Abstract
Purpose
Gorham-Stout disease is a very rare disorder characterized by progressive bone erosion and angiomatous proliferation; its etiopathogenesis is still unknown, and diagnosis is still performed by exclusion criteria. The alteration of bone remodeling activity has been reported in patients; in this study, we characterized circulating osteoclast and osteogenic precursors that could be important to better understand the osteolysis observed in patients.
Methods
Flow cytometry analysis of PBMC (Peripheral Blood Mononuclear Cells) was performed to characterize circulating osteoclast and osteogenic precursors in GSD patients (n = 9) compared to healthy donors (n = 55). Moreover, ELISA assays were assessed to evaluate serum levels of bone markers including RANK-L (Receptor activator of NF-κB ligand), OPG (Osteoprotegerin), BALP (Bone Alkaline Phosphatase) and OCN (Osteocalcin).
Results
We found an increase of CD16−/CD14+CD11b+ and CD115+/CD14+CD11b+ osteoclast precursors in GSD patients, with high levels of serum RANK-L that could reflect the increase of bone resorption activity observed in patients. Moreover, no significant alterations were found regarding osteogenic precursors and serum levels of BALP and OCN.
Conclusion
The analysis of circulating bone cell precursors, as well as of RANK-L, could be relevant as an additional diagnostic tool for these patients and could be exploited for therapeutic purposes.




Similar content being viewed by others
References
Gorham LW, Wright AW, Shultz HH, Maxon FC Jr (1954) Disappearing bones: a rare form of massive osteolysis; report of two cases, one with autopsy findings. Am J Med 17(5):674–682. https://doi.org/10.1016/0002-9343(54)90027-3
Dellinger MT, Garg N, Olsen BR (2014) Viewpoints on vessels and vanishing bones in Gorham-Stout disease. Bone 63:47–52. https://doi.org/10.1016/j.bone.2014.02.011
Hu P, Yuan XG, Hu XY, Shen FR, Wang JA (2013) Gorham-Stout syndrome in mainland China: a case series of 67 patients and review of the literature. J Zhejiang Univ Sci B 14(8):729–735. https://doi.org/10.1631/jzus.B1200308
Nikolaou VS, Chytas D, Korres D, Efstathopoulos N (2014) vanishing bone disease (Gorham-Stout syndrome): a review of a rare entity. World J Orthop 5(5):694–698. https://doi.org/10.5312/wjo.v5.i5.694
Patel DV (2005) Gorham’s disease or massive osteolysis. Clin Med Res 3(2):65–74. https://doi.org/10.3121/cmr.3.2.65
Homayun-Sepehr N, McCarter AL, Helaers R, Galant C, Boon LM, Brouillard P, Vikkula M, Dellinger MT (2021) KRAS-driven model of Gorham-Stout disease effectively treated with trametinib. JCI Insight. https://doi.org/10.1172/jci.insight.149831
Nozawa A, Ozeki M, Niihori T, Suzui N, Miyazaki T, Aoki Y (2020) A somatic activating KRAS variant identified in an affected lesion of a patient with Gorham-Stout disease. J Hum Genet 65(11):995–1001. https://doi.org/10.1038/s10038-020-0794-y
Li MH, Zhang HQ, Lu YJ, Gao P, Huang H, Hu YC, Wang Z (2018) Successful management of Gorham-Stout disease in scapula and ribs: a case report and literature review. Orthop Surg 10(3):276–280. https://doi.org/10.1111/os.12390
Hopman SM, Van Rijn RR, Eng C, Bras J, Alders M, van der Horst CM, Hennekam RC, Merks JH (2012) PTEN hamartoma tumor syndrome and Gorham-Stout phenomenon. Am J Med Genet A 158A(7):1719–1723. https://doi.org/10.1002/ajmg.a.35406
Rossi M, Buonuomo PS, Battafarano G, Conforti A, Mariani E, Algeri M, Pelle S, D’Agostini M, Macchiaiolo M, De Vito R et al (2020) Dissecting the mechanisms of bone loss in Gorham-Stout disease. Bone 130:115068. https://doi.org/10.1016/j.bone.2019.115068
Devlin RD, Bone HG 3rd, Roodman GD (1996) Interleukin-6: a potential mediator of the massive osteolysis in patients with Gorham-Stout disease. J Clin Endocrinol Metab 81(5):1893–1897. https://doi.org/10.1210/jcem.81.5.8626854
Falcini F, Ermini M, Bagnoli F (1998) Bone turnover is reduced in children with juvenile rheumatoid arthritis. J Endocrinol Invest 21(1):31–36. https://doi.org/10.1007/BF03347283
Rossi M, Rana I, Buonuomo PS, Battafarano G, De Martino V, D’Agostini M, Porzio O, Cipriani C, Minisola S, De Vito R et al (2021) Stimulation of treg cells to Inhibit osteoclastogenesis in Gorham-Stout disease. Front Cell Dev Biol 9:706596. https://doi.org/10.3389/fcell.2021.706596
Komano Y, Nanki T, Hayashida K, Taniguchi K, Miyasaka N (2006) Identification of a human peripheral blood monocyte subset that differentiates into osteoclasts. Arthritis Res Ther 8(5):R152. https://doi.org/10.1186/ar2046
Feehan J, Nurgali K, Apostolopoulos V, Duque G (2021) Development and validation of a new method to isolate, expand, and differentiate circulating osteogenic precursor (COP) cells. Bone Rep 15:101109. https://doi.org/10.1016/j.bonr.2021.101109
D’Amelio P, Cristofaro MA, Grimaldi A, Ravazzoli M, Pluviano F, Grosso E, Pescarmona GP, Isaia GC (2010) The role of circulating bone cell precursors in fracture healing. Calcif Tissue Int 86(6):463–469. https://doi.org/10.1007/s00223-010-9362-3
Suda RK, Billings PC, Egan KP, Kim JH, McCarrick-Walmsley R, Glaser DL, Porter DL, Shore EM, Pignolo RJ (2009) Circulating osteogenic precursor cells in heterotopic bone formation. Stem Cells 27(9):2209–2219. https://doi.org/10.1002/stem.150
Heffez L, Doku HC, Carter BL, Feeney JE (1983) Perspectives on massive osteolysis report of a case and review of the literature. Oral Surg Oral Med Oral Pathol 55(4):331–343. https://doi.org/10.1016/0030-4220(83)90185-8
Rana I, Buonuomo PS, Mastrogiorgio G, Del Fattore A, Jenkner A, Barbuti D, De Vito R, Pizzoferro M, Callea M, Crostelli M et al (2021) Expanding the spectrum of Gorham Stout disease exploring a single center pediatric case series. Lymphology 54(4):182–194
Rossi M, Rana I, Buonuomo PS, Battafarano G, Mariani E, D’Agostini M, Porzio O, De Martino V, Minisola S, Macchiaiolo M et al (2021) Dysregulated miRNAs in bone cells of patients with Gorham-Stout disease. FASEB J. https://doi.org/10.1096/fj.202001904RR
Gossiel F, Hoyle C, McCloskey EV, Naylor KE, Walsh J, Peel N, Eastell R (2016) The effect of bisphosphonate treatment on osteoclast precursor cells in postmenopausal osteoporosis: the TRIO study. Bone 92:94–99. https://doi.org/10.1016/j.bone.2016.08.010
Meirow Y, Jovanovic M, Zur Y, Habib J, Colombo DF, Twaik N, Ashkenazi-Preiser H, Ben-Meir K, Mikula I Jr, Reuven O et al (2022) Specific inflammatory osteoclast precursors induced during chronic inflammation give rise to highly active osteoclasts associated with inflammatory bone loss. Bone Res 10(1):36. https://doi.org/10.1038/s41413-022-00206-z
Muto A, Mizoguchi T, Udagawa N, Ito S, Kawahara I, Abiko Y, Arai A, Harada S, Kobayashi Y, Nakamichi Y et al (2011) Lineage-committed osteoclast precursors circulate in blood and settle down into bone. J Bone Miner Res 26(12):2978–2990. https://doi.org/10.1002/jbmr.490
Root SH, Aguila HL (2021) Novel population of human monocyte and osteoclast progenitors from pluripotent stem cells and peripheral blood. Blood Adv 5(21):4435–4446. https://doi.org/10.1182/bloodadvances.2021004552
Xue J, Xu L, Zhu H, Bai M, Li X, Zhao Z, Zhong H, Cheng G, Li X, Hu F et al (2020) CD14(+)CD16(-) monocytes are the main precursors of osteoclasts in rheumatoid arthritis via expressing Tyro3TK. Arthritis Res Ther 22(1):221. https://doi.org/10.1186/s13075-020-02308-7
Deodati A, Fintini D, Levtchenko E, Rossi M, Ubertini G, Segers H, Battafarano G, Cappa M, Del Fattore A (2022) Mechanisms of acute hypercalcemia in pediatric patients following the interruption of denosumab. J Endocrinol Invest 45(1):159–166. https://doi.org/10.1007/s40618-021-01630-4
Mun SH, Park PSU, Park-Min KH (2020) The M-CSF receptor in osteoclasts and beyond. Exp Mol Med 52(8):1239–1254. https://doi.org/10.1038/s12276-020-0484-z
Kodama H, Yamasaki A, Nose M, Niida S, Ohgame Y, Abe M, Kumegawa M, Suda T (1991) Congenital osteoclast deficiency in osteopetrotic (op/op) mice is cured by injections of macrophage colony-stimulating factor. J Exp Med 173(1):269–272. https://doi.org/10.1084/jem.173.1.269
Lee KH, Lee KJ, Kim TY, Hutomo F, Sun HJ, Cheon GJ, Park SI, Cho SW, Im SA (2020) Circulating osteocalcin-positive cells as a novel diagnostic biomarker for bone metastasis in breast cancer patients. J Bone Miner Res 35(10):1838–1849. https://doi.org/10.1002/jbmr.4041
Gossl M, Modder UI, Atkinson EJ, Lerman A, Khosla S (2008) Osteocalcin expression by circulating endothelial progenitor cells in patients with coronary atherosclerosis. J Am Coll Cardiol 52(16):1314–1325. https://doi.org/10.1016/j.jacc.2008.07.019
Acknowledgements
This work was supported by research grants (#MDBR-19-116-LGDA/LMI and #MDBR-21-111-LGDA/LMI) from the University of Pennsylvania Orphan Disease Center in partnership with Lymphangiomatosis & Gorham’s Disease Alliance and the Lymphatic Malformation Institute to ADF, by the Ricerca Finalizzata Ministero della Salute (GR-2019-12370244) to ADF, and by the Italian Ministry of Health (Current Research funds). MR, ST and JDG were supported by Fondazione Umberto Veronesi.
Funding
This work was supported by research grants (#MDBR-19-116-LGDA/LMI and #MDBR-21-111-LGDA/LMI) from the University of Pennsylvania Orphan Disease Center in partnership with Lymphangiomatosis & Gorham’s Disease Alliance and the Lymphatic Malformation Institute to ADF, by the Ricerca Finalizzata Ministero della Salute (GR-2019-12370244) to ADF, and by the Italian Ministry of Health (Current Research funds). MR, ST and JDG were supported by Fondazione Umberto Veronesi.
Author information
Authors and Affiliations
Contributions
MR, ST, GB, LDG, MDA, OP and JDG performed analysis of bone cells precursors and contributed to the discussion of the results. IR, PSB, MVG, CC and AJ recruited the patients and performed the ELISA assays. ADF and AB designed and supervised the work and wrote the paper. All authors reviewed the manuscript and approved the final version. ADF is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Ethical approval
All the procedures performed in this study involving human participants were in accordance with the ethical standards as laid down in the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Both patients and parents were required to sign the informed consent form to participate in the study.
Study approval statement
The study was approved by Bambino Gesù Children’s Hospital's ethics committee (Protocol No. GR-2019-12370244, 01/02/2021).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
40618_2024_2365_MOESM1_ESM.tif
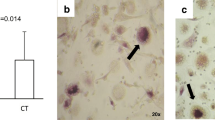
Supplementary file1 FACS negative staining controls. A Representative FACS plots of Fluorescence Minus One (FMO) control for A CD115-BV605 and B CD34-BV650 staining. Left panels: FMO control; right panels: fully stained (TIF 1208 KB)
40618_2024_2365_MOESM2_ESM.tif
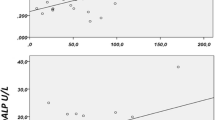
Supplementary file2 Correlations of serum markers with osteoclast precursor populations. A Correlations of RANK-L and CD16− (left panel) or CD16+ (right panel) cell percentage in the gate of CD14+CD11b+ cells. B Correlation of OPG and CD115+ cell percentage in the gate of CD14+CD11b+ cells. The p values are obtained from linear regression analysis (TIF 904 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rossi, M., Terreri, S., Battafarano, G. et al. Analysis of circulating osteoclast and osteogenic precursors in patients with Gorham-Stout disease. J Endocrinol Invest (2024). https://doi.org/10.1007/s40618-024-02365-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s40618-024-02365-8