Retinal capillary hemangioblastoma (RCH) is a rare tumor of the retinal vasculature that can occur sporadically or as part of von Hippel-Lindau (VHL) syndrome.1 Identifying an RCH can lead to the diagnosis of VHL, an autosomal-dominant and potentially life-threatening multi-organ neoplastic syndrome. Most RCHs are endophytic, meaning they grow inward toward the vitreous cavity, resulting in a characteristic red-orange, nodular, vascularized mass with dilated feeder vessels that are usually straightforward to diagnose. However, exophytic RCHs grow in the direction of the subretinal space, resulting in a subtle ophthalmoscopic appearance that is more challenging to diagnose, particularly when located near the optic disc.2 Exophytic juxtapapillary RCHs (JRCHs) can simulate more common conditions such as optic disc edema or peripapillary choroidal neovascularization (CNV).2,3
JRCH CASES
We recently published a retrospective case series describing the role of multimodal imaging for diagnosing exophytic JRCH (Figures 1-3).4 Of the 12 patients with exophytic JRCH, six were male, and the average age was 54 years. Five patients had been previously diagnosed with VHL syndrome, while the other seven had negative clinical and genetic workups for VHL.

Figure 1. This middle-aged patient with no known history of VHL syndrome had fovea-involving exudation with decreased visual acuity. There was subtle opacification of the superior juxtapapillary retina, blurring of the superior disc margin (arrows), and remote hard exudates. The referral diagnosis was peripapillary CNV, but the macular edema had not responded to anti-VEGF injections. The patient was diagnosed with an exophytic JRCH.
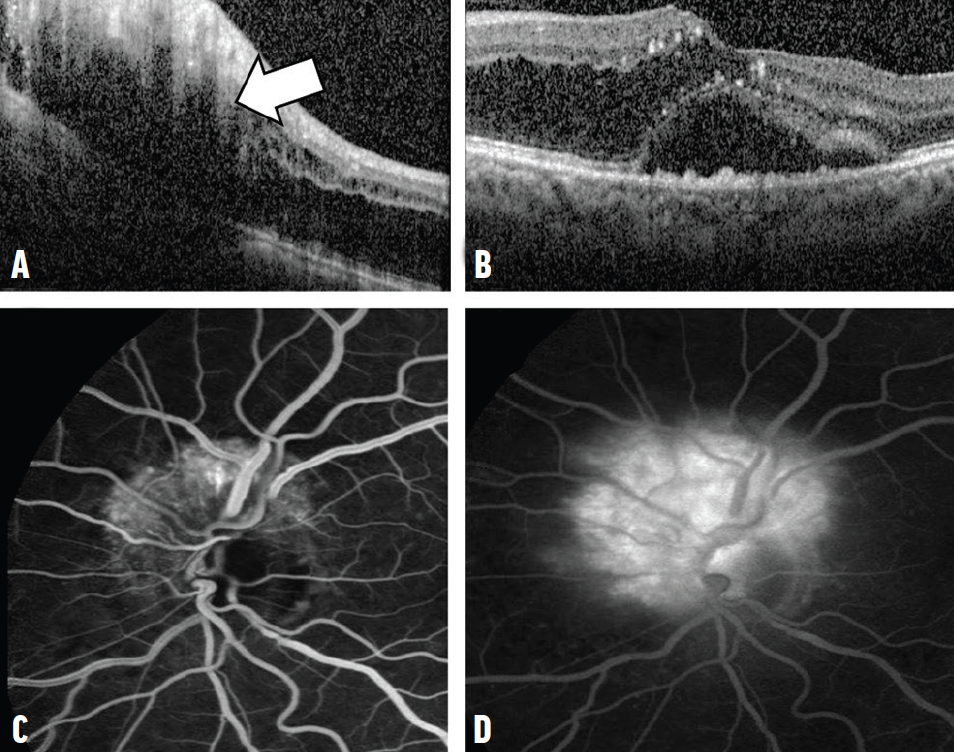
Figure 2. OCT through the juxtapapillary lesion in Figure 1 revealed a hyperreflective lesion (arrow) in the middle/outer retinal layers with outer retinal and choroidal shadowing and adjacent intraretinal fluid (A). Foveal OCT showed intraretinal fluid tracking from the disc and subretinal fluid (B). Early-frame FA showed hyperfluorescence of a juxtapapillary vascular lesion deep to the retinal vessels (C). Late-frame FA showed leakage/staining of the lesion (D).
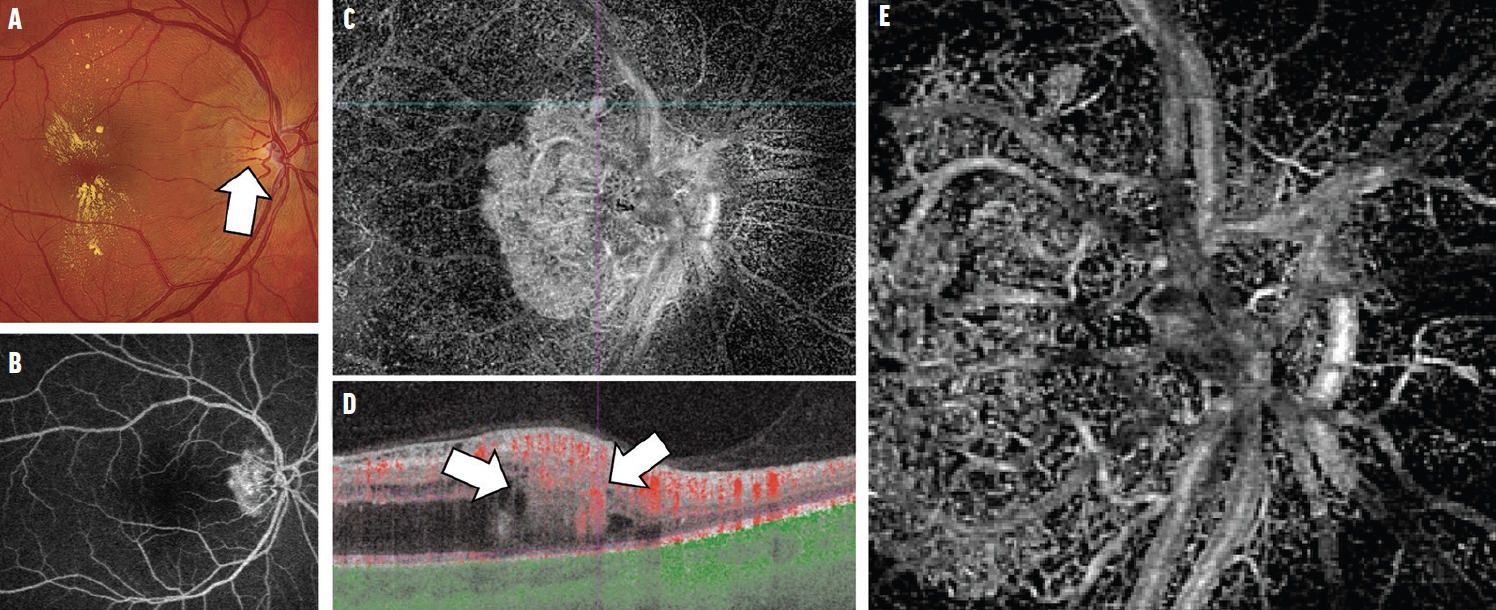
Figure 3. This patient with no known history of VHL syndrome had subtle thickening of the temporal juxtapapillary retina with sectoral blurring of the disc margin, dilated draining veins (arrow), remote hard exudates, and foveal macular edema that had not responded to 18 monthly anti-VEGF injections (A). The early-frame FA showed hyperfluorescence of a juxtapapillary vascular lesion deep to the retinal vessels (B). A 9x9 mm SS-OCTA image confirmed an intraretinal juxtapapillary vascular lesion (C). The corresponding B-scan showed a hyperreflective lesion (arrows) within the outer retinal layers and no PED (D). A 3x3 mm SS-OCTA image of the lesion characterized the individual vessels of the lesion in high resolution (E). The patient was diagnosed with exophytic JRCH.
The initial referring diagnoses included JRCH (in those with known VHL), peripapillary CNV (three patients), neuroretinitis (two patients), optic disc metastasis (one patient), and branch retinal vein occlusion (one patient). Multiple RCHs were present in three of the five patients with VHL, and none of the patients without VHL had multiple lesions. Treatments included photodynamic therapy (PDT), intravitreal anti-VEGF injections, laser photocoagulation, intravitreal or sub-Tenon’s triamcinolone, and observation.
THE CLINICAL PICTURE
The most common features of exophytic JRCHs are pink or red color (66%), lipid exudates (83%), and intraretinal fluid (92%).4 OCT in all exophytic JRCHs showed hyperreflective lesions in the outer retina with choroidal shadowing. On fluorescein angiography (FA), all cases showed early hyperfluorescence with late leakage and staining. OCT angiography (OCTA) showed abnormal vasculature within the middle and outer retinal layers. The lesions were hypoautofluorescent, and on B-scan they were hyperechoic and vascularized.
Clinical examination alone was inadequate to confidently diagnose exophytic JRCH. Ophthalmoscopically, the lesions manifested as a subtle bulge at the disc margin, often with remote lipid exudation. Lesions with a pink/red color were often mistaken for peripapillary CNV or a small subretinal hemorrhage. If they obscured the disc margin, they often mimicked optic disc edema or neuroretinitis. When the lesion caused pseudo-disc edema, the blurred disc margin was sectoral with hard exudates located farther from the disc than in papillitis or neuroretinitis. The differential diagnoses included combined hamartoma of the retina and retinal pigment epithelium, astrocytic hamartoma, and optic disc granuloma or metastasis.
IMAGING OPTIONS
Multimodal imaging is essential to differentiate these entities. For example, OCT of a peripapillary CNV will show a pigment epithelial detachment (PED) with associated subretinal vasculature, whereas exophytic JRCHs have no PED, and the abnormal vasculature resides in the middle/outer retinal layers. CNV tends to have more subretinal fluid than intraretinal fluid; the opposite is true for exophytic JRCH.
On FA, an eye with disc edema may have engorged disc vessels that are typically localized to the disc borders and encompass the entire disc, whereas the vessels of an exophytic JRCH extend beyond the disc border and only involve a segment of the disc. Swept-source (SS) OCTA can pinpoint the distribution and depth of abnormal vasculature, eliminating the need for dye-based angiography.5
HOW TO TREAT
Asymptomatic exophytic JRCHs require no treatment, but exudation can progress to threaten the fovea, so patients need to be monitored closely. Exophytic JRCHs in the papillomacular bundle are more likely to have macular exudation and vision loss.
We prefer full-fluence PDT as an initial treatment, sometimes supplemented with intravitreal anti-VEGF agents and intravitreal/periocular corticosteroids. Multiple PDT sessions may be necessary. Lesions outside of the papillomacular bundle can often be successfully treated with laser photocoagulation alone. Anti-VEGF therapy alone is generally inadequate to induce regression, although we recently used serial SS-OCTA imaging to demonstrate decreased vascular congestion and macular edema for a few weeks after anti-VEGF injections to treat an exophytic JRCH, suggesting that more frequent or higher dosing of anti-VEGF agents may be adequate to control exudation.5
CLINICAL PEARLS
Because of its association with VHL, the diagnosis of a JRCH should prompt a careful fundus examination for additional RCHs, which would be consistent with VHL.
Ultra-widefield FA can sometimes identify ophthalmoscopically invisible RCHs elsewhere in the fundus. More than one RCH confirms a diagnosis of VHL. Patients with solitary RCH lesions may benefit from systemic evaluation, imaging for tumors in other organs, and genetic testing for the VHL gene.
1. Wong WT, Agron E, Coleman HR, et al. Clinical characterization of retinal capillary hemangioblastomas in a large population of patients with von Hippel-Lindau disease. Ophthalmology. 2008;115(1):181-188.
2. Gass JD, Braunstein RA. Sessile and exophytic capillary angiomas of the juxtapapillary retina and optic nerve head. Arch Ophthalmol. 1980;98(10):1790-1797.
3. McCabe CM, Flynn Jr HW, Shields CL, et al. Juxtapapillary capillary hemangiomas. Clinical features and visual acuity outcomes. Ophthalmology. 2000;107(12):2240-2248.
4. Russell JF, Villegas VM, Schwartz SG, et al. Multimodal imaging in the diagnosis of exophytic juxtapapillary retinal capillary hemangioblastoma. Am J Ophthalmol. 2021;225:128-136.
5. Russell JF, Shi Y, Gregori G, Rosenfeld PJ. Longitudinal swept-source OCT angiography of juxtapapillary retinal capillary hemangioblastoma. Ophthalmol Retina. 2020;4(9):956-958.
























