Abstract
Monoclonal gammopathy of undetermined significance (MGUS) is the earliest discernible stage of multiple myeloma (MM) and Waldenström’s macroglobulinemia (WM). Early diagnosis of MG may be compromised by the low-level infiltration, undetectable to low-sensitive methodologies. Here, we investigated the prevalence and immunophenotypic profile of clonal (c) plasma cells (PC) and/or cB-lymphocytes in bone marrow (BM) and blood of subjects with a serum M-component from the iSTOPMM program, using high-sensitive next-generation flow cytometry (NGF), and its utility in the diagnostic classification of early-stage MG. We studied 164 paired BM and blood samples from 82 subjects, focusing the analysis on: 55 MGUS, 12 smoldering MM (SMM) and 8 smoldering WM (SWM). cPC were detected in 84% of the BM samples and cB-lymphocytes in 45%, coexisting in 39% of cases. In 29% of patients, the phenotypic features of cPC and/or cB-lymphocytes allowed a more accurate disease classification, including: 19/55 (35%) MGUS, 1/12 (8%) SMM and 2/8 (25%) SWM. Blood samples were informative in 49% of the BM-positive cases. We demonstrated the utility of NGF for a more accurate diagnostic classification of early-stage MG.
Similar content being viewed by others
Introduction
Plasma cell (PC) neoplasms comprise a heterogeneous group of neoplastic diseases of long-lived clonal (c) PC that accumulate in bone marrow (BM), and to a lesser extent, also in other tissues [1, 2]. Expanded cPC might also circulate in blood and they usually secrete a monoclonal (M) immunoglobulin (Ig) (i.e., the M-component) of the IgM, IgG, or IgA isotype, and, less frequently, an Ig light chain (Ig-LC), that is detectable in serum and/or urine [1,2,3].
Among all PC neoplasms, monoclonal gammopathy of undetermined significance (MGUS) is by far the most prevalent (3–5% of adults >50 years) [3, 4]. It is defined by the presence of a smaller (<30 g/l) serum M-component and <10% BM infiltration by PC, with no signs of myeloma-related end-organ damage [3,4,5,6,7]. At present, it is well-established that IgA, IgG and Ig-LC MGUS may progress to smoldering multiple myeloma (SMM), which has a prevalence of 0.53% of adults >40 years [8], and (clinical/symptomatic) multiple myeloma (MM) at a rate of ≈1%/year, while SMM cases progress to MM at a higher rate of ≈10%/year [3, 9,10,11]. Progression to MM is characterized by an increase in the percentage of BM PC (i.e., >10%) and the serum M-component (≥30 g/l), together with the emergence of end-organ damage (e.g., CRAB for hypercalcemia, renal insufficiency, anemia and/or bone lesions) or occurrence of other myeloma defining events [3, 5,6,7, 12]. In contrast, IgM-MGUS rarely evolves to an IgM-MM, and more frequently progresses to a subclinical/smoldering Waldenström’s macroglobulinemia (SWM), and WM with a progressive increase in serum IgM M-protein (≥30 g/l) in association with ≥10% infiltration of BM by (clonal) lymphoplasmacytic cells and, in case of WM, also organomegalies [1, 2, 6, 9, 12,13,14,15,16]. Thus, in both instances, intermediate/smoldering forms of the disease (SMM or SWM) have been defined based on a yet subclinical disease, but higher levels of serum M-component (≥30 g/l), and/or ≥10% infiltration either by cPC (in the absence of myeloma defining events) or by lymphoplasmacytic cells (in the absence of organomegalies), respectively [3, 10, 11, 13, 15, 16]. Of note, it has been recently proposed that SMM patients with an 80% risk of progression at two years should also be considered as MM and offered treatment [10, 17].
In addition to typical MGUS cases, a serum M-component associated with the involvement of extramedullary tissues (e.g., bone, skin and/or lymph nodes) by cPC without or with lymphoplasmacytic cells, might also be found (with no or minimal BM involvement) in case of solitary (and multifocal) plasmacytomas and lymphoplasmacytic lymphomas, respectively [1, 2, 6, 18, 19], with variable rates of disease progression and need for systemic therapy. Because of all the above, a national screening program for MG -the Iceland Screens, Treats, or Prevents Multiple Myeloma (iSTOPMM) project- [20] has recently started in Iceland aimed at defining the potential utility of early diagnosis and therapeutic interventions in subjects from the general population who present with an MG in the absence of other signs of disease.
Independently of the specific disease subtype, the diagnosis and classification of PC neoplasms currently require a BM study. However, due to the low levels of infiltration in BM, particularly at the early phases of the disease, and the limited sensitivity and specificity of cytomorphology for the discrimination between normal/reactive and neoplastic PC and B-cells, these might go undetected in current routine diagnostic practice, at the same time coexistence of distinct unrelated populations of clonal B-cells and/or PC might lead to misdiagnosis [21].
In recent years, next-generation flow cytometry (NGF) has proven to be a high-sensitive technique for the detection of low cPC and clonal B-lymphocyte levels in BM and blood based on their uniquely distinct aberrant immunophenotype, even at the very early stages of disease, when they are present at very low frequencies of e.g. 10−5– 10−6 [22,23,24,25,26,27,28]. In addition, cPC from SMM/MM and SWM/WM has long been shown to display clearly different immunophenotypic features, which mimic those of normal/reactive BM PC and blood circulating plasmablasts and/or related lymphoplasmacytic lymphoma-like B-cells, respectively [29,30,31].
Here, we investigated the presence and immunophenotypic characteristics of cPC and cB-lymphocytes in paired BM and blood samples from a series of (otherwise) healthy adults from Iceland who had been screened for the presence of a serum M-component and an underlying monoclonal gammopathy (MG) within the iSTOPMM program [20]. Our main goal was to gain insight into the potential utility of high-sensitive NGF for the identification and characterization of cPC and cB-lymphocytes in BM and blood of these individuals, for more accurate diagnosis and classification of patients presenting with MG, particularly at the (very) early stages of disease.
Materials and methods
Patients and samples
A total of 82 (otherwise) healthy adults aged ≥40 years (44 men and 38 women; median age of 67 years, ranging from 45 to 86 years) with a positive screening for a serum M-component by high-sensitive capillary zone electrophoresis and/or an altered free-Ig light chain (FLC)-ratio (The Binding Site Group Ltd, Birmingham, UK) [20] from the iSTOPMM project who were referred for a confirmatory serum M-component and underwent a BM aspiration procedure in a follow-up visit, fulfilling the diagnostic criteria for SWM/lymphoplasmacytic lymphoma, MGUS or SMM according to the International Myeloma Working Group (IMWG) [3, 5, 6], were selected to be further enrolled in this study. Subjects with prior diagnosis of lymphoproliferative disorders or with mature B cell/plasma cell neoplasms other than SWM, MGUS, and SMM, were excluded from this study. Following the IMWG diagnostic criteria [3, 5, 6], 82 subjects were initially enrolled in the study and subsequently classified into the following disease categories: i) MGUS, 55 subjects; ii) SMM, 12 patients; iii) MM, one case; iv) SWM, 8 donors; v) plasmacytoma, one case; and vi) one chronic lymphocytic leukemia (CLL) subject. In the remaining 4 individuals, the presence of a serum M-component was not confirmed in subsequent evaluations performed after the initial screening and were therefore classified as transient M-component cases [32]. Sample analysis was performed blindly from the distribution of subjects by disease category groups. Based on the predefined exclusion criteria, 7/82 cases (one diagnosed with symptomatic MM, one with plasmacytoma, one with CLL and 4 with a transient M-component) were further excluded from subsequent analyses. The remaining 75/82 subjects (MGUS, SMM, and SWM), represented the core series included in the analyses performed in this study.
A total of 150 EDTA-anticoagulated (paired) BM aspirated samples (2 ml/sample; n = 75) and blood samples (10 ml/sample; n = 75) were collected in Iceland from the 75 individuals enrolled in this study and sent by overnight express courier to the University of Salamanca (Salamanca, Spain) for processing within 36 h after collection.
All subjects enrolled in this study provided their informed consent to participate according to the Declaration of Helsinki. The study met the ethics criteria of Iceland and Spain and was approved by the Icelandic National Bioethics Committee (NCT03327597) as well as by the Icelandic Data Protection Agency, permission being granted from the Spanish Ministry of Health for the transfer of all biological samples for this study (Registration number: 2020/252).
Immunophenotypic studies
Paired BM (1 ml) and blood (4 ml) samples from each subject were stained in parallel with the EuroFlow NGF-MM minimal residual disease (MRD) (2-tube, 8-color) antibody (Ab) panel [26] (Supplementary Table 1, Panel A) and the Lymphoid Screening Tube [28] (Supplementary Table 1, Panel B), using the BD OneFlow (BD, Becton/Dickinson Bioscience, San Jose, CA, USA) dried tubes [33] as per the EuroFlow standard operating procedures (SOPs) for sample preparation and staining available at www.euroflow.org [26, 34]. Stained samples were acquired in FACSCantoTM II (BD) or FACSLyricTM (BD) flow cytometers for a median number of 107 (2–15 × 106) and 1.3 × 106 (0.2–5 × 106) cells, respectively. For (automated) flow cytometry data analysis, the InfinicytTM software (version 2.0.5.d; Cytognos SL., Salamanca, Spain) was used. Following previous criteria [26], the limit of detection for each cell population was set at ≥20 cells.
Clonal PC and cB-lymphocytes were identified based on their unique aberrant phenotypes and/or Ig-LC restriction [26, 27]. Flow cytometry-based immunophenotypic criteria were subsequently applied for further phenotypic classification of the clonal/aberrant PC and B-lymphocytes [13, 35, 36], which included: i) the presence of cPC and/or cB-cells in BM and; ii) the specific immunophenotypic characteristics of such cPC and cB-lymphocytes, respectively [13, 35, 36].
Statistical methods
The Spearman’s correlation coefficient (Spearman’s Rho) was used to calculate the degree of correlation between two (quantitative) variables. The Fisher’s exact test and, either the Mann-Whitney U or the Kruskal-Wallis tests, were used to assess the statistical significance of differences observed between groups of individuals for categorical and continuous variables, respectively. In turn, the MacNemar test was employed for the comparison of paired BM vs blood data. Bilateral significance was determined in these tests. Receiver operating characteristic (ROC) curve analysis was used to calculate the area under the curve defined by the percentage of cPC with respect to total BM PC that best distinguished between different disease groups. For all statistical analysis, the SPSS IBM-Statistical software Package for Social Sciences (SPSS v25.0; IBM Corp, Armonk, NY, USA) was used. Statistical significance was set at p values < 0.05.
Results
Serum M-component isotype and concentration
A persistent serum M-component and/or Ig-LC was detected in all (75/75, 100%) of the subjects investigated. IgG was the most frequently detected M-component (31/75, 41%), followed by IgM (26/75, 35%), IgA (14/75, 19%) and Ig-LC (3/75, 4%). One (1/75, 1%) case showed two different (IgG/κ and IgM/κ) M-peaks. The distribution of the different serum M-components per diagnostic category was as follows: MGUS, 24/55 subjects (43%) had an IgG M-component, 18/55 (33%) were IgM, 11/55 (20%) IgA and 2/55 (4%) LC cases; SMM, 7/12 (58%) IgG, 3/12 (25%) IgA, 1/12 (8%) LC and 1/12 (8%) IgG plus IgM subjects; and, SWM, 8/8 (100%) IgM cases per definition (Supplementary Table 2). Median (range) concentration of the M-component in serum increased from 0.8 g/l (<0.1–8.8 g/l) in MGUS to 2.5 g/l (0.4–17.2 g/l) in SWM and 7.1 g/l (<0.1–15.8 g/l) in SMM.
Prevalence of clonal PC and/or clonal B-lymphocytes in healthy adults presenting with a serum M-component
Overall, cPC and/or cB-lymphocytes were detected in BM and/or blood of 68/75 (91%) individuals investigated. These included 49/55 MGUS (89%) subjects, 12/12 SMM patients (100%) and 7/8 SWM subjects (88%) (Table 1). As detailed in Table 1, cPC were found in the great majority (63/75, 84%) of MG cases, while cB-lymphocytes were detected in less than half of the same individuals (34/75, 45%). In 34/75 (45%) subjects only cPC in the absence of cB-lymphocytes were found, while 5/75 (7%) cases displayed cB-lymphocytes without cPC, both populations of cPC and cB-lymphocytes coexisting in the remaining 29/75 (39%) subjects. For a detailed description of the frequency and type of Ig on each diagnostic category and their distribution according to the clonal cell type detected, see Supplementary Table 2. Among MGUS cases, cPC were detected in most (44/55, 80%) patients, either alone (27/55, 49%) or together with cB-lymphocytes (17/55, 31%). From the remaining MGUS subjects, 5/55 (9%) showed only cB-lymphocytes, while no clonal PC nor cB-lymphocytes were found in the other 6/55 (11%). In turn, 12/12 SMM patients showed cPC either in the absence (7/12, 58%) or the presence (5/12, 42%) of coexisting cB-lymphocytes. Finally, the coexistence of cPC and cB-lymphocytes was confirmed in all but one SWM patients (7/8, 88%), in whom no cPC or cB-lymphocytes were detected.
Interestingly, in half of those individuals harboring both cPC and cB-lymphocytes (15/29, 52%), both (clonal) cell populations displayed closely related phenotypic features, including the same Ig light chain. These mostly consisted of SWM (6/7, 86%) and MGUS cases (8/17, 47%), in addition to 1/5 (20%) SMM patients (Table 2). Among those 14/29 (48%) cases with coexisting but phenotypically unrelated cPC and cB-lymphocytes, the later cells showed immunophenotypic features of CLL-like MBL in 4/4 (100%) SMM patients and in 7/10 (70%) MGUS cases, non-CLL-like MBL clones being found in the other 3/10 (30%) MGUS individuals.
Utility of immunophenotyping for the diagnostic classification of patients with a serum M-component
Detailed analysis of the phenotypic features of cPC and cB-lymphocytes found in patients classified into the different diagnostic subtypes of PC neoplasms by the IMWG criteria [6] showed discrepancies in 22/75 (29%) cases. These included a significant fraction of MGUS (19/55, 35%), together with fewer -2/8 (25%)- SWM cases, and one SMM -1/12 (8%)- patient (Table 3).
Among the 19 discrepant MGUS cases, most corresponded to IgM-MGUS (16/19, 84%), another 2/19 (11%) were IgG-MGUS and the remaining patient had been classified as LC-MGUS (1/19, 5%) (Table 3, Supplementary Table 3). Interestingly, in half of the discrepant IgM-MGUS cases, cPC coexisted with cB-lymphocytes with a WM-like immunophenotype (8/16, 50%), while the other discrepant MGUS cases (11/19, 58%) included 8/16 IgM-MGUS in whom cPC could not be detected in BM nor in blood, either in the absence of other cB-cells (4/8, 50%) or in the presence of CLL-like or non CLL-like MBL cB-lymphocytes (4/8, 50%). The remaining 3 discrepant MGUS cases corresponded to 2 subjects (one IgG and one Ig-LC) without evidence of clonal cells, and one IgG showing only cB-cells. Among SWM patients, the 2/8 discrepant cases were due to the lack of cPC and cB-lymphocytes as detected by NGF in one case, and the coexistence of IgM cPC with a typical MM-like phenotype and an unrelated CLL-like MBL cB-cell population suggesting independent disorders. Finally, the (single) SMM discrepant case showed co-existence in serum of two IgG/κ and IgM/κ M-components, associated with phenotypically related cPC and cB-lymphocytes, both expressing Igκ, with an WM-like phenotype.
Presence of clonal PC and/or B-lymphocytes in BM vs blood
Overall, circulating cPC and/or cB-lymphocytes were found in 33/75 (44%) cases investigated, including half (33/68, 49%) of those cases who carried cPC and/or cB-lymphocytes in BM (Fig. 1A, Supplementary Table 4). These consisted of 22/55 (40%) MGUS -22/49 (45%) MGUS positive cases in BM-, 8/12 (67%) SMM, and 3/8 (38%) SWM -3/7 (43%) SWM positive subjects in BM- (Fig. 1A, Supplementary Table 4). Briefly, circulating cPC were detected in blood of 12/34 (35%) cases showing cPC (only) in BM -5/12 (42%) SMM and 7/55 (13%) MGUS cases- (Fig. 1A, Supplementary Table 4). Among those individuals who showed both cPC and cB-lymphocytes in BM (29/75, 39%), both populations were also detected in blood in 8/29 (28%) cases -2/8 (25%) SWM, 2/12 (17%) SMM and 4/55 (7%) MGUS cases- (Fig. 1A, Supplementary Table 4). In the remaining cases with coexisting cPC and cB-lymphocytes in BM (21/29, 72%) no circulating cPC populations were found. However, in 8/21 (38%) of these later subjects, including 6/8 (75%) MGUS, 1/8 (12%) SWM and 1/8 (12%) SMM cases, clonal (CLL-like or non-CLL-like) MBL populations were identified; the other 13/21 (62%) cases showed neither cPC nor cB-lymphocytes circulating in blood and they included 7/13 (54%) MGUS, 4/13 (31%) SWM and 2/13 (15%) SMM (Fig. 1A, Supplementary Table 4). Finally, in all cases in which a cB-lymphocyte population had been detected in BM in the absence of cPC (5/75, 7%), these were also present in blood (5/5, 100%) in the MGUS patients (Fig. 1A, Supplementary Table 4). Interestingly, in one SMM case with an IgG serum M-component, two different cPC (Igκ and Igλ, with otherwise overlapping phenotypic characteristics) together with a CLL-like MBL clone were detected in blood, while a single cPC population (Igλ) together with a CLL-like MBL was found in BM (Fig. 1A).
In (A), the correlation between the number of clonal plasma cells and clonal B-lymphocytes in BM (percentage values) and blood (number of cells/µl and percentage values) observed for each color-coded individual according to diagnosis is shown. B and C show the correlation between the concentration of serum M-component and the number of clonal plasma cells in bone marrow and in blood of the same individuals, respectively. In all plots, MGUS patients are depicted in green, SMM cases are colored in orange and SWM in blue. In (A), the type of clonal cell detected is distinguished by shapes: circles, cPC only; squares, coexisting cPC and cB-lymphocytes; triangles, cB-lymphocytes only; and empty rhombs, no clonal cells. In turn, in (B and C) (left plots) distinct shapes denote the type of serum M-component: circles, IgM+; squares, IgG+; triangles, IgA+; rhombs, light chain; and empty rhombs, no paraprotein. Box plots in (B, C) (right plots) show median values (middle line), the 25th and 75th percentile values (boxes), minimum and maximum values (whiskers) and the percentages of cPC in BM for each individual case (inner circles). BM bone marrow, cB-cells clonal B-lymphocytes, cPC clonal plasma cells, MGUS monoclonal gammopathy of undetermined significance, PNQ positive not quantifiable, SMM smoldering multiple myeloma, SWM smoldering Waldenström’s macroglobulinemia. !Detection of two cPC and one cB-cell populations in blood and one cPC and the cB-cell populations in BM; *Two M-peaks detected by immunofixation, IgG and IgM; ^Two M-peaks detected by immunofixation, IgM and IgM; #Two M-peaks detected by immunofixation, IgG and IgG.
Overall, the number of circulating cPC and/or cB-lymphocytes in blood significantly correlated (rho = 0.51; p < 0.001) with the percentage of clonal cells (cPC plus cB-lymphocytes) in BM (Fig. 1A), particularly among cases who had only cB-lymphocytes in the absence of cPC (rho = 1; p < 0.001). Of note, progressively higher (median; range) percentages of BM clonal cells were found in MGUS (0.34%; <0.0002–22.2%), SWM (1.2%; <0.0002–61%) (p = 0.08 vs MGUS) and SMM (2.3%; 0.6–17.8%) patients (p = 0.003 vs MGUS), while no significant differences were found in the median (range) distribution of clonal cells (cPC or cB-lymphocytes) in blood between MGUS (<0.01 cells/µl; <0.01–1 053 cells/µl), SWM (<0.01 cells/µl; <0.01–32.2 cells/µl) and SMM (0.04 cells/µl; <0.01–4.8 cells/µl) (p = 0.57).
Furthermore, in 13 (17%) cases with cPC, and in 12 (16%) cases with cB-cells, BM analysis revealed the presence of ≥2 unrelated PC and/or B-cells clones, while this was also found in blood in a minority -1/13 (8%) and 4/12 (33%), respectively- of those same cases.
Correlation between the serum M-component and the number of clonal PC in blood and BM
The number of cPC in blood (rho = 0.24; p = 0.04) and, particularly in BM (rho = 0.48; p < 0.001) (MGUS, rho = 0.37, p = 0.005; SMM, rho = 0.47, p = 0.12; and SWM, rho = 0.78, p = 0.02), significantly correlated with the concentration of the serum M-component. In line with these findings, significantly higher numbers of cPC in BM (p < 0.001) and in blood (p = 0.007) were found in cases presenting with <1 g/l vs ≥1 g/l of M-component in serum (Fig. 1B, C).
Association between the percentage of cPC/total PC in BM and B-cell counts in blood in the distinct diagnostic subtypes of MG
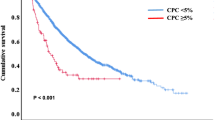
Overall, a significantly higher (median; range) percentage of cPC/total PC in BM was observed in SMM (89.6%; 51.2–99.5%) compared to MGUS (27.6%; 0–98.2%) (p < 0.001) and to a lesser extent also, SWM cases (42.4%; 0–93.2%) (p = 0.03). ROC curve analysis showed that the presence of >60% cPC from all BM PC, was the most accurate cut-off value to discriminate between MGUS and SMM -area under the curve (AUC) of 0.873; p < 0.001- with a sensitivity of 91.7% and a specificity of 70.9% (Fig. 2A). Similarly, the presence of 57.4% cPC/total BM PC also allowed discrimination between SMM and SWM (AUC of 0.823; p = 0.02) with a similar sensitivity (91.7%) and specificity (62.5%) (Fig. 2B). In contrast, the percentage of cPC/total BM PC was similar in MGUS and SWM and did not allow clearcut distinction between both diagnostic entities (p = 0.39) (Fig. 2C).
In (A–C) receiver operating characteristic (ROC) curve plots showing the power of percentage values of cPC/from all BM PC to discriminate between MGUS and SMM (A; 61%), SMM and SWM (B; 57.4%) and between MGUS and SWM (C; no discrimination power), are shown. In (D–F) the correlation between the percentage of B-cell precursors in BM vs the percentage of cPC from all BM nucleated cells (D) and BM PC (B) are shown, while in (F) the correlation between number of normal circulating B-lymphocytes in blood and the percentage of cPC from all BM nucleated cells is displayed. In Panels D-F, MGUS patients are depicted in green, SMM cases in orange and SWM in blue. AUC area under the curve, BM bone marrow, cPC clonal plasma cell, MGUS monoclonal gammopathy of undetermined significance, PC plasma cell, SMM smoldering multiple myeloma, SWM smoldering Waldenström’s macroglobulinemia.
Importantly, at the early stages of MG (MGUS and SMM) a tendency towards an inverse correlation was observed between the percentage of cPC -both out of nucleated cells (rho = -0.173; p = 0.14) and within the total PC population (rho = -0.179; p = 0.12)- and the relative distribution of other B-cell population compartments (e.g., B-cell precursors) in BM (Fig. 2D, E respectively), such inverse correlation being more pronounced in SMM patients (rho = -0.566; p = 0.06). In line with these findings, a significant (inverse) correlation was also found between the percentage of cPC in BM and the number of normal mature B-lymphocytes circulating in blood (rho = -0.267; p = 0.02) (Fig. 2F), even when MGUS and SMM subjects were separately considered -(rho = -0.351; p = 0.009) and (rho = -0.441; p = 0.15), respectively.
Discussion
MM and WM are malignant hematological neoplasms characterized by the presence of a serum M-component secreted by an expanded population of cPC, which are preceded by an MGUS, followed by intermediate SMM or SWM stages [1, 2]. In recent years, several risk factors have been identified which are associated with a greater risk of progression from MGUS, SMM or SWM to MM and WM, respectively. Preliminary data on (ultrahigh-risk) SMM and, to a lesser extent, also MGUS patients, but not SWM [16, 37], support a potential benefit for early therapeutic interventions [10, 17, 20]. These observations have highlighted the potential utility of screening for the presence of a serum M-component in the general population. However, at these early stages of PC neoplasms, low levels of BM infiltration by clonal PC and/or B-cells are detected (in association with smaller serum M-component) which might go undetected by conventional cytological and histopathological approaches [26, 38, 39]. Such limitation might be overcome through the use of NGF techniques because of their higher sensitivity for the identification and immunophenotypic characterization of minimal numbers of cPC and cB-lymphocytes both in BM and blood [26, 40]. Here, we used NGF to investigate its potential utility in confirming the presence of neoplastic B-cells in healthy subjects and patients presenting with a serum M-component in a routine laboratory screening test, and its contribution to a more accurate classification of the underlying PC disorder independently of the isotype of the secreted M-protein.
Overall, the concentration (median) of the M-component found in MGUS cases in our cohort was significantly lower than that observed in previous series reported in the literature, based on both hospital-referred patients (5–12 g/l) [41,42,43] and other population-based studies (3.9 g/l) [44], which probably reflects the diagnostic screening strategy carried out within the study [20], potentially translated also in a higher frequency of cases adjusted per age.
Despite the lower serum M-component levels found in our versus the previously reported cohorts [41,42,43,44], NGF demonstrated the presence of cPC cells in the BM of 84% of cases with a persisting serum M-component associated with a population of clonal B-lymphocytes in nearly half (46%) of these cases. Of note, both clonal cell populations coexisted in more than a third of these individuals, among whom they shared immunophenotypic features consistent with related conditions in half of the cases. As expected, virtually all SMM cases showed the presence of cPC in BM in the absence of related cB-lymphocytes [1,2,3, 5,6,7], coexistence of cB-lymphocytes systematically corresponding to CLL-like MBL, except for one individual showing SWM-like features associated with two M-peaks (a major IgGκ-peak and a minor IgMκ-peak) [1, 2, 13, 15, 16]. In contrast, almost every SWM case showed coexistence of two related populations of cPC and cB-lymphocytes, with an immunophenotypic profile consistent with a diagnosis of SWM in all but one patient who had cPC consistent with SMM/MM coexisting with a CLL-like MBL [1, 2, 13, 15, 16]. These results support the diagnosis of an IgM (MM-like) MGUS in the later subject, in contrast to the other IgM-SWM cases, pointing out the utility of NGF for the (currently challenging) differential diagnosis between IgM-MGUS and other IgM-related neoplasms (e.g., SWM) [45,46,47]. In contrast, the immunophenotypic profiles found in MGUS cases were significantly more heterogeneous, typically consisting of a cPC population alone or together with either a coexisting CLL-like or a non-CLL-like MBL population in two-thirds of the cases. In the remaining MGUS cases, no cPC were detected or two related populations of cPC and cB-lymphocytes sharing SWM-like immunophenotypic profiles associated with the presence of an IgM-peak in the serum, were identified [1, 2, 13, 15, 16]. Overall, this later case plus two other IgM-MGUS cases found to display MM-like immunophenotypic profiles in their cPC, suggest a relatively higher incidence (4% vs 0.5–1% of MG) of IgM-MM-like MGUS cases in our vs previous cohorts [45,46,47]. Further detailed (e.g., genetic) characterization of cPC from these patients is required for their accurate diagnostic classification (via e.g., demonstration of the presence vs absence of the MYD88L265P mutation in MM-like IgM-MGUS vs SWM) [45,46,47]. Of note, in around half of the other MGUS cases who showed no cPC in the BM, cB-lymphocytes with a CLL-like phenotype or, to a lesser extent, non-CLL-like MBL features, were detected; whether in the non-CLL-like MBL cases the clonal B-lymphocytes are responsible for the serum M-component remains to be established. Interestingly, however, in both the MGUS and the SWM cases in whom no cPC nor cB-lymphocytes were detected the median serum concentration of the M-component was significantly lower than that of the other MGUS and SWM cases, supporting the notion that these might correspond to the earliest stages of disease in which cPC in BM are below the detection limit of the NGF techniques. In line with this hypothesis, a significant correlation was observed in our cohort between the number of cPC (and cPC plus cB-cells) in BM or blood and the serum concentration of the M-peak, similarly to what has been previously reported in the literature [48,49,50]. Alternatively, the putative M-component found in these cases might also include a fraction of false positive cases, in whom longer follow-up studies are needed to confirm the reactive vs neoplastic nature of the M-peak. Interestingly, here we also confirm previous observations in hospital-based MGUS and SMM patients that the percentage of cPC in the BM by NGF clearly differs between MGUS and SWM on one side, and SMM on the other side, which reflects the different rates of expansion and accumulation of pathological cPC in BM throughout the whole spectrum of these diseases. Noteworthy, MBL (mostly CLL-like MBL) was detected in a significant fraction of our cases, its frequency being higher among individuals with (vs without) a coexisting cPC population.
Previous studies have shown the presence of circulating cPC by NGF in blood of a high percentage of SMM and MM, and to a less extent also MGUS cases [51,52,53,54], which could be used at diagnosis for a more comprehensive management of these patients, as regards the timing to perform a BM study. Thus, an additional goal of our study was to investigate the presence of circulating cPC in the blood of our subjects, in parallel to the BM study. Overall, in more than a third of those cases who showed cPC in BM, a cPC population with an identical immunophenotype was also found in blood. In addition, the majority of cases with coexisting cPC and cB-cells and all of those who had only clonal mature B-lymphocytes in BM, showed circulating cB-lymphocytes in blood as well. Despite previous reports from our group and others [51, 55] have found higher rates of circulating cPC in MGUS and SMM as compared to our current data, the lower rate reported here might be due to the differences in the nature of the distinct patient cohorts, since our cohort is based on a screening performed in the general population whereas the others correspond to hospital-based series [56, 57]. In line with this hypothesis, a significant correlation was found here between the percentage of clonal B-cells and cPC in BM and both their percentage and absolute number in blood, as well as between the percentage of cPC in blood and the serum concentration of the M-component [1,2,3, 58].
Most interestingly, here we found an inverse correlation between the percentage of cPC in the BM and both the percentage of BM B-cell precursors and the blood B-lymphocyte counts, supporting the notion that progressive accumulation of cPC in the BM of MG patients not only replaces normal PC in their BM niches, but it also progressively affects normal B-cell production, already at very early stages of disease [51, 59].
In summary, our results demonstrate that NGF immunophenotypic analysis of BM and, to a lesser extent also, blood samples from individuals at the very early stages of MG, provides complementary data to that obtained through conventional diagnostic procedures via a more precise definition of the clonal nature of the (either related or unrelated) cell populations involved, and contributes to a more accurate diagnosis and classification of PC neoplasms in around one third of MG presenting with a serum M-component in screening programs like iSTOPMM, being particularly useful in distinguishing SWM from IgM-MGUS cases. Based on these results, we envisage that high-sensitive blood investigation of circulating cPC and cB-cells might be included in the initial diagnostic workup of MG, to support disease diagnosis and classification and to help optimizing the timing of BM evaluation. The relative simplicity, high sensitivity, short time to results and worldwide availability of NGF, further facilitate the incorporation of the proposed assay in routine diagnostics for the characterization of patients with a serum M-component.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Alaggio R, Amador C, Anagnostopoulos I, Attygalle AD, Araujo IBdeO, Berti E, et al. The 5th edition of the World Health Organization classification of haematolymphoid tumours: lymphoid neoplasms. Leukemia 2022;36:1720–48.
Swerdlow SH, Campo E, Lee Harris N, Jaffe ES, Pileri SA, Stein H, et al. WHO classification of tumors of hematopoietic and lymphoid tissues. 2017.
Rajkumar SV. Multiple myeloma: 2022 update on diagnosis, risk stratification, and management. Am J Hematol. 2022;97:1086–107.
Murray D, Kumar SK, Kyle RA, Dispenzieri A, Dasari S, Larson DR, et al. Detection and prevalence of monoclonal gammopathy of undetermined significance: a study utilizing mass spectrometry-based monoclonal immunoglobulin rapid accurate mass measurement. Blood Cancer J. 2019;9:102.
Rajkumar SV. Multiple myeloma: 2020 update on diagnosis, risk-stratification and management. Am J Hematol. 2020;95:548–67.
Rajkumar SV, Dimopoulos MA, Palumbo A, Blade J, Merlini G, Mateos MV, et al. International Myeloma Working Group updated criteria for the diagnosis of multiple myeloma. Lancet Oncol. 2014;15:e538–48.
Rajkumar SV. Multiple myeloma: 2018 update on diagnosis, risk-stratification, and management. Am J Hematol. 2018;93:1091–110.
Thorsteinsdóttir S, Gíslason GK, Aspelund T, Rögnvaldsson S, Óskarsson JÞ, Sigurðardóttir GÁ, et al. Prevalence of smoldering multiple myeloma based on nationwide screening. Nat Med. 2023;29:467–72.
Kyle RA, Larson DR, Therneau TM, Dispenzieri A, Kumar S, Cerhan JR, et al. Long-Term Follow-up of Monoclonal Gammopathy of Undetermined Significance. N Engl J Med. 2018;378:241–9.
Mateos MV, Kumar S, Dimopoulos MA, González-Calle V, Kastritis E, Hajek R, et al. International Myeloma Working Group risk stratification model for smoldering multiple myeloma (SMM). Blood. Cancer J. 2020;10:102.
Musto P, Engelhardt M, Caers J, Bolli N, Kaiser M, van de Donk N, et al. 2021 European myeloma network review and consensus statement on smoldering multiple myeloma: How to distinguish (and manage) Dr. Jekyll and Mr. Hyde. Haematologica.2021;106:2799–812.
Fend F, Dogan A, Cook JR. Plasma cell neoplasms and related entities-evolution in diagnosis and classification. Virchows Arch Int J Pathol. 2023;482:163–77.
Gertz MA. Waldenström macroglobulinemia: 2021 update on diagnosis, risk stratification, and management. Am J Hematol. 2021;96:258–69.
Khwaja J, D’Sa S, Minnema MC, Kersten MJ, Wechalekar A, Vos JMI. IgM monoclonal gammopathies of clinical significance: diagnosis and management. Haematologica. 2022;107:2037–50.
Kyle R, Benson J, Larson D, Therneau T, Dispenzieri A, Melton LJ, et al. IgM monoclonal gammopathy of undetermined significance and smoldering Waldenström’s macroglobulinemia. Clin Lymphoma Myeloma. 2009;9:17–8.
Kyle RA, Benson JT, Larson DR, Therneau TM, Dispenzieri A, Kumar S, et al. Progression in smoldering Waldenström macroglobulinemia: Long-term results. Blood 2012;119:4462–6.
Rajkumar SV, Kumar S, Lonial S, Mateos MV. Smoldering multiple myeloma current treatment algorithms. Blood Cancer J. 2022;12:129.
Pham A, Mahindra A. Solitary plasmacytoma: a review of diagnosis and management. Curr Hematol Malig Rep. 2019;14:63–9.
Wang W, Lin P. Lymphoplasmacytic lymphoma and Waldenström macroglobulinaemia: clinicopathological features and differential diagnosis. Pathology. 2020;52:6–14.
Rögnvaldsson S, Love TJ, Thorsteinsdottir S, Reed ER, Óskarsson JÞ, Pétursdóttir Í, et al. Iceland screens, treats, or prevents multiple myeloma (iStopMM): a population-based screening study for monoclonal gammopathy of undetermined significance and randomized controlled trial of follow-up strategies. Blood Cancer J. 2021;11:94.
Sanchez ML, Almeida J, Gonzalez D, Gonzalez M, Garcia-Marcos MA, Balanzategui A, et al. Incidence and clinicobiologic characteristics of leukemic B-cell chronic lymphoproliferative disorders with more than one B-cell clone. Blood. 2003;102:2994–3002.
Paiva B, Merino J, Miguel JFS. Utility of flow cytometry studies in the management of patients with multiple myeloma. Curr Opin Oncol. 2016;28:511–7.
Galtseva IV, Davydova YO, Kapranov NM, Julhakyan HL, Mendeleeva LP. Minimal residual disease in multiple myeloma: Benefits of flow cytometry. Int J Lab Hematol. 2018;40:12–20.
Paiva B, Puig N, Cedena MT, Rosiñol L, CordónCord L, En Vidriales MB, et al. Measurable residual disease by next-generation flow cytometry in multiple myeloma. J Clin Oncol. 2019;38:784–92.
Anderson KC, Auclair D, Adam SJ, Agarwal A, Anderson M, Avet-Loiseau H, et al. Minimal residual disease in myeloma: application for clinical care and new drug registration. Clin Cancer Res. 2021;27:5195–212.
Flores-Montero J, Sanoja-Flores L, Paiva B, Puig N, García-Sánchez O, Böttcher S, et al. Next-generation flow for highly sensitive and standardized detection of minimal residual disease in multiple myeloma. Leukemia. 2017;31:2094–103.
Flores-Montero J, Grigore G, Fluxá R, Hernández J, Fernandez P, Almeida J, et al. EuroFlow Lymphoid Screening Tube (LST) data base for automated identification of blood lymphocyte subsets. J Immunol Methods. 2019;475:112662.
van Dongen JJM, Lhermitte L, Böttcher S, Almeida J, van Der Velden VHJ, Flores-Montero J, et al. EuroFlow antibody panels for standardized n-dimensional flow cytometric immunophenotyping of normal, reactive and malignant leukocytes. Leukemia. 2012;26:1908–75.
Dogliotti I, Jiménez C, Varettoni M, Talaulikar D, Bagratuni T, Ferrante M, et al. Diagnostics in Waldenström’s macroglobulinemia: a consensus statement of the European Consortium for Waldenström’s Macroglobulinemia. Leukemia. 2023;37:388–95.
San Miguel JF, Vidriales MB, Ocio E, Mateo G, Sánchez-Guijo F, Sánchez ML, et al. Immunophenotypic analysis of Waldenstrom’s macroglobulinemia. Semin Oncol. 2003;30:187–95.
Paiva B, Montes MC, García-Sanz R, Ocio EM, Alonso J, De Las Heras N, et al. Multiparameter flow cytometry for the identification of the Waldenström’s clone in IgM-MGUS and Waldenström’s Macroglobulinemia: new criteria for differential diagnosis and risk stratification. Leukemia. 2014;28:166–73.
Palmason R, Berlanga O, Sigurdsson JK, Rögnvaldsson S, Thorsteinsdottir S, Ekberg S, et al. Transient M-proteins: epidemiology, causes, and the impact of mass spectrometry: the Istopmm study. Blood. 2022;140:2338–40.
van der Velden VHJ, Flores-Montero J, Perez-Andres M, Martin-Ayuso M, Crespo O, Blanco E, et al. Optimization and testing of dried antibody tube: The EuroFlow LST and PIDOT tubes as examples. J Immunol Methods. 2019;475:112287.
Kalina T, Flores-Montero J, van Der Velden VHJ, Martin-Ayuso M, Böttcher S, Ritgen M, et al. EuroFlow standardization of flow cytometer instrument settings and immunophenotyping protocols. Leukemia. 2012;26:1986–2010.
Pérez-Persona E, Vidriales MB, Mateo G, García-Sanz R, Mateos MV, De Coca AG, et al. New criteria to identify risk of progression in monoclonal gammopathy of uncertain significance and smoldering multiple myeloma based on multiparameter flow cytometry analysis of bone marrow plasma cells. Blood. 2007;110:2586–92.
Strati P, Shanafelt TD. Monoclonal B-cell lymphocytosis and early-stage chronic lymphocytic leukemia: diagnosis, natural history, and risk stratification. Blood. 2015;126:454–62.
Cingam S, Sidana S. Differential diagnosis of Waldenström’s macroglobulinemia and early management: perspectives from clinical practice. Blood Lymphat Cancer Targets Ther. 2022;12:107–17.
Murray D, Puig N, Kristinsson S, Usmani SZ, Dispenzieri A, Bianchi G, et al. Mass spectrometry for the evaluation of monoclonal proteins in multiple myeloma and related disorders: an International Myeloma Working Group Mass Spectrometry Committee Report. Blood Cancer J. 2021;11:24.
Mills JR, Kohlhagen MC, Dasari S, Vanderboom PM, Kyle RA, Katzmann JA, et al. Comprehensive assessment of M-proteins using nanobody enrichment coupled to MALDI-TOF mass spectrometry. Clin Chem. 2016;62:1334–44.
Oliva-Ariza G, Fuentes-Herrero B, Carbonell C, Lecrevisse Q, Pérez-Pons A, Torres-Valle A, et al. High frequency of low-count monoclonal B-cell lymphocytosis in hospitalized COVID-19 patients. Blood. 2023;141:309–14.
Rajkumar SV, Kyle RA, Therneau TM, Melton LJ, Bradwell AR, Clark RJ, et al. Serum free light chain ratio is an independent risk factor for progression in monoclonal gammopathy of undetermined significance. Blood. 2005;106:812–7.
Kyle RA, Therneau TM, Rajkumar SV, Larson DR, Plevak MF, Offord JR, et al. Prevalence of monoclonal gammopathy of undetermined significance. N Engl J Med. 2006;354:1362–9.
Turesson I, Kovalchik SA, Pfeiffer RM, Kristinsson SY, Goldin LR, Drayson MT, et al. Monoclonal gammopathy of undetermined significance and risk of lymphoid and myeloid malignancies: 728 cases followed up to 30 years in Sweden. Blood. 2014;123:338–45.
García Mateo A. Gammapatía Monoclonal de Significado Incierto en la provincia de Segovia: Estudio poblacional y factores pronósticos (células plasmáticas en sangre periférica por inmunofenotipo y ensayo de cadena pesada-ligera de las inmunoglobulinas). 2019.
Castillo JJ, Jurczyszyn A, Brozova L, Crusoe E, Czepiel J, Davila J, et al. IgM myeloma: a multicenter retrospective study of 134 patients. Am J Hematol. 2017;92:746–51.
Laganà A, Parekh S.Distinct) origins of IgM myeloma.Blood. 2021;138:1914–5..
Lu H, Durkin L, Zhao X, Nakashima MO. IgM plasma cell myeloma. Am J Clin Pathol. 2022;157:47–53.
Keren DF, Schroeder L. Challenges of measuring monoclonal proteins in serum. Clin Chem Lab Med. 2016;54:947–61.
Murray DL, Ryu E, Snyder MR, Katzmann JA. Quantitation of serum monoclonal proteins: relationship between agarose gel electrophoresis and immunonephelometry. Clin Chem. 2009;55:1523–9.
Clavijo A, Ryan N, Xu H, Singh G. Measurement of monoclonal immunoglobulin protein concentration in serum protein electrophoresis: comparison of automated vs manual/human readings. Lab Med. 2019;51:252–8.
Sanoja-Flores L, Flores-Montero J, Garcés JJ, Paiva B, Puig N, García-Mateo A, et al. Next generation flow for minimally-invasive blood characterization of MGUS and multiple myeloma at diagnosis based on circulating tumor plasma cells (CTPC). Blood Cancer J. 2018;8:117.
Garcés JJ, Cedena MT, Puig N, Burgos L, Perez JJ, Cordon L, et al. Circulating tumor cells for the staging of patients with newly diagnosed transplant-eligible multiple myeloma. J Clin Oncol. 2022;40:3151–61.
Garcés JJ, Bretones G, Burgos L, Valdes-Mas R, Puig N, Cedena MT, et al. Circulating tumor cells for comprehensive and multiregional non-invasive genetic characterization of multiple myeloma. Leukemia. 2020;34:3007–18.
Termini R, Žihala D, Terpos E, Perez-Montaña A, Jelínek T, Raab M, et al. Circulating tumor and immune cells for minimally invasive risk stratification of smoldering multiple myeloma. Clin Cancer Res. 2022;28:4771–81.
Nowakowski GS, Witzig TE, Dingli D, Tracz MJ, Gertz MA, Lacy MQ, et al. Circulating plasma cells detected by flow cytometry as a predictor of survival in 302 patients with newly diagnosed multiple myeloma. Blood. 2005;106:2276–9.
Garcés JJ, San-Miguel J, Paiva B. Biological characterization and clinical relevance of circulating tumor cells: opening the pandora’s box of multiple myeloma. Cancers. 2022;14:1–11.
Sanoja-Flores L, Flores-Montero J, Pérez-Andrés M, Puig N, Orfao A. Detection of circulating tumor plasma cells in monoclonal gammopathies: methods, pathogenic role, and clinical implications. Cancers. 2020;12:1–26.
Wang Y, Liu J, Burrows PD, Wang JY. B cell development and maturation. Adv Exp Med Biol. 2020;1254:1–22.
Paiva B, Pérez-Andrés M, Vídriales MB, Almeida J, De Las Heras N, Mateos MV, et al. Competition between clonal plasma cells and normal cells for potentially overlapping bone marrow niches is associated with a progressively altered cellular distribution in MGUS vs myeloma. Leukemia. 2011;25:697–706.
Acknowledgements
The iSTOPMM study was funded by the International Myeloma Foundation-Black Swan Research Initiative and the Icelandic Centre for Research (grant agreement No 173857, 217897-051 and 228521-051), and received funding from the European Research Council (ERC) under the European Union’s Horizon 2020 research and innovation program (grant agreement No 716677 and 101045549), and is also supported by the EuroFlow Consortium and The Binding Site Group. OP-E was supported by a grant from the Government of Castilla y León (Orden EDU/601/2020), Spain. LS-F was supported by the Sara Borrell Grant (No CD21/00162) from Instituto de Salud Carlos III, Madrid, Spain. Mass spectrometry tests were performed by The Binding Site Ltd. Birmingham, UK.
Author information
Authors and Affiliations
Contributions
OP-E, JF-M, SÞ, SR, TJL, SYK, and AO contributed to the design, review of the protocol and supervision of the work. OP-E, JÞO, LS-F, JP, SM, ERR, and GKH performed the experiments and data acquisition. OP-E, JF-M, JÞO, LS-F, QL, ERR, GKH, SH, BD, SYK, and AO participated in data analysis, reporting and interpretation of the results. OP-E, JF-M, and AO wrote the paper. All authors critically reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
JF-M and AO are inventors of the EuroFlow-owned patents PCT/NL2010/050332 (Methods, reagents, and kits for flow cytometric immunophenotyping of normal, reactive and malignant leukocytes) and PCT/NL20 13/050420 (Methods, reagents and kits for detecting minimal residual disease), licensed to BD Biosciences (San José, CA, USA) which pay royalties to the EuroFlow Consortium. These royalties are exclusively used for continuation of the EuroFlow collaboration and sustainability of the EuroFlow Consortium. SYK has received research funding from Amgen and Celgene. SH is currently employed by The Binding Site. OP-E, JÞO, LS-F, JP, QL, SM, ERR, GKH, and BD declare no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pérez-Escurza, O., Flores-Montero, J., Óskarsson, J.Þ. et al. Immunophenotypic assessment of clonal plasma cells and B-cells in bone marrow and blood in the diagnostic classification of early stage monoclonal gammopathies: an iSTOPMM study. Blood Cancer J. 13, 182 (2023). https://doi.org/10.1038/s41408-023-00944-1
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41408-023-00944-1