Abstract
Purpose of Review
The aim of this review is to determine the efficacy of laser treatment in overactive bladder (OAB) syndrome in women.
Recent Findings
In international literature, there are few studies focusing on OAB symptoms. The proposed treatments included thulium laser, fractional CO2 laser and Erbium:YAG laser.
Summary
Although the analysed studies are not RCTs, the results show the efficacy of laser treatment in OAB symptoms, also compared to conventional medical and surgical treatments. However, these tests must be implemented with RCTs and with large patient samples.


Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. 2010;29:4–20. https://doi.org/10.1002/nau.20798.
Irwin DE, Milsom I, Hunskaar S, Reilly K, Kopp Z, Herschorn S, et al. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol. 2006;50:1306–15. https://doi.org/10.1016/j.eururo.2006.09.019.
Steward WF, Van Rooyen JB, CundiffGW AP, Herzog AR, Corey R, et al. Prevalence and burden of overactive bladder in the United States. World J Urol. 2003;20:327–36. https://doi.org/10.1007/s00345-002-0301-4.
White N, Iglesia CB. Overactive Bladder. Obstet Gynecol Clin N Am. 2016;43:59–68. https://doi.org/10.1016/j.ogc.2015.10.002.
Abrams P, Kelleher CJ, Kerr LA, Rogers RG. Overactive bladder significantly affects quality of life. Am J Manag Care. 2000;6:S580–90.
Nystrom E, Sjostrom M, Stenlund H, Samuelsson E. ICIQ symptom and quality of life instruments measure clinically relevant improvements in women with stress urinary incontinence. Neurourol Urodyn. 2014;34:747–51. https://doi.org/10.1002/nau.22657.
Thüroff JW, Abrams P, Andersson KE, Artibani W, Chapple CR, Drake MJ, et al. EAU Guidelines on Urinary Incontinence. Eur Urol. 2011;59:387–400. https://doi.org/10.1016/j.eururo.2010.11.021.
• Chapple CR, Khullar V, Gabriel Z, Muston D, Bitoun CE, Weinstein D. The effects of antimuscarinic treatments in overactive bladder: an update of a systematic review and meta-analysis. Eur Urol. 2008;54:543–62. https://doi.org/10.1016/j.eururo.2008.06.047Review and meta-analysis on the main available medical therapy for OAB.
Liang CC, Hsieh WC, Huang L. Outcome of coexistent overactive bladder symptoms in women with urodynamic urinary incontinence following anti-incontinence surgery. Int Urogynecol J. 2016;28:605–11. https://doi.org/10.1007/s00192-016-3153-y.
Athanasiou S, Grigoriadis T, Giannoulis G, Protopapas A, Antsaklis A. Midurethral slings for women with urodynamicmixed incontinence: what to expect? Int Urogynecol J. 2013;24:393–9. https://doi.org/10.1007/s00192-012-1859-z.
Jain P, Jirschele K, Botros SM, Latthe PM. Effectiveness of midurethral slings in mixed urinary incontinence: a systematic review and meta-analysis. Int Urogynecol J. 2011;22:923–32. https://doi.org/10.1007/s00192-011-1406-3.
Lin YH, Hsieh WC, Huang L, Liang CC. Effect of non-ablative laser treatment on overactive bladder symptoms, urinary incontinence and sexual function in women with urodynamic stress incontinence. Taiwan J Obstet Gynecol. 2017;56:815–20. https://doi.org/10.1016/j.tjog.2017.10.020.
•• Perino A, Cucinella G, Gugliotta G, Saitta S, Polito S, Adile B, et al. Is vaginal fractional CO2 laser treatment effective in improving overactive bladder symptoms in post-menopausal patients? Preliminary results. Eur Rev Med Pharmacol Sci. 2016;20:2491–7 One of the first trials on the application of laser CO 2for OAB symptoms.
Ogrinc UB, Senčar S, Lenasi H. Novel minimally invasive laser treatment of urinary incontinence in women. Lasers Surg Med. 2015;47:689–97. https://doi.org/10.1002/lsm.22416.
•• Athanasiou S, Pitsouni E, Grigoriadis T, Zacharakis D, Falagas ME, Salvatore S, et al. Microablative fractional CO2 laser for the genitourinary syndrome of menopause: up to 12-month results. Menopause. 2019;26:248–55. https://doi.org/10.1097/GME.0000000000001206This is the most trial on efficacy of laser CO 2for the genitourinary syndrome of menopause.
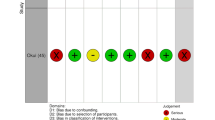
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA Statement. Int J Surg. 2010;8:336–41. https://doi.org/10.1016/j.ijsu.2010.02.007.
Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.handbook.cochrane.org.
Okui N. Comparison between erbium-doped yttrium aluminum garnet laser therapy and sling procedures in the treatment of stress and mixed urinary incontinence. World J Urol. 2019;37:885–9. https://doi.org/10.1007/s00345-018-2445-x.
•• Okui N. Efficacy and safety of non-ablative vaginal erbium:YAG laser treatment as a novel surgical treatment for overactive bladder syndrome: comparison with anticholinergics and β3-adrenoceptor agonists. World J Urol. 2019. https://doi.org/10.1007/s00345-019-02644-7This trial compared erbium:YAG laser treatment vs standard medical therapy.
Tovar-Huamani J, Mercado-Olivares F, Grandez-Urbina JA, Pichardo-Rodriguez R, Tovar-Huamani M, García-Perdomo H. Efficacy of fractional CO2 laser in the treatment of genitourinary syndrome of menopause in Latin American Population: First Peruvian experience. Lasers Surg Med. 2019;51:509–15. https://doi.org/10.1002/lsm.23066.
Athanasiou S, Pitsouni E, Antonopoulou S, Zacharakis D, Salvatore S, Falagas ME, et al. The effect of microablative fractional CO2 laser on vaginal flora of postmenopausal women. Climacteric. 2016;19:512–8. https://doi.org/10.1080/13697137.2016.1212006.
Pitsouni E, Grigoriadis T, Tsiveleka A, Zacharakis D, Salvatore S, Athanasiou S. Microablative fractional CO2-laser therapy and the genitourinary syndrome of menopause: an observational study. Maturitas. 2016;94:131-136. https://doi.org/10.1016/j.maturitas.2016.09.012
Pitsouni E, Grigoriadis T, Falagas ME, Salvatore S, Athanasiou S. Laser therapy for the genitourinary syndrome of menopause. A systematic review and meta-analysis. Maturitas. 2017;103:78–88. https://doi.org/10.1016/j.maturitas.2017.06.029.
Salvatore S, Nappi RE, Parma M, Chionna R, Lagona F, Zerbinati N, et al. Sexual function after fractional microablative CO2 laser in women with vulvovaginal atrophy. Climateric. 2015;18:219–25. https://doi.org/10.3109/13697137.2014.975197.
Perino A, Calligaro A, Forlani F, Tiberio C, Cucinella G, Svelato A, et al. Vulvo-vaginal atrophy: a new treatment modality using thermo-ablative fractional CO2 laser. Maturitas. 2015;80:296–301. https://doi.org/10.1016/j.maturitas.2014.12.006.
•• Flint R, Cardozo L, Grigoriadis Rantell TA, Pitsouni E, Athanasiou S. Rationale and design for fractional microablative CO2 laser versus photothermal non-ablative erbium:YAG laser for the management of genitourinary syndrome of menopause: a non-inferiority, single-blind randomized controlled trial. Climacteric. 2019;22:307–11. https://doi.org/10.1080/13697137.2018This trial compared CO2 laser and erbium:YAG laser for genitourinary syndrome of menopause.
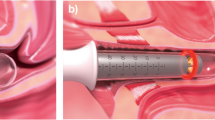
Gaspar A, Maestri S, Silva J, Brandi H, Luque D, Koron N, Vižintin Z. Intraurethral Erbium: YAG laser for the management of urinary symptoms of genitourinary syndrome of menopause: A pilot study. Lasers in surgery and medicine. 2018;50:802-807. https://doi.org/10.1002/lsm.22826
Gaspar A, Brandi H, Gomez V, Luque D. Efficacy of Erbium:YAG laser treatment compared to topical estriol treatment for symptoms of genitourinary syndrome of menopause. Lasers Surg Med. 2016;49:160–16. https://doi.org/10.1002/lsm.22569.
Drnovsek-Olup B, Beltram M, Pizem J. Repetitive Er:YAG laser irradiation of human skin: A histological evaluation. Lasers Surg Med. 2004;35:146–51. https://doi.org/10.1002/lsm.20080.
Tadir Y, Gaspar A, Lev-Sagie A, Alexiades M, Alinsod R, Bader A, et al. Light and energy based therapeutics for genitourinary syndrome of menopause: Consensus and controversies. Laser Surg Med. 2017;49:137–59. https://doi.org/10.1002/lsm.22637.
Salvatore S, Nappi RE, Zerbinati N, Calligaro A, Ferrero S, Origoni M, et al. A 12-week treatment with fractional CO2 laser for vulvovaginal atrophy: a pilot study. Climacteric. 2014;17:363–9. https://doi.org/10.3109/13697137.2014.899347.
• Behnia-Willison F, Sarraf S, Miller J, Mohamadi B, Care AS, Lam A, et al. Safety and long-term efficacy of fractional CO2 laser treatment in women suffering from genitourinary syndrome of menopause. Eur J Obstet Gynecol Reprod Biol. 2017;213:39–44. https://doi.org/10.1016/j.ejogrb.2017.03.036This trial reported data on long-term efficacy of CO 2laser for genitourinary syndrome of menopause.
Gaspar A, Addamo G, Brandi H. Vaginal fractional CO2 laser: a minimally invasive option for vaginal rejuvenation. Am J Cosmet Surg. 2011;28:156–62. https://doi.org/10.1177/074880681102800309.
Gandhi J, Chen A, Dagur G, Suh Y, Smith N, Cali B, et al. Genitourinary syndrome of menopause: an overview of clinical manifestations, pathophysiology, etiology, evaluation, and management. Am J Obstet Gynecol. 2016:704–11. https://doi.org/10.1016/j.ajog.2016.07.045.
Abrams P, Andersson KE, Buccafusco JJ, Chapple C, de Groat WC, Fryer AD, et al. Muscarinic receptors: their distribution and function in body systems, and the implications for treating overactive bladder. Br J Pharm. 2006;148:565–78. https://doi.org/10.1038/sj.bjp.0706780.
Benner JS, Nichol MB, Rovner ES, Jumadilova Z, Alvir J, Hussein M, et al. Patient-reported reasons for discontinuing overactive bladder medication. BJU Int. 2010;105:1276–82. https://doi.org/10.1111/j.1464-410X.2009.09036.x.
Kumar V, Templeman L, Chapple CR, Chess-Williams R. Recent developments in the management of detrusor overactivity. Curr Opin Urol. 2003;13:285–91. https://doi.org/10.1097/01.mou.0000079412.62186.66.
Duthie JB, Vincent M, Herbison GP, Wilson DI, Wilson D. Botulinum toxin injections for adults with overactive bladder syndrome. Cochrane Database Syst Rev. 2011;7:CD005493. https://doi.org/10.1002/14651858.CD005493.pub3.
Adile B, Speciale P, Gugliotta G, Consiglio P, Manzone M, Adile G, et al. Efficacy and acceptance of the sacral neuromodulation in the treatment of female lower urinary tract dysfunctions. Minerva Ginecol. 2018;70:236–8. https://doi.org/10.23736/S0026-4784.17.04135-1.
McGuire EJ, Fitzpatrick CC, WanJ BD, Sanvordenker J, Ritchey M, et al. Clinical assessment of urethral sphincter function. J Urol. 1993;150:1452–4. https://doi.org/10.1016/s0022-5347(17)35806-8.
Smith P. Estrogens and the urogenital tract. Studies on steroid hormone receptors and a clinical study on a new estradiol-releasing vaginal ring. Acta Obstet Gynecol Scand. 1993;157:1–25.
Falconer C, Ekman-Ordeberg G, Ulmsten U, Westergren-Thorsson G, Barchan K, Malmstrom A. Changes in paraurethral connective tissue at menopause are counteracted by estrogen. Maturitas. 1996;24:197–204.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Gloria Calagna, Marianna Maranto, Ognibene Emanuela, Salvatore Polito, Pasquale De Franciscis, Roberta Granese and Gaspare Cucinella declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Overactive Bladder
Rights and permissions
About this article
Cite this article
Calagna, G., Maranto, M., Ognibene, E. et al. Is Vaginal Laser Effective for Overactive Bladder? Results of a Systematic Review. Curr Bladder Dysfunct Rep 14, 308–317 (2019). https://doi.org/10.1007/s11884-019-00535-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11884-019-00535-6