Abstract
Background
The CHA2DS2-VASC score is used to assess the risk of cerebrovascular accident (CVA) in patients with atrial fibrillation (AF) or atrial flutter (AFL).
Objectives
We aimed to determine whether this score can determine the risk of CVA during the first year after hospitalization, in patients without known AF/AFL.
Design
Single-center retrospective cohort.
Patients
We included all patients aged ≥ 50 who were hospitalized between January 1, 2008, and December 31, 2018, to the internal medicine departments at the Chaim Sheba Medical Center, Israel. Exclusion criteria included history or new diagnosis of CVA, TIA, and AF/AFL and use of anticoagulation at any time.
Main Measures
Patients were stratified into 3 groups according to their CHA2DS2-VASC score (0–1, 2, or ≥ 3). The primary outcome was hospitalization with CVA/TIA within one year of the index hospitalization.
Key Results
Of the patients, 52,206 were included in the study. CVA/TIA occurred in 0.7%, 1.3%, and 1.7% of patients with a CHA2DS2-VASC score of 0–1, 2, and ≥ 3, respectively. Compared to a CHA2DS2-VASC score of 0–1, the HR for CVA/TIA occurrence for CHA2DS2-VASC scores of 2 and ≥ 3 was 1.77 (CI 1.42, 2.22) and 2.33 (CI 1.9, 2.85), respectively (p < 0.001 for both comparisons). Each additional CHA2DS2-VASC point increased the probability for readmission with CVA/TIA within 1-year by 26% (HR 1.26, CI 1.19, 1.32, p < 0.001). Similar trends were seen in subgroup analyses by gender, age, and renal function.
Conclusions
The CHA2DS2-VASC score is a predictor for CVA/TIA during the first year after hospitalization in patients without AF. High CHA2DS2-VASC scores warrant work-up for occult AF/AFL and other risk factors for CVA/TIA.
Similar content being viewed by others
BACKGROUND
Cerebrovascular event (CVA) is the second leading cause of death worldwide with an annual mortality rate of approximately 5.5 million people, and high morbidity with up to 50% of survivors suffering from a chronic disability. CVA also incurs substantial healthcare costs due to a high readmission rate, with more than half of the patients requiring readmission within 1 year.1,2,3,4,5 Despite the continued evolution of reperfusion strategies for patients with acute ischemic stroke, effective primary prevention remains the most important goal in lowering the burden of stroke.3,4
Patients hospitalized in the internal medicine wards are usually older and have a high burden of chronic diseases, including risk factors for stroke. In the first year after hospitalization, the risk for re-hospitalization is increased, including re-hospitalizations because of acute CVA.6 These readmissions pose a significant burden to patients and to the healthcare system, as they create significant mortality and morbidity. The latter is not only important regarding well-being, but also has an important economic impact on the health system. Therefore, identifying patients discharged from the internal ward who are at increased risk for readmission with CVA/TIA is important.
The CHA2DS2-VASC score was developed to predict the risk of thromboembolic events in patients with atrial fibrillation (AF) or atrial flutter (AFL) and is a straightforward and commonly used tool for treatment decisions on primary and secondary prevention in patients with AF.5 In addition to predicting the risk for stroke, the CHA2DS2-VASC score was shown to be associated with higher readmission rates, increased mortality, length of stay, and admission costs in patients with AF.7 Some studies showed a correlation between CHA2DS2-VASC score and atherosclerosis or left atrial thrombus (LAT),8,9 raising a potential correlation of the CHA2DS2-VASC score with the risk for CVA in patients who do not have AF.
OBJECTIVE
In this study, we aimed to determine whether the CHA2DS2-VASC score can serve to assess the risk of readmission with CVA/TIA within one year, in patients discharged from the internal medicine department, who do not harbor known AF or AFL and are not treated with chronic anticoagulation (AC).
Design
A retrospective cohort study of patients hospitalized over 10 years in a single center. The study received approval from the local Helsinki committee.
Patients
We included all patients older than 50 who were admitted (index hospitalization) to any of the seven internal medicine departments at our center (the Chaim Sheba Medical Center, Tel Hashomer, Ramat-Gan, Israel) between January 1, 2008, and December 31, 2018. We did not include patients younger than 50 because the mechanism of CVA in these younger patients might be different than atherosclerosis or cardioembolic (i.e., thrombophilia, patent foramen ovale, use of contraceptives etc.). Patients with missing data, patients with a history or a new diagnosis of CVA, TIA, AF, or AFL at any time point during the index hospitalization (based on their electronic medical record diagnoses-list), patients with mechanical or bioprosthetic valve, patients who died during their index hospitalization, and patients who were treated with AC at any time point before or during the index hospitalization or were discharged with a recommendation for treatment with AC from the index hospitalization were excluded from the study. All patients included in the study had an ECG recording at admission with sinus rhythm and had no documented history of AF in their medical records.
Patients’ information was recorded via electronic medical records, including drug therapy, admission, background, and discharge diagnoses.
Main Measures
CHA2DS2-VASC score was calculated for all patients during their index hospitalization and the patients were divided into 3 groups according to a CHA2DS2-VASC score of 0–1 (low risk), 2 (medium risk), and ≥ 3 (high risk). The score was calculated based on: https://www.mdcalc.com/cha2ds2-vasc-score-atrial-fibrillation-stroke-risk5. We then identified retrospectively all patients who were re-admitted to our institution with ischemic CVA/TIA within 1 year of their index hospitalization. Patients with hemorrhagic CVA were excluded. The rate of readmission with CVA/TIA was calculated for each CHA2DS2-VASC group.
Patients’ characteristics were presented as n (%) for categorical variables, and as mean (sd) or median [IQR] for normal/non-normal distributed continuous variables. A chi-square test for trends was used for comparison of categorical variables. Analysis of variance with 1 degree of freedom was performed for comparison of normally distributed continuous variables, and Kendall rank correlation, for non-normal distribution.
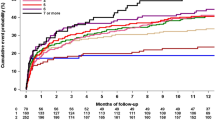
Survival curves were presented, and the Kaplan–Meier log-rank test was used to test the variable of interest on survival. Post-hoc comparisons were conducted using R::survminer package with the Benjamini–Hochberg adjustment for p-value.
Predefined subgroup analyses were performed according to gender, glomerular filtration rate (GFR) (GFR ≤ 60 ml/min/1.73m2 or > 60 ml/min/1.73m2), and age (< 75 years or ≥ 75 years).
All tests were conducted at a two-sided overall 5% significance level (aa = 0.05). All analyses were performed using R software (R Development Core Team, version 4.0.0, Vienna, Austria).
RESULTS
A total of 99,631 patients were hospitalized to the internal medicine wards between January 1, 2008, and December 31, 2018. After exclusion as detailed above, 52,206 patients were included in the final study population [Fig. 1]. Their baseline characteristics are shown in Table 1. Comparison of the baseline characteristics according to the outcome (CVA/TIA) is shown in Supplementary Table 1. The median age was 72 and 26,761 (51.4%) of the patients were men. A significant proportion of the cohort had background hypertension (16.1%), ischemic heart disease (10.6%), and/or diabetes mellitus (9.7%).
The distribution of the CHA2DS2-VASC score at the index hospitalization is shown in Fig. 2. After grouping the patients as described, there were a total of 18,411 (35.3%), 13,880 (26.6%), 19,735 (37.8%) patients with a low (0–1), medium (2), or high (≥ 3) CHA2DS2-VASC scores, respectively. The 1-year all-cause mortality rate was 13.8%, 19.2%, and 20.7% according to the CHA2DS2-VASC group (low vs. medium vs. high, respectively, p < 0.001).
Cerebrovascular Event Rate
During the first year after the index hospitalization, there were a total of 640 (1.2%) CVA/TIA cases: N = 133 (0.7%), N = 177 (1.3%), and N = 330 (1.7%) in patients with a CHA2DS2-VASC score of 0–1, 2, and ≥ 3, respectively (p for trend = 0.064). The event rate of CVA/TIA per 100 patient-years was 0.8, 1.48, and 1.96 according to the CHAD2DS2-VASC group (low risk vs. medium risk vs. high risk), respectively. The cumulative incidence of CVA/TIA according to the CHA2DS2-VASC group at 1 year follow-up is presented in the Kaplan–Meier survival analysis [Fig. 3].
Compared to a low CHA2DS2-VASC score (0–1), the HR for the occurrence of CVA/TIA for medium and high CHA2DS2-VASC score was 1.77 (CI 1.42, 2.22) and 2.33 (CI 1.9, 2.85), respectively (p < 0.001 for both comparisons). Each additional CHA2DS2-VASC point increased the probability for readmission with CVA/TIA within 1-year by 26% (HR 1.26, CI 1.19, 1.32, p < 0.001).
Subgroup Analysis
We also assessed the correlation between CHA2DS2-VASC score and CVA/TIA according to gender, renal function, and age. The number of patients in each group, the CHA2DS2-VASC scores, and rate of readmission with CVA/TIA within 1 year are detailed in Table 2.
Women and men had similar rates of CVA/TIA (1.2% in women versus 1.3% in men, p = 0.56), while patients older than 75 had a higher rate of CVA/TIA compared to younger patients (1.8% versus 0.8% respectively, p < 0.001) and patients with a low GFR had increased risk for CVA/TIA compared to higher GFR (1.6% vs 1%, respectively, p < 0.001) (Table 2). The survival analysis of CVA according to the CHA2DS2-VASC group is presented in Fig. 4; compared to the group with a low-risk score, medium- and high-risk scores correlated with the risk of CVA/TIA in all subgroups, except for patients older than 75. In patients younger than 75, only the high-risk score was significantly different than the low-risk score.
DISCUSSION
Our findings show that in patients older than 50 years old without AF, who are hospitalized in the internal medicine ward, the CHA2DS2-VASC score is associated with the risk of re-hospitalization with CVA/TIA within 1 year. This finding was consistent in patients younger than 75, regardless of gender and renal function.
Our study suggests that patients who are discharged from hospitalization in the internal medicine ward and who have a medium to high CHA2DS2-VASC score should be assessed rigorously for risk factors for CVA, i.e., occult AF, cerebral atherosclerosis, or left atrial thrombus, and treated intensively for risk factors for atherosclerosis, such as hypertension, hyperlipidemia, diabetes mellitus, and peripheral vascular disease.
Our results are in line with previous studies that showed that CHA2DS2-VASC and CHADS2 scores are associated with a higher risk of CVA/TIA in the absence of AF.10,11,12,13,14 Most of these studies had a small sample size,13 or were performed on specific populations such as patients with heart failure10 or coronary artery disease,11,12,14 thus limiting their generalizability to the general population. Saliba et al.15 demonstrated in a big community database, that the incidence of CVA/TIA in patients without AF above the age of 50 is higher with increasing CHA2DS2-VASC scores. Our study expands this data to hospitalized patients.
Subgroup analysis in our cohort showed that the risk for CVA/TIA in patients with low GFR (≤ 60 ml/min/1.73m2) was elevated compared to patients with higher GFR. This finding demonstrates the known importance of chronic kidney disease as a strong independent risk factor for CVA,16 which is highlighted in the relatively new R(2)CHADS(2) score, which was found to be superior to the CHA2DS-VASC score in predicting CVA in patients with AF and renal dysfunction.17
In the gender subgroup analysis, we found a linear relationship between the CHA2DS-VASC score and the risk for CVA/TIA in women, with the survival curve of the medium CHA2DS-VASC group more akin to the survival curve of the low CHA2DS-VASC group than that of the high CHA2DS-VASC group. In men, medium and high CHA2DS-VASC groups acted similarly [Fig. 4]. This finding indicates that the CHA2DS-VASC score may overestimate the risk for thromboembolic events that are attributed to female sex, as demonstrated previously,18,19 while in men a CHA2DS-VASC score of 2 and higher may already signify a significant risk for CVA/TIA.
Since many cryptogenic ischemic strokes are likely to have an embolic mechanism and occult AF may underlie a significant proportion of these events, thought must be given to improve detection of AF. Recently, Diederichsen et al.20 reported the low sensitivity of routine AF detection strategies compared to an implantable loop recorder for a period of 3 years, with a single 10-s ECG yielding a sensitivity of 1.5% for AF detection, increasing to only 34% for a single 30-day continuous monitoring device. Gladstone et al. showed that screening for AF in patients above the age of 75 with wearable ECG monitors increase AF detection by tenfold compared to standard practice, and lead in many instances to initiation of AC therapy.21 These findings, together with the results of our study, may justify a thorough investigation for occult AF in patients with high CHA2DS2-VASC scores, especially in the older population, by using advanced techniques such as longer monitoring of heart rhythm.
Current guidelines recommend initiation of AC treatment for primary prevention in AF patients with a CHA2DS2-VASC score of 2 or above, as this score puts them at a 2.2% risk for ischemic stroke per 100 patient-years and a 2.9% risk for stroke/TIA/peripheral emboli per 100 patient-years.22 In our study, the rate of CVA/TIA within 1 year in the high score group was 1.96%.
Limitations
Our study is a single-center study, thus limiting its generalizability. Additionally, data on patients that were re-admitted after the index hospitalization with CVA/TIA to a different institution was not available to us, as we did not have access to this data. This caveat may cause underestimation of the rate of stroke in the first year after hospitalization. Since our medical center is the largest in Israel, we can assume that the total number of these patients was relatively low and did not significantly impact our results. It is important to note that our data refer only to patients who were hospitalized and cannot be generalized to ambulatory patients. Additionally, we did not have data on the incident of new-onset AF during the first year after the index hospitalization and on the mechanism of ischemic stroke (cardioembolic vs. thrombotic or atherosclerotic).
CONCLUSION
Our study implies that the CHA2DS2-VASC score can be used to assess the risk for re-hospitalization within 1 year with CVA/TIA in patients hospitalized without AF. These results should raise the awareness of physicians and hospitalists that hospitalization for any reason should be used as an opportunity to assess the CHA2DS2-VASC score, in order to identify the risk of stroke and to assess for occult stroke culprits in patients with a medium to high CH2DS2-VASC score.
References
Donkor ES. Stroke in the 21st Century: A Snapshot of the Burden, Epidemiology, and Quality of Life. Stroke Res Treat. 2018;2018:3238165. https://doi.org/10.1155/2018/3238165
Johnson CO, Nguyen M, Roth GA, et al. Global, regional, and national burden of stroke, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2019;18(5):439-458. https://doi.org/10.1016/S1474-4422(19)30034-1
Meschia JF, Bushnell C, Boden-Albala B, et al. Guidelines for the primary prevention of stroke: A statement for healthcare professionals from the American heart association/American stroke association. Stroke. 2014;45(12):3754-3832.
Go AS, Mozaffarian D, Roger VL, et al. Heart Disease and Stroke Statistics - 2014 Update: A report from the American Heart Association. Circulation. 2014;129(3):e28-e292. https://doi.org/10.1161/01.cir.0000441139.02102.80
Crijns HJGM. Refining Clinical Risk Stratification for Predicting Stroke and Thromboembolism in Atrial Fibrillation Using a Novel Risk Factor-Based Approach American College of Chest Physicians. Chest. 2010;137(2):1-14. https://doi.org/10.1378/chest.09-1584
Brunner-La Rocca HP, Peden CJ, Soong J, Holman PA, Bogdanovskaya M, Barclay L. Reasons for readmission after hospital discharge in patients with chronic diseases- Information from an international dataset. Savarese G, ed. PLoS One. 2020;15(6 June):e0233457.
Lahewala S, Arora S, Patel P, et al. Atrial fibrillation: Utility of CHADS2 and CHA2DS2-VASc scores as predictors of readmission, mortality and resource utilization. Int J Cardiol. 2017;245:162-167.
Kim YD, Cha MJ, Kim J, et al. Increases in cerebral atherosclerosis according to CHADS2 scores in patients with stroke with nonvalvular atrial fibrillation. Stroke. 2011;42(4):930-934.
Cha MJ, Kim YD, Nam HS, Kim J, Lee DH, Heo JH. Stroke mechanism in patients with non-valvular atrial fibrillation according to the CHADS 2 and CHA 2DS 2-VASc scores. Eur J Neurol. 2012;19(3):473-479.
Melgaard L, Gorst-Rasmussen A, Lane DA, Rasmussen LH, Larsen TB, Lip GYH. Assessment of the CHA2DS2-VASc score in predicting ischemic stroke, thromboembolism, and death in patients with heart failure with and without atrial fibrillation. JAMA - J Am Med Assoc. 2015;314(10):E1-E9. https://doi.org/10.1001/jama.2015.10725
Poçi D, Hartford M, Karlsson T, Herlitz J, Edvardsson N, Caidahl K. Role of the CHADS2 score in acute coronary syndromes: Risk of subsequent death or stroke in patients with and without atrial fibrillation. Chest. 2012;141(6):1431-1440. https://doi.org/10.1378/chest.11-0435
Senoo K, Lip GYH. Prediction of stroke in patients without atrial fibrillation using the CHADS2 and CHA2DS2-VASc scores: A justification for more widespread thromboprophylaxis? Heart. 2014;100(19):1485-1486. https://doi.org/10.1136/heartjnl-2014-306161
Lip GYH, Lin HJ, Chien KL, et al. Comparative assessment of published atrial fibrillation stroke risk stratification schemes for predicting stroke, in a non-atrial fibrillation population: The Chin-Shan Community Cohort Study. Int J Cardiol. 2013;168(1):414-419. https://doi.org/10.1016/j.ijcard.2012.09.148
Welles CC, Whooley MA, Na B, Ganz P, Schiller NB, Turakhia MP. The CHADS2 score predicts ischemic stroke in the absence of atrial fibrillation among subjects with coronary heart disease: Data from the Heart and Soul Study. Am Heart J. 2011;162(3):555-561. https://doi.org/10.1016/j.ahj.2011.05.023
Saliba W, Gronich N, Barnett-Griness O, Rennert G. The role of CHADS2 and CHA2DS2-VASc scores in the prediction of stroke in individuals without atrial fibrillation: a population-based study. J Thromb Haemost. 2016;14(6):1155-1162. https://doi.org/10.1111/jth.13324
Lee M, Saver JL, Chang KH, Liao HW, Chang SC, Ovbiagele B. Low glomerular filtration rate and risk of stroke: Meta-analysis. BMJ. 2010;341(7776):767. https://doi.org/10.1136/bmj.c4249
Piccini JP, Stevens SR, Chang Y, et al. Response to letter regarding article, renal dysfunction as a predictor of stroke and systemic embolism in patients with nonvalvular atrial. Circulation. 2013;128(11):224-232. https://doi.org/10.1161/CIRCULATIONAHA.113.004013
Tomasdottir M, Friberg L, Hijazi Z, Lindbäck J, Oldgren J. Risk of ischemic stroke and utility of CHA2DS2-VASc score in women and men with atrial fibrillation. Clin Cardiol. 2019;42(10):1003-1009. https://doi.org/10.1002/clc.23257
Nielsen PB, Skjøth F, Overvad TF, Larsen TB, Lip GYH. Female sex is a risk modifier rather than a risk factor for stroke in atrial fibrillation should we use a CHA 2 DS 2 -VA Score Rather Than CHA 2 DS 2 -VASc? Circulation. 2018;137(8):832-840. https://doi.org/10.1161/CIRCULATIONAHA.117.029081
Diederichsen SZ, Haugan KJ, Kronborg C, et al. Comprehensive Evaluation of Rhythm Monitoring Strategies in Screening for Atrial Fibrillation: Insights from Patients at Risk Monitored Long Term with an Implantable Loop Recorder. Circulation. 2020;141(19):1510-1522. https://doi.org/10.1161/CIRCULATIONAHA.119.044407
Gladstone DJ, Wachter R, Schmalstieg-Bahr K, et al. Screening for Atrial Fibrillation in the Older Population: A Randomized Clinical Trial. JAMA Cardiol. 2021. https://doi.org/10.1001/jamacardio.2021.0038
Friberg L, Rosenqvist M, Lip GYH. Evaluation of risk stratification schemes for ischaemic stroke and bleeding in 182 678 patients with atrial fibrillation: The Swedish Atrial Fibrillation cohort study. Eur Heart J. 2012;33(12):1500-1510. https://doi.org/10.1093/eurheartj/ehr488
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lahad, K., Maor, E., Klempfner, R. et al. CHA2DS2-VASC Score Predicts the Risk of Stroke in Patients Hospitalized to the Internal Medicine Department Without Known Atrial Fibrillation. J GEN INTERN MED 37, 3355–3360 (2022). https://doi.org/10.1007/s11606-021-07262-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-021-07262-x