Hand Anatomy, Bones & Muscles
The Hand Anatomy is complex and important to understand, it consists of 27 bones, 27 joints, 34 muscles and a lot of ligaments that connects joints together.
To understand the complex hand anatomy, we will divide this article into: bones anatomy, joints anatomy, muscles and ligaments anatomy.
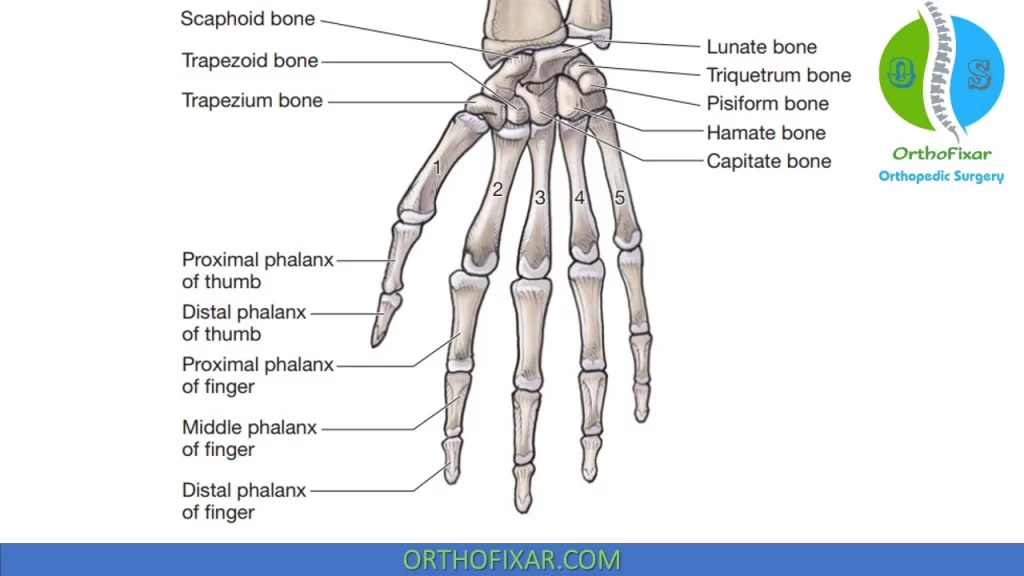
Bony Hand Anatomy
Metacarpals Bones
There are 5 metacarpals in each hand, each metacarpal consist of two ossification centers:
- One for the body (primary center of ossification), which ossifies at 8 weeks’ gestation (like most long bones).
- One distally at the neck, which usually appears before 3 years of age.
First metacarpal is a primordial phalanx, and its secondary ossification center is located at the base (like those of phalanges).
See Also: Hand & Wrist Movements
| Metacarpal | Features |
|---|---|
| I (Thumb) | Short, stout; base is saddle-shaped |
| II (Index) | Longest, largest base; medial at base |
| III (Middle) | Styloid process |
| IV (Ring) | Small quadrilateral base, narrow shaft |
| V (Small) | Tubercle at base (extensor carpi ulnaris) |
See Also: Bennett Fracture
Phalanges Bones
Each hand has 14 phalanges (three for each finger and two for the thumb), which are similar. All have secondary ossification centers proximally at their bases that appear at ages 3 years (proximal), 4
years (middle), and 5 years (distal).
Bases of the proximal phalanges are oval and concave, with the smaller heads ending in two condyles. Middle phalanges have two concave facets at their bases and pulley-shaped heads. Distal phalanges are smaller and have palmar ungual tuberosities distally.
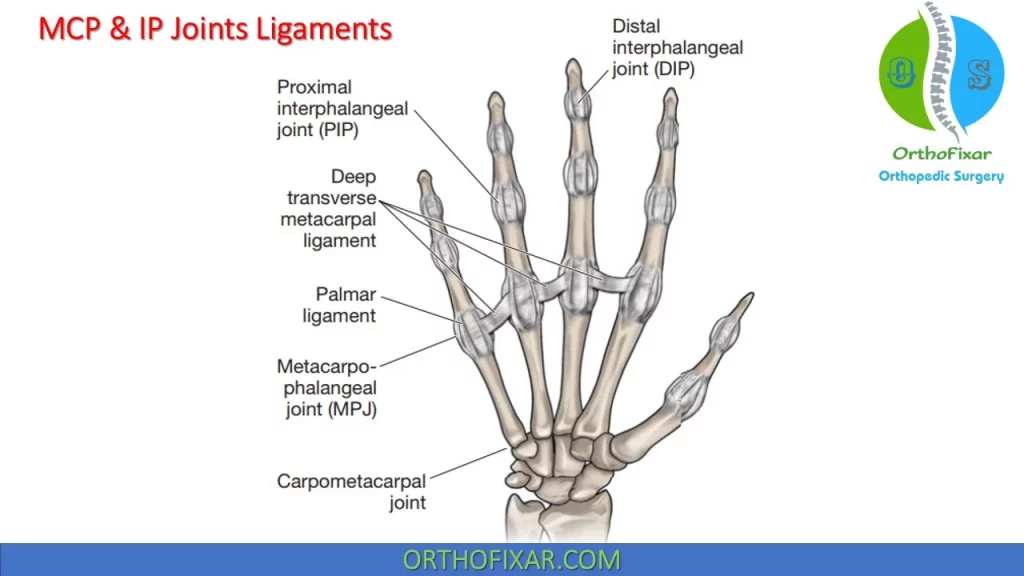
Hand joints Anatomy
The joints of hand anatomy consists of carpometacarpal joints (joints between carpal bones and metacarpals that is discussed in wrist anatomy), Metacarpophalangeal Joints (MCP Joints) and interphalangeal joints (IP Joints).
See Also: Wrist Anatomy
Metacarpophalangeal Joints:
The five metacarpals resemble miniature versions of the long bones of the body, with elongated shafts and expanded ends.
MCP of the Thumb Anatomy:
The metacarpophalangeal (MCP) joint of the thumb is a hinge joint. Its bony configuration, which resembles the interphalangeal (IP) joints, provides it with some inherent stability. In addition, support for the joint is provided by anterior (palmar) and collateral ligaments.
The thumb MCP joint consists of a convex surface on the head of the metacarpal and a concave surface on the base of the phalanx. The area of the articulating surface is increased by the presence of a volar plate, which allows greater range of motion than would be available otherwise.
Approximately 75–80 degrees of flexion is available at the thumb MCP joint. The extension movements as well as the abduction and adduction motions are negligible. Traction, gliding, and rotatory accessory movements are also present.
Other MCP Joint Anatomy:
The second through fifth metacarpals articulate with the respective proximal phalanges within biaxial joints. Their widened, proximal bases articulate with the carpals and with one another in plane joints.10 Their biconvex distal heads are broader anteriorly than posteriorly, the significance of which
is discussed later.
The MCP joints allow flexion–extension and medial–lateral deviation associated with a slight degree of axial rotation. The design of the MCP joint allows for great amplitude of movement, at the expense of stability. Approximately 90 degrees of flexion is available at the second MCP, with the amount of available flexion progressively increasing toward the fifth MCP. Active extension at these joints is 25–30 degrees, while 90 degrees can be obtained passively.
Approximately 20 degrees of abduction/adduction can occur in either direction at the MCP, with more being available in extension than in flexion. Abduction–adduction movements of the MCP joints are restricted in flexion and free in extension.
The joint capsules are attached to the articular margins of the metacarpals and phalanges and surround the MCP joints. The joint capsule of these joints is relatively lax and redundant, but is endowed with collateral ligaments that pass posterior to the joint axis for flexion/extension of the MCP joints. Although, these collateral ligaments are lax in extension, they become taut in approximately 70–90 degrees of
flexion of the MCP joint.
Contracture of the collateral ligaments is a major cause of loss of MCP flexion. The MCP joints should never, under any circumstances, be immobilized in extension or hyperextension by a retraction of the collateral ligaments, which would result in their locking. Instead the fingers should be splinted with the MCP joints flexed to 70–90 degrees.
The posterior (dorsal) hood apparatus reinforces (or replaces) the posterior (dorsal) joint capsules. The fibrocartilaginous volar plates reinforce the anterior (palmar) aspects of the joints. The volar plates attach firmly to the phalangeal bases but connect only loosely to the metacarpal heads by membranous fibers. Their posterior (dorsal) surface contributes to the joint area, whereas their anterior (palmar)
surface channels the finger flexor tendons.
The asymmetry of the metacarpal heads as well as the difference in length and direction of the collateral ligaments also explains the rotational movement of the proximal phalanx during flexion–extension and why the ulnar deviation of the digits normally is greater than the radial deviation. The rotary movements that occur are called conjunct rotations. The index finger has a conjunct rotation of internal rotation with abduction and flexion, whereas the ring and little finger each have a conjunct rotation of external rotation with abduction and flexion. The middle finger is not thought to have a conjunct rotation.
Hand IP Joints Anatomy
Adjacent phalanges articulate in hinge joints that allow motion in only one plane: sagittal. The congruency of the IP joint surfaces contributes greatly to IP joint stability. In addition, the IP joints are surrounded by joint capsules that are attached to the articular margins of the phalanges.
Proximal Interphalangeal Joint:
The proximal interphalangeal (PIP) joint is a hinged joint capable of flexion and extension.
The supporting ligaments and tendons provide the bulk of the static and dynamic stability of this joint as it travels through a normal range of 110 degrees.
The capsule surrounding the articular surface of the joint is composed of the volar plate, lateral and accessory collateral ligaments, and extensor expansion. The proximal IP joint is stable in all positions.
The configuration of the volar plate allows it to function as a static restraint to hyperextension and to influence the mechanical advantage of the flexor tendons at the initiation of PIP joint flexion. The volar plate also increases the surface area. This allows for a greater range of motion than would be available otherwise.
The thick collateral ligaments (true and accessory) of the PIP joint combine with the volar plate to provide lateral stability: the collateral ligaments of the PIP joints are maximally taut at 25 degrees of finger flexion. For this reason, the IP joints are usually splinted in 25 degrees of flexion following surgery to prevent joint contractures. The splinting position is changed as the patient resumes function.
The flexor tendon system at the level of the PIP joint is less complex than the extensor mechanism and contributes very little to injuries about the PIP joint.
The phalangeal bases effectively form a sellar surface, with bone projections allowing for a wide range of accessory movements to accommodate the gripping of a large array of irregular surfaces. The motions available at the Proximal Interphalangeal Joint consist of:
- approximately 110 degrees of flexion at the PIP joints and 90 degrees at the thumb IP joint.
- Extension reaches 0 degrees at the PIP joints and 25 degrees at the thumb IP joint.
- Traction, gliding, and accessory movements also occur at the IP joints.
Distal Interphalangeal Joints:
The distal interphalangeal (DIP) joint has similar structures as the PIP joint but less stability and allows some hyperextension. The motions available at the Distal Interphalangeal Joints consist of:
- approximately 90 degrees of flexion
- 25 degrees of extension.
- Traction, gliding, and accessory movements also occur at the DIP joints
Hand Muscles Anatomy
The hand muscles are those that originate and insert within the hand and are responsible for fine finger movements.
Short Muscles of the Thumb
Abductor Pollicis Brevis:
The APB arises from the flexor retinaculum and the trapezium bone and inserts on the radial aspect of the proximal phalanx of the thumb. It is innervated by the median nerve and functions to abduct the first metacarpal and proximal phalanx of the thumb.
Flexor Pollicis Brevis:
The FPB arises from two heads. The superficial head arises from the flexor retinaculum and the trapezium bone, while the deep head arises from the floor of the carpal canal. The FPB inserts on the base of the proximal phalanx of the thumb. The superficial head receives its innervation from the median nerve, while the deep head is innervated by the ulnar nerve. The FPB functions to flex the proximal phalanx of the thumb.
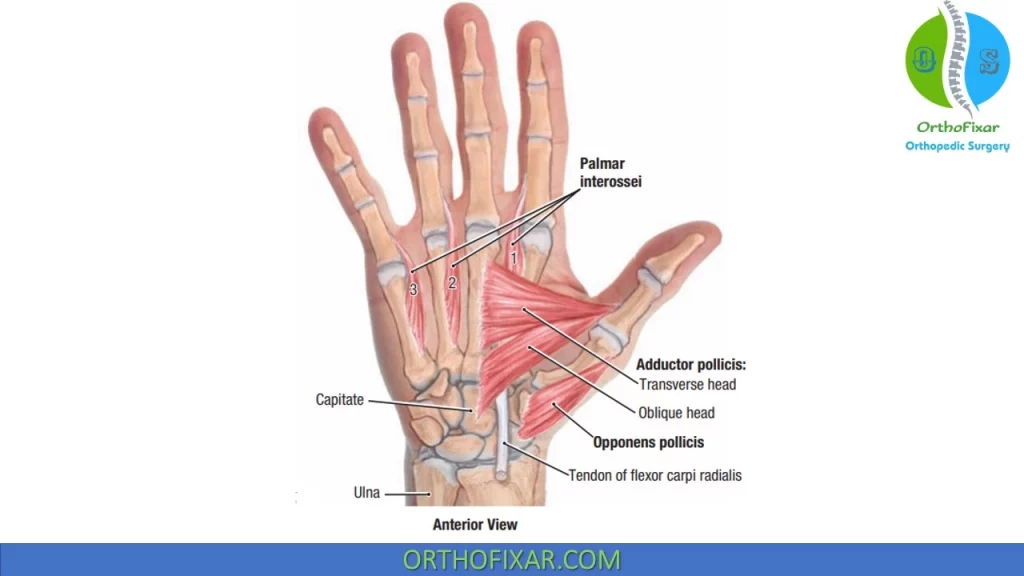
Opponens Pollicis:
The OP arises from the flexor retinaculum and the trapezium bone and inserts along the radial surface of the first metacarpal. The OP is innervated by the median nerve and functions to flex, rotate, and slightly abduct the first metacarpal across the palm to allow for opposition with each of the other digits.
Adductor Pollicis (AP):
The AP arises from two heads. The transverse head originates from the ventral surface of the shaft of the third metacarpal, while the oblique head originates from the trapezium, trapezoid, and capitate bones, and the base of the second and third metacarpal bone. The AP inserts on the ulnar side of the base of the proximal phalanx of the thumb and is innervated by the deep branch of the ulnar nerve. The AP functions to adduct the thumb and aids in thumb opposition.
Short Muscles of the Fifth Digit
Abductor Digiti Minimi.
The ADM arises from the pisiform bone and the tendon of the FCU. It inserts on the ulnar aspect of the base of the proximal phalanx of the fifth digit, together with the flexor digiti minimi (FDM) brevis. It is innervated by the deep branch of the ulnar nerve and functions to abduct the fifth digit.
Flexor Digiti Minimi.
The FDM originates from the flexor retinaculum and the hook of the hamate bone. It inserts on the ulnar aspect of the base of the proximal phalanx of the fifth digit, together with the ADM. It is innervated by the deep branch of the ulnar nerve and functions to flex the proximal phalanx of the fifth digit. Deep branches of the ulnar artery and nerve enter the thenar muscles mass and course into the deep region of the hand by passing between the ADM and the FDM.
Opponens Digiti Minimi (ODM)
The ODM arises from the flexor retinaculum and the hook of the hamate bone and inserts on the ulnar border of the shaft of the fifth metacarpal bone. It is innervated by the deep branch of the ulnar nerve and functions to provide a small amount of flexion and external rotation of the fifth digit.
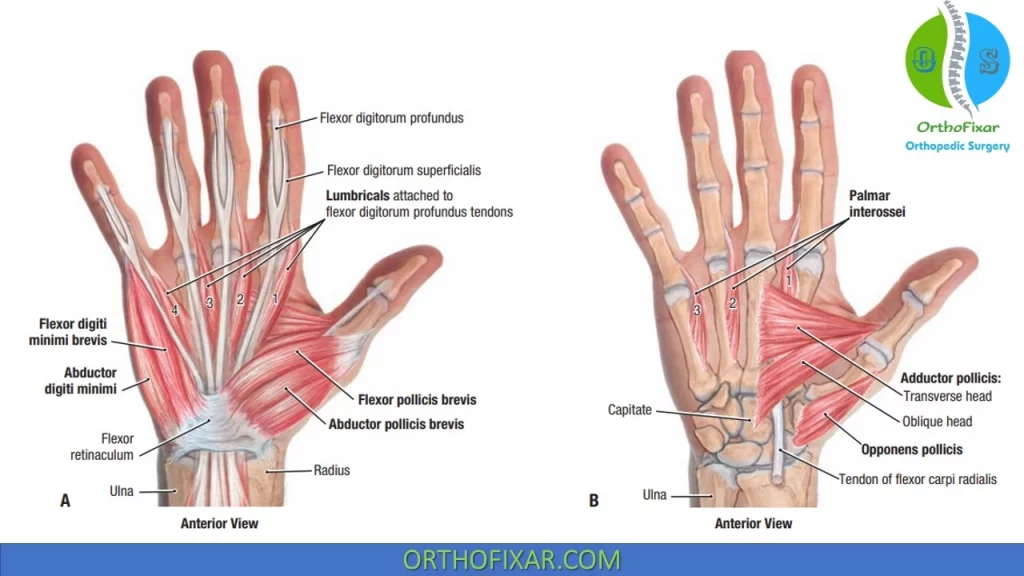
Interosseous Muscles of the Hand
The interossei muscles of the hand are divided by anatomy and function into anterior (palmar) and posterior (dorsal) interossei.
Palmar Interossei Muscles:
The three Palmar Interossei Muscles have a variety of origins and insertions:
- The first interosseus originates from the ulnar surface of the second metacarpal bone and inserts on the ulnar side of the proximal phalanx of the second digit.
- The second anterior (palmar) interosseus arises from the radial side of the fourth metacarpal bone and inserts into the radial side of the proximal phalanx of the fourth digit.
- The third anterior (palmar) interosseus originates from the radial side of the fifth metacarpal bone and inserts into the radial side of the proximal phalanx of the fifth digit.
The anterior (palmar) interossei are innervated by the deep branch of the ulnar nerve, and each muscle functions to adduct the digit to which it is attached toward the middle digit. The anterior (palmar) interossei also function to extend the distal and then the middle phalanges.
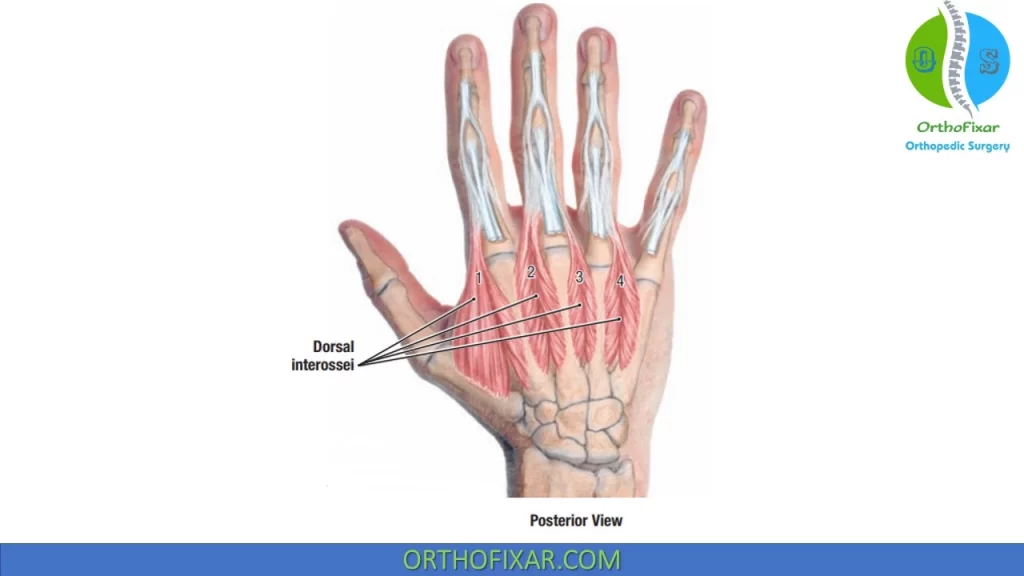
Dorsal Interossei Muscles:
The four Dorsal Interossei Muscles have a similar varied origin and insertion as their anterior (palmar) counterparts. The posterior (dorsal) interossei originate via two heads from adjacent sides of the metacarpal bones.
- The first posterior(dorsal) interosseus muscle inserts into the radial side of the proximal phalanx of the second digit.
- The second inserts into the radial side of the proximal phalanx of the third digit.
- The third inserts into the ulnar side of the proximal phalanx of the third digit and the fourth inserts into the ulnar side of the proximal phalanx of the fourth digit.
The posterior (dorsal)interossei receive their innervation from the deep branch of the ulnar nerve. The posterior (dorsal) interossei abduct the index, middle, and ring fingers from the midline of the hand.
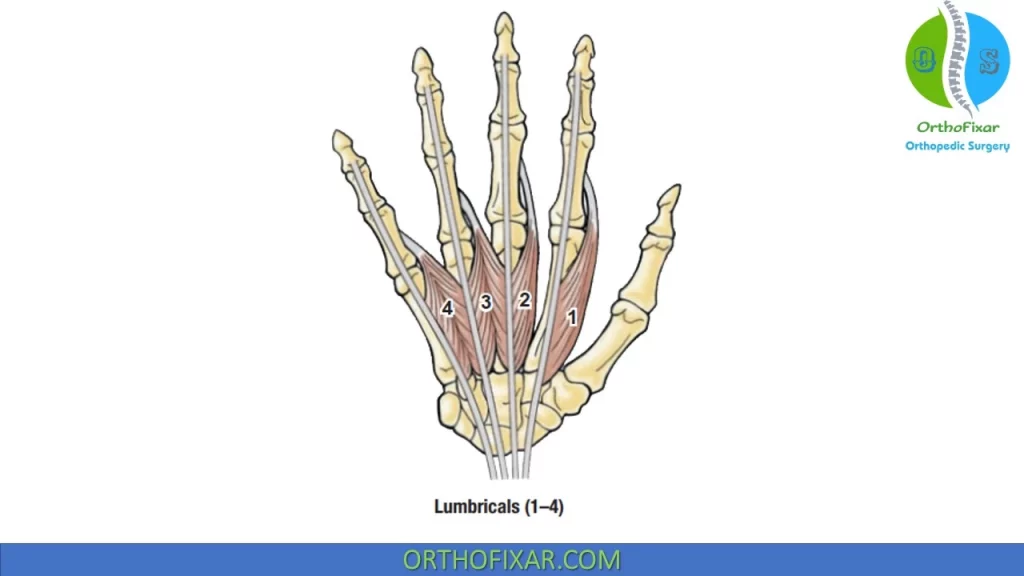
Lumbricals
The lumbrical muscles are usually four small intrinsic muscles of the hand that originate from the FDP tendons and insert into the posterior (dorsal) hood apparatus. Occasionally, more than four lumbricals are found in one hand. During contraction, they pull the FDP tendons distally, thus possessing the unique ability to relax their own antagonist.
They function to perform the motion of IP joint extension with the MCP joint held in extension and can assist in MCP flexion. The lumbrical muscles also serve an important role in the proprioception of the hand, providing feedback about the position and movement of the hand and finger joints. In instances of lumbrical spasm or contracture, attempts to flex the fingers via the profundus result in transmission of force through the lumbricals into the extensor apparatus, producing extension rather than flexion.
A lumbrical plus deformity occurs if there is excessive lumbrical force or if there is imbalance of opposing forces, which produces exaggerated lumbrical action (i.e., MCP joint flexion and IP joint extension).
The lumbricals have dual innervation:
- Lumbricals I and II are innervated typically by the median nerve,
- the third and fourth lumbricals are innervated by the ulnar nerve.
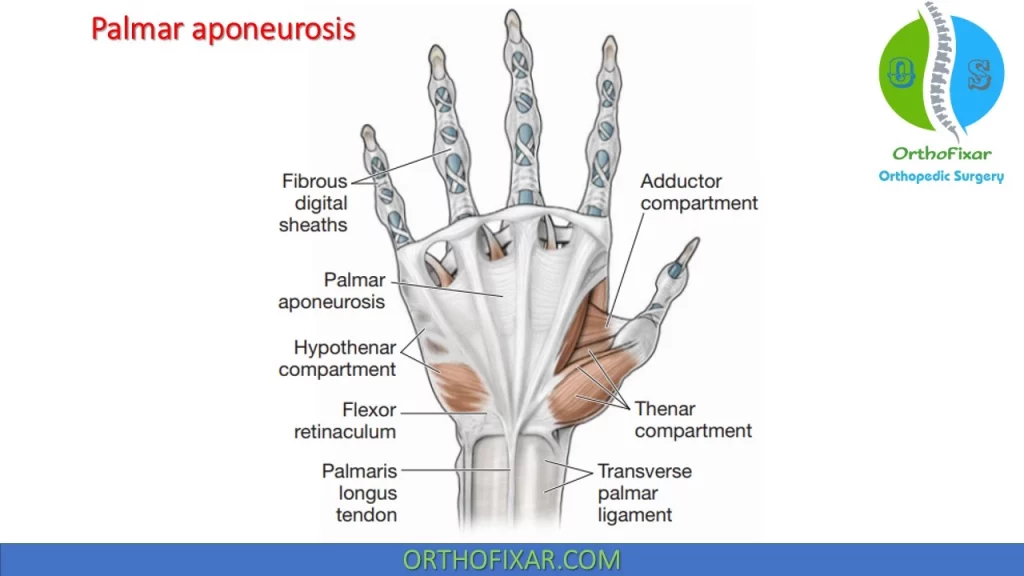
Palmar Aponeurosis
The anterior (palmar) aponeurosis, which consists of a dense fibrous structure continuous with the palmaris longus tendon and fascia covering the thenar and hypothenar muscles, is located just deep to the subcutaneous tissue. The aponeurosis travels distally to attach to the transverse metacarpal ligaments and flexor tendon sheaths.
The aponeurosis offers some protection for the ulnar artery and nerve, and digital vessels and nerves. From the central region of the palm, the aponeurosis continues toward the fingers and splits into four slips.
Dupuytren contracture is a fibrotic condition of the anterior (palmar) aponeurosis that results in nodule formation or scarring of the aponeurosis and which may ultimately cause finger flexion contractures.
See Also: Dupuytren contracture
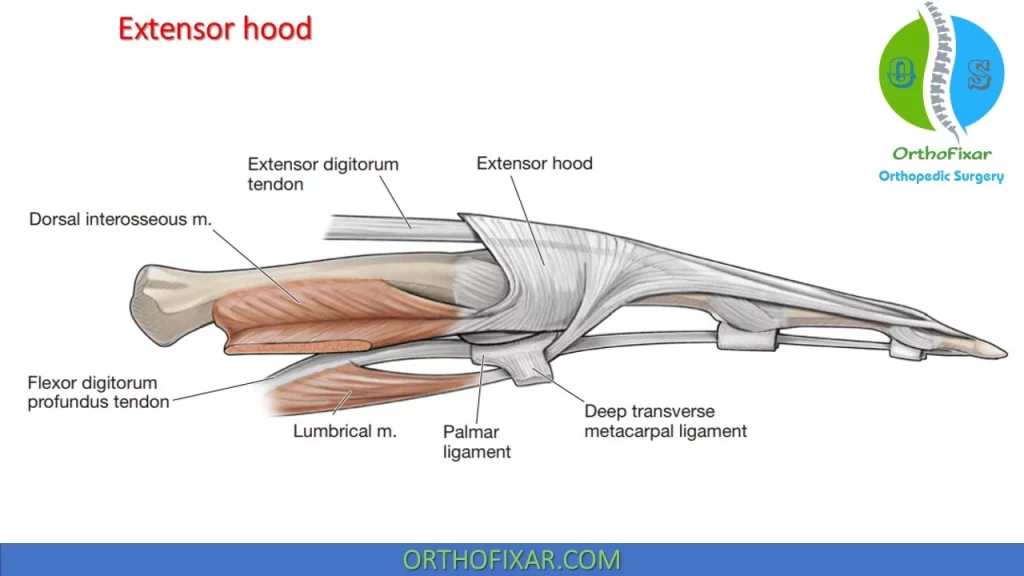
Extensor Hood
At the level of the MCP joint, the tendon of the ED fans out to cover the posterior (dorsal) aspect of the joint in a hood-like structure. A complex tendon that covers the posterior (dorsal) aspect of the digits is formed from a combination of the tendons of insertion from the ED, EI, and EDM. The distal portion of the hood receives the tendons of the lumbricals and interossei over the proximal phalanx.
The tendons of the intrinsic muscles pass anterior (palmar) to the MCP joint axes but posterior (dorsal) to the PIP and DIP joint axes.
Between the MCP and the PIP joints, the complete, complex ED tendon (after all contributions have been received) splits into three parts: a central slip and two lateral bands:
- A central band: This band inserts into the proximal posterior (dorsal) edge of the middle phalanx.
- The lateral bands: These bands rejoin over the middle phalanx into a terminal tendon, which inserts into the proximal posterior (dorsal) edge of the distal phalanx. Rupture of the tendon insertion into the distal phalanx produces a “mallet finger”. The lateral bands, comprise fibers from both extrinsic and intrinsic tendons, are prevented from dislocating posteriorly dorsally) by the transverse retinacular ligaments, which link them to the volar plates of the PIP joints.
The arrangement of the hand muscles and tendons in this expansion hood creates a cable-like system that provides a mechanism for extending the MCP and IP joints and allows the lumbrical and possibly interosseous muscles to assist in the flexion of the MCP joints. Stretching or laxity of these supporting structures allows of the lateral bands, which transmit excessive bowstringing extension force to the PIP joint.
The oblique retinacular ligament (Landsmeer ligament) assists in the extensor hood mechanism. The ligament attaches between the PIP volar plate, where it is anterior (palmar) to the PIP joint axis, and the terminal tendon, where it is posterior (dorsal) to the DIP joint axis. This relationship to the PIP and DIP joints is essentially the same as that of the intrinsic muscles (lumbricals and interosseous) to the MCP and PIP joints: when the PIP joint extends, the oblique retinacular ligament exerts a passive extensor force on the DIP joint, and when the PIP joint flexes, it allows the DIP joint to flex.
PIP joint position also may influence DIP joint position through lateral band action. The lateral bands normally slip palmarly upon PIP joint flexion, decreasing the excursion required for full DIP joint flexion. If scar tissue tethers the lateral bands so that they do not move palmarly, then simultaneous full flexion at both the PIP and the DIP joints is not possible.
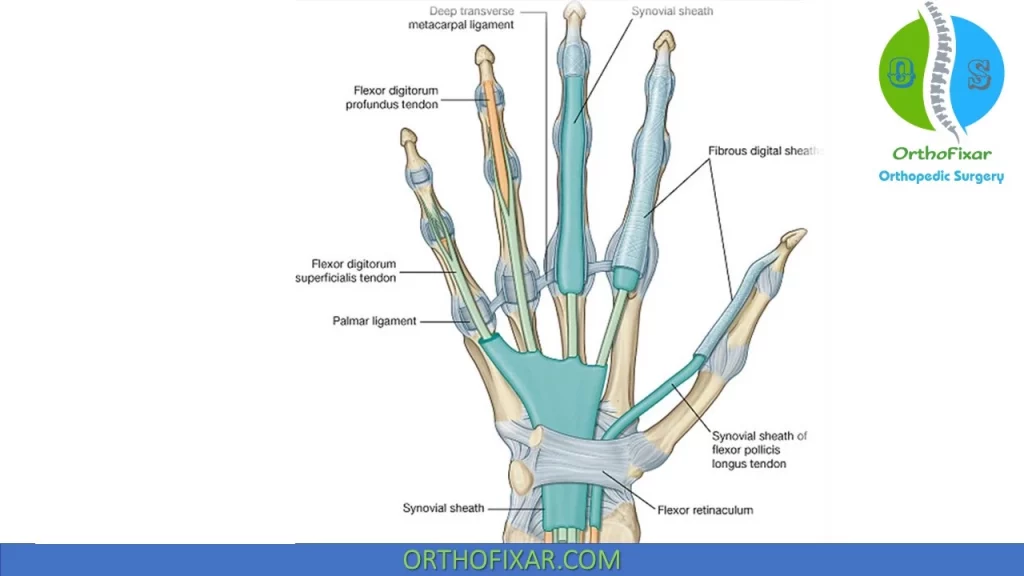
Synovial Sheaths
Synovial sheaths can be thought of as long narrow balloons filled with synovial fluid, which wrap around a tendon so that one part of the balloon wall (visceral layer) is directly on the tendon, while the other part of the balloon wall (parietal layer) is separate. During wrist motions, the sheaths move longitudinally, reducing friction.
At the wrist, the tendons of both the FDS and the FDP are essentially covered by a synovial sheath and pass posterior (dorsal) (deep) to the flexor retinaculum. The FDP tendons are posterior (dorsal) to those of the FDS. In the palm, the FDS and FDP tendons are covered for a variable distance by a synovial sheath.
At the base of the digits, both sets of tendons enter a formed by the bones of the digit “bro-osseous tunnel fi” (head of the metatarsals and phalanges) and a fibrous digital tendon sheath on the anterior (palmar) surface of the digits.
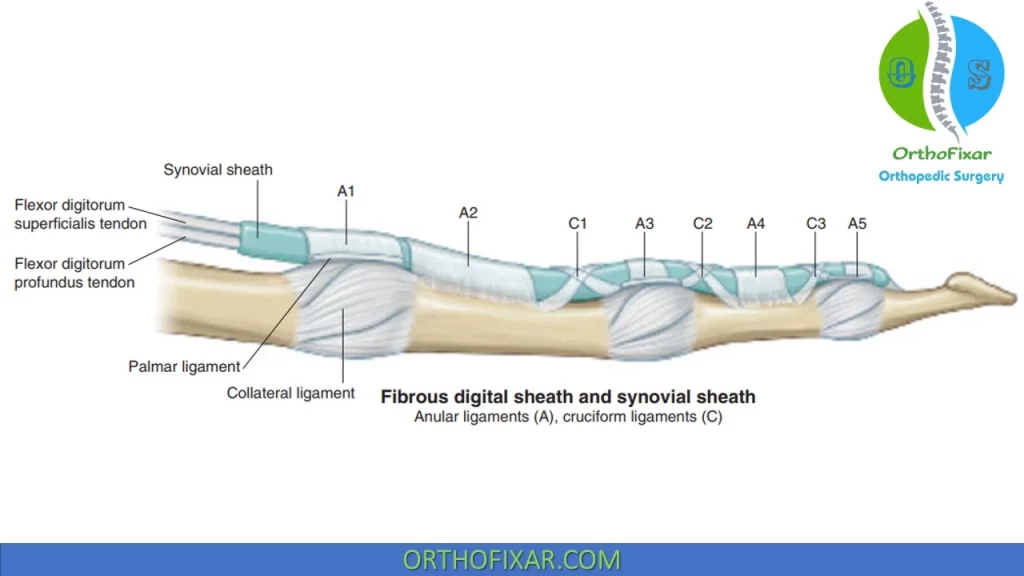
Flexor Pulleys
Annular (A) and cruciate (C) pulleys restrain the flexor tendons to the metacarpals and phalanges and contribute to fibro-osseous tunnels through which the tendons travel:
- The A1 pulley arises from the MCP joint and volar plate;
- A2 from the proximal phalanx;
- A3 from the PIP joint volar plate;
- A4 from the middle phalanx;
- A5 from the DIP joint volar plate.
The C1 pulley originates near the head of the proximal phalanx; C2 near the base of the middle phalanx; and C3 near the head of the middle phalanx.
The pulley system of the thumb includes the A1 arising from the MCP joint anterior (palmar) plate, A2 from the IP joint anterior (palmar) plate, and the oblique pulley from the proximal phalanx.
Anatomic Snuffbox
The anatomic snuffbox is a depression on the posterior (dorsal) surface of the hand at the base of the thumb, just distal to the radius. This structure can be observed during active radial abduction of the thumb.
The radial border of the Anatomic Snuffbox is formed by the tendons of the APL and EPB, while the ulnar border is formed by the tendon of the EPL. Along the floor of the Anatomic Snuffbox are the deep branch of the radial artery and the tendinous insertion of the ECRL. Underneath these structures, the scaphoid and trapezium bones are found.
Tenderness with palpation in the anatomic snuffbox suggests a scaphoid fracture but also can be present in minor wrist injuries or other conditions.

References
- Gray H: Gray’s Anatomy. Philadelphia, PA: Lea & Febiger, 1995.
- Wadsworth CT: Anatomy of the Hand and Wrist, Manual Examination and Treatment of the Spine and Extremities. Baltimore, MD: Williams & Wilkins Co, 1988:128–138
- Freiberg A, Pollard BA, Macdonald MR, Duncan MJ. Management of proximal interphalangeal joint injuries. Hand Clin. 2006 Aug;22(3):235-42. doi: 10.1016/j.hcl.2006.05.003. PMID: 16843790.
- Tubiana R, Thomine J-M, Mackin E: Examination of the Hand and Wrist. London: Mosby, 1996.
- Kuczynski K. The proximal interphalangeal joint. Anatomy and causes of stiffness in the fingers. J Bone Joint Surg Br. 1968 Aug;50(3):656-63. PMID: 5726917.
- Bowers WH, Wolf JW Jr, Nehil JL, Bittinger S. The proximal interphalangeal joint volar plate. I. An anatomical and biomechanical study. J Hand Surg Am. 1980 Jan;5(1):79-88. doi: 10.1016/s0363-5023(80)80049-9. PMID: 7365222.
- Zancolli E: Structural and Dynamic Basis of Hand Surgery, 3rd ed. Philadelphia, PA: JB Lippincott, 1979.
- Wadsworth C: Wrist and hand. In: Wadsworth C, ed. Current Concepts of Orthopedic Physical Therapy – Home Study Course. La Crosse, WI: Orthopaedic Section, APTA, 2001
- Lifetime product updates
- Install on one device
- Lifetime product support
- Lifetime product updates
- Install on one device
- Lifetime product support
- Lifetime product updates
- Install on one device
- Lifetime product support
- Lifetime product updates
- Install on one device
- Lifetime product support