Summer - United States Special Operations Command
Summer - United States Special Operations Command
Summer - United States Special Operations Command
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
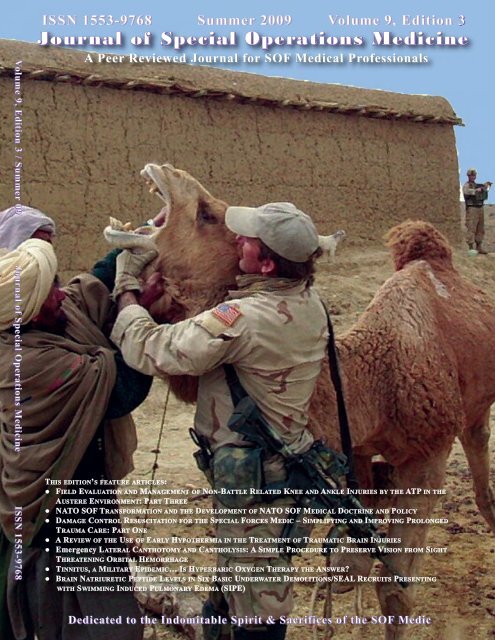
Volume 9, Edition 3 / <strong>Summer</strong> 09 Journal of <strong>Special</strong> <strong>Operations</strong> Medicine ISSN 1553-9768ISSN 1553-9768 <strong>Summer</strong> 2009 Volume 9, Edition 3Journal of <strong>Special</strong> <strong>Operations</strong> MedicineA Peer Reviewed Journal for SOF Medical ProfessionalsTHIS EDITION’S FEATURE ARTICLES:● FIELD EVALUATION AND MANAGEMENT OF NON-BATTLE RELATED KNEE AND ANKLE INJURIES BY THE ATP IN THEAUSTERE ENVIRONMENT: PART THREE● NATO SOF TRANSFORMATION AND THE DEVELOPMENT OF NATO SOF MEDICAL DOCTRINE AND POLICY● DAMAGE CONTROL RESUSCITATION FOR THE SPECIAL FORCES MEDIC – SIMPLIFYING AND IMPROVING PROLONGEDTRAUMA CARE: PART ONE● A REVIEW OF THE USE OF EARLY HYPOTHERMIA IN THE TREATMENT OF TRAUMATIC BRAIN INJURIES● Emergency LATERAL CANTHOTOMY AND CANTHOLYSIS: A SIMPLE PROCEDURE TO PRESERVE VISION FROM SIGHTTHREATENING ORBITAL HEMORRHAGE● TINNITUS, A MILITARY EPIDEMIC… IS HYPERBARIC OXYGEN THERAPY THE ANSWER?● BRAIN NATRIURETIC PEPTIDE LEVELS IN SIX BASIC UNDERWATER DEMOLITIONS/SEAL RECRUITS PRESENTINGWITH SWIMMING INDUCED PULMONARY EDEMA (SIPE)Dedicated to the Indomitable Spirit & Sacrifices of the SOF Medic
Journal of <strong>Special</strong> <strong>Operations</strong> MedicineEXECUTIVE EDITORDeal, Virgil T. MD, FACSVirgil.Deal@socom.milMEDICAL EDITORGilpatrick, Scott, APA-C, DMOMANAGING EDITORLanders, Michelle DuGuay, MBA, BSNDuguaym@socom.milASSISTANT EDITORCONTRIBUTING EDITORParsons, Deborah A., BSNSchissel, Daniel J., MD(“Picture This” Med Quiz)CME MANAGERSKharod, Chetan U. MD, MPH -- USUHS CME SponsorOfficersEnlistedLanders, Michelle DuGuay, MBA, BSNMcDowell, Doug, PA-CDuguaym@socom.milDouglas.McDowell@socom.milEDITORIAL BOARDAckerman, Bret T., DOAnders, Frank A., MDAntonacci Mark A., MDBaer David G., PhDBaskin, Toney W., MD, FACSBlack, Ian H., MDBower, Eric A., MD, PhD, FACPBriggs, Steven L., PA-CBruno, Eric C., MDCloonan, Clifford C., MDColdwell, Douglas M., PH.D., M.D.Davis, William J., COL (Ret)Deuster Patricia A., PhD, MPHDiebold, Carroll J. , MDDoherty, Michael C., BA, MEPC, MSSFlinn, Scott D., MDFudge, James M., DVM, MPVMGandy, John J., MDGarsha, Larry S., MDGephart, William, PA-SGerber, Fredrick E., MMASGiebner, Steven D., MDGiles, James T., DVMGreydanus, Dominique J., EMT-PGoss, Donald L.,DPT, OCS, ATC, CSCSGodbee, Dan C., MDHarris, Kevin D., DPT, OCS, CSCSHammesfahr, Rick, MDTEXT EDITORSAckermann, Bret T. DO, FACEPBoysen, HansDoherty, Michael C., BA, MEPC, MSSGephart, William J., PA-SGodbee, Dan C., MD, FS, DMOVanWagner, William, PA-CJournal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09Holcomb, John B., MDKauvar, David S., MDKersch, Thomas J., MDKeenan, Kevin N., MDKirby, Thomas R., ODKleiner Douglas M., PhDLaPointe, Robert L., SMSgt (Ret)Llewellyn, Craig H., MDLorraine, James R., BSNLutz, Robert H., MDMason, Thomas J. MDMcAtee, John M., PA-CMcManus, John G., MDMouri, Michael P., MD, DDSMurray Clinton K., MD, FACPOng, Richardo C., MDOstergaard, Cary A., MDPennardt, Andre M., MDPeterson, Robert D., MDRiley, Kevin F., PhD, MSCRisk, Gregory C., MDRosenthal, Michael D. PT, DScTaylor Wesley M. DVMTubbs, Lori A., MS, RDVanWagner, William, PA-CWedmore, Ian S., MD, FACEPWightman, John M., EMT-T/P, MDYevich, Steven J., MDHesse, Robert W., RN, CFRN, FP-CKleiner, Douglas M.Mayberry, Robert, RN, CFRN, EMT-PParsons, Deborah A., BSNPeterson, Robert D., MD
An 18D deworms a camel during a “Vet Cap” in Shkihn, Afghanistan.ISSN 1553-9768From the EditorThe Journal of <strong>Special</strong> <strong>Operations</strong> Medicine (JSOM) is an authorized official military quarterly publication of the <strong>United</strong> <strong>States</strong> <strong>Special</strong><strong>Operations</strong> <strong>Command</strong> (USSOCOM), MacDill Air Force Base, Florida. The JSOM is not a publication of the <strong>Special</strong> <strong>Operations</strong> MedicalAssociation (SOMA). Our mission is to promote the professional development of <strong>Special</strong> <strong>Operations</strong> medical personnel by providing a forumfor the examination of the latest advancements in medicine and the history of unconventional warfare medicine.JSOM Disclaimer Statement: The JSOM presents both medical and nonmedical professional information to expand the knowledge ofSOF military medical issues and promote collaborative partnerships among services, components, corps, and specialties. It conveys medicalservice support information and provides a peer-reviewed, quality print medium to encourage dialogue concerning SOF medical initiatives.The views contained herein are those of the authors and do not necessarily reflect the Department of Defense. The <strong>United</strong> <strong>States</strong> <strong>Special</strong><strong>Operations</strong> <strong>Command</strong> and the Journal of <strong>Special</strong> <strong>Operations</strong> Medicine do not hold themselves responsible for statements or products discussedin the articles. Unless so stated, material in the JSOM does not reflect the endorsement, official attitude, or position of the USSO-COM-SG or of the Editorial Board.Content: Content of this publication is not copyrighted. Published works may be reprinted provided credit is given to the JSOM and the authors.Articles, photos, artwork, and letters are invited, as are comments and criticism, and should be addressed to Editor, JSOM, USSOCOM,SOC-SG, 7701 Tampa Point Blvd, MacDill AFB, FL 33621-5323. Telephone: DSN 299-5442, commercial: (813) 826-5442, fax: -2568; e-mailJSOM@socom.mil.The JSOM is indexed with the National Library of Medicine (NLM) and included in MEDLINE. Citations from the articles indexed,the indexing terms, and the English abstract printed in the journal will be included and searchable using PubMed. The JSOM is serial indexed(ISSN) with the Library of Congress and all scientific articles are peer-reviewed prior to publication. The Journal of <strong>Special</strong> <strong>Operations</strong> Medicinereserves the right to edit all material. No payments can be made for manuscripts submitted for publication.Distribution: This publication is targeted to SOF medical personnel. There are several ways for you to obtain the Journal of <strong>Special</strong> <strong>Operations</strong>Medicine (JSOM). 1) USSOCOM-SG distributes the JSOM to all our SOF units and our active editorial consultants. 2) SOMA membersreceive the JSOM as part of membership. Please note, if you are a SOMA member and are not receiving the subscription, you cancontact SOMA through http://www.trueresearch.org/soma/ or contact Jean Bordas at j.bordas@trueresearch.org. SOMA provides avery valuable means of obtaining SOF related CME, as well as an annual gathering of SOF medical folks to share current issues. The JSOMis also available online throught the SOMA website. 3) For JSOM readers who do not fall into either of the above mentioned categories, theJSOM is available through paid subscription from the Superintendent of Documents, U.S. Government Printing Office (GPO), for only $30 ayear. Superintendent of Documents, P.O. Box 371954, Pittsburgh, PA 15250-7954. GPO order desk -- telephone (202) 512-1800; fax (202) 512-2250; or visit http://bookstore.gpo.gov/subscriptions/alphabet.html. You may also use this link to send a email message to the GPO Order Desk— orders@gpo.gov. 4) The JSOM is online through the Joint <strong>Special</strong> <strong>Operations</strong> University’s new SOF Medical Gateway; it is available to allDoD employees at https://jsoupublic.socom.mil/. Click on medical – Click on Journal Icon – Then click on the year for specific journal.We need continuing medical education (CME) articles!!!! In coordination with the Uniformed Services University of Health Sciences(USUHS), we offer CME/CNE to physicians, PAs, and nurses. SOCOM/SG Education and Training office offers continuing educationcredits for all SF Medics, PJs, and SEAL Corpsmen.JSOM CME consists of an educational article which serves to maintain, develop, or increase the knowledge, skills, and professionalperformance and relationships that a physician uses to provide services for patients, the public, or the profession. The content of CME is thatbody of knowledge and skills generally recognized and accepted by the profession as within the basic medical sciences, the discipline of clinicalmedicine, and the provision of healthcare to the public. A formally planned Category 1 educational activity is one that meets all accreditationstandards, covers a specific subject area that is scientifically valid, and is appropriate in depth and scope for the intended physician audience.More specifically, the activity must:• Be based on a perceived or demonstrated educational need which is documented• Be intended to meet the continuing education needs of an individual physician or specific group of physicians• Have stated educational objectives for the activity• Have content which is appropriate for the specified objectives• Use teaching/learning methodologies and techniques which are suitable for the objectives and format of the activity• Use evaluation mechanisms defined to assess the quality of the activity and its relevance to the stated needs and objectivesTo qualify for 1 CME, it must take 60 min to both read the article and take the accompanying test. To accomplish this, your articlesneed to be approximately 12 ─ 15 pages long with a 10 ─ 15 question test. The JSOM continues to survive because of the generous and timeconsumingcontributions sent in by physicians and SOF medics, both current and retired. See Submission Criteria in the back of this journal.We are looking for SOF-related articles from current and/or former SOF medical veterans. We want articles that deal with trauma, orthopedicinjuries, infectious disease processes, and/or environment and wilderness medicine. Mostly, we need you to write CME articles. Help keep eachother current in your re-licensure requirements. Don’t forget to send photos to either accompany the articles, or alone to be included in the PhotoGallery associated with medical guys and/or training. If you have contributions great or small… send them our way. Our e-mail is:JSOM@socom.mil.Lt Col Michelle DuGuay LandersFrom the Editor
<strong>Summer</strong> 09 Volume 9, Edition 3FEATURE ARTICLESField Evaluation and Management of Non-Battle Related 1Knee and Ankle Injuries by the ATP in the AustereEnvironment: Part ThreeJ.F. Rick Hammesfahr, MDNATO SOF Transformation and the Development of 7NATO SOF Medical Doctrine and Policy.LTC G. Rhett Wallace, MD FAAFPDamage Control Resuscitation for the <strong>Special</strong> Forces 14Medic: Simplifying and Improving Prolonged TraumaCare: Part OneCOL Gregory Risk MD; Michael R. Hetzler 18DReview Article of the Use of Early Hypothermia in the22Treatment of Traumatic Brain InjuriesJess Arcure BS, MSc; Eric E. Harrison MDEmergency Lateral Canthotomy and Cantholysis: 26A Simple Procedure to Preserve Vision from SightThreatening Orbital HemorrhageCPT Steven Roy Ballard, MD; COL Robert W. Enzenauer,MD, MPH; Col (Ret) Thomas O’Donnell, MD; James C.Fleming, MD; COL Gregory Risk, MD, MPH, FACEP;Aaron N. Waite, MDTinnitus, a Military Epidemic… Is Hyperbaric Oxygen 33Therapy the Answer?LCDR Thomas M. Baldwin, MD, MPTBrain Natriuretic Peptide Levels in Six Basic UnderwaterDemolitions/SEAL Recruits Presenting with SwimmingInduced Pulmonary Edema (SIPE)LCDR Damon Shearer (DMO/UMO) MDCDR Richard Mahon (DMO/UMO) MDAbstracts from Current Literature 51Previously Published 59Contents● Central Retinal Vein Occlusion in an Army Ranger withGlucose-6-Phosphate Dehydrogenase Deficiency● Should We Teach Every Soldier How to Start an IV?● Psychological Resilience and Postdeployment Social SupportProtect Against Traumatic Stress and DepressiveSymptoms in Soldiers Returning From <strong>Operations</strong> EnduringFreedom and Iraqi Freedom● Psychosocial Buffers of Traumatic Stress, Depressive Symptoms,and Psychosocial Difficulties in Veterans of <strong>Operations</strong>Enduring Freedom and Iraqi Freedom: The Role ofResilience, Unit Support, and Postdeployment SocialSupport44Editorials 79LTC Craig Myatt, PhD; Douglas C. Johnson, PhDBook Reviews 81● Blackburn’s Headhunters● The Battle of Mogadishu: Firsthand Accounts from the Menof Task Force RangerFrom the USSOCOM <strong>Command</strong> Surgeon 86COL Tom DealComponent Surgeons 87COL Peter BensonBrig Gen (S) Bart IddinsCAPT Jay SourbeerCAPT Anthony GriffayUSASOCAFSOCNAVSPECWARMARSOCTSOC Surgeons 92COL Rocky FarrSOCCENTCOL Frank NewtonUSASFC Surgeon 96LTC Andrew LandersSOCPACNATO Surgeon 97LTC Rhett WallaceUSSOCOM Psychologist 99LTC Craig Myatt, PhDUSSOCOM Veterinarian 101LTC Bill Bosworth, DVMNeed to Know 104Navy Safe HarborSOF Reading List 105Educational Resources 121Photo Gallery 127Meet the JSOM Staff 129Submission Criteria 130Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
Field Evaluation and Management of Non-BattleRelated Knee and Ankle Injuries by the ATP in theAustere Environment — Part ThreeJF Rick Hammesfahr, MDEditor’s Note: Part Three consists of ankle injury evaluation and taping.Part Two (taping procedures for the various knee injuries) was published in the JSOM Spring 09, Vol 9 Ed 2.Part One (evaluation of knee injuries) was published in the JSOM Winter 09, Vol 9 Ed 1.ANKLEThe most commonly injured ankle ligament isthe anterior talo-fibular ligament (ATFL) located at theanterolateral aspect of the ankle (Figure 58).Figure 59: Plantarflexion and inversion ofthe ankle leads to abnormal stretching andtearing of the anterior talo-fibular ligament(ATFL).Figure 58: Anterior talo-fibular ligament locationat the anterolateral aspect of the ankle.With respect to ankle sprains and injury to theATFL, the typical mechanism of injury involves a forcedmotion that is best described as a plantarflexion – inversiondeforming force (Figure 59).This injury is often accompanied by a history ofa pop; the patient often states that they rolled their ankle;there is pain and swelling with the most intense area ofsymptoms located at the anterolateral aspect of the ankle.When intact, the ATFL goes from the distal aspectof the fibula to the talus. In this position, it acts asa checkrein to prevent abnormal posterior subluxationof the tibia relative to the talus (Figure 60).Figure 60: Intact AFTL preventssubluxation of the tibia and fibularcomplex relative to the talus.Field Evaluation and Management of Non-Battle Related Knee and Ankle Injuries by the ATP in theAustere Environment — Part Three1
In testing for stability of the ATFL, which is amajor stabilizer of the ankle, an anterior drawer test isperformed. This is done much like the anterior drawertest of the knee. The knee is flexed to 90 degrees andthe foot is stabilized (Figure 61). By applying an anteriorlydirected force to the calcaneus, or by stabilizing thefoot, and then applying a posteriorly directed force to thetibia, the stability of the lateral ankle ligaments are tested.Figure 63: Torn ATFL with posterior tibia and fibula subluxation.Although xray stress views are shown for teachingpurposes, the posterior “clunk” as the bones sublux isreadily felt and may be visualized in most patients.Figure 61: Anterior drawer test of the ankle. With aposteriorly directed force applied to the tibia, and withthe foot stabilized, there is no subluxation of the tibiaand fibula posterior on the talus.If the ATFL is torn, the tibia and fibula will subluxposteriorly (Figure 62 and 63). It should be notedthat this test should always be performed with the kneeflexed. With the knee extended, there is false stabilitywhen doing the test.The treatment for an ankle sprain is to preventthe deforming forces of plantarflexion and inversion.This is performed by taping the ankle followed by administrationof non-steroidal anti-inflammatory medication.Further evaluation upon return to base isabsolutely required. Most likely the mission can becompleted.ANKLE TAPINGJust as with the knee, the taping at the ankle beginswith applying anchoring strips. The anchoringstrips are usually overlapped by approximately 30-50%.This taping method is demonstrated using two colors oftape so that the overlap and position of the tape may bebetter appreciated. As with taping the knee, the skinshould be clean and dry. If possible, shave the hair priorto tape application. However, tape should NOT be appliedover open wounds.Start by placing the ankle in the neutral position,perpendicular to the lower leg (Figure 64).Figure 62: Torn ATFL with posterior tibia andfibular subluxation on the talus after applyinga posteriorly directed force.Figure 64: Start with the ankle perpendicular to theforeleg and everted if possible.2Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
The circumferential anchoring strips are appliedwith approximately a 30%-50% overlap (Figure65). Strips are applied at the metatarsal phalangeal regiondistally as well as approximately half way up theforeleg.Figure 67: Second hindfoot anchoring strip applied.Figure 65: Proximal and distal anchoring strips.Following the basic anchoring strips, U-shapedstrips are applied. When applying these strips, startproximally and medially. As the tape is applied, thehindfoot is pulled into eversion, to decrease the stresson the damaged ATFL region. This allows for stabilityof the ankle with respect to inversion and eversion (Figure66 and 67).After two of these strips have been applied,U-shaped strips are applied beginning at the medialaspect of the foot and then continuing posterior to theankle, ending at the distal lateral aspect of the foot.This aids in stability of forefoot adduction and aids instability of inversion (Figure 68 and 69).Figure 68: Initial horizontal foot/ankle anchoring strip.Figure 66: Pull tape strips from medial to lateral toevert the hindfoot.Figure 69: Second horizontal foot/ankle anchoringstrip.Field Evaluation and Management of Non-Battle Related Knee and Ankle Injuries by the ATP in theAustere Environment — Part Three3
After completion of these two strips, the anchoringstrips (or heel lock taping) to specifically resistinversion are applied. The tape is started at themedial aspect of the ankle (Figure 70).Figure 72: Pull the ankle into eversion as the tape isapplied to the lateral border of the heel and ankle.Figure 70: Start at the proximal medial ankle with theheel lock tape strip.Finally, continue to pull the heel into eversion asthe tape is pulled to the medial side of the foreleg (Figure73).Pull the tape across the plantar aspect of theheel (Figure 71),Figure 73: Completed application of the heel locktape strip.Figure 71: Plantar application of the heel lock.The heel lock tape strip essentially pulls theankle into a position of eversion which takes the stressoff the damaged ligaments. Once the first heel lock stripis applied, three or four more are then placed (Figure 74-76).As the tape is pulled proximally and laterallyacross the lateral border of the heel and ankle, the heeland ankle should be everted to further increase the efficiencyof the heel lock tape strip and thereby decreaseany stress on the injured ATFL region (Figure 72).Figure 74: Completion of second heel lock strip.4Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
In doing so, all the skin is closed and coveredwith tape with the exception of the open area at theheel. This is done because ankle injuries are associatedwith a lot of swelling. If there are any breaks inthe tape and if skin is allowed to “peek” through thetape, this area will develop a very painful tape blister,which in the austere environment runs the risk of becominginfected (Figure 78).Figure 75: Starting the third heel lock strip.Figure 78: Complete taping with the heel left open.Figure 76: Completion of four heel lock strips.Once these strips have been applied, additionalcircumferential strips are applied (Figure 77).This type of taping results in excellent stabilityof the ankle joint. Obviously, the patient cannot returnto totally normal activities although he shouldremain functional.To appreciate the amount of stability that tapingprovides, look at the amount of inversion possiblein the untaped ankle (Figure 79) as opposed to thetaped ankle (Figure 80).Figure 77: Circumferential anchoring strips appliedto the foreleg and foot.Figure 79: Significant inversion of untaped ankle.Field Evaluation and Management of Non-Battle Related Knee and Ankle Injuries by the ATP in theAustere Environment — Part Three5
Figure 80: Minimal inversion of taped ankle asdetermined by inability to invert ankle/foot andraise the1st MTP joint off of the floor.GENERAL PRINCIPLES AND GUIDELINESIn trying to anticipate return to activity, ideallythere is no swelling or effusion, the patient has fullrange of motion and approximately 90% of normalstrength. However, the treating ATP must be awarethat as swelling decreases, the pain decreases and themotion increases. This gives a very false sense of healing.In fact, the symptoms will often disappear approximatelyfour weeks prior to completion of healing.Obviously, this sets up the situation whereby the patientis relatively asymptomatic, the healing is immatureand not complete, and a premature return toactivity leads to an extremely high re-injury rate.In general, successful treatment of non-battlefieldrelated knee and ankle injuries, in the austere situation,so that the patient may remain functional, requires severalthings:• The ATP must understand the anatomy involved.• He must know the questions to ask to identifythe mechanism of injury.• The ATP must understand the taping principles.• He must recognize that the taping is designedto support the injured tissue and decrease thestress load on the injury. To determine thetype of taping and to apply it successfully, itis obviously necessary to have a high probability of a working diagnosis.• He must know the possible diagnoses affectinga joint given a set of physical findingsand a mechanism of injury• Most importantly, a minimum of six weeksof healing is required, regardless of what thepatient says or how the patient feels.• The absence of pain does not equal healing• All of the injuries discussed here are significantinjuries that absolutely require furthermedical evaluation upon return to base.REFERENCEPerrin, David. (2005). Taping and Bracing, HumanKinetics.This completes our three-part series.JF Rick Hammesfahr, M.D. graduated from Colgate University in 1973 and the College of Medicineand Dentistry of New Jersey in 1977. He was Chief Resident in Orthopaedics at Emory Universityfrom 1980-1982. In addition to receiving numerous surgical awards, he has been on the speaking facultyof numerous medical and orthopaedic meetings serving as the co-director of several courses onknee surgery. His publications have focused on tactical medicine, arthroscopy, calcaneal fractures, abductorparalysis, wound healing, running injuries, meniscal repair, septic knees, and sports medicine.He has written two book chapters, one book, published 22 articles, serves on the editoral review boardof multiple medical journals, is a chief editor of the “Ranger Medic Handbook,” and has presented over120 CME lectures and talks on orthopedics and sports injuries.Dr Hammesfahr has served as president of the largest regional orthopaedic association, the Southern OrthopaedicAssociation. Currently, he is the Director of the Center for Orthopaedics and Sports Medicine and serves as the Chairmanof the USSOCOM Curriculum and Examination Board.6Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
NATO SOF Transformation and theDevelopment of NATO SOF MedicalDoctrine and PolicyG. Rhett Wallace, MD, FAAFPABSTRACTThe North Atlantic Treaty Organization (NATO) <strong>Special</strong> <strong>Operations</strong> Forces (SOF) Coordination Center(NSCC) is a new NATO memorandum of understanding (MOU) organization that is effecting rapid advancementin NATO’s ability to efficiently utilize SOF at the strategic/operational level. The NSCC’s lines ofdevelopment in communications information systems (CIS), education, training, and real life support to the InternationalSecurity Assistance Force (ISAF) SOF and the development of pivotal documents to develop and matureNATO SOF doctrine and policy are all occurring at lightning speed. Within this process of establishing aSOF community in NATO, the author’s focus is the development of previously non-existent NATO SOF medicaldoctrine and policy. Many barriers to change lie ahead, but through unity of effort, we will ensure certaintyof our actions.The focus of this article is to give a briefoverview of the development of the NATO SOF TransformationInitiative (NSTI), highlight the establishmentof the NSCC, and discuss the development ofNATO SOF medical doctrine and policy that willshape how NATO SOF operations are medicallyplanned and supported in current and future operations.The NSTI concept began in the spring of 2006as a multinational call to the Supreme Allied <strong>Command</strong>erEurope (SACEUR), the commanding officerof NATO’s Allied <strong>Command</strong> for <strong>Operations</strong> (ACO),Supreme Headquarters Allied Powers Europe(SHAPE). Several nations saw a need to develop aSOF capability for NATO, addressing gaps in NATO’sability to strategically and operationally employ nationalSOF elements in a cohesive alliance or coalitionenvironment.While NATO is established in accordancewith Article 51 of the <strong>United</strong> Nations Charter as a politicalalliance with a military branch organized for collectivedefense, NATO’s focus has historically beenbased on the conventional aspects of the alliance’s militarypower. Because of this, NATO’s motivations forchange were the identified gaps in its “response to unconventionalthreats that recognize no national boundaries,show open contempt for human rights, andinternational rule of law.” 1 As a result, in November2006, at the Riga Summit in Latvia, President GeorgeW. Bush, as the Dean of the North Atlantic Council(NAC), announced the NAC’s endorsement of theNSTI, with the NSCC, frame-worked by the <strong>United</strong><strong>States</strong>, as the centerpiece. 2The NSCC was established as a coordinationcenter under a memorandum of understanding (MOU)to streamline its development and implementation. The<strong>United</strong> <strong>States</strong> volunteered to be the framework nation,with Vice Admiral William McRaven, then the <strong>Command</strong>er,<strong>Special</strong> <strong>Operations</strong> <strong>Command</strong> Europe(SOCEUR), in Stuttgart, Germany, as its first “dualhatted”Director. With an initial cadre of 17 personnelselected from the SOCEUR Joint Staff, the intent wasto build the NSCC at Stuttgart, where it would remainfor three to five years before relocating to SHAPE.However, realignment of organizations at SHAPE allowedthe NSCC to transfer much earlier than expected,and in the summer of 2007, it was moved toSHAPE. Today, the NSCC has a staff of 110 multinationalpersonnel, having reached initial operational capabilityin August, 2008, with full operationalcapability expected by the end of May 2009, along withthe arrival of anoher 32 personnel. Most recently, as aresult of the NATO Summit in Strasbourg, the NSCChas been tasked to plan for a way ahead to move beyonda coordination center and to establish a full SOFheadquarters for NATO.The mission of the NSCC is to enable and supportNATO <strong>Special</strong> <strong>Operations</strong> Forces as the focalpoint for strategic SOF advice and operational planningto the NATO chain of command. This is accomplishedby providing subject matter expertise to theSACEUR and Joint Force <strong>Command</strong>s (JFCs) andtranslating strategic estimates into operational requirements.In addition, the NSCC is responsible for coordinationand synchronization of NATO SOF in theNATO SOF Transformation and the Development of NATO SOF Medical Doctrine and Policy7
force generation process, the development of NATO SOFpolicy and doctrine, and fostering interoperability andstandardization. In the area of interoperability, the NSCCfocuses on NATO SOF education, training, and exercises. 3The NSCC is aggressively accomplishing the goalsoutlined by the NAC and Military Committee. InitialNATO SOF operational concepts at the strategic and operationallevel were developed in the NSCC Handbook,and formalized in the development and ratification of theMilitary Committee’s documentation of NATO SOF Policyand Allied Joint Publication (AJP) 3.5. 4,5 Throughthese foundational documents, NATO has set the frameworkfor development of a SOF structure, doctrine, andpolicy. As one would expect, the complexities of coordinatingSOF from 23 different nations’ calls for concentratingon the basics. With this in mind, the missions ofNATO SOF are very straightforward. 61. SPECIAL RECONNAISSANCE AND SURVEILLANCE (SR)SR complements national and Allied theater intelligencecollection assets and systems by “obtaining specific,well-defined, and possibly time-sensitiveinformation of strategic or operational significance.” Itmay complement other collection methods where constraintsare imposed by weather, terrain-masking, hostilecountermeasures or other systems availability. SR is apredominately Human Intelligence (HUMINT) functionthat places “eyes on target” in hostile, denied, or politicallysensitive territory. SOF can provide timely analysisby using their judgment and initiative in a way that technicalintelligence, surveillance, target, acquisition,and reconnaissance(ISTAR) cannot. SOF may conductthese tasks separately, supported by, or in conjunctionwith, or in support of other component commands. Theymay use advanced reconnaissance and surveillance techniques,equipment, and collection methods, sometimesaugmented by the employment of indigenous assets.2. DIRECT ACTION (DA)These are precise operations that are normallylimited in scope and duration. They usually incorporatea planned withdrawal from the immediate objective area.DA is focused on “specific, well-defined targets of strategicand operational significance, or in the conduct of decisivetactical operations.” SOF may conduct these tasksindependently, with support from conventional forces, orin support of conventional forces.3. Military Assistance (MA)MA is a broad spectrum of measures in support offriendly forces throughout the spectrum of conflict. MAcan be conducted “by, with, or through friendly forces thatare trained, equipped, supported, or employed in varyingdegrees by SOF.” The range of MA is thus considerableand may vary from providing low-level military trainingor material assistance to the active employment ofindigenous forces in the conduct of major operations.4. OTHER MISSIONSOther missions include, but are not limited to,supporting counter-irregular threat activities, counteringchemical, biological, radiological, and nuclear (CBRN)weapons, hostage release operations, and faction liaison.In order to manage the wide range of missionsand requirements, one of the first things the NSCC addressedwas the lack of a common CIS by developingand fielding a NATO SOF common CIS network. Fortunately,an existing system, called the Battlefield InformationCollection and Exploitation System (BICES),was already available within NATO. Intended to be usedfor the intelligence community, BICES proved itself asan ideal means for further expansion to support of NATOSOF operational activities. Because BICES has a NATOSecret and Unclassified version, it is ready-made as asystem for collaboration of all allied or coalition SOF.In addition, BICES offers the ability to allow non-NATOnations to participate, enabling an even greater fusion ofintelligence, and wider synchronization of operations.The development of hardware, software, and deployablecontainer packages for NATO SOF is now ongoing. Theintent is to expedite fielding to the ISAF SOF Headquartersin Afghanistan, supporting the already establishedISAF SOF Fusion Cell.On the interoperability front, the NSCC is addressingstandardization and interoperability of internationalSOF by the development of NATO SOF StaffOfficers Course, NATO SOF Combined Joint Forces<strong>Special</strong> <strong>Operations</strong> Component <strong>Command</strong> (CJFSOCC)Planners Course, NATO SOF Intelligence Course, aNATO <strong>Special</strong> <strong>Operations</strong> Air Planners Course, and theNATO ISAF Pre-trainer Course. These courses are augmentedby products such as the CJFSOCC and <strong>Special</strong><strong>Operations</strong> Task Group (SOTG) Handbooks. Thesehandbooks cover the organization and staff functionswithin the CJFSOCC and at the SOTG level, their relationshipto other commands, and liaison roles and responsibilities.Other areas covered include SOFplanning, information operations, air support, targeting,battle tracking, intelligence, logistics, Force Health Protection(FHP), and communications. They provide toolsfor developing a common understanding of the CJF-SOCC and SOTG structure, implementation, responsibilities,and procedures within the Combined Joint TaskForce (CJTF) construct. As NATO SOF contributes to8Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
current and future operations, these tools will cultivatefuture development of NATO SOF doctrine and policy.To understand the basis for the foundationalwork in developing NATO SOF medical doctrine, wemust first understand NATO conventional medical support,and the gaps in NATO’s conventional health servicesupport (HSS) and FHP. NATO medical doctrinecan be reviewed in depth in AJP 4.10 and MC 326/2. 7NATO FHP is a patriarchal system primarily organizedaround fixed medical treatment facilities (MTFs) basedon Allied Nations HSS provided to NATO operations.NATO defines roles of medical care as:Role 1 is the lowest level at which a physiciantreats casualties. Role 1 provides advanced trauma/tacticalmedical care to stabilize and prepare casualties forevacuation to Role 2/3.Role 2 is the first level at which damage controlsurgery (DCS) is performed. Role 2 has two sub-categories:Role 2 Enhanced (Role 2E) – a “mobile” MTFthat it is put in place, but a logistical burden to moveonce in place, and Role 2 Light Maneuver (Role 2LM)– again a “mobile” DCS capability intended to supportInfantry or SOF. However, National Role 2LM is oftentoo heavy and immobile to adequately support infantryor SOF advancing on maneuvers.Role 3 is the level at which primary surgery islocated, and typically has advanced or sub-specialty surgicalservices associated. Role 3 MTFs generally providearea support within a Joint Operational Area (JOA).Role 4 is generally a national fixed MTF.NATO has standardization agreements(STANAGs) 8 and allied medical publications (AMedP) 9that address medical standards for individual trainingand equipment. These are currently being updated andspecifically identify or limit doctors as the personnel tobe trained with advanced medical techniques. AMedP-17 is the first NATO publication to recognize the term“medic,” and apply it to non-credentialed providers.Medic is not a formal definition in Allied AdministrativePublication-6 (AAP-6). 10 For example, Annex A2 11 outlineswhat medical procedures “Independent medics”may perform; these are by exception restricted to noninvasivetechniques. Annex B 12 refers to “doctors”when outlining minimum requirements for medicaltraining of medical personnel. Within NATO’s policieson individual training, many contributing nations do nothave civilian equivalent “medical providers” outside ofcredentialed doctors or nurses. This highlights variationsin acceptable standards of care within NATO; forexample, Nation “X” records reservations to AMedP-17 stating “medical and surgical treatment techniquescan only be applied by physicians.” 13As the Senior Medical Advisor (MEDAD) forthe NSCC, the author is working to establish a commondescription of NATO SOF medical capability, definingSOF medical doctrine and policy, developing a “scopeof practice” for SOF medics, and to provide guidance topromote the highest quality, evidence-based healthcarewithin NATO SOF. By defining NATO SOF medicalprofessionals, and providing a definition for standardizedSOF medical capability, the author is striving to establishstandards for NATO SOF medical professionalsto meet relative to educational preparation, professionalstanding, and technical ability. These standards are met,in part, by the application for – and maintenance ingood standing of – a license or certificate in nations thathave civilian equivalent medical care providers, and/ora NATO SOF Advanced Tactical Provider (ATP) typeregistration based on the proposed “scope of practice,”along with the ACO MEDAD and the Committee of theChiefs of Military Medical Services (COMEDS) guidanceon common medical standards and clinical governancein NATO. 14The author defines NATO SOF medical professionalindividual tasks using the Battle Focus Trainingmodel, basing essential core tasks on the unit’sMission-Essential Task List (METL). AJP 3.5 and MC437/1 provide the definition for NATO SOF elements,and authorize missions SOF will conduct under the alliance.NATO SOF are specially organized, trained, andequipped military forces to achieve military strategic oroperational objectives by unconventional militarymeans in hostile, denied, or politically sensitive areas.These operations are conducted across the full range ofmilitary operations, independently or in conjunctionwith conventional forces. Political-military considerationsoften shape SOF operations, requiring discreet,covert, or low visibility techniques that may include operationsby, with, and through indigenous forces.SOF operations differ from conventional operationsin the degree of physical and political risk, operationaltechniques, modalities of employment, andindependence from friendly support. Due to the natureof NATO SOF operating in remote, austere, at timesprimitive conditions, at the operational extremes, outsideof conventional forces direct or indirect support,SOF Soldiers and SOF medical professionals shouldpossess and maintain medical skills equal to and abovethose required to support conventional forces. It is criticalthat SOF Soldiers and SOF medical professionalsbe fully trained initially, and have robust medical sus-NATO SOF Transformation and the Development of NATO SOF Medical Doctrine and Policy9
tainment training programs on a broad spectrum of primaryand emergency medical care techniques, as wellas, preventive medicine, zoonotic and parasitic diseases,veterinarian care, dental care, CBRN, advancedtrauma, pharmacology, life saving or sustaining invasivesurgical and anesthesia techniques. These skillsare essential to provide adequate medical force protectionsupport for NATO SOF, and are the basis forpromoting SOF medical professional standardizedtraining and promoting interoperability of capabilityand medical equipment.Once established, NATO SOF medical trainingguidance will identify the essential components forindividual and collective medical training. Due to thebroad definition of SOF, specific SOF units will havedifferent training needs and requirements based on environment,location, equipment, dispersion, and similarfactors. SOF operating in a variety ofenvironments, such as hypo/hyperbaric conditions, extremesof heat and cold, mountains or high altitude,should augment the unit level medical training plan toaccount for medically relevant and specific diagnosisand treatments. Therefore, the SOF medical trainingguidance should be used as a guide for conducting unittraining, not as a rigid standard, and designed to assistthe commanders in preparing a SOF unit medical trainingplan which satisfies integration, cross-training, interoperability,and sustainment training requirementsfor NATO SOF medical professionals.Within the past 10 years, SOF LessonsLearned has contributed to advancement in medicalcare from point of injury to primary surgery. 15 Advances,such as SOF tactical combat casualty care(SOF TCCC) training, SOF individual first aid kits(SOF IFAKs), 16 and development of SOF evacuationkits to create casualty evacuation (CASEVAC) platformsout of transportation of opportunity to get casualtiesin austere environments to DCS, have beenpivotal in reducing died of wounds (DOW) rates forSOF Soldiers. 17 These advances are critical to providingadequate SOF HSS. Promoting the understandingthat advanced training and modernized equipment suchas the single handed tourniquet and haemostatic bandagesfor hemorrhage control is good, but DCS or primarysurgery is still required to addressnon-compressible hemorrhage to complete adequateSOF HSS for SOF casualties. Often conventional Role2/3 is unable to meet SOF HSS requirements due tothe great distance or the inflexibility of conventionalstructures to adapt to rapidly changing requirements;other issues revolve around non-existent/inadequatehost national medical support. SOF requires flexible innovativemedical planners to accommodate for gaps incapability. In light of this recurring issue multiple nationshave or are developing a Role 2 ultra-LM elementthat provides a truly light, maneuverable surgical andcritical evacuation team who are familiar with SOF missionsets, tactics and techniques, are operationally readon,small and light enough to maneuver with SOF, andunder the command and control (C2) of the SOF <strong>Command</strong>.The author defines this capability as Role 2 <strong>Special</strong><strong>Operations</strong> Surgical/Evacuation Team (Role 2 SOST).NATO comprehensive political guidance projectsan environment of change that “is and will be complexand global, and subject to unforeseeabledevelopments.” 18 SOF missions and operational conceptsare conducted across the range of military operationsthrough peacetime, conflict, various stages of war,and Article 5 collective defense or non-Article 5 CrisisResponse <strong>Operations</strong>. The SOF TCCC depends on anenhanced capability for first responders, SOF CombatMedic (SOCMs), SOF medical providers (SFMPs), andadaptive standard and non-standard platforms for CA-SEVAC in emergencies. Patients are CASEVAC’d tothe nearest host nation or Role 2/3 MTF capability, butSOF TCCC capabilities are of little benefit if there is notimely resuscitative surgical care available.As defined earlier, SOF operations by nature areremote, austere, and in primitive conditions at operationalextremes outside of conventional forces orfriendly direct or indirect support. SOF operate in smallteams and are often cross-trained in multiple skill sets toensure economy of effort and redundancy of capability.Advanced first responder training is essential for all SOFSoldiers. It is imperative that all SOF Soldiers be crosstrainedas medical first responders.SOF medical professionals can include a widerange of medical and paramedical professions. The followingdescriptions are included to assist in understandingthe capability that each medical professionalprovides as a combat multiplier.NATO in general does not specifically define the“medic.” Conventional medics have the skill sets to provideemergency care and entry level nursing care for patients.They attend a military/civilian medical trainingprogram that provides them with a certification (nationalor military) to provide medical care within their scopeof practice. Course content usually includes, but is notlimited to, trauma management, pre-hospital traumamanagement and care, basic life support (BLS), advancedlife support (ALS), and inpatient nursing skills.They can perform basic medical care under the supervi-10Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
sion of a physician, and limited preventive medicine.They can directly support combat units, ambulanceteams, or Role 1 medical support facilities. 19The author purposes creating a SOF CombatMedic (SOCM) as a new definition to be applied toNATO SOF medical professionals. A SOCM is a Soldiertrained in advanced medical care directly assignedor attached to SOF and who provides direct health servicesupport to <strong>Special</strong> <strong>Operations</strong> Task Units (SOTUs)on operations. SOCMs are trained to initially treat andsustain a casualty from point of injury for up to 36 hoursbefore transfer of the casualty to MEDEVAC or nonstandardmedical treatment facility. SOCMs maintainthe skill set trained to medical first responders, commoncore tasks for conventional medics, advanced tacticalproviders 20 (the DA/SR medical skill sets), preventivemedicine, and environmental/tropical medicine. Initialtraining for SOCMs includes courses in basic humananatomy, basic human physiology, basic medical terminology,pharmacology calculations, and basic math.The SOCM course content should include, but is notlimited to, basic trauma management, pre-hospitaltrauma management and care, advanced trauma life support,BLS, ALS, inpatient/post-operative nursing skills,minor and invasive surgical procedures.The author also purposes creating a SOF medicalprovider (SFMP) as a new definition to be appliedto NATO SOF medical professionals. SFMP was chosento highlight the “independent provider” status of theadvanced training for a SFMP. A SFMP is a SOF Soldiertrained in advanced medical care, or a medical professionaldirectly assigned or attached to SOF and whoprovides direct health service support to SOTUs on operations.SFMPs are trained to operate independentlyfrom the direct supervision of a physician. SFMPs aretrained to initially treat and sustain a casualty from pointof injury for up to 72 hours, and in some mission sets foreven longer periods before transfer of the casualty toMEDEVAC or non-standard medical treatment facility.The SFMPs’ medical skill sets are based on the types ofpatients expected in a conventional forces environment,as well as those in hostile, denied, or politically sensitiveareas. By nature, SOF operations are conducted acrossthe full range of military operations, independently orin conjunction with conventional forces. Political-militaryconsiderations often shape SOF operations, requiringdiscreet, covert, or low visibility techniques thatmay include operations by, with, and through indigenousforces. SOF operations differ from conventionaloperations in degree of physical and political risk, operationaltechniques, modalities of employment, and independencefrom friendly support. These mission requirementsare the nexus for the following list of subjectareas and specific task that are core medical skills to beinitially trained and sustainment training requirementsfor SFMPs. Initial training requirements for SFMPs includeall of the training for SOCMs, with additionaltraining in primary, preventive medicine, anesthesia, andadvanced invasive procedures as described under “primarycare or emergency care doctor.” 21NATO SOFs’ ability to triage, treat, transfer,and recovery of casualties is critical to sustainment andregeneration of the force. Role 2 SOSTs will providethe ability to mitigate death from non-compressiblehemorrhage, the leading cause of death to SOF Soldierswho die of wounds. 22 The Role 2 SOST will be able toperform up to 10 DCSs without re-supply; manage twocritical care patients for up to 48 hours; perform en routecritical care for up to two patients at a time; and integrateseamlessly with SOF. 23SOF medical capabilities have been invaluable inestablishing rapport with allied and coalition regular andirregular forces, assisting the local populace, and counteringenemy propaganda about international motivesand intentions. SOF TCCC, SOCMs, SFMPs, and Role2 SOST capabilities enhance our ability to provide lifesaving treatment to combatants and non-combatants affectingthe outcome of any casualty situation. In additionto saving the lives of SOF Soldiers, coalitionpartners, and non-combatants, it plays a vital role acrossNATO SOF missions. The care provided to indigenouspeople is one of our strongest weapons in the battle for“hearts and minds.” It brings a universal message ofNATO as liberators rather than occupiers and gains popularsupport, willing cooperation, and intelligence. 24With an understanding of the current developmentin defining the capabilities for NATO SOF HSS,let’s review some identified areas that are resistant tochange, or may impede the progress of NSTI withinSOF HSS and FHP.Currently, no centralized knowledge base on allalliance and coalition SOF medical capability exists.The author intends to develop this information for medicalplanning and is continuing dialogue with contributingnations to establish this information. Establishingworking relationships with the ACO MEDAD, JFCs,ISAF, and national SOF medical staff will enable theNSCC to develop this working knowledge, and be ableto advise and assist NATO SOF planners on current andfuture operations.National strategic considerations have limitedwhat information some countries are willing to share inNATO SOF Transformation and the Development of NATO SOF Medical Doctrine and Policy11
egard to their capabilities. The NSCC will continue tofoster a climate of trust. Safeguarding national concernsis essential to information sharing within NATO.Currently, no standardized definition exists forNATO SOF non-credentialed providers. WhereasNATO has policies for doctors and nurses, it has restrictivepolicies for non-credentialed providers.NATO conventional non-credentialed medicalproviders are based on conventional medical supportsystems within MTFs in direct support of or in proximityto a credentialed providers. The author is gatheringnational input and consensus on the proposeddefinitions for NATO SOF medical professionals. Thiswork will be the foundation for development of initialand sustainment medical training requirements withinNATO SOF. The lack of a certain level of SOF medicalprofessional is not a sign of a nation’s inability tosupport SOF, but rather a planning consideration in theforce generation process.European Union and national policies currentlylimit advanced medical training and sustainmenttraining of non-credentialed providers who lack a recognizedcivilian equivalent medical provider. ManyNATO contributing nations have patriarchal civilianmedical systems, where the “doctor” is the primary decisionmaker and completes most invasive procedures;this is reflected in their concepts and policies relatingto HSS. Medical reforms within NSTI will revolvearound lessons learned and the realities of combat casualties’deaths that may ensue as the result of ColdWar medical polices and doctrine based around robusthost nation infrastructure and response. It is imperativethat a system be developed to enable the NSCC to bea gathering point of best SOF medical practices basedon lessons learned fed by input from SOF on currentand recent operations.Some contributing nations have limited or nopermanent medical staff within their national SOFcommand structures that limits their ability to effectivelyinfluence timely change. There are also nationalmedical structures that do not delegate authority ofSOF medical training requirements and points of instructionto their national SOF commands. This can beovercome by education of SOF specific medical requirements,best practices for joint level staffing/manning,SOF medical lessons learned, and best practicesto positively influence international chiefs of medicaldepartments, and mentor NATO SOF members whoare limited by people, funding, technology, or trainingrestrictions.The author will be engaging NATO’s conventionalmedical planners this spring at the NATO MedicalConference where he will highlight similarities andsignificant differences between NATO conventionaland SOF HSS capabilities and identify current gaps inrequirements. The intent will be to stimulate thought,generate dialogue, and make formal contact betweenthe NSCC and national SOF command level medicalstaff. At the NATO Medical Conference in the fall of2009, the author intends to engage NATO and Partnersfor Peace (PfP), SOF Surgeons, and medical plannersin a NATO SOF Medical Working Group (WG) to refineand further develop NATO SOF medical doctrineand policy. The development of an ongoing NATOSOF Medical WG will be reviewed at that time.This article gave a brief overview of the establishmentand development of the NSCC, and reviewedthe NSTI concept development. It proposedthe establishment of new NATO SOF definitions to defineSOF medical capability using the battle focusedtraining model. Through an understanding of the definitionof “SOF medical professionals,” sharing medicalintelligence resources, and identified best practicesfor medical support to SOF we can foster best practiceswithin NATO SOF. The article discussed the developmentof NATO SOF medical doctrine and policy, andreviewed some barriers to change. Lastly, it set anagenda for change over this coming year to establishrelationships between the NSCC and NATO <strong>Special</strong><strong>Operations</strong> medical staff at strategic and operationallevels. Please contact the author to provide input intothe development of NATO SOF medical doctrine andpolicy. Your contributions are critical to this effort andare essential to corporate understanding, improved interoperabilityand to establish NATO SOF common“capability” or definitions.12Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
REFERENCES1. James L. Jones, “A blueprint for change: TransformingNATO <strong>Special</strong> <strong>Operations</strong>,” Joint Forces Quarterly; Issue45, 2nd quarter 2007, page 36.2. George W. Bush, remarks in Riga, Latvia, 28 November 2006.3. NSCC Handbook, 5 April 2009, page 7.4. Military Committee Decision 437/1, <strong>Special</strong> <strong>Operations</strong> Policy,11 Jun 2006.5. Allied Joint Publications 3.5, Allied Joint Doctrine for <strong>Special</strong><strong>Operations</strong>, 27 January 2009.6. AJP 3.5, page 2-1 through 2-4.7. Allied Joint Medical Support Doctrine, 2002, and MilitaryCommittee Decision 326/2, NATO Medical <strong>Operations</strong>, 2006.8. STANAG 2126, Ed 5, First Aid Kits and Emergency MedicalKits. STANAG 2122, Ed 2, Medical training in firstaide, basic hygiene, and emergency care.9. Allied Medical Publication (AMedP) – 17, Training Requirementsfor Health Care Personnel in International Missions,10 March 2009.10. Allied Administrative Publication-6, dated 2008.11. AMedP-17, Annex A2.12. Ibid, Annex B.13. AMedP-17, page v.14. ACO MEDAD Medical Directive, October 2008.15. John B. Holcombe, et all, “Understanding combat casualtycare statistics,” The Journal of Trauma Injury, Infection, andCritical Care; 60:2, 397-401.16. Recommendations based on findings of the Committee onTactical Combat Casualty Care, July 2008.17. John B. Holcombe, et al. (2007). Causes of death in U.S.<strong>Special</strong> <strong>Operations</strong> Forces in the Global War on Terrorism,Annuals of Surgery;245: 6, June.18. NATO Comprehensive Political Guidance, endorsed by NATOHeads of State and Government on 29 November 2006.19. AMedP-17, Annex A2.20. Ibid, Annex B.21. Ibid, Annex A2.22. John B. Holcombe, “Causes of Death in U.S. <strong>Special</strong> <strong>Operations</strong>Forces in the Global War on Terrorism,”23. USSOCOM Surgeons, CIPT for TSOST, 2009.24. Ibid.LTC Gary Rhett Wallace, MD, FAAFP, SFS, DMO is currently the Senior Medical Advisor andChief, NATO <strong>Special</strong> <strong>Operations</strong> Coordination Center Medical Branch. He is Board Certified asa Fellow of the American Academy of Family Physicians. He has had the honor of working inoperational billets and for U.S. Army <strong>Special</strong> <strong>Operations</strong> <strong>Command</strong> for 12 years, serving as aBattalion/Flight Surgeon, Group Surgeon, and at the USASOC/USASFC level before being assignedto NATO. He also has spent three years as a Flight Surgeon for the 1/17 (Air) Cav, andthree years as a Clinic <strong>Command</strong>er in Europe. He has had three combat tours to Afghanistanwhere he served once as a Battalion Surgeon and twice as CJSOTF-A Surgeon.LTC Wallace, can be reached at COM: +32 65 44 8262; DSN: 314 423-8262; or by emailat unclassified: Gary.wallace@nscc.bices.org; NATO Secret: wallagr@nsn.bices.org; U.S. SIPR:gary.rhett.wallace@eur.army.smil.milNATO SOF Transformation and the Development of NATO SOF Medical Doctrine and Policy13
Damage Control Resuscitation for the<strong>Special</strong> Forces Medic:Simplifying and Improving ProlongedTrauma Care: Part OneCOL Gregory Risk MD; Michael R. Hetzler 18DABSTRACTCurrent operational theaters have developed to where medical evacuation and surgical assets are accessiblein times comparable to the <strong>United</strong> <strong>States</strong>. While this has been an essential tool in achieving the best survivabilityon a battlefield in our history, the by-product of this experience is a recognized shortcoming in currentprotocols and capabilities of <strong>Special</strong> Forces medics for prolonged care. The purpose of this article is to providea theory of care, identify training and support requirements, and to capitalize on current successful resuscitationtheories in developing a more efficient and realistic capability under the worst conditions.Our forces enjoy high confidence in rapid casualtyevacuation and surgical intervention thanks tothe proximity and availability of those assets in today’sdeveloped theaters. While prehospital care hasevolved to an exceptionally high standard due to thesecapabilities, the ability of <strong>Special</strong> Forces (SF) medicsto conduct independent and prolonged care has sufferedbecause of them. Past experiences and futurepossibilities will require a return to prolonged, sustainedcare, as well as the development of new standardsfor all <strong>Special</strong> <strong>Operations</strong> Forces (SOF) medicsbased on the latest and proven theories. This capabilitycan have significant application in today’s missionsranging from Foreign Internal Defense in austere environments,a distant outstation isolated by weather, a<strong>Special</strong> Reconnaissance patrol inaccessible due to conditionsin a mountain range, or even in short-term directaction missions when cut off from friendly forcesand support. We can also take lessons from the recentIsraeli invasion of southern Lebanon in 2006 whenboth conventional and <strong>Special</strong> Forces medics wereforced into long term care. In this example of a modernlow intensity conflict, even casualty evacuationover short distances was limited due to battlefield dynamics,troop disposition, and terrain. 1Critical care and resuscitation between pointof injury and surgical intervention may be the missingelement here, and should include the capacity for extendedcare, delayed hand-off, and late surgical success.Prehospital care is relative to the situation. Formost, it is only the treatment given at the point of injuryimmediately prior to hand-off to an evacuation platform.In <strong>Special</strong> <strong>Operations</strong> those lines are neither soclear nor so rapid; the scope and duration of care providedby SF medics may equate to that of a physicianat more than one conventional level. Prehospital carefor operations in austere environments includes: pointof injury, evacuation concerns, resuscitation, prolongedcare, as well as all the skills required of those (Figure1). Sustaining a patient in an operational environmentfor days post-event is no easy task. And while maintenanceof a casualty for 72 hours post-op is requiredtraining at the <strong>Special</strong> Warfare Center, the focus here isthe implementation of current and proven strategies tomaximize the patient’s chances of survival.Figure 1: The stages of care differ remarkably not only dueto the assets involved, but by the scope of care requiredfrom SF medics and Independent Duty Corpsmen whencompared to conventional systems.14Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
This article is the first of two meant to providean approach to critical care using damage control resuscitation(DCR) as a guideline adapted for our use. DCRis a current and proven practice and provides aggressiveand effective trauma management with minimal supportwhile preparing the patient for the next level of care.DCR consists of two parts: first, keeping blood pressureat approximately 90mmHg, and second, to rapidly reversecoagulopathy and restore oxygen carrying capacitywith fresh frozen plasma (FFP) and packed red bloodcells (PRBC). 2 Since FFP and PRBCs are unavailablefar forward, we are advocating the earlier and more aggressiveuse of type-specific fresh whole blood (FWB) asthe only workable solution for salvaging patients withlife-threatening injuries. Fresh whole blood delivers normalphysiological ratios of essential elements, with moreactive clotting factors than banked component blood, andat normothermic temperatures. 3 Indications for FWB useis based on patient presentation and lab results such aslactate, base deficit, pH, and hematocrit which will alsolater serve as endpoints in resuscitation, ensuring efficienttherapeutic objectives. While “balanced” or “hypotensive”resuscitation works well in the short term, apatient left hypotensive and under-resuscitated for a prolongedperiod cannot be sustained. Trauma patients whodo not normalize their pH or base deficit have significantlyhigher mortality at 24 hours and near universalmortality at 48 hours. 4Patient care in the austere environment is incomparableto that in a U.S. hospital. With that in mind,the scope of practice, therapeutic guidelines, proceduresused, benefit vs. risk analysis, and clinical tenets, significantlydiffer from a civilian emergency room or eventhat of a combat surgical hospital (CSH). Many mayquestion the standards of care recommended, but theyprobably do not appreciate the challenges SF medicsface. Prolonged care in the primitive setting cannot supportcurrent hospital-based parameters, and a return tounconventional warfare practices is warranted and necessary.Strict clinical practices are respected and exercised,but not always attainable in our environment.Careful review of many long forgotten practices fromprevious conflicts may yield surprising results. The useof tourniquets, damage control surgery, and plasma andwhole blood transfusions, are all being resurrected withimproved patient outcomes in the 21st century. Many believethe most difficult challenges are found in the austereenvironment, and this may be where DCR is of mostbenefit.The following recommendations to SF medic’swere gathered from a number of physicians and institutionsthat have compiled an impressive bank of credibleand groundbreaking theories over the last seven years.Our effort here is to capitalize on those lifesaving protocols,merge the conventional levels of care with ouroverlapping SOF capabilities, and apply them in our rigorousenvironment.OVERVIEWThe Tactical Combat Casualty Care Committee(TCCC) has continually updated guidelines since 1996for prehospital care on the battlefield as defined in threelevels: Care Under Fire, Tactical Field Care, and TacticalEvacuation Care. These guidelines are based onmedic, corpsman, and physician input and experiencesthrough quarterly conferences. However, TCCC guidelinesonly provide the basis for care at the point of injurythrough evacuation. This article maintains those guidelines,but will leave initial management behind as SFmedics move on to 12 to 96 hours post event.Damage control surgery (DCS) is a well establishedand proven modality of medical intervention inboth civilian and military practice. 5 The U.S. Army Instituteof Surgical Research (ISR) has provided the mostup-to-date collection, evaluation, and development ofcritical care for war wounded, and additionally hasdriven implementation of this theory within all the services.Damage control focuses on principles that allowfor highly efficient care while compensating for inexperienceand limited resources as the “great equalizer” oftrauma surgery. 6 Using the damage control model for aship, the goal is to rapidly implement measures that preventfurther deterioration before irreversible injury occurs,or “the ship sinks.” Most initial treatments aretemporary to minimize patient exposure to stressful surgicalconditions and to reduce a physiological loss whichmaximizes the patient’s preparation for more extensivecare. Definitive surgical repair of injuries prior to adequateresuscitation may lead to a fully repaired but unsalvageablepatient. The primary and most immediategoal is surgical control of hemorrhage with judiciousfluid resuscitation, which is accomplished with a numberof advanced surgical procedures such as rapid closure,shunting, or packing. Stopping furthercontamination through exploration and additional therapeuticserves as a concurrent effort and significantlydecreases septic effects that can impact mortality overtime. The patient then moves to the intensive care unitto receive resuscitative care preparing him for return tothe operating room within 24 to 48 hours for definitivesurgical repair. Understanding this entire process isparamount to “act tactically, but think strategically” 7 inpreparing patients for a successful outcome. This treatmentstrategy must be understood to prepare the patientDamage Control Resuscitation for the <strong>Special</strong> Forces Medic:Simplifying and Improving Prolonged Trauma Care: Part One15
at this level; the SOF medics primary goal is to ensure thatthe patients arrive at surgical assets properly resuscitated.Figure 2: The lethal triad easily visualized, attributed toColonel John Holcomb.Damage control resuscitation guidelines arespecifically focused on the prevention of the “lethal triad”consisting of hypothermia, coagulapathy, and acidosis; allof which can be either mutually supporting or mutuallydestructive (see Figure 2). The factors of the lethal triadare all proven independent and codependent indicators ofmortality which also apply to DCS. Damage control resuscitationguidelines also include aggressive hypotensiveand hemostatic resuscitation while providing parametersfor addressing all three areas of the lethal triad. Ensuringthat these efforts are proactive and continuous from thepoint of injury provides the most efficient care possibleand uses a more scientific and therapeutic approach tocombat trauma for SOF medics. Again, the medics carecan and should potentiate success in supporting bothTCCC and DCS in the hospital.Figure 3: An OSS doctor conducts minor surgery in China circa 1944.(Courtesy USASOC Historian’s Office)IMPORTANCE OF HEMOSTASISThe single most essential weapon for DCR isimmediate and effective hemostasis, and it is at the pointof injury where resuscitation begins for the SOF medic.Hemorrhage control is the conservation of every singledrop of blood and with it every key ingredient that providessuccess against the lethal triad. The loss of bloodleads to hypoperfusion of tissues, relative hypoxia, andpromotes anaerobic metabolism. This subsequentlypromotes acidosis, hypothermia, and loses key coagulationfactors that are not easily reclaimed. Minimizingblood loss by immediate and effective treatments is afundamental trauma skill. Perfecting the basics willgain hemorrhage control in the least amount of time andwith minimal supplies while increasing survivabilitywith DCR.The physiologic picture resulting from hemorrhageeasily demonstrates the interacting and accumulatingfactors that will be important later. Blood lossnot only includes red blood cells essential for tissueoxygenation but also critical coagulation componentssuch as platelets, clotting factors, and enzymes. Currentlythese factors can only be replenished in the mostdifficult procedures for the SF medic, especially whentime, enemy situation, and supplies may all be at odds.A loss of blood volume reduces total oxygen carryingcapability, which is compensated by increases in bothinotropic (contractility) and chronotropic (heart rate) effortuntil the mismatch in oxygen delivery and demandresult in tissue hypoxia, or true shock. At this point, theaffected tissues convert from aerobic to anaerobic metabolism,which exacerbates all three components of thelethal triad. Cellular hypoxia results in a 90%reduction in energy production and an increasedrate of lactate production promotingmetabolic acidosis. This action leads to cellularswelling and edema, which further diminishescapillary flow and microcirculationirrespective of mean arterial pressure (MAP).Additional hypoperfusion due to vasoconstrictionoccurs naturally and simultaneously bylowered blood pressure, pain, and corticalrecognition of injury. A lack of blood supplyto the liver results in decreased glucose andclotting factors further complicating coagulapathies.Other physiological damage occurswhen pro-inflammatory mediators are releaseddue to hemorrhage and tissue damage, andshock affects neuroendocrine responses producingsevere metabolic changes. 8Direct pressure is always the first step forhemostasis. As soon as hemorrhage is noted, dig-16Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
Figure 4 : A <strong>Special</strong> Forces medic conducts an I & Dprocedure in Bolivia in 1967.(Courtesy USASOC Historian’s Office)ital or manual pressure is paramount and almost alwaysassures immediate effectiveness. Remember, the goalis not just to limit the amount of blood loss, but to saveevery single drop possible. Paramount towards this endis the expectation that each Soldier, if able, performsself-care. This requires mental preparation, musclememory, and psychological hardening to perform underphysical pain, stress, and challenging conditions. Pressurepoints are next, or act as an adjunct to minimizeblood loss and always attempt to use other Soldiers todeal with pressure points even under the best circumstances.The benefit is reduced time to hemostasis andpreserved blood volume, while maintaining combatpower during the fight. Other essential multipliers includethe medic placing pressure with his own kneewhile he works, or effective support from his teammatesfrom prior cross-training or on-scene instruction.Tourniquets are extremely effective in the treatment ofextremity wounds and their success since 9/11 is inarguable.There have been no reports of amputations duringthe conflict directly attributable to tourniquet usage.Remember that bleeding control is a graded response,so if a limb is mangled enough a tourniquet will likelybe the first step in hemorrhage control. 9 Tourniquet effectivenessis based on the principles of ensuring theyare placed proximal to the wound, active bleeding stops,the distal pulse is absent, and that reassessment is frequentand continuous. Keep in mind that the durationa tourniquet is applied will bring new concerns in prolongedcare. Present standards call for removal withintwo hours and, if conscious, the patient will remind themedic of this with the pain that normally accompaniesprolonged tourniquet use. Application over two hourscan also predispose the patient to increased morbiditysuch as fasciotomies and amputations, all of which maylater be the medic’s responsibility in this scenario. 10Converting a tourniquet to an effective pressure dressingas soon as possible while leaving the tourniquet looseand in place, for use if reapplication is necessary, willlikely prevent issues later in prolonged care.Packing wounds is a science in itself, requiringeffective technique, proper supplies, and completed witha pressure dressing to optimize the medic’s work. Makingthe decision to pack early is important too; packingis dependent on the patient’s ability to form good clotsand if too many factors are lost, then packing will notbe effective. Bowl-type wounds must be addressed immediatelyby packing with a maximum of two fingersusing unrolled Kerlix® and working from the bottom ofthe wound up, left to right or circumferentially, as if fillinga bucket. Finding and addressing all potential spacein the wound to ensure that there is no opportunity forany leakage of blood is a difficult task, especially whilepacking blindly, in the dark, and under stress at speed.An effective packing job can provide hemostasis with aminimum amount of supplies. Packing should not onlybe reserved for bowl-type wounds but also used inanatomical girdle areas such as the groin or shoulder.Hemostatic agents provide additional tools for more difficultwounds but they require thorough training, ideallyduring predeployment trauma training, to utilize effectively.The same rule applies for hemostatics as withpacking: hemostatics + packing + pressure = success.Future technologies that are presently being developedfor advanced hemostatics such as vessel closure andpressurized viscotic hemostatics may offer additional adjunctsin time.PREVENTION OF HYPOTHERMIAWithin the lethal triad itself, the prevention ofhypothermia is probably the simplest and most practicedeffort for SOF medics. Hypothermia has significant effectsand yields 100% mortality to severely traumatizedpatients with core temperatures less than 90ºF (32ºC). 11The goal is to maintain the casualty’s core temperature togreater than 95ºF (35ºC). Preventing hypothermia takesfar less effort and time than attempting to treat it undercombat conditions.Temperature monitoring should be as continuousas possible. Use every tool in sequence from skincolor and extremity warmth, patient feedback, and mentation.Objective findings can be obtained from toolsDamage Control Resuscitation for the <strong>Special</strong> Forces Medic:Simplifying and Improving Prolonged Trauma Care: Part One17
such as inexpensive temperature dots placed on the foreheador intermittent temperatures taken with an oto-thermometer,or use a digital rectal thermometer forcontinuous and high confidence readings. The fact thatmost wounded patients very often feel cold post-insultor the observance of spontaneous shivering, should alwayskey the medic in to the above steps. In short, simplytreat every single patient relentlessly forhypothermia.Hypothermia prevention should start immediatelypost-injury. Consideration of heat loss goes handin-handwith the initial assessment and optimally shouldoccur during the primary survey or just immediatelythereafter. Most of this work can be accomplished bycross-trained teammates automatically and simultaneouslyas the medic treats. Plan, prepare, and practicehypothermia prevention during all aspects of training;immediately insulating patient contact with the ground,minimizing exposure during the primary exam, removingonly wet clothing, and even keeping the patient cleanare all essential principles decreasing heat loss. Useevery opportunity to get the patient off the ground, driedif possible, covered, and out of the elements and beginall proactive efforts for economy of time.Both passive and active measures should beplanned for. Standard commercial hypothermia kitsshould include a durable and effective solar blanket anda chemical warming blanket, and these should be keptwith litter kits. Open the warming blankets first as theynormally take some time to reach its full exothermic reaction.The solar blankets are normally vacuum sealedso it should be stretched to full size to open any incorporatedair cells. Position it diagonally on the litter sothat the head and feet lie on the longest ends of the blanketand move the casualty to the blanket as quickly aspossible to get him off the ground and negate conduction.The patient should then be “burrito” wrapped withthe blanket as tightly as possible; it is the air closest tothe patient, or within the air cells of the blanket, that providesthe insulation for heat retention. Trapped air betweenthe patient and the blanket is warmed by the bodyand then retained and protected from loss or change bythe blanket. If standard hypothermia kits are not available,wool or space blankets wrapped in the same mannerand with some kind of head insulation (up to 60%heat loss here) such as a wool skull cap will providemuch of the same effects.Active warming measures require prior planningand usually cannot be achieved through improvisation.The chemical warming blanket opened firstshould be laid between the patient and the solar blanketto provide some degree of active heat on all patients. Beaware that there are differences in products and manufacturersso always rehearse this procedure. There aremany different types of commercial kits and each hasvarying temperatures, durations, and effectiveness.Warming all fluids before giving should be the goal nomatter what type, route, or environment. IV warmerssuch as the enFlow® warming system or the ThermalAngel® have proven effective, but both have specificsthat need to be appreciated in the tactical environment.A significant amount of heat can be lost through theadministration line. Using a closed-system kept next tothe patient with minor infusion pressure, or protectingthe administration line with insulation and minimizingits exposure to the elements, is important. Althoughthe lack of a fluid warmer does not preclude establishingIV/IO access or administering appropriate fluids,witholding warm fluids is of detriment to the patient.Primitive warming in an austere environmentcan be simple and is limited only by the medic’s imagination.Using vegetation to insulate patients from theground, finding civilian blankets from a house, simpleshielding or overhead cover from the elements, heatbottles and active heat sources, and proper nutritionwould all be beneficial. Primitive means to warmingfluids such as using MRE heaters packaged in plasticbags are effective as well, but must be rehearsed andlearned. Body bags, although not without possible psychologicaleffect, are extremely effective in heat retentionand protection and have been used in greatsuccess in Operation Enduring Freedom (OEF) andOperation Iraqi Freedom (OIF).Expedited evacuation has become the norm inOIF, but exists as a double edged sword. Timely evacuationmitigates the environmental effects of prolongedFigure 5: A Detachment 101 surgeon works on woundedin an austere environment during World War II.(Courtesy USASOC Historian’s Office)18Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
exposure. Conversely, the customary rapid rotary wingevacuation may contribute significantly to converting apatient from normothermic to profoundly hypothermic;remember not to negate the benefits of a speedy transportationwith an ill-protected patient. Timely air evacuationby itself is not the solution as a 2004 study fromOIF found that 91% of all casualties that arrived to theCSH by air were hypothermic as exposure and convectionfrom wind flow took its toll. 12 Optimization ofthese critically ill patients during transport is an importantstrategy to increase survival on the battlefield, replacinghope with capability. 13Hypothermia exacerbates coagulapathies primarilyby negating the full potential of the clottingprocess itself due to a loss of homeostasis. If the bodyfunctions optimally at 98.7°F then anything less decreasesits physiological response to a severe insult,thereby compounding the issues overall. Coagulationfunction in total is decreased by 10% with every degreepoint between 34°C and 32°C itself, and also independentlyaffects specific clotting factors at differentlevels. Mortality is also significantly increased; atrauma patient with a core temperature below 90°F(32°C) is associated with near 100% mortality. 14-16 Hypothermiaadditionally delays the onset of thrombingeneration, thrombin function, and additional cofactorsrequired in the clotting cascade. Concurrently, plateletadhesion, interaction, and aggregation are debilitatedoutside of normal temperatures and all of the enzymesrequired in the clotting cascade are also suppressed.MANAGING ACIDOSISThe prevention of acidosis is the final componentof the lethal triad which must be considered inmanaging patients for prolonged periods. Acidosis developsprimarily due to cells being forced into anaerobicpathways for energy, and the degree of acidosis inthe blood markedly underestimates the degree of intracellularacidosis. As cells die, they release an increasingamount of lactic acid into the system. As such,marked decreases in systemic pH may be a premorbidevent, and mark irreversible uncompensated shock.Even more challenging is the fact that if perfusion is restoredto previously hypoxic cells, accumulated acidswill be released into the systemic circulation leading toa reperfusion syndrome. Therefore, combat casualtieswith any degree of hemorrhage should be considered atrisk for developing acidosis, especially when the shorttermcare and rapid evacuation become a long-term resuscitationchallenge due to a changing battlefield. Theability to maintain adequate breathing and ventilation,achieving the appropriate goals for endpoints, and againrapid evacuation, mutually supports all other efforts.Small changes in pH have more profound effectson coagulation than even small changes in coretemperature. The coagulation proteases necessary forthe activation of both the intrinsic and extrinsic pathwaysare optimized to function in the alkaline range. Adecrease in pH from 7.4 to 7.0 reduces the activity ofthe enzyme complex that activates thrombin by 70%. 17The previous point leads to the possibility that activecorrection of pH and administration of thrombin may beareas of future research in hemorrhagic trauma.Hypothermia and acidosis provides a clear exampleof how the three factors in the lethal triad are interrelated:Acute hemorrhage leads to hypotension withdecreased systolic blood pressures, which in turn leadsto reduced oxygen perfusion to tissue. Decreased O2delivery results in a change in energy consumption fromaerobic to anaerobic metabolism, which then produceslactic acid as a byproduct, which contributes to overallacidosis. Anaerobic metabolism itself is inefficient anddecreases normal energy production and heat generationwhich then negates the body’s ability to recover fromtemperature loss. The resulting acidosis interferes withthe clotting cascade, and leads to further hemorrhageduring resuscitation, leading to death if not prevented oraggressively interrupted.CORRECTING COAGULAPATHIESAddressing presenting coagulapathies is the primaryfocus of DCR seconding acidosis and hypothermiain priority. As mentioned before, minimizing bloodloss from the very onset with hemorrhage control keepsRBCs and clotting factors onboard, and assists in maintaininga natural acid base balance for as long as possible.Hemostatic dressings and vascular access provideadditional lifesaving capabilities with increasingly effectiveproducts on the market, and advanced techniquesdeveloped to address non-compressible hemorrhages.The early use of recombinant Factor rVIIa in severeblood loss and coagulapathy can be another choice as atreatment adjunct. Rapid evacuation to the next level ofcare again provides access to surgical interventions andblood banking to interrupt the progress of the shock. Ifrapid transport is unavailable, we must consider otherapproaches to maintaining the casualty, and interventionsof a more creative nature.Additionally, it appears that a subset of traumapatients present coagulapathic, not secondarily as a resultof blood loss, acidosis, and hypothermia, but as aprimary response to the traumatic insult. 18 This groupDamage Control Resuscitation for the <strong>Special</strong> Forces Medic:Simplifying and Improving Prolonged Trauma Care: Part One19
of patients become coagulopathic much earlier for reasonsthat are at present not well delineated. That fact,coupled with the hemorrhage due to penetrating traumamay lead to a disproportionate loss of clotting factors,inactivation of normal coagulation due to acidosis andhypothermia, and inactivity of factors due to storage inbanked blood and blood components. Consequently,in non-compressible hemorrhage on the battlefield, inan otherwise young and healthy population, there maybe a role for early augmentation of the coagulation cascade.As previously noted, the proteolytic enzymes ofthe coagulation cascade function poorly at pH below7.2. Acidosis slows the rate of thrombin generation,while hypothermia delays the onset of thrombin generation.Biologically plausible arguments can be madefor optimizing and augmenting the coagulation pathwaysand processes before significant hemorrhage occursand shock develops as will be discussed.While we have for the most part solved thechallenge of extremity injury with the use of tourniquets,pressure, and wound packing, the developmentsof new types of hemostatic agents in the form of a pad,packing sponge, or gel have provided adjuncts forcompressible and accessible wounds. The current challengein the field for the medic is the non-compressibleand non-accessible wounds, primarily in theabdomen and pelvis in the absence of immediate surgicalassets. Because of this, the use of non-surgicalsolutions needs to be aggressively considered. Thiswould include the use of Factor VIIa, along with adjunctssuch as calcium and sodium bicarbonate to optimizethe biological activity of this potentiallylifesaving modality. Factor VIIa works by activatingthrough thrombin and various feedback loops both theintrinsic and extrinsic coagulation pathways. The desiredendpoint is assistance in the formation of a thrombusat the site of injury in an otherwise inaccessiblelocation such as solid organs (liver, spleen, and kidney),large vessels, and pelvic structures. This mightbe thought of as mobilizing a damage control party tothe site of injury in our ship analogy. Because of thetime involved, this must be considered for administrationrelatively early if severe hemorrhage is suspected.Delays awaiting conclusive evidence of Class III/IVshock may prove insurmountable. Interestingly, thereis some evidence that thrombus created with rVIIa administrationmay be more resistant to lysis and breakdownwith reperfusion.Correcting coagulapathies will also be assistedby administering the proper blood products, and althoughFWB and FFP are specifically advocated in thisarticle due to their natural contributions, they will beaddressed in Part Two, complete with all other fluidchoices. In addition to resuscitation, prolonged carerequires an exceptional skill set. Tracheotomies, fasciotomies,blood transfusions, anesthesia, and primaryand delayed closure, all play an important role here.These are advanced skills and as such require propersustainment. Nursing skills also have a huge importancein critical care and without them none of theabove would be successful. Competence in aseptictechnique, antibiotic therapy, labs for the monitoringof endpoints, input and output, and basic nursing careincluding patient hygiene need to be appreciated.Other concerns requiring attention are pre and post surgicalskills, wound care, nutrition, rehabilitation, andeven logistical needs. This skill set is now rarely exercised,except in the schoolhouse during records andreports, but is essential in the austere scenario.The authors hope that Part One provides afoundation in general knowledge of DCR for the SFmedic; Part Two will identify options for measuringshock and recommend relative endpoints to serve asgoals in resuscitation. Additionally we will proposenot only the special equipment required, but the minimalequipment needed in care, and identify the criticalcare and nursing skills required to support DCR in ourenvironment.REFERENCES1. BG Yeheskel Levy. (2007). Lecture. Advanced TechnologyApplications for Combat Casualty Care Conference.2. Holcomb J. (2007). Damage control surgery. Journal ofTrauma; 62:S36-S37.3. Blackbourne L, McMullin N, Eastridge B, Baskin T, HolcombJ. (2007). Aggressive proactive combat damagecontrol surgery. AMEDD Journal; January-March.4. Kaplan L, Bailey H. (2007). Ongoing resuscitation endpointsand strategies; Trauma;Emergency Resuscitation Vol1. Inpharma Healthcare.5. Blackbourne L. (2008). Combat damage control surgery.Critical Care Medicine; 36,7:S304-S310.6. Hirshberg A, Mattox K (2006). Top Knife, The 3-D TraumaSurgeon, tfm Publishing Ltd, p. 5-17.20Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
7. Ted Westmoreland. (2006). Attributed quote.8. Anjaria D, Mohr A, Deitch D. (2008). Haemorrhagic shocktherapy. Informa Healthcare.9. Hirshberg A, Mattox K (2006). Top Knife. Stop That Bleeding,tfm Publishing Ltd, p. 19-34.10. Kragh J, Walters T, Baer D, et al. (2008). Practical use ofemergency tourniquets to stop bleeding in major limb trauma.Journal of Trauma;64:S38-S50.11. Beekley A. (2008). Damage control resuscitation: A sensibleapproach to the exsanguinating surgical patient. CriticalCare Medicine;36:S267-S274.12. Arthurs Z, Cuadrado D, Beekley A, et al. (2006). The impactof hypothermia on trauma care at the 31st combat supporthospital. The American Journal of Surgery; 191:610-614.13. Blackbourne L, Gratwohl K, et al. (2007). Optimizing transportof postoperative damage control patients in the combatzone. AMEDD Journal; January-March.14 Krishna G, Sleigh J, Rahman H. (1998). Physiological predictorsof death in exsanguinating trauma patients undergoingconventional trauma surgery. Aust NZ Surg; 68:826-829.15. Jurkovich G, Greiser W, et al. (1987). Hypothermia intrauma victims: An ominous predictor of survival. Journal ofTrauma; 1019-24.16. Pend R, Bongard F. (1999). Hypothermia in trauma patients.J Am Coll Surg; 188:685-96.17. Hoffman M. (2004). The cellular basis of traumatic bleeding.Mil Med; 169,12:000.18. MacCleod J. (2008). Trauma and coagulapathy: A new paradigmto consider. Arch of Surgery; 143(8):797-801.COL Gregory Risk is an Emergency Physician/Flight Surgeon currently assigned to USASOC. He completed SFQC asan 18D in 1982 and was assigned to 7th SFG. He graduated from the Indiana University School of Medicine in 1993 andcompleted emergency medicine residency at Methodist Hospital in 1996. COL Risk was previously assigned as AsstDean, Joint <strong>Special</strong> <strong>Operations</strong> Medical Training Center.Michael Hetzler has served as a <strong>Special</strong> Forces Medic for over 15 years in both 1st <strong>Special</strong> Forces Group and USASOC.Damage Control Resuscitation for the <strong>Special</strong> Forces Medic:Simplifying and Improving Prolonged Trauma Care: Part One21
A Review of the Use of EarlyHypothermia in the Treatment ofTraumatic Brain InjuriesJess Arcure BS, MSc; Eric E Harrison MDABSTRACTTraumatic brain injury (TBI) is an assault to the brain that disrupts neurological activity. Known as thesignature wound of combat during <strong>Operations</strong> Iraqi Freedom (OIF) and Enduing Freedom (OEF), it has becomeone of the most common injuries to American Soldiers. While affected Soldiers may remain stable after the primaryinjury, progressing secondary mechanisms can produce neurological degeneration. Hypothermic medicineis the treatment of injuries by cooling the core body temperature below normal physiological levels. Such treatmentmay be indicated to improve neurological outcomes after traumatic brain injuries by reducing the evolvingsecondary deterioration.To date, clinical trials have reached mixed conclusions. Trials have used unique temperature goals fortreatment, different methods and times to reach such goals, and different durations at therapeutic temperature.Such variances in procedure and experimental populations have made it difficult to assess significance.In the article written by Markgraf et al. in 2001, research in animals showed the effect of hypothermictreatment within rats. Their results suggest that early initiation of hypothermic medicine after an induced traumaticbrain injury (TBI) improved neurological outcomes when the body was cooled to 30°Celsius (C) withinfour hours. An ongoing study by Clifton et al., on adults diagnosed with TBI, is examining the neurological outcomeof early hypothermic medicine by centrally cooling the body to 33°C and maintaining that temperature for48 hours.While previous hypothermic devices were unable to cool rapidly, new technology allows achievementof the goal temperature within 20 minutes. Implementation of such new treatment may show an improvementin neurological outcomes for patients when treatment target temperature is reached within a four-hour window.We recommend that the use of hypothermic medicine should be re-evaluated for its indication in TBI due to thecapabilities of a new extremely rapid cooling device.INTRODUCTIONTraumatic brain injury (TBI) is an insult to thebrain that disrupts neurological activity and has becomeone of the most common injuries to AmericanSoldiers subjected to explosions from improvised explosivedevices (IEDs), vehicle borne IEDs (VBIEDs),and suicide bombers. One report indicated that by January2008, over 5,500 Soldiers had suffered such injuryduring the Iraq and Afghanistan conflicts. 1 In2008, about 33% of Soldiers requiring medical evaluationfor battle-related injuries who were transportedfrom areas of armed conflict to Walter Reed ArmyMedical Center (WRAMC) had TBI. 2,3Traumatic brain injury occurs most commonlydue to proximity to blast explosions as expanding airpressures apply extreme forces to the head, but it canoccur with other types of head trauma, such as penetratingwounds, violent physical blows, and from impactwith any propelled solid object including shrapnelfrom explosions or explosively formed penetrators(EFPs). A TBI can also result from rapid accelerationsdecelerationsof the head due to blast waves even in theabsence of an impact from a solid object. 3,4,5Mild TBI includes any trauma to the head thatmay result in loss of consciousness or alterations inmental status. However, the definition of mild TBI isdifficult to establish and may only present as headache,dizziness, lack of concentration, or memory loss. SevereTBI is an insult that leaves patients in a persistentcoma following medical and surgical therapy. 6Multiple factors can initially result in damageat the time of the assault: Nerve fibers can shear inwhich neurons are stretched and torn, the brain tissuecan bruise, and vessels can be compromised producingischemia or forming destructive pressures.In addition to the initial disruptions, secondaryinjuries from multiple elements can lead to new or furtherneurological deterioration. Increased intracranialpressures (ICPs) are typically at the highest within the22Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
first three days of injury, although one-quarter of TBIpatients reached maximal ICPs after day five. 7 Otherdelayed injuries can be due to factors released duringinjury that in time induce inflammation, production offree radicals, release of the excitatory neurotransmitterglutamate, electrolyte disturbances of the neuron, andmitochondrial dysfunction. 6 Even though affected Soldierscan be stable and functional after the TBI, thesesecondary factors can lead to severe neurological deteriorationwithin three to five days post-injury. In standardhealthcare, the concentration of care for TBIpatients goes into reducing these secondary effects. Itwould be optimal to prevent secondary injuries in orderto prevent secondary neurological damageHypothermic medicine, which is the treatmentof injuries by cooling the core body temperature belownormal physiological levels, was studied in use of braininjuries for over 50 years. Mild hypothermia has beenstudied extensively in animal models and is defined inhumans as the achievement of core body temperaturesof 33-34°C. Such treatment may be indicated to improveneurological outcomes after TBI by reducing theevolving secondary injuries through multiple means.One of these was the decrease of cerebral edema andbrain swelling. 8 In an animal-model experiment byMarkgraf in 2001, early administration of hypothermictreatment within four hours was shown to reduce maximalICPs at 24 and 48 hours after TBI. 9Mild hypothermia may also inhibit the buildupof the neurotransmitter glutamate 10,11 and reduce the8, 12metabolic rate of neurons.Hypothermic medicine may attenuate neuronaldeath by turning off several chemical pathways of cellularapoptosis. 13,14 Such treatment may also inhibit theinflammatory response by preserving the blood brainbarrier 15 or reducing pro-inflammatory cytokines. 16After trauma the reperfusion of brain tissueforms free oxygen radicals that damage the cellularmembrane of neurons leading to cell death. Hypothermictreatment increases the function of superoxide dismutase,an enzyme that limits the damage of freeoxygen radicals and protects the cellular membrane.Ultimately, hypothermic medicine may assistin the reduction of secondary insults to neurological tissue,perhaps not through all means discovered in thelaboratory, but probably through more than one factordescribed.ADVERSE EFFECTSTreatment with hypothermic medicine carriesthe adverse risks of cardiac arrhythmia and thrombocytopenia.However, arrhythmia risk is typically only increasedduring moderate hypothermia, when the body iscooled below 30°C. Since most controlled treatmentsremain above these temperatures, it is rare to find arrhythmiasin hypothermic studies. 17Even though it is a common notion that lowerbody temperatures increase hemorrhage due to impairedfunction of platelets and coagulation proteins, 18 surgicalpatients undergoing controlled hypothermia at levels between32.5 and 33.5°C for cerebral aneurysm clippingshowed no greater significant blood loss. 19EQUIPMENTVarious methods exist with which to administermild hypothermia; however, to date only surface coolingand intranasal cooling systems have been tested in humansfollowing TBI. 17The simplest method of inducing mild hypothermiafor treatment is surface cooling. In the past,techniques included applied ice packs and submergingthe patient in ice baths to drop core body temperature.The water-circulating surface cooling device consists ofblankets placed directly on the patient with regulatedcold water circulating through the blankets. The degreeof cooling treatment water is determined by feedbackfrom a rectal thermometer. Gel-coated surface coolingdevices also exist that work on the same principles asthe water-circulating blankets. Only here instead ofblankets, transfer pads coated with adhesive gel are attachedto the body along the back, abdomen, and bilateralthighs. More recently, helmets and caps have beendesigned to produce cooling in a more localized area.Invasive methods such as intravenous coolingconsist of a central venous catheter placed within the inferiorvena cava. Cooled saline is pushed through thecatheter balloons, which are in adjacent contact with thepatient’s blood. In this procedure the core body temperatureis gauged by rectal means. This measured temperatureinduces a feedback loop that regulates thetemperature of the therapeutic saline entering the body.This allows control over therapeutic measures. Anotherinvasive method includes rapid infusion of lactatedRinger’s at 4°C combined with surface cooling using icepacks. However, both these invasive methods compromisevasculature access and increase risk of infectionand hemorrhage.In a study by Hoedemaekers et al., it was shownthat surface methods of water-circulating blankets andgel pads along with cooled at a rate of 1.33°C/hr, and1.04°C/hr, respectively. Intravenous cooling with centralcatheter placement cooled at 1.46°C/hr. These threemethods were far more effective than the conventionaltreatment of running cold lactated ringers solution(0.32°C/hr) and air-circulating cooling systems(0.18°C/hr). 20A new ice water immersion system propels andcirculates a thin film of ice-cooled water directly aroundthe patient’s body in a special molded enclosed environmentto reduce core body temperatures at a rate of4.7°C to 6.6°C/hr. Patients may reach target hypothermicconditions within 20 minutes, at which time the de-A Review of the Use of Early Hypothermia in the Treatment of Traumatic Brain Injuries23
vice can be removed and the core body temperature willremain at a constant lowered value for hours. 21 Thisportable cooling system is presently the fastest coolingavailable and is comparable to controlled ice water immersion.(see Figure 1)TRIALSFigure 1: ICE ImmersionTo date, clinical results have been conflicting;many reports have been unable to reach proper efficacy inhuman trials due to a lack of comparable data betweencontrol and treatment groups. In association with this,different trials have used unique temperature goals fortreatment, different methods and times to reach suchgoals, and different durations at therapeutic temperature. 22In 2001 a clinical trial by Clifton et al. presentedno significant neurological outcome difference in severebrain injury patients who were treated with mild hypothermiacompared to a normothermic control group. Inthis study the experimental group reached the therapeutictemperature goal of 33°C in the mean time of 8.4 ± 3.0hours. 23 Results of Markgraf et al. (2001) study suggeststhat early initiation of hypothermic medicine within onehour of an induced traumatic brain injury with rats, improvedneurological outcomes when the body was cooledto 30°C. The therapeutic device utilized in this studyachieved hypothermic target temperatures within threehours. Overall this meant that target core body temperatureswere reached in less than four hours. When initiationoccurred after 90 minutes, there was no observedchange in neurological outcome. 9An ongoing study by Clifton et al. is examiningthe impact on neurological outcome of using hypothermicmedicine to centrally cool the body to 33°C withinfour hours of traumatic brain injury and then maintainingthat temperature for 48 hours. 24CONCLUSIONTBI is considered by many to be the “signaturewound” of the present conflicts in Iraq and Afghanistan,thus, further understanding of the mechanisms of injuryand the treatment for such is imperative to militarymedical personnel.While Soldiers may remain stable after the primaryinjury, progressing secondary mechanisms canproduce neurological degeneration. Results of preliminarystudies with hypothermic medicine suggest thatthis treatment may reduce some of the secondary mechanismsof TBI and also be an effective treatmentthrough other means.To date the clinical trials of therapeutic hypothermiahave given mixed results. Results in animalstudies of Markgraf et al. (2001) indicate that early inductionof mild hypothermia could produce neuroprotectiveabilities, when target core body temperatures arereached within four hours after an induced neurologicalassault. If continued, a National Institute of Health clinicaltrial by Clifton et al. may be modified to achievetherapeutic temperatures of 33°C with the new fastestcooling portable system clinically available. While previouslyimpossible to obtain such timely new treatment,advances in technology give new opportunities to answerthe questions we have posed concerning preventionof secondary injury, and if the data is supportive ofthis concept, an opportunity to implement a field-readysystem that has the potential for forward deployment.REFERENCES1. Landers, Susan J. (2009). Traumatic brain injury has becomethe signature wound of the wars in Iraq andAfghanistan, yet its effects are often overlooked. AmericanMedical News. Posted on Jan. 5, 2009.2. Betty Clooney Foundation Website. (2009). Retrievedfrom http://www.bcftbi.org/aboutSoldiers.asp, on May 3,2009.3. Army News Service. (2009). Most Soldiers with traumaticbrain injury heal. March 4, 2009.4. Soldiers story of traumatic brain injury. (2005). Retrievedfrom http://www.wsoctv.com/health/5392779/detail.html.5. Hardman JM, Manoukian A. (2002) Pathology of headtrauma. Neuroimaging Clinics of North America; 12(2):175–87.6. Park E, Bell J, Baker A. (2008) Traumatic brain injury:Can the consequences be stopped? Canadian Medical AssociationJournal; 178 (9).7. Stocchetti N, Colombo A, Ortolano F, et al. (2007). Timecourse of intracranial hypertension after traumatic braininjury. Journal of Neurotrauma; 24:1339-1346.8. Jiang JY, Lyeth BG, Kapasi MZ, Jenkins LW, PovlishockJT. (1993) Moderate hypothermia reduces blood-brainbarrier disruption following traumatic brain injury in therat. Acta Neurophalol; 84:495-500.24Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
9. Markgraf CG, Clifton GL, Moody MR. (2001). Treatmentwindow for hypothermia in brain injury. Journal ofNeurosurgery; 95(6):979-83.10. Busto R, Globus MYT, Dietrich WD, Martinez E, ValdesI, Ginsberg MD. (1989). Effect of mild hypothermia onischemic-induced release of neurotransmitters and freefatty acids in rat brain. Stroke; 20:904-10.11. Globus MY, Alonso O, Dietrich WD, et al. (1995). Glutamaterelease and free radical production followingbrain injury: Effects of posttraumatic hypothermia. Journalof Neurochemistry; 65:1704-1711.12. Kochanek PM. (2005). Brain trauma: Laboratory studies.Therapeutic Hypothermia. Tisherman SA and SterzF (eds.) Springer Science and Business Media, Inc., pp63-86.13. Xu RX, Nakamura T, Nagao S, et al. (1998). Specific inhibitionof apoptosis after cold-induced brain injury bymoderate postinjury hypothermia. Neurogsurgery;43:107-114.14. Ji X, Luo Y, Ling F, Stetler RA, et al. (2002). Mild hypothermiadiminishes oxidative DNA damage and prodeathsignaling events after cerebral ischemia: Amechanish for neuroprotection. Front Bioscience;12:1737-1747.15. Smith SL, Hall ED. (1996). Mild pre and post traumatichypothermia attenuates blood-brain barrier damage followingcontolled cortical impact injury in rats. Journalof Neurotrauma; 13:1-9.16. Wang GJ, Deng HY, Maier CM, Sun GH, Yenari MA.(2002). Mild hypothermia reduces ICAM-1 expression,neutrophil infiltration and microglia/monocytic accumulationfollowing experimental stroke. Neuroscience;114:1081-1090.17. Christian E, Zada G, Sung G, Giannotta S. (2008). A reviewof selective hypothermia in the management of traumaticbrain injury. Neurosurg Focus; 25:1-8.18. Rajagopalan S, Mascha E, Na J, Sessler DI. (2008). The effectsof mild perioperative hypothermia on blood loss andtransfusion requirement. Anesthesiology; 109(2):353.19. Todd MM, Hindman BJ, clarke WR, Torner JC. (2005).Mild intraoperative hypothermia during surgery for intracranialaneurysm. New Englad Journal of Medicine;352:135-145.20. Hoedemaekers C, Ezzahti M, Gerritsen A, van der HoevenJ. (2007). Comparison of cooling methods to induce andmaintain normo-and hypothermia in intensive care unit patients:A prospective intervention study. CriticalCare;11:R91.21. Ohley WJ, Schock RB, Howes D, Holzer M, Dorian P,Freedman R. (2008). Rapid Surface Cooling in UnconsciousPost Resuscitation Patients Following Cardiac Arrest:Safter, Efficacy, and Outcomes. Resuscitation ScienceSymposium, American Heart Association Scientific Sessions.22. Marion DW, Penrod L, Kelsey S, Obrist W, Kochanek P,Palmer A, Wisniewski S, DeKosky S.(1997). Treatment ofTraumatic Brain Injury With Moderate Hypothermia. TheNew England Journal of Medicine; 336:540-5.23. Clifton G, Miller E, Choi S, Levin H, McCauley S, SmithK, Muizelaar JP, Wagner F, Marion D, Luerssen T, ChesnutR, Schwartz M. (2001). Lack of effect of induction of hypothermiaafter acute brain injury. New England Journal ofMedicine; 344(8):556-563.24. Clifton G, Drever P, Valadka A, Zygun D, Okonkwo D.(2009). Multicenter trial of early hypothermia in severebrain injury. Journal of Neurotrauma; 26(3): 393-397.Jess Arcure is originally from Farmington, West Virginia. He is currently a fourth-year medicalstudent, graduating in May 2010, with a Doctor of Medicine degree from Saba University Schoolof Medicine. He received his Bachelor of Science degree in Chemical Engineering from West VirginiaUniversity in 2005. He received his Masters of Science degree in Hyperbaric Medicine also fromSaba University in 2008.Jess currently lives and works in Tampa, Florida and plans on specializing in physical medicineand rehabilitation.Dr. Eric Harrison attended Vanderbilt University and received his Bachelor of Science Degree from RollinsCollege. He received his medical degree from the University of Kentucky and completed internship, Internal Medicineresidency, and Cardiology Fellowship at the University of South Florida.He was a founder of the Tampa Fire Rescue Paramedic Program and Hillsborough County EMS Program. Heis the National Director of Advanced Cardiac Imaging for IASIS Healthcare, Inc. and Director of the Joint Memorial Hospitaland University of South Florida Advanced Cardiac Imaging Program.Dr. Harrison was one of the first to use therapeutic hypothermia for Cardiac Arrest patients in the <strong>United</strong> <strong>States</strong>,starting in 2002. Dr. Harrison now teaches the Advanced Hypothermic Life Support (AHLS) Course for credentialingby Cardiac Care Critique.He is starting the American Society for Hypothermic Medicine.A Review of the Use of Early Hypothermia in the Treatment of Traumatic Brain Injuries25
Emergency Lateral Canthotomy andCantholysis: A Simple Procedure toPreserve Vision from Sight ThreateningOrbital HemorrhageCPT Steven Roy Ballard, MD; COL Robert W. Enzenauer, MD,MPH; Col (Ret) Thomas O’Donnell, MD; James C. Fleming, MD;COL Gregory Risk, MD, MPH, FACEP; Aaron N. Waite, MDABSTRACTRetrobulbar hemorrhage is an uncommon, but potentially devastating complication associated with facialtrauma. It can rapidly fill the orbit and cause an “orbital compartment syndrome” that subsequently cuts offperfusion to vital ocular structures, leading to permanent visual loss. Treatment must be initiated within a limitedtime in order to prevent these effects; however, specialty consultation is not always available in remote fieldenvironments. This article addresses the mechanism, diagnosis, and treatment of retrobulbar hemorrhage via lateralcanthotomy and cantholysis, and recommends that 18D medical sergeants be properly trained to evaluateand perform this sight-saving procedure in emergent settings where upper echelons of care are not immediatelyavailable.INTRODUCTIONRetrobulbar hemorrhage is a vision-threateningemergency often necessitating immediate lateralcanthotomy for preservation of vision. 1 Prompt recognitionand appropriate treatment of this ocular emergencyis imperative, for timely managementdetermines the ultimate outcome. 2 The medical literaturedescribes multiple causes for true spontaneousorbital hemorrhage; however, head and facial trauma,as well as post-surgical complications, constitute themajority of emergent cases. 3-14 Reports of injuries inOperation Iraqi Freedom document the risk of orbitalhemorrhage and subsequent orbital compartment syndrome(OCS) from penetrating trauma and the potentialvision-threatening consequences. 15Retrospective studies show an incidence of coexistingretrobulbar hemorrhage in patients with orbitalfractures of only 0.45-0.6%. 16 However, inpatients experiencing acute vision loss in the setting oftraumatic retrobulbar hemorrhage, the potential forpermanent blindness is high (44-52%). 17,18 Althoughrare, the potential ophthalmic concern in a war-timeenvironment becomes increasingly real, due to thehigher incidence of facial trauma and delayed presentationto upper echelons where definitive ophthalmiccare can be undertaken.We agree with earlier assessments that theskills to recognize and treat vision-threatening orbitalcompartment syndrome (OCS) due to retrobulbar hemorrhageshould be within the scope of a <strong>Special</strong> <strong>Operations</strong>Forces (SOF) medic and concur with therecommendation of Burns and DeLellis that the proceduresof lateral canthotomy and cantholysis could andshould be introduced into the SOF medical training curriculum.19MECHANISMRetrobulbar hemorrhage causes a mass effectwithin the confined space of the orbit, and as it expandsit impinges on sensitive ocular tissues reducing perfusionof the optic nerve. 20 The compartment is restrictedin its ability to expand due to the bony walls. Anteriorexpansion does occur, causing subsequent proptosis,but it is ultimately limited by the orbital septum and thefact that the globe is tethered to the optic nerve. 16,21-24An OCS ultimately develops, increasing orbital pressure,damaging the optic nerve by direct compression,and causing ocular ischemia via decreased perfusionfrom compromised vascular flow, not unlike that seenin other compartment syndromes. 25 If the patient is unconsciousor uncooperative and has periorbital trauma,26Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
the only sign of OCS may be elevated intraocular pressure(IOP). 26 Without proper perfusion, sensitive structuressuch as the optic nerve and retina have a limitedtime for survival and recovery. Review of the literaturesuggests that the window for visual recovery from theonset of decreased visual acuity to decompression is perhapslimited to approximately 120 minutes. 10,27 Two casereports document a four hour delay with improvement invision to baseline, but these appear to be rare exceptions.28 Hayreh’s studies on Rhesus monkeys demonstratedcentral retinal artery occlusion of 105 minutes orlonger produced irreversible optic nerve damage, andtotal optic nerve atrophy occurred with occlusion timesthat were greater than 240 minutes. 16,29 It is therefore ofthe utmost importance to recognize and treat retrobulbarhemorrhage with prompt decompression early in this 120minute window if the devastating effects on vision are tobe reversed.Referral for immediate specialist assessment, ifavailable, should not be delayed even in doubtful cases. 24Similarly, primary examiners should not waste preciousminutes with unnecessary investigations that delay treatmentin the event specialist care is not present. 24,28,30 Ideallyan ophthalmologist would be expected to performthis emergency orbital decompression. However, if anemergency ophthalmology consult is unavailable, anyemergency responder trained to do the procedure shouldact immediately. 26 According to U.S. Navy family physicianDr. Mark Benton, “Knowledge of this procedure isa must for physicians, especially those in remote areaswhere access to ophthalmology is not readily available.The emergent lateral canthotomy can be a potentiallysight-saving procedure.” 31 In the setting of the militaryfield environment, this time window can easily lapseprior to presentation to a trained ophthalmologist. <strong>Special</strong>Forces units are at particular risk due to separationfrom upper levels of care. In these settings, promptrecognition and treatment by 18D medical sergeants maybe required for vision saving care to be provided.DIAGNOSISIn order to undertake proper treatment, it is imperativeto recognize the signs and symptoms of acuteretrobulbar hemorrhage in the setting of trauma. OCSshould always be considered whenever there is impairmentof vision following blunt facial trauma. 32 As thepressure increases, patients may experience double vision,nausea, and vomiting. Signs of retrobulbar hemorrhageinclude a progressively tense and painful proptosis,decreasing ocular motility, asymmetric visual acuity,field restriction on confrontation testing, and decreasedpupil responsiveness – including failure to constrict todirect light stimulation or even loss of the consensual responsein comparison with the other eye. The eyelidscan become tense and edematous, and periorbital or subconjunctivalhemorrhage/ecchymosis are frequentlypresent (Figure 1). 24,33 These signs and symptoms areprogressive over minutes and changes should raise suspicionof retrobulbar pathology. 16,34,35Figure 1: OCS secondary to acute retrobulbarhemorrhage of the left eye sustained fromorbital trauma.In the setting of blunt or penetrating trauma,retrobulbar hemorrhage and OCS may be accompaniedby open globe injuries. When evaluating these patients,it is imperative that first responders maintain a high suspicionfor globe perforation first. Care should be exercisedduring examination of the ocular and periorbitalstructures to avoid undue pressure on the affected eye.Manipulation of the lids should be minimal to limit therisk of extrusion of intraocular contents in the eventglobe trauma is present. If suspicion remains based onclinical history, or signs of obvious foreign body, irregularglobe shape, peaked pupil, visible corneal or conjunctivallacerations, flat anterior chamber, or hyphema,the eye should be protected with a shield and interventionshould be left for upper echelons of care. Nevertheless,even in ideal settings, retrobulbar hemorrhage isa clinical diagnosis. Treatment cannot wait for imagingto confirm the presence of hemorrhage within the orbitor for on-call ophthalmologic personnel to arrive. Delaysfor such studies are at the expense of continued ocularischemia. Definitive care must be undertakenimmediately, once the diagnosis of orbital compartmentsyndrome from retrobulbar hemorrhage is made and thepotential of rupture or penetrating injury has been carefullyascertained and ruled out sufficiently to proceed.MEDICAL/SURGICAL INTERVENTIONMild cases of retrobulbar hematoma have beenmanaged with simple observation and medical treatment.36-38 Acute OCS requires surgical intervention toprevent vision loss. 39 However, there is often reluctanceto interfere surgically in cases of orbital hemorrhage.According to Markovits, when imperative, variousmethods including aspiration, continuous suction, andopen orbitotomy by brow and lateral approach can beEmergency Lateral Canthotomy and Cantholysis: A Simple Procedure to Preserve Vision fromSight Threatening Orbital Hemorrhage27
used. 40-42The goal of treatment for retrobulbar hemorrhageis orbital decompression to release the pressure onsensitive orbital contents — such as the optic nerve andvessels. By far the most common method involves performinga canthotomy and cantholysis of the tendon securingthe lateral eyelid. This technique is described inmany ophthalmic and surgical texts. 21-23,27,30,34,35,43,44 Performinga lateral canthotomy exposes the lateral canthaltendon, allowing surgical section via cantholysis of theinferior and/or superior crus of the tendon from their naturalattachments. This causes laxity of the lower lid andprovides a sufficient increase in orbital compartmentspace to immediately relieve the compressive forces inmost instances.C. Advance the jaws of a small hemostat (one anteriorand one posterior to the tissue plane) horizontally acrossthe lateral canthus from the angle of the eyelid to themargin of the lateral orbital rim and clamp shut for oneminute. This crushing force will help compress theswollen tissues, provide additional hemostasis, and leavea physical marker of the proper region to be cut duringthe canthotomy (Figure 3).TECHNIQUE OF LATERAL CANTHOTOMY ANDCANTHOLYSISThe procedure can be performed in the following stepwisefashion:A. The surgical area of the affected eye should beprepped in sterile fashion if possible. If available, gentlyclean with 5% betadine; however, due to the immediatenature of the situation, saline irrigation is sufficient if thisis not available.B. Pain control and hemostasis are achieved via local injectionof approximately 1cc of 2% lidocaine with epinephrine.Using a 27-gauge needle, anesthetize thecutaneous and deep tissues just lateral to the lateral angleof the affected eyelid with the needle directed away fromthe eye. Care should be taken to inject into the local cutaneousregion and NEVER into the eye or orbit itself.The quantity of anesthetic should be sufficient to coverthe region between the angle and the bony lateral orbitalrim, and additional anesthetic should be applied if the patientis experiencing discomfort (Figure 2).Figure 3: Clamp a small hemostat horizontally across thelateral canthus from the angle of the eyelid to the margin ofthe lateral orbital rim.D. After removing the hemostat, advance a pair of blunttipped scissors with blades open, one anterior and oneposterior to the crushed region previously marked. Withthe scissors, the lateral canthotomy is then performed bycutting horizontally, from the lateral angle of the eyelidto the bony margin of the orbital rim; approximately a1cm cut (Figure 4).Figure 2: The cutaneous and deep tissues just lateral to thelateral angle are anesthetized with 2% lidocaine withepinephrine.Figure 4: With blunt tipped scissors, cut horizontally fromthe lateral angle of the eyelid to the bony margin of the orbitalrim along the line left by the hemostat.28Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
E. The canthotomy allows for additional exposure of thedeeper tissue, including the inferior and superior crus ofthe lateral canthal tendon. Maximize this exposure bygently taking your hemostat or tooth forceps to grasp thelower lid laterally and pull down and away to help evertthe lid and expose this tissue plane.F. Identify the now exposed tendon in the surgical field.This can be done more easily by palpation than visually.Using the closed blades of a pair of scissors it is possibleto strum the crus in order to further identify theproper structure.G. Once identified, a cantholysis can be performed. Cutthe inferior crus of the lateral canthal tendon with thescissors pointed inferoposteriorly to release it completelyfrom its attachment to the lower lid (Figure 5). This incisionwill be 1-2cm in length and depth. Upon propercantholysis the lower lid should fall away from the lidmargin. If not, repeat this step until the tendon has beenreleased properly and the lid relaxes (Figure 6).Figure 5: Cut the inferior crus of the lateral canthal tendonwith the scissors pointed inferoposteriorly to release it completelyfrom its attachments.Figure 6: Upon proper cantholysis the lower lid should fallaway from the lid margin.H. Do not close the surrounding tissue. The surgicalfield can be covered lightly by gently taping a sterile 4x4gauze pad loosely over the area, but closure should bedelayed for a higher echelon of care after the acuteretrobulbar hemorrhage has resolved.COMPLICATIONSIf properly performed, the risks of this procedureare relatively low. Cosmetic concerns due to theloss of suspension of the lower lid can be addressed at alater date by trained ophthalmologists with excellent resultsand minimal scarring, despite the delay in closure.Deeper orbital contents can be avoided. Sensitive surroundingstructures, including the levator aponeurosis,lacrimal gland, and the lacrimal arteries are found superiorto the surgical site and easily avoided with goodtechnique. The key to minimizing surgical complicationsis recognizing the indications and contraindicationsfor performing orbital decompression, and conductingproper training of first line responders in the correct lateralcanthotomy and cantholysis technique.Lateral canthotomy and cantholysis is performedinfrequently in emergency departments; therefore,a laboratory-based curriculum using a swine modelwas developed to teach emergency medicine residentsand pediatric emergency medicine fellows the propertechnique and to provide them with hands-on training. 45The University of Nebraska Medical Center Departmentof Emergency Medicine has an organized “EmergencyProcedures Laboratory” that provides an opportunity toassess procedure skills, including lateral cantholysis, ina controlled environment. 46 Successful use of a porcinemodel for training has been documented in the literatureand would be an excellent option for teaching the properskill set to forward personnel. 45,47CONCLUSIONWartime environments task first line providerswith the difficult responsibility of providing immediatecare to save life, limb, and sight. As described above,the uncommon complication of retrobulbar hemorrhagecan quickly become a vision-threatening emergency inpatients with facial trauma, particularly when higher echelonassets are unavailable for definitive care. In thesecircumstances, knowledge of how to recognize and treatthis threat to sight immediately upon presentation is necessaryfor vision preservation.While the overall incidence may be low, whenpresent it is a blinding condition where visual outcomescould otherwise be saved by well-trained non-ophthalmologistscomfortable handling live tissue. Although allfirst responders do not have the basic training necessaryto perform this technique, EMT-P trained providers, suchas 18D medical sergeants, have attained a reasonableskill set through prior handling of live tissue from whicha method for basic orbital decompression could be appropriatelyadded. In addition, 18D medical sergeantsEmergency Lateral Canthotomy and Cantholysis: A Simple Procedure to Preserve Vision fromSight Threatening Orbital Hemorrhage29
are more likely to find themselves in austere environmentswhere delayed evacuation would merit the needfor such skills. Teaching this subset of first respondershow to properly perform a lateral canthotomy and cantholysiswould provide them an invaluable tool to bettercare for their wounded in a timely fashion. Thistraining could occur through the use of live tissue modelsunder supervision, as occurs for emergency physiciansin their residency programs. Training 18Dmedical sergeants to recognize and treat the clinicalsigns and symptoms of OCS from retrobulbar hemorrhagevia this technique brings a potentially vision-savingintervention closer to the Soldier who is in need ofemergent care.REFERENCES1. Selezinka, W. (1988). Evaluation of the injured eye. CanFam Physician; 34:2267-2273.2. Pokhrel, P.K. and Loftus, S.A. (2007). Ocular emergencies.Am Fam Physician; 76(6):829-836.3. Law, F.W. (1971). Spontaneous orbital haemorrhage. BrJ Ophthalmol; 55(8):556-558.4. Whitwell, J. (1956). Spontaneous haematoma of theorbit. Br J Ophthalmol; 40(4):250-251.5. Roberts, W. (1955). Hematoma of the orbit. Report oftwo cases. Am J Ophthalmol; 40:215-219.6. Brooks, A.M.V. and Finkelstein, E. (1984). Spontaneousorbital haemorrhage. Br J Ophthalmol; 68:838-840.7. Kwon, J.-H., et al. (2008). Spontaneous intraorbital hemorrhage:A case report. J Korean Neurosurg Soc; 44:156-158.8. Dutton, G.N., et al. (1981). Ophthalmic consequencesof midface trauma. Eye; 6:86-89.9. Ord, R.A. (1981). Postoperative retrobulbar haemorrhageand blindness complicating trauma surgery. Br JOral Surg; 19:205-207.10. Larsen, M. and Wiesland, E.S. (1999). Acute orbitalcompartment syndrome after lateral blow-out fracture effectivelyrelieved by lateral cantholysis. Acta OphthalmolScand; 77(2):232-233.11. Long, J.C. and P.P. Ellis. (1971). Total unilateral visualloss following orbital surgery. Am J Ophthalmol;71(1):218-220.12. Krohel, G.B. and Wright, J.E. (1979). Orbital hemorrhage.Am J Ophthalmol; 88(2):254-258.13. Todd, B.J., Sullivan, T.J., and Gole, G.A. (2001). Delayedorbital hemorrhage after routine strabismus surgery.Am J Ophthalmol; 131(6):818-819.14. Warburton, G. and Brahim, J. (2006). Intraorbitalhematoma after removal of upper third molar: A case report.J Oral Maxillofac Surg; 64(4):700-704.15. Butler (2006). Penetrating Injury to the Orbit. NOM-LLC Case Report 0601; 29 Nov 2006.16. Lewis, C.D. and Perry, J.D. (2007). Retrobulbar hemorrhage.Expert Rev Ophthalmol; 2(4):557.17. Zachariades, N., Papavassilious, D., and Christopoulos,P. (1996). Blindness after facial trauma. Oral Surg OralMed Oral Pathol Oral Radiol Endod; 81(1):34-37.18. Ansari, M.H. (2005). Blindness after facial fractures: A19-year retroscpective study. J Oral Maxillofac Surg;63(2):229-237.19. Burns, G.D. and DeLellis, S.M. (2007). Lateral canthotomyin orbital compartment syndrome: <strong>Special</strong> <strong>Operations</strong>medics on the battlefield can save the eye. J <strong>Special</strong><strong>Operations</strong> Medicine; 7(3):33-36.20. Bailey, W.K., Paul, C., and Evans, L.S. (1993). Diagnosisand treatment of retrobulbar haemorrhage. J OralMaxillofac Surg; 51:780-781.21. Peak, D.A. (2007). Acute orbital compartment syndrome.eMedicine Journal (Serial Online). RetrievedJuly 5, 2009 from emedicine.com website. Website:http://www.emedicine.com/emerg/topic881.htm.22. McInnes, G. and Howes, D.W. (2002). Lateral canthotomyand cantholysis: A simple, vision-saving procedure.Can J Emerg Med; 4(1):49-52.23. Vassallo, S., et al. (2002). Traumatic retrobulbar hemorrhage:Emergent decompression by lateral canthotomyand cantholysis. J Emerg Med; 22(3):251-256.24. Carrim, Z.I., Anderson, I.W.R., and Kyle, P.M. (2007).Traumatic orbital compartment syndrome: Importance ofprompt recognition and management. European J EmergMed; 14(3):174-176.25. Gerbino, G., Ramien, G.A., and Nasi, A. (2005). Diagnosisand treatment of retrobulbar haematomas followingblunt orbital trauma: A description of eight cases. Int JOral Maxillofac Surg; 34:127-131.26. Harrahill, M. (2006). A case report of traumatic eyecompartment syndrome. J Emergency Nursing; 1:104-105.27. Saussez, S., et al. (1998). Lateral canthotomy: A simpleand safe procedure for orbital haemorrhage secondary toendoscopic sinus surgery. Rhinology; 36(1):37-39.28. Katz, B., Herschler, J., and Brick, D.C. (1983). Orbitalhaemorrhage and prolonged blindness: A treatable posterioroptic neuropathy. Br J Ophthalmol; 67(8):549-553.29. Heyreh, S.S. and Jonas, J.B. (2000). Optic disk and retinalnerve fiber layer damage after transient central retinalartery occlusion: An experimental study in Rhesusmonkeys. Am J Ophthalmol; 129(6):786-795.30. Goodall, K.L., et al. (1999). Lateral canthotomy and inferiorcantholysis: An effective method of urgent orbitcaldecompression for sight threatening acute retrobulbarhaemorrhage. Injury; 3(7):385-390.31. Benton, M.D. (2004). The use of emergent lateral canthotomyto restore vision (letter). Am Fam Physician;69(9).32. Perry, M., et al. (2005). Emergency care in facial trauma:A maxillofacial and ophthalmic perspective. Injury;36:875-896.30Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
33. Rosdeutscher, J.D. and Stradelmann, W.K. (1998). Diagnosisand treatment of retrobulbar haemorrhage resultingfrom blunt periorbtial trauma. Ann Plast Surg;41:618-622.34. Iwamoto, M.A. and Iliff, N.T. (1998). Management oforbital trauma. In T.W. and E.A. Jaeger, Ed. Duane’sClinical Ophthalmology. Philadelphia, LippincottWilliams & Wilkins. 1998, Chapter 87, p 1-4.35. Rhee, D.J. and Pyfer, M.F. (2002). Traumatic retrobulbarhemorrhage. In D.J. Rhee and M.F. Pyfer Ed. TheWills Eye Manual. Office and emergency room diagnosisand treatment of eye disease. Philadelphia, LippincottWilliams & Wilkins. 2002, p. 41-44.36. Han, J.K., et al. (2008). Management of retrobulbarhematoma. Am J Rhinol; 22(5):522-524.37. McIlwaine, G.G., Fielder, A.R., and Brittain, G.P. (1989).Spontaneous recovery of vision following an orbitalhaemorrhage. Br J Ophthalmol; 73:926-927.38. Wood, C.M. (1989). The medical management of retrobulbarhaemorrhage complicating facial fractures: A casereport. Br J Oral Maxillofacial Surg; 27:291-295.39. Prodhan, P., et al. (2003). Orbital compartment syndromemimicking cerebral herniation in a 12-year-oldboy with severe traumatic asphyxia. Ped Crit Care Med;4(3):367-369.40. Markovits, A.S. (1977). Evacuation of orbital hematomaby continuous suction. Ann Ophthalmol; 9(10):1255-1258.41. Liu, D. (1993). A simplified technique of orbital decompressionfor severe retrobulbar hemorrhage. Am JOphthalmol; 116(1):34-37.42. Markovits, A.S. (1994). A simplified technique of orbitaldecompression for severe retrobulbar hemorrhage(Letter to the Editor). Am J Ophthalmol; 117(1):124.43. Friedberg, M.A. and Rapuano, C.J. (1990). Traumaticretrobulbar hemorrhage. In M.A Friedberg and C.J. RapuanoEd. Wills Eye Hospital office and emergency roomdiagnosis and treatment of eye disease. Philadelphia, J.B.Lippincott company. P. 36-38.44. Liu, L. and Hackett, T.S. (2006). Lateral orbital canthotomy.eMedicine Journal (Serial Online). Retrieved July5, 2009 from emedicine.com website. Website:http://www.emedicine.com/proc/topic82812.htm.45. Suner, S., Simmons, W., and Savitt, D.L. (2000). Aporcine model for instruction of lateral canthotomy. AcadEmerg Med; 7(7):837-838.46. Wadman MC. (2007). Emergency Procedures Laboratory.University of Nebraska Medical Center. EmergencyMedical Education. Retrieved July 6, 2009 from Universityof Nebraska Medical Center website. Website:http://www.unmc.edu/dept/emergency/education/index.cfm?L2_ID=34&L1_ID=2&L3_ID=33&CONREF=2847. Sanchez, L.S., et al. (2006). Procedure lab used to improveconfidence in the performance of rarely performedprocedures. Eur J Emerg Med; 13(1):29-31.CPT Steven Roy Ballard graduated from Brigham Young University with a BS in Finance and Zoologyin 2000. He received his commission to the Army in 2001 and completed his medical degreefrom Uniformed Services University in 2005. Upon completion of a transitional internship at EisenhowerArmy Medical Center in 2006 he was assigned to Fort Carson, CO, as a GMO where he wasprivileged to care for the 2nd Brigade Combat Team rear detachment during their deployment toIraq. He is currently engaged in his final year of ophthalmology residency training at the Universityof Tennessee in Memphis, and will return to military service in 2010.Robert W. Enzenauer, MD is currently professor of ophthalmology and Chief of Ophthalmology at theChildren's Hospital in Aurora, CO. Dr. Enzenauer is board certified in ophthalmology, preventivemedicine (aerospace medicine), and pediatrics. With over 35 years of uniformed service on activeduty and in the Army National Guard, for the past decade COL Enzenauer has served as a Senior FlightSurgeon and the Battalion Surgeon of the 5/19th SFG(A), Colorado Army National Guard. He deployedto Afghanistan 2002-2003 during OEF and to Iraq 2003-2004 during OIF.Thomas J. O’Donnell, MD, Col, USAF, MC (Ret) earned his undergraduate degree at the University ofTennessee, Knoxville, and his medical degree at the University of Tennessee Health Science Center inMemphis (UTHSC). He served as a Naval flight surgeon and then completed an ophthalmology residencyat UTHSC. He retired from the U.S. Air Force after serving 22 years of active duty including toursas an ophthalmologist, Chief of the Medical Staff, and squadron commander. He completed a neuroophthalmologyfellowship at Duke University Medical Center, and is currently Director of the Neuro-Ophthalmology and Low Vision services at the Hamilton Eye Institute, UTHSC.Emergency Lateral Canthotomy and Cantholysis: A Simple Procedure to Preserve Vision fromSight Threatening Orbital Hemorrhage31
Dr. James C. Fleming, received his medical degree from the University of Tennessee Center for theHealth Sciences in June, 1974. He continued his medical training at the University of Tennessee in ophthalmologyand pursued fellowship training in ophthalmic plastic and reconstructive surgery at the Universityof Arizona. Returning to Memphis in 1980, he has served as Chief of Oculoplastics at the levelI trauma center for over twenty years. He joined the UT Department of Ophthalmology as a full-timephysician in January 1997 to head the Oculoplastic Service, and currently is honored to hold the PhilipM. Lewis Professor of Ophthalmology Chair. His service in the field of ophthalmology has been recognizedon a national level by the presentation of the Senior Achievement Award from the AmericanAcademy of Ophthalmology in 2005. He has held the office of president for the Tennessee Medical Association, andcontinues to serve as the chairman of the Tennessee Medical Association Delegation to the American Medical Association.Also, he was honored to serve as president of the American Society of Ophthalmic Plastic and ReconstructiveSurgery, his subspecialty organization.COL Gregory Risk is an Emergency Physician/Flight Surgeon currently assigned to USASOC. He completed SFQC asan 18D in 1982 and was assigned to 7th SFG. He graduated from the Indiana University School of Medicine in 1993and completed emergency medicine residency at Methodist Hospital in 1996. COL Risk was previously assigned as AsstDean, Joint <strong>Special</strong> <strong>Operations</strong> Medical Training Center.Aaron Noble Waite graduated from Brigham Young University with a BS in Zoology in 2001. He completedhis medical degree from the University of Utah School of Medicine in 2006 and an internal medicineinternship at the University Medical Center in Las Vegas Nevada in 2007. He is currently engagedin his final year of ophthalmology residency training at the University of Tennessee in Memphis.32Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
Tinnitus, a Military Epidemic:Is Hyperbaric Oxygen Therapy the Answer?LCDR Thomas M. Baldwin, MD, MPTABSTRACTTinnitus is the phantom perception of sound in the absence of overt acoustic stimulation. Its impact on themilitary population is alarming. Annually, tinnitus is the most prevalent disability among new cases added to theVeterans Affairs numbers. Also, it is currently the most common disability from the War on Terror. Conventional medicaltreatments for tinnitus are well documented, but prove to be unsatisfying. Hyperbaric oxygen (HBO 2 ) therapymay improve tinnitus, but the significance of the level of improvement is not clear. There is a case for large randomizedtrials of high methodological rigor in order to define the true extent of the benefit with the administration ofHBO 2 therapy for tinnitus.THE PHYSIOLOGY OF HEARINGHearing is a series of events in which soundwaves in the air produce electrical signals and causenerve impulses to be sent to the brain where they are interpretedas sound. The auditory system consists of theexternal, middle, and inner ears, as well as the centralauditory pathways in the brain. Sound waves enter theexternal ear via the pinna and reach the middle earwhere they strike the eardrum and cause it to vibrate.The vibrations set the middle-ear bones (malleus,incus, stapes) in motion. Movement of the stapescauses pressure waves in the fluid contained within thecochlea, which contains the organ of Corti, the sensoryorgan for hearing. The primary sensory receptors forhearing, the inner hair cells, are found within the organof Corti as are the outer hair cells, which primarily facilitatethe sensory response of the inner hair cells. 1The fluid in the cochlea moves the top portion of thehair cells, called the hair bundle, which initiates thechanges that lead to the production of the nerve impulses.The nerve fibers connected to the hair cells, primarilythe inner hair cells, are excited and transfer theauditory information to the brain where they are interpretedas sound. 1, 2THE ETIOLOGY OF TINNITUSTinnitus, the perception of sound in the absenceof an external source, is a chronic and debilitatingcondition often described as ringing, hissing,buzzing, chirping, high-pitched squealing, or roaringin the ears or in proximity to the head. 2-4 According tothe National Research Council, tinnitus is considered asymptom rather than an illness. 2 The perceived noisecan be within one or both ears, within or around thehead, or perceived as an outside distant noise. It can bepulsatile or nonpulsatile and be continuous or occur intermittently.Tinnitus can be caused by or accompanymany conditions, including presbycusis, Meniere’s disease,otosclerosis, head injury, cerebellar-pontine angletumors, otitis media, meningitis, dental disorders, andcertain medications. However, most tinnitus is due tonoise induced sensorineural hearing loss with result-2, 5, 6ing dysfunction within the auditory system.The presence of tinnitus often is an early indicatorof cochlear hair cell dysfunction or loss, as in thecase of excessive noise exposure. 3 The pathogenesis isassumed to consist of micromechanical traumatic andbiochemical-metabolic damage to the outer hair cells. 3Studies have shown how hair cells of the inner earreact to damage caused by noise. 7,8 In acoustic trauma,defined as an acute impairment of hearing caused bysharp sounds, like that of a gun going off, the partialpressure of oxygen decreases significantly in the fluidspaces of the inner ear. 7 Morphological damage results,leading to intra and extracellular ion imbalancesand hearing damage. Histological findings areswelling and structural damage of the dendrites, alterationsof mitochondria and the cell-structure, separationof hair-cells from tectorial membrane, oedema ofthe endothelium, and oedematous closure of functionalendarteries with blocking of the microcirculation. 7 Ifthe swelling persists for a prolonged period, the haircells degenerate and are replaced by non-functioningendothelial cells. 7,9 PET scanning and functional MRIstudies indicate that the loss of cochlear input to neuronsin the central auditory pathways (such as occurswith cochlear hair cell damage due to noise trauma)can result in abnormal neural activity in the auditorycortex. 3 Such activity has been linked to tinnitus. It isimportant to note, that sounds of moderate intensity asencountered in everyday life usually do not affect theTinnitus, a Military Epidemic:Is Hyperbaric Oxygen Therapy the Answer?33
oxygen tension within the cochlea. 7 As tinnitus is usuallyaccompanied by hearing loss, similar mechanismsare likely involved.THE CHARACTERISTICS OF NOISENoise, defined medically as an intense soundcapable of producing damage to the inner ear, leads toone of the most common conditions evaluated by otolaryngologist:noise induced hearing loss (NIHL).Noise can be further categorized as impulse noise, theproduct of explosive devices, or impact noise, causedby a collision of two hard surfaces. However described,both are produced by a sudden intense soundwave capable of causing inner ear damage. Excessivenoise exposure is the most common cause of hearingloss. 2,5,6 When an individual is exposed to sounds thatare too loud or loud sounds over a long period of time,sensitive structures of the inner ear can be damaged,resulting in NIHL. In humans, outer hair cells are usuallythe first type of sensory cell to be damaged. 2 Asthe hearing loss progresses and becomes more permanent,the degeneration involves both outer andinner hair cells. As the number of hair cells decreases,so does an individual’s hearing. With severe permanenthearing losses, both sensory and supporting cellsof the organ of Corti are missing. In these cases, thedegenerative layer of the organ of Corti is replaced byan undifferentiated layer of squamous epithelium andthe sensory nerve fibers are destroyed. 9 The type andamount of the resulting hearing loss are typically determinedby the following acoustic parameters: the intensityof the noise, the duration of exposure to thenoise, and the type of noise.Intensity of sound is measured in units calleddecibels (dB), a measurement of the amount of energyor air pressure moving from the source to our ear. 10,11,20The faintest sound humans with normal hearing candetect has a value between zero and ten decibels, andthe loudest sound the human ear can tolerate withoutpain is about 120 decibels. 10 Decibels are measuredlogarithmically, being 20 times the log of the ratio ofa particular sound pressure to a reference sound pressure.This means that as decibel intensity increasesby units of 20, each increase is 10 times the lower figure.Thus, 20 decibels is 10 times the intensity of 0decibels, and 40 decibels is 100 times as intense as 20decibels. 20 The Navy considers any sound above84dB as noise hazardous and having the potential tocause hearing damage if it is loud enough or lasts longenough. 4,5,10,12 The higher the intensity of the sound,the greater its potential to cause hearing damage. Singleexposures to impulse noises above 140 decibelshave the potential to cause permanent damage. 4 Accordingto the U.S. Army Center for Health and PreventativeMedicine, a gunner on a 105 millimetertowed howitzer experiences an impulse noise of183dB. 2,4 A servicemember who shoots a rifle is exposedto 157-163dB and a gunner with a machine gun,145dB. 2,5,10,12 Those suffering from an improvised explosivedevice (IED) are exposed to impulse noise inexcess of 180dB. 13Duration is defined as the length of time youare exposed to a noise. The louder the sound and moreprolonged the exposure, the shorter amount of time ittakes to cause hearing damage. For unprotected ears,the allowed exposure time decreases by one half foreach 5dB increase in the average noise level. 5,14 Forinstance, exposure is limited to eight hours per day at90dB, four hours per day at 95dB, and two hours perday at 100dB. The highest permissible noise exposurefor the unprotected ear is 115dB for 15 minutes perday. 5,14 Sounds of less than 75dB, even after long exposure,are unlikely to cause hearing loss.Hearing loss that results from exposure tosound with energy spread across a wide range of frequencies,such as impulses common to military settings,is often characterized by a gradual increase inthreshold as frequencies increase. The hearing losstypically reaches a maximum between 3000 and 6000hertz (Hz), followed by a return toward normal hearingat still higher frequencies. This pattern of hearing lossis often referred to as the “noise-notch” audiogram andis a clinical hallmark often used to distinguish noise-relatedhearing loss from that associated with other etiologies,such as ototoxic medications or aging. 2CHRONIC NOISED-INDUCED HEARING LOSS ANDACOUSTIC TRAUMAChronic NIHL is a disease process that occursgradually over many years of exposure to less intensenoise levels. It is generally caused by long term exposureto high intensity continuous noise with superimposedepisodic impact or impulse noise. The hearingloss associated with chronic NIHL is variable betweenindividuals, but the principal characteristics remain relativelyconsistent: 14-17• It is always sensorineural affecting the hair cells inthe inner ear.• It is nearly always bilateral and symmetric.• It will only rarely produce a profound loss.• It will not progress once noise exposure is stopped.• The higher frequencies (3000-6000Hz) are more affectedthan the lower frequencies, with the greatestloss usually occurring at 4000Hz.• Continuous noise is more damaging than intermittentnoise.• Tinnitus is often associated with NIHL.One exception to these features would be theindividual who had significant noise exposure secondaryto rifle shooting. In this case, an asymmetrical loss,with the ear nearest the gun barrel demonstratingslightly worse hearing, would be expected. 1434Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
The development of chronic NIHL progressesthrough two phases. A brief hearing loss, more commonlyreferred to as a temporary threshold shift (TTS),characterizes the first stage. It occurs after noise exposureand completely resolves after a period of rest.Often reported as auditory fatigue, most studies indicatethat it is associated with no sensory cell damage orminimal, reversible cell changes. 14,18 Eventually, afterrepeated exposure to noises intense enough to produceTTS, a permanent threshold shift (PTS) will occur.This is an irreversible increase in hearing thresholdsand defines the second stage of chronic NIHL. At thispoint, there has been irreversible hair cell damage. 5,14,18In contrast to chronic NIHL, acoustic traumarefers to a sudden permanent hearing loss caused by asingle exposure to an intense sound. It occurs whenexcessive sound energy strikes the inner ear. Exposureto noise from firearm use during military service isprobably the most frequent etiology of acute acoustictrauma worldwide; therefore, it may be regarded as aprofessional disease in military populations. 19 Thesound pressure levels capable of causing acoustictrauma vary between individuals but average around130-140dB. 14 The hearing loss is sudden, sometimespainful, and is often followed by a new onset of tinnitus.For the vast majority of patients, tinnitus presentsas the most annoying symptom, with the risk for permanenttinnitus being considered more critical for thepatient than any degree of hearing loss resulting fromacoustic trauma. 19 Although the audiogram may showthe typical 3000-6000Hz sensorineural notch seen withchronic NIHL, down-sloping or flat audiograms thataffect a broad range of frequencies are more common.2,14,20 Direct mechanical injury to the sensory cellsof the cochlea is thought to be the mechanism of injuryin acoustic trauma.Noise exposure and NIHL are the most commoncause of tinnitus. 2,5,6 The relationship betweennoise exposure, NIHL and tinnitus has been addressedin a number of articles. A review of these studies waspresented by Axelsson & Barrenas, 1991, and it wasfound that noise exposure and NIHL were by far themost common cause of tinnitus; if “acoustic trauma”was included, at least one-in-three cases were causedby noise. 6 Tinnitus may occur following a single exposureto high-intensity impulse/impact noise (a shortburst of acoustic energy which can either be a singleburst or multiple bursts of energy), long-term exposureto repetitive impulses, long-term exposure to continuousnoise, or exposure to a combination of impulsesand continuous noise. 2,4,6THE “IMPACT” OF NOISE ON THE MILITARYA staggering number of Soldiers and Marinescaught in roadside bombings and firefights in Iraq andAfghanistan are coming home with ringing in theirears. High rates of tinnitus among patients exposed togunfire and explosive detonations suggest that impulse/impactnoise is likely to precipitate tinnitus associatedwith acoustic trauma, excessive noiseexposure, and NIHL. 2,4,6,10,12 According to researchpublished in the December 2005 issue of AmericanJournal of Audiology (AJA), Soldiers sent to battlezones are over 50 times more likely to suffer NIHL lossand/or tinnitus than Soldiers who do not deploy. 21 Accordingto a report released in 2007 by the House AppropriationsSubcommittee on Military Quality of Life,as a result of ongoing combat operations, one in threepost-deploying Soldiers report acute acoustic traumaand one in four report hearing loss and/or hearing complaintsto include tinnitus. 12From World War II and well through the VietnamWar, hearing damage has been a leading disability.According to the Department of Veterans Affairs,hearing damage is the number one disability in the Waron Terror, with some experts predicting the true tollcould take decades to become clear. 13 According to theAmerican Tinnitus Association (ATA), more will bespent on veterans’ disability compensation for tinnitusand other hearing conditions over the coming yearsthan for any other medical injuries from the Iraq andAfghan wars. 4 Between 2000 and 2005, the number ofveterans with tinnitus disabilities more than doubledand the amount paid to veterans with tinnitus disabilitieswent up more than two-and-a-half times. 4,22Presently, tinnitus is the most prevalent disabilityamong new cases added to Veterans Affairs numbers;nearly 70,000 of the more than 1.3 million troops whohave served in Afghanistan and Iraq are collecting disabilityfor tinnitus. 13,23 In fact, recent studies demonstratedthat 49-50% of all Soldiers exposed to explosiveblasts in Iraq and Afghanistan had tinnitus and 60%had tinnitus, often related to hearing loss. 4,13,22,24 Thenumber of servicemembers on disability because ofhearing damage is expected to grow 18% a year, withpayments totaling $1.1 billion annually by 2011. 4,13The economic consequences to the military forhearing impairment, to include tinnitus, include losttime and decreased productivity, loss of qualifiedworkers through medical disqualification, military disabilitysettlements, retraining, and expenses related tomedical treatment such as hearing aids and audiometrictesting. 10 While the economic consequences are significant,the military implications in a combat zone canbe deadly.A study published in the Army RD&A Bulletinin 1990, concluded that those with hearing impairmentswere 36% more likely to hear the wrong command, and30% were less likely to correctly identify their target. 4Additionally, it was noted that Soldiers with hearingimpairments only hit the enemy target 41% of the time,while Soldiers without hearing impairments hit theenemy target 94% of the time. Those with hearing impairmentswere 8% more likely to take the wrong tar-Tinnitus, a Military Epidemic:Is Hyperbaric Oxygen Therapy the Answer?35
get shot and 21% more likely to have their entire tankcrew killed by the enemy. 4Hearing damage has been a battlefield riskever since the introduction of explosives and artillery,and the U.S. military recognized it in Iraq andAfghanistan and issued earplugs early on. But thesheer number of injuries and their nature, particularlythe high incidence of tinnitus, came as a surprise tomilitary specialists and outside experts. According toVA figures, despite all that has been learned over theyears, U.S. troops are suffering hearing damage atabout the same rate as World War II veterans. 13,21Given today’s unpredictable weaponry (i.e. roadsidebombs), even the best hearing protection is only partlyeffective, and only if it’s properly used.It makes more sense to prevent hearing damagethan to provide a lifetime of disability, but evenhearing protection has its limits and it is important tonote that some hearing impairments are unavoidabledespite use of hearing protection and other measures.Some exposures are so extreme that they will exceedthe protective capability of hearing protective devices.As previously noted, damage can occur at 85 decibels.The best protection cuts that by only 20-25dB. 13 Thatis not enough to protect the ears against an explosionor a firefight, which can range upwards of 180+ dB.Furthermore, much of the fighting consists of ambushes,bombings, and firefights, which come suddenlyand unexpectedly, giving Soldiers little time touse their issued hearing protection. In addition, someInfantrymen resist or refuse to wear their hearing protectionfor fear of dulling their senses and missing criticalcommands or sounds that can make the differencebetween life and death.HBO 2 THERAPY EFFICACY IN TINNITUSMedical treatments for tinnitus are well documentedand there is probably no other disease forwhich such a variety of treatments have been proposed.Yet, still today, many different treatment regimens arebeing propagated. Vasodilators, vitamins, steroids, anticoagulants,heparin, histamine, tranquillizers, diuretics,prostacyclin, hypervolemic hemodilution,carbogen, and stellate ganglion block. 3,25 Whether appliedseparately or together, all have demonstrated limitedeffectiveness at best. Experimentally, rheologicalagents and plasma expanders neither cause an improvementin inner ear blood supply nor result in ahigher oxygen supply in the inner ear. 26 In addition,two forms of tinnitus rehabilitation are currently beingprescribed, tinnitus masking and psychological treatment;both offer symptomatic treatment, with the goalof treatment being only to lessen the awareness of tinnitusand its impact on quality of life.Since the end of the 1960s, hyperbaric oxygen(HBO 2 ) therapy has been used experimentally for certainacute and chronic illnesses of the inner ear. 25 Therole of HBO 2 in the treatment of tinnitus was investigatedin the past: Pilgramm et al. in 1985, firstly, andSchumann et al. in 1990, secondly, reported aboutHBO 2 usefulness in tinnitus treatment, reporting animprovement of 62.2% in 557 patients’ tinnitus afterreceiving 10 applications of HBO 2 therapy. 25,27 Whileskepticism remains high in the Untied <strong>States</strong>, physiciansin Germany and Japan continue to recognize itsclinical applications in diseases of the inner ear andhave demonstrated improved outcomes in the treatmentof acute acoustic trauma, NIHL, and tinnitususing HBO 2 therapy. 7,26 The rationale for this therapyis based on the oxygen transportation mechanism inhuman organisms.The basis for hyperbaric oxygenation is thebreathing of pure oxygen at a pressure which is increasedcompared to atmospheric pressure (1.0ATA). 9,26,28-30 The effectiveness of high pressure oxygentherapy is based on raising the partial pressure ofoxygen in the blood and thus the pressure differenceto tissue. The concentration of oxygen in the atmosphereis 21%. At 1.0 ATA, the oxygen in blood is almostentirely carried by hemoglobin. Becausehemoglobin is approximately 97% saturated under normalconditions, greatly increasing the oxygen-carryingcapacity of blood by increasing hemoglobinsaturation is not possible.During hyperbaric oxygen therapy the patientsits inside a pressurized chamber. Air pressure insidethe chamber is increased up to 2.5 times normal atmosphericpressure at sea level (2.5 ATA). The patientthen breathes pure oxygen from a mask. Inhalation ofhyperbaric oxygen can enhance the amount of oxygencarried in blood by increasing the quantity of oxygendissolved in plasma. When breathing 100% oxygen ata surrounding pressure of 2.5 ATA, the quantity of dissolvedoxygen in 100ml of plasma increases from0.3ml, to 6.8ml, which is approximately 20 timeshigher than normal. 9,26The driving force for oxygen diffusion fromthe capillaries to tissue can be estimated by the differencebetween the partial pressure of oxygen on the arterialside and the venous side of the capillaries. Thedifference in the partial pressure of oxygen from thearterial side to the venous side of the capillary systemis approximately 37 times greater when breathing100% oxygen at 3.0 ATA than air at 1.0 ATA. 29The increased tissue oxygenation achievedduring HBO 2 therapy can support poorly perfused andhypoxic areas. Under this increased pressure, theamount of dissolved oxygen is sufficient, even withouthemoglobin, to supply body tissues with oxygenby diffusion. With an increase of the pressure of oxygenin the inner ear, it is possible to influence the auditorysensory cells (inner and outer hair cells) and theperipheral auditory nerve fibers. 30 These cells have nodirect vascular supply and depend entirely on oxygen36Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
supplied by diffusion. During exposure to HBO 2 therapy,the oxygenation in the cochlea increases by 460-600% and is still 60% above normal one hour aftertermination of the therapy. 9,26,30 An increase in oxygenpressure can compensate for oxygen deficiency causedby trauma and gives rise to biological mechanismswhich can facilitate cellular and vascular repair. 9,30 Additionally,HBO 2 therapy has been shown to improvehemorheology by causing a reduction in hematocrit, areduction of platelet aggregation, and an increase in theflexibility of erythrocytes. 31 Hyperoxia has also beenshown to reduce edema by reducing vascular permeabilityand causing a rapid and significant vasoconstriction.29HBO 2 is considered a relatively benign interventionwith few adverse effects. Visual disturbance,usually reduction in visual acuity secondary to conformationalchanges in the lens, and barotrauma, affectingthe middle ear, are the most frequently reported complications.15,16,29 The majority of patients recover spontaneouslyover a period of days to weeks from theirvisual disturbances and most episodes of barotraumado not require the therapy be abandoned. Barotraumaof the middle ear can be treated by placement of pressureequalization tubes or milder cases with decongestantsand/or instruction regarding pressure equalizationtechniques. Less commonly, estimated only to occur inone in 5,000 to 11,000 treatments, HBO 2 may be associatedwith acute central nervous system oxygen toxicity.15,16,29 Exposure to 100% oxygen at 3.0 ATA forthree hours induces grand mal seizures in most people;at less than 3.0 ATA, seizures are rare. 29 Oxygen-inducedseizures are typically benign and produce nolong-term sequelae. Additional complications includebarotraumas affecting the dental cavities and sinuses,pulmonary barotraumas, drug reactions, and injuries ordeath related to chamber fires. Decompression sicknesscan also occur, though rare in patients breathing100% oxygen with short air breaks.CURRENT LITERATUREThe evidence for HBO 2 therapy for acute andchronic tinnitus based on randomized controlled trialsis poor. In July 2004, Bennett et al. underwent an extensivesearch of what they considered to be “suitable”randomized human trials assessing the outcome of tinnituswith HBO 2 therapy. The inclusion criteria consistedof a randomized controlled study, a review withnew data, was not a comparative trial in which all subjects/groupsreceived HBO 2 therapy, subjects were randomlyallocated, and report was not a case study. 15,16The initial search identified six randomized human trialsmeeting the criteria. However, after appraisal of thefull report, three articles were excluded because theydid not contain new data. A follow-on search was conductedby Bennett et al. in 2006; no additional studieswere identified. 16 Using the same inclusion criteria, theauthor of this paper was unable to identify any additionalstudies that met all the criteria, but was able tofind a number of prospective and retrospective studiesevaluating the benefits of HBO 2 therapy for the treatmentof tinnitus.PROSPECTIVE STUDIESTwo of the randomized controlled trials, identifiedby Bennett et al., reported on improvements intinnitus for patients with an early/acute presentation.15,16,26 The Hoffmann et al. 1995a trial contributed20 subjects with idiopathic sudden sensorineural hearingloss (ISSHL) with or without tinnitus; all subjectshad no improvement after 14 days of pharmacologicaltreatment with hydroxyethyl starch, pentoxifylline, andcortisone. The Schwab et al. 1998 trial contributed 33subjects with sudden hearing loss and tinnitus seenwithin two weeks of onset of tinnitus and without anyprior therapy. In each study the HBO 2 group’s therapyconsisted of 100% oxygen at 1.5 ATA for 45 minutesdaily, five days each week for two to four weeks (10 to20 sessions). The control groups underwent no treatment.While the two trials reported a greater mean improvementin tinnitus (using a visual analogue scalebetween 0 and 10) in the HBO 2 arm compared to thecontrol arm, statistical pooling was not possible due tothe authors neglecting to report the standard deviationaround the means. As a consequence, clinical significancecould not be determined.The third article considered suitable, by Hoffmannet al. 1995b, was the only randomized humancontrolled trial reporting on improvements in tinnitusfor patients with a chronic presentation. 15,16 This studycontributed 44 subjects with ISSHL and tinnitus forlonger than six months. HBO 2 therapy consisted of100% oxygen at 1.5 ATA for 45 minutes daily, fivedays each week for three weeks. The control groupbreathed air at 1.5 ATA on the same schedule as theHBO 2 group. While the HBO 2 therapy group diddemonstrate some improvement in tinnitus, the improvementdid not reach statistical significance:p=0.12. 15,16In each of these studies the HBO 2 therapy consistedof breathing 100% oxygen at 1.5 ATA for 45minutes. In studies reporting significant improvements,HBO therapy consisted of breathing 100% oxygenat 2.0 to 2.5 ATA for 90 minutes.In 2007, a comparative trial by Porubsky et al.evaluating the influence of time interval from the onsetof tinnitus until the first HBO 2 therapy was published. 31In addition to time interval, the study compared the influenceof other factors: treatment protocols, gender,noise characteristic, and pretreatment expectations.This author will only comment on treatment protocolsand time interval from tinnitus onset to treatment.In this study, 360 patients suffering from tinnituswere randomized into two HBO 2 treatment pro-Tinnitus, a Military Epidemic:Is Hyperbaric Oxygen Therapy the Answer?37
tocols: group A: 2.2 ATA for 60 minutes and group B:2.5 ATA for 60 minutes. Both series were administeredonce a day for 15 consecutive days; 156 patients underwentprotocol A and 156 protocol B. Forty-eightpatients were treated inconsistently, leaving out singledays of treatment. No patient had less than twelveHBO 2 sessions. One month after the end of HBO 2treatment, the therapeutic effect was evaluated accordingto the patient’s subjective assessment of tinnitus.A non-treatment control group was not indentified.In 92 patients HBO 2 therapy was started within thefirst two weeks after the onset of tinnitus; in 93 therewas a delay between two weeks and six months; in 41cases the delay was 6-12 months; and in 126 patientsmore than one year elapsed between the onset of tinnitusand HBO 2 treatment. Eight patients did not answerthe question.A complete remission of tinnitus was reportedby 12 (3.3%) subjects, 122 (33.9%) felt a decrease inintensity, 157 (56.3%) patients did not notice anychanges and 25 (6.9%) patients complained that theirtinnitus became louder after HBO 2 . 31 Out of the 12 patientswho had a complete remission of tinnitus, 10(83.3%) had HBO 2 within the first two weeks after theonset of tinnitus and two (16.6%) later than two weeksbut within the first six months. Out of the 122 patientswho felt that their tinnitus had lessened, 37 (30.3%)had HBO 2 therapy within the first two weeks after theonset and 39 (31.9%) were treated within the first sixmonths. Only nine (7.4%) who started HBO 2 six totwelve months after the onset of tinnitus had improvementand thirty-four (27.9%) felt a lessening of tinnitusafter more than twelve months delay until HBO 2 . 31The authors determined there was no statisticallysignificant difference between treatment groupsA and B (p > .05). Furthermore, they concluded thereis no statistically significant difference between thetime intervals until the start of HBO 2 therapy. 31This study compared a treatment protocol of2.2 ATA for 60 minutes to a treatment protocol of 2.5ATA for 60 minutes. This study could have been enhancedif it would have compared two groups in whichthere was a bigger difference between treatment protocols(i.e. one group breathing 100% oxygen at lessthan 2.0 ATA) and/or included a non-HBO 2 therapycontrol group. Additionally, the study grouped patientsinto a treatment group receiving therapy within the firsttwo weeks after onset of tinnitus and one in which thepatient received therapy later than two weeks butwithin the first six months. Again the authors reportedno statistical significant difference between the timeintervals until the start of HBO 2 therapy. Most studiesgroup subjects into those suffering from tinnitus forthree months or less and those suffering from tinnitusfor greater than three months, but less than six months.Of the 122 patients treated, 39 (31.9%) who weretreated within the first six months, but after two weeksfrom the onset of their tinnitus, reported improvement.Of the 39, how many were treated within three monthsfrom the onset of their tinnitus, and if added to thosewho demonstrated improvement if treated within twoweeks from the onset of their tinnitus, would a significantdifference between time intervals be seen?In a study published in 2003 by Narozny et al.,61 patients with tinnitus (29 acute, 32 chronic) underwentHBO 2 therapy with simultaneous pharmacotherapy(group A). 25 HBO 2 therapy was administered oncedaily at a pressure of 2.5 ATA for 90 minutes (three periodsof 20 minutes with two five-minute air breaksand 20 minutes needed for compression and decompression).The patients breathed 100% oxygenthroughout the treatment with exception of the twofive-minute air breaks. Patients with acute tinnitus underwent15 + 6 HBO 2 expositions, patients withchronic tinnitus 18 + 6 expositions. Before, immediately,and six months after the end of treatment, thelevel of tinnitus was assessed by means of a visual analogscale (VAS), Vernon’s tinnitus severity scores(VTSS), and questionnaire by Tyler and Baker. Theobtained results were compared with 122 patients(group B) with tinnitus (70 acute and 52 chronic)treated only pharmacologically. Tinnitus improvementafter therapy was stated by comparison of tinnitus levelbefore and after therapy (in percentage).Satisfactory improvement of tinnitus loudness(more than 50% in comparison to primary state), usingthe VAS, was demonstrated in 58.6% of patients withacute tinnitus in group A. Of the 58.6% who demonstratedsatisfactory improvement, 41.4% showed excellentimprovement (75% to 100%) and 17.2%showed some improvement (50% to 75%). No improvement(less than 50%) was seen in 41.4% of theacute tinnitus patients in group A. Comparative analysisof group B subjects with acute tinnitus reflected41.4% with satisfactory improvement, 30.0% with excellentimprovement, and 11.4% with some improvement.No improvement was noted in 58.6% of theacute tinnitus patients in group B. Satisfactory tinnitusimprovement in patients with chronic tinnitus(group A) was 81.3%, 6.3% with excellent improvement,and 75.0% with some improvement. No improvementwas noted in 18.7%. Comparative analysisof group B subjects with chronic tinnitus revealed65.4% with satisfactory improvement, 25.0% with excellentimprovement, and 40.4% with some improvement.No improvement was noted in 34.6% of thechronic tinnitus patients in group B. 25 Similar resultswere obtained by VTSS and questionnaire. After sixmonths, there was an inconsiderable regression of thepositive effect of therapy, especially in patients withchronic tinnitus, in group A as well as in group B.The authors (Narozny et al.) concluded HBO 2therapy may contribute to the treatment of tinnitus, particularlyits chronic severe form. Their results were38Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
similar to those of other authors, indicating that HBO 2therapy can reduce tinnitus even if it has been presentfor a long time. 25-27The authors reported the wrong data for theacute tinnitus group B patients in their results sectionand unfortunately based their conclusions using the incorrectdata. Using the correct data (shown in Table 2of there study) HBO 2 therapy is shown to be more beneficialin the acute tinnitus stage (group A compared togroup B) than it is in the chronic stage (group A comparedto group B). While there is a 17.2% difference insatisfactory improvement in acute tinnitus patients comparinggroup A to group B, there is only a 15.9% differencein satisfactory improvement in chronic tinnituspatients comparing group A to group B.In a prospective controlled study conducted byBiesinger et al.(1998), 211 cases of acute tinnitus (tinnitusfor less than three months) were assessed after receivingone of three treatment protocols. 32 Of the 211cases of acute tinnitus, 69 patients were treated withhaemodilution and cortisone alone and had no HBO 2therapy. Of the 142 patients that had HBO 2 therapy, 72of these were after unsuccessful haemodilution.Of the 69 cases in which the patients receivedhaemodilution only, 36.2% healed completely, 38.8%cases did not notice a change, and 25% of the patientsreported a decompensation. Of the 142 cases receivingHBO 2 therapy, 64.1% healed completely, 17.9% experiencedno change, and 18% reported a decompensation.Out of the 72 cases receiving HBO 2 therapy afterfailure of haemodilution, 51.4% healed completely,whereas 37.5% reported improvement, 11.1% experiencedno change in their tinnitus, and 0% of the casesworsened. 7,32 The results demonstrated a better outcomefor patients with acute tinnitus if they received HBO 2therapy, especially the high rate of decompensated tinnitusin patients receiving solely haemodilution.In a study published in 1997 by Delb et al., 33 atotal of 193 patients, having undergone and failed primaryintravenous hemorheologic therapy, were treatedwith HBO 2 therapy. Tinnitus was evaluated before,after ten sessions, and after 15 sessions using a tinnitusquestionnaire. Measurable improvements of the tinnitusoccurred in 22% of the patients, moderate improvementin 17% of cases, excellent improvement in 10.4%of cases and complete resolution in two patients. 33Though clinical significance was not reported, the improvementrate decreased in those cases where the timefrom onset of tinnitus exceeded 40 days. In addition,while the improvement rate slightly increased in patientsreceiving 15 sessions compared to those receiving10 sessions, the clinical significance, once again, wasnot reported. The authors concluded that HBO 2 therapyseems to be a moderately effective additional treatmentin the therapy of tinnitus after primaryhemorheologic therapy, provided the time from onset oftinnitus is less than one month. 33In another study published in 1997 by Kau etal., 26 355 patients with tinnitus, who had not respondedto treatment with medications, were given HBO 2 therapy.Of the 355 patients, 192 suffered from tinnitus forless than three months and 163 suffered from tinnitusfor more than three months. HBO 2 therapy consistedof a pressure increase phase of 20 minutes, at the endof which a diving depth of 2.5 ATA was reached. Thispressure was held for 70 minutes which was then followedby an ascent phase lasting 20 minutes. Pureoxygen was inhaled by mask during the entire treatmentperiod. The number of treatments was not reportedand a non-HBO 2 therapy control group was notidentified. Subjective evaluation of tinnitus was expressedby means of a visual analog scale.For the patients in whom the first episode oftinnitus was within three months before HBO 2 therapy,excellent improvement was seen in 6.7%, noticeableimprovement in 44.3%, unchanged in 44.3%, and atemporary increase in the severity of tinnitus in4.7%. 26,30 Patients who had tinnitus for more than threemonths before HBO 2 therapy showed a less favorableresponse. In none of the patients did the tinnitus fullyresolve. Noticeable improvement was reported by34.4% of the patients, no change in tinnitus was appreciatedby 62% of the patients and an intermittent increasewas reported by 3.6% of the patients. 26,30The authors feel the results justify the positionthat patients, who have been treated unsuccessfully by“conventional” means, may still have a chance of improvementin their symptoms when they can be givenHBO 2 therapy within three months of the onset of theirtinnitus. 26In 1997, an article by Bohmer was publishedreporting on two prospective studies conducted at theInstitute for Hyperbaric Medicine, Orthopaedic UniversityClinic, Frankfurt, Germany. 28 In the first study,47 patients received HBO 2 therapy within three monthsof tinnitus first occurring. In each case they receivedpharmacotherapy often combined with cortisone priorto undergoing HBO 2 therapy. In 64% of the cases animprovement was attained. During the follow-up examinations27% of the patients confirmed a further decreaseof the ringing in their ears during the twomonths following treatment.In the second study, 381 patients underwentHBO 2 therapy for the treatment of their tinnitus. Onaverage 15 single treatments for 90 minutes with apressure of 2.2 to 2.5 ATA were carried out. Daily, atthe same time each day, the patients were asked to subjectivelyannotate their sound volume. Complete resolutionof tinnitus was seen in 3.9% of the patients.Noticeable improvement was seen in 34.1%, slight improvementin 31.8%, no improvement in 28.1%, andworsening of tinnitus in 2.1% of the patients. 28 WithHBO 2 therapy, the improvement of tinnitus sound from“becoming less” to “being completely healed” was ap-Tinnitus, a Military Epidemic:Is Hyperbaric Oxygen Therapy the Answer?39
preciated in the first six months of tinnitus first occurring.The major advances starting with “unbearablyloud” to “bearable” were made during the first two tothree months.The author recommends that HBO 2 therapyshould be liberally applied when infusion therapyshows no success. Even after four to six months successfulresults were obtained with tinnitus patients. 28RETROSPECTIVE STUDIESIn 1998, Lamm et al., and in 2003, Lamm reportedon a retrospective meta-analysis of 50 clinicalstudies carried out on a total of 4,109 patients who receivedHBO 2 therapy following unsuccessful conventionaltreatment with drugs for patients suffering fromtinnitus. 30,34 Providing the onset of the disorder waslonger than two weeks but not longer than six weeks,4% of the patients suffering from tinnitus reportedcomplete resolution, 81.3% observed a decrease in tinnitusintensity, 13.5% reported no change and 1.2% reporteda temporary increase in tinnitus. 30,34 Theseresults were confirmed in some of the prospective studiesdescribed above as well as additional studies byNakiashima et al. (1998), Shiraishi et al. (1998) andMurakawa et al. (2000). 26,33 The authors concludedthat HBO 2 therapy is recommended and warranted inthose patients treated within three months of the onsetof symptoms. 30,34In a retrospective evaluation of 7766 patientsin 13 publications showed reduction of the molestationand intensity of tinnitus by 50% in approximately 70%of the cases (30%-88%) if treated within the first threemonths. 7,9,35 Chronic tinnitus with duration of morethan three months or bilateral manifestation showedimprovement rates of 50% in around 30% of the casesafter ineffective conservative treatment. Follow-upsshowed no change in 12 months.An additional retrospective study published byHoffmann et al.. 28 250 patients who had been treatedunsuccessfully with infusion therapy received HBO 2therapy. These subjects were compared to patients whodid not receive HBO 2 therapy. The subjects wereunder observation for 21 months. In this study, 60% ofpatients undergoing HBO 2 therapy ascertained a steadytinnitus improvement. Other HBO 2 therapy centershave also shown good results; Almeling et al. (1996),Dauman et al. (1985), Meazza et al. (1996), and Takahashiet al. (1989).DISCUSSIONTinnitus is the phantom perception of sound inthe absence of overt acoustic stimulation. 36 Its impacton the military population is alarming. Annually, tinnitusis the most prevalent disability among new casesadded to Veterans’ Affairs rolls and is currently thenumber one disability in the War on Terror. There ismore being spent on veterans’ disability compensationfor tinnitus than on any other disability, with paymentsexpecting to reach $1.1 billion annually by 2011. 4,13A considerable number of therapies have beenproposed since tinnitus first appeared in medical literature.However, the results of established, conservativemedical treatment regimes for tinnitus areunsatisfying. It has been shown that common pharmacologicaltreatment does not yield better results thanplacebo therapy. 30,31,36 The knowledge of hyperbaricoxygen therapy for the hyperoxygenation of tissue hasled to further development of medical indications overthe past 50 years. Indications for ENT therapy includedecompression trauma of the inner ear, idiopathic suddenhearing loss, acute acoustic trauma, acute noiseinducedhearing loss, osteoradionecrosis andosteomyelitis, otogenic infection of the skull base, andotitis externa maligna. 30 HBO 2 treatment increases theinner ear pO 2 ; decreases hematocrit, plasma viscosity,and platelet aggregation, and improves microcirculation.29,30,37 In spite of its clear-cut rationale, an effectivenessof HBO 2 therapy has not been objectivelydocumented for tinnitus and its use in the <strong>United</strong> <strong>States</strong>has not been widely applied (this is not approved bythe Undersea and Hyperbaric Medicine Society). Dueto the low number of recognized, controlled, doubleblindclinical trials demonstrating the effectiveness ofHBO 2 therapy for tinnitus, this therapy lacks officialrecognition and skepticism remains high. Poormethodological quality in many of the reported trials,variability and poor reporting of entry criteria, the inconsistentnature and timing of outcomes, and poor reportingof both outcomes and methodology makecomparisons and meta-analysis impossible. In addition,treatment protocols and patient inclusion criteriaare not standard, and poorly reported in some trials. Nostandard severity scale is employed across these trials,and the time to entry varies from within hours to years.Many of the patients were negatively selected, they hadalready been treated by various methods and only thosewho had not responded to these therapies were treatedwith HBO 2 therapy. Moreover, many of the studiesneglected to identify a control group and many did notassess HBO 2 as a monotherapy.CONCLUSIONMany of the reports indicate the effectivenessof HBO 2 therapy for tinnitus, but a majority of themare retrospective and many suggest using HBO 2 therapyas an adjuvant to standard medical treatment.Nonetheless, the results justify the position that patientswith tinnitus, who have been treated conventionally,may still have a chance of improvement of their conditionwhen they can be given HBO 2 therapy withinthree to six months. These studies have shown that hyperbaricoxygenation treatment can suppress acute andeven longer existing tinnitus. It appears that during thefirst six months, HBO 2 therapy has a positive and40Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
promising effect on tinnitus. However, the most significantimprovement in tinnitus is notable when HBO 2therapy is administered within the first three months atpressures between 2.0 and 2.5 ATA.FUTURE RESEARCHBecause of its subjective nature, assessing thelevel of distress remains the primary impediment in theappraisal of tinnitus studies. In patient studies, differencesin the level of tinnitus, duration, medical history,and involvement of etiological factors in the initiationand mental habituation may obscure any correlationwith a treatment outcome. 38 There is a case for largerandomized trials of high methodological rigor in orderto define the true extent of the benefit (if any) from administrationof HBO 2 therapy to patients sufferingfrom tinnitus. A critical multicenter analysis with identicaldocumentation of a large number of patientsshould establish the therapeutic value of HBO 2 therapyfor well defined groups of patients. In addition,further studies to evaluate the actual effect of HBO 2therapy should concentrate on the development of double-blind,case controlled trials.Though the authors of several studies reportvarious degrees of improvement in up to 50% to 70%of patients undergoing HBO 2 therapy, actual cure oftinnitus is rare. In no study was it reported to be greaterthan 3.9%. If HBO 2 therapy is scientifically establishedto be beneficial in the treatment of tinnitus, costanalysis for treating tinnitus versus paying out VA benefitsshould be conducted. Will curing approximately4% of cases significantly reduce VA compensation fortinnitus and/or will a significant reduction in a patient’stinnitus affect VA compensation? A final evidencebased recommendation will be possible after conclusionof several randomized, controlled, double-blindstudies. Currently, there are six major prospective trialsbeing carried out in Germany. 7,9ACKNOWLEDGEMENTSThe opinions or assertions contained herein are theprivate views of the author and are not to be constructed asofficial or reflecting the views of the Department of theNavy, Department of Defense, nor the U.S. Government.REFERENCES1. Medical College of Wisconsin (2001). Noise-induced hearingloss. Retrieved March 16, 2009, fromHealthlink MedicalCollege of Wisconsin Website: http://healthlink.mcw.edu/article/965928293.html2. Humes, LE, Joellenbeck, LM, Durch, JS (2006). Noise andmilitary service: Implications for hearing loss and tinnitus.Washington D.C.: The National Academies Press.3. Deschler, DG, (2008). Pathogenesis, diagnosis and treatmentof tinnitus. Retrieved December 2008, from Up-to-date Wesite: http://utdol.com/online/tinnitus/treatment.html4. Lite, J. (2007). Iraq & Afghanistan war vets suffer from hearingloss, tinnitus. The New York Daily News, November 11.5. American Hearing Research Foundation (2008). Noise-inducedhearing loss. Retrieved March 16, 2009, from American HearingResearch Foundation Website: http://www.americanhearing.org/disorders/hearing/noise_induced.html6. Axelsson, A; Prasher, D. (2000). Tinnitus induced by occupationaland leisure noise. Noise & Health:A QuarterlyInter-disciplinary International Journal; 2(8): 47-54.7. Reimer Hyperbaric of Canada (1998). Hyperbaric oxygen inthe treatment of sudden deafness, acute tinnitus and acuteacoustic trauma. Retrieved March, 5 2009, from Reimer Hyperbaricof Canada Website: http://www.reimerhbo.com/tinnitus.html8. Oeken, Jens. (1998). Distortion product otoacoustic emissionsin acute acoustic trauma. Noise & Health: A Quarterly InterdisciplinaryInternational Journal; 2(1): 56-66.9. Keate, B. (2008). Hyperbaric oxygen therapy for tinnitus.Retrieved March 16, 2009, from Arches Tinnitus FormulasWebsite: http://www.tinnitusformula.com/infocenter/articles/treatments/hyperbaric.aspx10. Naval Safety Center (2008). Acquisition safety – noise controlaboard ships. Retrieved December 2, 2008, from Navy SafetyCenter Website: http://www.safetycenter.navy.mil/acquisition/noise/index.aspx11. National Institute of Health (2008). Noise-induced hearing lossRetrieved March 16, 2009, fromNational Institute on Deafnessand Other Communication Disorders Website:http://www.nidcd.nih.gov/health/hearing/noise.aspx12. Whittle, R. (2006). Hearing loss on rise among troops: Armyplans to reduce military audiologist, add civilians. The DallasMorning News, March 5, p.A10.13. MSNBC (2008). Hearing loss is silent epidemic in U.S. Troops:Soldiers coming home with permanent hearing damage andringing in ears. Retrieved December 2, 2008, from MSNBCWebsite: http://www.msnbc.msn.com/id/23523729/.14. Rosen, E.J.; Vrabec, J.T.; Quinn, F.B.. (2001). Noise-inducedhearing loss. Grand Rounds Presentation, UTMB, Dept. of Otolaryngology;January 2001.15. Bennett, MH; Kertesz, T; Yeung, P. (2005). Hyperbaric oxygentherapy for idiopathic sudden sensorineural hearing loss and tinnitus:A systematic review of randomized controlled trials. TheJournal of Laryngology and Otology; 119(10): 791-798.16. Bennett, MH; Kertesz, T; Yeung, P. (2007). Hyperbaric oxygentherapy for idiopathic sudden sensorineural hearing loss and tinnitus.Cochrane Database of Systematic Reviews; Issue 1. Art.17. Rabinowitz, PM. (2000). Noise-induced hearing loss. RetrievedMarch 16, 2009, from The American Family Physician Website:http://www.aafp.org/afp/20000501/2749.html18. Bredenkamp, JK; Schoenfield. (2008). Noise-induced hearingloss and its prevention. Retreived March 16, 2009, from MedicineNet Website: http://www.medicinenet.com/noise_induced_hearing_loss_and_its_prevention/article.html19. Daniilidis, IC. (2004). Evaluation of various therapeuticschemes in the treatment of tinnitus due to acute acoustictrauma. Kulak Burun Bogaz Ihtis Derg; 12(5-6): 107-114.Tinnitus, a Military Epidemic:Is Hyperbaric Oxygen Therapy the Answer?41
20. Zalin, H. (1971). Noise-induced hearing loss: Session I:Differential Diagnosis. Section of Occupational Medicinewith Section of Otology: Joint Meeting No.2; 64: 187-190.21. The ASHA Leader. Hearing loss rises among U.S. Soldiersin Iraq. The ASHA Leader 2006; 11(4):5, 19.22. Hearing Review, The Insider (2006). Military Vets sufferdramatic increase in tinnitus and other hearing damage. RetrievedDecember 2, 2008, from Hearing Review Website:http://www.hearingreview.com/insider/2006-10-12_1861.aspx23. U.S. Army Center for Health Promotion and PreventativeMedicine (2003). Just the facts…Tinnitus and noise-inducedhearing loss. Retrieved March 16, 2009, from The USACHPPM Website:http://chppm-www.apgea.army.mil/documents/FACT/51-003-1103.pdf24. Ritenour, AE; Wickley, A; Ritenour, JS; Kriete, BR; Brian,R; Blackbourne, LH; Holcomb, JB; Wade. (2008). TympanicMembrane perforation and hearing loss from blastoverpressure in Operation Enduring Freedom and OperationIraqi Freedom wounded. The Journal of Trauma Injury, Infectionand Critical Care; 64(2): S174-S178.25. Narozny, W; Sicko, Z; Kuczkowski, J; Stankiewwicz, C;Przewozny, T. (2003). Usefulness of hyperbaric oxygentherapy in patients with sensorineural acute and chronic tinnitus.International Congress Series; 1240: 277-286.26. Kau, RJ; Sendther-Gress, K; Ganzer, U; Arnold, W. (1997).Effectiveness of hyperbaric oxygen therapy in patients withacute and chronic cochlear disorders. ORL; 59: 79-83.27. Schumann, K; Lamm, K; Hettich, M. (1990). Effect and effectivenessof hyperbaric oxygen therapy in chronic hearingdisorders. HNO; 38(11): 408-411.28. Bohmer, D. (1997). Treating tinnitus with hyperbaricoxygenation. International Tinnitus Journal; 3(2): 137-140.29. Mathur, NN; Prince, M. (2006). Hyperbaric oxygen. RetrievedMarch 5, 2009 from eMedicine Website:http://emedicine.med scape.com/article/853951-overview.30. Lamm, K; Lamm, H; Arnold, W. (1998). Effect of hyperbaricoxygen therapy in comparison to conventional orplacebo therapy or not treatment in idiopathic sudden hearingloss, acoustic trauma, noise-induced hearing loss andtinnitus: A literature Survey. Adv Otorhinolaryngology; 54:86-99.31. Porubsky, C; Stiegler, P; Matzi, V; Lipp, C; Kontaxis, A;Klemen, H; Walch, C; Smolle-Juttner, F. (2007). Hyperbaricoxygen in tinnitus: Influence of psychological factors ontreatment results? ORL; 69: 107-112.32. Biesinger, E; Heiden, C; Greimel, V; Lendle, T; Hoing, R;Albegger, K. (1998). Strategien in der ambulanten behandlung des tinnitus. ORL; 46: 157-169.33. Delb, W; Muth, CM; Hoppe, U; Iro, H. (1999). Outcome ofhyperbaric oxygen therapy in therapy refractory tinnitus.HNO; 47(12): 1038-1045.34. Lamm, K. (2003). Hyperbaric oxygen therapy for the treatmentof acute cochlear disorders and tinnitus. ORL; 65: 315-316.35. Lamm, H. Der einfluss der hyperbaren sauerstofftherapie aufden tinnitus und den horverlust bei akuten und chronischen innenohrschaden.36. Stiegler, P; Matzi, V; Lipp, C; Kontaxis, A; Klemen, H;Walch, C; Smolle-Juttner, F. (2006). Hyperbaric oxygen(HBO 2 ) in tinnitus: Influence of psychological factors ontreatment results? UHM; 33(6): 429-437.37. Dundar, K; Gumus, T; Ay, H; Yetiser, S; Ertugrul, E. (2007).Effectiveness of hyperbaric oxygen on sudden sensorineuralhearing loss: Prospective clinical research. The Journal of Otolaryngology;36(1): 32-37.38. Tan, J; Tange, RA; Dreschler, WA; Kleij, A; Tromp, EC.(1999). Long-term effect of hyperbaric oxygenation treatmenton chronic distressing tinnitus. Scand Audiolology; 28: 91-96.42Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
ADDITIONAL REFERENCESHoffmann, G; Bohmer, D; Desloovere, C. (1995). Hyperbaricoxygenation as a treatment of chronic forms of inner ear hearingloss and tinnitus. In: Li W-R Cramer F. eds. Proceedings of theEleventh International Congress on Hyperbaric Medicine. BestPublishing; 141-145.Hoffmann, G; Bohmer, D; Desloovere, C. (1995). Hyperbaricoxygenation as a treatment for sudden deafness and acute tinnitus.In: Li W-R. Cramer F. eds. Proceedings of the Eleventh InternationalCongress on Hyperbaric Medicine. Best Publishing;146-51.Schwab, B; Flunkert, C; Heermann, R; Lenarz, T. (1998). HBOin the therapy of cochlear dysfunctions – First results of a randomizedstudy. In: Gennser M. ed EUBS Diving and HyperbaricMedicine: Controlled manuscripts of XXIV Annual ScientificMeeting of the European Underwater and Baromedical Society.Stockholm: EUBS; 40-42.Pilgramm, M; Lamm, H; Schumann, K. (1985). Hyperbaric oxygentherapy in sudden deafness. Laryngologie, Rhinologie,Otologie; 64(7): 351-354.Schumann, K; Lamm, K. Hetlich, (1990). Zur Wirksamheit derhyperbaren Saurestofftherapie bei alten Horstorungen. Berichtuber 557 Fale aus dem Jahre 1989, HNO; 38: 408-411.LCDR Thomas Baldwin is the Senior Medical Officer at <strong>Special</strong> Boat Team Twenty-Two,Stennis Space Center, Mississippi. He is a graduate of the University of Texas Health ScienceCenter at San Antonio Medical School and also holds a Master’s Degree in PhysicalTherapy from the U.S. Army-Baylor University program at Fort Sam Houston.Tinnitus, a Military Epidemic:Is Hyperbaric Oxygen Therapy the Answer?43
Brain Natriuretic Peptide Levels in SixBasic Underwater Demolitions/SEALRecruits Presenting with SwimmingInduced Pulmonary Edema (SIPE)LCDR Damon Shearer, DO (DMO/UMO); CDR Richard Mahon,MD (DMO/UMO)ABSTRACTSwimming induced pulmonary edema (SIPE) is associated with both SCUBA diving and strenuous surfaceswimming; however, the majority of reported cases and clinically observed cases tend to occur during or afteraggressive surface swimming. 1 Capillary stress failure appears to be central to the pathophysiology of this disorder.Regional pulmonary capillaries are exposed to relatively high pressures secondary to increased vascularvolume, elevation of pulmonary vascular resistance, and regional differences in perfusion secondary to forces ofgravity and high cardiac output.Acute pulmonary edema can be classified as either cardiogenic or noncardiogenic or both. Cardiogenicpulmonary edema occurs when the pulmonary capillary hydrostatic pressure exceeds plasma oncotic pressure.Noncardiogenic pulmonary edema occurs when pulmonary capillary permeability is increased. Given the pathophysiologynoted above, SIPE can be described as a cardiogenic pulmonary edema, at least in part, since an increasedtransalveolar pressure gradient has been implicated in the pathogenesis of SIPE. 2Brain natriuretic peptide (BNP) is used in the clinical setting to differentiate cardiac from pulmonarysources of dyspnea, specifically to diagnose cardiogenic pulmonary edema. 3,4 During clinical management, BNPlevels were drawn on six BUD/S recruits simultaneously presenting with pulmonary complaints consistent withSIPE, after an extended surface bay swim. This paper analyzes that data after de-identification and reviews thepathophysiology and clinical management of SIPE.LEARNING OBJECTIVES1. Describe the signs and symptoms of SIPE.2. Describe the immediate care and treatment of SIPE.3. Demonstrate understanding of the fundamental pathophysiology of SIPE.BACKGROUNDThe pathophysiology of SIPE is multifactorial.Numerous physiologic, environmental, and behavioralfactors have been implicated. However, capillary stressfailure appears to be central to the pathophysiology ofthis condition. The pulmonary capillary measures approximatelytwo to six microns in diameter. This structurehas the difficult task of facilitating gas transferbetween the alveoli and pulmonary vasculature whilstmaintaining structural integrity. Capillary stress failureoccurs when the capillary is exposed to relativelyhigh transmural pressures.Intense exercise is capable of generating theseelevated pressures. Stress fracture of the pulmonarycapillaries has been documented with electron microscopyin equine models when exposed to capillarytransmural pressures of 75-100mmHg. Additionally,necropsy of equine athletes has demonstrated evidenceof pulmonary capillary stress failure. 5 Lower pressuresare required to cause fracture in canines and rabbits(40mmHg) and likely in man. 6Elite human athletes are capable of generatingmean pulmonary artery pressures of 37mmHg. Reeves44Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
et al. demonstrated that both right atrial and wedge pressuresrise with heavy exercise in normal men with somewedge pressures measured greater than 30mmHg. Theysurmised that these high cardiac filling pressures “couldcontribute both to elevated pulmonary arterial pressureand to increased filtration of water into the lung.” 7Bernheim et al. demonstrated exercise induced increasesin systolic right ventricular to atrial pressuregradients (RVPGs) in 39 subjects. Of note, individualssusceptible to high-altitude pulmonary edema (HAPE)demonstrate greater increases in RVPG from baselinethan normal controls. 8Bronchoalveolar lavage (BAL) findings in suchathletes indicate elevated levels of protein and red bloodcells. Intense exercise impairs the integrity of theblood-gas barrier in elite athletes. Vigorous exercisenot only may result in increased RBCs and total proteinon BAL, but also a lack of pro-inflammatory markers.This supports the hypothesis that the insult to the barrieris mechanical. 9 Ludwig et al., demonstrated BAL evidencehigh molecular weight protein edema fluid andred blood cells consistent with capillary fracture, in fiveBUD/S trainees diagnosed with SIPE. 10The factors that lead to elevated pulmonary arterypressures and capillary fracture are both physicaland physiological. Partial immersion, gravity dependentflow in the pulmonary vasculature, and extreme exertioncombine to elevate pulmonary artery pressuresbeyond physiologic norms and lead to failure of the pulmonarycapillary.Head above water immersion has both cardiovascularand pulmonary effects. Increased venous returnleads to central pooling of blood, which therebyincreases cardiac preload. 11 Additionally, immersion independentlyleads to elevated pulmonary artery pressures.Arborelius et al., described a 700cc increase inthoracic blood volume and a 32% increase in cardiacoutput along with elevations of mean pulmonary arterypressure associated with head above water immersion. 12Exercise with head out immersion leads to significantlygreater stroke volume and cardiac output when comparedwith exercise on land. 13 Additionally, immersionalone increases sympathetic activity, thereby contributingto additional peripheral vasoconstriction and centralpooling of blood volume.Water temperature may have a role in SIPE aswell. Immersion in cold water is known to cause peripheralvasoconstriction. Conceivably, this could contributeto increased vascular resistance (afterload), aswell as contribute to the central pooling of blood (preload).Cold-water immersion has been demonstrated toincrease central vascular volume and forearm vascularresistance and cold showers have been documented toincrease pulmonary vascular resistance and increasecardiac output by as much as 59-100%. 14,15The pulmonary effects of immersion are alsoprominent, such as decreased vital capacity, decreasedfunctional residual capacity, and increased closing volume.These effects induce a non-uniform pulmonaryvasoconstriction. Capillaries not protected by arterialconstriction experience high pressures and are prone tomicro-fracture. Negative pressure breathing of head outimmersion results in an alveolar pressure less than mouthpressure. This produces hydrostatic forces that favor afluid shift from the vasculature to the alveoli. 16There is a 65% increase in respiratory work associatedwith immersion to the xiphoid process comparedwith immersion to the neck. 17 Extreme effort, inducedby both intense swimming and this increased work ofbreathing, could increase peak airway pressures and resultin increased capillary permeability. 18Gravity dependent flow in the pulmonary vasculatureis an additional contributing factor to SIPE. Thereis a 200% increase in perfusion in the gravity-dependentlung, while swimming in the lateral decubitus position.This combination of cardiovascular and pulmonaryeffects can increase capillary transmural pressurevia a decrease in the amount of capillary bed availablefor thoracic blood to flow through. Additional contributingfactors have been proposed. Over-hydrationcould reasonably be presumed to increase central bloodvolume and increase preload, thus predisposing to elevatedpulmonary pressures and capillary fracture.Weiler-Ravell et al. described six cases of SIPE occurringin Israeli soldiers after the individuals drank fiveliters of water in the two hours preceding the exercise.His team deduced that over-hydration was a contributingfactor in these cases. 19 Finally, constrictive wet suits havealso been implicated as a causative agent in at least onecase report of SIPE. 2 Presumably, the causality in thiscase would be similar to the effects of submersion, resultingin increased work of breathing. Of note, there isalso evidence that tight-fitting wetsuits likely do not playa significant role in SIPE, as evidenced by the lack of significantinfluence on pulmonary function studies. 20Brain natriuretic peptide (BNP) is secreted bymyocardial ventricular cells, mainly cardiomyocytes.BNP is known to have natriuretic, diuretic, and vasorelaxantproperties. It plays an important role in fluidhomeostasis and blood pressure. Elevations in BNP reflectmyocardial wall stress and are often in response tohigh ventricular filling pressures. Numerous studies haveshown elevations in plasma BNP levels in left ventricularsystolic and diastolic dysfunction, left ventricular hypertrophy,and right ventricular dysfunction in pulmonaryhypertension, cardiomyopathy, acute coronary syndromes,and pulmonary embolism. 21-23 Additionally BNPcorrelates with pulmonary artery pressures. 24BNP levels have been utilized clinically in differentiatingcardiac from non-cardiac causes of dyspnea.Berdague et al. demonstrated that NT-proBNP is a sensitiveand specific means of distinguishing pulmonary fromcardiac causes of dyspnea in elderly patients. Theydemonstrated 86% sensitivity and 71% specificity withBrain Natriuretic Peptide Levels In Six Basic Underwater Demolitions/SEAL Recruits Presenting withSwimming Induced Pulmonary Edema (SIPE)45
overall accuracy of 80% for cardiac dyspnea. 4 Additionally,brain natriuretic peptide has a sensitivity of82% and specificity of 92% for identification of cardiaccauses of syncope, when a cut-off value of40pg/ml is used. 25It is of note, that resting BNP concentrationsare not elevated in physiologically hypertrophiedhearts of endurance athletes. 26CLINICAL CONSIDERATIONSTypical symptoms of SIPE include dyspnea,cough which may be productive of pink or white frothysputum, chest pain or tightness, and hemoptysis. Uponinitial symptom onset, patients may exhibit confusionsecondary to hypoxemia. Typical signs include laboredbreathing, tachypnea, and hypoxemia.SIPE can be confidently diagnosed in any patientpresenting with the above noted signs and symptomsoccurring during or immediately after aswimming event, in association with a demonstrablechest radiograph abnormality. The treatment of SIPEis primarily supportive. It is imperative to deliver supplementaloxygen to the patient, titrated to maintainnormal oxygen saturation. In the military setting,Corpsmen or First Responders covering training evolutionswith an inherent risk for the development ofSIPE, should be equipped with pulse oximetry, supplementaloxygen, and inhaled beta agonists. Theyshould be trained in Basic Life Support (BLS/CPR).Prompt evaluation by a physician with access to radiography,Advanced Cardiac Life Support (ACLS) capability,and laboratory support is important formoderate to severe cases of SIPE. However, there is noevidence in the literature that ACLS has been necessaryin the treatment of SIPE.Clinical experience has shown long acting inhaledbeta agonists, such as salmeterol, to be of utility.This agent accelerates resolution via improved alveolarfluid clearance and also provides symptomatic reliefto the patient. 16 Diuretics generally are not necessaryin the treatment of SIPE. 27Occasionally patients with SIPE will requireinpatient admission, though frequently patients can bedischarged directly from the emergency departmentafter a period of treatment and observation, once oxygensaturation has returned to baseline on room air.A hallmark of SIPE is rapid resolution. Frequently,symptoms resolve within 12 to 24 hours withchest radiographs demonstrating resolution within 24to 48 hours. Frequently, patients can be returned to fullduty within 72 hours.Historically, there is no evidence that individualswho suffer from an episode of SIPE are predisposedto have additional occurrences. Typically,BUDS candidates who suffer from SIPE have graduationrates commensurate with their fellow students whohave not had a SIPE event. In fact, testing in dry conditionsof individuals previously diagnosed with SIPErevealed that they do not have abnormal pulmonaryfunction tests, abnormal exercise capacity, or abnormalpulmonary arterial pressure response to hypoxemia. 10There are no definite predisposing factors forSIPE. However, Shupak et al. did demonstrate thatbaseline FVC, FEV1, and FEF were 25 to 75% lowerin twenty-one individuals diagnosed with SIPE. Thuslower initial lung volumes and flows may be predictiveof vulnerability to SIPE. 28METHODSSix BUD/S recruits presented to the ED withpulmonary complaints after a surface bay swim. Thediagnosis of SIPE was made on all six individualsbased on presenting complaint, chest radiograph findings,and physical examination. BNP levels weredrawn on these individuals as part of the clinical evaluationof dyspnea, cough, and pulmonary edema in theemergency department setting. Transport time to theED was approximately thirty to forty-five minutes fromsymptom onset. Labs were drawn within two hours ofswim termination.The case definition of SIPE for the purposes ofthis report is hypoxemia occurring during or immediatelyafter a swimming event, a demonstrable chest radiographabnormality, improvement or resolution ofsaid abnormality in less than 48 hours, absence of evidenceof pulmonary infection, and absence of a historyof breathing against a closed glottis or aspiration ofwater.RESULTS AND PATIENT DATASee Table 1 on page 47ResultsBNP levels ranged from 6.3pg/ml to39.7pg/ml. The average was 26.55pg/ml. All valuesfell within the NMCSD laboratory range of normal, 1-100pg/ml. All six individuals demonstrated abnormalchest radiographs with both interstitial and airspaceprocesses. The cardiac and mediastinal silhouetteswere normal in all cases. Three patients were admittedto the internal medicine service. One patient was admittedto the ICU. Two patients were discharged totheir command. The patients admitted to the hospitalstayed an average of twenty-four hours. Their treatmentconsisted of supplemental oxygen and beta-agonists(alveolar fluid clearance). All were returned tofull duty within seventy-two hours. Two of the six individualswent on to complete BUD/S training and becameSEALs. This graduation rate of 33% is consistentwith normal rates in individuals attending BUD/S.This likely indicates that a single episode of SIPE doesnot cause long-term decrements in physical performancefrom a cardiovascular standpoint.46Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
TYPICAL CHEST RADIOGRAPH FINDINGS IN SIPE: Mixed interstitial & airspace process,prominent pulmonary vasculature, Kerley B-lines, normal cardiac, and mediastinal silhouettes.Table 1Brain Natriuretic Peptide Levels In Six Basic Underwater Demolitions/SEAL Recruits Presenting withSwimming Induced Pulmonary Edema (SIPE)47
Discussion of ResultsIt is well known that BUD/S training is extremelyarduous. The extreme physical and psychologicaldemands of the training, in concert with theenvironment in which the training is conducted, frequentlyresults in illness and injury. Pulmonary infectionsare relatively common in this population.Therefore, utilization of BNP as a method for differentiatingthe source of dyspnea in these BUD/Strainees was prudent. Our experience indicates thatplasma BNP is not elevated in SIPE. However, thesefindings may be limited by a delay of up to two hoursfrom symptom onset to blood draw. There is currentlylittle data in the literature describing the amount ofBNP reserve in the ventricular cells. The time coursefor BNP elevations to occur is not incredibly well defined.BNP is significantly elevated above baselinewithin one hour after ventricular septal defect repair inchildrenand BNP rapidly rises (within hours) in the settingof acute myocardial infarction. 29,30 Serial BNPlevels were not drawn in these patients, thus it is theoreticallypossible that BNP levels may have elevatedafter initial diagnostic work-up was performed in theemergency room. This seems unlikely however, in thatBNP levels are thought to increase within a very shorttime period of the development of clinically significantpulmonary edema.Discussion of PatientsThese six patients all experienced symptomsconsistent with SIPE at various points or timeframesduring the same surface bay swim. These swims wereperformed in the lateral decubitus position. Water conditionswere reported as “cold and rough.”These patients share several similarities inpresentation and symptoms, physical examination findings,and laboratory abnormalities. All six patients presentedwith various symptoms of shortness of breath,cough, chest pain/tightness, and hemoptysis. Severalof the patients were noted to be hypoxemic by pulseoximetry in the field. This hypoxia is common inSIPE, as noted in two of three patients reported on byLund et al. and as noted by Adir et al. 16,31 Additionally,mild hypothermia was commonly noted.Several of the individuals’ laboratory studiesexhibit a mild anemia. This slight anemia is commonin BUD/S trainees. One of the three SIPE patients reportedon by Lund et al., exhibited this phenomenon. 16BUD/S trainees admitted to NMCSD for other diagnosessuch as cellulitis and pneumonia, frequentlydemonstrate a mild anemia. Though not specificallyaddressed in the literature, this common finding inBUD/S trainees is likely due to the extreme daily physicalstress of this course of instruction. The anemia isnot likely related to the development of SIPE.CONCLUSIONSwimming induced pulmonary edema is ofclinical significance, particularly in the military, andmost notably in <strong>Special</strong> <strong>Operations</strong> trainees and recruits.It is a clinical entity noteworthy for its rapidonset, rapid recovery, and return to full duty. The rapiddiagnosis of this condition by medical personnel coveringstrenuous surface swims in the Naval <strong>Special</strong>Warfare community is critical to avoid serious morbidityand mortality. BNP levels are not elevated inswimming induced pulmonary edema, rendering thislaboratory test of little value in the clinical evaluationof pulmonary edema associated with swimming. Furtherstudy of the pathophysiology, etiology, and treatmentof swimming induced pulmonary edema isrequired.REFERENCES1. Pons M, Blickenstorfer D, Oechslin E, et al. (1995). Pulmonaryedema in healthy persons during scuba diving andswimming. Eur Respir J;8:762-767.2. Slade JB, Hattori T, Ray CS, Bove AA, Cianci P. (2001).Pulmonary edema associated with scuba diving. Chest;Nov;120:1686-1694.3. Siebert U. (2006). Cost-effectiveness of using N-terminal prbrainnatriuretic peptide to guide the diagnostic assessmentand management of dyspneic patients in the emergency department.Am J Cardiol; Sep; 98(6):800-5.4. Berdague P. (2006). Use of N-terminal prohormone brainnatriuretic peptide assay for etiologic diagnosis of acute dyspneain elderly patients. Am Heart J.; Mar; 151(3): 690-8.5. Birks EK, Mathieu-Costello O, Fu Z, Tyler WS, West JB.(1997). Very high pressures are required to cause stress failureof pulmonary capillaries in Thoroughbred racehorses. J.Appl Physiol. 82(5): 1584 – 1592.6. West JB, Tsukimoto K, Mathieu-Costello O, Prediletto R.(1991). Stress failure in pulmonary capillaries. J Appl Physiol.Vol 70, Issue 4 1731-1742.7. Reeves JT, Groves BM, Cymerman A, Sutton JR, WagnerPD, Turkevich D, Houston CS. (1990). Operation Everest:Cardiac filling pressures during cycle exerise at sea level.Respir Physiol. May-Jun;80(2-3):147-54.8. Bernheim AM, Kiencke S, Fischler M, et al. (2007). Acutechanges in pulmonary artery pressures due to exercise andexposure to high altitude do not cause left ventricular diastolicdysfunction. Chest; 132:380-387.9. Hopkins SR, Schoene RB, Henderson WR, Spragg RG, MartinTR, West JB. (1997). Intense exercise impairs the integrityof the pulmonary blood-gas barrier in elite athletes. AmJ Respir Crit Care Med; 155:1090-4.10. Ludwig B, Mahon RT, Parrish JS. Pulmonary edema incombat swimmers: Clinical and bronchoalveolar lavagedescription demonstrating stress failure of the pulmonarycapillaries. Undersea and Hyperbaric Medicine Vol 31Number 3: C-42,318.48Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
11. Norsk P, Bonde-Petersen F, Warberg J. (1986). Central venouspressure and plasma arginine vasopressin in man during waterimmersion combined with changes in blood volume. Eur JAppl Physiol;54:608-16.12. Arborelius M Jr, Ballidin UI, Lilja B, Lundgren CE. (1972).Hemodynamic changes in man during immersion with thehead above water. Aerosp Med;43(6):592-8.13. Sheldahl LM, Tristani FE, Clifford PS, Hughes CV,Sobocinski KA, Morris RD. (1987). Effect of head-outwater immersion on cardiorespiratory response to dynamicexercise. J Am Coll Cardiol; 10(6):1254-8.14. Pons M, Blickenstorfer D, Oechslin E, et al. (1995). Pulmonaryedema in healthy persons during scuba-diving and swimming.Eur Respit J;8:762-767.15. Keatinge WR, McIlroy MB, Goldfien A. (1964). Cardiovascularresponses to ice cold showers. J Appl Physiol; 19:145-1150.16. Lund KL, Mahon RT, Tanen DA, Bakhda S. (2003). Swimming-inducedpulmonary edema. Ann Emerg Med; 41:251-256.17. Hong, S. K., P. Cerretelli, J. C. Cruz, and H. Rahn. (1969).Mechanics of respiration during submersion in water. J. Appl.Physiol; 27: 535-538.18. Parker JC, Townsley MI, Rippe B, et al. (1984). Increasedmicrovascular permeability in dog lungs due to high peakairway pressures. J Appl Physiol; 57:1809-1816.19. Weiler-Ravell D, Shupak A, Goldenberg I, Halpern P,Shoshani O, Hirschhorn G, Margulis A. (1995). Pulmonaryedema and haemoptysis induced by strenuous swimming.BMJ;:311:362.20. Mahon RT, Norton D, Krizek S, et al. (2002). Effects of wetsuitson pulmonary function studies in Basic UnderwaterDemolition/SEAL (BUD/S) trainees in the <strong>United</strong> <strong>States</strong>Navy. Abstract presented at 35th Annual Undersea and HyperbaricMedicine Society Scientific Meeting; June 28-30;La Jolla, CA.21. Krishnaswamy P, Lubien E, Clopton P, Koon J, Kazanegra R,Wanner E, Gardetto N, Garcia A, DeMaria A, Maisel AS.(2001). Utility of B-natriuretic peptide levels in identifyingpatients with left ventricular systolic or diastolic dysfunction.Am J Med; Sep; 111(4):274-9.22. Yamamoto K, Burnett JC, Jougasaki M, Nishimura RA, BaileyKR, Saito Y, Nakao K, Redfiled MM. (1996). Superiorityof brain natriuretic peptide as a hormonal marker ofventricular systolic and diastolic dysfunction and ventricularhypertrophy. Hypertension. Dec; 28(6):988-994.23. Nagaya N, Nishikimi T, Okano Y, Uematsu M, Satoh T, KyotaniS, Kuribayashi S, Hamada S. (1998). Plasma brain natriureticpeptide levels increase in proportion to the extent ofright ventricular dysfunction in pulmonary hypertension. JAm Coll Cardiol. Jan;31(1):202-8.24. Maisel AS, Krishnaswamy P, Nowak RM, et al. (2002).Rapid measurement of B-type natriuretic peptide in theemergency diagnosis of heart failure. N Engl J Med;347:161.25. Tanimoto K, et al. (2004). Usefulness of brain natriureticpeptide as a marker for separating cardiac and noncardiaccauses of syncope. Am J Cardiol. Jan; 93(2).26. Scharhag J, et al. (2005). Independent elevations of N-terminalpro-brain natriuretic peptide and cardiac troponins inendurance athletes after prolonged strenuous exercise. AmHeart J. Dec; 150(6).27. Yoder JA, Viera AJ. (2004). Management of swimming-inducedPulmonary Edema. American Family Physician. 3/1/2004, Vol. 69Issue 5, p1046-1049.28. Shupak A, Weiler-Ravell D, Adir Y, Daskalovic YI, RamonY, Kerem D. (2000). Pulmonary edema induced by strenuousswimming: A field study. Respir Physiol. Jun;121(1):25-31.29. Mainwaring RD, Parise C, Wright SB, Juris AL, Achtel RA,Fallah H. (2007). Brain natriuretic peptide levels before andafter ventricular septal defect repair. Ann Thorac Surg.Dec;84(6):2066-9.30. Mukoyama M, Nakao K, Obata K, Jougasaki M, YoshimuraM, Morita E, Hosoda K, Suga S, Ogawa Y, Yasue H, et al.(1991). Augmented secretion of brain natriuretic peptide inacute myocardial infarction. Biochem Biophys Res Commun.Oct 15;180(1):431-6.31. Adir Y, Shupack A, Gil A, Peled N, Keynan Y, DomachevskyL, Weiler-Ravell D. (2004). Swimming-induced pulmonaryedema clinical presentation and serial lung function.Chest. Aug; 126(2).Brain Natriuretic Peptide Levels In Six Basic Underwater Demolitions/SEAL Recruits Presenting withSwimming Induced Pulmonary Edema (SIPE)49
LCDR Shearer, MD served as the Medical Department Head for Mobile Diving and SalvageUnit TWO and the Senior Medical Officer of Naval <strong>Special</strong> Warfare Group FOURwhile on active duty as a Diving Medical Officer. He is currently a PGY3 resident in radiologyat Loyola University Medical Center in Chicago and serving in the Navy Reserves.LCDR Shearer has spoken at the Royal Navy Institute of Naval Medicine, the Armed ForcesOperational Medicine Symposium, and Eastern Virginia Medical School on the subjects ofundersea and hyperbaric medicine.CDR Richard T. Mahon, MD is a Navy Undersea Medical Officer and a board certified specialistin pulmonology and critical care medicine. He graduated from the Navy Undersea Medical Institutein 2004 and was subsequently stationed as the Head of the Undersea Medical Departmentat the Naval Medical Research Center in Bethesda, MD.50Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
ABSTRACTS FROM CURRENT LITERATUREMass Casualty in an Isolated Environment:Medical Response to a Submarine CollisionCDR Christopher John Jankosky, MC USNMilitary Medicine Vol 173, No 8 August 2008EXCERPTOn January 8, 2005, the U.S.S. SAN FRANCISCO (SSN 711), a nuclear-powered submarine, collided witha seamount in a remote Pacific Ocean location. The high-speed impact resulted in injuries to 90% of the crew.Subsequent emergency medical response is described as well as the 3-month physical and psychological morbidity.Recommendations for medical training, equipment, and policy for workers in isolated environments arediscussed.Terror-Inflicted Thermal Injury: A Retrospective Analysis of Burns in the Israeli-Palestinian Conflict Between the Years 1997 and 2003Haik, Josef MD; Tessone, Ariel MD; Givon, Adi BA; Liran, Alon MD; Winkler, Eyal MD; Mendes, David MD;Goldan, Oren MD; Bar-Meir, Eran MD; Regev, Eli MD; Orenstein, Arie MD; Peleg, Kobi PhD, MPHJournal of Trauma-Injury Infection & Critical Care. 61(6):1501-1505, December 2006.ABSTRACTBackground: Terror attacks have changed in the past decade, with a growing tendency toward explosives andsuicide bombings, which led to a rise in the incidence of thermal injuries among victims. The Israeli-Palestinianconflict of October 2000 marked a turning point when an organized terror campaign commenced. This articlepresents data of terror-associated burns from the Israeli National Trauma Registry (ITR) during the years1997 to September 2000 and October 2000 to 2003. Methods: We analyzed demographic and clinical characteristicsof 219 terror-related burn patients and 6,546 other burn patients admitted to hospitals in Israel between1997 and 2003. Data were obtained from the ITR. Results: Burns contributed about 9% of all terror relatedtrauma and about 5% of all other trauma (p < 0.0001). These percentages have not changed significantly beforeand after October 2000. Terror-related burns afflict Jewish males more than predicted by their percentage in thepopulation, whereas other burns afflict non-Jewish males more than predicted. Adults and young adults (15-59years) are the predominant group in terror-related burns (80%), whereas children younger than 15 years are thepredominant group in other burns (50%). Large burns (20% to 89% total body surface area) are more commonin terror casualties, with greater mortality (6.4% in terror-related versus 3.4% in others; p = 0.0258). Conclusion:Although the incidence of burns has risen because of an organized campaign, this change was noticeablein other trauma forms as well in similar proportions. Terror-related burns afflict a targeted population, and generallytake on a more severe course with greater mortality rates, thus requiring appropriate medical treatment.Abstracts From Current Literature51
Longer-Term Career Outcomes of Uniformed Services University of the HealthSciences Medical School Graduates: Classes of 1980-1989COL Daniel L. Cohen, USAF MC (Ret.); Steven J. Durning, MD; David Cruess, PhD; COL Richard MacDonald,MC USA (Ret.)Military Medicine May 2008, Vol 173, No 5ABSTRACTBackground: The Uniformed Services University of the Health Sciences (USUHS) F. Edward Hébert Schoolof Medicine exists to provide physicians who will become leaders in military medicine in both war and peacetime.Studying the career accomplishments of graduates who have reached or are near the end of their militarycareer is one way to assess how well USUHS is meeting this societal charge. Methods: Self-reported surveyof all 2,689 USUHS graduates since its inception in 1976. Data were collected with regard to residency completed,additional degrees obtained, leadership positions and rank obtained, deployment experience, and academicaffiliations. Results: Our survey resulted in a 59% response rate (712 of 1,199 respondents) for the matriculatingclasses of 1980-1989 and a 68% (1,822 of 2,689 respondents) total response rate for all graduates. Careeroutcome data were analyzed for graduates of the 1980-1989 classes in this article. For this cohort, the board certificationrate was 99%; 20% obtained additional degrees; 96% have worked as full-time clinicians; 14% receivedbelow-the-zone promotions; 51% had deployed for combat and 42% for humanitarian missions; and 57%continue to hold medical school faculty appointments. Discussion: Many accomplishments, to include highsustained board certification rates from a diverse array of specialties, broad deployment experience, achievementof high leadership responsibilities and senior rank, as well as important contributions to academic medicinewere achieved by these graduates. Our results support that USUHS is accomplishing its societal charge.Air Medical Evacuations of Soldiers Due to Oral-Facial Disease and Injuries,<strong>Operations</strong> Enduring Freedom/Iraqi FreedomLTC Timothy A. Mitchener, DC USA; Keith G. Hauret, MPT; Edward L. Hoedebecke, DVM; Salima Darakjy,MPH; Bruce H. Jones, MDMilitary Medicine, Volume 174, Number 4, April 2009 , pp. 376-381(6)ABSTRACTThis retrospective study was conducted to assess the nature and causes of serious oral-facial illnessesand injuries among U.S. Army personnel deployed to Iraq and Afghanistan in 2003 and 2004. Information forthis study came from the U.S. Air Force Transportation Regulating and <strong>Command</strong> & Control Evacuation Systemdatabase for medical evacuations (MEDEVACS) for 2003 to 2004. The study found 327 oral-facial MEDE-VACS out of Iraq (cumulative incidence: 11/10,000 Soldiers per year) and 47 out of Afghanistan (cumulativeincidence: 21/10,000 Soldiers per year), for a total of 374 MEDEVACS. Forty-two percent (n = 158) of all oralfacialMEDEVACS were due to diseases of the oral cavity, salivary glands, and jaw. Another 36% (n = 136) oforal-facial MEDEVACS were for battle injuries, primarily fractures of the mandible, caused by acts of war.Twenty-one percent (n = 80) of oral-facial MEDEVACS were due to nonbattle injuries, primarily fractures ofthe mandible, mainly caused by motor vehicle accidents and fighting.Prehospital Tourniquet Use in Operation Iraqi Freedom:Effect on Hemorrhage Control and OutcomesBeekley, Alec C. MD, FACS; Sebesta, James A. MD; Blackbourne, Lorne H. MD; Herbert, Garth S. MD; Kauvar,David S. MD; Baer, David G. PhD; Walters, Thomas J. PhD; Mullenix, Philip S. MD; Holcomb, John B.MC; Members of the 31st Combat Support Hospital Research GroupJournal of Trauma-Injury Infection & Critical Care. Advances in Combat Casualty Care: Clinical Outcomes fromthe War. 64(2) Supplement:S28-S37, February 2008.ABSTRACTBackground: Up to 9% of casualties killed in action during the Vietnam War died from exsanguination fromextremity injuries. Retrospective reviews of prehospital tourniquet use in World War II and by the Israeli DefenseForces revealed improvements in extremity hemorrhage control and very few adverse limb outcomes when52Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
tourniquet times are less than 6 hours. Hypothesis: We hypothesized that prehospital tourniquet use decreasedhemorrhage from extremity injuries and saved lives, and was not associated with a substantial increase in adverselimb outcomes. Methods: This was an institutional review board-approved, retrospective review of the 31stcombat support hospital for 1 year during Operation Iraqi Freedom. Inclusion criteria were any patient with atraumatic amputation, major extremity vascular injury, or documented prehospital tourniquet. Results: Among3,444 total admissions, 165 patients met inclusion criteria. Sixty-seven patients had prehospital tourniquets(TK); 98 patients had severe extremity injuries but no prehospital tourniquet (No TK). Extremity Acute InjuryScores were the same (3.5 TK vs. 3.4 No TK) in both groups. Differences (p < 0.05) were noted in the numbersof patients with arm injuries (16.2% TK vs. 30.6% No TK), injuries requiring vascular reconstruction (29.9% TKvs. 52.5% No TK), traumatic amputations (41.8% TK vs. 26.3% No TK), and in those patients with adequatebleeding control on arrival (83% TK vs. 60% No TK). Secondary amputation rates (4 (6.0%) TK vs. 9 (9.1%)No TK); and mortality (3 (4.4%) TK vs. 4 (4.1%) No TK) did not differ. Tourniquet use was not deemed responsiblefor subsequent amputation in severely mangled extremities. Analysis revealed that four of seven deathswere potentially preventable with functional prehospital tourniquet placement. Conclusions: Prehospital tourniquetuse was associated with improved hemorrhage control, particularly in the worse injured (Injury SeverityScore >15) subset of patients. Fifty-seven percent of the deaths might have been prevented by earlier tourniquetuse. There were no early adverse outcomes related to tourniquet use.Effect of Plasma and Red Blood Cell Transfusions on Survival in Patients WithCombat Related Traumatic InjuriesSpinella, Philip C. MD; Perkins, Jeremy G. MD; Grathwohl, Kurt W. MD; Beekley, Alec C. MD; Niles, SarahE. MD, MPH; McLaughlin, Daniel F. MD; Wade, Charles E. PhD; Holcomb, John B. MCJournal of Trauma-Injury Infection & Critical Care. Advances in Combat Casualty Care: Clinical Outcomesfrom the War. 64(2) Supplement:S69-S78, February 2008.ABSTRACTBackground: The amount and age of stored red blood cells (RBCs) are independent predictors of multiorgan failureand death in transfused critically ill patients. The independent effect of plasma transfusion on survival hasnot been evaluated. Our objective was to determine the independent effects of plasma and RBC transfusion onsurvival for patients with combat-related traumatic injuries receiving any blood products. Methods: We performeda retrospective review of 708 patients transfused at least one unit of a blood product at one combat supporthospital between November 2003 and December 2004. Admission vital signs, laboratory values, amountof blood products transfused in a 24-hour period, and Injury Severity Score (ISS) were analyzed by multivariatelogistic regression to determine independent associations with in-hospital mortality. Results: Seven hundredand eight of 3,287 (22%) patients admitted for traumatic injuries were transfused a blood product. Median ISSwas 14 (range, 9-25). In-hospital mortality was 12%. Survival was associated with admission Glasgow ComaScale score, SBP, temperature, hematocrit, base deficit, INR, amount of RBCs transfused, and massive transfusion.Each transfused FFP unit was independently associated with increased survival (OR: 1.17; 95% CI: [1.06-1.29]; p = 0.002); each transfused RBC unit was independently associated with decreased survival (OR: 0.86;[0.8-0.92]; p = 0.001). A subset analysis of patients (n = 567) without massive transfusion (1-9 RBC/FWB units)also revealed an independent association between each FFP unit and improved survival (OR: 1.22; 95% CI: [1.0-1.48]; p = 0.05) and between each RBC unit and decreased survival (OR: 0.77; [0.64-0.92]; p = 0.004). Conclusion:For trauma patients transfused at least one unit of a blood product, FFP and RBC amounts wereindependently associated with increased survival and decreased survival, respectively. Prospective studies areneeded to determine whether the early and increased use of plasma and decreased use of RBCs affect mortalityfor patients with traumatic injuries requiring transfusion.Abstracts From Current Literature53
The Emerging Role of Preventive Medicine in Health Diplomacy after the 2005Earthquake in PakistanMancuso, James D.; Price, E. Owen; West, David F.Military Medicine, Volume 173, Number 2, February 2008, pp. 113-118(6)ABSTRACTOn October 22, 2005, a preventive medicine team deployed with the 212th Mobile Army Surgical Hospitalto assist with earthquake relief efforts in Pakistani-controlled Kashmir. These efforts included core fieldpreventive medicine but quickly extended into other efforts. In collaboration with the host nation and other organizations,the preventive medicine team performed additional support for operations outside the U.S. compound,including water and sanitation assessments of camps for internally displaced persons, communicabledisease investigation and control, and vaccination programs. Preventive medicine personnel were vital to healthdiplomacy efforts in this operation, particularly because of security concerns that prevented other U.S. medicalassets from leaving the compound. Comparisons with the U.S. responses during other humanitarian operationsare made. Preventive medicine missions in health diplomacy will continue to increase. Training and collaborativerelationships with other government agencies, such as the U.S. Agency for International Development, andwith nongovernmental organizations should continue to be developed.Impact of Prolonged Exercise in the Heat and Carbohydrate Supplementation onPerformance of a Virtual Environment TaskBailey, Stephen P.; Holt, Craig; Pfluger, Kent C.; La Budde, Zina; Afergan, Daniel; Stripling, Roy; Miller, PaulC.; Hall, Eric E.Military Medicine, Volume 173, Number 2, February 2008 , pp. 187-192(6)ABSTRACTPurpose: The purpose of this investigation was to determine whether performance of a virtual environment(VE) task is influenced by exercise in the heat and carbohydrate supplementation. Methods: Ten males completedfour exercise trials to fatigue. During each trial, subjects cycled at a submaximal workload. Subjects exercisedin a normal environment (NORM) and in a hot environment on different occasions. During exercise,subjects drank 10 mL × kg −1 × hour −1 of body weight of a 6% carbohydrate beverage (CHO) or a placebo. Subjectscompleted a VE task before, during exercise, and after fatigue. Results: More failures occurred duringplacebo than CHO during exercise. The NORM CHO trial had the fewest failures at fatigue. More kills occurredduring exercise in the NORM CHO. Conclusions: Performance of a VE task was negatively influenced byprolonged exercise and heat stress. CHO supplementation may have a positive impact on performance of the VEtask following prolonged exercise.Emergency Medicine in Lebanon: Overview and ProspectJamil D. Bayram MD, MPHThe Journal of Emergency Medicine Volume 32, Issue 2, February 2007, Pages 217-222ABSTRACTEmergency Medicine, established in the <strong>United</strong> <strong>States</strong> as a specialty in 1979 and in Canada in 1980, isdrawing interest among countries throughout Europe, Asia, and the Middle East. Lebanon, located on the easterncoast of the Mediterranean Sea, like many other developing countries, struggles to advance its medical system.One of the main hurdles is the continuing violence and political turmoil. Attempts at health care systemrecovery have been met with a number of deep-seated structural problems. Data and references regarding emergencyhealthcare are rare. This article presents an overview of the current status of emergency medicine inLebanon as well as ongoing related activities over the past decade and the plans for future development.Parts of this article have been presented by the author at the Second Mediterranean Emergency MedicineCongress in Sitges, Spain, September 16, 2003. This article is the result of an extensive literature searchon health and emergency medicine in Lebanon. It presents an expanded analysis with a comprehensive bibliography.The author is emergency medicine trained at Stroger Hospital of Cook County (Chicago) and has hadthree years experience in Southern Lebanon as a Chairman of the emergency department at Hammoud Hospi-54Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
tal from July 1999 to June 2002. International Emergency Medicine is coordinated by Jeffrey Arnold, MD, ofTufts University School of Medicine and Baystate Medical Center, Springfield, Massachusetts.Recombinant Activated Coagulation Factor VII and Bleeding Trauma PatientsRizoli, Sandro B. MD, PhD; Nascimento, Bartolomeu Jr MD; Osman, Fahima MD; Netto, Fernando SpencerMD, PhD; Kiss, Alex PhD; Callum, Jeannie MD; Brenneman, Frederick D. MD; Tremblay, Lorraine MD, PhD;Tien, Homer C. MDJournal of Trauma-Injury Infection & Critical Care. 61(6):1419-1425, December 2006.ABSTRACTBackground: Recombinant activated coagulation factor VII (rFVIIa) is increasingly being administered to massivelybleeding trauma patients. rFVIIa has been shown to correct coagulopathy and to decrease transfusion requirements.However, there is no conclusive evidence to suggest that rFVIIa improves the survival of thesepatients. The purpose of this study was to determine whether or not rFVIIa has an effect on the in-hospital survivalof massively bleeding trauma patients. Methods: A retrospective cohort study was conducted from January1, 2000 to January 31, 2005, at a Level I trauma center in Toronto, Canada. Inclusion criteria includedtrauma patients requiring transfusion of 8 or more units of packed red cells within the first 12 hours of admission.The primary exposure of interest was the administration of rFVIIa. Primary outcome was a 24-hour survivaland secondary outcome was overall in-hospital survival. Results: There were 242 trauma patientsidentified who met inclusion criteria; 38 received rFVIIa. rFVIIa patients were younger, had more penetratinginjuries, and fewer head injuries. However, rFVIIa patients required more red cell transfusions initially, and weremore acidotic. Administering rFVIIa was associated with improved 24-hour survival, after adjusting for baselinedemographics and injury factors. The odds ratio (OR) for survival was 3.4 (1.2-9.8). Furthermore, therewas a strong trend toward increased overall in-hospital survival. The OR of in-hospital survival was 2.5 (0.8-7.6). Also, subgroup analysis of rFVIIa patients showed that 24-hour survivors required a slower initial rate ofred cell transfusion (4.5 vs. 2.9 units/hr, p = 0.002), had higher platelet counts (175 vs. 121 [x10-9/L], p = 0.05)and smaller base deficits (7.1 vs. 14.3, p = 0.001) compared with rFVIIa patients who died during the first 24hours. Conclusion: rFVIIa may be able to improve the early survival of massively bleeding trauma patients.However, surgical control of massive hemorrhage still has primacy, as rFVIIa did not appear efficacious if extremelyhigh red cell transfusion rates were required. Also, correction of acidosis and thrombocytopenia maybe important for rFVIIa efficacy. Prospective studies are required.Resolution and Severity in Decompression IllnessVann, Richard D.; Denoble, Petar J.; Howle, Laurens E.; Weber, Paul W.; Freiberger, John J.; Pieper, Carl F.Aviation, Space, and Environmental Medicine, Volume 80, Number 5, May 2009 , pp. 466-471(6)ABSTRACTWe review the terminology of decompression illness (DCI), investigations of residual symptoms of decompressionsickness (DCS), and application of survival analysis for investigating DCI severity and resolution.The Type 1 and Type 2 DCS classifications were introduced in 1960 for compressed air workers andadapted for diving and altitude exposure with modifications based on clinical judgment concerning severityand therapy. In practice, these proved ambiguous, leading to recommendations that manifestations, not cases,be classified. A subsequent approach assigned individual scores to manifestations and correlated total casescores with the presence of residual symptoms after therapy. The next step used logistic regression to find thestatistical association of manifestations to residual symptoms at a single point in time. Survival analysis, acommon statistical method in clinical trials and longitudinal epidemiological studies, is a logical extension oflogistic regression. The method applies to a continuum of resolution times, allows for time varying information,can manage cases lost to follow-up (censored), and has potential for investigating questions such as optimaltherapy and DCI severity. There are operational implications as well. Appropriate definitions of mild andserious manifestations are essential for computing probabilistic decompression procedures where severity determinesthe DCS probability that is acceptable. Application of survival analysis to DCI data would require morespecific case information than is commonly recorded.Abstracts From Current Literature55
Arterial Compliance in Divers Exposed to Repeated Hyperoxia UsingRebreather EquipmentGole, Yoann; Rossi, Pascal; Fontanari, Pierre; Gavarry, Olivier; Boussuges, AlainAviation, Space, and Environmental Medicine, Volume 80, Number 5, May 2009 , pp. 482-484(3)ABSTRACTBackground: Acute hyperoxic exposure is known to modify cardiovascular parameters like a decrease in cardiacoutput, arterial vasoconstriction, and autonomic nervous system changes. We hypothesized that repeatedhyperbaric hyperoxic exposures, as experienced by military oxygen divers, lead to long-term arterial alterations.Methods: Arterial blood pressure measurements and pulse wave velocity (PWV) recordings were performed duringbasal conditions in 15 elite military oxygen divers, and compared to 15 non-diver controls. The two groupswere matched appropriately for physical characteristics (age: 35 ± 5 yr, weight: 77 ± 8 kg, height: 177 ± 6 cm,body mass index: 24.6 ± 2.0 kg • m−2), and aerobic capacity (o2max: 52 ± 7 ml • min−1 • kg−1). Results: No significant difference was found in systolic blood pressure (120 ± 11mmHg), diastolic blood pressure (70 ± 8 mmHg), or pulse pressure (50 ± 7 mmHg). Furthermore, there was nosignificant difference in the carotid-femoral PWV (6.7 ± 0.9 m • s−1), the carotid-radial PWV (8.7 ± 1.7 m • s−1),or the carotid-pedal PWV (8.1 ± 1.1 m • s−1) between divers and controls. Conclusion: No difference in arterialcompliance was observed in physically well-trained military oxygen divers in comparison with matchedcontrols.Suicide among Discharged Psychiatric Inpatients in theDepartment of Veterans AffairsRani A. Desai, PhD; David Dausey, PhD; Robert A. Rosenheck, MDMilitary Medicine Vol 173, No 8 August 2008ABSTRACTObjective: The objective of this study was to explore correlates of the use of firearms to commit suicide. Methods:A national sample of psychiatric patients discharged from Department of Veterans Affairs medical centerswas followed from the time of discharge until December 1999. The study explores state-level measures as correlatesof overall suicide and suicide by firearm, controlling for individual sociodemographic characteristics andpsychiatric diagnosis. The outcomes of interest were completed suicide and suicide by firearm. Results: Patientswho were male, Caucasian, and who had a diagnosis of substance abuse or post-traumatic stress disorderwere significantly more likely to use a firearm than another means to commit suicide. Multivariable models indicatedthat Veterans living in states with lower rates of gun ownership, more restrictive gun laws, and highersocial capital were less likely to commit suicide with a firearm. Conclusions: Gun ownership rates, legislation,and levels of community cohesiveness are significantly associated with the likelihood of psychiatric patientscommitting suicide with a gun.56Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
Operation Sadbhavana: Winning Hearts and Minds in theLadakh Himalayan RegionLT COL Mudera P. Cariappa, Indian Army Medical Corps; Col Eugene V. Bonventre, USAF MC; MAJ GENBikash K. Mohanti, AVSM (Ret.)Military Medicine Vol 173, No 8 August 2008ABSTRACT“Sadbhavana” literally means “goodwill among people.” The Indian Army has evolved a military strategy ofwinning hearts and minds, with this being just a phase in the broader war on terror. We have focused on actionsto address the border regions of Ladakh in the Himalayas. The government of India strives against difficultconditions to provide essential services (including health care) to its population in an equitable manner; in remoteareas with fragile security and hamstrung provincial government systems, the Indian Army fills this role.The Army’s medical units have played a pivotal role in providing comprehensive health care as a keystone ofthe strategy. The endeavors of the doctors in uniform have succeeded in winning over an alienated population.A total of 163 medical camps were held in 2004, with attendance of 14,050 patients seeking medical attentionand 264 patients seeking dental attention; in 2005, 87 camps were conducted, with attendance totals of 7,562 and559, respectively. The Operation Sadbhavana military strategy has paid rich dividends in the form of changesin the perspective of the denizens of the remote and exotic locales of Ladakh. Planners must carefully analyzethe target audiences and the messages delivered to those audiences at the onset of such projects. Future effortswould be enhanced by attempts to quantify the effects of medical missions on the health of the population andon population attitudes toward the Indian Army and the central government.The Challenge of Controlling Lead and Silica Exposures from Firing Ranges in a<strong>Special</strong> <strong>Operations</strong> ForceMancuso, James D.; McCoy, John; Pelka, Bruce; Kahn, Patrice J.; Gaydos, Joel C.Military Medicine, Volume 173, Number 2, February 2008, pp. 182-186(5)ABSTRACTIn 2000, Soldiers from a <strong>Special</strong> <strong>Operations</strong> Force had airborne lead exposures 20 to 38 times the permissibleexposure limit. Their average blood lead level was 13.9 µg/dL. Immediate implementation of pertinentOccupational Safety and Health Administration regulations was recommended. In 2003, investigatorslearned that the unit also used an outdoor firing range with exposures exceeding the permissible exposure limit.Attempts to conduct more detailed evaluations and control measures were hindered by frequent deployments inthe unit and a strong commitment to realistic training. Despite these challenges, the controls implemented resultedin limited success. The average blood lead level in the unit was 6.8 µg/dL in 2005, a reduction of 51% .Proper initial range construction is essential to controlling lead exposures at firing ranges. Occupational healthspecialists caring for these Soldiers must identify, assess, and mitigate exposures from firing ranges while respectingthe importance of realistic training.The Overlooked Heroines: Three Silver Star Nurses of World War ILTC Richard M. Prior, AN USA; William Sanders Marble, PhDMilitary Medicine May 2008, Vol 173, No 5ABSTRACTAs members of forward-deployed combat hospitals, World War I Army nurses Miss Jane Rignel, MissLinnie Leckrone, and Miss Irene Robar received the Citation Star for gallantry in attending to the woundedwhile under artillery fire in the month of July 1918. In 1932, they were authorized to exchange their CitationStars for the new Silver Star Medal. Nursing in the war was difficult and required caring for patients exposedto chemical weapons and trauma while in harsh field conditions. These women were among the many Armynurses decorated for their performance in World War I.Abstracts From Current Literature57
Loss of Consciousness and Seizure During Normobaric Hypoxia TrainingMoniaga, Natalie C.; Griswold, Cheryl A.Aviation, Space, and Environmental Medicine, Volume 80, Number 5, May 2009 , pp. 485-488(4)ABSTRACTLoss of consciousness is a symptom with a broad differential diagnosis. Distinguishing between syncopeand seizure in a patient with a history of loss of consciousness can be equally difficult as their presentationcan be very similar. We present the case of a naval electronic countermeasures officer who experienced a lossof consciousness while undergoing hypoxia training with the reduced oxygen breathing device (ROBD). Duringthe episode the patient experienced tonic-clonic contractions with subsequent vertebral fractures, resultingin a prolonged grounding period. The patient's work-up focused on ruling out inherent cardiac and neurologicetiologies. After extensive examination and consultation with neurology, the patient was diagnosed with hypoxiainducedseizure, but was not felt to have an underlying seizure disorder. After reviewing his case, the Naval AerospaceMedical Institute felt that this incident represented a physiologic event and not a medical condition inherentto the aviator. It was, therefore, determined that this episode was not considered disqualifying and did not requirea waiver for return to duties involving flight. Our discussion details the appropriate work-up for loss ofconsciousness, examines possible physiologic explanations for this event, and describes aeromedical considerations.The authors include the patient's physiology instructor, one of the primary witnesses for the event, andthe patient's flight surgeon, who was extensively involved in his care.Ventilated Vest and Tolerance for Intermittent Exercise in Hot, Dry ConditionsWith Military ClothingBarwood, Martin J.; Newton, Phillip S.; Tipton, Michael J.Aviation, Space, and Environmental Medicine, Volume 80, Number 4, April 2009 , pp. 353-359(7)ABSTRACTIntroduction: Recent research has focused on developing air-ventilated garments to improve evaporative coolingin military settings. This study assessed a ventilated vest (Vest) in hot (45°C), dry (10% RH) ambient conditionsover 6h of rest and exercise. It was hypothesized that the Vest would lower the thermal strain and increasethe amount of exercise done by subjects. Methods: Eight healthy heat-acclimated men, wearing combat clothing,body armor, and a 19-kg load in webbing walked on a treadmill at 5 km • h−1 at a 2% incline until rectaltemperature (Trec) reached 38.5°C. They then rested until Trec reached 38°C, at which point they recommencedwalking. On one occasion the subjects wore a Vest, blowing ambient air around the torso. On the second occasionsubjects did not wear the vest (NoVest). Exercise/rest ratio, Trec, skin temperature (Tsk), sweat responses,rating of perceived exertion (RPE), and thermal comfort (TC) were measured. Results: Subjects wearing theVest exercised for significantly longer (18%; 11 min/h) as a percentage of total exposure time, stopped exercisesignificantly less often [Mean (SD); NoVest: 3 (2) stops; Vest: 1 (2) stops], and maintained significantly lowerskin temperature under the body armor [Tchest: NoVest 37.55 (0.51)°C; Vest: 35.33 (1.00)°C; Tback: NoVest:36.85 (0.83)°C; Vest: 35.84 (0.88)°C]. The Vest provided 28 W of cooling during exercise and 73 W when atrest as estimated by thermometry. Conclusion: A ventilated vest can provide cooling, and thereby reduce thermalstrain and increase exercise done in dry environmental temperatures up to 45°C, without causing skin irritationand discomfort.58Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
CENTRAL RETINAL VEIN OCCLUSION IN AN ARMY RANGER WITHGLUCOSE-6-PHOSPHATE DEHYDROGENASE DEFICIENCYLTC Russ S. Kotwal, MC, USA*; CAPT Frank K. Butler, Jr., MC, USN (Ret.)† ;LTC Clinton K. Murray, MC, USA‡;MAJ Guyon J. Hill, MC, USA§; LTC John C. Rayfield, MC, USA; CPT Ethan A. Miles, MC, USA*Previously published in Military Medicine, 174, 5:544, 2009. Permission granted to republish in the JSOM.ABSTRACTGlucose-6-phosphate dehydrogenase (G6PD) deficiency is the most prevalent human enzyme deficiency, affecting anestimated 400 million people worldwide. G6PD deficiency increases erythrocyte vulnerability to oxidative stress and may precipitateepisodes of hemolysis when individuals are exposed to triggering agents. Although central retinal vein occlusion(CRVO) does occur in G6PD-deficient individuals, G6PD-deficient individuals exposed to oxidative stressors have not beenpreviously reported to have an increase in CRVO incidence. This is a case of an Army Ranger who deployed to Afghanistanwith unrecognized G6PD deficiency and was placed on primaquine following his return to the <strong>United</strong> <strong>States</strong> and subsequentlydeveloped CRVO. Primaquine is a well-recognized cause of hemolysis in individuals with G6PD deficiency. Hemolytic anemiamay contribute to thrombosis as a result of increased erythrocyte aggregation and erythrocyte-endothelium interaction.This case underscores the continued need for routine G6PD screening and avoidance of known triggers in G6PD-deficient individuals.INTRODUCTIONGlucose-6-phosphate dehydrogenase (G6PD) deficiencyis the most common human enzyme disorder in theworld, with over 440 genetic variants and more than 400 millionpeople affected worldwide. 1,2,3 G6PD-deficient individualscan develop acute hemolytic anemia and other associatedreactions when exposed to oxidative stressors including infections,toxins, foodstuffs, and medications. According to existingliterature regarding the occurrence of retinal veinocclusions in this population, G6PD-deficient individuals arepostulated to have a significantly lower risk of developing centralretinal vein occlusion (CRVO). 4 However, the literaturedoes not state the risk of CRVO development in a G6PD-deficientindividual with an on-going oxidative stressor. Retinalvein occlusion, which includes branch retinal vein occlusionand CRVO, is the second most common sight-threatening retinalvascular disorder worldwide following diabetic retinopathy.5 This case presents a patient with unrecognized G6PDdeficiency who was placed on primaquine for malaria prophylaxisand subsequently developed a CRVO.CASE REPORTA 35-year-old active duty Army Ranger of Mediterraneandescent presented to his primary care provider with thechief complaint of constant blurred vision in his right eye withassociated symptoms of photophobia and a “seasick” sensationupon awakening one morning. These symptoms continuedto progressively worsen up until the time of hispresentation two weeks later. He denied ocular pain or anyother symptoms at the time of his initial evaluation.The patient’s past medical history was unremarkableexcept for intermittent mild normocytic normochromic ane-mia of unknown origin initially noted on a routine physical examinationfive years earlier. The patient denied any history ofvisual complaints, treatment for ophthalmologic conditions, tobaccouse, drug allergies, and prior medication complications.The patient’s recent medication history consisted ofdoxycycline 100mg daily for malaria chemoprophylaxis, whichhe consumed before, during, and after a three month deploymentto Afghanistan. He also consumed a two-week course ofprimaquine base 15mg daily concomitantly during the last twoweeks of his doxycycline regimen. Both medications werecompleted the month prior to symptom onset. The patientstated that he was compliant with the medication regimens.The physical examination at the time of presentationrevealed a distance visual acuity without correction of 20/200OD and 20/20 OS. His medical record denoted that he had previouslymaintained a visual acuity of 20/20 bilaterally withoutcorrection. The remainder of his physical exam was unremarkableto include stable vital signs with a normal blood pressure.He was referred to an ophthalmologist who confirmed thedecreased vision in the right eye and also noted an afferentpupillary defect, or Marcus Gunn reaction, of the right pupil.Additionally, the right eye fundoscopic examination was remarkablefor dilated, tortuous veins, diffuse four-quadrant intraretinalhemorrhage, and macular edema. (Figure) Theremainder of the ophthalmologic exam was normal to includenoncontact tonometry intraocular pressures of 14mmHg in eacheye and an unremarkable slit lamp examination.The ophthalmologist diagnosed nonischemic CRVO,and the patient was given a two-week course of brimonidine0.2% one drop twice a day, Cosopt (dorzolamide 2% and timolol0.5%) one drop twice a day, latanoprost 0.005% one dropPreviously Published 59
OD – Central Retinal Vein OcclusionOS – NormalFigure. Bilateral fundoscopic evaluation of patient’s eyes. OS is normal and OD is remarkable for dilated tortuous veins, diffuse intraretinalhemorrhage, and macular edema (“blood and thunder” fundus), which is characteristic of central retinal vein occlusion.at bedtime, and acetazolamide 500mg one capsule daily. Thepatient was also started on aspirin 325mg one tablet daily,which he continued throughout the year.The ophthalmologist conducted an initial laboratoryworkup which included a complete blood count, fasting glucose,prothrombin time/partial thromboplastin time, protein Cantigen, protein S activity, homocysteine, antithrombin IIIantigen, anticardiolipin panel, antinuclear antibody screen,rapid plasma reagin, and Treponema pallidum antibody. Allof these lab results were noted to be within normal limits.Also conducted was a bilateral carotid ultrasound that depictedno significant stenosis or atherosclerotic plaques.The ophthalmologist referred the patient to a retinalspecialist and an internist. The retinal specialist provided regularmonitoring and administered a series of intravitreal triamcinoloneinjections throughout the following year toreduce the macular edema present. The internal medicinephysician reviewed the previous labs and ordered additionallaboratory testing to include a urinalysis, complete bloodcount, comprehensive metabolic panel, prothrombintime/partial thromboplastin time, antinuclear antibody screen,antithrombin III antigen, factor V Leiden DNA, factor VIIIA,von Willebrand factor, factor XIIA, protein C antigen, complementprotein C3 and C4, complement CH50, lupus anticoagulantbattery, dilute Russell Viper venom time,immunoglobulin antibodies, cryoglobulin screen, and hepatitisB and C panel. All of these lab results were noted to bewithin normal limits. A computerized tomography (CT) scanof the chest and abdomen depicted minimal pleuralparenchymaldensities scattered in the left peripheral lungfield with a few tiny calcifications representing residua froma prior inflammatory disease. The patient denied any pulmonarysymptoms and no prior CT scans were available forcomparison. The internal medicine physician consulted ahematologist who reviewed the lab and CT results and offeredno further diagnostic or treatment options beyond thosecurrently being provided by the retinal specialist.It was not until a year later that a new primary careprovider noted that the patient was G6PD-deficient duringroutine lab screening for G6PD prior to initiating primaquinetherapy for a subsequent deployment to Afghanistan. The patient’sG6PD value was 0.2 IU/g Hb (reference range for normal7.0-20.5 IU/g Hb), and he was categorized as havingsevere enzyme deficiency (< 10% of normal). However, hedid not fulfill the full Class II criteria depicted by the WorldHealth Organization as there was no historical evidence ofintermittent hemolysis with erythrocytic stress or chronic hemolyticanemia. 2 Following a review of the patient’s records,this provider hypothesized a possible connection between thepatient’s G6PD deficiency, his previous intake of primaquine,and the development of CRVO that ensued following his previousdeployment to Afghanistan. This provider conducted athorough literature search and discussed the case with preventivemedicine specialists at the U.S. Army Center forHealth Promotion and Preventive Medicine, an infectious diseasespecialist at Brooke Army Medical Center, and ophthalmologyspecialists in the Army and Navy. A similar case wasnot previously cited.The patient continued routine treatment and followupwith his ophthalmologist and the retinal specialist. At thetwo-year follow-up he was noted to have an uncorrected visualacuity of 20/20 OD and OS. There was no afferent pupillarydefect and noncontact tonometry intraocular pressureswere 15mmHg OD and 12mmHg OS. The slit lamp examinationwas negative for iris neovascularization OD. The ODfundoscopic exam denoted mild residual disk edema, vasculartortuosity, and macular edema with a few scattered retinalhemorrhages. The fundus was normal OS.DISCUSSIONG6PD DeficiencyG6PD is a critical metabolic enzyme that supportsreduction and oxidation in aerobic cells such as erythrocytes.The gene for G6PD is sex linked and found on the long arm60Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
of the X chromosome. Notable is that more than 400 millionpeople carry a G6PD-deficient gene. 1,2,3 Although dispersedworldwide, G6PD deficiency occurs with increased frequencythroughout Africa, Asia, the Middle East, and the Mediterraneanregion. While G6PD deficiency may provide a biologicaladvantage through relative resistance to Plasmodiumfalciparum malaria, it has over 440 known genetic variantsthat result in varying degrees of enzymopathy and a wide spectrumof clinical outcomes ranging from asymptomatic to severehemolytic reactions resulting in transfusion or death. 1,2G6PD deficiency has conventionally been the archetype of enzymopathyhemolytic anemias and is a leading model of hemolyticanemia resulting from intracorpuscular andextracorpuscular interaction, as most of these hemolytic casesare triggered by an exogenous agent. These exogenous triggersinclude infections, toxins, foodstuffs (ie, fava beans), andmedications (ie, antimicrobials).Although the antimicrobial primaquine prompted thediscovery of G6PD deficiency over 50 years ago, 1 primaquinecontinues to be an important adjunct used routinely for antimalarialtherapy. As a response to frequent deployments ofnumerous Army personnel to malaria-endemic regions includingAfghanistan, the Department of the Army directed thatall deploying U.S. Army personnel would undergo G6PD deficiencyscreening in order to safeguard against hemolytic reactionsresulting from primaquine therapy. 6 In this case report,it is uncertain how the individual described did not receivescreening for G6PD deficiency prior to the initiation of primaquinetherapy.By itself, primaquine is a cause of increased levels ofmethemoglobin in many patients who take it, but the levelsachieved seldom cause symptoms. However, pathologicmethemoglobinemia and hemolytic anemia do routinely occurin G6PD-deficient individuals who consume primaquine. Primaquineis known to be associated with visual accommodationcomplaints, although a review of the literature does notreveal documentation of other visual disorders to includeCRVO. However, the finding of increased erythrocyte aggregationand erythrocyte-endothelium interaction observed inhemolytic disease states may contribute to diffuse microvascularthrombosis in various organ systems to include the eye. 7Central Retinal Vein OcclusionRetinal vein occlusion includes branch retinal vein occlusionand central retinal vein occlusion. Following diabeticretinopathy, retinal vein occlusion is the second most commonsight-threatening retinal vascular disorder. The prevalence ofCRVO in the <strong>United</strong> <strong>States</strong> has been reported to be 1 per 1000and is slightly more common in men than in women. 5The majority of people diagnosed with CRVO areover the age of 50. The most common symptom of CRVO isacute and persistent monocular visual loss. Patients characteristicallypresent with an abrupt, painless, unilateral loss ofvision of variable severity. CRVO is generally categorized asischemic or nonischemic. The hallmark fundus finding ofCRVO is four-quadrant retinal hemorrhage. The more commonnonischemic form has good perfusion to the retina andrelatively good visual acuity on presentation. Vision may returnto normal if not decreased by persistent macular edema.Nonischemic CRVO can progress to ischemic CRVO, withone-third of nonischemic cases progressing to ischemic withina year. Frequent follow-up is needed to monitor for thischange. Patients can also have ischemic CRVO on initial presentationwith visual acuity typically 20/400 or worse. IschemicCRVO typically presents with more extensive retinal hemorrhage,cotton wool spots, disc edema, and often an afferentpupillary defect. Intravenous fluorescein angiogram is commonlyused to help define the level of retinal non-perfusion inCRVO. Vision loss in ischemic CRVO may result from ganglioncell ischemia, macular edema, or neovascular complicationswith secondary glaucoma.Although CRVO can occur without a known underlyingcause, it is often associated with systemic disease (atherosclerosis,autoimmune disease, diabetes, hypertension,intravenous drug abuse, renal insufficiency, tobacco use, vasculitis)or local pathology (ocular trauma, orbital abscess, orbitaltumor, glaucoma). 5,8 When CRVO occurs in youngerpatients it is often associated with blood dyscrasias such as coagulationdisorders and hyperviscosity syndromes.Sickle cell disease has been associated with a hypercoagulablestate. 7 Given the hyperviscosity and vaso-occlusivetendencies of individuals with sickle cell crisis, 9 it isinteresting that only one case of CRVO in a sickle cell patienthas been reported in the literature. 10 Additionally, it is notablethat in this sickle cell case report, a comorbid protein S deficiencymay have contributed to the ultimate CRVO pathogenesis.Furthermore, an extensive review of the medicalliterature also detected only one article describing CRVO incidencein G6PD-deficient patients. 4 However, this article postulatedprotection against CRVO in Sardinian G6PD-deficientpatients with the Mediterranean variant. The investigators inthis study cited a 3.55% incidence of CRVO in their G6PDdeficientpopulation versus a 10-15% incidence of CRVO intheir general population. Not stated in this article was the riskof CRVO development in a G6PD-deficient individual with anactive oxidative stressor.Treatment of CRVO has historically been directed towardthe management of the contributing or associated systemicmedical problem, as few treatments have had provenefficacy in the treatment of CRVO. Treatment options includeaspirin, non-steroidal anti-inflammatory drugs, plasmapheresis,anticoagulation, fibrinolytics, and systemic corticosteroids.Anti-platelet agents are frequently prescribed; however, theirefficacy is controversial. Panretinal photocoagulation is usedfor patients experiencing neovascular complications to reduceor reverse angiogenesis and avoid the development of neovascularglaucoma.Additional treatment options with improved efficacyhave recently become available. Intravitreal triamcinolone hasproven effective in reducing edema and improving vision forpatients with macular edema, 11,12 and is more likely to be efficaciousin patients without ischemic CRVO or diabetes. However,these patients sometimes have rebound symptoms andrequire continued treatment.A new approach to treating CRVO is the use of intravitrealbevacizumab. 13 Elevated levels of vascular endothelialgrowth factor (VEGF) have been found in CRVO andhave been positively correlated with the onset and progressionPreviously Published 61
of CRVO neovascular complications. 14 The ability of VEGFblockers to decrease vascular permeability has also suggestedits usefulness in treating macular edema. This therapy wassuccessful in improving the vision of one patient with a nonischemicCRVO from 20/200 to 20/25 eight weeks followinginjection. Bevacizumab also offers the advantage of not causingincreases in intraocular pressure sometimes seen with intravitrealtriamcinolone injections. 13A new option for treating ischemic CRVO may behyperbaric oxygen therapy (HBOT). 15 There is a strong theoreticalbasis for HBOT to be useful in managing ischemicCRVO, and there are multiple case reports documenting successwith this treatment modality. As with central retinal arteryocclusion, there is likely a time window beyond whichHBOT is less likely to be effective, but this time window isnot well defined for CRVO. 16,17,18CONCLUSIONG6PD-deficiency is noted to affect 2.5% of militarymales, with up to 12% of the African American military population.6 Although uncertain that the CRVO experienced bythe individual described in this report was a result of his primaquinetherapy, this case still underscores the continued requirementfor routine G6PD deficiency screening indeploying military personnel and the avoidance of all potentialtriggers in patients who are G6PD-deficient. G6PD-deficientindividuals may suffer hemolytic reactions and otheradverse reactions when exposed to oxidative stressors suchas primaquine. In this case report, it may be possible that exposureto primaquine in a patient with unrecognized G6PDdeficiency may contribute to the development of CRVO.DISCLAIMERThe views, opinions, and findings contained in this reportare those of the authors and should not be construed as official orreflecting the views of the Department of Defense. There is nocopyright to be transferred as the authors are employees of the U.S.government and this report was prepared as part of their official duties.This report was approved for public release by the 75th RangerRegiment and USASOC Public Affairs Office on February 26,2008.REFERENCES1. Beutler E: G6PD deficiency. Blood 1994; 84: 3613-36.2. Cappellini M, Fiorelli G: Glucose-6-phosphate dehydrogenase deficiency.Lancet 2008; 371: 64-74.3. Frank J: Diagnosis and management of G6PD deficiency. Am FamPhysician 2005; 72: 1277-82.4. Pinna A, Carru C, Solinas G, et al: Glucose-6-phosphate dehydrogenasedeficiency in retinal vein occlusion. Invest Ophthalmol Vis Sci2007; 48: 2747-52.5. Kelley J, Opremcak E: Central retinal vein occlusion. Contemp Ophthalmol2007; 6: 1-8.6. Chinevere T, Murray C, Grant E, et al: Prevalence of glucose-6-phosphate dehydrogenase deficiency in U.S. Army personnel. MilMed 2006; 171: 905-7.7. Lewis D, Nyska A, Potti A, et al: Hemostatic activation in a chemicallyinduced rat model of severe hemolysis and thrombosis. ThrombRes 2006; 118: 747-53.8. Prisco D, Marcucci R: Retinal vein thrombosis: Risk factors, pathogenesisand therapeutic approach. Pathophysiol Haemost Thromb2002; 32: 308-311.9. Johnson C: Arterial blood pressure and hyperviscosity in sickle celldisease. Hematol Oncol Clin North Am 2005; 19: 827-37.10. Hasan S, Elbedawi M, Castro O, et al: Retinal vein occlusion in sicklecell disease. South Med J 2004; 97: 202-4.11. Bashshur Z, Ma’luf R, Allam S: Intravitreal triamcinolone for themanagement of macular edema due to nonischemic central retinal veinocclusion. Arch Ophthalmol 2004; 122: 1137-40.12. Cekic O, Chang S, Tseng J: Intravitreal triamcinolone treatment formacular edema associated with central retinal vein occlusion andhemiretinal vein occlusion. Retina 2005; 25: 846-50.13. Spandau U, Ihioff A, Jonas J: Intraviteal bevacizumab treatment ofmacular edema due to central retinal vein occlusion. Acta OphthlamolScand 2006; 84: 555-6.14. Boyd S, Zachary I, Chakravarthy U, et al: Correlation of increasedvascular endothelial growth factor with neovascularization and permeabilityin ischemic central vein occlusion. Arch Ophthalmol 2002;120: 1644-50.15. Butler FK, Hagan C, Murphy-Lavoie H: Hyperbaric oxygen therapyand the eye. Undersea Hyperb Med 2008; 35: 333-87.16. Wright J, Franklin B, Zant E: Clinical case report: Treatment of acentral retinal vein occlusion with hyperbaric oxygen. Undersea HyperbMed 2007; 34: 315-9.17. Johnson G: A navigator with non-ischemic central retinal vein occlusionprogressing to ischemic central retinal vein occlusion. AviatSpace Environ Med 1990; 61: 962-5.18. Gismondi A, Colonna S, Micalella F, Metrangolo C: Hyperbaric oxygentherapy in thrombotic occlusion of the central retinal vein. MinervaMed 1981; 72: 1413-5.62Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
AUTHORS*75th Ranger Regiment6420 Dawson LoopFort Benning, GA 31905russ.kotwal@us.army.milethan.miles@us.army.mil(706) 545-4230†Department of OphthalmologyNaval Operational Medicine Institute220 Hovey RoadPensacola, FL 32508frank.butler@med.navy.mil(850) 452-7720‡ Infectious Diseases ServiceBrooke Army Medical Center3851 Roger Brooke DriveFort Sam Houston, TX 78234clinton.murray@us.army.mil(210) 916-4355§1st <strong>Special</strong> Forces Group (Airborne)9190 Chapman CircleFort Lewis, WA 98433guyon.hill@us.army.mil(210) 378-9037Department of Emergency MedicineBrooke Army Medical Center3851 Roger Brooke DriveFort Sam Houston, TX 78234john.rayfield@us.army.mil(210) 916-1006Contact and Guarantor: LTC Russ S. Kotwal, MC, USAAddress: HQ, 75th Ranger Regiment, 6420 Dawson Loop, FortBenning, GA 31905Phone: Work 706/545-4545, Cell 706/366-2104Email: russ.kotwal@us.army.mil, kotwalr@soc.mil,kotwals@earthlink.netPreviously Published 63
SHOULD WE TEACH EVERY SOLDIER HOW TO START AN IV?MAJ Robert L. Mabry, MC USA *; MAJ Peter J. Cuenca, MC USA tPreviously published in Military Medicine,. 2009 Jun;174(6):iii-v. Permission granted to republish in the JSOM.The recent mandate by the U.S. Army Training andDoctrine <strong>Command</strong> (TRADOC) requiring all soldiers enteringbasic combat training (BCT) after October 1, 2007 to be combatlifesaver (CLS) certified is an outstanding step to improvetraining across the Army in lifesaving first-aid skills. 1 However,requiring all Soldiers to be competent in placing an intravenousline and initiating treatment with IV fluids, per thecurrent CLS standards, may not be the best use of precioustraining resources in light of the most recent medical researchand battlefield experience.The outcome of a battle casualty will often be determinedby whomever provides initial care. In most cases thiswill be a fellow Soldier, not the medic. The CLS course wasdeveloped to bridge the gap between self-aid or buddy aid untilcare could be provided by the platoon 68W combat medic. 2The CLS concept has been further refined over the last decadeto reflect the concepts of TC3. Tactical combat casualty carefocuses on treating the leading causes of preventable battlefielddeath while minimizing the risk to first-aid providers andthe tactical mission. 3 The TC3 concept is possibly the mostsignificant advance in point of injury care since the distributionof the individual field dressing in the late 1800s. 4The most important battlefield first-aid skill is controllinghemorrhage, by far the leading and most preventablecause of battlefield death in modern warfare. Bellamy showed9% of those killed in action during the Vietnam conflict diedof potentially preventable extremity hemorrhage. 5 A similarfatality rate from compressible extremity hemorrhage in Iraqwas demonstrated by Cuadrado et al. 6 Proper tourniquet applicationis the most important method in controlling severehemorrhage in the tactical setting.Other lifesaving skills emphasized in the TC3 includeneedle decompression of a tension pneumothorax and airwaymanagement, the second and third leading causes of preventablebattlefield deaths, causing 4% and 1% of all fatal injuresrespectively 5,7The main purpose of performing IV catheterization inthe setting of trauma is to administer fluids or blood productsto treat hemorrhagic shock. Seven percent of patients on thebattlefield require aggressive resuscitation. 8 Current transfusionprotocols emphasize fresh whole blood and procoagulantsrather than crystalloids to restore organ perfusion, prevent thedilution of clotting factors, and avoid hypothermia. 8 For patientsin significant hemorrhagic shock, aggressive hemorrhagecontrol at the point of wounding, followed by expeditioustransport to surgical care is most important. Evacuation andsubsequent surgical management of noncompressible truncalhemorrhage should not be delayed by attempts to place an IV.In the management of shock, the traditional strategyof early fluid resuscitation beginning in the field and continuinginto the operating room has been challenged, specificallyin the context of penetrating thoracic trauma. In 1994, aprospective trial by Bickell et al. compared immediate versusdelayed fluid resuscitation in hypotensive patients with pene-trating torso injuries. They reported that patients in whom fluidswere restricted until arrival in the operating room hadlower mortality, fewer postoperative complications, andshorter hospital length of stay. 9 In a follow-up prospectivetrial, patients were divided into either restrictive resuscitation(goal systolic blood pressure (SBP) greater than 80mmHg)versus liberal resuscitation (goal SBP greater than 100mmHg).There was not a significant difference in mortality betweengroups but hemorrhage did take longer to control in the groupwith the liberal fluid strategy. 10These studies were largely responsible for significantchanges in the management of injured soldiers on the battlefieldand were adopted by American Military and Israeli DefenseForces. 11-15 In 2003, the term “hypotensiveresuscitation” was introduced in a article entitled, “Fluid Resuscitationin Modern Combat Casualty Care: LessonsLearned from Somalia.” 15 Current military prehospital doctrinenow emphasizes restricting IV fluids in casualties whohave controlled hemorrhage, normal mental status, and stablevital signs or even mild hypotension (systolic blood pressuregreater than 90). A relatively small percentage of all combatcasualties are likely to benefit from IV fluid resuscitation onthe battlefield.These include patients with significant hypotensionresulting from severe hemorrhage that has been controlled;and, those with hypotension or severe hemorrhage and a headinjury. All other casualties with uncontrolled hemorrhage andsigns of shock may be challenged with a very limited amountof IV fluid (l,000mL of Hextend). Further fluid administrationis likely to be detrimental. The practice of permissive hypotensionis designed to prevent “popping the clot” off an injuredvessels as well as diluting clotting factors with massiveamounts of crystalloid fluid.Intravenous placement is a skill that requires significanttime to acquire. In the current CLS course, the IV portionis the longest, most resource and instructor intensive block oftraining. This is precious training time that could be used fortactical casualty scenarios and practicing sustainable, lifesavingskills such as hemorrhage control techniques. In the civiliansector, basic emergency medical technicians (EMT-B) arenot taught IV insertion. The first level of civilian EMT to haveIV placement in their scope of practice is EMT-Intermediates.The national standard curriculum for EMT-I requires 300-400hours of classroom and field instruction after EMT -8 certification.EMT-I students are required to place a minimum of25 IVs on live patients of various age groups under instructorsupervision to be considered competent in this skill. 16 Thecurrent 2006 CLS Course Instructor Guide (Edition B, Subcourse IS00873) does not specify the number of successful IVcatheterizations required to certify a CLS in this skill. It is leftto the unit’s medical officer. Certification as a CLS will notmean these Soldiers are competent at placing IVs. At best itwill mean they are familiar with the procedure.64Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
Casualties presenting in overt shock typically have difficultintravenous access. They are often extremely diaphoreticand their peripheral vasculature is constricted. Placement ofan IV in a trauma patient in a moving ambulance by an experiencedEMT-I or higher level provider takes 10 to 12 minutesand has a 10% to 40%, failure rate. 17 Paradoxically, starting anIV in those patients who would most benefit from limited fluidresuscitation will be extremely difficult for even the mostskilled medical provider. During a hostile tactical situationcombined with darkness, fatigue, and fear it will be very unlikelythat a Soldier without significant medical experience willbe able to place an IV under battlefield conditions. For thisreason, TC3 guidelines emphasize sternal intraosseous catheterplacement for fluid resuscitation. 18Insertion of an IV catheter is not without risks. Complicationsinclude local and systemic infections, deep venousthrombosis, thrombophlibits, catheter embolism, and injury toassociated nerves, tendons, and arteries. 19-21 Complications areinversely related to skill and experience of the medicalprovider.On the basis of the available literature and the lessonsbeing learned from both Iraq and Afghanistan, it is clear that IVplacement is not a critical lifesaving skill, while hemorrhagecontrol is. Training all Soldiers to start IVs without the requisiteunderstanding of the indications, contraindications, risks,and benefits of who would benefit from IV fluids and whocould be harmed, could result in many receiving unneeded ordetrimental care on the battlefield. If Soldiers spend the vastmajority of their first-aid training time learning IV placement,the most time-consuming skill in the CLS course, yet one thatdoes not save lives, which tool will they reach for under thestress of combat? Will Soldiers be killed by snipers as theywaste precious minute starting IVs? Will evacuation to lifesavingsurgical care be delayed while attempts to “get the IV”are made? Will proper tourniquet and dressing application beneglected while focusing on the more “technical” and “highspeed”IV insertion?While most Soldiers will not benefit from IV training,it may have a place in some units. Units operating far forwardwith little or no organic medical support such as <strong>Special</strong> <strong>Operations</strong>Forces (SOF) may benefit from this training. These unitsare often small and have the time and resources to train to ahigh standard in advanced first-aid skills.Many line commanders likely participated in “IV training”led by their unit medical officers during their formativeyears. Insertion of an IV on the “first stick” is considered bymany as the quintessential battlefield medical skill. It is not.Rapid hemorrhage control is. Additional medical training forall Soldiers is much needed. TRADOC has taken an excellentfirst step. Our battlefield commanders want robust first-aidtraining for our warriors. We must continue to synthesize thetactical and medical lessons from the present conflicts to guideour training. It is the duty of the AMEDD and military healthcareproviders to develop best practices of battlefield care andadvise our combat commanders how to implement them so togetherwe can save lives on the battlefield and accomplish theArmy mission.REFERENCES1. Glasch MA: IV injections added to BCT requirement The Leader,TRADOC News Service. Available at www.tradoc.army.mil/pao/TNSarchives/September%2007/091407-1.html: Accessed September 14,2007.2. FM 4-02.4. APPENDIX C Role of the Combat Lifesaver.3. Butler F: Tactical Combat Casualty Care: Combining good medicinewith good tactics. Editorial J Trauma Inj Infect Crit Care 2001;54(Suppl 5) S2-3.4. Mabry RL. McManus JG. Prehospital advances in the management ofsevere penetrating trauma. 2009 (in press)5. Bellamy RF: The causes of death in conventional land warfare: Implicationsfor combat casualty care research. Mil Med 1984; 149(2):55-62.6. Cuadrado D. Arthurs Z. Sebesta J, et al: Cause of death analysis at the31st Combat Support Hospital during Operation Iraqi Freedom. Presentedat the 28th Annual Gary P. Wratten Army Surgical Symposium.Silver Spring, Maryland. Walter Reed Army Institute of Research. May2006.7. McPherson JJ, Feigin DS, Bellamy RF: Prevalence of tension pneumothoraxin fatally wounded combat casualties. J Trauma 2006;60:573-8.8. Beekley A. Starnes B, Sebesta J: Lessons Learned from modern militarysurgery. Surgical Clinics of North America, Volume 87, Issue 1,February 2007.9. Bickell W, Wall M. Pepe P, et al: Immediate versus delayed fluid resuscitationfor hypotensive patients with penetrating torso injuries. N EnglJ Med 1994; 331(17): 1105-9.10. Dutton R. Mackenzie C, Scalea T: Hypotensive resuscitation during activehemorrhage: Impact on in-hospital mortality. J Trauma 2002: 52(6):1141-6.11. Holcomb J: Fluid resuscitation in modern combat casualty care: Lessonslearned from Somalia. J Trauma 2003: 54(Suppl 5): S46-51.12. Champion H: Combat fluid resuscitation: Introduction and overview ofconferences. J Trauma 2003; 54(Suppl 5): S7-12.13. Butler F. Hagmann J. Richards D: Tactical management of urban warfarecasualties in <strong>Special</strong> <strong>Operations</strong>. Mil Med 2000: 165(Supp14): 1-48.14. Krausz M: Fluid resuscitation strategies in the Israeli army. J Trauma2003; 54(Suppl 5): S39-42.15 Rhee P, Koustova E, Alam H: Searching for the optimal resuscitationmethod: Recommendations for the initial fluid resuscitation of combatcasualties. J Trauma 2003: 54(Suppl 5): S52-62.16. NREMT National Standard Curriculum for NREMT EMT-Intermediate:1998. Available at http://www.nh!sa.dot.gov/peoplc/injury/ems/EMT-Uindex.html.17. Lewis F: Prehospital intravenous fluid therapy: Physiologic computermodeling. J Trauma 1986: 26(9): 804-11.18. Butler FK, Holcomb JB. Giebner SD, et al: Tactical Combat CasualtyCare 2007: Evolving Concepts and Battlefield Experience. U.S. Armyinstitute of Surgical Research Technical Report. March .10. 2007.19. Bregenzer T. Conen D, Sakmann P, Widmer A: Is routine replacementof peripheral intravenous catheters necessary? Arch Intern Med 1998:158: 151-6.20. Levine R, Spaite D, Valenzuela T. Criss E, Wright A., Meislin H:Comparison of clinically significant infection rates among prehospitalversus in-hospital-initiated IV lines. Ann Emerg Med 1995: 25:502-6.21. Elliot T, Faroqui M: Infection and intravascular devices, Br J HospMed 1992: 48: 496-503.Previously Published 65
FURTHER READINGSBeekley A, Sebesta J. Blackbourne L. et al: Pre-Hospital tourniquetuse in Operation Iraqi Freedom: Effect on hemorrhage control andoutcomes. Presented at the 30th Annual Scientific Meeting of theWestern Trauma Association. Big Sky, Montana. March 2006.Little R: Modern combat lacking in old medical supply. BaltimoreSun. March 6, 2005*Medical Director for Academics, Department of Combat Medic Training,Fort Sam Houston, TX.tStaff Emergency Physician, Department of Emergency Medicine, BrookeArmy Medical Center, Fort Sam Houston, TX.The opinions or assertions contained herein are the private viewsof the authors and are not to be construed as official or as reflecting the viewsof the Department of the Army or the Department of Defense.Mabry RL: Tourniquet use on the battlefield. Mil Med 2006: 171(5):352-6.66Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
PSYCHOLOGICAL RESILIENCE AND POSTDEPLOYMENT SOCIAL SUPPORT PROTECTAGAINST TRAUMATIC STRESS AND DEPRESSIVE SYMPTOMS IN SOLDIERS RETURNINGFROM OPERATIONS ENDURING FREEDOM AND IRAQI FREEDOMRobert H. Pietrzak, Ph.D., M.P.H., 1,2 Douglas C. Johnson, Ph.D., 3 Marc B. Goldstein, Ph.D., 4James C. Malley, Ph.D., 5 and Steven M. Southwick, M.D. 1,2Previously Published in Depression and Anxiety 0 : 1–7 (2009). Permission granted to republish in the JSOM.ABSTRACTBackground: A number of studies have examined the prevalence and correlates of posttraumatic stress disorder (PTSD),depression, and related psychiatric conditions in Soldiers returning from <strong>Operations</strong> Enduring Freedom and Iraqi Freedom(OEF/OIF), but none have examined whether factors such as psychological resilience and social support may protectagainst these conditions in this population. Methods: A total of 272 predominantly older reserve/National Guard OEF/OIFveterans completed a mail survey assessing traumatic stress and depressive symptoms, resilience, and social support. Results:Resilience scores in the full sample were comparable to those observed in civilian outpatient primary-care patients.Respondents with PTSD, however, scored significantly lower on this measure and on measures of unit support and postdeploymentsocial support. A hierarchical regression analysis in the full sample suggested that resilience (specifically, increasedpersonal control and positive acceptance of change) and postdeployment social support were negatively associatedwith traumatic stress and depressive symptoms, even after adjusting for demographic characteristics and combat exposure.Conclusions: These results suggest that interventions to bolster psychological resilience and postdeployment social supportmay help reduce the severity of traumatic stress and depressive symptoms in OEF/OIF veterans.INTRODUCTIONA large number of Soldiers serving in <strong>Operations</strong> EnduringFreedom and Iraqi Freedom (OEF/OIF) are returningfrom their deployments with posttraumatic stress disorder(PTSD), depression, and related psychological problems thatimpair functioning and quality of life. 1 Although severalstudies have examined the prevalence and correlates of theseconditions in this population, 2,3 little research has examinedfactors that may be protective against traumatic stress anddepressive symptoms.Psychological resilience and social support may protectagainst the development of traumatic stress 4,5 and depressivesymptoms. 6 Psychological resilience and relatedconstructs such as hardiness are characteristics that enable anindividual to adapt positively to adversity and that confer protectionagainst the development of psychopathology. 5,7 Theyhave been shown to protect against the development of PTSDfollowing combat in Vietnam veterans 4,8 and Army ReserveSoldiers. 9 Higher perceived social support, which is operationalizedas an individual’s perception or experience of helpfuland unhelpful social interactions, is also negativelyassociated with PTSD 10,11 and depression, 5 with higher perceivedsocial support associated with lower risk of PTSD 4,12,13and depression. 5 These findings suggest that increased psychologicalresilience and perceived social support may helpprotect against the deleterious effects of traumatic stress anddepression.To date, however, no known study has examinedvariables that may confer protection against traumatic stressand depressive symptoms in OEF/OIF veterans. An examinationof differential aspects of resilience and social supportis important because it may provide insights into cognitive,behavioral, social, and spiritual factors that may protect militarypersonnel exposed to trauma against the development ofPTSD, depression, and related conditions, and potentially informtraining and treatment strategies to enhance resilienceto stress. The purpose of this study was to: (1) provide a descriptiveanalysis of aspects of resilience endorsed byOEF/OIF veterans; (2) compare endorsements of various aspectsof resilience between OEF/OIF veterans with and withoutPTSD; and (3) examine whether resilience and socialsupport may protect against traumatic stress and depressivesymptoms after controlling for demographic characteristicsand severity of combat exposure. We hypothesized thatOEF/OIF veterans would report relatively high levels of resiliencein general, that compared to veterans without PTSD,veterans with PTSD would score lower on measures of resilienceand social support, and that increased resilience andsocial support would be negatively associated with severityof traumatic stress and depressive symptoms.METHODSSAMPLERespondents were 272 OEF/OIF veterans from Connecticutwho completed the Connecticut OEF/OIF VeteransNeeds Assessment Survey (dates of military service: 01/03–03/07). This survey was developed to identify the salientneeds of OEF/OIF veterans in Connecticut and provide recommendationsfor legislative and public policy initiatives toimprove readjustment to civilian life. The target populationwas all Connecticut veterans who served in OEF/OIF since2003. Potential respondents were identified by the inspectionof copies of discharge papers (DD-214s) that were sent to theCommissioner of Veterans Affairs for the state. Her staffidentified eligible veterans and selected the first 1,050 (alphabetically)for the target sample. One thousand and fiftysurveys were mailed and 285 were returned (27.1% returnPreviously Published 67
ate). A reminder postcard was sent 1 week after the surveyswere mailed. Respondents were older than nonrespondents inthe sampling frame (33.4 versus 31.3 years, t52.87, P5.004).On average, surveys were completed 26.9 months (standarderror of the mean [SEM] 5.7) following return from deployment.Institutional review boards of the Yale University, theCentral Connecticut State University, and the VA ConnecticutHealthcare System approved the study.ASSESSMENTSThe Connor–Davidson Resilience Scale (CD-RISC 14 )is a 25-item self-report assessment of psychological resilience.Items are scored on a 5-point range: ‘‘0’’ for ‘‘Not true at all,’’‘‘1’’ for ‘‘Rarely true,’’ ‘‘2’’ for ‘‘Sometimes true,’’ ‘‘3’’ for‘‘Often true,’’ and ‘‘4’’ for ‘‘True nearly all of the time.’’ Totalscores, which range from 0 to 100, and five subscales, whichwere generated using exploratory factor analysis in the initialvalidation study of this instrument, 14 are computed: (1) personalcompetence, (2) tolerance of negative affect and stressrelatedgrowth, (3) acceptance of changes, (4) personalcontrol, and (5) spiritual orientation to the future. In this sample,Cronbach’s α on CD-RISC items was .94.The Combat Experiences Scale (CES) is a 15-itemself-report instrument from the Deployment Risk and ResilienceInventory (DRRI, 15,16 available upon request from:http://www.ncptsd.va.gov/ncmain/ assessment/assessmt_request_form.html).It assesses exposure to combat, such as firinga weapon, being fired on by enemy or friendly fire, andwitnessing injury and death. Higher scores represent greatercombat exposure. A previous validation study in OIF veteransfound that CES scores correlated positively with measures ofPTSD and depression symptoms and negatively with mentalhealth functioning. 16 In this sample, Cronbach’s a on CESitems was .93.The Posttraumatic Stress Disorder Checklist—MilitaryVersion (PCLM 17 ) is a 17-item screening instrument basedon diagnostic criteria for PTSD. Respondents who scored >50and who met B, C, and D criteria for PTSD were identified asscreening positive for PTSD. This definition provides a conservativeestimate of the prevalence of PTSD, which correspondsto Diagnostic and Statistical Manual of MentalDisorders—Fourth Edition criteria for PTSD. Cronbach’s αon PCL-M items was .96.The Patient Health Questionnaire—9 (PHQ-9 18 ) is anine-item self-report screening instrument for depression derivedfrom the clinician-administered Primary Care Evaluationof Mental Disorders. Higher scores indicate greaterdepressive symptoms, with scores > 15 indicating a positivescreen for depression. Cronbach’s α on these items was .92.The Unit Support Scale (USS) is a 12-item self-reportinstrument from the DRRI 15,16 that assesses the amount of assistanceand encouragement in the war zone from unit leadersand members, and the military in general. Questions include,‘‘My unit was like a familyto me,’’ ‘‘My superiors made a real attempt to treat me as aperson,’’ and ‘‘I could go to most people in my unit for helpwhen I had a personal problem.’’ A validation study in GulfWar veterans found that scores on the USS correlate negativelywith measures of PTSD, depression, and anxiety. 15 Inthis sample, Cronbach’s α on USS items was .93.The Postdeployment Social Support Scale (PSSS) is a15-item selfreport measure from the DRRI 15,16 that assessespostdeployment emotional support and instrumental assistanceprovided by family, friends, coworkers, employers, and community.Validation studies in OIF and Gulf War veterans foundthat PSSS scores correlated negatively with measures ofPTSD, depression, and physical symptoms and positively withmeasures of physical, mental, and cognitive functioning. 15,16In this sample, Cronbach’s α on these items was .82.DATA ANALYSISLogarithmic base 10 transformations were used totransform nonnormally distributed continuous variables (e.g.,PCL-M scores) prior to analysis. Demographic characteristicswere compared using independent-samples t tests and x 2 tests.Scores on each of the CDRISC items by PTSD status werecompared using univarate analyses of covariance (two-tailed,α 5.05) with demographic variables that differed between thegroups entered as covariates. Cohen’s d values ([Meangroup1_ Mean group2 ]/pooled standard deviation) were computedto estimate effect sizes of group differences. 19 Post hoc t testswere used to compare total CD-RISC scores to norms reportedin Connor and Davidson 14 and to examine group differenceson individual CD-RISC items, with P < .01 considered significantin the latter analyses.Hierarchical regression analyses were conducted toexamine predictors of traumatic stress and depressive symptomseverity. All respondents, including those with and withoutPTSD and with and without positive screens fordepression, were included in these analyses. Continuousscores on the PCL-M and PHQ-9 were entered as dependentvariables in separate analyses. Variables hypothesized to berelated to PTSD and depressive symptoms were entered as independentvariables. Step 1 included demographic variables(age, sex, race/ethnicity, education, relationship status, dutytype: active versus reserve), Step 2 included a measure of combatexposure (CES), and Step 3 included potentially protectivefactors (USS, PSSS, CDRISC). Complete data were availablefor 255 respondents.RESULTSDEMOGRAPHIC CHARACTERISTICS, COMBAT EXPERIENCESEVERITY, AND PSYCHOSOCIAL MEASURESIn the full sample, mean age was 34.9 (SE = .4), 89.4%were white, 82.4% completed at least some college education,27.8% were active duty, and 72.2% were in the National Guardor Reserves: 87.4% were in the Army, 9.1% Marines, 2.2% AirForce, and 1.3% multiple branches. Demographic characteristicsand scores on combat experience and psychosocial measuresby PTSD status are given in Table 1. The PTSD groupwas younger than the no PTSD group, but did not differ bysex, race/ethnicity, education, relationship status, and servicetype. They scored higher on the CES (large effect size), andlower on the postdeployment social support (large effect size)and unit support (medium effect size) measures.Mean PCL-M scores were 35.9 (SD = 18.0) for the fullsample, 64.3 (SD = 10.2) for respondents with PTSD, and 27.8(SD = 9.7) for respondents without PTSD. Mean PHQ-9scores were 7.3 (SD = 6.9) for the full sample, with respondentswith PTSD (M = 16.5, SD = 5.9) scoring higher than re-68Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
spondents without PTSD (M = 4.6, SD = 4.4; t = 16.96, P .17).DISCUSSIONTo our knowledge, this is one of the first studies ofOEF/OIF veterans to examine the relationship between protectivefactors such as psychological resilience and social support,and traumatic stress and depressive symptoms. Overall,OEF/OIF veterans reported a level of resilience consistent withcivilian outpatient primary-care patients, but veterans withPTSD reported lower levels of resilience and unit and postdeploymentsocial support compared to veterans without PTSD.Increased resilience and postdeployment social support werenegatively associated with severity of traumatic stress and depressivesymptoms, even after controlling for demographiccharacteristics and combat exposure severity.The mean resilience score in this sample of OEF/OIFveterans is consistent with that observed in primary-care patients.14 The mean score of the group without PTSD was betweenthat observed in the general population and primary-carePreviously Published 69
70Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
patients, whereas the mean score of the group with PTSD wasconsistent with that observed in civilian PTSD patients. 14These findings suggest that OEF/OIF veterans are quite resilientdespite having endured war. However, the PTSD groupscored more than one full standard deviation lower than the noPTSD group, suggesting that this group may be less hardy orresilient to stress, a finding consistent with previous reports. 14The most pronounced difference between the PTSD and noPTSD groups was on the CD-RISC subscale personal control,which assesses the extent to which an individual feels in controlof his or her life, knows where to turn for help, and has asense of purpose in their life. This finding corroborates previousreports showing that individuals with PTSD tend to havelower coping self-efficacy compared to individuals withoutPTSD. 21,22 Lower coping self-efficacy, in turn, has been linkedto greater distress, intrusion, and avoidance symptoms, 21 evenat 2 years posttrauma. 23 Veterans with PTSD in this study alsoscored lower on measures of unit support and postdeploymentsocial support, which is consistent with previous studiesdemonstrating moderate correlations between these measuresand PTSD symptoms. 15,16,20Higher resilience and postdeployment social supportscores were associated with decreased traumatic stress and depressivesymptoms, even after controlling for demographic factorsand combat exposure. The subscales personal control andacceptance of changes were the only two CD-RISC subscalesassociated with traumatic stress. This finding is consistent withBandura’s 24 social cognitive theory, which maintains that beliefsabout one’s capacity to manage and control events in lifeare important in determining behavioral and affective responsesto highly stressful situations. For example, in a study of 600sexual assault survivors, the only protective factor againstPTSD symptoms was survivors’ perception that they hadgreater control over the recovery process. 25 In a study of Israelirecruits, perceived control predicted positive changes in mentalhealth over the course of an intense 4-month combat trainingperiod, with these changes mediated by reduced appraisalof threat and the use of problem solving and support-seekingstrategies. 26 Individuals with high perceived control also tendto seek positive solutions to problems by using active ratherthan passive coping mechanisms, 27 which promotes greaterself-efficacy and decreases risk for PTSD. 28 Taken together,these findings underscore the importance of cognitive-behavioralinterventions that promote perceptions of control and selfefficacy,encourage positive appraisals and acceptance ofchange, and increase adaptive coping strategies in individualswith PTSD. 29 One example of such an intervention is wellbeingtherapy, which focuses on enhancing personal growth,purpose in life, autonomy, selfacceptance, and positive relationswith others, and has been shown to improve symptomsassociated with mood and anxiety disorders. 30 Postdeploymentsocial support was also negatively associated with traumaticstress and depressive symptoms, which suggests that efforts toenhance social support and help veterans learn how to seek outsocial support may be effective in reducing the negative impactof traumatic stress.It is likely that resilience and social support operate inconcert with one another to reduce the likelihood of developingtrauma-related psychopathology. A previous study of a nationallyrepresentative sample of 1,632 Vietnam veteranssimilarly found that hardiness and postwar social support werenegatively associated with PTSD symptoms and that functionalsocial support accounted for a substantial amount of theindirect effect of hardiness on PTSD. 4 This finding is consistentwith reports that individuals who are resilient to stresstend to be skilled at constructing social networks and seekingout social support in times of need. 4, 27, 31 Of note, in this study,the magnitude of the association between resilience and traumaticstress symptoms (β = –.34) was equal to that betweencombat exposure severity and traumatic stress symptoms (β =.34). This suggests that efforts to promote psychological resiliencemay help counteract the potentially deleterious effectof combat exposure on the development of traumatic stressand related symptoms.Psychological resilience and social support may beprotective against traumatic stress and depressive symptomsby improving emotional regulation, decreasing fear-related appraisalsand cognitions, promoting cognitions that the world issafe and nonthreatening, enhancing self-efficacy and control, 5and decreasing hypothalamic-pituitary-adrenal axis reactivity32–34 and stress-related physiological arousal. 35,36 Resilienceis also related to active task-oriented coping, 37 which may enhanceadaptation to stress by decreasing avoidance symptoms,behavioral withdrawal, and emotional disengagement. 5,38 Furtherresearch is needed to examine interrelationships amongthese biological factors, resilience, social support, and stressrelateddisorders.Methodological limitations of this study must benoted. First, the generalizability of these results may be limited,as the response rate to the survey was relatively low, respondentswere older than nonrespondents, only data on age ofnonrespondents were recorded, and the sample was ethnicallyand geographically homogeneous. The reasons for this lowresponse rate are not entirely clear, but may be related to thelength of the survey, which included more than 200 questions.Second, PTSD status was determined using a strict method,which required respondents to score >50 and meet B, C, andD criteria. Thus, when less strict methods of classification areused, individuals with PTSD will likely report higher levelsof resilience and/or social support. Third, only a select numberof measures of psychological resilience and social supportwere administered. Because these constructs are multidimensional,more research using a broader array of these types ofmeasures and employing analytic methods such as structuralequation modeling may be helpful in elucidating the complexinterrelationships among these variables. For example, onemay examine the possibility that more resilient individuals attractmore social support, which in turn decreases traumaticstress and depressive symptoms, and that individuals with increasedtraumatic stress and depressive symptoms may be lessresilient and in turn less able to garner postdeployment socialsupport. Fourth, the subscales of the CD-RISC in this studywere drawn from the original publication of this instrument,which derived these subscales using exploratory factor analysis.14 Confirmatory factor analytic studies are needed to examinethe factor structure of the CD-RISC and other measuresof resilience and social support in military samples. Finally,the cross-sectional nature of this study precluded examinationof the temporal association between resilience, social support,and PTSD/depressive symptoms. Longitudinal studies arePreviously Published 71
needed to examine whether resilience and support factors do infact protect PTSD/depressive symptoms or whether individualswith PTSD/depressive symptoms perceive themselves asless resilient and having less social support.Despite these limitations, this study is among the firstto examine adaptive aspects of recovery from combat and theimportance of resilience and social support in protectingagainst traumatic stress and depressive symptoms in OEF/OIFveterans. Given the low response rate to the survey employedin this study, future research should endeavor to replicate thesefindings in larger, more representative samples of OEF/OIFveterans as well as in other military and civilian populations,examine specific roles of protective factors in mitigating psychopathologyand functioning, and develop and test the efficacyof preventive and treatment interventions designed tobolster resilience and social support in veteran and othertrauma-exposed populations.ACKNOWLEDGMENTSWe thank the veterans who participated in this survey.We appreciate the assistance of the Center for Public Policyand Social Research at Central Connecticut State Universityand the Connecticut Department of Veterans’ Affairs in conductingthis research. This work was supported by a grantfrom the State of Connecticut, the National Center for PTSD,and a private donation.REFERENCES1. Milliken CS, Auchterlonie JL, Hoge CW. Longitudinal assessment ofmental health problems among active and reserve component Soldiersreturning from the Iraq war. J Am Med Assoc 2007;298:2141–2148.2. Hoge CW, Castro CA, Messer SC et al. Combat duty in Iraq andAfghanistan, mental health problems, and barriers to care. N Engl J Med2004;351:13–22.3. Hoge CW, Auchterlonie JL, Milliken CS. Mental health problems, useof mental health services, and attrition from military service after returningfrom deployment to Iraq or Afghanistan. J Am Med Assoc2006;295:1023–1032.4. King LA, King DW, Fairbank JA et al. Resilience-recovery factors inpost-traumatic stress disorder among female and male Vietnam veterans:Hardiness, postwar social support, and additional stressful lifeevents. J Pers Soc Psychol 1998;74:420–434.5. Charuvastra A, Cloitre M. Social bonds and posttraumatic stress disorder.Ann Rev Psychol 2008;59:301–328.6. Southwick SM, Vythilingam M, Charney DS. The psychobiology of depressionand resilience to stress: Implications for prevention and treatment.Ann Rev Clin Psychol 2005;1:255–291.7. Hoge EA, Austin ED, Pollack MH. Resilience: research evidence andconceptual considerations for posttraumatic stress disorder. DepressAnxiety 2007;24:139–152.8. Waysman M, Schwarzwald J, Solomon Z. Hardiness: An examinationof its relationship with positive and negative longterm changes followingtrauma. J Trauma Stress 2001;14:531–548.9. Bartone PT. Hardiness protects against war-related stress in ArmyReserve forces. Consult Psychol J 1999;51:72–82.10. Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factorsfor posttraumatic stress disorder in trauma-exposed adults. J ConsultClin Psychol 2000;68:748–766.11. Ozer EJ, Best SR, Lipsey TL, Weiss DS. Predictors of posttraumaticstress disorder and symptoms in adults: A metaanalysis. Psychol Bull2008;129:52–73.12. Engdahl B, Dikel TN, Eberly R, Blank Jr A. Posttraumatic stress disorderin a community group of former prisoners of war: A normativeresponse to severe trauma. Am J Psychiatry 1997;154:1576–1581.13. Kaspersen M, Matthiesen SB, Gotestam KG. Social network as a moderatorin the relation between trauma exposure and trauma reaction:A survey among UN soldiers and relief workers. Scand J Psychol2003;44:415–423.14. Connor KM, Davidson JR. Development of a new resilience scale:The Connor–Davidson Resilience Scale (CD-RISC). Depress Anxiety2003;18:76–82.15. King LA, King DW, Vogt DS et al. Deployment Risk and ResilienceInventory: A collection of measures for studying deployment-relatedexperiences of military personnel and veterans. Mil Psychol 2006;18:89–120.16. Vogt DS, Proctor SP, King DW et al. Validation of scales from the DeploymentRisk and Resilience Inventory in a sample of Operation IraqiFreedom veterans. Assessment 2008;15:391–403.17. Weathers F, Huska J, Keane T. The PTSD Checklist Military Version(PCL-M). Boston, MA: National Center for Posttraumatic StressDisorder, 1991.18. Kroenke K, Spitzer RL. The PHQ-9: A new depression diagnostic andseverity measure. Psychiatr Ann 2002;32:509–521.19. Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nded. New Jersey: Lawrence Erlbaum; 1988.20. Fikretoglu D, Brunet A, Poundja J et al. Validation of the DeploymentRisk and Resilience Inventory in French-Canadian veterans:Findings on the relation between deployment experiences and postdeploymenthealth. Can J Psychiatry 2006;51:755–763.21. Sumer N, Karanci AN, Berument SK, Gunes H. Personal resources,coping self-efficacy, and quake exposure as predictors of psychologicaldistress following the 1999 earthquake in Turkey. J Trauma Stress2005;18:331–342.22. Benight CC, Harper ML. Coping self-efficacy perceptions as a mediatorbetween acute stress response and long-term distress followingnatural disasters. J Trauma Stress 2002;15:177–186.23. Heinrichs M, Wagner D, Schoch W et al. Predicting posttraumaticstress symptoms from pretraumatic risk factors: A 2-year prospectivefollow-up study in firefighters. Am J Psychiatry2005;162:2276–2286.24. Bandura A. Social cognitive theory. In: Vasta R, ed. Annals of ChildDevelopment: 6. Six Theories of Child Development. Greenwich,CT: JAI Press; 1989: 1–60.25. Ullman SE, Filipas HH, Townsend SM, Starzynski LL. Psychosocialcorrelates of PTSD symptom severity in sexual assault survivors. JTrauma Stress 2007;20:821–831.26. Florian V, Mikulincer M, Taubman O. Does hardiness contribute tomental health during a stressful real-life situation? The roles of appraisaland coping. J Pers Soc Psychol 1995;68:687–695.27. Sharkansky EJ, King DW, King LA et al. Coping with Gulf War combatstress mediating and moderating effects. J Abnorm Psychol2000;109:188–197.28. Ginzburg K, Solomon Z, Kekel R, Neria Y. Battlefield functioningand chronic PTSD: Associations with perceived self-efficacy andcausal attribution. Pers Individ Diff 2003;34:463–476.72Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
29. Whealin JM, Ruzek JI, Southwick S. Cognitive-behavioral theory andpreparation for professionals at risk for trauma exposure. Trauma ViolenceAbuse 2008;9:100–113.30. Fava GA, Rafanelli C, Cazzaro M, Conti S, Grandi S.Well-being therapy.A novel psychotherapeutic approach for residual symptoms of affectivedisorders. Psychol Med 1998;28:475–480.31. Gribble PA, Cowen EL,Wyman PA et al. Parent and child views of parent–childrelationship qualities and resilient outcomes among urbanchildren. J Child Psychol Psychiatry 1993;34:507–519.32. Abelson JL, Khan S, Liberzon I et al. Effects of perceived control andcognitive coping on endocrine stress responses to pharmacological activation.Biol Psychiatry 2008;64:701–707.33. Kirschbaum C, Klauer T, Filipp SH, Hellhammer DH. Sex-specific effectsof social support on cortisol and subjective responses to acute psychologicalstress. Psychosom Med 1995;57:23–31.34. Rosal MC, King J, Ma Y, Reed GW. Stress, social support, and cortisol:Inverse associations? Behav Med 2004;30:11–21.35. Haglund ME, Nestadt PS, Cooper NS et al. Psychobiological mechanismsof resilience: Relevance to prevention and treatment of stress-relatedpsychopathology. Dev Psychopathol 2007;19:889–920.36. Ozbay F, Fitterling H, Charney D, Southwick S. Social support and resilienceto stress across the life span: A neurobiologic framework. CurrPsychiatry Rep 2008;10:304–310.37. Campbell-Sills L, Cohan SL, Stein MB. Relationship of resilience topersonality, coping, and psychiatric symptoms in young adults. BehavRes Ther 2006;44:585–599.38. Tiet QQ, Rosen C, Cavella S et al. Coping, symptoms, and functioningoutcomes of patients with posttraumatic stress disorder. J Trauma Stress2006;19:799–811.AUTHORS1. Department of Psychiatry, Yale University School of Medicine,New Haven, Connecticut2. National Center for Posttraumatic Stress Disorder, VA ConnecticutHealthcare System, West Haven, Connecticut3. Naval Center for Combat Operational Stress Control, and Departmentof Psychiatry, University of California San DiegoSchool of Medicine, San Diego, California4. Department of Psychology, Central Connecticut State University,New Britain, Connecticut5. Department of Counseling and Family Therapy, Central ConnecticutState University, New Britain, ConnecticutPreviously Published 73
PSYCHOSOCIAL BUFFERS OF TRAUMATIC STRESS, DEPRESSIVE SYMPTOMS, ANDPSYCHOSOCIAL DIFFICULTIES IN VETERANS OF OPERATIONS ENDURING FREEDOMAND IRAQI FREEDOM: : T HE ROLE OF RESILIENCE, UNIT SUPPORT,AND POSTDEPLOYMENT SOCIAL SUPPORTRobert H. Pietrzak a,b,* , Douglas C. Johnson c , Marc B. Goldstein d , James C. Malley e ,Alison J. Rivers a,b , Charles A. Morgan a,b , Steven M. Southwick a,bPreviously published in the Journal of Affective Disorders, (2009), doi:10.1016/j.jad.2009.04.015. Permission granted to republishin the JSOM.ABSTRACTBackground: Little research has examined the role of protective factors such as psychological resilience, unit support, andpostdeployment social support in buffering against PTSD and depressive symptoms, and psychosocial difficulties in veteransof <strong>Operations</strong> Enduring Freedom (OEF) and Iraqi Freedom (OIF). Materials and methods: A total of 272 OEF/OIF veteranscompleted a survey containing PTSD and depression screening measures, and questionnaires assessing resilience,social support, and psychosocial functioning. Results: Lower unit support and postdeployment social support were associatedwith increased PTSD and depressive symptoms, and decreased resilience and psychosocial functioning. Path analysessuggested that resilience fully mediated the association between unit support and PTSD and depressive symptoms, and thatpostdeployment social support partially mediated the association between PTSD and depressive symptoms and psychosocialfunctioning. Limitations: Generalizability of results is limited by the relatively low response rate and predominantly olderand reserve/National Guard sample. Conclusions: These results suggest that interventions designed to bolster unit support,resilience, and postdeployment support may help protect against traumatic stress and depressive symptoms, and improvepsychosocial functioning in veterans.1.INTRODUCTIONEpidemiologic surveys of Operation Iraqi Freedom(OIF)and Operation Enduring Freedom (OEF) veteranshave found high rates of posttraumatic stress disorder(PTSD), depression, and related conditions (Tanielian andJaycox, 2008). While it is well known that these conditionsmay negatively affect psychosocial functioning and quality oflife in this population (e.g., Milliken et al., 2007), little researchhas examined the role of protective factors such aspsychological resilience, unit support, and postdeploymentsocial support in buffering against PTSD and depressivesymptoms, and psychosocial difficulties.Psychological resilience, which refers to an individual’scapacity to successfully adapt or change in the face ofadversity, protects against the development of combat-relatedPTSD in Vietnam veterans (King et al., 1998;Waysman et al.,2001) and Army Reserve Soldiers (Bartone, 1999). Aspectsof resilience such as positive emotions, cognitive flexibility,meaning making, and active coping also protect against thedeleterious effects of depression (Southwick et al., 2005).Social support also protects against depression(Paykel, 1994; Southwick et al., 2005), and PTSD, withmeta-analyses suggesting that it is among the strongest negativepredictors of PTSD (Oliver et al., 1999; Brewin et al.,2000; Ozer et al., 2008). Higher perceived social support hasalso been linked to increased resilience (Bonanno et al.,2007) and lower risk of PTSD in Vietnam veterans (King etal., 1998), prisoners of war (Engdahl et al., 1997) and <strong>United</strong>Nations soldiers (Kaspersen et al., 2003). An understandingof associations between resilience, social support, PTSD anddepressive symptoms, and functioning in OEF/OIF veteransis important, as it may help guide the development of interventionsto enhance resilience and support, and promote successfulreadjustment to civilian life after deployment.This study examined associations between resilience,unit support, postdeployment social support, traumaticstress and depressive symptoms, and psychosocialfunctioning two years following return from deployment ina sample of OEF/OIF veterans. Path analyses tested the hypothesesthat unit support may help enhance psychologicalresilience (Bartone, 2006; Oliver et al., 1999), which in turnreduces PTSD and depressive symptom severity, and thatpostdeployment social support may mediate the relationshipbetween PTSD and depressive symptoms and psychosocialdifficulties (Oxman and Hull, 2001; Zatzick et al., 1997). Wehypothesized that resilience would mediate the relationshipbetween unit support and PTSD and depressive symptoms,and that postdeployment social support would mediate therelationship between PTSD and depressive symptoms andpsychosocial difficulties.2. METHODS2.1. SampleParticipants (N=272) completed the ConnecticutOEF/OIF Veterans Needs Assessment Survey. OEF/OIF veteranswere identified alphabetically from a review of copiesof discharge papers (DD-214s) by the Connecticut Departmentof Veterans’Affairs until names and addresses of 1000potential respondents were obtained. To maintain confidentiality,surveys were addressed and mailed by the ConnecticutDepartment of Veterans’Affairs. No personal identifyinginformation was made available to the authors. The surveywas mailed in October 2007 to a sample of 1000 veteranswho had served between 1/1/03 and 3/1/07; as of 2/08, 285surveys were returned for an overall return rate of 28.5%.Respondents were older than non-respondents in the samplingframe (33.4 vs. 31.3 years, t(998)=2.87, p =.004). On74Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
average, time between return from deployment to OEF/OIFand survey completion was 26.9±.7 months.2.2. Assessment instrumentsThe Unit Support Scale (USS) is a self-report measurefrom the Deployment Risk and Resilience Inventory(DRRI; King et al., 2006) that assesses the quality of relationshipsand degree of cohesion between a Soldier andhis/her unit. Cronbach’s α=.93.The Postdeployment Social Support Scale is a selfreportmeasure from the DRRI that assesses the extent towhich family, friends, coworkers, employers, and communityprovide postdeployment emotional support and instrumentalassistance. Cronbach’s α=.82.The Connor–Davidson Resilience Scale (Connor andDavidson, 2003) is a self-report measure of psychological resilience.Higher scores reflect greater resilience. Cronbach’sα=.94.The Combat Experiences Scale (CES) is a self-reportinstrument from the DRRI that assesses exposure tocombat (e.g., firing a weapon, witnessing injury and death).Higher scores reflect more combat exposure. Cronbach’sα=.93.The Posttraumatic Stress Disorder Checklist-MilitaryVersion (PCL-M; Weathers et al., 1991) is a 17-item instrumentbased on DSM-IV criteria for PTSD. Higher scoresindicate greater posttraumatic stress symptoms. Cronbach’sα=.96.The Patient Health Questionnaire-9 (Kroenke andSpitzer, 2002) is a 9-item self-report screening instrument fordepression derived from the clinician-administered PrimaryCare Evaluation of Mental Disorders. Higher scores indicategreater depressive symptoms. Cronbach’s α=.92.The Psychosocial Difficulties Scale (PDS) is a 23-item questionnaire developed by two of the authors (M.B.G.,J.C.M.) that assesses psychosocial functioning in family andpeer relationships (e.g., “have difficulty connecting emotionallywith family and/or friends”), and work, school, andfinancial functioning (e.g., “have difficulty finding employment”;“have difficulty paying bills”). Ratings are “Not aconcern”, “A slight concern”, “A moderate concern”, and “Amajor concern”. Higher scores indicate greater psychosocialdifficulties. Cronbach’s α=.89.2.3. Data analysisNon-normally distributed data (e.g., PCL-M scores)were transformed using logarithmic base 10 transformations.Pearson correlations were computed between measures of socialsupport and resilience, PTSD and depressive symptoms,and psychosocial difficulties. Path analyses were conductedto test the hypotheses that resilience mediates the relationshipbetween unit support and PTSD and depressive symptoms;and that postdeployment social support mediates therelationship between PTSD and depressive symptoms andpsychosocial difficulties. Data from all respondents were includedin these analyses, including those with and withoutpositive screens for PTSD and depression. Model fit wasevaluated using a number of fit statistics, including χ2, rootmean square error of approximation (RMSEA), comparativefit index (CFI), and Tucker–Lewis Index (TLI). By convention,lower, non-significant χ2 values, RMSEA values ≤.08,and CFI and TLI values ≥.90 indicate acceptable model fit(Kline, 2005). Path coefficients are presented as standardizedregression weights (β).3. RESULTSThe mean age of the total sample was 34.9±.4 years,89% were white, 82% completed at least some college education,the majority (72%) were in the National Guard or reservesand 28% were on active duty; 87% were in the Army,9% Marines, 2% Air Force, and 2% multiple branches.Table 1 shows mean scores and standard errors, andcorrelations between all measures. Unit support scores correlatedwith scores on all other variables except combat exposureand psychosocial difficulties. Postdeployment socialsupport scores correlated positively with resilience scores andnegatively with scores on all other variables. Resiliencescores correlated negatively with measures of PTSD and depressivesymptoms, and psychosocial difficulties, but theywere not associated with combat exposure. Combat exposurescores correlated negatively with postdeployment socialsupport scores and positively with measures of PTSD and depressivesymptoms, and psychosocial difficulties. PTSD anddepressive symptoms correlated positively with scores on ameasure of psychosocial difficulties.Previously Published 75
Fig. 1 shows the final path models, both of which hada good fit: PTSD symptom model: χ2(7)=4.78, p=.69;RMSEA=.00, CFI=1.00, TLI=1.00; Depressive symptommodel: χ2(7)=5.86, p=.12; RMSEA=.04; CFI=.99; TLI=.96.All paths in the final models were statistically significant (allp’sb.001). In the just-identified models (i.e., perfect fit todata with paths between all variables), the paths between unitsupport and PTSD and depressive symptoms, combat exposureand unit support, resilience, and functioning, and resilienceand functioning were not significant (all β’s < .06, allp’s > .26); accordingly, these paths were removed from thefinal models. As shown in Fig. 1, resilience fully mediated therelationship between unit support and both PTSD and depressivesymptoms; unit support also predicted increasedpostdeployment social support. Combat exposure was associatedwith increased PTSD symptoms, resilience with increasedpostdeployment social support, and PTSD anddepressive symptoms with greater psychosocial difficulties.Postdeployment social support partially mediated the associationbetween PTSD and depressive symptoms and psychosocialdifficulties.4. DISCUSSIONThis study examined the role of protective factorssuch as resilience and social support in protecting against traumaticstress and depressive symptoms, and psychosocial difficultiesin OEF/OIF veterans. Results suggested thatresilience, unit support, and postdeployment social supportserve as psychosocial buffers of PTSD and depressive symptoms,and psychosocial difficulties at 2 years after deployment.Resilience fully mediated the relationship betweenunit support and PTSD and depressive symptoms. Previousresearch on resilience similarly found that social support is associatedwith increased resilience (Bonanno et al., 2007;Oliver et al., 1999) and lower risk of PTSD in military samples(King et al., 1998; Engdahl et al., 1997; Kaspersen et al.,2003). This finding suggests that high levels of perceived unitsupport were associated with increased resilience, which inturn is associated with decreased PTSD and depressive symptoms.Unit support may enhance resilience by promoting feelingsof personal control and self-efficacy, which may fosterthe development of active coping styles and increased abilityto reappraise stressful situations (Sumer et al., 2005; Benightand Harper 2002; Southwick et al., 2005; Bartone, 2006). Unitsupport may also bolster resilience by promoting meaningmakingin the face of stressful experiences (Cole et al., 2006).While more research is needed to tease apart the temporal relationshipbetween unit support and resilience (i.e., does unitsupport lead to increased resilience or do more resilient peopleattract more unit support?), this finding highlights the importanceof unit support and resilience in protecting againstPTSD and depressive symptoms in OEF/OIF veterans.Postdeployment social support partially mediated therelationship between PTSD and depressive symptoms and psychosocialdifficulties. This finding replicates previous researchdemonstrating the protective role of social support in preserv-76Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
ing functioning in both PTSD (Zatzick et al., 1997) and depression(Taylor, 2004; Oxman and Hull, 2001). It also suggeststhat providing early social support may reduce thedocumented postdeployment increase in PTSD symptoms andcomorbid conditions for OEF/OIF veterans (Milliken et al.,2007). Social support may enhance functioning by fosteringeffective coping strategies (Holahan et al., 1995), reducinginvolvement in high-risk behaviors or avoidance coping(Muris et al., 2001), promoting self-efficacy (Hays et al.,2001), and reducing loneliness (Bisschop et al., 2004). Resilienceand social support likely operate synergistically todecrease the likelihood of developing PTSD and depression.Indeed, a study of a nationally representative sample of 1632Vietnam veterans found that both hardiness, an aspect of resilience,and postwar social support were negatively associatedwith PTSD symptoms, and that social support accountedfor a substantial amount of the indirect effect of hardiness onPTSD (King et al., 1998).The finding that increased resilience was associatedwith increased postdeployment social support also corroboratesprevious research, which found that resilient individualstend to be skilled at constructing social networks and seekingout social support in times of need (Sharkansky et al., 2000).Resilience and social support may also protect against PTSDand depressive symptoms and enhance functioning by decreasinghypothalamic–pituitary–adrenal (HPA) axis reactivityand stress-related physiological arousal (Heinrichs et al.,2003; Southwick et al., 2005). They may also promote activetask-oriented coping (Campbell-Sills et al., 2006), which enhancesadaptation to stress by decreasing avoidance symptoms,behavioral withdrawal, and emotional disengagement(Southwick et al., 2005; Tiet et al., 2006).Methodological limitations of this study must benoted. First, given the relatively low response rate to the survey,generalizability of the findings may be limited. Nevertheless,demographic, deployment, and clinical characteristicsof survey respondents in the current study were generallycomparable to those of a nationally representative sample ofOEF/OIF veterans (Tanielian and Jaycox, 2008), though thecurrent survey sample consisted of older, and predominantlywhite and Army Reserve/National Guard veterans, so resultsare likely best generalized to this population. Second, self reportscreening instruments were used to assess PTSD and depressionsymptoms. Whether these results are generalizableto larger, predominantly active duty, and/or more diverse samplesof OEF/OIF veterans when formal clinical interviewsand diagnostic instruments are utilized remains to be examined.Finally, due to the cross-sectional design of this study,we were unable to examine temporal relationships among thevariables assessed. More research is needed to examine theinterrelationships among these variables with respect to deployment.For example, it is not clear whether unit supportenhances resilience or if resilient individuals are better able toattract unit support. Future research should also employ abroader array of biological and psychosocial measures, includingmeasures of successful adjustment, in examining predictorsof psychological symptoms/disorders and functioning,and evaluate the utility of interventions designed to bolsterunit support, resilience, and postdeployment social support inimproving readjustment to civilian life in OEF/OIF veteransand other trauma-exposed populations.ROLE OF FUNDING SOURCENone of these funding sources had a role in study design; in thecollection, analysis and interpretation of data; in the writing of thereport; or in the decision to submit the paper for publication.CONFLICT OF INTERESTNone of the authors have any conflicts of interest.ACKNOWLEDGEMENTSWe thank the veterans who participated in this survey. We appreciatethe assistance of the Center for Public Policy and Social Researchat Central Connecticut State University and the ConnecticutDepartment of Veterans’ Affairs in conducting this research. Thiswork was supported by a grant from the State of Connecticut, Departmentof Mental Health and Addiction Services, the NationalCenter for PTSD, and a private gift.REFERENCESBartone, P.T., 1999. Hardiness protects against war-related stress in ArmyReserve forces. Consult Psychol J. 51, 72–82.Bartone, P.T., 2006. Resilience under military operational stress: Canleaders influence hardiness? Mil Psychol 18 (Suppl), S131–S148.Benight, C.C., Harper, M.L., 2002. Coping self-efficacy perceptions as amediator between acute stress response and long-term distress followingnatural disasters. J Trauma Stress 15, 177–186.Bisschop, M.I., Kriegsman, D.M.W., Beekman, A.T.F., Deeg, D.J.H., 2004.Chronic diseases and depression: The modifying role of psychosocialresources. Soc Sci Med 4, 721–733.Bonanno, G.A., Galea, S., Bucciarelli, A., Vlahov, D., 2007. What predictspsychological resilience after disaster? The role of demographics, resources,and life stress. J Consult Clin Psychol 75, 671–682.Brewin, C.R., Andrews, B., Valentine, J.D., 2000. Meta-analysis of riskfactors for posttraumatic stress disorder in trauma-exposed adults.J Consult Clin Psychol 68, 748–766.Campbell-Sills, L., Cohan, S.L., Stein, M.B., 2006. Relationship ofresilience to personality, coping, and psychiatric symptoms in youngadults. Behav Res Ther 44, 585–599.Cole, M., Bruch, H., Vogel, B., 2006. Emotions as mediators betweenperceived supervisor support and psychological hardiness on employeecynicism. J Organ Behav 27, 463–484.Connor, K.M., Davidson, J.R., 2003. Development of a new resiliencescale: The Connor-Davidson Resilience Scale (CD-RISC). DepressAnxiety 18, 76–82.Engdahl, B., Dikel, T.N., Eberly, R., Blank Jr., A., 1997. Posttraumaticstress disorder in a community group of former prisoners of war: Anormative response to severe trauma. Am J Psychiatry. 154, 1576–1581.Hays, J.C., Steffens, D.C., Flint, E.P., Bosworth, H.B., George, L.K., 2001.Does social support buffer functional decline in elderly patients withunipolar depression? Am J Psychiatry. 158, 1850–1855.Holahan, C.J., Moos, R.H., Holahan, C.K., Brennan, P.L., 1995. Socialsupport, coping, and depressive symptoms in a late-middle-aged sampleof patients reporting cardiac illness. Health Psychol. 14, 152–163.Heinrichs, M., Baumgartner, T., Kirschbaum, C., Ehlert, U., 2003. Socialsupport and oxytocin interact to suppress cortisol and subjective responsesto psychosocial stress. Biol Psychiatry. 54, 1389–1398.Previously Published 77
Kaspersen, M., Matthiesen, S.B., Gotestam, K.G., 2003. Social networkas a moderator in the relation between trauma exposure and trauma reaction:A survey among UN soldiers and relief workers. Scand J Psychol.44, 415–423.King, L.A., King, D.W., Fairbank, J.A., Keane, T.M., Adams, G.A., 1998.Resilience-recovery factors in post-traumatic stress disorder among femaleand male Vietnam veterans: Hardiness, postwar social support, andadditional stressful life events. J Pers Soc Psychol. 74, 420–434.King, L.A., King, D.W., Vogt, D.S., Knight, J.A., et al., 2006. DeploymentRisk and Resilience Inventory: A collection of measures for studyingdeployment related experiences of military personnel and veterans.Mil Psychol. 18, 89–120.Kline, R.B., 2005. Principles and Practice of Structural Equation Modeling,2nd ed. The Guilford Press, New York, NY.Kroenke, K., Spitzer, R.L., 2002. The PHQ-9: A new depression diagnosticand severity measure. Psychiatry Ann 32, 509–521.Milliken, C.S., Auchterlonie, J.L., Hoge, C.W., 2007. Longitudinal assessmentof mental health problems among active and reserve componentSoldiers returning from the Iraq war. JAMA. 2298, 2141–2148.Muris, P., Schmidt, H., Lambrichs, R., Meesters, C., 2001. Protective andvulnerability factors of depression in normal adolescents. Behav ResTher. 39, 555–565.Oliver, L.W., Harman, J., Hoover, E., Hayes, S.M., Pandhi, N.A., 1999. Aquantitative integration of the military cohesion literature. Mil Psychol.11, 57–83.Oxman, T.E., Hull, J.G., 2001. Social support and treatment response inolder depressed primary care patients. J Gerontol Psychol Sci. 56, 35–45.Ozer, E.J., Best, S.R., Lipsey, T.L.,Weiss, D.S., 2008. Predictors of posttraumatic stress disorder and symptoms in adults: A meta-analysis. PsycholBull. 129, 52–73.Paykel, E.S., 1994. Life events, social support and depression. Acta PsychiatrScand. 377 (Suppl), 50–58.Sharkansky, E.J., King, D.W., King, L.A., Wolfe, J., Erickson, D.J., Stokes,L.R., 2000. Coping with Gulf War combat stress: Mediating and moderatingeffects. J Abnorm Psychol. 109, 188–197.Southwick, S.M., Vythilingam, M., Charney, D.S., 2005. The psychobiologyof depression and resilience to stress: Implications for prevention andtreatment. Ann Rev Clin Psychol 1, 255–291.Sumer, N., Karanci, A.N., Berument, S.K., Gunes, H., 2005. Personal resources,coping self-efficacy, and quake exposure as predictors of psychologicaldistress following the 1999 earthquake in Turkey. J TraumaStress. 18, 331–342.Tanielian, T., Jaycox, L.H., 2008. Invisible wounds of war: Psychologicaland cognitive injuries, their consequences, and services to assist recovery.The RAND Center for Military Health Policy Research, SantaMonica, CA.Tiet, Q.Q., Rosen, C., Cavella, S., Moos, R.H., Finney, J.W., Yesavage, J.,2006. Coping, symptoms, and functioning outcomes of patients withposttraumatic stress disorder. J Trauma Stress. 19, 799–811.Waysman, M., Schwarzwald, J., Solomon, Z., 2001. Hardiness: An examinationof its relationship with positive and negative long-term changesfollowing trauma. J Trauma Stress. 14, 531–548.Weathers, F., Huska, J., Keane, T., 1991. The PTSD Checklist MilitaryVersion (PCL-M). National Center for Posttraumatic Stress Disorder,Boston, MA.Zatzick, D.F., Marmar, C.R.,Weiss, D.S., Browner,W.S.,Metzler, T.J.,Golding, J.M., Stewart, A., Schlenger,W.E.,Wells, K.B., 1997. Posttraumatic stress disorder and functioning and quality of life outcomesin a nationally representative sample of male Vietnam veterans. Am JPsychiatry. 154, 1690–1695.AUTHORSa. National Center for Posttraumatic Stress Disorder, VA ConnecticutHealthcare System, West Haven, CT, USAb. Department of Psychiatry, Yale University School of Medicine,New Haven, CT, USAc. Naval Center for Combat and Operational Stress Control,Naval Medical Center and Department of Psychiatry, Universityof California San Diego School of Medicine, San Diego,CA, USAd. Department of Psychology, Central Connecticut State University,New Britain, CT, USAe. Department of Counseling and Family Therapy, Central ConnecticutState University, New Britain, CT, USA* Corresponding author — Department of Psychiatry, Yale UniversitySchool of Medicine, National Center for PTSD, VA ConnecticutHealthcare System, 950 Campbell Avenue/151E, WestHaven, CT 06510, USA. Tel.: +1 860 638 7467; fax: +1 203 9373481.E-mail address: robert.pietrzak@yale.edu (R.H. Pietrzak).78Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
Editorial Comment on “Psychological Resilience and Postdeployment Social SupportProtect Against Traumatic Stress and Depressive Symptoms in Soldiers Returning from<strong>Operations</strong> Enduring Freedom and Iraqi Freedom”Depression and Anxiety (Pietrzak et al., 2009a).LTC Craig A. Myatt, PhD; Douglas C. Johnson, PhD(The referred article can be read in this edition’s Previously Published section.)Pietrzak et al. (2009a) used a cross-sectional methodologicalapproach to support the premise that increased resilienceand adequate social support protect against thepotentially deleterious effects of traumatic stress. The emergingconcern about behavioral health in servicemembers servingin <strong>Operations</strong> Enduring Freedom and Iraqi Freedom(OEF/OIF) has prompted a wave of research that is now almosta 10 years in the making. Several studies introduced inthe literature during that time examined post-traumatic stressdisorder (PTSD), depression, and related psychopathologicalproblems. However, prior to the Pietrzak et al. (2009a) study,no known research in OEF/OIF veterans examined variablesthat may confer protection against traumatic stress and depressivesymptoms. Their study demonstrated that two keyvariables which appear to confer protection are psychologicalresilience and perceived social support.Pietrzak et al. (2009a) hypothesized that OEF/OIFveterans with PTSD would score lower on measures of resilienceand social support than veterans without PTSD.Their hypothesis also stated that increased resilience and socialsupport would be negatively associated with severity oftraumatic stress and depressive symptoms. They used thePost-traumatic Stress Disorder Checklist – Military Version(PCL-M) to measure PTSD and the Connor-Davidson ResilienceScale (CD-RISC) to measure psychological resiliencein a battery of self-report assessments that alsoexamined combat experiences, depressive symptoms, unitsupport, and post-deployment social support. The researchersestablished a cut-off score on the PCL-M to identify veteranswith PTSD. Among the 272 Active and Reserve componentveterans from all services who participated in the study asvolunteer respondents from the state of Connecticut, those inthe PTSD group scored lower on the CD-RISC (less resilience)than those in the no-PTSD group. In addition, regressionanalysis techniques suggested that scores measuringpsychological resilience on the CD-RISC and post deploymentsocial support were negatively associated with PTSDand depressive symptoms.The authors of the study adequately addressed thelimitations in their study, one of which involved the crosssectionalnature of the study. The cross-sectional study provideda “snap-shot” in time on the behavioral health ofOEF/OIF veterans. They addressed this limitation by emphasizingthe need for longitudinal studies that examine therole of resilience and support factors over time. Pietrzak etal., (2009a) convincingly conclude that resilience and socialsupport may be protective against traumatic stress and depressivesymptoms by a host of mechanisms. Those mechanismsinclude: decreased hypothalamic-pituitary-adrenal axisreactivity, decreased stress related physiological arousal, decreasedfear-related appraisals and cognitions, improvedemotional regulation, and enhanced self-efficacy and control.Several of those mechanisms shed light on the importance ofadopting a biopsychosocial perspective in the considerationof future research and applications.Editorial 79
Editorial Comment on “Psychosocial Buffers of Traumatic Stress, Depressive Symptoms,and Psychosocial Difficulties in Veterans of <strong>Operations</strong> Enduring Freedom and IraqiFreedom: The Role of Resilience, Unit Support, and Post-Deployment Social Support”Journal of Affective Disorders (Pietrzak et al., 2009b).LTC Craig A. Myatt, PhD; Douglas C. Johnson, PhD(The referred article can be read in this edition’s Previously Published section.)Resilience and social support appear to operate synergisticallylowering the likelihood of developing posttraumaticstress disorder (PTSD) and depression, according to Pietrzak etal., (2009b). Their recent findings demonstrate that two keyvariables which appear to confer protection are psychologicalresilience and perceived social support. Pietrzak et al., (2009b)generated a two-part hypothesis stating, “… Resilience wouldmediate the relationship between unit support and PTSD anddepressive symptoms, and that post-deployment social supportwould mediate the relationship between PTSD and depressivesymptoms and psychosocial difficulties.” Resilience, unit support,PTSD, depressive symptoms, post-deployment social support,and psychosocial difficulties served as the six key factorsin their hypothesis.At approximately two years post-deployment for allparticipants, Pietrzak et al., (2009b) used the Connor-DavidsonResilience Scale (CD-RISC) to measure psychological resilience,the Unit Support Scale taken from the DeploymentRisk and Resilience Inventory to measure unit support, the PosttraumaticStress Disorder Checklist – Military Version (PCL-M) to measure PTSD, and the Patient Health Questionnaire-nineto measure depressive symptoms. The Post-deployment SocialSupport Scale measured social support following redeploymentto home station duties and responsibilities, while the PsychosocialDifficulties Scale measured psychosocial functioning withfamily, peers, work, school, and finances. The Combat ExperiencesScale (CES) was also used in the battery of self-report instrumentsto assess combat exposure.Pietrzak et al., (2009b) obtained 272 Active and Reservecomponent veterans from all services as volunteer participantsfrom the state of Connecticut after initial screening for1000 potential volunteers among respondents to the ConnecticutOEF/OIF Veterans Needs Assessment Survey. FollowingPCL-M score, logarithmic base 10 transformations for PTSDdata that showed a non-normal distribution, Pietrzak et al.(2009b) computed Pearson correlations between measures ofresilience, unit support, PTSD, depressive symptoms, post-deploymentsocial support, psychosocial difficulties, and combatexposure. Path analyses demonstrated that increased resiliencewas associated with less PTSD and fewer depressive symptoms,while increased post-deployment social support was associatedwith less PTSD and fewer depressive symptoms. Combat exposurescores correlated positively with measures of PTSD, depressivesymptoms, and psychosocial difficulties, but correlatednegatively with scores on post-deployment social support.The findings of the Pietrzak et al. (2009b) study in theJournal of Affective Disorders demonstrate that resilience andsocial support lower the likelihood of developing PTSD and depressivesymptoms in service members at two years post-deployment.Their conclusions suggest that resilience, unitsupport and other forms of social support (i.e., Family, peer, andfinancial) confer a synergistic protective role in service members.While the current study did not explore the synergistic relationshipbetween resilience and social support in the Familymembers of the post-deployment veterans, its findings and conclusionsoffer compelling reasons for including Family membersin the broader scope of research and applications. Finally,since hardiness as an aspect of resilience is negatively associatedwith PTSD symptoms (to include depressive behavior), thefindings on combat exposure appear inconclusive. The reportedcombat exposure findings, nevertheless, provide a stimulatingprospect for future study in demographically diverse groups thatshow high-versus low-hardiness and high-versus low-resilience.LTC Craig A. Myatt is currently assigned to the U.S. <strong>Special</strong> <strong>Operations</strong> <strong>Command</strong> as the <strong>Command</strong> Psychologist. He earned his Ph.D.in Health Psychology at Walden University with a two-year pre-doctoral fellowship in the Neuropsychology Section, Department ofNeuro-Oncology, at the University of Texas M.D. Anderson Cancer Center. His previous assignments include command of the 145thMedical Logistics Bn; command of Delta Comp, 232d Medical Bn; and medical platoon leader for the 2/11th Armored Cavalry Reg andthe 1-52d Infantry (Mechanized). His staff officer assignments include deputy G-4 for Task Force 3 Medical <strong>Command</strong> (Iraq); observercontrollerand trainer in Task Force Bravo, 1st Brigade, 75th Division (Training Support); executive officer of the 10th Bn, 5th MedicalBrigade; assistant S-3 and S-6 in the 228th Combat Support Hospital; biomedical information systems course developer in the Center forHealthcare Education and Studies at the U.S. Army Medical Department Center and School; and biomedical information systems officerin the Office of the Deputy Chief of Staff for Information Management at the <strong>United</strong> <strong>States</strong> Army Medical <strong>Command</strong>.Douglas C. Johnson is the Department Head for Research Facilitation at the Naval Center for Combat Operational Stress Control (NC-COSC), and is currently Asst. Professor in Psychiatry at the University of California-San Diego (UCSD) School of Medicine. He earnedhis Ph.D. in clinical and cognitive psychology at the University of California-Los Angeles (UCLA), followed by two-years of post-doctoraltraining at Yale University School of Medicine and the Clinical Neurosciences Division of the National Center for PTSD. Dr. Johnsonis a former counter-terrorism analyst with the FBI and in 2006 was selected as the American Psychological Association (APA)<strong>Summer</strong> Research Fellow in Counterintelligence. Prior to graduate training Dr. Johnson served 10-years on active duty, as both enlistedand officer, in the U.S. Coast Guard, and is a 1993 graduate of the U.S. Coast Guard Academy.80Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
Blackburn’s HeadhuntersPhilip Harkins.New York: W.W. Norton & Company, Inc., 1955. ISBN-10 1299651186, hardcover, 326 pages.Reviewed by MAJ Pete Franco, MSCBlackburn’s Headhunters is the true story ofDonald Blackburn. Blackburn was the Army Officermost responsible for pioneering guerilla warfare and insurgencyoperations in the Philippines after the Japaneseinvasion during WWII. The time span of this book runsfrom around the fall of Bataan to the liberation on VJ Day(approximately 1942-1945). Most of the book deals withBlackburn’s training and integration of native Igorat andIfugao Filipino tribes along with the training of regularFilipino soldiers and American Soldiers. The accountstarts as a narrative but then transitions to excerpts fromBlackburn’s reports and diaries throughout the secondhalf of the book.The book begins with then 1LT Blackburn’s arrivalto the Philippine AOR on orders to train a section ofthe Philippine Army, the 12th Filipino Infantry Regiment.He was assigned with MAJ Russell Volckmann who togetherhad responsibility for the 11th Filipino InfantryRegiment. Both Backburn and Voalckmann employedstrong, early attempts to empower the Filipino Army;however, they failed to muster an initial force that couldcombat the Japanese. The book clearly illustrated thePhilippine Army’s lack of training, equipment, and theiralmost immediate collapse. Skillfully, Blackburn wasable to escape from the Japanese. The quick collapse ofthe Filipino Regular Army forces propelled Blackburninto beginning a fight “unconventionally.”The account focuses heavily on the unconventionalGW fight for the majority of the rest of the book.After realizing the initial superiority of the JapaneseArmy, the U.S. command gave 1LT Blackburn and MAJVolckmann orders to peacefully surrender; however, theydid not! (Hence the title of the later Hollywood accountof this book “Surrender – Hell!”) Instead they immediatelycontacted the higher Philippine Army command toassist them in their resistance. They went on to furtherrecommend the formation of an insurgency and the creationof a guerilla army. The Philippine <strong>Command</strong>agreed, however they were not up to the task. They partiallymobilized and joined the resistance but were extremelylimited in most areas. They also fell prey toJapanese fear tactics and extreme torture methods employedon all Filipinos’ creating ANY form of resistance.1LT Blackburn and MAJ Volkmann took on the task tocreate the insurgency and the guerilla army.The author, Philip Harkin, skillfully used Blackburn’smemoirs and records to re-create the portrayal ofhis guerilla warfare training and operations in the Philippines.1LT Blackburn, along with MAJ Volckmann, tookBook Review 81
on, of their own accord, the task to build this force. Thebook shows the difficulty that they encountered at everystep, and in every sense. Their frustration was apparent,even in the initial screening of the varied groups of Filipinos.Some were ready to fight, but many wanted tojust sit by and watch and remain uncommitted to eitherside. The uncommitted ones became known as the“fence-sitters.” Next, and most importantly, the bookbrings out the importance for them to meld with and gainthe Filipinos’ trust. Although extremely difficult, Blackburnemployed local tribes to include Ilocano and Fuegonative headhunters to create the bulk of his guerilla army,hence the name “Blackburn’s Headhunters.” The successof the native forces, along with his own survival,was in direct proportion to the degree that he integratedand empowered them.Throughout the book, Blackburn’s accountsshowed the brutal Japanese treatment of the Filipinoswho resisted, and often equally brutal treatment even tothose who did not resist. He described methods of torturethat without question equal and top the most heinous andevil anywhere, at any time. The fact that the guerillaforce kept going in the face of the risk of torture showedthe level of trust that Blackburn had earned. Blackburn’seffectiveness, integrity, and leadership grew throughoutthe continued training and employment of the nativeguerilla army.The medical significance of this book is minimal.There were plenty of medical issues and concernsin the Philippines during WW II, but most of the medicalchallenges and issues have been better documentedand written about elsewhere. In short, there was practicallyno medical capability present in the PhilippineArmy, and the U.S. Army medical capability was verylimited outside of the major cities and few major militarybases. Among the biggest medical problem in thePhilippines was dysentery. It ran rampant in many areasof the Philippines – especially in the central jungle areas,which was where Blackburn spent most of his time traininghis force. The author also refers often to the manyother intestinal tract diseases and parasites that produceda drain on his men, to include nausea, diarrhea, fever, anddehydration. Mosquitoes and leeches added significantlyto infection, malaria, fever, and general extreme discomfort.Quinine, if they could get it, was referenced as thecure for just about everything. According to Blackburn,it helped some, but nowhere near enough.The SOF significance of Don Blackburn is extensive.Throughout Don Blackburn’s career he continuedto contribute and build on the lessons andaccomplishments from the Philippines. Shortly after hissuccessful tour in the Philippines, Blackburn was assignedto Military Advisory Group – South Vietnam anddid a great deal of work with the South Vietnamese Armyin the Mekong Delta area. Shortly afterward, COLBlackburn was given command of the 77th <strong>Special</strong>Forces Group (soon to become 7th <strong>Special</strong> Forces Group)at Fort Bragg, NC, where he immediately establishedtraining designed to enable his ODAs to provide infantrytraining to foreign indigenous personnel. COL Blackburnwas responsible for sending the first group of ODAsinto Laos, under the famed LTC Arthur D. “Bull” Simons,to assist the Laotian Government in training theirArmy. This program became an in country preparationfor <strong>Special</strong> Forces deploying to Southeast Asia and amodel for the training program given to the Army of theRepublic of Vietnam (ARVN).After his command of the 77th SFG (A), Blackburnwas instrumental in growing <strong>Special</strong> Forces and infurther developing their employment and training. Heworked closely with famed BG William Yarborough atthe <strong>Special</strong> Warfare Center and was significant in furtherimproving failed intelligence operations in Vietnam. Outof Blackburn’s increased efforts in Vietnam came the developmentof the critically needed Military Assistance<strong>Command</strong> Vietnam – Studies and Observations Group(MACV-SOG), of which Blackburn became the secondcommander. The intelligence benefits of MACV-SOGwere critical to the successes in Vietnam – when theywere acted upon. COL Blackburn was soon appointedto BG and was the designer and recruiter for the famousSon Tay Prison Raid in which COL Bull Simons led theforces into the compound to rescue 70 American prisonersheld hostage. BG Blackburn continued to contributeto the empowerment of <strong>Special</strong> Forces at the highest levelsof the DOD and he is considered to be one of thefounders, if not “the” founder, of Army <strong>Special</strong> Forcestoday. His experience bears relevance also to theongoing missions of today.BG (Retired) Blackburn passed away in 2008 inhis home in Sarasota, Florida. He epitomized contributionand service and made an enormous difference forboth <strong>Special</strong> Forces and for this country overall. He isgreatly missed but his spirit lives on in <strong>Special</strong> Forces.See also:http://www.arlingtoncemetery.net/ddblackburn.htm82Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
The Battle of Mogadishu:Firsthand Accounts from the Men of Task Force RangerEdited by Matt Eversmann and Dan Schilling. Forward by Mark Bowden New York: Presidio Press. 2005.ISBN: 0-345-45966-0.Review by LTC Craig A. MyattIt was a difficult way to earn military pay on acouple of hard days in Somalia. The Battle of Mogadishu:Firsthand Accounts from the Men of Task Force Ranger,edited by Eversmann and Schilling, is a telling account ofsix different descriptions of one single battle that manyknow from Mark Bowden’s Black Hawk Down: A Story ofModern War. Six men share their personal thoughts on amission planned initially for straightforward, standard operatingprocedures, to be executed in the Horn of Africa.At the time, the October 1993 Mogadishu mission becamethe fiercest ground combat that the U.S. had fought sincethe Tet Offensive in Vietnem in 1968.What draws the reader into the realities of modernday war in Eversmann’s and Schilling’s work in amanner distinct from Bowden’s literary and cinematicaccounts? The draw is the dialogue and thoughts of warriorswritten by warriors. One of the strengths of Bowden’sliterary exploit, not necessarily reflected in itscinematic portrayal, is an account of Somali viewpointsthroughout the Battle of Mogadishu. What did the averageSomali think about the American threat and carnageon his, or her, streets? What did the Osama Bin LadentrainedSomali devotee of Mohammad Farrah Aidid thinkthroughout the battle? Bowden unveils this. Eversmannand Schilling do not. They disregard the thoughts of theSomalis, and focus on their own tactics, thoughts, perceptions,and feelings in battle. The battle-smeared perspectivesof six highly trained <strong>United</strong> <strong>States</strong> warriorscaught in more of a fight than what they planned revealsthe absolute sense of courage required in war.Six men with six different accounts of one battlebecomes a streamlined series of American perspectiveson how one battle could have been, should have been,and ultimately was fought. The lessons learned in the seriesof accounts are important, but more important is thebreadth and depth of thought that led the <strong>United</strong> <strong>States</strong> tovictory through the chaos of battle. Did they plan? Ofcourse, they planned. Their planning, nonetheless, led towhat all careful planners plan to avoid — the unexpected.Confronted by the unexpected, did they pray? Yes. Werethey profane? Yes. Did they question their own actionsor the actions of others? Yes. Did they feel an impendingsense of doom? Yes. Did they quit? No.Eversmann’s and Schilling’s text is a story ofhow six men displayed the courage not to quit based onthe expert level of training they went through prior to battleand their sense of commitment to their buddies, unit,family, and nation. Each man showed ne plus ultra determinationin their heated confrontation with Somalifighters loyal to Mohammed Farrah Aidid. The Somalifighters generated a formidable force employing methodsto shoot down helicopters and go face-to-face inBook Review 83
combat against anything and anyone, especially Americans.The Somali fighters battled with no sense of lettingdown. The precise attacks from Somali fighters, followedby relatively well-coordinated ambushes, incorporated tacticsthat had proven successful in Soviet-Afghan warfare inthe 1980s.In Mogadishu on October 3, 1993, <strong>United</strong> <strong>States</strong>Army Rangers and Delta Force teams in Operation GothicSerpent started a relatively routine mission to capture tierone personalities serving under the Somali warlord MohammedFarrah Aidid. Staff Sergeant Matt Eversmann, achalk leader, was with the first group of Rangers who fastroped from one of the Black Hawk helicopters involved inthe mission. He was the last to exit his aircraft. By thetime he descended down the rope, Somali bullets had alreadystruck one of his men.Fast roping into the battle and establishing immediatecasualty collection points (CCPs) became a prominenttheme throughout the six chapter text. Fast roping isalways potentially dangerous. In Mogadishu that day, thedanger of fast roping exceeded its potential. Early in thecourse of the battle, the need to establish CCPs rapidlytransitioned into the need to maintain CCPs.A straightforward mission chaotically unraveledinto a death-defying rescue operation. Sergeant RaleighCash did not enter the raging battle by fast roping. He advancedinto battle in an eight-vehicle ground convoy sentto rescue his besieged buddies. Cash became the primaryforward observer charged with rescuing those who crashedin the first downed Black Hawk.In <strong>Special</strong> <strong>Operations</strong> Forces, if rank is less importantthan tactical proficiency, knowledge, and the will toovercome challenges, then it is no surprise that a <strong>Special</strong>ist(E-4) uttered the famed “Black Hawk Down” call in battle.<strong>Special</strong>ist Mike Kurth, a radio and telephone operator,former infantryman, and native of Texas, was on the radioas soon as he saw the first Black Hawk go down: “All stationsbe advised – we have a bird down, we have a BlackHawk down.” Thinking clearly, Kurth made initial radiocontact to let everyone know what had just happened. Hefelt that the sooner his higher command knew about it, thebetter. Radio contact then became more than intense. Itbecame frantic. Everybody (friendly and foe) in the vicinityof the battle wanted to find the crash site.By the time Sergeant John Belman engaged in thebattle he had fast roped into the biggest firefight of the battleand his helicopter had already been hit with a rocketpropelled grenade (RPG). As he slid off the rope, with approximatelya 40-foot drop, he hit the ground hard andthought it a big mistake to use Black Hawk helicopters toprovide sniper cover. Mistake, or not, his role on the CombatSearch and Rescue (CSAR) team meant he had a job todo. But his thoughts about the use of Black Hawk helicoptersto provide sniper cover could not be avoided. ADelta sniper who had been on the first Black Hawkdowned lay on the ground disoriented with severe facialinjuries. Belman aided the sniper, but ran out of ammunitionvery quickly. In the course of the battle, existentialperspectives overwhelmed him as he thought that ifhe were killed, he did not want anyone to have to die toprotect his dead body. After making way to a CCP, hegrabbed additional ammunition and made sure he stayedalive for the fight.Pararescueman (PJ) Tim Wilkinson served asone of the Air Force PJs who conserved life for many ofhis buddies in battle under intense Somali fire. He claimsthat during his insertion he saw more RPGs streakingthrough the sky than he had ever seen on any of his previousmissions. He knew the men on the ground werelocked in mortal combat. His job was to maintain life atthe established CCPs and facilitate medical evacuation.Wilkinson vividly recalls saying a silent prayer beforehis insertion. His fast rope experience became intenselydangerous, as it had been for all the others, but more soin his case because he shouldered the added weight ofapproximately 90 pounds of equipment and medical supplies.Wilkinson’s recollections demonstrate the scopeof mental focus balanced by creative distractions. “Themind is a funny thing,” he states. All he could thinkabout in one of the most chaotic combat scenarios hefaced was a scene from the movie The Jerk starring SteveMartin. With so much information being directed at himall at once, and chaos all around, he found thoughts ofMartin’s role in The Jerk to be enough of a creative distractionfor him to remain in touch with his battlefield realitybut not consumed by it.Staff Sergeant Dan (Dano) Schilling, an AirForce combat controller responsible for directing closeair support from rotary wing aircraft, made several foraysby ground into battle to rescue his buddies. The designated“medic” on his team, not only did he plan key partsof the mission as a combat controller, but also he renderedlife saving techniques and procedures that sparedmany others in battle. His drive and commitment literallymade him the last out among the six contributingwarriors in the book and in the battle itself. He claimedthat in the Battle of Mogadishu, the sensation for himwas different than any he had experienced before onother missions. He could feel the difference, but couldnot define it. When he and the others finally made it outto a safe zone, his most poignant thoughts were of hisfriends, alive and dead.In a two-day battle in which 18 <strong>United</strong> <strong>States</strong>servicemembers died and 73 were wounded, the men of84Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
Task Force Ranger encountered enemy tactics, techniques,and procedures that served as a forerunner of futurethreats in Southwest Asia. Task Force Rangerincluded not only Ranger and Delta Force teams, but alsoAir Force Pararescue and Combat Controller teams,Navy SEAL Operators, and the 160th <strong>Special</strong> <strong>Operations</strong>Aviation Regiment. The task force configuration used inOperation Gothic Serpent is still common among thoseused in support of overseas contingency operations today.In this book, Eversmann and Schilling revisit aseminal military mission that reflects hard lessonslearned from the experiences of battle against a formidableopponent. Their literary contribution is an excellentread for both warriors and historians. Eversmannand Schilling share an accurate depiction of a battle thattaxed the thoughts, perceptions, feelings, and perspectiveson life for them and four of their friends: Cash,Kurth, Belman, and Wilkinson. I highly recommend thework for anyone engaged in the new norm of modern,21st century warfare, especially for those working in <strong>Special</strong><strong>Operations</strong>.Book Review 85
From the <strong>Command</strong> SurgeonVirgil “Tom” Deal, MDCOL, USA<strong>Command</strong> SurgeonHQ USSOCOMWell, to say that I’m a bit awed would be an exercisein understatement. The contributions of theSOCOM Surgeon’s Office over that last eight years havebeen highly significant. The improvement in the diagnostictools and the effectiveness of an increased array oftherapeutic interventions available to the <strong>Special</strong> <strong>Operations</strong>medical personnel throughout the prosecution ofthe conflicts at hand has been huge. I really have tosalute the surgeons, senior enlisted medical advisors(SEMAs), and staff that have stood the watch in Tampaand beyond since 9/11.Now that the music has stopped for this summer’sround of medical musical chairs, I am astonishedto find myself standing beside the one that oughta beclearly labeled “Rocky”. Please join me in saluting oneof our finest as he heads to the other side of MacDill,AFB – and the other side of the planet – to take the reinsas the SOCCENT Surgeon. Stay safe, Rocky! Don’tstray too far from the STU for those times when I andthe rest of us need to ask the tough questions!Our year ahead certainly promises to be interesting.The <strong>Command</strong>’s awareness of the issues atten-dant to the impact of stress on the force continues to bekeen. LTC Craig Myatt chaired a two-day meeting ofthe Resilience Enterprise Working Group this month andwill be working with you and your reps to delineate bestpractices from what you guys are already doing to mitigatethe effects of the stress of eight-plus years of nearcontinuous deployments.Congratulations are certainly in order to JimLorraine, the first Director of the SOCOM Care Coalition,who’s been called upon by the Chairman to act ashis advisor on issues related to casualty care. Jim’s contributionson the long-term care of our SOF sick andwounded has been a new chapter in how we approachthe entire constellation of issues when providing for thewounded and dealing with the disability process.We’re looking forward to next month’s AdvancedTechnologies meeting in St Petersburg. Thatmeeting and your continued lessons learned input onwhat widgets are working and which ones aren’t providesmuch of the basis for a continued smooth acquisitionprocess. Please keep the critiques coming in.See you at the SOMA Conference, 12-15 Dec!86Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
Peter J. Benson, MDCOL, USA<strong>Command</strong> SurgeonThe summer always brings personnel changes tothe medical community, and Fort Bragg is no exception.I have left the U.S. Army <strong>Special</strong> Forces <strong>Command</strong> (Airborne),<strong>Command</strong> Surgeon position in the able hands ofLTC Andrew (Drew) Landers, formerly the 7th <strong>Special</strong>Forces Group Surgeon. I have replaced COL Tom Dealas the U.S. Army <strong>Special</strong> <strong>Operations</strong> <strong>Command</strong> (US-ASOC), <strong>Command</strong> Surgeon. This was a somewhat precipitousmove, but hopefully all the pieces will fall intoplace as we proceed about the business of supporting the<strong>Command</strong> and subordinate units in the provision ofHealth Service Support (HSS). I want to thank all themedical providers in the <strong>Special</strong> Forces Regiment fortheir support and input as the <strong>Special</strong> Forces <strong>Command</strong>Surgeon’s Office was established and found its way. Ihave every confidence that LTC Landers will do an outstandingjob in continuing to build the office and supportingthe Regiment as the Surgeon’s Office matures.As the new USASOC <strong>Command</strong> Surgeon, I feelprivileged to be chosen to follow such august gentlemenas COL Farr, COL Diamond, and COL Deal. I hope tovalidate the trust and confidence of the <strong>Command</strong> in havingbeen chosen. The Surgeon’s Office will continue tobe the advocate for providing the right personnel, equipment,and training to medically enable the force. I planto take a look at some new, as well as some old, initiativesthat will have long-range effects on the medical partof the force. This includes the creation of an organic US-ASOC organic Forward Surgical Resuscitative Element(FSRE) capability, an Female Treatment Team capability,strategies for critical care CASEVAC, an advanced clinicaltraining course for <strong>Special</strong> Forces Medical Sergeants,the establishment of additional medical Modified Table ofOrganization & Equipment (MTOE) positions in the 4thPSYOP Group, among others. Another initiative for US-ASOC has been the recent approval for selected specialstaff officers to attend the 18A <strong>Special</strong> Forces QualificationCourse. This program, recently approved by MGCsrnko, the <strong>Command</strong>ing General of the John F. Kennedy<strong>Special</strong> Warfare Center and School, will once again allowselected medical corps and medical specialist corps officersthe opportunity to become <strong>Special</strong> Forces qualified.Although not granted the 18A MOS, this will provide asolid core of foreign internal defense (FID) and unconventionalwarfare (UW) trained providers to be the advocatesfor HSS as it relates to <strong>Special</strong> Forces <strong>Operations</strong>.This pilot program will fix a 16-year hiatus in training SFqualified medical officers.I would like to commend all the providers at alllevels within USASOC for doing their very best to providethe best medical support possible to their units. Asforces prepare to conduct the ongoing operations of theNation’s persisting engagement, I encourage all to remaindiligent and steadfast in their roles as providers. Continueto maintain your skills and equipment, train your peers andsubordinates and remain one step ahead of the threat.Component Surgeon 87
Bart Iddins, MDBrig Gen (S), USAF<strong>Command</strong> SurgeonThis article continues with the discussion ofAFSOC Surgeon’s priorities and focuses on Priority 4:Develop an AFSOC healthcare engagement strategy andcapability that supports counterinsurgency (COIN), irregularwarfare (IW), foreign internal defense (FID), security,stability, transition, reconstruction (SSTR),disaster response, and humanitarian operations (seeJSOM, Winter 2009 for complete priority list; JSOM’sSpring 2009 edition for detailed review of Priorities 1through 3).As evidenced by the lessons of history, the contemporaryconflicts in Iraq and Afghanistan, and fromsituations such as those now unfolding in Pakistan, it isclear that the <strong>United</strong> <strong>States</strong> of America must maintain arobust and viable capability for conducting COIN, IW,SSTR, disaster response, and humanitarian operations.If, despite the aforementioned examples, one is still unconvincedof this absolute requirement, one only needsto examine Brookings Institution’s Index of State Weaknessin the Developing World. This index factors economic,political, security, social welfare, and per capitagross national income (GNI) data from 141 states intoan overall weakness score of 0.00 (worst) to 10.00(best). According to this methodology, the five weakeststates are Somalia, Afghanistan, Democratic Republicof the Congo, Iraq, and Burundi. Furthermore, 56 of the141 states are listed in the bottom two quintiles and areat significant risk for unrest, instability, and potentialcollapse.Failed states are unequivocally not in the nationalinterest of the <strong>United</strong> <strong>States</strong>, nor in the national interestof any other developed nation. While the previousstatement is intuitively obvious, its solution is more elusive,but illustrates the absolute requirement for forcesthat can effectively apply “soft power with a hard edge.”This description by Admiral Eric Olson regarding one ofthe many capabilities SOF contributes to national defensealso perfectly highlights an underutilized SOF medicalcapability. While SOF medical forces serve in traditionalsupportive and enabling roles, they can equally deliver anunrivaled form of “soft power with a hard edge” in supportof COIN, IW, FID, and SSTR operations. Additionally,senior leadership, as demonstrated by the followingquotes, recognizes and espouses the imperative to embraceand deliver “soft power with a hard edge.”“The Nation is at war…whether our contributionis in irregular warfare in Iraq andAfghanistan, the fight to save lives through humanitarianrelief operations, or deterrence and dissuasionof potential adversaries, the Air F o rc eis a key contributor to the national defenseof America.”USAF Chief of Staff, General Norton Schwartz, 2008“…the kinds of [security] challenges Americawill face…from global terrorism to ethnic conflictscannot be overcome by traditional militarymeans alone. Conflict will be…political in natureand will require the integration of all elementsof national power.”“These new realities…should be reflected inour training and doctrine. The Air Force willbe…called on to conduct civil-military or humanitarianoperations with interagency andnon-governmental partners, and deal directlywith local populations.”Secretary of Defense Robert Gates, AWC speech, 200888Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
Numerous military and civilian governmental/non-governmentalorganizations are heavily involvedin healthcare engagement activities. The vast majorityof these organizations, to include SOF units, are doingheroic, often unheralded work in demanding and dangerousenvironments in many of the world’s developingnations, trouble spots, and war zones; however, in spiteof these herculean efforts and notwithstanding the bestof intentions, much of this critically important work isbeing conducted without an overarching strategy. As aresult, many organizations conducting well-intendedhealthcare engagement missions habitually fail to adequatelycoordinate and integrate their efforts. Predictably,this lack of an overarching strategy and failureto coordinate/integrate activities further cascades into aloss of unity of effort and potential synergy, becomescounterproductive, and may, in fact, ultimately underminethe desired effect of the healthcare engagementmission. In response, AFSOC has created the USAF’sfirst and only IW/Healthcare Engagement Division.This division (AFSOC/SGK), under the leadership ofLt Col (Dr) Mike Hartzell, a veterinarian with a master’sdegree in Public Health, is staffed by a medicalplanner, international health specialist (IHS), and a seniornon-commissioned officer. The division is chargedwith the following:• Organize, train, and equip (OT&E) AFSOCmedical forces for healthcare engagement insupport of COIN, FID, IW, SSTR, disasterresponse, and humanitarian operations• Develop overarching healthcare engagementstrategy, doctrine, tactics, techniques, andprocedures (TTP)• Plan, coordinate, deconflict, and integratehealthcare engagement activities• Serve as subject matter experts; provide healthcareengagement, COIN, FID, IW, SSTR,disaster response, and humanitarian operations’expertiseIn short, AFSOC’s IW/Healthcare EngagementDivision will significantly increase AFSOC medical supportto COIN, FID, IW, SSTR, disaster response, and humanitarianoperations. Furthermore, the IW/HealthcareEngagement Division will ensure that the AFSOC healthcareengagement is conducted in accordance with a strategicplan designed to create effects that directly supportoverall theater campaign initiatives and theater engagementstrategy.Component Surgeons 89
Jay Sourbeer, MDCAPT, USN<strong>Command</strong> SurgeonIn my capacity as the Force Medical Officer ofNaval <strong>Special</strong> Warfare, this is my final letter to the Journalof <strong>Special</strong> <strong>Operations</strong> Medicine. As a deep sea diverwho came to <strong>Special</strong> <strong>Operations</strong> as a tech from anothercommunity and who eventually returned as Force MedicalOfficer, I’ve brought a different view to the SOFworld than my conventional career <strong>Special</strong> <strong>Operations</strong>colleagues. Whether it is Master Chief Mercer posing asa diver, COL Rocky Farr putting a ruler to a stack ofjournals, or the combined efforts of all of you to improveforward surgical care and bring professionalism tohuman performance, I want to thank you for your contributionsto several highly enjoyable years of service.In particular I would like to thank COL RockyFarr for his practical leadership and advice, and especiallyfor sharing his rich insights into <strong>Special</strong> <strong>Operations</strong>over the years. CAPT Frank Butler, hispredecessor, left important lasting contributions that Igreatly appreciate as well. I treasure my association withthe next generation of Army, Air Force, and Marine <strong>Special</strong><strong>Operations</strong> leaders. It is a great joy to see COL JimCzarnik, COL Rob Lutz, COL Ric Ong, and COL MarkErwin serving the nation professionally. There are manymore – I cannot name all, but I will always appreciatethe work of those who set interests aside in service of ournation’s ideals as embodied in the Constitution.I hope you will extend a warm welcome to mysuccessor at WARCOM Medical, CAPT Gary Gluck. Heis board certified in emergency medicine and brings diverseexperience in <strong>Special</strong> <strong>Operations</strong>, having servedpreviously at the Naval <strong>Special</strong> Warfare Center and mostrecently at SDVT-1. As with my earlier allusion to colleaguesin the other services, it is a great satisfaction toknow that I am putting a treasured responsibility in suchable hands.I am being assigned as a student to the NavalWar College, Newport, Rhode Island, to add further tomy professional education. Although I am looking forwardto the exciting challenges ahead, I sincerely hope tokeep the friendships I have made in <strong>Special</strong> <strong>Operations</strong>.It has been an honor to serve with you.Thank you.90Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
Anthony M. Griffay, MDCAPT, USN<strong>Command</strong> SurgeonMarine Corps <strong>Special</strong> <strong>Operations</strong> <strong>Command</strong>(MARSOC) and MARSOC Medical continue to changeand evolve. Not only are we in the beginnings of a majorchange in medical personnel due to end of tour orders, butMARSOC has evolved from two operational battalionsand an Advisor Group into three battalions and a RegimentalHeadquarters. At the same time MARSOC is continuingto deploy teams down range and plan for anincreased presence and responsibility in higher levels ofintra-theater command and control.My filling the large shoes left by CAPT McCartneymarks the beginning of a 75% turn-over in the medicalleadership within MARSOC. As with all military units,turnover is inevitable, and to those moving on I would liketo express my sincere admiration and gratitude. This departinggroup of professionals helped build MARSOCMedical from nothing, into an organization capable of supportingteams around the world. Their experience anddedication will be truly missed. For the incoming personnel,this is an exciting time in MARSOC as it transitionsfrom growing and organizing to defining its future in the<strong>Special</strong> <strong>Operations</strong> community. From developing the culturally-specificmedical training needed for foreign internaldefense (FID), to supporting and training theater<strong>Special</strong> <strong>Operations</strong> Surgical Teams required to support directaction operations, MARSOC Medical will evolve andgrow to meet any needs.MARSOC has recently reorganized our organizationalstructure into a Regimental Headquarters and threebattalions, adopting a more standard military formationand standardizing the capabilities of the deployable elements.Now all three battalions train to operate across thefull spectrum of special operations, emphasizing FID andspecial reconnaissance (SR) while retaining a robust directaction (DA) skill set. With this, the medical supportsection and the medical capabilities will need to grow andexpand. This will be our biggest challenge! To train andsupport MARSOC in the future we will need to work, coordinateand train with our fellow components both within<strong>United</strong> <strong>States</strong> <strong>Special</strong> <strong>Operations</strong> <strong>Command</strong> (USSOCOM)and throughout the “big” Navy. Like all of SOF, MAR-SOC is small and exists in a financial reality which willnever allow us to own all of the assets that we need. However,regardless of whether a medical element is SOFownedor SOF-capable, we must take an active role indefining, equipping, training, and preparing it to supportour SOF missions.This reorganization will not only allow MARSOCto provide better command and control over an increasingnumber of teams but also provide the higher level headquarterselements it needs. These elements will be the coreof <strong>Special</strong> <strong>Operations</strong> Task Forces (SOTFs) and CoalitionJoint <strong>Special</strong> <strong>Operations</strong> Task Forces (CJSOTFs) as MAR-SOC begins to plan for and increase its role at the SOFhigher headquarters within the Central <strong>Command</strong> Area of<strong>Operations</strong> (AOR) and throughout the world.As I already mentioned, this is an exciting time tobe part of MARSOC and USSOCOM. I am looking forwardto my time here and hope to meet and work with asmany of you within the SOF community as possible.Please feel free to contact me at any time if there is somethingI may be able to assist with. COMM 910-451-3462DSN 751-3462 or anthony.griffay@usmc.milSIPR anthony.griffay@marsoc.socom.smil.mil.Component Surgeon 91
Warner D. “Rocky”Farr, MDCOL USASOCCENT SurgeonI am writing this on USSOCOM’s nickel in lateJune before I go on PCS leave for my strenuous PCS offive whole miles within MacDill AFB, to SOCCENTHeadquarters. I would like to thank all who have helpedme in getting done all that I have gotten done in my threeyears at USSOCOM. As my CSM back in 1973 in Germanyused to say, “And you know who you are!” I wentover 42 years active service on 23 April 2009. It is goodto still be upright and breathing and contributing to thewar effort.We have had some successes at USSOCOM inthe last three years, much of it on the backs of my predecessorswho set me up for success. The Journal of <strong>Special</strong><strong>Operations</strong> Medicine (JSOM) is bigger and betterand the pocket size Advanced Tactical Provider AnnualTraining Supplement seems to be well received. The AdvancedPractitioner Card now has reciprocity with severalother registries. The Tactical Combat Casualty CareAcquisition program is proceeding and medics are gettingmore of what they need as we branch into extractionand surgical kits. The Theater <strong>Special</strong> <strong>Operations</strong><strong>Command</strong> Surgeon slots are in place and filled – one byME, quite unexpectedly. MC Mercer’s Warrior RehabilitationPerformance Center Program has funding andis proceeding. The program is the key capstone topreservation of human capital! The Level-2 surgicalpiece of medical support has been approved as a concept,now we just have to figure how to resource it.Colonel Deal, “Post! Sir, your ball.”I plan to continue to contribute to the JSOM asthe SOCCENT Surgeon but probably not much of an operationalnature, security and all. Therefore, this quarter’sentry will be yet another book review.Khyber, British India’s North West Frontier:The Story of an Imperial MigraineCharles MillerNew York, New York: Macmillan and Company, 1977.393 pages. ISBN-10: 0025848607; ISBN-13: 978-002584860392Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
This is a great read that speaks directly totoday’s ongoing events. This book was published waybefore 9/11. I found it and read it again after 9/11. It ispart of the answer to the question of why bin Laden isstill at large. No one has ever really controlled that borderarea; not Alexander the Great, the Arabs, the British,not the Afghans, the Persians, the Indians, the Sikhs, northe Russians, nor even the tribes themselves. This bookshould be a must read for every GWOT leader inAfghanistan. It explains the issue of the Afghans not toleratingan occupying military force well at all. It is awell-written work covering both the political and thestrategic/tactical episodes, all of which shaped the Britishin their attempts to conquer Afghanistan for over 100years and in their attempts to control the Northwest Frontier.It actually has a large amount of medicine in it,telling several stores on early missionary efforts – mostwere killed. Several British Army unit surgeons playprominent parts in it including one, Surgeon WilliamBrydon, who becomes the only escapee of an entireBritish Army, wiped out to the next to the last man, withhim being the only man to survive the retreat to Pakistanand to tell the tale. He later goes on to fight in the “SecondAfghan War,” the British having not learned anythingfrom the first one!This book is the very best of popular history. Itis a book that is colorful, well written, and flows nicely.It has good references but not a large number of footnotes.The bibliography itself is interesting to read tosee such works as “Cabool: A Personal Narrative of aJourney to, and Residence in That City in the Years1936, 7, and 8.” With the new interests in Afghanistan,Pakistan, and currently the entire Northwest Frontierarea, this book, written in 1977, is suddenly timely! Itwould be nice to see an updated edition including theSoviet debacle, the rise, and destruction of the Taliban,and the American presence in Afghanistan. Copies arefindable on Amazon and the other used-books sites. It isalways interesting to read a book about the British “colonial”experiences, especially when they lose, as they seldomdid in the “Colonial Wars.” Just like in Basra, theywere there before us.TSOC Surgeon 93
Frank J. Newton, MDCOL USA<strong>Command</strong> SurgeonFORCE HEALTH PROTECTION (FHP) AND A REVIEWOF COUNTERMEASURES TO REDUCE THE THREAT OFRABIES TO U.S. MILITARY FORCESOur commanders have come to expect that they willhave a healthy, fit force that is prepared to execute any mission,at any time, and under any conditions. Surgeons, theirstaffs, and a robust medical network rapidly conveys informationabout disease outbreaks and emerging threats (likethe H1N1 flu virus), better than ever in our history to countermedical threats to U.S. military forces..Looking over the specific medical threats in Southand SE Asia, with rare exception, our troops are immunizedagainst many of the disease threats encountered. Two notableexceptions, which do not have immunizations availablefor primary prevention are some diarrheal illnesses andDengue. In both cases, personal protective measures, gooddiscipline, and command emphasis are required to maintainfitness to complete the mission and redeploy in good health.Rabies, a medical threat frequently encountered bySOF in the developing countries where they are employed,requires constant vigilance and command emphasis. Thevirus is transmitted by the saliva of infected mammalsthrough bite wounds, open cuts in skin, and when there ismucous membrane contact, with saliva or other infectious tissuesuch as brain. In the U.S., wildlife (especially raccoons,skunks, and bats) are responsible for most human and domesticanimal infections. In most of the world where rabiesis enzootic, including most of Asia, Latin America, andAfrica, dogs remain the major source of rabies transmission.SOF personnel receive primary or pre-exposure vaccinationfor rabies. This is an important FHP measure, consideringthat infection with rabies is universally fatal, and thatSOF operates in austere settings where there is a high prevalenceof rabies, and medical support, including biologics(vaccine and RIG) may not be immediately available. Manyof the support personnel that deploy to augment our taskforces have not received rabies vaccination. Their exposureto rabid animals (or even suspected rabid animals) is a medicalurgency.Recently, such an exposure occurred in the Philippines,where the incidence of rabies is ranked number six inthe world. The servicemember had been playing with a sixmonth-olddog outside of a military camp when the unprovokeddog bit the Soldier on the hand, causing afull-thickness injury. The dog was quarantined, and wasfound dead in his kennel less than 24 hours later. Brain fluorescencefor the rabies antibody was positive.Treatment for an animal bite includes immediatecleansing of the wound with soap and water, or preferablypovidone-iodine (betadine).* For previously vaccinated individuals,post-exposure treatment consists of two IM dosesof rabies vaccine, (1.0ml each) ), into the deltoid muscle. Thefirst is given as soon as possible after exposure and the secondis given three days later. Unvaccinated individuals aregiven a five shot series on day zero, three, seven, fourteen94Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
and twenty-eight. Rabies immune globulin (RIG) is administeredonly once, to previously unvaccinated individuals, andshould be administered as soon as possible after exposure.The dog or cat that bit the servicemember should bequarantined for up to ten days of observation to see if theywill exhibit signs of rabies. If the animal exhibits signs ofrabies, then it should be euthanized by the closest militaryveterinary treatment facility or authorized contract agency,and the head submitted for definitive testing. Any animalother that a cat or dog that bites a servicemember will be immediatelyeuthanized and the head submitted for testing. Thepreferred method of euthanasia is an injection of euthanasiasolution. If euthanasia solution is unavailable, then any approvedmethod that preserves the brain should be used.A discussion of rabies testing submission procedurescan be found in the <strong>Command</strong> Veterinarian column.Link to CDC, Human rabies prevention-U.S.http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5703a1.htm.*Editor’s note: The 5th Edition of Auerbach’s Wilderness Medicineadvises (p 1218) us not to trust reports of vaccination of dogs in foreigncountries as … “fatal rabies has been reported in U.S. citizensand in others who were bitten by “vaccinated” dogs in developingcountries.” On this same page, the former Chief of the Viral and RickettsialZoonoses Branch of the CDC advises us that “… local treatment[i.e., cleansing wound with soap and water] is perhaps the singlemost effective means of preventing rabies.”TSOC Surgeon 95
LTC Andrew Landers, MDCOL, USA<strong>Command</strong> SurgeonI would like to introduce myself as the new US-ASFC(A) <strong>Command</strong> Surgeon – having made the smallleap across the street from 7th SFG(A). I would also liketo thank COL Pete Benson for giving me the opportunityto continue the great works that he started during histenure with USASFC(A).The Surgeon’s Office is running on all cylinderswith my assigned friends: MSG Oscar Ware, SeniorMedical Enlisted Advisor, leading the way for all 18D,SAV, and CIP issues, and CPT Chad Vermillion, DeputySurgeon, in charge of medical operations and logistics.There are two new additions to the office: SFC Curt Unterreiner(MED TNG NCO) and SFC Fred Ziems (MEDOPS NCO). These are dynamic times, and the need for<strong>Special</strong> Forces Soldiers is on the rise. This means thatflexibility, adaptability, and planning will be the keys toour success.There are a few items that I would like to addressfrom this office. First, the proposed BAND V growthhas been approved by USASOC and is currently beingreviewed at USSOCOM. It includes the expansion of amedical company consisting of 36 personnel for eachGroup. Hopefully, we will be able to push this all theway and gain the medical flexibility and staffing that isneeded at the Group level. Second, as the need for <strong>Special</strong><strong>Operations</strong> Forces increases in support of overseascontingency operations, you need to look hard at theJoint Manning Document (JMD) of the Task Force,available resources in theater, and what you will need toprovide Health Service Support (HSS) to your TaskForce. Remember, if you need a capability that US-ASOC cannot resource internally, the request for forces(RFF) must be submitted from theater. Make sure thatyou are talking with your counterparts for the latest andgreatest. We are standing by to assist you, so please, donot hesitate to contact us. If we do not know what youneed, we cannot help you. Third, it is extremely importantto collect and articulate lessons learned from trainingand deployments. We need to stay ahead of thecurve; we cannot afford to practice “status quo” medicine.No one likes to write reports, but it can make areal difference on the future of our battlefield. Fourth, aswe look to the future with the SOMA Conference aroundthe corner, please contact me or MSG Ware with yoursuggestions on topics that you would like covered in theSF breakout sections. The goal is to make it more educationalfor the SF medics and provide the most relevant,and up-to-date information. Lastly, theUSASFC(A) Surgeon’s Office will continue to handleprofessional assignments and staffing of the Groups. Weare working on FY10 slating, so now is the time to contactus with any staffing issues.Again, it is a pleasure to work with each of youin the Regiment and I look forward to the future. Whilewe are all aware of the challenges that operational medicinefaces, we all need to continually remind ourselvesthat with these challenges come numerous opportunitiesto make a real difference in the lives of those who relyupon us. De Oppresso Liber!96Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
Rhett Wallace MD FAAFPLTC MC SFS DMOSenior Medical AdvisorNATO SOF Coordination CenterBonjour from the Supreme Headquarters AlliedPowers Europe (SHAPE), deep in the heart of Wallonia inMons, Belgium. Since my arrival a year ago as the firstNorth Atlantic Treaty Organization (NATO) SOF SeniorMedical Advisor (MEDAD), the NATO <strong>Special</strong> <strong>Operations</strong>Coordination Center (NSCC) has moved from “concept,”through initially operational capable, to declaring full operationalcapability, with recent approval to progress toward becominga NATO SOF Headquarters (NSHQ). Currently westand as a fully-functioning and operationally relevant organizationtasked with advising, coordinating, and influencingNATO operations, policies, and exercises.Many readers are familiar with the challenges of establishinga new organization – wading through the processof identifying priorities, developing a network of key stakeholders,writing standard operating procedures, and movingforward with the work at hand. This year has included all ofthat and more. It is more than a job; it’s an adventure!As all good SOF operations begin, so has this one,with gathering information, learning the language and cultureof the locals, establishing relationships, and then throughand with the indigenous population affecting our desiredchange (in this context, however, the indigenous populationis made up of the Allies). My goal as the Senior Medical Advisoris to set the conditions and create the policy and doctrinefor defining and understanding international SOFmedical capabilities and requirements. This will enableNATO SOF to support operations with the right people (capability),in the right place, at the right time to keep our forceshealthy, mitigate risk, and decrease morbidity and mortality.Understanding NATO and operating within its combined,joint structure can at times be frustrating. Some ofyou have experienced this while operating within current orpast NATO operations. NATO has its own culture, language,and politics all filtered through a collective consensus of politicalwill.NATO is currently an Alliance of 28 nations with Albaniaand Croatia added this year; and 26 of these possesstheir own <strong>Special</strong> <strong>Operations</strong> Forces. Each nation within theAlliance has as an equal voice, and remains sovereign as theycontribute politically to exert their national wills, agendas,and goals within the Alliance. The North Atlantic Counsel(NAC) is NATO’s supreme political body and is located inBrussels, Belgium. The NAC’s guidance is delegatedthrough the International Staff (IS) dealing with political issues,and through the Defense Planning Committee (DPC)and Military Committee (MC) dealing with military aspectsof NATO. The Allied <strong>Command</strong> for <strong>Operations</strong> (ACO),under the <strong>Command</strong> of the Supreme Allied <strong>Command</strong>er Europe(SACEUR), is the military arm of this consensual politicalbody. The ACO is located in Mons, Belgium at SHAPE.The ACO, through the direction of the NAC, the DefensePlanning Counsel (DPC), the Military Committee (MC) andthe International Staff (IS) is NATO’s military means by elective,collective contribution to effect change desired byNATO’s consensual political will.TSOC Surgeon 97
Unlike the <strong>United</strong> <strong>States</strong> military decision-makingprocesses, where operational control and chain-of-commandare, hopefully, clear and established, NATO operations are oftentimesmanaged under administrative control, using a varietyof potential lead-nations, with contributing nationsretaining sovereignty to opt in or out of specified missions,based on their national-political motivations. These nationalcaveats can be frustrating, but are essential to maintaining nationalsovereignty within the Alliance. The challenge then ofunderstanding and effectively operating within NATO is to realizenot only the capability of each contributed force, but alsothe political sensitivities and restrictions of each nation withina given operational environment. Savey vous!?With that in mind, I continue to work to gain consensusto establish policies, directives, and SOF medical doctrineas a foundation for NATO SOF medical operations and planning.The key being establishing common ground and agreementand, through dialogue and debate, negotiating the finernuances of what is salient.Within the NSCC’s educational activities, SOF HealthService Support Planning is currently included in our CombinedJoint Staff Officer’s and the International Security AssistanceForces (ISAF) Staff Officer’s Courses. Within thenewly published <strong>Special</strong> <strong>Operations</strong> Task Group (SOTG) andCombined Joint Forces <strong>Special</strong> <strong>Operations</strong> Component <strong>Command</strong>(CJFSOCC) Manuals chapters are dedicated to MedicalSupport Planning. These manuals are used as reference materialswithin NATO SOF courses, ISAF, and by nations contributingto NATO SOF operations.Another item that needs to be highlighted and disseminatedis the ISAF SOF HQ medical directive. This directivewas developed by the NSCC, in coordination withACO, Joint Forces <strong>Command</strong> (JFC) Brunnsum, and ISAFMEDAD’s. It provides SOF medical planners with a theaterlevelmedical support planning tool, and promulgates understandingof regional nuance, national caveats, and capabilitiesthat directly affect SOF operations. The intent of this documentis to provide SOF elements at any level who contributeto ISAF operations, situational awareness and the tools to effectivelyconduct SOF operations either regionally or intertheater.If your unit is currently contributing to ISAF, or isplanned to do so, please contact me at the NSCC for access,exchange of information, and updates.I would also like to request your participation in importantupcoming events to keep NATO SOF medical supportand capability visible at the Operational <strong>Command</strong> and InternationalMedical <strong>Command</strong> level. The 2nd SOF <strong>Command</strong>ersSymposium to be held in Rome, Italy, this September willhighlight to SOF <strong>Command</strong>ers the progress made thus farwithin ISAF SOF Medical support. Our goal will also be topromote consensus on medical capability standards for adequatesupport across the operational continuum to SOF operations.The next opportunity then will be the 2nd NATOMedical <strong>Operations</strong> Conference to be held in Heidelberg,Germany, this October. The NSCC has coordinated a subconference,the first NATO SOF Medical <strong>Operations</strong> Conference.The intent of this conference is to bring Medical<strong>Command</strong> and SOF Medical Surgeons/Planners together tofoster dialogue, develop consensus, and inculcate internationaladvances and lessons learned into new NATO policy,doctrine and standards relating to medical capability and requirements.Other opportunities for collaboration are the <strong>Special</strong><strong>Operations</strong> Medical Association (SOMA) meeting in Tampa,Florida, and the Tactical Combat Casualty Care Symposiumin Pfullendorf, Germany, held annually in December andJune, respectively. At SOMA this December, I plan to providean update on the decisions, advances or barriers tochange thus far in publishing NATO SOF Medical policyand doctrine. The TCCC Symposium in Pfullendorf is theEuropean version of SOMA hosted by Germany. It providesan excellent opportunity to establish contact with internationalSOF Surgeons, share ideas and concepts on equipmentand technologies, and discuss lessons learned.Lastly, with the help of a few friends and experts intheir respective fields I have revised and re-written the jobdescriptions of the Medical Branch within the NSCC; I expectthat the changes will be approved and implementedwhen the NSCC transitions to the NSHQ later this year.NATO will move away from Joint Staff designations to functionalareas in April of 2010. The NSHQ Medical Branchwill reflect the recommended changes having a <strong>Command</strong>Surgeon dual-hatted within the <strong>Command</strong> Group as specialstaff to the <strong>Command</strong>er, and Medical Branch Chief, withinthe Medical Branch, under the Deputy Chief of Staff forSupport. This will maintain the command relationship andalso the functional area of the Medical Branch. I am hopingto expand the Medical Branch from the current two positionsto a more capable organization of five. This will require approvalas a part of our transition to NSHQ, but more importantlyactually providing people against these positions frombidding nations to become a reality.Over this past year I have had significant input andsupport from multiple <strong>Special</strong> <strong>Operations</strong> <strong>Command</strong> surgeons.I want to express heart-felt thanks for your support.I look forward to expanding this collective group of friendsand colleagues, and continuing to use your input and insightsto developing the way ahead.98Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
LTC Craig A. Myatt, Ph.D., HQ USSOCOM PsychologistThe <strong>Special</strong> <strong>Operations</strong> Forces (SOF) psychologycommunity heralds the leadership and success of theoutgoing USSOCOM <strong>Command</strong> Surgeon and welcomesthe same measure of professionalism from his successor.The outgoing <strong>Command</strong> Surgeon’s vision, to develop abehavioral health element in the <strong>Command</strong> Surgeon’sOffice, was timely and will ultimately enhance the effectivenessof SOF and strengthen the role that psychologistsin the SOF community provide to commanders,first-line supervisors, team leaders, and Families.The ongoing guidance provided to the ResilienceEnterprise Working Group (REWG) from theUSSOCOM <strong>Command</strong>er, combined with the immediateassistance rendered by the incoming <strong>Command</strong> Surgeon,give the REWG continued and undisrupted leadershipsupport to remain focused on an essential endstate goal:to sustain enduring operational readiness in SOF and fortheir Families.While guidance, assistance, support, and commitmentare essential for the development of a USSO-COM Resilience Enterprise Program, one of the moresalient factors ensuring initial success for the program isgood old-fashioned HARD WORK. REWG memberssaw the successful approval of the initial capabilitiesdocument (ICD) for the REWG in accordance with thegroup’s charter. The March 13, 2009, REWG charterstipulated that an ICD must be generated within 75 workingdays. Several products from the April 9, 2009,REWG meeting met requirements for inclusion of theREWG as a specific capability in the Warrior RehabilitationPerformance Center Program ICD. As a part ofthe Human Capital Preservation program of record, theREWG obtained ICD approval from the USSOCOMDeputy <strong>Command</strong>er on June 2, 2009, through approvalof the WRPC Program ICD. Hard work from the REWGmembers made that happen.The REWG held its first conference on 7 and 8July and included the participation of both the outgoingand incoming USSOCOM <strong>Command</strong> Surgeons. TheJuly conference marked another milestone in the developmentof the USSOCOM Resilience Enterprise Program.During the proceedings, REWG members definedresilience (for SOF-peculiar applications) as the ability tosustain, enhance, and quickly recover an optimal levelof performance. The members also revised the REWGrestated mission as the following: “To sustain combatpower by increasing resilience in SOF and SOF Familiesto meet the challenges of a changing environment.”Finally, as part of an extensive action plan, the REWGset the stage for the rapid development (within threeweeks) of a draft DCR (Doctrine, Organization, Training,Materiel, Leadership and Education, and FacilitiesChange Recommendation) for circulation through theREWG in August. Hard work from the REWG membersmade that happen too.Hard work by the REWG is recognized as a necessaryresponse to the difficult challenges faced daily bySOF and SOF Families. Within the SOF psychologycommunity there is a growing awareness that our forcesdo not have a significant problem with respect to behavioralhealth. On the other hand, there is a growing senseof the potential for “burnout” in both SOF and their Families.One of the REWG members recently discussedhow SOF warriors and their Families face significantemotional and physical burnout because of the sustainedand recurring nature of overseas contingency operations,USSOCOM Psychologist99
igorous training, ongoing garrison functions, informationoverload, the inability to disengage from threats to self andFamily, and the unpredictability of deployment cycles.Burnout in that context is a measurable form offatigue. Fatigue is both emotional and physical. It can beseparate from, but related to, cognitive performance andmanifests itself in several different ways. Fatigue (orburnout in the words of an REWG member) decreases theoverall capacity of individuals, Families, and organizationsto negotiate the challenges they face. He went on tostate that burnout (or fatigue) “affects job performance,retention, Family dynamics (Family interactions), and behavioralhealth status.”From that perspective, resilience is not a behavioralhealth issue by itself, but a subset of broader organizationalcharacteristics that include leadership, education,training, and culture. Some members of the REWGagree that “resilience generally emerges in people whohave trained hard (proving themselves physically tough),have particular attitudes, cognitive and emotional skills,and a deep determination to overcome serious challenges(physical and intellectual).” Demonstrating exactly howresilience as a SOF-peculiar application for SOF personneland their Families is an organizational and leadershipissue, as well as an operational force-protection issue, isa daunting challenge. It will not be easy. However, continuedhard work on the part of the REWG members willdemonstrate precisely how resilience as a SOF peculiarapplication for SOF personnel and their Families is anorganizational, leadership, cultural, and force-protectionissue, combined, and how building resilience in SOF andSOF Families sustains combat power.100Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
LTC Bill Bosworth, DVM, USSOCOM VeterinarianCOL Newton has brought up a great topic on theForce Health Protection measures we take to protectservice members against rabies. I’m going to expandupon his article by outlining the procedures to submit asample for rabies testing to the two DOD veterinary laboratoriesfrom theater. The contact information for bothlabs is listed at the end of this article.The process for submitting samples fromAfghanistan and Iraq is well established, and the theaterVeterinary Treatment Facilities (VTFs) submit samplesto the Veterinary Laboratory-Europe (VLE) on a weeklybasis. It is best to let the Medical Detachments, VeterinaryServices (MDVS) in those areas submit samples thatyou have, rather than try to submit them on your own.For contingency operations in areas that do not have aconventional veterinary unit presence, it is recommendedthat the unit conduct a “dry run” sample submission.This will identify any areas where the sample can be delayed,such as foreign customs offices. When submittinga dry run sample submission, notify the laboratory thatyou are sending it to, use the same shipping materials youwould use in a real submission, and submit somethingthe same approximate size and weight as an animal head,such as a five pound ham or turkey breast. The use offood will give the lab an idea if the sample can maintainthe proper temperature during shipping. You can contactthe closest theater VTF or either laboratory if you haveany questions about how to submit a sample.Here is the extract from the Laboratory SubmissionGuide to submit a brain for rabies testing at either ofthe two labs:7-3. Diagnostic Samples (Blood,serum and tissue samples)a. Rabies Diagnosis Sample -brain tissueb. Submit all requests for rabiesdiagnosis testing on DD Form 2620,“Request for and Report of LaboratoryRabies Test” (electronic form availableat http://www.dtic.mil/whs/directives/infomgt/forms/eforms/dd2620.pdf).c. Wild animals, domesticateddogs and cats (whose owners cannot bereadily identified) that have exposed aperson should be euthanized immediatelyupon capture and submitted fortesting.d. Preparation of Specimen:(1) Decapitate the animal andplace the head in a plastic bag and seal.Place the sealed specimen in a secondheavy plastic bag and seal the secondbag. Send the entire carcass of small animalssuch as bats.(2) Refrigerate immediately.Freezing animal specimens is not recommendedunless a delay in shipment isexpected.e. Packing Shipping Containers:(1) Add sufficient refrigerantto an insulated shipping container tomaintain a temperature of 0 to 4°C duringtransit.USSOCOM Veterinarian101
(2) Use drip-free gelpacks as a refrigerant. Pack refrigerantin a separate bag than the sample. Liquidmust not leak from the shippingcontainer during transit so DO NOTUSE wet ice to ship!(3) Labeling ShippingContainers and ShippingDocuments(a) Animal specimensfor rabies diagnosis areconsidered DIAGNOSTICspecimens. <strong>Special</strong> labeling isnot required for shipment of diagnosticspecimens. DO NOTlabel the exterior of the shippingcontainer as a “rabies specimen.”(b) Place the completedDD Form 2620 in asealed plastic bag and place iton top, between the inner andouter containers. Affix a copyof the request form, in an envelope,to the top of the outershipping container. Be sure toinclude a point of contact whocan receive the laboratory reportupon completion of testing.Phone numbers for that individual(day and night) must belisted.(c) The phrase“Diagnostic Specimen – Animal”should be used on alltransportation documents(GBL, Airbill, etc.) to describethe specimen shipped. DONOT mention “rabies.”c. Method of Shipment: Ship bythe most expeditious means (overnight,next day delivery) available. If shippingon a Friday, the shipper must be specificallytold that the item needs to be delivered(the following day) on aSaturday and the laboratory notified sothat they can have an employee availableto receive on a Saturday.d. Notify the laboratory by telephoneas soon as the specimenhas been shipped and providethe following:(1) Type of animal.(2) Indicate whether or nothuman exposure was involved.(3) Specify the method ofshipment used and the sample’s estimatedtime of arrival to the lab.NOTE: Notification is vitally important,especially when a rabies suspect sampleis shipped for Saturday or holiday delivery.The laboratory is normally notstaffed on weekends/holidays and specialarrangements must be made to receiveand process the specimen.One of the capabilities that the MDVS now havein Iraq and Afghanistan is a rabies screening test that canbe conducted at the VTF. The direct rapid immunohistochemistrytest (DRIT) was developed at the Centers forDisease Control and Prevention (CDC) as an environmentalsurveillance, screening, and data gathering tool.Army veterinary pathologist LTC Greg Saturday fromVLE was trained by the CDC to conduct the test, and hehas traveled to Iraq and Afghanistan training the MDVSto run the DRIT test in their VTFs. The DRIT test is aten-step process that can be completed in about an hour.Impression smears of the obex of the brain stem are madeand fixed in formalin, and are then held until there areenough to batch test – usually ten samples plus a negativeand positive control. At the end of the hour long process,the samples are viewed under a microscope to look forred inclusions in the sample. The presence of red inclusionsindicates a rabies positive sample. Any DRIT positivesample tissue must be sent to VLE for aconfirmatory direct fluorescent antibody (DFA) test.Studies have shown that the DRIT has specificity andsensitivity equivalent to the DFA.POINTS OF CONTACTWorldwide:DOD Veterinary Food Analysis and Diagnostic Laboratory(FADL)Attn: MCVS-Lab2472 Schofield Rd Suite 2630Fort Sam Houston, TX 78234-6232Capabilities: Full chemical, microbiological and diagnosticDeputy Director: MAJ Alisa Wilma, 210-295-4322,Alisa.WilmaMAJAMEDDCS@amedd.army.milRabies POCs: Edwin Cooper, 210-295-4920,Edwin.cooper@amedd.army.mil; Michael Gray, 210-295-4736, Micheal.gray@amedd.army.milDSN: 421-4604/4761Comm: 210-295-4604/4761Sample receiving area: 210-295-4210FAX: 210-270-2559102Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
Europe, Mideast, Africa and SWAU.S. Army Veterinary Laboratory-Europe (VLE)CMR 402APO AE 09180Capabilities: Most chemical, microbiological, and limiteddiagnosticChief of Diagnostics: LTC Greg Saturday, DSN 314-486-8963, greg.saturday@us.army.milRabies POC: Mrs. Leslie Fuhrmann,leslie.fuhrmann@us.army.milDSN: 314-486-8300/7241Comm: 011-49-6371-86-8300/7241(Landstuhl, GE)DSN FAX: 314-486-7075Comm FAX: 011-49-6371-86-7075REFERENCESSample Submission Guide, January 2009; DOD Veterinary FoodAnalysis and Diagnostic Laboratory (FADL),http://www.vetlab.army.mil/documents/LABguide2009.pdf.Standard Operating Procedures for the Direct Rapid ImmunohistochemistryTest (DRIT) for the detection of rabies virus antigen; Centersfor Disease Control and Prevention, Rabies Section.Evaluation of a Direct, Rapid Immunohistochemical Test for RabiesDiagnosis, Lembo, et.al., Emerging Infectious Diseases, Vol. 12, No.2, Feb 2006.Blank DD Form 2620, Request for and Report of Laboratory Examination for Rabieshttp://www.dtic.mil/whs/directives/infomgt/forms/eforms/dd2620.pdfUSSOCOM Veterinarian103
Navy Safe HarborTaking Care of Wounded, Ill, and Injured Sailors, Coast Guardsmen, andTheir FamiliesHM2 Debora GatzkeNavy Safe Harbor provides Sailors, CoastGuardsmen, and their Families a beacon of hopethrough non-medical support following a serious illnessor injury.Navigating the waters of recovery following aserious illness or injury is often overwhelming and exhaustingfor a servicemember and his or her Family.“Questions about pay and benefits, housingadaptation, and employability murky the waters of therecovery process,” said <strong>Command</strong>ing Officer of NavySafe Harbor, CAPT Key Watkins. “While providingbedside care for their loved-ones, Families often don’thave the resources or time to manage these arisingissues.”Seventeen Safe Harbor non-medical care managerstailor support to each enrolled servicemember’srecovery and reintegration needs. Support includes payand personnel issues, invitational travel orders, lodgingand housing adaptation, child and youth care, respitecare, recreation and leisure opportunities, transportationneeds, legal and guardianship issues, education andtraining benefits, commissary and exchange access,traumatic brain injury/post-traumatic stress supportservices, and much more.The non-medical care managers are located atseven major Navy treatment facilities throughout the<strong>United</strong> <strong>States</strong>, four VA polytrauma centers, BrookeArmy Medical Center, and the USSOCOM Care Coalition.The non-medical care manager located at USSO-COM assists specifically with SOF issues.This is a program that has been around for awhile, but needs to be spread within the corpsman andmedical community. We, as a whole, need to find waysto spread this wonderful opportunity to our woundedSailors and SOF Warriors.A Navy Safe Harbor representative would beglad to visit and educate Navy medical personnel on theprogram and answer any questions pertaining to theirpatients’ care.“Enrollment eligibility is not limited to combatrelatedwounds or injuries,” said Watkins. “Sailors injuredduring liberty or through shipboard accidents, aswell as those that have incurred a serious illness,whether physical or psychological, are all welcomed intoNavy Safe Harbor.”Enrollment in Safe Harbor is voluntary. Sailorsand Coast Guardsmen may be referred to Safe Harborthrough a number of advocates, including the medicaltreatment facilities medical staff, the Wounded WarriorResource Center, or their VA clinical case manager.Families and individuals may also self-enroll throughSafe Harbor’s 24/7 toll-free care line, 877-746-8563; theWebsite, www.safeharbor.navy.mil; or sending an inquiryto safeharbor@navy.mil. USSOCOM Sailors andFamilies may contact HM2 Gatzke directly at 813-826-2601 or by email at Debora.gatzke@socom.mil.Navy Safe Harbor’s goal is to return Sailors toduty and, when not possible, work collaboratively withfederal agencies including the VA, Department of Labor,and state and local organizations to ensure successfulreintegration of Sailors back into their communities.“Navy Safe Harbor support does not end at themedical treatment facilities’ door,” said Watkins. “Thekey to Safe Harbor’s success is providing servicememberswith a lifetime of care and support.”104Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
SOF and SOF Medicine Book ListWe haven’t published the SOF reading list since the <strong>Summer</strong> 06 edition and recently received a request to republishit.Those of you who know COL Farr’s history of joining the Army at age 18 may realize that he has evidentlyconned the Army into sending him off for long term civilian schooling for his bachelor’s degree, two master’s degrees,and his doctor of medicine. Each time, he bought books. So below is his book list of military medical history and <strong>Special</strong><strong>Operations</strong> Forces history books currently in his library. For a detailed list with the publishers and date of publication,please contact the JSOM at JSOM@socom.mil.If anyone has other books they would like to add to the list, let us know. The intent is to present a concise list of thevast array of reading material available that pertains to the mission of <strong>Special</strong> <strong>Operations</strong> – both past and present.We also strongly encourage readers to write a short review for the books they have read and/or have personal firsthand knowledge concerning a specific selection. This will help maintain a high degree of content validity.TITLE AUTHOR ISBN15 Months In SOG: A Warrior’s Tour T.L. Nicholson, T.P. Nichols 080411872890 Minutes at Entebbe W. Stevenson, U. Dan 0553104829200 Years of Military Medicine R.C. EngelmanA Bugle Calls: The Story of the Witwatersr and Rifles S. Monic 62013984A Concise History of U.S. Army <strong>Special</strong> <strong>Operations</strong> Forces G.T. Barker 0922004099A Concise History of the U.S. Army Airborne Infantry G.T. Barker 0922004021A Concise History of U.S. Army Airborne Infantry G.T. Barker 0922004013A Concise History of U.S. Army <strong>Special</strong> <strong>Operations</strong> Forces G.T. BarkerA Confederate Nurse: The Diary of Ada W. Bacot A.W. Bacot, J.V. Berlin 0872499707A Confederate Surgeon’s View of Ft. Donaldson… J. StanberyA Historical Perspective of SOF as Instruments of Strategy G.D. Jones CGSC 1991A History of Medicine in South Carolina: 1825-1900 J.I. Waring, R.H. Shryock SCMAA History of Military Medicine R.A. Gabriel, K.S. Metz 031327746XA History of <strong>Special</strong> Forces in Somalia 1992-5J.D. CeleskiA Man Called Intrepid W. Stevenson 0345310233A Medical Tour Through the Whole Island of Great Britain L. Appleby 05711739XA Prototype of a Confederate Hospital Center… P.W. Houck B0006ELBYYA Saw, Pocket Instruments, and Two Ounces of Whiskey:Frontier Military Medicine in the Great Basin A.P. Sohn 0870622722A Soldier with the Arabs J.B. Glubb 0006DI81OA Soldier’s Story: The Double Life of a Confederate Spy D.L. Phillips 567994253A <strong>Special</strong> Breed of Man E. Edell 0934588082A Surgeon’s Civil War: The Letters of Daniel M. Holt J.M. Greiner, et al. 0873384946A Study of the Medical Support to the Union & ConfederateArmies During the Battle of Chickamauga: Lessons &Implications for Today’s U.S. Army Medical Department LeadersD.A. Rubenstein CGSC, 1990A Swift, Elusive Sword: What if Sun Tzu and John Boyd Dida National Defense Review? C.W. Richards 1932019014A Systematic Review of “<strong>Command</strong>o” (<strong>Special</strong>) <strong>Operations</strong>1939-1980 E. Lutwak, et al.A Texas Surgeon in the C. S. A. J.Q. Anderson 0007E4AEGA Vast Sea of Misery: A History and Guide to the Unionand Confederate Field Hospitals at Gettysburg,July 1 to November 20, 1863 G.A. Coco 0939631091A Woman Doctor’s Civil War: The Diary of Esther Hawks G. Schwartz, E.H. Hawks 0872494357A Woman of Valor: Clara Barton and the Civil War S.B. Oates 0028740122About Face: Odyssey of an American Warrior D.H. Hackworth, J. Sherman 0671526928SOF Reading List 105
TITLE AUTHOR ISBNAfrican Guerrillas C.S. Clapham 25321243XAFSOF: A Unique Application of Aerospace Power J.A. Hill AU Press, 1993Airborne: A Guided Tour of an Airborne Task Force T. Clancy 0425157709Air <strong>Command</strong>o! 1950-1975, AFSOC M.E. Haas 0006PF6DAAmerica and Guerrilla Warfare A.J. Joes 0813121817An Historical Survey: The U.S. Army Vietnam IndividualTraining Group (UITG) Program, 1971-73 K.R. Bowra AWC 1991An Intimate History of Killing:Face-To-Face Killing in Twentieth-Century Warfare J. Bourke 0465007376Angels of Mercy M.P. Oakes, I. Sumner 1885938128Any Place, Any Time, Any Where: The 1st Air <strong>Command</strong>osin WWII R.D. Van Wagner 076430447XApollo’s Warriors: USAF <strong>Special</strong> Ops during the Cold War M.E. Haas, et al. 1585660353April ‘65: Confederate Covert Action in the American CivilWar W.A. Tidwell 0873385152Army Badges and Insignia Since 1945 G. Rosignoli 0713706481Army Medical Department 1775-1818 M.C. Gillett 1410202380Army Medical Department, 1818-1865 M.C. Gillett 0160019540Army Medical Department, 1865-1917 M.C. Gillett 9994162853Army of Mississippi’s Medical Department Apr-Jul 1862 P.A. Ussery U MS Press, 1981Armed Progressive: A Study of the Military and PublicCareer of Leonard Wood J.C. Lane 0891410090Art of the Warrior R.D. Sawyer, Sun Pin 1570621632Assault at Mogadishu K. Hermann, P. Koch 0552107743Asymmetrical Warfare on the Great Plains, A Review of theAmerican Indian Wars - 1865-1891 L.S. Yarbrough AWC 2002At the Hurricane’s Eye G. Walker 0804109559Badges and Insignia of the Elite Forces L. Thompson 1854095110Battle Exhaustion: Soldiers and Psychiatrists in the CanadianArmy, 1939-1945 T.T. Copp, B. McAndrew 0773507744Behind Fascist Lines A.K. Starinov 0345444574Behind Japanese Lines: An American Guerrilla in thePhilippines R.C. Hunt, B. Norling 0813109868Belle Boyd: Siren of the South R. Scarborough 0865545553Beret Insignia of the U.S. Army W.A. Hudspeath, R.W. Smith .. B000714ZSKBlack Hawk Down: A Story of Modern War M. Bowden 0871137380Blank Check T. Weiner 0446514527Bravo Two Zero A. McNab 059303421XCambodia: Analysis of U.S. Military Assistance K.R. Bowra ACGSC 1983Casebook on Insurgency and Revolutionary Warfare P.A. Jureidini, et al. SORO, 1962Casualties & Consensus: The Historical Role of Casualtiesin Domestic Support for U.S. Military <strong>Operations</strong> E.V. Larson 0833023705Central Burma: The <strong>United</strong> <strong>States</strong> Army Campaigns ofWorld War 2 G.L. Macgarrigle 0160481376Champ Ferguson. Confederate Guerilla T. Sensing 0826512127Chimborazo: The Confederacy’s Largest Hospital C.C. Green 1572333162Civil War Medicine S.M. Brooks B0007DN1N8Civil War Medicine 1861-1865 C.K. Wilbur 0791052079Civil War Medicine: Care & Comfort of the Wounded R.E. Denney 0806908793Civil War Medicine: Challenges and Triumphs A.J. Bollet 1883620082Civil War Nurse: The Diary and Letters of Hannah Ropes H.A. Ropes, J.R. Brumgardt 0870492802Civil War Pharmacy: A History of Drugs, Drug Supply andProvision, and Therapeutics for the Union and Confederacy M.A. Flannery 0789015021Civil War Schemes and Plots W.B. Garrison 0517162873Classics of Strategy and Counsel, Volume 1 T.F. Cleary 1570627274Code-Name Bright Light: The Untold Story of U.S. POWRescue Efforts During the Vietnam War G.J. Veith 0440226503Code Name Copperhead J.R. Garner, A.M. Fine 671864351106Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
TITLE AUTHOR ISBNCohesion, the Key to <strong>Special</strong> <strong>Operations</strong> Teamwork R.E. McDonald B00010X2WCCold Injury, Ground Type T.F. Whayne 00071O36ECombat Surgeons J. Laffin 0750921730Combined <strong>Operations</strong> L. Mountbatten, H. Saunders 417987413<strong>Command</strong> and Control J.D. Mitchell 0425117774<strong>Command</strong>o Raids: 1946-1983 B. Hoffman B0006EQN60<strong>Command</strong>oes D.C. Waller 0671787179<strong>Command</strong>os and Rangers of World War II J.D. Ladd 0312151675<strong>Command</strong>os from the Sea: Soviet Naval Spetsnaz in WorldWar II Y.F. Strekhnin, J.F. Gebhardt 1557508321Come Retribution: The Confederate Secret Service and theAssassination of Lincoln W.A. Tidwell, et al. 0878053484Complete Art of War Sun Pin, et al. 0813330858Conduct of the Partisan War in the Revolutionary War South K.E. Jacobsen CGSC 2003Confederate Agent, a Discovery in History J.D. Horan B0007EW656Confederate <strong>Command</strong>o and Fleet Surgeon J.W. Lynn, D.B. Conrad 1572492201Confederate Courage on Other Fields: Four Lesser KnownAccounts of the War Between the <strong>States</strong> M.J. Crawford 786407204Confederate Hospitals on the Move: Samuel H. Stout and theArmy of Tennessee G.R. Schroeder-Lein 0872499642Confederate Spy L.A. Sigaud, B. Boyd B0007EDK7EConfederate <strong>States</strong> Medical and Surgical Journal S.P. Moore, W.D. Sharpe 0810809729Confederate Surgeon: Aristides Monteiro S. Dannett, R.H. Burkart 0396058965Confederate Surgeon: The Personal Recollections ofE.A. Craighill E.A. Craighill, P.W. Houck 0930919912Confederate <strong>Operations</strong> in Canada and New York J.W. Headley 0809442841Countering the New Terrorism I.O. Lesser, et al. 0833026674Counterinsurgency Lessons from Malaya and Vietnam:Learning to Eat Soup with a Knife J.A. Nagl 0275976955Coup d’Etat E. Luttwak 0674175476Crippled Eagle: A Historical Perspective R. Lenahan 1886391238Cushing: Civil War SEAL R.J. Schneller 1574886967Dark Lanterns: Secret Political Societies, Conspiracies andTreason Trials in the Civil War F.L. Klement 0807115673Darkmoon: Eighth Army <strong>Special</strong> <strong>Operations</strong>in the Korean War E. Evanhoe 1557502463Debris of Battle G.A. Patterson 081170498XDelta: America’s Elite Counterterrorist Force T. Griswold, D.M. Giangreco 0879386150Delta Force C.A. Beckwith, D. Knox 0151246572Desperate Deception: British Covert <strong>Operations</strong> in the<strong>United</strong> <strong>States</strong>, 1939-44 T.E. Mahl, R. Godson 1574880802Deterrence and Influence in Counterterrorism: AComponent in the War on Al Qaeda P.K. Davis, B.M. Jenkins 0833032860Diary of Dr. J. F. Shaffner, Sr: Commencing September13, 1863, ending February 5, 1865 J.F. Shaffner B00086U8U8Disease and History F.F. Cartwright 0880296909Doctor to the Front: The Recollections of ConfederateSurgeon Thomas Fanning Wood, 1861-1865 T.F. Wood, D.B. Koonce 1572330821Doctors in Blue G.W. Adams, H. Schuman 0890290865Doctors in Gray H.H. Cunningham 0844605662Dr. J. G. M. Ramsey: Autobiography and Letters J.G. Ramsey, et al. 1572331739Dr. Mudd and the Lincoln Assassination: The Case Reopened J.P. Jones 0938289500Ducimus. The Regiments of the Canadian Infantry M. Mitchell CA War Mus., 1992Early Texas Physicians 1830-1915 R.M. Hood, T.R. Fehrenbach 1880510634Edward Lansdale: The Unquiet American C.B. Currey 1574881760Elite Warriors: 300 Years of America’s Best Fighting Troops L.Q. Zedric, M.F. Dilley 0934793603Elusive Victory: The Arab-Israeli Wars, 1947-1974 T.N. Dupuy 0840378629Encyclopedia of Guerrilla Warfare I.F.W. Beckett 0874369290SOF Reading List 107
TITLE AUTHOR ISBNEyes of the Hammer B. Mayer 0312928629Euphemia Mary Goldsborough, 1836-1896, Exile to SweetDixie: The Story of Euphemia Goldsborough, ConfederateNurse and Smuggler E.F. Conklin, E.M. Goldsborough 1577470443Faded Coat of Blue O. Parry 0380797399Farmcarts to Fords: A History of the Military Ambulance J.S. Haller 0809318172Field Medical Services at the Battles of Manassas H.H. Cunningham 0935523170Field Surgeon at Gettysburg C.B. Kernek 1878208322Fighting Elite I. Padden 0553253581Fighting for Life A.E. Cowdrey 0029068355Fighting in the Streets: A Manual of Urban Guerilla Warfare Urbano 094263747XForeign Internal Defense Does Air Force <strong>Special</strong> <strong>Operations</strong>Have What it Takes? M.C. Koster B00010X5QUFoundation for Victory: <strong>Operations</strong> and Intelligence HarmoniouslyCombine in Jackson’s Shenandoah Valley Campaign (1862) S.B. Smith NPS, 1993Fourth Dimension of Warfare. Vol. 1 Intelligence /Subversion / Resistance M. Elliott-Bateman 0719004373From a Dark Sky O. Kelly 0671009176From OSS to Green Berets: The Birth of <strong>Special</strong> Forces A. Bank 0891412719From the Sierra to the Cities: The Urban Campaign of theShining Path G.H. McCormick 0833012320Gangrene and Glory: Medical Care During the AmericanCivil War F.R. Freemon 0838637531The Generals’ War: The Inside Story of theConflict in the Gulf M.R. Gordon, B.E. Trainor 0316321729General Crook & Counterinsurgency Warfare W.L. Greenberg CGSC 2001Georgia’s Confederate Hospitals M. Jordan Emory U., 1942Ghost Force: Secret History of the SAS K. Connor 0752826972Ghost Soldiers: The Forgotten Epic Story of World War II’sMost Dramatic Mission H. Sides 0385495641Green Berets at War S.L. Stanton 0804118841Green Berets Seals and Spetsnaz J.M. Collins 0080357466Green Berets: Unconventional Warriors H. Halberstadt 0891412808Guerilla E.P. Hoyt 0025552104Guerilla Surgeon L. Rogers B0006DBYX8Guerilla Warfare C. Guevara, et al. 0803270100Guerrilla Warfare: A Historical & Critical Study W. Laqueur 0765804069Guerrillas, Unionists and Violence on the ConfederateHome Front D.E. Sutherland 1557285497Hard to Forget S.M. Yedinak 0804118094Hazardous Duty: An American Soldier in the 20th Century J. Singlaub, M. McConnell 0671705164Heart’s Work: Civil War Heroine and Champion of theMentally Ill, Dorothea Lynde Dix C. Schlaifer, L. Freeman 1557784191Heavy Hook (<strong>Command</strong> and Control, No 4) J.D. Mitchell 0425127281Heavy Matter: Urban <strong>Operations</strong>’ Density of Challenges R.W. Glenn 0833029096Hippocrates in a Red Vest: The Biography of aFrontier Doctor B.B. Beshoar 0910118310History of Medicine in Alabama H.L. Holley 0817300856History of the Combat Support BranchesL.W. LaFramboiseHospital Life Within the Confederate Medical Department C.D. BarnettHospital Medicine in Richmond, VA during the Civil War: AStudy of Hospital No. 21, Howard’s Grove & Winder Hospitals C.F. BallouHospital Sketches L.M. Alcott 0918222788Humanitarian Intervention: Assisting the Iraqi Kurds inOperation Provide Comfort, 1991 G.W. Rudd B0006RRQRCHunter Holmes McGuire: Doctor in Gray J.W. Schildt 0093677202Hunting the Jackal B. Waugh, T. Keown 0060564091108Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
TITLE AUTHOR ISBNI Acted from Principle: The Civil War Diary of Dr. William M.McPheeters, Confederate Surgeon in the Trans-Mississippi(The Civil War in the West) C.D. Pitcock, et al. 1557287252Illustrated Guide to Modern Elite Forces M. Walmer 0668060646In Hospital and Camp: The Civil War Through the Eyes ofits Doctors and Nurses H.E. Straubing 0811716317In Search of the Warrior Spirit R. Strozzi-Heckler, G. Leonard 1556431163In the Combat Zone: <strong>Special</strong> Forces Since 1945 R. Neillands 0814757952India-Burma. The U.S. Army campaigns of World War II D.W. Hogan 0160358817Inside the Blue Berets S.J. Zaloga 0891413995Inside the Green Berets C.M. Simpson 0425091465Intelligence <strong>Operations</strong> of the Army of the Cumberlandduring Tullahoma and Chickamauga D.D. Broome CGSC 1989Jedburgh Team <strong>Operations</strong> in Support of the 12thArmy Group S.J. LewisB0006DA8FIJoseph Jones, M.D: Scientist of the Old South J.O. Breeden 0813112966Kate: The Journal of a Confederate Nurse K. Cumming, et al. 080712267XKilling Pablo: The Hunt for the World’s Greatest Outlaw M. Bowden 0871137836Knight’s Cross A. Bank, E.M. Nathanson 0843937246Kommando: German <strong>Special</strong> Forces of World War Two J.S. Lucas 030435127XLeave No Man Behind: U.S. <strong>Special</strong> Forces Raids andRescues from 1945 to the Gulf War D.C. Isby 0297846744Lessons for Contemporary Counterinsurgencies:The Rhodesian Experience B. Hoffman, et al. 0833011235Letters and Journal of a Civil War Surgeon S.J. Petrie, M.W. Robinson 1571970959Letters to Laura: A Confederate Surgeon’s Impressions ofFour Years of War U.G. Owen, et al. 0961652632LIC 2010: <strong>Special</strong> <strong>Operations</strong> & Unconventional Warfarein the Next Century R. Paschall 0080359825Lieutenant Ramsey’s War: From Horse Soldier to Guerrilla<strong>Command</strong>er E.P. Ramsey, S.J. Rivele 1574880527Little by Little M.B. Tyquin 1876439157Looking for Trouble P. De la Billiere 0002552450Lost Crusade: America’s Secret Cambodian Mercenaries P. Scott 1557508461Low-Intensity Conflict: The Pattern of Warfare in the ModernWorld L.B. Thompson 066920045XMACV-SOG <strong>Command</strong> Histories(Annexes A, N & M 1964-1966) C.F. Reske 0939427621MACV-SOG <strong>Command</strong> History Annex B 1971-1972 C.F. Reske 0939427613MACV-SOG <strong>Command</strong> History Annex B 1971-1972:The Last Secret of the Vietnam War C.F. Reske 0939427605Madness, Malingering and Malfeasance: The Transformationof Psychiatry and the Law in the Civil War Era R.G. Lande 1574883526Manual of Confederate Surgery J.J. Chisolm 0890290687Masters of Chaos: The Secret History of the <strong>Special</strong> Forces L. Robinson 1586482491Medical Cover-Ups in the White House L. Curry, E.B. MacMahon 0918535018Medical Department of the U.S. Army in the Civil War L.C. Duncan 0942211308Medical Histories of Confederate Generals J.D. Welsh 0873385055Medical Histories of Union Generals J.D. Welsh 0873385527Medical Materiel Support to the Army of the Potomac A.E. Rhodes AWC, 1991Medical Practices in the Civil War S.P. Beller 1558702644Medical Recollections of the Army of Potomac J. Letterman 1877791016Medical Roots: The Evolution of Modern Support Doctrinein the American Civil War M.E. Turner AWC, 1983Medicine: For Mountaineering & Other Wilderness Activities5th Edition J.A. Wilkerson (Editor) 0898867991Medicine in Virginia in the Nineteenth Century W.B. Blanton B0006AMBZ6Medicine Under Sail Z. Friedenberg 1557502978SOF Reading List 109
TITLE AUTHOR ISBNMemoranda During the War W. Whitman, P Coviello 1557091323Memories: A Record of Personal Experience and AdventureDuring Four Years of War F.A. Beers 0809444704Merrill’s Marauders E.P. Hoyt 052341529XMerrill’s Marauders: February to May, 194478813275XMicrobes and Minnie Balls: An Annotated Bibliography ofCivil War Medicine F.R. Freemon 0838634842Mike Force H. Burrus 0671669451Military Leadership: In Pursuit of Excellence R.L. Taylor, W.E. Rosenbach 0813330246Mobile Guerrilla Force J.C Donahue 0312961642Modern Guerrilla Warfare: Fighting Communist GuerrillaMovements, 1941-1961 F.M. Osanka B0006AXT6GMountain and Arctic Warfare: From Alexander to Afghanistan B. Gregory 1852600144Mountain Troops and Medics: Wartime Stories of a FrontlineSurgeon in the U.S. Ski Troops A.H. Meinke 0963374206My <strong>Command</strong>o <strong>Operations</strong>: The Memoirs of Hitler’s MostDaring <strong>Command</strong>o O. Skorzeny, D. Johnston 0887407188New York City Draft Riots: Their Significance for AmericanSociety and Politics in the Age of the Civil War I. Bernstein 0195050061North Korean <strong>Special</strong> Forces J.S. Bermudez 1557500665Not a Good Day to Die S. Naylor 0425196097Number and Losses in the Civil War in America 1861-65 T.L. Livermore 052757600XOn Guerrilla Warfare Mao, S.B. Griffith 0252068920On Killing: The Psychological Cost of Learning to Kill inWar and Society D. Grossman 0316330000On Wings of Eagles K. Follett 0451131517One Hundred Unorthodox Strategies M. Sawyer, et al. 0813328616One Surgeon’s Private War: Doctor William W. Potter of the57th New York W.W. Potter, J.M. Priest 1572490217Operation Enduring Freedom: October 2001-March 2002 R.W. Stewart 0160515890Operation Rollback: America’s Secret War Behind theIron Curtain P. Grose 0395516064<strong>Operations</strong> Against Enemy Leaders S.T. Hosmer 0833030280Orthopedic Injuries of the Civil War: An Atlas of OrthopedicInjuries and Treatments During the Civil War J.E. Kuz, B.P. Bengtson 0963586173Out of the Mist: The Foundation of Modern Pathologyand Medicine During the Nineteenth Century H.M. Milking 0963768905Outlines of the Chief Camp Diseases of the <strong>United</strong> <strong>States</strong>Armies J.J. Woodward, I.M. Rutkow 0930405439Oxford Handbook of Tropical MedicineM. Eddleston, R. Davidson,R. Wilkinson, S. Pierini 0198525095Pamwe Chete (Selous Scouts) R.F. Ried-Daly 0620237562Parachute Badges and Insignia of the World: In Colour J.R. Bragg, R. Turner 0713708824Partisan Hospitals in Yugoslavia, 1941-1945 D. Dragic B0006BXY7YPartisan Warfare 1941-45 T.P. Abbott 0850455138Perilous Options: <strong>Special</strong> <strong>Operations</strong> as an Instrument ofU.S. Foreign Policy L.S. Vandenbroucke 0195045912Phoenix and the Birds of Prey M. Moyar, H.G. <strong>Summer</strong>s 1557505934Physician-Generals in the Civil War: A Study in 19th Mid-Century American Medicine P.E. Steiner 0398018537Pictorial Encyclopedia of Civil War Medical Instrumentsand Equipment, Vol. I, II, and III. G.E. Dammann 0933126328Piercing the Reich: The Penetration of Nazi Germany byAmerican Secret Agents During World War II J.E. Persico 076070242XPrairie Fire K. White 0938936077Project Omega: Eye of the Beasts J.E. Acre 1555715117Psychological <strong>Operations</strong>: Principles and Case Studies F.L. Goldstein, B.F. Findley 9996617491Queen Victoria’s Gene D.M. Potts, W.T.W. Potts 0750908688110Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
TITLE AUTHOR ISBNRats, Lice, & History H. Zinsser 0333395670Red Berets and Red Crosses C. Naill 908047181XReflections of a Warrior F.D. Miller, et al. 0671753967Regimental Losses in the American Civil War W.F. Fox 0890290075Reminiscences of the Cuban Revolutionary War C. Guevara 0237716321Repairing the March of Mars: The Civil War Diaries ofJohn Samuel Apperson, Hospital Steward in theStonewall Brigade, 1861-1865 J.H. Roper, et al. 0865547793Resting Rebels: A Medical History of the San AntonioConfederate Cemetery W.D. Farr 1990Rorke’s Drift 1879: Pinned Like Rats in a Hole I .Knight, et al. 1855329514Sabotage and Subversion: The SOE and OSS at War I Dear 0304352020Saddle Bag and Spinning Wheel: Being the Civil War lettersof George W. Peddy, M.D., Surgeon, 56th Ga. Vol. Reg.,C.S.A. and his Wife Kate Featherston G.W. Peddy, et al. 0865540047Sage of the OSS J. Sage 0440075807Science and Medicine in the Old South R.L. Numbers, T.L. Savitt 0807114642Secret Armies: Inside the American Sovietand European <strong>Special</strong> Forces J. Adams 0871132230Secret Army, Secret War: Washington’s Tragic Spy Operationin North Vietnam S.D. Tourison 1557508186Secret <strong>Command</strong>os J.L. Plaster 0684856735Secret Missions of the Civil War P. Stern 0517000024Secret Soldier: The True Life Story of Israel’s Greatest<strong>Command</strong>o M. Betser, R. Rosenberg 0871136376Secret Soldiers: <strong>Special</strong> Forces in the War Against Terrorism P. Harclerode, M. Dewar 0304355070Secret War in North Vietnam D. Andrade, K. Conboy 0700610022Secret Warriors: Inside the Covert Military <strong>Operations</strong> ofthe Reagan Era S. Emerson 0399133607Semi-regular and Irregular Warfare in the Civil War E.C. BarksdaleShadow Warriors: Inside the <strong>Special</strong> Forces T. Clancy, et al. 0399147837Shadows of Glory O. Parry 0380820870Sideshow W. Shawcross 0671230700Simon Baruch: Rebel in the Ranks of Medicine, 1840-1921 P.S. Ward 0817305890Snake Eater D. Bendell 0440211417SOG J.L. Plaster 1581600585SOG, MACV Studies and Observations Group: BehindEnemy Lines, 4 volumes H. Saal 0962597031SOG: The Secret Wars of America’s <strong>Command</strong>os in Vietnam J.L. Plaster 0684811057Soldier Under Three Flags: Exploits of <strong>Special</strong> Forces’Captain Larry A. Thorne H.A. Gill, L.A. Thorne 0934793654Soldiers on Skis F. Whitlock, B. Bishop 0873646762Soldiers, Spies, and the Rat Line: America’s Undeclared WarAgainst the Soviets J.V. Milano, P. Brogan 1574880500Source Book of Medical History L. Clendening 0486206211Spec Ops: Case Studies in <strong>Special</strong> <strong>Operations</strong> Warfare W.H. McRaven 891415440<strong>Special</strong> Forces: A Guided Tour of U.S. Army <strong>Special</strong> Forces T. Clancy, J. Gresham 0425172686<strong>Special</strong> Forces: The Changing Face of Warfare M. Lloyd 1854091700<strong>Special</strong> Forces in the Invasion of France, Histoire& Collections P. Gaujac 2908182947<strong>Special</strong> Forces of the <strong>United</strong> <strong>States</strong> Army 1952-82 I. Sutherland 0912138432<strong>Special</strong> <strong>Operations</strong> Forces: An Assessment J.M. Collins 0160431913<strong>Special</strong> <strong>Operations</strong> Forces and Elusive Enemy Ground Targets:Lessons from Vietnam and the Persian Gulf War W. Rosenau 083303071X<strong>Special</strong> <strong>Operations</strong> in the American Civil War A.M. Raper CGSC, 1996<strong>Special</strong> <strong>Operations</strong> in <strong>United</strong> <strong>States</strong> Strategy 0160016126Spetsnaz: The Inside Story of the Soviet <strong>Special</strong> Forces V. Suvorov 0393026140SOF Reading List 111
TITLE AUTHOR ISBNSpies and <strong>Command</strong>os: How America Lost the SecretWar in North Vietnam D. Andrade, K.J. Conboy 0700610022War in the Shadows: The Guerrilla in History R.B. Asprey 0688128157Spies and Spymasters of the Civil War D.E. Markle 08180227XSpies for the Blue and Gray H.T. Kane 385014643Spies! Women in the Civil War P. Colman 1558702679Spy of the Rebellion: Being a True History of the SpySystem of the <strong>United</strong> <strong>States</strong> Army During the LateRebellion, Revealing Many Secrets of the War A. Pinkerton 0803287224Stonewall Jackson’s Surgeon Hunter Holmes McGuire M.F. Shaw 1561900478Subnational Conflict in the Mediterranean Region B.M. Jenkins, M. Ghimire 9993340715Sun Pin: The Art of Warfare Sun. Pin, et al. 0345379918Sun Tzu J.H. Huang, Sun Tzu 0688124003Sun Tzu’s Art of War: The Modern Chinese Interpretation T. Hanshang, Y. Shibing 0806927895Sun-Tzu: The Art of War R.T. Ames, Sun Tzu 034536239XSunzi Speaks T.C. Chung, B. Bruya 0385472587Swords of Lightning: <strong>Special</strong> Forces and the ChangingFace of Warfare T. White 0080409768Tabulating Equipment and Army Medical Statistics A.G. Love, et al. B0007DX0NYTailwind: A True Story R.V. Buskirk 0849903416Tarnished Scalpels: The Court-Martials of Fifty UnionSurgeons T.P. Lowry, J.D. Welsh 0811716031Team Sergeant W.T. Craig 0804117144Terror Out of Zion: Irgun Zvai Leumi, Lehi and thePalestine Underground, 1929-1949 J.B. Bell 0380393964The Air Force Role in Low-Intensity Conflict D.J. Dean B0006EL93CThe Art of Rulership: A Study of Ancient ChinesePolitical Thought R.T. Ames, Huai-Nan 0791420620The Art of War Sun Tzu 1570629781The Art of War Sun Tzu, J. Minford 0670031569The Art of War Sun Tzu, J. Clavell 0385299850The Art of Strategy: A New Translation of Sun Tzu R.L. Wing, Sun Tzu 0385237847The Art of War: In Sun Tzu’s Own Words Sun Tzu, G. Gagliardi 1929194005The Bay of Pigs: The Leaders’ Story of Brigade 2506 H.B. Johnson 0393042634The Black Devil Brigade: The True Story of the First <strong>Special</strong>Service Force in World War II J.A. Springer 0935553509The Black Scalpel G. Parker 0718300815The Cape Town Highlanders, 1885-1970 N.D. Orpen B0006CRUVYThe CIA’s Secret War in Tibet K.J. Conboy, J. Morrison 0700611592The Civil War Letters of Dr. Harvey Black: A Surgeonwith Stonewall Jackson H. Black, et al. 0935523456The Company They Keep A.J. Simons, C. Bolte 0684828162The Confederate Cause and Conduct in the War Betweenthe <strong>States</strong> H.H. McGuire, G.L. Christian 0964149109The Country Team R. Moore B0006BOOEQThe Dahlgren Affair: Terror and Conspiracy in the Civil War D.P. Schultz 0393046621The Devil’s Brigade R.H. Adleman, G.H. Walton 1591140048The Eagle’s Talons: The American Experience at War D.M. Drew, D.M. Snow 1410200698The Elite: The Story of the Rhodesian <strong>Special</strong> Air Service B. Cole 0620074213The Evolution of Preventive Medicine in the US Army S. Bayne-Jones 1114667943The Fall of Eben Emael J. Mrazek 0891416641The German Northern Theater of <strong>Operations</strong>, 1940-1945 E.F. Ziemke B0007ETEOMThe Golden Jubilee of the Association of Military Surgeonsof the <strong>United</strong> <strong>States</strong>, a History of its First Half-Century-1891-1941 E.E. Hume B0007EZYV4The Great Raid on Cabanatuan W.B. Breuer 0471037427The Green Berets R. Moore 0312984928The Healers: A History of American Medicine J. Duffy 0252007433112Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
TITLE AUTHOR ISBNThe Healer’s Road J.L. Reasoner 0515117625The Hunt for Bin Laden R. Moore 0375508619The Illustrated Art of War Sun Tzu, T. Cleary 1570624224The Imperial War Museum Book of War Behind Enemy Lines J.F. Thompson157488381XThe Intrepid Guerrillas of North Luzon B. Norling 0813121183The Jungle is Neutral F. Spencer-Chapman 0583128165The Killing of Reinhard Heydrich: The SS Butcher of Prague C.A. MacDonald 0306808609The Kinder, Gentler Military S. Gutmann 0684852918The Lincoln Conspiracy D.W. Balsiger, C.E .Sellier 091721403XThe Man Who Tried to Burn New York, N.H. Brandt 0425119181The Medical Support System for the Confederate Army ofTennessee During the Georgia Campaign, May-Sept. 1864 F.R. Freemon TN Hist. Q., 1993The Medics’ War. <strong>United</strong> <strong>States</strong> Army in the Korean War A.E. Cowdrey B0006ELAA4The One That Got Away C. Ryan 1574881566The Parachute Ward: A Canadian Surgeon’s WartimeAdventures in Yugoslavia B.J. Street 0886191033The Partisans, <strong>United</strong> <strong>States</strong> Holocaust Memorial Museum Y. Arad 0896040100The Protected Will Never Know L. Wade 0804117136The Roots of Counter-Insurgency: Armies andGuerrilla Warfare I.R. Beckett 0713719222The Secret War Against Hanoi: Kennedy and Johnson’s Useof Spies, Saboteurs, and Covert Warriors in North Vietnam R.H. Shultz 0060194545The Secret War for the Union: The Untold Storyof Military Intelligence in the Civil War E.C. Fishel 0395742811The Secret War Report of the OSS A.C. Brown 0425032531The Seven Military Classics of Ancient China R.D. Sawyer 0813312280The Silent War: South African Recce <strong>Operations</strong> 1969 to 1994 P. Stiff 1919854045The Six Secret Teachings on the Way of Strategy R.D. Sawyer, et al. 1570622477The Social Transformation of American Medicine P. Starr 0465079342The Southern Soldier’s Health Guide J.S. Wilson 1877791075The Soviet Partisan Movement, 1941-1944: A CriticalHistoriographical Analysis L.D. Grenkevich, D.M. Glantz 0714644285The Story the Soldiers Wouldn’t Tell: Sex in the Civil War T.P. Lowry 0811715159The Story of the Arab Legion J.B. Glubb B0007J7994The Sword and the Olive: A Critical History of the IsraeliDefense Force M.L. Van Creveld 1891620053The Tao of War Wang Chen, R.D. Sawyer 0813340810The Tao of Peace Wang Chen, R.D. Sawyer 1570625115The Tao of Spycraft: Intelligence Theory and Practice inTraditional China R.D. Sawyer 0813333032The Uncivil War: Irregular Warfare in the Upper South,1861-1865 R.R. Mackey 0806136243The Vietnams of the Green Berets G.M. Patric B0006EKUAAThe War Between the Spies: A History of EspionageDuring the American Civil War A. Axelrod 0871134829The War for the Cities R. Moss 0698104498The Witch Doctor M. Temchin 0896040453The Wounded River: The Civil War Letters of John VanceLauderdale, M.D. J.V. Lauderdale, P. Josyph 0870133284The Wrong War: Why We Lost in Vietnam J. Record 155750699XTheory and Practice in American Medicine G.H. Brieger 0882021583This Awful Drama: General Edwin Gray Lee, C.S.A. andHis Family A.L. Levin 0533072425Trends in Outside Support for Insurgent Movements D.L. Byman, et al. 0833030523True Americanism: Green Berets and War Resisters D.M. Mantell 0807724297Twilight Warriors: Inside the World’s <strong>Special</strong> Forces M.C. Arostegui 0312152345Ukrainian Resistance Movement-Medical Services M. Ripeckyi 0920092306SOF Reading List 113
TITLE AUTHOR ISBNUnconventional Warfare: Rebuilding U.S. <strong>Special</strong><strong>Operations</strong> Forces S.L. Marquis 0815754752Uneasy Warriors: Coming Back Home V. Coppola 1563521970<strong>United</strong> <strong>States</strong> Army in World War II: <strong>Special</strong> Studies Military RelationsBetween the <strong>United</strong> <strong>States</strong> and Canada 1939-1945 S.W. Dziuban 0160018714<strong>United</strong> <strong>States</strong> Army Logistics, 1775-1992: An Anthology C.R. Shrader, J.W. Mountcastle 0898755301U.S. Army <strong>Special</strong> Forces, 1961-1971 F.J. Kelly B0006C7SMKU.S. Army Counterinsurgency and Contingency <strong>Operations</strong>Doctrine, 1860-1941 A.J. Birtle 0788173278U.S. Army Heraldic Crests: A Complete Illustrated Historyof Authorized Distinctive Unit Insignia B.J. Stein, P.J. Capelotti 0872499634U.S. Army <strong>Special</strong> <strong>Operations</strong> In World War II D.W. Hogan 141021690XU.S. Army <strong>Special</strong> Warfare: Its Origins A.H. Paddock 0700611770U.S. <strong>Special</strong> <strong>Operations</strong> Forces in Action:The Challenge of Unconventional Warfare T.K. Adams 0714643505USA Airborne 50th Anniversary Commemorative Edition B. Hagerman 0938021907War in Cambodia 1970-75 K. Conboy, K.R. Bowra 85045851XWar in the Shadows, Volumes 1 & 2 R.B. Asprey 0385034709Warrior Politics: Why Leadership Demands a Pagan Ethos Robert D. Kaplan 0375505636Weapon of Choice C.H. Briscoe, et al. ACGSC 2003When Sherman Marched North from the Sea:Resistance on the Confederate Home Front J. Glass-Campbell 0807828092White Dragon Two K. Sibounheuang 1885354142White Roses: Women Nurses in the Civil War R.D. Larson 1577470117White Tigers: My Secret War in North Korea B.S. Malcom, R. Martz 1574881981Who’s Who from MACV-SOG S. Sherman 1996With Courage and Delicacy: Civil War on the Peninsula:Women and the U.S. Sanitary Commission N. Scripture-Garrison 1882810392Women at the Front: Hospital Workers in Civil War America J.E. Schultz 080782867XYellow Fever and the South M. Humphreys 0813518202Yoni Netanyahu: <strong>Command</strong>o at Entebbe D. Newberger-Speregen 0827606427You’re No Good to Me Dead: Behind Japanese Lines in thePhilippines R. Stahl 1557507937New Additions since first list: 1A Hundred Osamas: Islamist Threats & the Future ofCounterinsurgency S. Zuhur SSI 2005A Murder in Wartime: The Untold Spy Story That Changedthe Course of the Vietnam War J. Stein 0312070373Age of the Guerrilla F. Sully 0380023318American Soldier T. Franks 0060731583Auguste Blanqui and the Art of Insurrection S. Bernstein 0853152438Chariots of the Damned: Helicopter <strong>Special</strong> <strong>Operations</strong>from Vietnam to Kosovo M. McKinney, M. Ryan 0312291183Charlie Wilson’s War G. Crile 0802141242Combat in Russian Forests and Swamps 0160019451Counterinsurgency Warfare D. Galula 0275989410Crisis Fleeting - Original Reports on Military Medicinein India and Burma in the Second World War J.H. Stone B000BKRZL6Daring to Win: <strong>Special</strong> Forces at War D. Eshel 1854091557Duel for Kilimanjaro: An Account of the East AfricanCampaign, 1914-1918 L.O. Mosley B0007EE85CEffects of Climate on Combat in European Russia 9997584538Fatal Glory: Narciso Lopez and the First Clandestine U.S.War Against Cuba T. Chaffin 0813916739Five Years to Freedom J.N. Rowe 0345314603German Defense Tactics Against Russian Breakthroughs 9990202907114Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
TITLE AUTHOR ISBNGuerilla warfare N.M. Blair B0007JTGE0Guerrilla D. Rooney 1857533526Guerrilla and Terrorist Organizations: World Directory andBibliography P. Janke 0029161509Guerrilla Strategies: An Historical Anthology from the LongMarch to Afghanistan G. Chaliand 0520044444Guerrilla Warfare: Che Guevara E.C. Guevara 0803270755Guerrillas J.L. Anderson 0142004979Honduras To Haiti: Five Years In The Life Of A <strong>Special</strong>Forces Sergeant R.W. Johnson 1410792781Imperial Grunts R.D. Kaplan 1400061326Insurgency & Terrorism: Inside Modern RevolutionaryWarfare B.E. O’Neill, E.C. Meyer 1574883356Insurgency and Counterinsurgency in the 21st Century S. Metz 1584871792JSOU/NDIA Essays 2004-5Kitchener: Architect of Victory, Artisan of Peace J. Pollock 0786708298Lapham’s Raiders: Guerrillas in the Philippines, 1942-1945 R. Lapham, B. Norling 0813119499Lettow-Vorbeck’s Soldiers W. Dobbertin 089839340XMacarthur’s Undercover War: Spies, Saboteurs, Guerrillas,and Secret Missions W.B. Breuer 0785820485Medical Support of the Army Air Forces in World War II M.M. Link 0912799692Medicine: For Mountaineering & Other WildernessActivities 5th Edition, J.A. Wilkerson, (Editor) 0898867991Military Improvisations During the Russian Campaign 0160019443Military Improvisations During the Russian Campaign 1410220842Modern Insurgencies and Counter-Insurgencies; Guerrillasand Their Opponents Since 1750 I.F.W. Beckett 0415239346Modern Irregular Warfare: In Defense Policy and as aMilitary Phenomenon F.A. Heydte 0933488491Mogadishu! K. DeLong, S. Tuckey 0275949257My Reminiscences of East Africa P. Lettow-Vorbeck 0898391547Night Combat A. Toppe 0788170805Night Stalkers: 160th <strong>Special</strong> <strong>Operations</strong> Aviation Regiment(Airborne) F. Pushies 0760321418Non-state Threats and Future Wars R. Bunker 0714683086Operationalizing COINJ. Celeski<strong>Operations</strong> of Encircled Forces - German Experiences in WWIIB000AW7DIAOSS R.H. Smith 1592287298Oxford Handbook of Tropical MedicineM. Eddleston, S. Pierini,R. Wilkinson, R. Davidson 0198525095Red Acropolis, Black Terror: The Greek Civil War and theOrigins of Soviet-American Rivalry, 1943-1949 A. Gerolymatos 0465027431Resisting Rebellion: The History and Politics of CounterinsurgencyA.J. Joes 0813123399Revolutionary War in World Strategy, 1945-1969 R.G. Thompson, 0800867858Rumsfeld’s War: The Untold Story of America’s Anti-Terrorist <strong>Command</strong>er R. Scarborough 0895260697Russian-Soviet Unconventional Wars in the Caucasus,Central Asia, and Afghanistan R. Baumann 0160419530SAS: With the Maquis I. Wellsted 85367186XSharp Corners: Urban <strong>Operations</strong> at Century’s End R.J. Spiller B0006RP25USmall Unit Actions During the German Campaign in RussiaB000AMB17YSoldiers to the Rescue. The Medical; Responce to the PentagonAttack.S. Marble, E. Milhider<strong>Special</strong> Men and <strong>Special</strong> Missions: Inside American <strong>Special</strong><strong>Operations</strong> Forces, 1945 to the Present J. Nadel, J.R. Wright 1853671592Stoic Warriors N. Sherman 0195152166SOF Reading List 115
TITLE AUTHOR ISBNSub Rosa S. Alsop 0156863006Tanganyikan GuerrillaJ.R. SibleyTerrain Factors in the Russian Campaign016001946XThe Art of War Plus The Ancient Chinese Revealed Sun Tzu 1929194196The Dressing Station: A Surgeon’s Chronicle of War andMedicine J. Kaplan 0802117074The First Professional Revolutionist E.L. Eisenstein 0674304004The Medical Department: Medical Service in the WarAgainst Japan M. Condon-Rall, A. Cowdrey 0160492653The Philippine War, 1899-1902 B.A. Linn 0700612254The Politics of Resistance in France, 1940-1944: A Historyof the Mouvements unis de la Résistance J. Sweets 0875800610The Propensity of Things: Toward a History of Efficacy inChina F. Jullien, J. Lloyd 0942299949The Shadow Warriors: O.S.S. and the Origins of the C.I.A. B.F. Smith 0233975772The Shining Path: A History of the Millenarian War in Peru G.G. Ellenbogen, G. Gorriti 0807846767The Withered Vine C.R. Shrader 0275965449The Women Who Lived for Danger M. Binney 0060540877The Zapatista Social Netwar in Mexico D. Ronfeldt, et al. 0833026569Theoretical Perspectives of Terrorist Enemies as Networks R.G. SpulakThey fought alone J. Keats B0006AYKWITito’s Partisans 1941-45 V. Vuksic 1841766755U.S. <strong>Special</strong> <strong>Operations</strong> Forces in the Cold War L. Thompson 1853675067<strong>United</strong> <strong>States</strong> Army and World War 2: Selected Papers Fromthe Army’s Commemorative Conferences J.L. Bellafaire 016049589XWar of the Flea: Classic Study of Guerrilla Warfare R. Taber, B.E. O’Neill 1574885553War Stories of the Green Berets H. Halberstadt 076031974XWarfare in the Far North W. Erfurth 00075X6Wilderness Medicine: Management of Wilderness andEnvironmental Emergencies. P. Auerbach, MD 0323032281Witness to War: An American Doctor in El Salvador C. Clements 0553050648The following is a compiled list of SOF related books recommended for your reading by those who were there. This list is complementsof Len Blessing. Every attempt is made to maintain the list’s integrity with respected and legitimate works. I have removedthe books that duplicated COL Farr’s list. Readers who feel a selection does not merit inclusion are encouraged to contact us with disputes.TITLEAUTHOR00:19:57 Dave F. StaffordA Tear For SomaliaDouglas T. Collins(Written by a Brit who married a Somali woman while serving as amember of the British Camel Corps after the end of WWII.Not a history, but it does give insight into Somali society.)A Very Short WarJohn F. Guilmartin Jr(About the last gunfight and the last sacrifices of the Vietnam-erawar in the recovery of the crew and ship SS Mayaguez in 1975.)Advice and Support: The Early YearsRonald H. SpectorAirborne and “<strong>Special</strong> Forces”Hans Halberstadt(non-fiction, good quick references, especially for family or civilians)American GuerrillaUnknown(WW II U.S. led guerrillas in Phillipines)Band of BrothersStephen Ambrose(A great story about “E” Company, 506th PIR, 101st ABN Division in WWII.)Battle for the Central Highlands: A <strong>Special</strong> Forces StoryGeorge E. DooleyBeyond Nam DongRoger Donlon116Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
TITLEAUTHORBlack Eagles(Fiction)Blackburns Headhunters(Part of a series of books on the area from Turkey to Tibet.Well researched and an excellent view of the region, its history,and various societies that live within the region.)Blackjack -33: With <strong>Special</strong> Forces in the Viet Cong Forbidden ZoneBlackjack -34 (Previously titled “No Greater Love”)Break Contact Continue Mission(Fiction)Bunard: Diary of a Green BeretChe Guevarra on Guerrilla WarfareCovert WarriorDanger Close(Non-fiction. SF member charged with murder in a bar fight within3 days of graduation from the Q Course.)Fighting Men: Stories of SoldieringFire Your FPL’sFive FingersFive Years To FreedomFlags of our FathersForeign Devils on the Silk Road(Part of a series of books on the area from Turkey to Tibet.Well researched and an excellent view of the region, its history, andvarious societies that live within the region.)Greatest Rescue Mission(Ranger operation to free POWs in the Philippines)Green Berets at War: U.S. Army <strong>Special</strong> Forces in Asia 1956-1975Green Berets in the Vanguard: Inside <strong>Special</strong> Forces 1953-1963Guerrilla Warfare: On Guerrilla WarfareHazardous DutyHell In A Very Small Place(Siege of Dien Bien Phu)Ho Chi Minh: A LifeIn The Village of the ManInside Al Qaeda, Global Network of TerrorInside Delta Force: The story of America’s elite counterterrorist unitInside the Green Berets: The First Thirty YearsIt Doesn't Take A HeroLaos: War and RevolutionLike Hidden Fire(Part of a series of books on the area from Turkey to Tibet.Well researched and an excellent view of the region, its history, andvarious societies that live within the region.)Logistical Support of <strong>Special</strong> <strong>Operations</strong> Forces During<strong>Operations</strong> Desert Shield and Desert StormLong Shadows(Fiction)Lost Crusader: The Secret Wars of CIA Director William ColbyLove and DutyMedal Of HonorMemories Of Maggie: Martha Raye: A Legend Spanning Three WarsMy American JourneyMy Secret WarNight Jungle <strong>Operations</strong>Night of the Silver Starts: The Battle of Lang VeiLarry CollinsCOL Donald BlackburnJames C. DonahueJames C. DonahueRaymond D. HarrisLarry CrileErnesto GueverraWarner SmithMike YonJim MorrisMike Di RoccoGayle RiversJames N. RoweJames Bradley; Ron PowersPeter HopkirkShelby L. StantonChalmers Archer Jr.Mao Tse tungDavid H. Hackworth (COL); Tom MathewsBernard FallWilliam J. DurkerLoyd LittleRohan GunaratnaEric L. HaneyCharles M. Simpson IIINorman H. Schwarzkopf (GEN Ret); Peter PetreNina S. Adams (Ed)Peter HopkirkDonald W. BettsKent WhiteJohn PradosBen and Anne PurcellRoy P. BenavidezNoonie FortinColin Powell (GEN Ret); Joseph E. PersicoRichard S. DruryThomas B. BennettWilliam R. PhillipsSOF Reading List 117
TITLEAUTHORNo Surrender(Japanese soldier who evaded capture and survived 30 years inthe Philippines; it’s a great book about perseverance andcommitment to warrior ideals.)Once A Warrior King: Memories of an Officer in VietnamO O T W Target CubaOperation VultureOSS to Green BeretsParthian ShotPathfinder: First In, Last Out(A very well written account of Richie Burns’ first tour in RVN, duringwhich he provided support to a Mike Force mission, and which describesother activities very similar to SF missions during the war.)Peoples’ War, Peoples’ArmyPerilous Options: <strong>Special</strong> <strong>Operations</strong> as an Instrument ofU.S. Foreign PolicyPhantom Warriors, Book IIPhantom Warriors: LRRPs, LRPs, and Rangers in Vietnam, Book IPresidents’ Secret Wars: CIA and Pentagon Covert <strong>Operations</strong>from World War II Through the Persian GulfRangers at War: Combat Recon in VietnamRescue Of River CityReturn of The Enola GayReturn With HonorSetting the East Ablaze(Part of a series of books on the area from Turkey to Tibet.Well researched and an excellent view of the region, its history, andvarious societies that live within the region.)Seven Pillars of Wisdon(Middle East insight)SF Bibliography: Collection of articles and other readingswith <strong>Special</strong> Forces topicsShadow War: <strong>Special</strong> <strong>Operations</strong> and Low Intensity ConflictSilent Birdmen(281st AHC pilot account; Project Delta Ops in Ashau Valley.)Slow Walk In A Sad RainSOG and SOG Photo BookSOG: Volume I, II, III and IVSPEC OPS: Case Studies in <strong>Special</strong> <strong>Operations</strong> Warfare:Theory and Practice<strong>Special</strong> Forces 1941-1987<strong>Special</strong> Forces, the U.S. Army’s experts in Unconventional Warfare<strong>Special</strong> Men and <strong>Special</strong> Missions: Inside American <strong>Special</strong><strong>Operations</strong> Forces, 1945 to the PresentSpies And <strong>Command</strong>osStolen ValorStrategy and Policy Background Umbrella Concept forLow Intensity ConflictStreet Without Joy(French in Indochina; Good groundwork for SF in Vietnam)Taking The High Ground: Military Moments With GODTalking with Victor Charlie: An Interrogator’s StoryTam PhuThe Barking Deer(Fiction)The Blood Road: The Ho Chi Minh Trail and the Vietnam WarThe Chindit WarHiroo OnodaDavid DonovanRobin Moore; J.C. LambJohn PradosAaron Bank (COL Ret)Loyd LittleRichard C. BurnsVo Nguyen GiapLucien S. VandenbrouckeGary A. LindererGary A. LindererJohn PradosShelby L. StantonDrew DixPaul W TibbetsScott O’Grady (Capt); Jeff CoplonPeter HopkirkT.E. LawrenceRadix Press/Dan GodbeeH.T. HaydenA.L. RamponeJohn P. McAfeeJohn PlasterHarve SaalWilliam H. McRavenLeRoy ThompsonCaroll B. ColbyJoel Nadel; J.R. WrightKenneth ConboyB.G. Burkett; Glenna WhitleyAlex and Hamilton BoozBernard B. FallJeff O’Leary (Col)Sedgwick D. Tourison JrLeigh WadeJonathan RubinJohn PradosShelford Bidwell118Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
TITLE(Good section on Merrill’s Marauders)The Devil’s Guard(A non-SF book; a good read and supposedly historically accurate.Covers the war from the viewpoint of the ex-Nazi’s who were in theFrench Foreign Legion fighting the Viet Minh.)The Dying Place(Fiction)The Great Game(Part of a series of books on the area from Turkey to Tibet.Well researched and an excellent view of the region, its history,and various societies that live within the region.)The Green Berets in Vietnam, 1961-71The Hidden History of the Vietnam WarThe Last ConfucianThe Making of a QuagmireThe Montagnards of South VietnamThe New LegionsThe Politics of Heroin in SE Asia(Essential reference for understanding the Golden Triangle.)The Price of Exit(Helicopter pilot, Lam Son 719 and CCN)The RaidThe Ravens(The classic about our Bird Dog brothers)The Rescue of Bat-21The Road to Arnhem: A Screaming Eagle in HollandThe Secret Wars: A Guide to Sources in English, Volume II, Intelligence,Propaganda and Psychological Warfare, Covert <strong>Operations</strong>, 1945-1980The Sorrow of War: A Novel of North Vietnam(This is a work of fiction with many facts written by a NVA Officer.)Tiger the Lurp Dog(Fiction)Tragedy in Paradise: A Country Doctor at War in LaosTrespassers on the Roof of the World(Part of a series of books on the area from Turkey to Tibet.Well researched and an excellent view of the region, its history,and various societies that live within the region.)Umbrella Concept for Low Intensity ConflictUnconventional <strong>Operations</strong> Forces of <strong>Special</strong> <strong>Operations</strong>Uneasy WarriorU.S. Army <strong>Special</strong> Forces 1952-84U.S. Army Handbook for North Vietnam Dept. of Army: 550-57U.S. Army Handbook for Cambodia Dept. of Army: DA Pam: 550-50U.S. Army Handbook for Laos Dept. of Army: DA Pam: 550-58U.S. Army Handbook for South Vietnam Dept. of Army: DA Pam: 550-55U.S. Army Handbook: Minority Groups in the Republic of Vietnam:Ethnographic Series Dept. of Army:DA Pam: 550-105U.S. Army <strong>Special</strong> <strong>Operations</strong> in World War IIU.S. <strong>Special</strong> ForcesUrgent Fury: The Battle for GrenadaValley of Decision: The Siege of Khe SanhVietnam Above The Tree Tops: A Forward Air Controller ReportsVietnam in American LiteratureVietnam Military Lore: Legends, Shadow and HeroesVietnam Order of Battle: A Complete, Illustrated Reference to the U.S.Army and Allied Ground Forces in Vietnam, 1961 - 1973Vietnam Studies: <strong>Command</strong> and Control 1950-1969Vietnam: A HistoryAUTHORGeorge R. ElfordDavid A. MaurerPeter HopkirkFrancis J. KellyJohn PradosDenis WarnerDavid HalberstamRobert L. MoleDonald DuncanAlfred McCoyTom MarshallBenjamin F. SchemmerChristopher RobbinsDarrel D. WhitcombDonald R. BurgettMyron J. SmithBao NinhKenneth MillerCharles Weldon, MDPeter HopkirkAlex and Hamilton BoozMark D. BoyattVincent CoppolaGordon L. RottmanDavid W. Hogan Jr.Peter McDonaldMark AdkinJohn PradosJohn F. FlanaganPhilip H. MellingRay E. Bows (MSG Ret)Shelby StantonMaj Gen George EckhardtStanley KarnowSOF Reading List 119
TITLEVietnam: The Origins of RevolutionVietnam: The Secret WarWar Stories of the Green Berets: The Vietnam ExperienceWar StoryWarrior HealersWe Were Soldiers Once and YoungAUTHORJohn T. McAlister JrKevin M. GenerousHans HalberstadtJim MorrisLeonard D. Blessing Jr.Harold G. Moore (LTG); Joseph L. Galloway120Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
GENERAL REFERENCESALERTS & THREATSBio-security Center: http://www.upmc-biosecurity.org/Epidemic and Pandemic Alert: http://www.who.int/csr/en/Global Disease Alert Map: http://healthmap.org/enMedical Threats Briefings (by Topic): http://usachppm.apgea.army.mil/hiomtb/Relief Web: http://www.reliefweb.int/rw/dbc.nsf/doc100?OpenFormSecurity News: http://www.planetdata.net/ and http://www.globalsecurity.orgBASIC REFERENCE:Anatomy Atlases Online: http://www.anatomyatlases.org/Health and Medical Sites: http://www.lib.uiowa.edu/hardin/md/idx.htmlHealth Sciences Libraries Online: http://www.lib.uiowa.edu/hardin/hslibs.htmlMartindale’s Medical References: http://www.martindalecenter.com/Medical.htmlMedical Algorithms, Assessments, Scales, Scoring Systems & Tools: http://www.medal.org/visitor/login.aspxMedical Dictionary Online: http://cancerweb.ncl.ac.uk/omd/Merck Health Guides Online: http://www.mercksource.com/Military Medical Resources: http://www.medtrng.com/medicaloperations.htmNational Library of Medicine Gateway: http://gateway.nlm.nih.gov/gw/CmdPractice Guides: http://www.fpnotebook.com/ ; http://www.emedicine.com/ ; http://www.lib.uiowa.edu/hardin/md/ andhttp://www.acep.org/practres.aspx?id=30232USUHS Learning Resource Center: http://www.lrc.usuhs.mil/BOOKS (ONLINE)Books for Doctors: http://www.freebooks4doctors.com/fb/special.htme-Learning Toolkit for Essential Surgical Care: http://www.steinergraphics.com/surgical/index.htmlEnvironmental Medicine Text: http://www.envimed.com/emb.shtmlDermatology: http://telemedicine.org/stamford.htmDSM-IV (Revised): http://psych.org/MainMenu/Research/DSMIV.aspxFirst Aid in Armed Conflicts: http://www.icrc.org/web/eng/siteeng0.nsf/html/p0870Global Health Council Publications: http://www.globalhealth.org/publicationsMedical Bookshelf: http://www.ncbi.nlm.nih.gov/sites/entrez?db=booksMedical Books Online: http://www.flyingpublisher.comMilitary Medicine: http://www.bordeninstitute.army.mil/published.htmlMilitary Bio-defense Manuals: http://usamriid.detrick.army.mil/education/instruct.htmMerck Manuals Online: http://www.merck.comMerck - Medicus Portal: http://www.merckmedicus.com/pp/us/hcp/hcp_home.jspNavy Diving Manual: http://www.supsalv.org/manuals/diveman5/divManual5.htmOperational Medicine: http://www.operationalmedicine.org/Primary Trauma Care Manual: http://www.steinergraphics.com/surgical/manual.htmlCOURSES (ONLINE)Medical Super Courses: http://iier.isciii.es/supercourse/assist/topicsearch.htmVirology Course: http://web.uct.ac.za/depts/mmi/jmoodie/welcome1.htmlJOURNALS (ONLINE)Federal Medicine: http://www.usmedicine.com/index.cfmMedical Journals: http://www.biomedcentral.com/ ; and http://www.plos.org/Educational Resources 121
Medical and Science Journals: http://www.ispub.com/ostia/index.php?xmlFilePath=journals.xmlMedical and Science Journals for the Developing World: http://www.biomedcentral.com/developingcountriesTRAININGAdvanced Burn Life Support: http://www.ameriburn.org/ablscoursedescriptions.phpAdvanced Disaster Life Support: http://www.bdls.com/Advanced Hazmat Life Support: http://www.ahls.org/ahls/ecs/main/ahls_home.htmlAdvanced Medical Life Support: http://www.naemt.org/AMLS/default.htmAdvanced Wilderness Life Support: http://awls.org/index.htmAviation Medicine School: http://usasam.amedd.army.mil/Airway Management: http://www.theairwaysite.com/Bio-defense Education: http://www.biodefenseeducation.org/Biochemical Organic Radiological Disaster Educational Response System: http://www.bordersalertandready.com/Blast Injury Training: http://www.bt.cdc.gov/masscasualties/tiidefacts.aspCenter for Domestic Preparedness: http://cdp.dhs.gov/index.htmlCombat Lifesaver: http://www.combatreform.com/combatlifesaver.htmDiploma in Remote and Offshore Medicine: http://www.diprom.rcsed.ac.uk/Disaster Education Extension Network: http://eden.lsu.eduDisaster Mental Health Institute: http://www.usd.edu/dmhi/Diver Medical Technician Training: http://www.nbdhmt.com/dmt.htmlFamily and Primary Care Medicine Studies: http://www.graham-center.orgFlight Medic Course: http://usasam.amedd.army.mil/_fm_course/index.htmEmergency Management Institute: http://www.training.fema.gov/EMIWEB/Health Care: http://www.medweb.emory.edu/MedWeb/SPT—Home.phpHumanitarian Resource Institute: http://www.humanitarian.net/International Trauma Life Support Course: http://www.itrauma.org/JEMS Training Links: http://www.jems.com/education_and_training/index.htmlNAEMT Training: http://www.naemt.org/educationalPrograms/Medicine for Mariners: http://www.medicineformariners.com/Medicine in Challenging Environments: http://www.trueresearch.org/mice2006/Pathology Training: http://library.med.utah.edu/WebPath/webpath.htmlPre Hospital Trauma Life Support: http://www.naemt.org/PHTLS/Remote Area EMS: http://www.raems.com/index.htmlRemote Medicine Guides: http://www.remotemedicine.org/Guides.htmSurgical Education Online: http://www.vesalius.com/cfoli.aspTCCC Guidelines and References: http://www.usaisr.amedd.army.mil/tccc.htmlTerror Medicine: http://www.terrormedicine.org/Training in Tropical Diseases: http://www.who.int/tdr/index.htmlUSMA Terrorism and Counter terrorism Training: http://www.teachingterror.com/MEDICAL REFERENCESADMINISTRATION AND CONTINGENCY PLANNINGDisrupted Health Services: http://www.who.int/hac/techguidance/tools/disrupted_sectors/en/index.htmlHealth and Disaster Preparedness Tools (USH&HS): http://www.ahrq.gov/prep/Hospitals for War Wounded - A Guide for Set Up: http://www.icrc.org/web/eng/siteeng0.nsf/html/p0714Emergency Preparedness Planning (CDC): http://www.bt.cdc.gov/planning/Public Health Emergency Countermeasures: http://www.hhs.gov/aspr/ophemc/index.htmlPublic Health Emergency Countermeasures: http://www.hhs.gov/aspr/ophemc/index.htmlPublic Health Preparedness Tools: http://www.phpreparedness.info/tools.phpSurge Capacity: http://www.bt.cdc.gov/masscasualties/surgecapacity.asp ; andhttp://www.bt.cdc.gov/masscasualties/capacity.aspPediatric Hospital Surge Capacity: http://www.ahrq.gov/prep/pedhospital/AEROSPACE AND AVIATION MEDICINE AND PATIENT TRANSPORTAerospace Medical Resources: http://aeromedical.org/Links/avmed_links.htmlAviation Medicine (Pt factors): http://emedicine.medscape.com/article/810246-overview122Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
Aviation Medicine Resources: http://www.nh-tems.com/Aviation_medicine.htmlFlight Medic Resources: http://www.flightweb.com/glinks/index.php?category=2ALTERNATIVE MEDICINECenter for Complementary and Alternative Medicine: http://nccam.nih.gov/Center for Traditional Medicine: http://www.who.int/medicines/areas/traditional/collabcentres/en/Traditional Medicine Programs: http://www.arctichealth.org/tm.php ; andhttp://americanindianhealth.nlm.nih.gov/trad-healing.htmlEthno-botanical Resource Directory: http://www.cieer.org/directory.htmlEthno-medicine Links: http://www.ethnomedico.com/english/links.htm ; and http://www.univie.ac.at/ethnomedicine/Ethno-pharmacology Resources: http://medicinus.info/research/areas/ethnopharmacology/Herbals: http://www.botanical.com/botanical/mgmh/comindx.htmlIndigenous and Traditional Medicine Links: http://hsclibrary.uchsc.edu/strauss#s14Natural Medicines Comprehensive Database: http://www.naturaldatabase.com/Psychoactive Substances: http://www.ethnopharmacology.com/; and http://www.erowid.org/psychoactives/psychoactives.shtmlCHEMICAL, BIOLOGICAL, RADIOLOGICAL AND HAZARDOUS MATERIALS (CBNRE)Bioterrorism Emergencies Preparedness and Response: http://www.bt.cdc.gov/bioterrorism/Chemical Emergencies Emergency Preparedness and Response: http://www.bt.cdc.gov/chemical/Radiation Emergencies Emergency Preparedness and Response: http://www.bt.cdc.gov/radiation/CBNRE Information & Analysis Center: http://www.cbiac.apgea.army.mil/Food Safety, Animal and Plant Health Portal: http://www.ipfsaph.org/En/default.jspHazardous Materials Database: http://www.cameochemicals.noaa.gov/Poison Control: http://www.aapcc.org/DNN/Poison Plants Database: http://www.cbif.gc.ca/pls/pp/poison?p_x=pxToxicology Databases: http://www.atsdr.cdc.gov/toxpro2.htmlDENTALDental Emergencies: http://www.webmd.com/oral-health/guide/handling-dental-emergenciesDental Emergencies and Injuries: http://www.ada.org/public/manage/emergencies.aspDental Disease and Trauma Research: https://www.usaccc.org/research/DentalDisease.jspDERMATOLOGYAtlas of Dermatology: http://www.brooksidepress.org/Products/OperationalMedicine/DATA/operationalmed/Manuals/GMOManual/clinical/Dermatology/AtlasofDermatology.htmDermatology Links and Resources: http://www.hsc.stonybrook.edu/som/dermatology/links.cfmGlobal Skin Atlas: http://www.globalskinatlas.com/diagindex.cfmDISASTER MEDICINE AND MANAGEMENTCenters for Disaster Medicine: http://hsc.unm.edu/som/cdm/index.shtml ; http://www.gwemed.edu/1189844732663.html ; andhttp://www.mcg.edu/ems/COM/Disaster/Civil-Military Guidelines for Complex Emergencies:http://ochaonline.un.org/cmcs/guidelinesComplex Emergencies: http://www.certi.org/ ; http://www.cedat.be/ ; andhttp://www.the-ecentre.net/resources/e_library/doc/OECD.pdfDisaster and Pre-Hospital Medicine: http://pdm.medicine.wisc.edu/home.htmlCenters for Disaster and Humanitarian Assistance: http://www.cdham.org/ ; http://www.cdmha.org/Resources.htm ; andhttp://coe-dmha.org/Disaster Medicine Links: http://pdm.medicine.wisc.edu/links.htmlDisaster Management Toolkit: http://www.hsc.usf.edu/nocms/publichealth/cdmha/toolkit_dm/Index_English.pdfDisaster Reduction Resources: http://www.unisdr.org/Non-Traditional Partners in Disaster Response: http://rems.ed.gov/views/documents/TapIn2CmunityPartnrs4ERMgmt.pdfDIVING AND HYPERBARIC MEDICINEDiver’s Alert Network: http://www.diversalertnetwork.org/Diving Medicine Links: http://scuba-doc.com/lnks.htmlDiving Diseases Research Center: http://www.ddrc.org/Diving Medicine Symptoms and Treatment: http://scuba-doc.com/sitemap.htmlHyperbaric Medicine Links: http://www.scuba-doc.com/hbolnks.htm ; andhttp://www.virtual-anaesthesia-textbook.com/vat/hyperbaric.htmlEducational Resources 123
EMERGENCY MEDICINE (INTERNATIONAL)Center for International Emergency Medicine: http://www.iemh.org/Links and Resources: http://www.acep.org/ACEPmembership.aspx?id=25148ENVIRONMENTS, ENVIRONMENTAL HEALTH AND MEDICINEEnvironmental Health Links: http://www.sis.nlm.nih.gov/enviro/envirohealthlinks.htmlEnvironmental Health in Emergencies: http://www.who.int/water_sanitation_health/hygiene/emergencies/en/Environmental Medicine Links: http://www.uib.no/isf/guide/occu.htmInternational Union for Circumpolar Health: http://www.iuch.org/Maritime Medicine Center: http://www.gwemed.edu/maritime.htmMedicine in Challenging Environments: http://www.trueresearch.org/mice2009/index.aspxTravel Medicine Resources: http://gorgas.dom.uab.edu/geomed/links2.htmlNeglected Tropical Diseases: http://gnntdc.sabin.org/Tropical Medicine Library and Resources: http://lib.itg.be/bibhome.htmTropical Medicine Links: http://www.astmh.org/links/index.cfmWilderness Medicine Links: http://wms.org/links/interest.aspGEOSPATIAL HEALTH RESOURCESGeospatial Mapping: http://www.cdc.gov/nchs/gis.ht ; http://datawarehouse.hrsa.gov/ ; andhttp://www.who.int/health_mapping/en/HUMANITARIAN ASSISTANCEEmergency Nutrition Network: http://www.ennonline.net/Global Humanitarian Studies Links: http://www.sipa.columbia.edu/academics/concentrations/ha/ghsi/introduction.htmlGlobal Health Cluster Response Toolkit: http://www.humanitarianreform.org/humanitarianreform/Default.aspx?tabid=75Interagency Standing Committee for Humanitarian Aid Response: http://www.humanitarianinfo.org/iasc/pageloader.aspxRelief Web Library: http://www.reliefweb.int/rw/lib.nsf/doc205?OpenFormUN Humanitarian Information Management Toolbox: http://www.humanitarianinfo.org/IMToolbox/IMPROVISED MEDICINEImprovised Medicine: http://www.paladin-press.com/category/sMidwives Handbook: http://www.hesperian.org/Publications_and_Resources.phpWhere There is No Doctor: http://www.healthwrights.org/books/WTINDonline.htmWhere There is No Dentist: http://www.healthwrights.org/books/WTINDentistonline.htmWhere Women Have No Doctor: http://www.hesperian.org/Publications_and_Resources.phpWhere There Is No Psychiatrist: http://www.asksource.info/pdf/30256_wherethereisnopsych_ch3_2003.pdfINFECTIOUS DISEASESCenter for the Control of Infectious Diseases: http://www.cdc.gov/ncpdcid/Communicable Disease Control in Emergencies: http://whqlibdoc.who.int/publications/2005/9241546166_eng.pdfDisease Control Priorities Project: http://www.dcp2.org/main/Home.htmlGlobal Viral Forecasting Initiative: http://gvfi.org/index.htmlOutbreaks and Surveillance: http://www.who.int/csr/don/enWildlife Disease Information Node: http://wildlifedisease.nbii.gov/Zoonotic, Vector Borne & Enteric Disease Center: http://www.cdc.gov/nczved/INTERNATIONAL, CROSS-CULTURAL AND PUBLIC HEALTHCross Cultural Healthcare Program http://www.xculture.org/Cross Cultural Medicine Resources: http://www.ethnomed.org ; andhttp://medicine.ucsf.edu/resources/guidelines/culture.htmlGlobal Health Office (CDC): http://www.cdc.gov/cogh/index.htm/Global Health Office (Issues & Resources): http://www.globalhealth.govGlobal Public Health References: http://www.pbs.org/wgbh/rxforsurvival/resources.htmlInternational Medicine Programs: http://www.gwemed.edu/1189932253869.htmlPublic Health Association Resources: http://www.apha.org/programs/resources/Public Health Preparedness Centers: http://www.asph.org/cphp/cphp_home.cfmPublic Health Links: http://www.sph.emory.edu/PHIL.php124Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
LABORATORYClinical Lab Science Resources: http://members.tripod.com/~LouCaru/index-5.htmlLaboratory Links: http://wwwn.cdc.gov/nltn/mltl.aspxMASS CAUSALITIESCommunity Based Mass Prophylaxis: http://www.ahrq.gov/research/cbmprophyl/cbmpro.htmMass Care and Shelters Guide: http://www.cdsscounties.ca.gov/coplanners/Mass Causality & Refugee Evacuation: http://www.ahrq.gov/prep/natlsystem/Mass Causality Resources: http://www.bt.cdc.gov/masscasualties/National Mass Fatalities Institute: http://www.nmfi.org/MATERNAL-CHILD HEALTHAntenatal Guidelines for Crisis Conditions: http://www.icrc.org/web/eng/siteeng0.nsf/html/p0875Maternal/Child Health Resources: http://www.who.int/making_pregnancy_safer/publications/en/MENTAL HEALTHMental Health Resources: http://www.bt.cdc.gov/mentalhealth/Disaster Mental Health Resources: http://www.trauma-pages.com/disaster.phpInternational Mental Health and Resources: http://www.iop.kcl.ac.uk/international/?project_id=80MORGUE AND REMAINS MANAGEMENTDisaster Victim Identification Guide: http://www.interpol.int/Public/DisasterVictim/guide/default.aspDisaster Morgue <strong>Operations</strong>: http://www.winid.com/dmort7/Final%204-WHITE.docManagement of Human Remains: http://www.icrc.org/web/eng/siteeng0.nsf/html/p0858NEUROLOGYTraumatic Brain Injuries: http://www.neure.com/ ; and http://www.mayoclinic.com/health/traumatic-brain-injury/DS00552OBSTETRICS AND GYNECOLOGYReproductive Health Care in Emergencies: http://www.who.int/reproductivehealth/pages_resources/listing_emergency.en.htmlOPERATIONAL MEDICINE CENTERShttp://www.mcg.edu/ems/COM/ ; http://www.gwemed.edu/1193734316069.html ;https://www.momrp.org/ ; and http://www.med.navy.mil/sites/navmedmpte/nomi/Pages/default.aspxOPHTHALMOLOGYAmerican Academy of Ophthalmology Resources: http://www.aao.org/Eye Disorders Online: http://www.merck.com/mmpe/sec09.html and http://www.ophthalmologyweb.com/default.aspxPATHOLOGYArmed Forces Institute of Pathology: http://www.afip.org/Investigative Pathology: http://www.asip.org/Pathology Links: http://www.asip.org/links/biomedical.htmPEDIATRICSChild Health in Emergencies: http://www.who.int/child-adolescent-health/publications/pubemergencies.htmPediatric Immunization Guide: http://aapredbook.aappublications.org/current.shtmlPediatric Patient Management: http://practice.aap.org/topicBrowse.aspx?nodeID=4000Pediatric Resources: http://pages2.inrete.it/mbiomed/pedi.htm ; and http://www.lib.uiowa.edu/hARDIN/MD/ped.htmlPHARMACOLOGYEssential Medicines: http://www.who.int/medicines/publications/en/Merck’s Clinical Pharmacology: http://www.merck.com/mmpe/sec20.htmlPsychopharmacology Resources: http://www.ascpp.orgRADIOLOGY AND MEDICAL IMAGINGMed Pix Medical Image Database: http://rad.usuhs.edu/medpix/index.htmlRadiology Education Gateway: http://tmcr.usuhs.mil/Radiology Links and Resources: http://www.radiologyeducation.com/Public Health Image Library: http://phil.cdc.gov/Phil/home.aspEducational Resources 125
REFUGEE MANAGEMENTCenter for Refugee and Disaster Medicine: http://www.jhsph.edu/refugee/Refugee Decision Support Resources: http://www.unhcr.org/cgi-bin/texis/vtx/refworld/rwmainHumanitarian Aid Links: http://www.unhcr.org/cgi-bin/texis/vtx/reflink/download.htmRefugee Resources: http://www.unhcr.org/cgi-bin/texis/vtx/reflinkSURGERYIntegrated Management Tools for Essential and Emergency Surgical Care:http://www.who.int/surgery/publications/imeesc/en/index.htmlSurgical Care in Emergencies: http://www.who.int/surgery/en/ESC_in_disasters.pdfSurgical Care at the District Hospital: http://www.who.int/surgery/publications/en/SCDH.pdfSurgery for Victims of War: http://www.icrc.org/web/eng/siteeng0.nsf/html/p0446TACTICAL MEDICINETactical Medicine Centers: http://www.mcg.edu/ems/COM/Tactical/ ; and https://www.usaccc.org/index.jspVETERINARY MEDICINEAnimal Disease Alerts, Information and Resources: http://www.oie.int/eng/en_index.htmAnimal/Plant Health Inspection Service and Resources: http://www.aphis.usda.gov/Bio-security Center for Animal Health Emergencies: http://www.biosecuritycenter.org/Diagnostic Tests and Vaccines for Terrestrial Animals: http://www.oie.int/eng/normes/mmanual/A_summry.htmGlobal Early Warning System for Animal Diseases: http://www.who.int/zoonoses/outbreaks/glews/en/index.htmlVeterinary Resources: http://informatics.vetmed.vt.edu/Projects.htmVeterinary Emergency and Critical Care Links: http://veccs.org/Veterinary Environmental Health Center: http://www.emc.ncsu.edu/Veterinary Public Health and Zoonotic Disease: http://www.who.int/zoonoses/vph/en/Wildlife Disease Information Node: http://wildlifedisease.nbii.gov/World Veterinary Association Links: http://www.worldvet.org/Web_Links.html126Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
A 11 year old boy whose tibia continuedgrowing after a below knee amputation. Heoriginally had his right great toe amputateddue to infection. A year later his right foothad to be amputated due to infection. A fewmonths later he received a BKA. His familychose not to make the three day travel toKabul for any more surgeries so they washedhis bandages for two years while the tibiacontinued growing and punched through hisskin. An 18D whose habit was to inspect andredress any bandages he saw found thisstump. He coordinated to have the boy andhis father flown to Bagram where he was operatedon by American surgeons. Threemonths later the boy was fitted for a prostheticleg. A year later he was seen again,walking fine, no infection and probably thehappiest Afghan in Paktika Province.Photo courtesy of Victor AndersenWhile watching vehicles outside of a Shura meeting in PaktikaProvince, Afghanistan, an 18D treats fresh wounds on a little girl whorefused to identify who had beaten her up.Photo courtesy of Victor AndersenA 5-year-old boyhad been burnedwhile filling hisfamily’s woodstove.He was treated fivedays in a row by an18D doing “TailgateSickcall” inOrgun, Afghanistan.Photo courtesy ofVictor AndersenPhoto Gallery127
An Afghan had been shot in the arm, chest, and head. Hewas treated and saved by an 18D who performed a tubethoracostomy and cricothyroidotomy while awaitingCASEVAC.Photo courtesy of Victor AndersenA child lame since age three is brought to the team medic. Themedic was able to get the boy a wheelchair but no miracle cure.Photo courtesy of Victor AndersenWhile the rest of the team searches a compound, an 18Dconducts sick call on civilians in an effort to maintain rapportand justify the Americans’ presence.Photo courtesy of Victor AndersenAn 18D does a physical exam and deworms one ofhis favorite Afghans.Photo courtesy of Victor AndersenCol (Dr) Gary Geracci-Oral & Maxillofacial Surgeon-USS-COM CEB and MSgt Rodolfo Palacios-Aeromedical Technician99MDG suture a scalp laceration on a young boy during aHumanitarian med mission in Nicaragua.Photo courtesy of Col Gary Geracci128Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
Meet Your JSOM StaffEXECUTIVE EDITORVirgil T. Deal, MD, FACSVirgil.Deal@socom.milPrior to becoming the USSOCOM <strong>Command</strong> Surgeon, COL “Tom” Dealserved in staff positions at USASOC, JSOC, 7th SFG, and XVIII Airborne Corps. Hehas commanded field and stateside hospitals and served as Chief of Surgery in the86th Evac Hospital in ODSS and at Army and civilian community hospitals.COL Deal obtained his medical degree from University of Tennessee Collegeof Medicine, Memphis, Tennessee, 1974. He completeted his general surgery residencyat Brooke Army Medical Center 1977-1981 and is certified by the AmericanBoard of Surgery.COL Deal competed his Flight Surgeon’s Course – 2003, Army War College– 1997, <strong>Command</strong> & General Staff College – 1994, AMEDD Officer AdvancedCourse – 1991, Military Free Fall School – 1977, <strong>Special</strong> Forces Officers Course –1976, and Airborne School – 1975.COL Deal has also completed Combat Casualty Care Leadership Course (C4A) –1991, Pre-<strong>Command</strong>Course, Fort Leavenworth – 1994, Senior Officer’s Legal Orientation, Charlottesville -- 1994, Combatant <strong>Command</strong>er’sSurgeons Course – 1996, AMEDD Pre-<strong>Command</strong> Course, Fort Sam Houston – 1998, Basic Life Support– current, Advanced Cardiac Life Support, Advanced Trauma Life Support, and Pilot, single engine, land,instrument.MANAGING EDITORMichelle DuGuay Landers, RNduguaym@socom.milLt Col Landers joined the Army Reserve in 1987 and served as a nurse in aCombat Support Hospital unit for three years before switching services in 1990 to becomean Air Force C-130 Flight Nurse. She is currently an IMA reservist attached tothe SOCOM/SG office where she has been in charge of management, production, publication,and distribution of the JSOM since its inception in Dec 2000. Lt Col Landershas a Bachelors in Nursing and a Masters in Business Administration/Management.Her 23 year nursing career includes being a flight nurse in both the military and privatesector, 15 years of clinical experience in emergency and critical care nursing aswell as being an EMT and a legal nurse consultant. She also served as the military liaisonto the FL 3 Disaster Medical Assistance Team (DMAT). Prior to the SG office,Lt Col Landers’ experience at USSOCOM includes an assignment in the Center forForce Structure, Resources, Requirements, and Strategic Assessments.Meet the JSOM Staff 129
Submission Criteria1. Use the active voice when possible. This is our most common editorial problem and often requires extensive re-writes.Use the sequence “subject - verb - object.”2. Secure permission before including names of personnel mentioned in your piece. Do not violate copyright laws. If the workhas been published before, include that information with your submission.3. Format articles to be single-spaced, eleven point Times Roman font, aligned on the left, and justified on the right. Double space betweensentences.4. Important: Include an abstract, biography, and headshot photo of yourself as part of the article. Important: Include an abstract, biography,and headshot photo of yourself as part of the article. Include three learning objectives and ten test questions if article issubmitted for continuing education.5. Use a minimum of acronyms; spell out all acronyms when first used. Remember that your audience is inter-service, civilian,and international.6. Put the point of the article in the introductory paragraph and restate it in the closing or summary. Subtlety is not usually a virtuein a medical publication.7. We do not print reviews of particular brands of items or equipment unless that brand offers a distinct advantage not present inother products in the field. The author must specify in the article the unique features and advantages the product offers in orderto justify an exception to this rule. The author must also specify whether the article was purchased by him or his unit, or suppliedfor free by the seller or manufacturer. Finally, the author must disclose any relationship with the manufacturer or seller,whether financial, R&D, or other.8. Cite all references in chronological order. DO NOT insert footnotes or use roman numerals. Give the full name of thejournal, book, or website cited. Use the following style of citation when referencing a Journal article - Vogelsang, R. (2007). Careof the military working dog by medical providers. Journal of <strong>Special</strong> <strong>Operations</strong> Medicine; 7(2)(Spring):33-47.Newspaper article - Di Rado, A. (1995, March 15). Trekking through college: Classes explore modern society using the world ofStar Trek. Los Angeles Times, p. A3. Book article or chapter - Giger, Urs (2000). Blood typing and crossmatching to ensure compatibletransfusions. In John Bonagura Ed. Kirk’s Current Veterinary Therapy XIII Small Animal Practice. Philadelphia, WB SaundersCo. 2000, p. 140-147. Website - Miles, D. (2004, Sep. 3), Military working dogs protect Forces, bases during terror war. ArmedForces Press Service. Retrieved July 1, 2008 from Defense Link website. Website: http://www.defenselink.mil/news/newsarticle.aspx ?id=25393. If unsure, please contact us at jsom@socom.mil.9. Submit high resolution (300dpi) quality photographs with your article. Send photos separately from the document to facilitatehigh resolution conversion into a publishing format. Images imbedded into word documents do not transfer to publishing programsand lose resolution when pulled out of the word document, resulting in a poor quality image. We prefer that images besent electronically in a jpeg format. Please name all images as to what they are (i.e., Figure 1, Figure 2, etc.) and designateplacement in the article using the filename. If you send original pictures, we will make every attempt to return your pictures,but will not account for lost or damaged items.10. Send submissions by email (preferred method) to JSOM@socom.mil, or you may send articles on diskette, or CD, by mail to:USSOCOM Surgeon’s Office ATTN: JSOM Editor, 7701 Tampa Point Blvd. MacDill AFB, FL 33621- 5323. Retain a copy foryourself.11. We reserve the right to edit all material for content and style. We will not change the author’s original point or contention,but may edit clichés, abbreviations, vernacular, etc. Whenever possible, we will give the author a chance to respond to andapprove such changes. We may add editorial comments, particularly where controversy exists, or when a statement is contraryto established doctrine. However, the author must assume responsibility for his own statements, whether in accordance withdoctrine or not. Both medical practice and the military doctrine are living bodies of knowledge, and JSOM’s intent is not to stifleresponsible debate.12. <strong>Special</strong> <strong>Operations</strong> require sensitivity to natives of host countries, occupied regions, and so on. We feel that patronizing termsgenerally are inappropriate for our pages. Realistic language of operators (including some “four-letter” words) may be toleratedin anecdotal and historical articles, especially when used as direct quotes or when such use is traditional among operators.We will delete or change blatantly offensive use.13. All articles written by USSOCOM members must be reviewed and pre-approved by your commander, component surgeon,and PAO prior to submission to the JSOM. Authors must adhere to standard OPSEC practices and refrain frommentioning specific units, specific locations, troop strengths, names of actively serving SOCOM personnel, TTPs, vulnerabilities,and any other information that could be of use to an adversary.14. Authors must adhere to standard OPSEC practices and refrain from mentioning specific units, specific locations, troop strengths,names of actively serving SOCOM personnel, TTPs, vulnerabilities, and any other information that could be of use to an adversary.15. The JSOM is your journal and serves as a unique opportunity for you to pass your legacy to the SOF medical community!130Journal of <strong>Special</strong> <strong>Operations</strong> Medicine Volume 9, Edition 3 / <strong>Summer</strong> 09
<strong>Special</strong> Forces Aidman's PledgeAs a <strong>Special</strong> Forces Aidman of the <strong>United</strong> <strong>States</strong> Army, I pledge my honor and my conscience to theservice of my country and the art of med-icine. I recognize the responsibility whichmay be placed upon me for the health,and even lives, of others. I confess thelimitation of my skill and knowl-edge in the caring for the sick and injured.I promise to follow the maxim "Primum non- nocere" ("First,thou shalt do no harm"), and toseek the assistance of more competentmedical authority whenever it is available. These confidences whichcome to me in my attendance onthe sick, I will treat as secret. I recognizemy responsibility to impart toothers who seek the service of medicinesuch knowledge of its art and practiceas I possess, and I resolve to continue toimprove my capability to this purpose. Asan American Soldier, I have determined ultimatelyto place above all considerations of self the mission of my team and the cause of my nation.Pararescue CreedI was that which others did not want tobe. I went where others feared to go, anddid what others failed to do. I askednothing from those who gave nothing,And reluctantly accepted the thought of eternal lonliess ... shouldI fail. I have seen the face of terror;felt the stinging cold of fear, and enjoyedthe sweet taste of a moment's love. I have cried, pained andhoped...but most of all, I have livedtimes others would say best forgotten.Always I will be able to say, thatI was proud of what I was: a PJ It ismy duty as a Pararescueman to save alife and to aid the injured. I will performmy assigned duties quickly and efficiently, placing these duties before personal desires and comforts.These things I do,"That Others May Live."A Navy PoemI'm the one called “Doc"...I shall not walk in your footsteps, but I will walk by your side.I shallnot walk in your image, I've earnedmy own title of pride. We've answeredthe call together, on seaand foreign land. When the cryfor help was given, I've beenthere right at hand. Whether I amon the ocean or in the jungle wear-ing greens, Giving aid to my fellowman, be it Sailors or Marines.So the next time you see a Corpsmanand you think of calling him "squid,”think of the job he's doing as those beforehim did. And if you ever have to go out there and your life is on the block, Look at the one rightnext to you...I'm the one called "Doc".~ Harry D. Penny, Jr. USN Copyright 1975
UNITED STATES SPECIAL OPERATIONS COMMANDATTN: SOCS-SG7701 Tampa Point Blvd.MacDill AFB, FL 33621-5323OFFICIAL BUSINESSMEDIA MAIL