Abstract
Background
Despite a high degree of satisfaction with laparoscopic Heller–Dor surgery (LHD) for esophageal achalasia, some cases show no improvement in postoperative esophageal clearance. We investigated whether an objective evaluation is essential for determining the therapeutic effect of LHD.
Methods
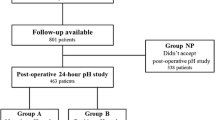
We investigated the difference in symptoms, regarding esophageal clearance, using timed barium esophagogram (TBE), in 306 esophageal achalasia patients with high postoperative satisfaction who underwent LHD. Furthermore, these patients were divided into two groups, in accordance with the difference in postoperative esophageal clearance, in order to compare the preoperative pathophysiology, symptoms, and surgical results.
Results
Although the poor postoperative esophageal clearance group (117 cases, 38%) was mostly male and the ratio of Sigmoid type was high compared to the good postoperative esophageal clearance group (p = 0.046, p = 0.001, respectively); in patients with high surgical satisfaction, there was no difference in terms of preoperative symptom scores and surgical results. However, although the satisfaction level was high in the poor esophageal clearance group, the scores in terms of the postoperative dysphagia and vomiting were high (p = 0.0018 and p = 0.004, respectively). The AUC was 0.9842 upon ROC analysis regarding the presence or absence of clearance at 2 min following postoperative TBE and the postoperative feeling of difficulty swallowing score, with a cut-off value of 2 points (sensitivity: 88%, specificity: 100%) in cases with a high degree of surgical satisfaction.
Conclusion
The esophageal clearance ability can be predicted by subjective evaluation, based on the postoperative symptom scores; so, an objective evaluation is not essential in cases with high surgical satisfaction.




Similar content being viewed by others
References
Moonen A, Boeckxstaens G (2014) Current diagnosis and management of achalasia. J Clin Gastroenterol 48:484–490
Furuzawa-Carballeda J, Torres-Landa S, Valdovinos MÁ, Coss-Adame E, Martín Del Campo LA, Torres-Villalobos G (2016) New insights into the pathophysiology of achalasia and implications for future treatment. World J Gastroenterol 22:7892–7907
Pandolfino JE, Gawron AJ (2015) Achalasia: a systematic review. JAMA 313:1841–1852
Reynolds JC, Parkman HP (1989) Achalasia. Gastroenterol Clin North Am 18:223–255
Spiess AE, Kahrilas PJ (1998) Treating achalasia: from whalebone to laparoscope. JAMA 280:638–642
Patient Care Committee Society for Surgery of the Alimentary Tract (2004) Esophageal achalasia: SSAT patient care guidelines. J Gastrointest Surg 8:367–368
Stefanidis D, Richardson W, Farrell TM, Kohn GP, Augenstein V, Fanelli RD (2012) SAGES guidelines for the surgical treatment of esophageal achalasia. Surg Endosc 26:296–311
Katada N, Sakuramoto S, Yamashita K, Shibata T, Moriya H, Kikuchi S, Watanabe M (2012) Recent trends in the management of achalasia. Ann Thorac Cardiovasc Surg 18:420–428
Zhong C, Tan S, Ren Y, Lu M, Peng Y, Fu X, Tang X (2020) Quality of life following peroral endoscopic myotomy for esophageal achalasia: a systematic review and meta-analysis. Ann Thorac Cardiovasc Surg 26:113–124
Doubova M, Gowing S, Robaidi H, Gilbert S, Maziak DE, Shamji F, Sundaresan S, Villeneuve PJ, Seely AJE (2020) Long-term symptom control following laparoscopic Heller and Dor fundoplication for achalasia. Ann Thorac Surg. https://doi.org/10.1016/j.athoracsur.2020.06.095,Sep3,2020
Schlottmann F, Luckett DJ, Fine J, Shaheen NJ, Patti MG (2018) Laparoscopic Heller myotomy versus peroral endoscopic myotomy (POEM) for achalasia: a systemic review and meta-analysis. Ann Surg 267:451–460
Kostic SV, Rice TW, Baker ME, Decamp MM, Murthy SC, Rybicki LA, Blackstone EH, Richter JE (2000) Timed barium esophagogram: a simple physiologic assessment of achalasia. J thorac Cardiovasc Surg 120:935–943
Neyaz Z, Gupta M, Ghoshal UC (2013) How to perform and interpret timed barium esophagogram. J Neurogastroenterol Motil 19:251–256
Tsuboi K, Omura N, Yano F, Kashiwagi H, Yanaga, (2009) Results after laparoscopic Heller-Dor operation for esophageal achalasia in 100 consecutive patients. Dis Esophagus 22:169–176
Patti MG, Molena D, Fisichella PM, Whang K, Yamada H, Perretta S, Way LW (2001) Laparoscopic Heller myotomy and Dor fundoplication for achalasia: analysis of success and failures. Arch Surg 136:870–877
Balm ME, Delfyett W, Levine MS, Metz DC, Katzka DA (2002) Achalasia: a disease of varied and sbtle symptoms that do not corelate with radiographic findings. Am J Gastroenterol 97:1916–1923
Nicodeme F, de Ruigh A, Xiao Y, Rajeswaran S, Teitelbaum EN, Hungness ES, Kahrilas PJ, Pandolfino JE (2013) A comparison of symptom severity and bolus retention with Chicago classification esophageal pressure topography metrics in patients with achalasia. Clin Gastroenterol Hepatol 11:131–137
Carlson DA, Beveridge CA, Lin Z, Balla M, Gregory D, Tye M, Ritter K, Kahrilas PJ, Pandolfino JE (2018) Improved assessment of bolus clearance in patients with achalasia using high-resolution impedance manometry. Clin Gastroenterol Hepatol 16:672–680
de Olivaira JM, Birgisson S, Doinoff C, Einstein D, Herts B, Davros W, Obuchowski N, Koehler RE, Richter J, Baker ME (1997) Timed barium swallow: a simple technique for evaluating esophageal emptying in patients with achalasia. AJR Am J Roentgenol 169:473–479
Kahrilas PJ, Bredenoord AJ, Fox M, Gyawali CP, Roman S, Smout AJ, Pandolfino JE; International High Resolution Manometry Working Group (2015) The Chicago classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil 27:160–174
Japan esophageal society 2017 Descriptive Rules for Achalasia of the Esophagus, June 2012: 4th edition. Esophagus 14:275–289
Tsuboi K, Omura N, Yano F, Hoshino M, Yamamoto SR, Akimoto S, Masuda T, Kashiwagi H, Yanaga K (2020) Therapeutic efficacy of laparoscopic Helle-Dor surgery for chest pain in patients with achalasia: a single institutional experience. Esophagus 17:197–207
Tsuboi K, Omura N, Yano F, Hoshino M, Yamamoto SR, Akimoto S, Masuda T, Kashiwagi H, Yanaga K (2017) Impact of esophageal flexion level on the surgical outcome in patients with sigmoid esophageal achalasia. Surg Today 47:1339–1346
Omura N, Kashiwagi H, Tsuboi K, Ishibashi Y, Kawasaki N, Yano F, Suzuki Y, Yanaga K (2006) Therapeutic effects of a laparoscopic Heller myotomy and Dor fundoplication of the chest pain associated with achalasia. Surg Today 36:235–240
Vaezi MF, Pandlfino JE, Vela MF (2013) ACG clinical guideline: diagnosis and management of achalasia. Am J Gastroenterol 108:1238–1249
Vaezi MF, Baker ME, Achkar E, Richter JE (2002) Timed barium oesophagram: better predictor of long term success after pneumatic dilation in achalasia than symptom assessment. Gut 50:765–770
Sadowski DC, Ackah F, Jiang B, Svenson LW (2010) Achalasia: incidence, prevalence and survival: a population-based study. Neurogastroenterol Motil 22:e256–e261
Acknowledgements
None
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Tsuboi, Yano, Omura, Hoshino, Yamanoto, Akimoto, Masuda, Sakashita, Fukushima, and Ikegami have no conflicts of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tsuboi, K., Yano, F., Omura, N. et al. Is an objective evaluation essential for determining the therapeutic effect of laparoscopic surgery among patients with esophageal achalasia?. Surg Endosc 36, 3932–3939 (2022). https://doi.org/10.1007/s00464-021-08712-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08712-7