Abstract
Objective
Left ventricular diastolic dysfunction (LVDD) is a common manifestation of cardiac involvement in systemic sclerosis (SSc), which is associated with increased mortality, but little is known about the risk factors. The aim is to determine the frequency and potential predictors of SSc-LVDD.
Methods
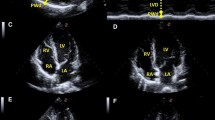
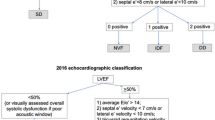
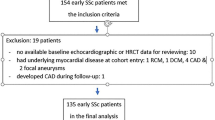
We conducted a prospective multi-center cohort study, enrolling 784 SSc patients assessed by echocardiography between April 2008 and June 2019. Diagnosis of systemic sclerosis was according to the 2013 American College of Rheumatology (ACR)/the European League Against Rheumatism (EULAR) classification criteria. Data were compared between patients with and without LVDD, while univariate and multivariate regression analysis was performed to determine the factors independently associated with LVDD.
Results
LV diastolic dysfunction was present in 246/784 (31.4%) of the subjects. There were no significant differences in gender, BMI, or disease duration between the two groups. Around 40% of the patients in the SSc-LVDD group and in the SSc-non LVDD group had diffused cutaneous involvements. Factors independently associated with LV diastolic dysfunction in multivariable analysis included age at onset (OR 1.053, 95%CI 1.021–1.086, p = 0.001), pulmonary arterial hypertension (OR 3.057, 95%CI 1.468–6.367, p = 0.003), positivity of anti-RNP antibody (OR 2.455, 95%CI 1.049–5.745, p = 0.038), increased WBC count (OR 1.156, 95%CI 1.037–1.287, p = 0.009), elevated levels of uric acid (OR 1.003, 95%CI 1.000–1.006, p = 0.036), and triglyceride (OR 1.515, 95%CI 1.106–2.077, p = 0.010).
Conclusion
LV diastolic dysfunction was prevalent in the SSc population. Advanced onset age, PAH, positive anti-RNP antibody, increased WBC count, and adverse metabolic status were independent risk factors for SSc-related LVDD.
Key Points • In this Chinese multi-center cohort of systemic sclerosis, LVDD is not a rare complication, with a prevalence of 31.4%. • The presence of advanced onset age, PAH, positive anti-RNP antibody, increased WBC count and adverse metabolic status were baseline predictors of developing LVDD in SSc. |

Similar content being viewed by others
Availability of supporting data and materials
All data generated or analyzed during this study are included in the article.
References
Hughes M, Herrick AL (2019) Systemic sclerosis. Br J Hosp Med (Lond) 80:530–536. https://doi.org/10.12968/hmed.2019.80.9.530
Zhong L, Pope M, Shen Y, Hernandez JJ, Wu L (2019) Prevalence and incidence of systemic sclerosis: A systematic review and meta-analysis. Int J Rheum Dis 22:2096–2107. https://doi.org/10.1111/1756-185X.13716
Allanore Y, Meune C (2010) Primary myocardial involvement in systemic sclerosis: evidence for a microvascular origin. Clin Exp Rheumatol 28:S48–53
Bulkley BH, Ridolfi RL, Salyer WR, Hutchins GM (1976) Myocardial lesions of progressive systemic sclerosis. A cause of cardiac dysfunction. Circulation 53:483–490. https://doi.org/10.1161/01.cir.53.3.483
Wangkaew S, Prasertwitayakij N, Phrommintikul A, Puntana S, Euathrongchit J (2017) Causes of death, survival and risk factors of mortality in Thai patients with early systemic sclerosis: inception cohort study. Rheumatol Int 37:2087–2094. https://doi.org/10.1007/s00296-017-3846-7
Ferri C, Valentini G, Cozzi F, Sebastiani M, Michelassi C, La Montagna G, Bullo A, Cazzato M, Tirri E, Storino F, Giuggioli D, Cuomo G, Rosada M, Bombardieri S, Todesco S, Tirri G; Systemic Sclerosis Study Group of the Italian Society of Rheumatology (SIR-GSSSc) (2002) Systemic sclerosis: demographic, clinical, and serologic features and survival in 1,012 Italian patients. Medicine (Baltimore) 81:139–153. https://doi.org/10.1097/00005792-200203000-00004
Aguglia G, Sgreccia A, Bernardo ML, Carmenini E, Giusti De Marle M, Reali A, Morelli S (2001) Left ventricular diastolic function in systemic sclerosis. J Rheumatol 28:1563–1567
Faludi R, Költő G, Bartos B, Csima G, Czirják L, Komócsi A (2014) Five-year follow-up of left ventricular diastolic function in systemic sclerosis patients: determinants of mortality and disease progression. Semin Arthritis Rheum 44:220–227. https://doi.org/10.1016/j.semarthrit.2014.04.001
Allanore Y, Simms R, Distler O, Trojanowska M, Pope J, Denton CP, Varga J (2015) Systemic sclerosis. Nat Rev Dis Primers 23:15002. https://doi.org/10.1038/nrdp.2015.2
Galiè N, Humbert M, Vachiery JL, Gibbs S, Lang I, Torbicki A, Simonneau G, Peacock A, Vonk Noordegraaf A, Beghetti M, Ghofrani A, Gomez Sanchez MA, Hansmann G, Klepetko W, Lancellotti P, Matucci M, McDonagh T, Pierard LA, Trindade PT, Zompatori M, Hoeper M; ESC Scientific Document Group (2015) 2015 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension: The Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Heart J 37:67–119. https://doi.org/10.1093/eurheartj/ehv317
Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA, Waggoner AD, Flachskampf FA, Pellikka PA, Evangelisa A (2009) Recommendations for the evaluation of left ventricular diastolic function by echocardiography. Eur J Echocardiogr 10:165–193. https://doi.org/10.1093/ejechocard/jep007
Nagueh SF, Smiseth OA, Appleton CP, Byrd BF 3rd, Dokainish H, Edvardsen T, Flachskampf FA, Gillebert TC, Klein AL, Lancellotti P, Marino P, Oh JK, Alexandru Popescu B, Waggoner AD; Houston, Texas; Oslo, Norway; Phoenix, Arizona; Nashville, Tennessee; Hamilton, Ontario, Canada; Uppsala, Sweden; Ghent and Liège, Belgium; Cleveland, Ohio; Novara, Italy; Rochester, Minnesota; Bucharest, Romania; and St. Louis, Missouri (2016) Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 17:1321–1360. https://doi.org/10.1093/ehjci/jew082
Heine JJVAFPAUPUFKM (1926) Über ein eigenartiges Krankheitsbild von diffuser Skelerosis der Haut und innerer Organe. Virchows Arch Pathol Anat Physiol Klin Med 262:351–382
Fernández-Codina A, Simeón-Aznar CP, Pinal-Fernandez I, Rodríguez-Palomares J, Pizzi MN, Hidalgo CE, Guillén-Del Castillo A, Prado-Galbarro FJ, Sarria-Santamera A, Fonollosa-Plà V, Vilardell-Tarrés M (2017) Cardiac involvement in systemic sclerosis: differences between clinical subsets and influence on survival. Rheumatol Int 37:75–84. https://doi.org/10.1007/s00296-015-3382-2
Vemulapalli S, Cohen L, Hsu V (2016) Prevalence and risk factors for left ventricular diastolic dysfunction in a scleroderma cohort. Scand J Rheumatol 46:281–287. https://doi.org/10.1080/03009742.2016.1206963
Akdogan A, Kaya EB, Sahin A, Okutucu S, Yakut E, Kalyoncu U, Aksoy H, Karadag O, Calguneri M, Tokgozoglu L, Kiraz S, Ertenli I (2011) Relationship between left ventricular diastolic dysfunction and six minute walk test in patients with systemic sclerosis. Int J Rheum Dis 14:379–383. https://doi.org/10.1111/j.1756-185X.2011.01672.x
Hinchcliff M, Desai CS, Varga J, Shah SJ (2012) Prevalence, prognosis, and factors associated with left ventricular diastolic dysfunction in systemic sclerosis. Clin Exp Rheumatol 30:S30–37
Fischer M, Baessler A, Hense HW, Hengstenberg C, Muscholl M, Holmer S, Döring A, Broeckel U, Riegger G, Schunkert H (2003) Prevalence of left ventricular diastolic dysfunction in the community. Results from a Doppler echocardiographic-based survey of a population sample. Eur Heart J 24:320–328. https://doi.org/10.1016/s0195-668x(02)00428-1
Kloch-Badelek M, Kuznetsova T, Sakiewicz W, Tikhonoff V, Ryabikov A, González A, López B, Thijs L, Jin Y, Malyutina S, Stolarz-Skrzypek K, Casiglia E, Díez J, Narkiewicz K, Kawecka-Jaszcz K, Staessen JA; European Project On Genes in Hypertension (EPOGH) Investigators (2012) Prevalence of left ventricular diastolic dysfunction in European populations based on cross-validated diagnostic thresholds. Cardiovasc Ultrasound 19:10. https://doi.org/10.1186/1476-7120-10-10
Kuznetsova T, Herbots L, López B, Jin Y, Richart T, Thijs L, González A, Herregods MC, Fagard RH, Díez J, Staessen JA (2009) Prevalence of left ventricular diastolic dysfunction in a general population. Circ Heart Fail 2:105–112. https://doi.org/10.1161/CIRCHEARTFAILURE.108.822627
Meune C, Avouac J, Wahbi K, Cabanes L, Wipff J, Mouthon L, Guillevin L, Kahan A, Allanore Y (2008) Cardiac involvement in systemic sclerosis assessed by tissue-doppler echocardiography during routine care: A controlled study of 100 consecutive patients. Arthritis Rheum 58:1803–1809. https://doi.org/10.1002/art.23463
Ciurzyński M, Bienias P, Irzyk K, Kostrubiec M, Bartoszewicz Z, Siwicka M, Kurzyna M, Demkow U, Pruszczyk P (2013) Exaggerated increase of exercise-induced pulmonary artery pressure in systemic sclerosis patients predominantly results from left ventricular diastolic dysfunction. Clin Res Cardiol 102:813–820. https://doi.org/10.1007/s00392-013-0594-x
Tennøe AH, Murbræch K, Andreassen JC, Fretheim H, Garen T, Gude E, Andreassen A, Aakhus S, Molberg Ø, Hoffmann-Vold AM (2018) Left Ventricular Diastolic Dysfunction Predicts Mortality in Patients With Systemic Sclerosis. J Am Coll Cardiol 72:1804–1813. https://doi.org/10.1016/j.jacc.2018.07.068
Desai CS, Colangelo LA, Liu K, Jacobs DR Jr, Cook NL, Lloyd-Jones DM, Ogunyankin KO (2013) Prevalence, prospective risk markers, and prognosis associated with the presence of left ventricular diastolic dysfunction in young adults: the coronary artery risk development in young adults study. Am J Epidemiol 177:20–32. https://doi.org/10.1093/aje/kws224
Hajdu MA, Heistad DD, Siems JE, Baumbach GL (1990) Effects of aging on mechanics and composition of cerebral arterioles in rats. Circ Res 66:1747–1754. https://doi.org/10.1161/01.res.66.6.1747
Dai DF, Chen T, Johnson SC, Szeto H, Rabinovitch PS (2011) Cardiac aging: from molecular mechanisms to significance in human health and disease. Antioxid Redox Signal 16:1492–1526. https://doi.org/10.1089/ars.2011.4179
Carreira PE, Carmona L, Joven BE, Loza E, Andréu JL, Riemekasten G, Vettori S, Balbir-Gurman A, Airò P, Walker U, Damjanov N, Matucci-Cerinic M, Ananieva LP, Rednic S, Czirják L, Distler O, Farge D, Hesselstrand R, Corrado A, Caramaschi P, Tikly M, Allanore Y (2019) Differences associated with age at onset in early systemic sclerosis patients: a report from the EULAR Scleroderma Trials and Research Group (EUSTAR) database. Scand J Rheumatol 48:42–51. https://doi.org/10.1080/03009742.2018.1459830
Jaeger VK, Wirz EG, Allanore Y, Rossbach P, Riemekasten G, Hachulla E, Distler O, Airò P, Carreira PE, Balbir Gurman A, Tikly M, Vettori S, Damjanov N, Müller-Ladner U, Distler JH, Li M, Walker UA; EUSTAR co-authors (2016) Incidences and Risk Factors of Organ Manifestations in the Early Course of Systemic Sclerosis: A Longitudinal EUSTAR Study. PLoS One 11:e0163894. https://doi.org/10.1371/journal.pone.0163894
Tonelli AR, Plana JC, Heresi GA, Dweik RA (2012) Prevalence and prognostic value of left ventricular diastolic dysfunction in idiopathic and heritable pulmonary arterial hypertension. Chest 141:1457–1465. https://doi.org/10.1378/chest.11-1903
Smith V, Riccieri V, Pizzorni C, Decuman S, Deschepper E, Bonroy C, Sulli A, Piette Y, De Keyser F, Cutolo M (2013) Nailfold capillaroscopy for prediction of novel future severe organ involvement in systemic sclerosis. J Rheumatol 40:2023–2028. https://doi.org/10.3899/jrheum.130528
Repa A, Avgoustidis N, Kougkas N, Bertsias G, Zafiriou M, Sidiropoulos P (2019) Nailfold videocapillaroscopy as a candidate biomarker for organ involvement and prognosis in patients with systemic sclerosis. Mediterr J Rheumatol 30:48–50. https://doi.org/10.31138/mjr.30.1.48
Jia G, Habibi J, Bostick BP, Ma L, DeMarco VG, Aroor AR, Hayden MR, Whaley-Connell AT, Sowers JR (2015) Uric acid promotes left ventricular diastolic dysfunction in mice fed a Western diet. Hypertension 65:531–539. https://doi.org/10.1161/HYPERTENSIONAHA.114.04737
Georgiopoulos G, Tsioufis C, Kalos T, Magkas N, Roussos D, Chrysohoou C, Sarri G, Syrmali K, Georgakopoulos P, Tousoulis D (2019) Serum uric acid is independently associated with diastolic dysfunction in apparently healthy subjects with essential hypertension. Curr Vasc Pharmacol 17:99–106. https://doi.org/10.2174/1570161116666171226124959
Lee HJ, Kim HL, Lim WH, Seo JB, Kim SH, Zo JH, Kim MA (2019) Subclinical alterations in left ventricular structure and function according to obesity and metabolic health status. PLoS One 14:e0222118. https://doi.org/10.1371/journal.pone.0222118
Widya RL, de Mutsert R, den Heijer M, le Cessie S, Rosendaal FR, Jukema JW, Smit JW, de Roos A, Lamb HJ; NEO Study Group (2016) Association between hepatic triglyceride content and left ventricular diastolic function in a population-based cohort: the Netherlands epidemiology of obesity study. Radiology 279:443–450. https://doi.org/10.1148/radiol.2015150035
Ayalon N, Gopal DM, Mooney DM, Simonetti JS, Grossman JR, Dwivedi A, Donohue C, Perez AJ, Downing J, Gokce N, Miller EJ, Liang CS, Apovian CM, Colucci WS, Ho JE (2014) Preclinical left ventricular diastolic dysfunction in metabolic syndrome. Am J Cardiol 114:838–842. https://doi.org/10.1016/j.amjcard.2014.06.013
McMurray JJ, Adamopoulos S, Anker SD, Auricchio A, Böhm M, Dickstein K, Falk V, Filippatos G, Fonseca C, Gomez-Sanchez MA, Jaarsma T, Køber L, Lip GY, Maggioni AP, Parkhomenko A, Pieske BM, Popescu BA, Rønnevik PK, Rutten FH, Schwitter J, Seferovic P, Stepinska J, Trindade PT, Voors AA, Zannad F, Zeiher A; ESC Committee for Practice Guidelines (2012) ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developedin collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J 33:1787–1847. https://doi.org/10.1093/eurheartj/ehs104
Acknowledgements
We thank CRDC multi-center co-authors as above for assistance with cases collections
Funding
This study was supported by the CAMS Innovation Fund for Medical Sciences (CIFMS) (2019-I2M-2–008).
Author information
Authors and Affiliations
Contributions
Min Hui and Jiaxin Zhou: Data curation, Writing-Original draft preparation.
Liyun Zhang and Xinwang Duan: Supervision.
Mengtao Li and Qian Wang: Visualization, Investigation.
Jiuliang Zhao: Conceptualization, Methodology, Software.
Yong Hou: Software, Validation.
Dong Xu and Xiaofeng Zeng: Writing- Reviewing and Editing.
Corresponding authors
Ethics declarations
Ethical approval and consent to participate
This study was approved by Chinese Rheumatism Data Center (CRDC) with the number S-478. Informed consent was obtained.
Consent for publication
Not applicable.
Consent to participate
Not applicable.
Conflict of interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hui, M., Zhou, J., Zhang, L. et al. Prevalence and risk factors for left ventricular diastolic dysfunction in systemic sclerosis: a multi-center study of CRDC cohort in China. Clin Rheumatol 40, 4589–4596 (2021). https://doi.org/10.1007/s10067-021-05804-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-021-05804-6