia (14, 33–35).
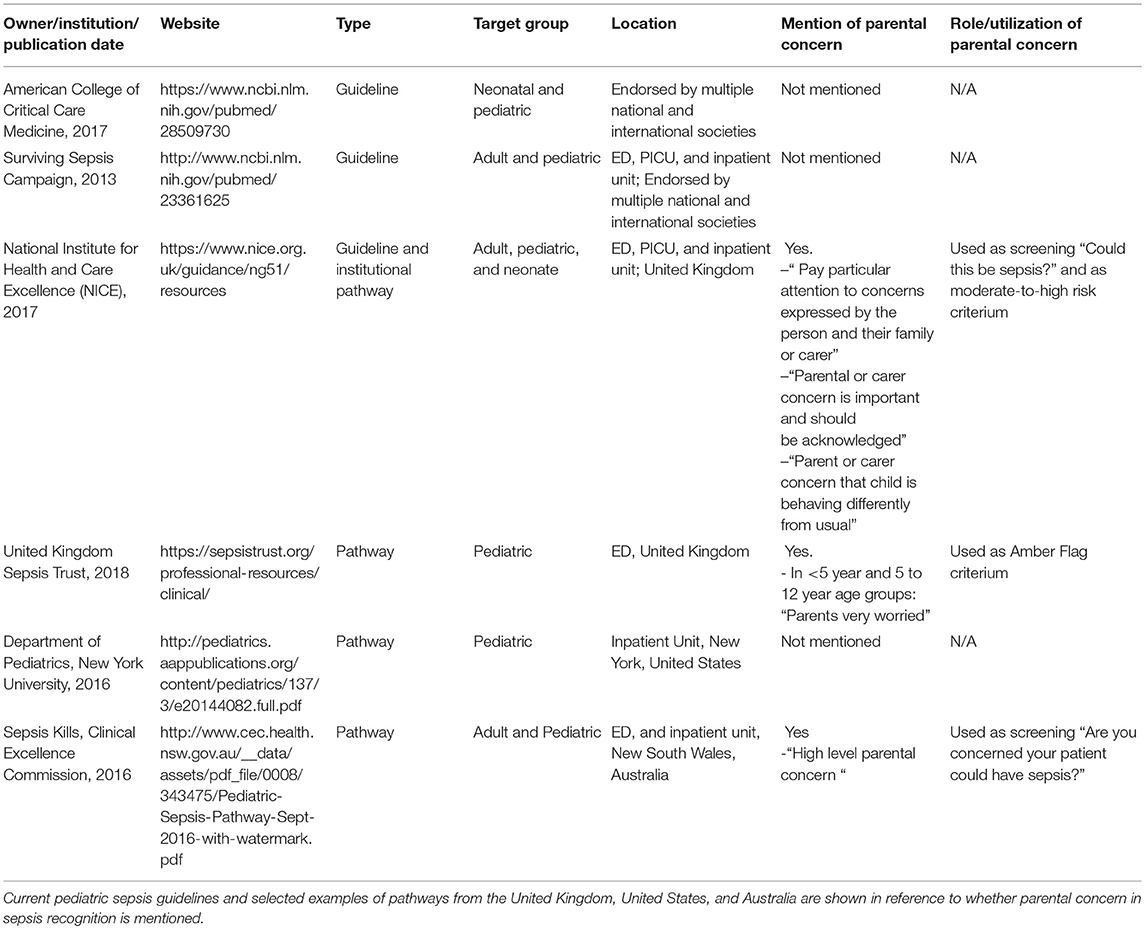
Table 4. Selected examples of online available guidelines and pathways on pediatric sepsis recognition.
Two recent international guidelines pertinent to pediatric age groups, the American College of Critical Care Medicine Guidelines 2017 (48), and the 2013 Surviving Sepsis Campaign (49) guidelines, recommend that institutions implement sepsis screening tools. Parental concerns are not featured in these two guidelines. In contrast, the National Institute for Health and Care Excellence (NICE) (https://www.nice.org.uk/guidance/ng51/resources) and Sepsis Trust (Sepsis 6) (https://sepsistrust.org/professional-resources/clinical/) guidelines in the U.K. Both list parental concern as a feature of sepsis recognition. Two examples of institutional pathways from New York State, United States (http://pediatrics.aappublications.org/content/pediatrics/137/3/e20144082.full.pdf), and New South Wales, Australia (http://www.cec.health.nsw.gov.au/__data/assets/pdf_file/0008/343475/Pediatric-Sepsis-Pathway-Sept-2016-with-watermark.pdf), further illustrate that the utilization of parental concern varies in these pathways. Some list parental concern specifically as a feature that should support clinicians to think “Could this be sepsis,” others list it as one of several criteria prompting treatment, and some do not mention parental concern specifically.
Discussion
In this literature review on parental concerns as a tool to assist in the recognition of sepsis, we identified a paucity of evidence to guide best practice. Only one study was found which assessed diagnostic accuracy of parental concerns in serious infections, suggesting superior performance of parental concern in comparison to routine physiological-based criteria. Several reviews highlighted the potential of parental concerns in recognizing children with life-threatening infections. Despite the fact that sepsis starts most commonly at home, the role of recognition of sepsis by parents to improve accuracy of early sepsis diagnosis represents a neglected field. Yet, several institutional and national sepsis quality improvement tools have embedded assessment for parental concerns as part of standardized sepsis screening. Our findings indicate an urgent need for well-designed diagnostic accuracy studies to define the value of assessing parental concerns in sepsis recognition in acute care settings. To the best of our knowledge this is the first review providing a comprehensive overview in the field.
The study by Van den Bruel prospectively assessed parental concerns, defined as a parental perception that the disease was different from previous illnesses (37). Despite the sample size of this well-designed study including 3982 visits to General Practitioners, Pediatricians, and Emergency Settings, the prevalence of serious infections was very low, and very few of the serious infections were reported as sepsis, hence resulting in low power for sepsis as an outcome. Despite these limitations, the performance of parental concern was clearly superior to routinely used physiological markers. The authors assessed as well the diagnostic value of clinician‘s gut feeling with serious infections and identified both parental and healthcare worker concerns as good predictors (38). Yet these findings may not necessarily reflect diagnostic performance in Emergency Department settings where patient acuity is higher. In addition, in larger Emergency Departments, a majority of parents already has gone through a selection process by community physicians and parental concern potentially may be less discriminative, restricting the generalizability of the findings by Van den Bruel.
Qualitative studies have shown that parents of children presenting with severe infections report on changes in their child‘s observed behavior ranging from altered crying or mentation, to moaning or inconsolability (43, 47), highlighting the role of parents as experts of their child‘s behavior. The value of parental involvement in healthcare decision-making and provision has been increasingly recognized in areas other than sepsis, building up on the unique position of parents being experts of their child. Structured parental education on early recognition of severe infections has become standard in the management of oncologic children and children discharged with indwelling medical devices (50, 51). While the setting fever and neutropenia may allow easier operationalization than the more vague concept of sepsis, parents of immunosuppressed children are empowered to raise concerns and are often considered part of the experts in making informed decisions about best care to their children. Importantly, in resource poor settings, maternal education has been demonstrated to lead to reduced infection-related mortality during childhood (28), likely through improved prevention and faster recognition of disease leading to earlier treatment.
At present, several campaigns incorporate parental education and empowerment on sepsis, for example the Sepsis Assessment and Management (SAM) tool in the United Kingdom (http://www.southdevonandtorbayccg.nhs.uk/your-health/Documents/sam-sepsis-leaflet.pdf). The Public Health England and the UK Sepsis Trust jointly lead a campaign to improve parental awareness and knowledge of sepsis (http://www.independent.co.uk/life-style/health-and-families/health-news/sepsis-campaign-nhs-jeremy-hunt-children-condition-what-are-symptoms-signs-child-health-a7476426.html. In New York State, education of children on sepsis has become mandatory as part of the Rory Staunton regulations (http://www.nysed.gov/curriculum-instruction/sepsis). Kerkhof et al analyzed data from over 6,000 children and assessed the predictive performance of NICE criteria and suggested future iterations should consider parental concern (52). The more recent NICE guidelines on the recognition of sepsis in children include parental concerns.
Several challenges may arise when including parental concerns as a tool to recognize sepsis: First, the prevalence of sepsis is very low across most pediatric Emergency Departments where hundreds of children present daily with non-septic febrile infections. At the same time, most parents of children with acute infections attending Emergency Departments (rather than General Practitioners) may have substantial concerns. Second, the parental understanding on the possible life-threatening nature of a disease is likely influenced by common belief (“cough” or “fever” is dangerous) rather than specific features of disease. Yet, the paternalistic approach assuming that medical practitioners and Early Warning Tools (19, 53, 54) perform superior to parents may falls short of daily challenges in the provision of medical care: the level of experience of many doctors involved in initial patient assessment may be low, and during busy periods medical staff may not always have sufficient time to assess all patients thoroughly.
Third, the need for, and the benefit of antimicrobial stewardship may not be directly evident to parents who present with a child with a mild disease yet are concerned this could be sepsis—some parents may request antibiotic therapy to prevent or treat potential progression to a severe disease (25). Indeed, a cluster randomized controlled factorial trial evaluated a brief intervention to elicit parental concern combined with safety net advice and found increased antibiotic prescribing in children allocated to this arm (55). The study findings imply that over-prescription of antibiotics needs to be considered as a balancing measure when designing interventions focusing on parental concern. Forth, a study in east Africa (56) investigated the educational background of parents in relation to presentations for pediatric illness and demonstrated that the majority of the parents had very limited knowledge of their children's health problems as assessed in the study. This illustrates the considerable cultural and educational challenges in applying parental concern-based approaches in low income settings. Finally, individual parents may have different perceptions and approaches to risks related to infectious diseases and treatment (57).
Future studies should prospectively assess the diagnostic accuracy of parental assessment of infectious disease severity across low, middle, and high income settings with particular focus on sepsis and septic shock. Further information is needed to specifically analyze the benefit of providing targeted sepsis education to parents. Given the unique role of parents as experts of their child, such interventions have in principle a substantial potential to enhance the diagnostic performance of screening for sepsis as part of a rule-in approach. Yet, such approaches needs to be balanced against the risk that creating community awareness of sepsis may lead to excessive consumption of healthcare resources for children with mild infections, and lead to unnecessary treatment. Hence, while it may be beneficial for clinicians to include questions pertinent to the level of parental concern in their assessment of the acutely ill child evaluated for infection, clinicians should be empowered to consider diagnoses other than sepsis and make an informed decision to rule-out sepsis if such is considered unlikely (25). Parents should be considered key partners in safety netting of such children where sepsis was ruled out—ongoing observation at home with the availability for prompt representation to reassess may potentially reduce adverse outcomes from late sepsis presentations.
Limitations
Several limitations of this review need to be considered. First, only one original study was identified reporting on the diagnostic accuracy of parental concerns in the recognition of sepsis, with a very small number of children meeting the outcome, and a meta-analysis could not be performed. Second, the design and quality of included articles was variable, ranging from original quantitative studies, original qualitative studies, and high quality systematic reviews to non-systematic narratives. In view of the lack of data, the review was extended to include original studies not reporting on diagnostic accuracy and reviews referring to parental concern in children with sepsis. Third, only abstracts leading to full text publications in English were considered, and this may have further reduced the yield of the search. Finally, the overview of institutional sepsis pathways represents a selection pertinent to recently published international sepsis guidelines, and jurisdictions who have reported on sepsis pathway implementation.
Conclusion
In conclusion, this review identified a paucity of data analyzing the role of parental concerns in recognizing sepsis. Several guidelines and institutional protocols emphasize the importance of listening to parents and utilize parental concerns as one of the trigger criteria for sepsis recognition. Parental concern needs to be considered to improve accuracy in recognizing life-threatening infections in children. Education on utilizing parental concerns to recognize sepsis has the potential to lead to better outcomes in paediatric sepsis. However, understanding parental perceptions of sepsis, and parental decision-making in seeking advice is urgently needed to inform on optimal design of education campaigns, and to assist in the design of sepsis recognition bundles. Prospective studies are needed testing the sensitivity, specificity, and negative and positive predictive value of parental concerns in sepsis in various settings, while assessing the potential impact on antibiotic and health care resource use.
Author Contributions
AH and LS designed the study. All abstracts were checked by AH and LS. AH and LS went through each of the full texts. JL assisted in study design, review of results, and manuscript writing. LS and AH wrote the first draft of the manuscript. All authors contributed to manuscript revision and approved the final version.
Funding
LS holds a National Health and Medical Research Council Practitioner Fellowship and is supported by the Children's Hospital Foundation, Brisbane, Australia.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank Kate McEnery, Pediatric Critical Care Research Group, Brisbane, for critical comments on the topic which have informed the design of this project, and the librarians at the Gold Coast University Hospital, Southport, Australia, for help in database searches.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fped.2019.00161/full#supplementary-material
References
1. Fleischmann-Struzek C, Goldfarb DM, Schlattmann P, Schlapbach LJ, Reinhart K, Kissoon N. The global burden of paediatric and neonatal sepsis: a systematic review. Lancet Respir Med. (2018) 6:223–30. doi: 10.1016/S2213-2600(18)30063-8
2. Schlapbach LJ, Straney L, Alexander J, MacLaren G, Festa M, Schibler A, et al. Mortality related to invasive infections, sepsis, and septic shock in critically ill children in Australia and New Zealand, 2002-13: a multicentre retrospective cohort study. Lancet Infect Dis. (2015) 15:46–54. doi: 10.1016/S1473-3099(14)71003-5
3. Ruth A, McCracken CE, Fortenberry JD, Hall M, Simon HK, Hebbar KB. Pediatric severe sepsis: current trends and outcomes from the pediatric Health Information Systems database. Pediatr Crit Care Med. (2014) 15:828–38. doi: 10.1097/PCC.0000000000000254
4. Reinhart K, Daniels R, Kissoon N, Machado FR, Schachter RD, Finfer S. Recognizing sepsis as a global health priority - A WHO resolution. N Engl J Med. (2017) 377:414–7. doi: 10.1056/NEJMp1707170
5. Kissoon N, Reinhart K, Daniels R, Machado FR, Schachter RD, Finfer S. Sepsis in children: global implications of the world health assembly resolution on sepsis. Pediatr Crit Care Med. (2017) 18:e625–7. doi: 10.1097/PCC.0000000000001340
6. Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. (2017) 43:304–77. doi: 10.1007/s00134-017-4683-6
7. Schlapbach LJ, MacLaren G, Festa M, Alexander J, Erickson S, Beca J, et al. New Zealand intensive care society centre for, E. resource, Australian, and G. New Zealand Intensive Care Society Paediatric Study, Prediction of pediatric sepsis mortality within 1 h of intensive care admission. Intensive Care Med. (2017) 43:1085–96. doi: 10.1007/s00134-017-4701-8
8. Agyeman KA, Schlapbach LJ, Giannoni E, Stocker M, Posfay-Barbe KM, Heininger U, et al. Swiss pediatric sepsis, epidemiology of blood culture-proven bacterial sepsis in children in Switzerland: a population-based cohort study. Lancet Child Adolesc Health. (2017) 1:124–33. doi: 10.1016/S2352-4642(17)30010-X
9. Cvetkovic M, Lutman D, Ramnarayan P, Pathan N, Inwald DP, Peters MJ. Timing of death in children referred for intensive care with severe sepsis: implications for interventional studies. Pediatr Crit Care Med. (2015) 16:410–7. doi: 10.1097/PCC.0000000000000385
10. Weiss SL, Balamuth F, Hensley J, Fitzgerald JC, Bush J, Nadkarni VM, et al. The epidemiology of hospital death following pediatric severe sepsis: when, why, and how children with sepsis die. Pediatr Crit Care Med. (2017) 18:823–30. doi: 10.1097/PCC.0000000000001222
11. Maitland K, Kiguli S, Opoka RO, Engoru C, Olupot-Olupot P, Akech SO, et al. Mortality after fluid bolus in African children with severe infection. N Engl J Med. (2011) 364:2483–95. doi: 10.1056/NEJMoa1101549
12. Nadel S, Goldstein B, Williams MD, Dalton H, Peters M, Macias WL, et al. R.E.s. Sepsis, and g. Organ dysfunction in children: a gLobal perspective study, Drotrecogin alfa (activated) in children with severe sepsis: a multicentre phase III randomised controlled trial. Lancet. (2007) 369:836–43. doi: 10.1016/S0140-6736(07)60411-5
13. Angus DC, Barnato AE, Bell D, Bellomo R, Chong CR, Coats TJ, et al. A systematic review and meta-analysis of early goal-directed therapy for septic shock: the ARISE, ProCESS and ProMISe Investigators. Intensive Care Med. (2015) 41:1549–60. doi: 10.1007/s00134-015-3822-1
14. Evans IVR, Phillips GS, Alpern ER, Angus DC, Friedrich ME, Kissoon N, et al. Association between the new york sepsis care mandate and in-hospital mortality for pediatric sepsis. JAMA. (2018) 320:358–67. doi: 10.1001/jama.2018.9071
15. Weiss SL, Fitzgerald JC, Balamuth F, Alpern ER, Lavelle J, Chilutti M, et al. Delayed antimicrobial therapy increases mortality and organ dysfunction duration in pediatric sepsis. Crit Care Med. (2014) 42:2409–17. doi: 10.1097/CCM.0000000000000509
16. Launay E, Gras-Le Guen C, Martinot A, Assathiany R, Martin E, Blanchais T, et al. Why children with severe bacterial infection die: a population-based study of determinants and consequences of suboptimal care with a special emphasis on methodological issues. PLoS ONE. (2014) 9:e107286. doi: 10.1371/journal.pone.0107286
17. Kumar A, Roberts D, Wood KE, Light B, Parrillo JE, Sharma S, et al. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med. (2006) 34:1589–96. doi: 10.1097/01.CCM.0000217961.75225.E9
18. Seymour CW, Gesten F, Prescott HC, Friedrich ME, Iwashyna TJ, Phillips GS, et al. Time to treatment and mortality during mandated emergency care for sepsis. N Engl J Med. (2017) 376:2235–44. doi: 10.1056/NEJMoa1703058
19. Balamuth F, Alpern ER, Abbadessa MK, Hayes K, Schast A, Lavelle J, et al. Improving recognition of pediatric severe sepsis in the emergency department: contributions of a vital sign-based electronic alert and bedside clinician identification. Ann Emerg Med. (2017) 70:759–768.e2. doi: 10.1016/j.annemergmed.2017.03.019
20. Irwin AD, Grant A, Williams R, Kolamunnage-Dona R, Drew RJ, Paulus S, et al. Predicting risk of serious bacterial infections in febrile children in the emergency department. Pediatrics. (2017) 140:e20162853. doi: 10.1542/peds.2016-2853
21. Lane RD, Funai T, Reeder R, Larsen GY. High reliability pediatric septic shock quality improvement initiative and decreasing mortality. Pediatrics. (2016) 138:e20154153. doi: 10.1542/peds.2015-4153
22. Verbakel JY, Lemiengre MB, De Burghgraeve T, De Sutter A, Aertgeerts B, Bullens DM, et al. Validating a decision tree for serious infection: diagnostic accuracy in acutely ill children in ambulatory care. BMJ Open. (2015) 5:e008657. doi: 10.1136/bmjopen-2015-008657
23. Geldsetzer P, Williams TC, Kirolos A, Mitchell S, Ratcliffe LA, Kohli-Lynch MK, et al. The recognition of and care seeking behaviour for childhood illness in developing countries: a systematic review. PLoS ONE. (2014) 9:e93427. doi: 10.1371/journal.pone.0093427
24. Schlapbach LJ, Kissoon N. Defining Pediatric Sepsis. JAMA Pediatr. (2018) 172:312–4. doi: 10.1001/jamapediatrics.2017.5208
25. Schlapbach LJ, Weiss SL, Wolf J. Reducing collateral damage from mandates for time to antibiotics in pediatric sepsis-primum non nocere. JAMA Pediatr. (2019). doi: 10.1001/jamapediatrics.2019.0174. [Epub ahead of print].
26. Klompas M, Calandra T, Singer M. Antibiotics for sepsis-finding the equilibrium. JAMA. (2018) 320:1433–4. doi: 10.1001/jama.2018.12179
27. Singer M. Antibiotics for sepsis: does each hour really count, or is it incestuous amplification? Am J Respir Crit Care Med. (2017) 196:800–2. doi: 10.1164/rccm.201703-0621ED
28. Gakidou E, Cowling K, Lozano R, Murray CJ. Increased educational attainment and its effect on child mortality in 175 countries between 1970 and 2009: a systematic analysis. Lancet. (2010) 376:959–74. doi: 10.1016/S0140-6736(10)61257-3
29. Schlapbach LJ, Ostrowski JA, MacLaren G. The excess burden of severe sepsis in Indigenous Australian children: can anything be done? Med J Aust. (2017) 207:45–6. doi: 10.5694/mja17.00464
30. Goldstein B, Giroir B, Randolph A. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med. (2005) 6:2–8. doi: 10.1097/01.PCC.0000149131.72248.E6
31. Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS international sepsis definitions conference. Crit Care Med. (2003) 31:1250–6. doi: 10.1097/01.CCM.0000050454.01978.3B
32. Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. (2016) 315:801–10. doi: 10.1001/jama.2016.0287
33. Burrell AR, McLaws ML, Fullick M, Sullivan RB, Sindhusake D. SEPSIS KILLS: early intervention saves lives. Med J Aust. (2016) 204:73.e1–7. doi: 10.5694/mja15.00657
34. Daniels R, Nutbeam T, McNamara G, Galvin C. The sepsis six and the severe sepsis resuscitation bundle: a prospective observational cohort study. Emerg Med J. (2011) 28:507–12. doi: 10.1136/emj.2010.095067
35. McMenamin L, Murch N, Daniels R. Severe sepsis, social media and the #Sepsis 6: ‘Tweeting' national innovations. Acute Med. (2013) 12:83–8.
36. Oostenbrink R, de Groot R, Moll HA. Fever of unknown origin in a young child: diagnosis and treatment. Nederlands Tijdschrift Voor Geneeskunde. (1999) 143:185–90.
37. Van den Bruel A, Aertgeerts B, Bruyninckx R, Aerts M, Buntinx F. Signs and symptoms for diagnosis of serious infections in children: a prospective study in primary care. Br J Gene Pract. (2007) 57:538–46.
38. Van den Bruel A, Thompson M, Buntinx F, Mant D. Clinicians' gut feeling about serious infections in children: observational study. BMJ. (2012) 345:e6144. doi: 10.1136/bmj.e6144
39. Van den Bruel A, Bruyninckx R, Vermeire E, Aerssens P, Aertgeerts B, Buntinx F. Signs and symptoms in children with a serious infection: a qualitative study. BMC Family Pract. (2005) 6:36. doi: 10.1186/1471-2296-6-36
40. Brennan CA, Somerset M, Granier SK, Fahey TP, Heyderman RS. Management of diagnostic uncertainty in children with possible meningitis: a qualitative study. Br J Gene Pract. (2003) 53:626–31.
41. Kai J. What worries parents when their preschool children are acutely ill, and why: a qualitative study. BMJ. (1996) 313:983–6.
42. Niehues T. The febrile child: diagnosis and treatment. Deutsches Aerzteblatt Int. (2013) 110:764–74. doi: 10.3238/arztebl.2013.0764
43. Thompson M, Van den Bruel A, Verbakel J, Lakhanpaul M, Haj-Hassan T, Stevens R, et al. Systematic review and validation of prediction rules for identifying children with serious infections in emergency departments and urgent-access primary care. Health Technol Assess. (2012) 16:1–100. doi: 10.3310/hta16150
44. Long LE. Stress in families of children with sepsis. Crit Care Nurs Clin N Am. (2003) 15:47–53. doi: 10.1016/S0899-5885(02)00041-2
45. Printz V, Hobbs AM-E, Teuten P, Prosad Paul S. Clinical update: assessment and management of febrile children. Commun Pract. (2016) 89:32–7.
46. Yung AP, McDonald MI. Early clinical clues to meningococcaemia. Med J Aust. (2003) 178:134–7. doi: 10.5694/j.1326-5377.2003.tb05106.x
47. Van den Bruel A, Haj-Hassan T, Thompson M, Buntinx F, Mant D. Diagnostic value of clinical features at presentation to identify serious infection in children in developed countries: a systematic review. Lancet. (2010) 375:834–45. doi: 10.1016/S0140-6736(09)62000-6
48. Davis AL, Carcillo JA, Aneja RK, Deymann AJ, Lin JC, Nguyen TC, et al. American college of critical care medicine clinical practice parameters for hemodynamic support of pediatric and neonatal septic shock. Crit Care Med. (2017) 45:1061–93. doi: 10.1097/CCM.0000000000002425
49. Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock, 2012. Inten Care Med. (2013) 39:165–228. doi: 10.1007/s00134-012-2769-8
50. Ku BC, Bailey C, Balamuth F. Neutropenia in the febrile child. Pediatr Emerg Care. (2016) 32:329–34. doi: 10.1097/PEC.0000000000000809
51. Ammann RA, Hirt A, Luthy AR, Aebi C. Predicting bacteremia in children with fever and chemotherapy-induced neutropenia. Pediatr Infect Dis J. (2004) 23:61–7. doi: 10.1097/01.inf.0000106782.30100.4f
52. Kerkhof E, Lakhanpaul M, Ray S, Verbakel JY, Van den Bruel A, Thompson M, et al. The predictive value of the NICE “red traffic lights” in acutely ill children. PLoS ONE. (2014) 9:e90847. doi: 10.1371/journal.pone.0090847
53. Chapman SM, Wray J, Oulton K, Pagel C, Ray S, Peters MJ. ‘The Score Matters': wide variations in predictive performance of 18 paediatric track and trigger systems. Arch Dis Child. (2017) 102:487–95. doi: 10.1136/archdischild-2016-311088
54. Balamuth F, Alpern ER, Grundmeier RW, Chilutti M, Weiss SL, Fitzgerald JC, et al. Comparison of two sepsis recognition methods in a pediatric emergency department. Acad Emerg Med. (2015) 22:1298–306. doi: 10.1111/acem.12814
55. Lemiengre MB, Verbakel JY, Colman R, De Burghgraeve T, Buntinx F, Aertgeerts B, et al. Reducing inappropriate antibiotic prescribing for children in primary care: a cluster randomised controlled trial of two interventions. Br J Gene Pract. (2018) 68:e204–e210. doi: 10.3399/bjgp18X695033
56. Makworo D, Laving AM. Acute medical conditions in under five year old children at a public hospital in Kenya. East Afr Med J. (2010) 87:340–4.
Keywords: child, concern, diagnosis, infection, parent, recognition, sepsis, septic shock
Citation: Harley A, Latour JM and Schlapbach LJ (2019) The Role of Parental Concerns in the Recognition of Sepsis in Children: A Literature Review. Front. Pediatr. 7:161. doi: 10.3389/fped.2019.00161
Received: 24 December 2018; Accepted: 08 April 2019;
Published: 03 May 2019
Edited by:
Jan Hau Lee, KK Women's and Children's Hospital, SingaporeReviewed by:
Jhuma Sankar, All India Institute of Medical Sciences, IndiaEduardo Villamor, Maastricht University Medical Centre, Netherlands
Copyright © 2019 Harley, Latour and Schlapbach. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Luregn J. Schlapbach, l.schlapbach@uq.edu.au
 Amanda Harley
Amanda Harley Jos M. Latour
Jos M. Latour Luregn J. Schlapbach
Luregn J. Schlapbach