Abstract
Objectives
Clinical infection is a common complication in children with systemic lupus erythematosus (SLE). However, few studies have investigated immune alterations in children with SLE complicated with clinical infection. We assessed lymphocyte subsets in children with SLE to explore the possibility of clinical infection.
Methods
We retrospectively analyzed the proportion of peripheral lymphocyte subsets in 140 children with SLE. Children with SLE were classified into different clusters according to the proportion of peripheral blood lymphocyte subsets: (CD3 + /CD4 + T cell, CD3 + /CD8 + T cell, CD3 + /CD4 + /CD8 + T cell, CD3 + /CD4-/CD8- T cell, CD19 + B cell, and CD3-/CD16 + /CD56 + NK cell). Differences in the proportion of lymphoid subsets, infection rates, and systemic lupus erythematosus disease activity index (SLEDAI) scores were compared between clusters. In addition, we grouped the subjects according to the presence or absence of infection. Proportions of lymphoid subsets, demographic variables, clinical presentation, and other laboratory variables were compared between the infected and uninfected groups. Finally, the diagnostic ability of lymphocyte subset ratios to distinguish secondary infection in children with SLE was predicted using an ROC curve.
Results
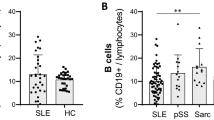
Cluster C2 had a higher proportion of B cells than Cluster C1, while Cluster C1 had a lower proportion of NK cells, CD3 + T cells, CD3 + /CD4 + T cells, CD3 + /CD8 + T cells, and CD3 + /CD4-/CD8- T cells. Infection rates and SLEDAI scores were higher in Cluster C2 than in Cluster C1. The infected children had a higher proportion of B cells and a lower proportion of CD3 + T cells, CD3 + /CD4 + T cells, CD3 + /CD8 + T cells, and CD3 + /CD4-/CD8- T cells. There were no significant differences in lymphoid subsets between children in Cluster C2 and the infected groups. The area under the ROC curve of B lymphocytes in predicting SLE children with infection was 0.842. The area under the ROC curve was 0.855 when a combination of B cells, NK cells, CD4 + T cells, and CD8 + T cells was used to predict the outcome of coinfection.
Conclusions
A high percentage of B cells and a low percentage of CD3 + T cells, CD3 + /CD4 + T cells, CD3 + /CD8 + T cells, CD3 + /CD4 + /CD8 + T cells, and CD3 + /CD4-/CD8- T cells may be associated with infection in children with SLE. B cells was used to predict the outcome of coinfection in children with SLE.
Key Points • A high percentage of B cells and a low percentage of CD3 + T cells, CD3 + /CD4 + T cells, CD3 + /CD8 + T cells, CD3 + /CD4 + /CD8 + T cells, and CD3 + /CD4-/CD8- T cells may be associated with infection in children with SLE • B cells was used to predict the outcome of coinfection in children with SLE |






Similar content being viewed by others
References
Ameer MA, Chaudhry H, Mushtaq J, Khan OS, Babar M, Hashim T, Zeb S, Tariq MA, Patlolla SR, Ali J, Hashim SN, Hashim S (2022) An Overview of Systemic Lupus Erythematosus (SLE) Pathogenesis, Classification, and Management. Cureus 14:e30330
Tucker LB, Uribe AG, Fernández M, Vilá LM, McGwin G, Apte M, Fessler BJ, Bastian HM, Reveille JD, Alarcón GS (2008) Adolescent onset of lupus results in more aggressive disease and worse outcomes: results of a nested matched case-control study within LUMINA, a multiethnic US cohort (LUMINA LVII). Lupus 17:314–322
Brunner HI, Gladman DD, Ibañez D, Urowitz MD, Silverman ED (2008) Difference in disease features between childhood-onset and adult-onset systemic lupus erythematosus. Arthritis Rheum 58:556–562
Karrar S, Cunninghame Graham DS (2018) Abnormal B cell development in systemic lupus erythematosus: what the genetics tell us. Arthritis Rheum (Hoboken, NJ) 70:496–507
Zandman-Goddard G, Shoenfeld Y (2003) SLE and infections. Clin Rev Allergy Immunol 25:29–40
Hochberg MC (1997) Updating the american college of rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 40:1725
Ministry of Health of the People's Republic of China (2001) Diagnostic criteria for Nosocomial infection (Trial). Natl Med J China 81(5):314–320
Wilkerson MD, Hayes DN (2010) ConsensusClusterPlus: a class discovery tool with confidence assessments and item tracking. Bioinformatics (Oxford, England) 26:1572–1573
Kaul A, Gordon C, Crow MK, Touma Z, Urowitz MB, van Vollenhoven R, Ruiz-Irastorza G, Hughes G (2016) Systemic lupus erythematosus. Nat Rev Dis Primers 2:16039
Hiraki LT, Feldman CH, Liu J, Alarcón GS, Fischer MA, Winkelmayer WC, Costenbader KH (2012) Prevalence, incidence, and demographics of systemic lupus erythematosus and lupus nephritis from 2000 to 2004 among children in the US Medicaid beneficiary population. Arthritis Rheum 64:2669–2676
Ocampo-Piraquive V, Nieto-Aristizábal I, Cañas CA, Tobón GJ (2018) Mortality in systemic lupus erythematosus: causes, predictors and interventions. Expert Rev Clin Immunol 14:1043–1053
Ospina FE, Echeverri A, Zambrano D, Suso JP, Martinez-Blanco J, Canas CA, Tobon GJ (2017) Distinguishing infections vs flares in patients with systemic lupus erythematosus. Rheumatology (Oxford) 56:i46–i54
Beça S, Rodríguez-Pintó I, Alba MA, Cervera R, Espinosa G (2015) Development and validation of a risk calculator to differentiate flares from infections in systemic lupus erythematosus patients with fever. Autoimmun Rev 14:586–593
Doria A, Arienti S, Rampudda M, Canova M, Tonon M, Sarzi-Puttini P (2008) Preventive strategies in systemic lupus erythematosus. Autoimmun Rev 7:192–197
Torres-Ruiz J, Mejía-Domínguez NR, Zentella-Dehesa A, Ponce-de-León A, Morales-Padilla SR, Vázquez-Rodríguez R, Alvarado-Lara MR, Reyna-de-la-Garza RA, Tapia-Rodríguez M, Juárez-Vega G, Merayo-Chalico J, Barrera-Vargas A, Alcocer-Varela JC, Gómez-Martín D (2018) The systemic lupus erythematosus infection predictive index (LIPI): a clinical-immunological tool to predict infections in lupus patients. Front Immunol 9:3144
Iwata S, Tanaka Y (2016) B-cell subsets, signaling and their roles in secretion of autoantibodies. Lupus 25:850–856
Fritzler MJ (1996) Clinical relevance of autoantibodies in systemic rheumatic diseases. Mol Biol Rep 23:133–145
Parodis I, Gatto M, Sjowall C (2022) B cells in systemic lupus erythematosus: Targets of new therapies and surveillance tools. Front Med (Lausanne) 9:952304
Du AX, Gniadecki R, Osman M (2022) Biomarkers of B cell activation in autoimmune connective tissue diseases: More than markers of disease activity. Clin Biochem 100:1–12
Wellmann U, Letz M, Herrmann M, Angermüller S, Kalden JR, Winkler TH (2005) The evolution of human anti-double-stranded DNA autoantibodies. Proc Natl Acad Sci USA 102:9258–9263
Sobel ES, Kakkanaiah VN, Kakkanaiah M, Cheek RL, Cohen PL, Eisenberg RA (1994) T-B collaboration for autoantibody production in lpr mice is cognate and MHC-restricted. J Immunol (Baltimore, Md: 1950) 152:6011–6016
Zotos D, Coquet JM, Zhang Y, Light A, D’Costa K, Kallies A, Corcoran LM, Godfrey DI, Toellner KM, Smyth MJ, Nutt SL, Tarlinton DM (2010) IL-21 regulates germinal center B cell differentiation and proliferation through a B cell-intrinsic mechanism. J Exp Med 207:365–378
Zhang X, Lindwall E, Gauthier C, Lyman J, Spencer N, Alarakhia A, Fraser A, Ing S, Chen M, Webb-Detiege T, Zakem J, Davis W, Choi YS, Quinet R (2015) Circulating CXCR5+CD4+helper T cells in systemic lupus erythematosus patients share phenotypic properties with germinal center follicular helper T cells and promote antibody production. Lupus 24:909–917
Comte D, Karampetsou MP, Yoshida N, Kis-Toth K, Kyttaris VC, Tsokos GC (2017) Signaling lymphocytic activation molecule family member 7 engagement restores defective effector CD8+ t cell function in systemic lupus erythematosus. Arthritis Rheum (Hoboken, NJ) 69:1035–1044
Chen PM, Tsokos GC (2021) T cell abnormalities in the pathogenesis of systemic lupus erythematosus: an update. Curr Rheumatol Rep 23:12
Stohl W (1995) Impaired polyclonal T cell cytolytic activity. A possible risk factor for systemic lupus erythematosus. Arthritis Rheum 38:506–516
Lu Z, Li J, Ji J, Gu Z, Da Z (2019) Altered peripheral lymphocyte subsets in untreated systemic lupus erythematosus patients with infections. Braz J Med Biol Res=Revista brasileira de pesquisas medicas e biologicas 52:e8131
Chen PM, Tsokos GC (2021) The role of CD8+ T-cell systemic lupus erythematosus pathogenesis: an update. Curr Opin Rheumatol 33:586–591
Zimmer CL, Cornillet M, Solà-Riera C, Cheung KW, Ivarsson MA, Lim MQ, Marquardt N, Leo YS, Lye DC, Klingström J, MacAry PA, Ljunggren HG, Rivino L, Björkström NK (2019) NK cells are activated and primed for skin-homing during acute dengue virus infection in humans. Nat Commun 10:3897
Laky K, Fleischacker C, Fowlkes BJ (2006) TCR and Notch signaling in CD4 and CD8 T-cell development. Immunol Rev 209:274–283
Nascimbeni M, Pol S, Saunier B (2011) Distinct CD4+ CD8+ double-positive T cells in the blood and liver of patients during chronic hepatitis B and C. PLoS One 6:e20145
Frahm MA, Picking RA, Kuruc JD, McGee KS, Gay CL, Eron JJ, Hicks CB, Tomaras GD, Ferrari G (2012) CD4+CD8+ T cells represent a significant portion of the anti-HIV T cell response to acute HIV infection. J Immunol (Baltimore, Md: 1950) 188:4289–4296
Parel Y, Chizzolini C (2004) CD4+ CD8+ double positive (DP) T cells in health and disease. Autoimmun Rev 3:215–220
Wu Y, Cai B, Feng W, Yang B, Huang Z, Zuo C, Wang L (2014) Double positive CD4+CD8+ T cells: key suppressive role in the production of autoantibodies in systemic lupus erythematosus. Indian J Med Res 140:513–519
Chang K, Na W, Liu C, Xu H, Liu Y, Wang Y, Jiang Z (2022) Peripheral CD4 (+)CD8 (+) double positive T cells: A potential marker to evaluate renal impairment susceptibility during systemic lupus erythematosus. J Biomed Res 37:59–68
Crispín JC, Oukka M, Bayliss G, Cohen RA, Van Beek CA, Stillman IE, Kyttaris VC, Juang YT, Tsokos GC (2008) Expanded double negative T cells in patients with systemic lupus erythematosus produce IL-17 and infiltrate the kidneys. J Immunol (Baltimore, Md : 1950) 181:8761–8766
Shivakumar S, Tsokos GC, Datta SK (1989) T cell receptor alpha/beta expressing double-negative (CD4-/CD8-) and CD4+ T helper cells in humans augment the production of pathogenic anti-DNA autoantibodies associated with lupus nephritis. J Immunol (Baltimore, Md : 1950) 143:103–112
Ohl K, Wiener A, Schippers A, Wagner N, Tenbrock K (2015) Interleukin-2 treatment reverses effects of cAMP-responsive element modulator alpha-over-expressing T cells in autoimmune-prone mice. Clin Exp Immunol 181:76–86
Quaglia M, Merlotti G, De Andrea M, Borgogna C, Cantaluppi V (2021) Viral infections and systemic lupus erythematosus: New Players in an Old Story. Viruses 13(2):277
Rigante D, Mazzoni MB, Esposito S (2014) The cryptic interplay between systemic lupus erythematosus and infections. Autoimmun Rev 13:96–102
Rigante D, Esposito S (2015) Infections and systemic lupus erythematosus: binding or sparring partners? Int J Mol Sci 16:17331–17343
Pan Q, Liu Z, Liao S, Ye L, Lu X, Chen X, Li Z, Li X, Xu YZ, Liu H (2019) Current mechanistic insights into the role of infection in systemic lupus erythematosus. Biomed Pharmacother = Biomedecine Pharmacotherapie 117:109122
Koyanagi N, Kawaguchi Y (2020) Evasion of the Cell-Mediated Immune Response by Alphaherpesviruses. Viruses 12(12):1354
Randall RE, Griffin DE (2017) Within host RNA virus persistence: mechanisms and consequences. Curr Opin Virol 23:35–42
Levet S, Charvet B, Bertin A, Deschaumes A, Perron H, Hober D (2019) Human endogenous retroviruses and type 1 diabetes. Curr DiabRep 19:141
Acknowledgements
This study was supported by Self-funded research projects of Guangxi Health and Family Planning Commission(Z20210246)
Funding
Self-funded research projects of Guangxi Health and Family Planning Commission (Z20210246).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yan Deng and Ying-ying Ou contributed equally to this work.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Deng, Y., Ou, Yy., Mo, CJ. et al. Characteristics and clustering analysis of peripheral blood lymphocyte subsets in children with systemic lupus erythematosus complicated with clinical infection. Clin Rheumatol 42, 3299–3309 (2023). https://doi.org/10.1007/s10067-023-06716-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10067-023-06716-3