Abstract
Objectives
To clarify which parameters are associated with unsuccessful pessary fitting for pelvic organ prolapse (POP) at up to 3 months follow-up.
Methods
Embase, PubMed and Cochrane CENTRAL library were searched in May 2020. Inclusion criteria were: (1) pessary fitting attempted in women with symptomatic POP; (2) pessary fitting success among the study outcomes with a maximal follow-up of 3 months; (3) baseline parameters compared between successful and unsuccessful group. A meta-analysis was performed using the random effects model.
Main results
Twenty-four studies were included in the meta-analysis. Parameters associated with unsuccessful pessary fitting were: age (OR 0.70, 95% CI 0.56–0.86); BMI (OR 1.35, 95% CI 1.08–1.70); menopause (OR 0.65 95% CI 0.47–0.88); de novo stress urinary incontinence (OR 5.59, 95% CI 2.24–13.99); prior surgery, i.e. hysterectomy (OR 1.88, 95% CI 1.48–2.40), POP surgery (OR 2.13, 95% CI 1.34–3.38), pelvic surgery (OR 1.81, 05% CI 1.01–3.26) and incontinence surgery (OR 1.87, 95% CI 1.08–3.25); Colorectal-Anal Distress Inventory-8 scores (OR 1.92, 95% CI 1.22–3.02); solitary predominant posterior compartment POP (OR 1.59, 95% CI 1.08–2.35); total vaginal length (OR 0.56, 95% CI 0.32–0.97); wide introitus (OR 4.85, 95% CI 1.60–14.68); levator ani avulsion (OR 2.47, 95% CI 1.35–4.53) and hiatal area on maximum Valsalva (OR 1.89, 95% CI 1.27–2.80).
Conclusion
During counselling for pessary treatment a higher risk of failure due to the aforementioned parameters should be discussed and modifiable parameters should be addressed. More research is needed on the association between anatomical parameters and specific reasons for unsuccessful pessary fitting.
Similar content being viewed by others
Introduction
Vaginal pessaries are widely used as a conservative treatment option in the management of pelvic organ prolapse (POP) [1, 2] and have proven effective in relieving POP symptoms [3,4,5]. However, multiple attempts with different pessaries are sometimes required before obtaining an adequate fit [6]. Additionally, pessary fitting is reported as unsuccessful in up to 59% of the women [7], the most common reasons being pessary dislodgment, discomfort/pain, de novo urinary symptoms and failure to relieve POP symptoms [8]. Many studies have been published on the factors associated with (un) successful pessary fitting for POP [7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39]. Among other potential predictors, age, body mass index (BMI), prior surgeries, predominant POP compartments and advanced POP have been assessed, but results differ across studies. It is thus necessary to clarify which parameters are associated with unsuccessful pessary fitting. This knowledge could improve the clinical practice of physicians dealing with POP: the counselling for pessary treatment would be more effective and more targeted, and potential parameters associated with failure would be known and discussed with the patient. In addition, modifiable factors could be addressed to increase the probability of success.
The aim of the current review and meta-analysis is to clarify which clinical, demographical and anatomical (assessed by clinical examination or imaging techniques) parameters are associated with unsuccessful pessary fitting for POP up to 3 months follow-up. A maximum of 3 months follow-up was chosen to focus on pessary fitting process instead of long-term pessary use.
Methods
Sources
The first author searched Emtree/MeSH terms and keywords related to prolapse, pessary and the exposures (i.e. parameters associated with unsuccessful pessary fitting) through Embase, PubMed and the Cochrane CENTRAL library. The outcome, e.g. unsuccessful pessary fitting, was not included in the search to avoid the risk of missing relevant records. The terms searched through Embase are reported in Table 1 (the same search strategy was translated to PubMed and Cochrane CENTRAL library). The final search was made on the 8 May 2020. No time restrictions were applied, while restrictions were used for language (i.e. English). All results were exported to RefWorks (Legacy version), and duplicates were removed. If an abstract and a paper reporting the same data were retrieved, the abstract was considered a duplicate and removed.
Eligibility criteria
Studies were included in which (1) pessary fitting was attempted in women with symptomatic POP (at least 80% of the study population had to have symptomatic POP), (2) one of the assessed outcomes was the success of “initial fitting” and/or “fitting process” with a maximal follow-up of 3 months (in the case of a longer follow-up, at least 80% of the unsuccessful group had to have discontinued the pessary within 3 months from the initial fitting) and (3) baseline parameters (i.e. clinical, demographic and anatomical parameters) were compared between the successful and unsuccessful group. Study design was not a selection criterion and studies reported only in conference abstracts were not excluded. In the following, “initial fitting” will refer to the first visit, which is considered successful if the patient leaves the clinic with a pessary that stays comfortably in place. “Fitting process” will refer to pessary use from initial fitting until a defined follow-up time. It is considered successful if the patient is still using the pessary at follow-up. “Pessary fitting” will refer to both initial fitting and fitting process, if no distinction between the two is needed.
Study selection
To select records eligible for full text assessment, title and abstract were screened by the first and second author, independently from each other. Any disagreement was resolved by discussion and the opinion of a third party (last author). The full text of the selected records was independently assessed by the same two authors. Disagreements were again resolved by discussion and the opinion of a third party (last author). The authors of a record were contacted if the full text of their paper was not accessible either online or at our institutional library and if some relevant parts of the records were unclear [e.g. definition of pessary fitting (un)success, time to follow-up, statistical significance of the observed differences or incorrect numbers].
Data extraction
A standardized data extraction form was created to retrieve the information relevant to the research question. The following data were extracted: reference (first author, year, journal citation), study design type, study setting, inclusion and exclusion criteria, sample size, prolapse assessment (i.e. Pelvic Organ Prolapse Quantification system or Baden-Walker), pessary types used, assessment of initial fitting and/or fitting process, definition of successful fitting, success rate, time to follow-up, parameters compared between successful and unsuccessful group, significant parameters on univariate analysis and significant parameters on multivariate analysis (if performed). In case a record reported follow-ups beyond 3 months, only the parameters relating to the follow-ups of the first 3 months were extracted.
Assessment of risk of bias
The Newcastle-Ottawa Scale (NOS) for case-control studies was used to assess the risk of bias of the included full-text articles [40]. Records only available as abstracts (i.e. no full-text available) were not assessed because of the limited amount of information they can provide. The NOS is specifically designed for non-randomized studies. It consists of three domains: Selection, Comparability and Exposure. The maximum total score is nine (four for the Selection domain, two for the Comparability domain and three for the Exposure domain). The first item assessed in the Selection domain is the adequacy of case definition and requires an independent validation. Since the success of pessary fitting is mostly patient self-reported, and no independent validation is applicable, no points could be given to this item. Therefore, the maximum score for the Selection domain was 3. A standard criterion for what constitutes a high-quality study base on the NOS has not yet been established. Generally, a study scoring ≥ 7 is considered high quality [41]. However, since no studies could get the maximum score on the Selection domain, we used a score of ≥ 6 as definition of high-quality studies.
Data synthesis
To produce a qualitative synthesis of the results, all parameters assessed on their association with unsuccessful pessary fitting were clustered in a limited number of domains. For each domain one table was produced enumerating all studies in which a specific parameter was assessed on univariate and/or multivariate analysis.
To assess pessary fitting success rate, the weighted success rate at different times to follow-up was calculated. Sub-analyses were made for those studies which excluded and included women with unsuccessful initial fitting.
A meta-analysis of the parameters compared between successful and unsuccessful group in at least two records was performed. All available studies were combined without making any distinction based on the time to follow-up. A study was not included in the meta-analysis if the necessary input data were not reported and if, after having contacted the authors, they did not provide the requested data. In case of overlap between study populations of two records, the record with the largest sample size reporting the parameter of interest was included in the analysis. The meta-analysis was done with the Comprehensive Meta-analysis (CMA) version 3 software. Input data for dichotomous variables were number of exposed (i.e. number of patients with a specific parameter, e.g. prior hysterectomy) and sample size of unsuccessful and successful group, when available, or odds ratio (OR) and confidence intervals. In the last case, unadjusted ORs were used in the meta-analysis. For continuous variable input data were mean, standard deviation (SD) and sample size of unsuccessful and successful group or, if a t-test was run to compare the two groups, p value and sample size of the two groups. If the data were reported as median and range (minimum-maximum) or interquartile range (IQR), the authors were contacted and asked for mean and SD. In case of no response, mean and SD would have to be imputed to include the study in the meta-analysis. At first, the meta-analysis was run excluding the studies that required data imputation. To test if the imputed data would have influenced the results, the meta-analysis was also run after data imputation. If the data were reported as median and range, the mean was imputed using the method described by Hozo et al. [42] and the SD was imputed using the method described by Wan et al. [43]. If the data were reported as median and IQR, mean and SD were derived using Wan’s method. Authors were also contacted if they reported a parameter as significant or not significant without providing quantitative data. A random effect model was applied for the analysis. The summary measure used was OR. Heterogeneity was assessed with Q test and I-squared. For the significant parameters the risk of publication bias was assessed with the trim and fill procedure [44]. The meta-analysis without data imputation is presented in the result section, while the meta-analysis with data imputation is reported in Appendix E.
The review was conducted in adherence to the PRISMA and MOOSE guidelines. The protocol of the review was not registered before implementation.
Results
Study selection
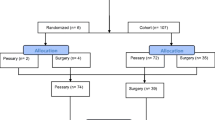
Using the search strategy described, 1084 unique records were identified. The screening of title and abstract left 151 records. Of these, 119 were excluded after full text assessment and are reported in Appendix A. Thirty-two records (27 papers and five conference abstracts) were included in the qualitative synthesis and 24 in the meta-analysis (Fig. 1).
Study characteristics
The characteristics of the 32 included records are enumerated in Table 2. In the following, the included records will be referred to according to the numbers reported in Table 2 and a superscript number will be used in the text. It has to be noted that there is an overlap between the study populations of Cheung et al. (2017) and Cheung et al. (2018) and Manchana (2011) and Manchana et al. (2012). In Appendix B the list of the authors contacted during the review process is reported.
Risk of bias
In Table 3 the Newcastle-Ottawa Scale scores for the three domains and the total scores are reported. Mean total score was 6.
Synthesis of results: success rate
Pessary fitting success rate ranged from 41%17 to 96%19. In Table 4 the weighted means at different times to follow-up are shown. Sub-analyses were made for those studies which excluded and included women with unsuccessful initial fitting. When the unsuccessful initial fitting was included, the success rates were overall lower (data at 3–4 weeks and 3 months). No sub-analysis was run for studies assessing fitting process success rate at 1/2 weeks, because only one study excluded women with unsuccessful initial fitting2.
Synthesis of results: parameters
The parameters assessed on their association with unsuccessful pessary fitting by different authors were clustered into nine domains: (1) Demographics, (2) Obstetric history, (3) (Uro) gynaecological symptoms and medications, (4) Prior surgeries, (5) General history, (6) Questionnaires, (7) POP and pelvic floor assessment, (8) Pessary and (9) Imaging. Appendix C shows the domain tables enumerating all studies in which a specific parameter was assessed on univariate and/or multivariate analysis. The results of the meta-analysis excluding imputed data are shown in Table 5 and the corresponding forest plots in Figs. 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13, 14 (significant parameters) and Appendix D (non-significant parameters).
Parameters associated with unsuccessful pessary fitting are: younger age, higher BMI, pre-menopausal status, stress urinary incontinence (SUI), prior surgery (i.e. hysterectomy, POP surgery, pelvic surgery, and incontinence surgery), higher Colorectal-Anal Distress Inventory-8 (CRADI-8) scores (which assess symptoms of obstructive defecation, anal incontinence, pain during defecation, faecal urgency and rectal bulging), shorter total vaginal length (TVL), wide introitus, levator ani avulsion and larger hiatal area on maximum Valsalva. The heterogeneity between studies and risk of publication bias is low for age, BMI, menopausal status, prior hysterectomy, prior pelvic surgery and prior incontinence surgery. SUI, prior POP surgery and TVL show a low risk of publication bias, but a relatively high heterogeneity between studies. For CRADI-8 scores, wide introitus, levator ani avulsion and hiatal area on Valsalva, the heterogeneity between studies is low, but the impact of publication bias could not be quantified because only two studies could be included in the analysis.
In Appendix E the results of the meta-analysis including imputed data are shown and in Appendix F the corresponding forest plots. Running the analysis without and with the imputed data did not qualitatively change the results: significant parameters remained significant and non-significant parameters remained non-significant. Sub-analyses were made for the parameters SUI and predominant posterior compartment. SUI is associated with unsuccessful pessary fitting (OR 2.06, 95% CI 1.15–3.66, z-value 2.45, p value 0.01). However, grouping the studies into those which assessed pre-existing SUI only and those which also assessed de novo SUI (alone or in combination with pre-existing SUI), de novo SUI remains significant (OR 5.59, 95% CI 2.24–13.99, z-value 3.68, p value 0.00), while pre-existing SUI does not (OR 1.44, 95% CI 0.88–2.36, z-value 1.45, p value 0.15) with small heterogeneity within groups (Q-value 11.17, p value 0.13).
Predominant posterior compartment is not associated with unsuccessful pessary fitting (OR 1.78, 95% CI 0.98–3.24, z-value 1.88, p value 0.06). However, in case of predominant multiple compartments (e.g. maximum POP stadium in the apical and posterior compartment), the patient was included in all relevant groups (e.g. predominant apical compartment POP and predominant posterior compartment POP). Analysing solitary predominant posterior compartment POP (i.e. excluding women with multiple predominant compartments), a significant association with unsuccessful fitting is observed (OR 1.59, 95% CI 1.08–2.35, z-value 2.37, p value 0.02, Q-value 4.51, df (Q) 5, Q-test p value 0.48, I-squared 0.00) with low risk of publication bias (trim and fill procedure: OR 1.75, 95% CI 1.21–2.53, Q-value 7.04).
Discussion
The aim of the current review and meta-analysis was to clarify which clinical, demographical and anatomical parameters are associated with unsuccessful pessary fitting for POP up to 3 months follow-up.
Main findings: success rate
In the current review the success rate of pessary fitting ranged from 41% to 96%. However, these differences become smaller if sub-analyses are made based on the follow-up time. From initial fitting to 3 to 4 weeks follow-up, the mean success rate decreased from 86% (95% CI 78%–92%) to 65% (95% CI 54%–75%). Interestingly, after 4 weeks the success rate remained substantially stable [success rate of 63% (95% CI 53%–72%) at 3 months follow-up]. This suggests that planning a follow-up at 4 weeks after initial fitting would ensure the vast majority of the unsuccessful fittings were identified (as also reported by Lone et al. [45]). Studies in which only women with successful initial fitting were included reported higher success rates compared to studies in which also women with unsuccessful initial fitting were included. Therefore, our suggestion for future research is to clearly report whether this selection is made or not.
Main findings: parameters
Parameters associated with unsuccessful pessary fitting include: younger age, higher BMI, pre-menopausal status, SUI, prior surgery (i.e. hysterectomy, POP surgery, pelvic surgery and incontinence surgery), higher CRADI-8 scores, shorter TVL, wide introitus, levator ani avulsion and larger hiatal area on maximum Valsalva.
In the case of SUI and prior POP surgery, the risk of publication bias is small, but the heterogeneity is relatively high. With respect to SUI, analysing separately the studies which assessed pre-existing SUI only, and those which also assessed de novo SUI, the heterogeneity within groups becomes smaller. Interestingly, de novo SUI remains significant, while pre-existing SUI does not. This suggests that pre-existing SUI alone is not associated with failure. Therefore, when counselling a patient for pessary treatment for POP, presence of pre-existing SUI should not be considered a reason for advising a different treatment. With respect to prior POP surgery, a possible explanation for the relatively high heterogeneity is that all women of the unsuccessful group in the study of Nemeth et al. (2017) had prior POP surgery with consequent extremely high OR in this study compared to the others.
Some parameters that are significant in the meta-analysis have to be taken with caution. First, TVL shows high heterogeneity between studies. Second, the impact of publication bias could not be quantified for CRADI-8, wide introitus, levator ani avulsion and hiatal area on Valsalva because only two studies could be included in the analysis. In addition, levator avulsion shows moderate heterogeneity, which can be explained by the different definitions of unsuccessful pessary fitting: pessary expulsion in the study of Cheung et al. and pessary discontinuation within 3 months follow-up in the study of Turel et al. The same explanation can be given to the moderate heterogeneity of other non-significant parameters, i.e. predominant apical compartment, advanced POP and GH. These parameters were associated with pessary dislodgment in the study of Cheung et al. but were not associated with unsuccessful pessary fitting when no distinction was made between different reasons for unsuccessful pessary fitting. The reasons for unsuccessful pessary fitting are numerous, e.g. dislodgment, discomfort/pain, de novo urinary symptoms and failure to relieve POP symptoms [8]. Some parameters could be associated only with specific reasons for pessary fitting failure, but not others; future research should analyse the association between anatomical parameters and individual causes of pessary fitting failure.
Parameters related to obstetric history, e.g. number of pregnancies, deliveries and vaginal deliveries, were not found to be associated with unsuccessful pessary fitting. However, no study assessed the influence of prior vaginal delivery vs no prior vaginal delivery on pessary fitting failure. If pessaries are supported by the pelvic floor muscles, prior vaginal delivery (which can cause pelvic floor muscles damage [46]) could be a risk factor for failure, even if POP mostly occurs in parous women. Being sexually active and hormone replacement therapy (HRT) use are not associated with (un) successful pessary fitting. Therefore, a sexually active woman with POP can be encouraged to try this treatment option and prescribing HRT only in case of indication is confirmed to be good practice.
Interestingly, advanced POP stage (3–4) is not associated with unsuccessful fitting. Therefore, pessary treatment can be advised to women with any stage of POP. Predominant anterior, apical or posterior compartment POPs are also not associated with unsuccessful fitting. However, higher CRADI-8 scores (which assess colorectal symptoms) and solitary predominant posterior compartment POP (i.e. maximum POP stage only in the posterior compartment, while women with multiple predominant compartments being excluded) are associated with unsuccessful fitting. These results confirm that pessary treatment is less effective in relieving colorectal symptoms [47].
Recently, a systematic review and meta-analysis has been published on the factors associated with unsuccessful pessary fitting in women with symptomatic POP [48]. Differences between their work and ours are the following. First, the follow-up for pessary fitting was 1 to 3 weeks in their work, while we included studies with a maximal follow-up of 3 months. Second, our search was performed in Embase, PubMed and Cochrane CENTRAL library, while theirs was performed in PubMed, and we screened 1084 records, while they screened 350. Third, they only included prospective studies, while we also included retrospective studies. Fourth, we assessed the weighted success rate of pessary fitting at different times to follow-up, which was not assessed in their work, while they assessed the reasons for pessary discontinuation after successful insertion, which we did not assess. Fifth, in our meta-analysis 24 studies were included, while 21 studies were included in theirs. Sixth, we performed a meta-analysis of 29 parameters, while they performed a meta-analysis of seven parameters. Seventh, we performed the analysis without and with data imputation, while they did not specify if imputed data were also included. With respect to the results, BMI and prior POP surgery were associated with pessary fitting failure in both works. In addition, GH was consistently not associated with pessary fitting failure. Different results were obtained for age, TVL, prior hysterectomy and advanced POP, which can be partially due to the differences described above. Furthermore, more studies were included in our meta-analysis, which should make our results more solid. Only three studies were included in the meta-analysis of the parameter “advanced POP” in their work. The one with the highest relative weight was the study of Cheung et al. in which the definition of failure was pessary dislodgment. It might be that advanced POP is a predictor of pessary dislodgment but not a predictor of other reasons for failure. Lastly, since we analysed more parameters, we also observed that menopausal status, de novo SUI, solitary predominant posterior compartment POP, higher CRADI-8 score, wide introitus, levator ani avulsion and larger hiatal area on maximum Valsalva are associated with unsuccessful pessary fitting.
Strengths and limitations
The current review and meta-analysis has several strengths. It was conducted according to the PRISMA and MOOSE guidelines. Multiple databases were searched. Study selection was made, independently, by two authors. The included papers were, on average, high-quality studies with a low risk of bias, as assessed by the Newcastle-Ottawa Scale. Moreover, authors were contacted in the case of missing information. Some limitations have to be acknowledged. Meta-analyses have the limitation that the interaction between different parameters cannot be assessed. For example, it is highly probable that younger age and pre-menopausal status are correlated. However, we cannot establish whether one of the two is a confounder or both are independently associated with unsuccessful pessary fitting. In addition, mean and SD of continuous variables are needed to perform a meta-analysis, but some authors reported only median and range or median and IQR. To include these studies in the meta-analysis, mean and SD would have to be imputed. While we decided to exclude these studies from the meta-analysis to avoid any possible bias due to data imputation, we note that imputing mean and SD in these studies and including them do not qualitatively change the results: significant parameters remain significant and non-significant parameters remain non-significant. This suggests that our conclusions are robust.
Conclusions
In women with symptomatic POP, younger age, higher BMI, pre-menopausal status, de novo SUI, prior surgery (i.e. hysterectomy, POP surgery, pelvic surgery or incontinence surgery), solitary predominant posterior compartment POP, presence of colorectal symptoms, shorter TVL, wide introitus, levator ani avulsion and larger hiatal area on maximum Valsalva are associated with unsuccessful pessary fitting up to 3 months follow-up.
These results do not imply that an alternative treatment should always be recommended to women with these characteristics, but rather that the higher risk of failure should be acknowledged and discussed during counselling for pessary treatment. Women with high risk of unsuccessful fitting because of, among others, a high BMI could work on this modifiable parameter to increase their probability of success, especially if they do not have many other treatment options (e.g. women who wish to have more children or those unwilling or not suitable to undergo surgery [49]). If pessary treatment is chosen, being aware of the higher risk of failure would relieve some of the frustration related to the unsuccessful pessary fitting process. One might object that such a counselling could lower women’s expectation thus increasing the risk of failure. However, any counselling should be evidence based and should allow women to make informed decisions to be ethical. In addition, the risk of pessary fitting failure should be weighted against the risks related to other treatments (e.g. surgery), which in many cases would encourage women to try pessary treatment.
Ethnicity, obstetric history, pre-existing SUI, sexual activity, use of HRT, smoking, predominant anterior, apical or multiple compartment POP, and advanced POP are not associated with unsuccessful pessary fitting. Therefore, women with these characteristics can be reassured that they do not have an increased risk of failure and can be encouraged to try pessary treatment.
With respect to the anatomical parameters (assessed by clinical examination or imaging techniques), more research is needed to investigate their association with specific reasons for unsuccessful pessary fitting, i.e. whether it is dislodgment, discomfort/pain or other reasons. In addition, only two studies included in the meta-analysis assessed the association between TPUS parameters and unsuccessful pessary fitting. Therefore, the added value of TPUS in the pessary fitting process should be further investigated.
Abbreviations
- BMI:
-
Body mass index
- CRADI-8:
-
Colorectal-Anal Distress Inventory-8
- GH:
-
Genital hiatus
- HRT:
-
Hormone replacement therapy
- POP:
-
Pelvic organ prolapse
- SUI:
-
Stress urinary incontinence
- TPUS:
-
Transperineal ultrasound
- TVL:
-
Total vaginal length
References
Gorti M, Hudelist G, Simons A. Evaluation of vaginal pessary management: a UK-based survey. J Obs Gynaecol. 2009;29:129–31. https://doi.org/10.1080/01443610902719813.
Cundiff GW, Weidner AC, Visco AG, Bump RC, Addison WA. A survey of pessary use by members of the American Urogynecologic Society. Obstet Gynecol. 2000;95:931–5. https://doi.org/10.1016/s0029-7844(00)00788-2.
Clemons JL, Aguilar VC, Tillinghast TA, Jackson ND, Myers DL. Patient satisfaction and changes in prolapse and urinary symptoms in women who were fitted successfully with a pessary for pelvic organ prolapse. Am J Obs Gynecol. 2004;190:1025–9. https://doi.org/10.1016/j.ajog.2003.10.711.
Ding J, Chen C, Song XC, Zhang L, Deng M, Zhu L. Changes in prolapse and urinary symptoms after successful fitting of a ring pessary with support in women with advanced pelvic organ prolapse: a prospective study. Urology. 2016;87:70–5. https://doi.org/10.1016/j.urology.2015.07.025.
Bugge C, Adams EJ, Gopinath D, Reid F. Pessaries (mechanical devices) for pelvic organ prolapse in women. Cochrane Database Syst Rev. 2013. https://doi.org/10.1002/14651858.CD004010.pub3.
Clemons JL. Vaginal pessary treatment of prolapse and incontinence. UpToDate, Post, TW (Ed), UpToDate, Waltham, MA, 2014 2020.
Mutone MF, Terry C, Hale DS, Benson JT. Factors which influence the short-term success of pessary management of pelvic organ prolapse. AJOG. 2005;193:89–94. https://doi.org/10.1016/j.ajog.2004.12.012.
Mao M, Ai F, Zhang Y, Kang J, Liang S, Xu T, et al. Predictors for unsuccessful pessary fitting in women with symptomatic pelvic organ prolapse: a prospective study. BJOG. 2018;125:1434–40. https://doi.org/10.1111/1471-0528.15260.
Cheung RYK, Lee JHS, Lee LL, Chung TKH, Chan SSC. Levator ani muscle avulsion is a risk factor for expulsion within 1 year of vaginal pessary placed for pelvic organ prolapse. Ultrasound Obstet Gynecol. 2017;50:776–80. https://doi.org/10.1002/uog.17407.
Cheung RYK, Lee LLL, Chung TKH, Chan SSC. Predictors for dislodgment of vaginal pessary within one year in women with pelvic organ prolapse. Maturitas. 2018;108:53–7. https://doi.org/10.1016/j.maturitas.2017.11.008.
Clemons JL, Aguilar VC, Tillinghast TA, Jackson ND, Myers DL. Risk factors associated with an unsuccessful pessary fitting trial in women with pelvic organ prolapse. Am J Obstet Gynecol. 2004;190:345–50. https://doi.org/10.1016/j.ajog.2003.08.034.
Cundiff GW, Amundsen CL, Bent AE, Coates KW, Schaffer JI, Strohbehn K, et al. The PESSRI study: symptom relief outcomes of a randomized crossover trial of the ring and Gellhorn pessaries. Am J Obstet Gynecol 2007;196:405.e1–8. https://doi.org/10.1016/j.ajog.2007.02.018.
Ding J, Chen C, Song X-C, Zhang L, Deng M, Zhu L. Successful use of ring pessary with support for advanced pelvic organ prolapse. Int Urogynecol J. 2015;26:1517–23. https://doi.org/10.1007/s00192-015-2738-1.
Fernando RJ, Thakar R, Sultan AH, Shah SM, Jones PW. Effect of vaginal pessaries on symptoms associated with pelvic organ prolapse. Obstet Gynecol. 2006;108:93–9. https://doi.org/10.1097/01.AOG.0000222903.38684.cc.
Geoffrion R, Zhang T, Lee T, Cundiff GW. Clinical characteristics associated with unsuccessful pessary fitting outcomes. Female Pelvic Med Reconstr Surg. 2013;19:339–45. https://doi.org/10.1097/SPV.0b013e3182a26174.
Ko PC, Lo TS, Tseng LH, Lin YH, Liang CC, Lee SJ. Use of a pessary in treatment of pelvic organ prolapse: quality of life, compliance, and failure at 1-year follow-up. J Minim Invasive Gynecol. 2011;18:68–74. https://doi.org/10.1016/j.jmig.2010.09.006.
Lekskulchai O, Wanichsetakul P. Factors affecting successfulness of vaginal pessary use for the treatment of pelvic organ prolapse. J Med Assoc Thail. 2015;98(Suppl 3):S115–20.
Maito JM, Quam ZA, Craig E, Danner KA, Rogers RG. Predictors of successful pessary fitting and continued use in a nurse-midwifery pessary clinic. J Midwifery Womens Healt. 2006;51:78–84. https://doi.org/10.1016/j.jmwh.2005.09.003.
Manchana T. Ring pessary for all pelvic organ prolapse. Arch Gynecol Obs. 2011;284:391–5. https://doi.org/10.1007/s00404-010-1675-y.
Manchana T, Bunyavejchevin S. Impact on quality of life after ring pessary use for pelvic organ prolapse. Int Urogynecol J. 2012;23:873–7. https://doi.org/10.1007/s00192-011-1634-6.
Markle D, Skoczylas L, Goldsmith C, Noblett K. Patient characteristics associated with a successful pessary fitting. Female Pelvic Med Reconstr Surg. 2011;17:249–52. https://doi.org/10.1097/SPV.0b013e31822f00ae.
Mokrzycki ML, Hatangadi SB, Zaccardi JE, Cox S. Preexisting stress urinary incontinence: a predictor of discontinuation with pessary management. J Low Genit Tract Dis. 2001;5:204–7.
Nemeth Z, Nagy S, Ott J. The cube pessary: an underestimated treatment option for pelvic organ prolapse? Subjective 1-year outcomes. Int Urogynecol J. 2013;24:1695–701. https://doi.org/10.1007/s00192-013-2093-z.
Nemeth Z, Farkas N, Farkas B. Is hysterectomy or prior reconstructive surgery associated with unsuccessful initial trial of pessary fitting in women with symptomatic pelvic organ prolapse? Int Urogynecol J. 2017;28:757–61. https://doi.org/10.1007/s00192-016-3184-4.
Nguyen JN, Jones CR. Pessary treatment of pelvic relaxation: factors affecting successful fitting and continued use. J Wound, Ostomy, Cont Nurs Off Publ Wound, Ostomy Cont Nurses Soc. 2005;32:253–5. https://doi.org/10.1097/00152192-200507000-00010.
Panman CMCR, Wiegersma M, Kollen BJ, Burger H, Berger MY, Dekker JH. Predictors of unsuccessful pessary fitting in women with prolapse: a cross-sectional study in general practice. Int Urogynecol J. 2017;28:307–13. https://doi.org/10.1007/s00192-016-3107-4.
Paterson FS, Abdool Z. Is pelvic floor morphology a predictor of successful pessary retention? Original research and review of the literature. S Afr J Obstet Gynaecol. 2018;24. https://doi.org/10.7196/sajog.1360.
Ramsay S, Tu LM, Tannenbaum C. Natural history of pessary use in women aged 65–74 versus 75 years and older with pelvic organ prolapse: a 12-year study. Int Urogynecol J. 2016;27:1201–7. https://doi.org/10.1007/s00192-016-2970-3.
Wu V, Farrell SA, Baskett TF, Flowerdew G. A simplified protocol for pessary management. Obstet Gynecol. 1997;90:990–4. https://doi.org/10.1016/s0029-7844(97)00481-x.
Yamada T, Matsubara S. Rectocoele, but not cystocoele, may predict unsuccessful pessary fitting. J Obstet Gynaecol. 2011;31:441–2. https://doi.org/10.3109/01443615.2011.577253.
Yang J, Han J, Zhu F, Wang Y. Ring and Gellhorn pessaries used in patients with pelvic organ prolapse: a retrospective study of 8 years. Arch Gynecol Obstet. 2018;298:623–9. https://doi.org/10.1007/s00404-018-4844-z.
Turel Fatakia F, Pixton S, Caudwell Hall J, Dietz HP. Predictors of successful ring pessary use in women with pelvic organ prolapse. Aust New Zeal J Obstet Gynaecol. 2020:1–6. https://doi.org/10.1111/ajo.13152.
Cho MMM. Use of pelvic organ prolapse quantification (POPQ) measurements to predict pessary type for successful fitting. Female Pelvic Med Reconstr Surg. 2015;21:S77.
Hooper G, Davis A, Stafford M. Cube pessary use and quality of life in women with pelvic organ prolapse. Female Pelvic Med Reconstr Surg. 2018;24:S99.
Umachanger J, Marcussen M, Bøgild H, Kjærgaard N, Glavind K. First-line treatment of pelvic organ prolapse. IUJ. 2018;29:S60.
Zhu L, Wang W, Lang J, Chen H, Li L. Prospective study of ring pessary treatment for women with pelvic organs prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2011;22:S1423.
Triepels CP, Notten KJ, Weemhoff M, Kruitwagen RF, van Kruijk SM, Futterer JJ. Comparison of anatomical structures in women with successful and unsuccessful pessary therapy for pelvic organ prolapse (POP) 2019.
Handa VL, Jones M. Do pessaries prevent the progression of pelvic organ prolapse? Int Urogynecol J Pelvic Floor Dysfunct. 2002;13:349–51; discussion 352. https://doi.org/10.1007/s001920200078.
Jones K, Yang L, Lowder JL, Meyn L, Ellison R, Zyczynski HM, et al. Effect of pessary use on genital hiatus measurements in women with pelvic organ prolapse. Obstet Gynecol. 2008;112:630–6. https://doi.org/10.1097/AOG.0b013e318181879f.
Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2013 n.d. https://doi.org/10.1207/s15551407vcq1302_4.
Islam MM, Iqbal U, Walther B, Atique S, Dubey NK, Nguyen PA, et al. Benzodiazepine use and risk of dementia in the elderly population: a systematic review and Meta-analysis. Neuroepidemiology. 2017;47:181–91. https://doi.org/10.1159/000454881.
Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:1–10. https://doi.org/10.1186/1471-2288-5-13.
Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol 2014;14:1–13. https://doi.org/10.1186/1471-2288-14-135.
Shi L, Lin L, Omboni S. The trim-and-fill method for publication bias: Practical guidelines and recommendations based on a large database of meta-analyses. Med (United States) 2019;98. https://doi.org/10.1097/MD.0000000000015987.
Lone F, Thakar R, Sultan AH, Karamalis G. A 5-year prospective study of vaginal pessary use for pelvic organ prolapse. Int J Gynaecol Obstet. 2011;114:56–9. https://doi.org/10.1016/j.ijgo.2011.02.006.
Kamisan Atan I, Lin S, Dietz HP, Herbison P, Wilson PD. It is the first birth that does the damage: a cross-sectional study 20 years after delivery. Int Urogynecol J. 2018;29:1637–43. https://doi.org/10.1007/s00192-018-3616-4.
Dengler EG, Mounsey LA, Gines F, Agha M, Long T, Geller EJ. Defecatory dysfunction and other clinical variables are predictors of pessary discontinuation. Int Urogynecol J. 2019;30:1111–6. https://doi.org/10.1007/s00192-018-3777-1.
de Albuquerque Coelho S, Brito L, de Araujo C, Juliato C. Factors associated with unsuccessful pessary fitting in women with symptomatic pelvic organ prolapse: systematic review and metanalysis. Neurourol Urodyn 2020:1–10. https://doi.org/10.1002/nau.24458.
Barber MD. Pelvic organ prolapse. BMJ. 2016;354:1–9. https://doi.org/10.1136/bmj.i3853.
Funding
The study was part of the Gynaecological Imaging using 3D UltraSound (GYNIUS) project with number 15301, which is financed by the Dutch Research Council (NWO). Philips and TOMTEC contributed to the project by providing an ultrasound machine and an analysis software, which were not used for the current paper. The funding sources had no involvement in the study design, analysis, interpretation of data, report writing or preparation of this publication.
Author information
Authors and Affiliations
Contributions
Claudia Manzini: Conceptualization, Record screening, Formal analysis, Writing - Original Draft, Review and Editing.
Lisan M. Morsinkhof: Record screening, Writing - Review and Editing.
C. Huub van der Vaart: Conceptualization, Writing - Review and Editing.
Mariëlla I.J. Withagen: Writing - Review and Editing.
Anique T.M. Grob: Conceptualization, Record screening, Writing - Review and Editing.
Ethics declarations
Conflict of interest
Authors declare no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix A List of the records excluded after full text assessment
-
1
Adams E, Thomson A, Maher C, Hagen S. Mechanical devices for pelvic organ prolapse in women. Cochrane Database Syst Rev. 2004:CD004010. https://doi.org/10.1002/14651858.CD004010.pub2.
-
2
Ai FF, Mao M, Zhang Y, Kang J, Zhu L. Effect of generalized anxiety disorders on the success of pessary treatment for pelvic organ prolapse. Int Urogynecol J 2018;29:1147–53. https://doi.org/10.1007/s00192-018-3562-1.
-
3
Ai F-F, Zhu L, Mao M, Zhang Y, Kang J. Depressive symptoms affect outcomes of pessary use in postmenopausal women with uterine prolapse. Climacteric 2018;21:184–8. https://doi.org/10.1080/13697137.2018.1430130.
-
4
Al-Badr A. Quality of life questionnaires for the assessment of pelvic organ prolapse: Use in clinical practice. LUTS Low Urin Tract Symptoms 2013;5:121–8. https://doi.org/10.1111/luts.12006.
-
5
Alnaif B, Drutz HP. The association of smoking with vaginal flora, urinary tract infection, pelvic floor prolapse, and post-void residual volumes. J Low Genit Tract Dis 2001;5:7–11. https://doi.org/10.1046/j.1526-0976.2001.51002.x.
-
6
Alperin M, Khan A, Dubina E, Tarnay C, Wu N, Pashos CL, et al. Patterns of pessary care and outcomes for medicare beneficiaries with pelvic organ prolapse. Female Pelvic Med Reconstr Surg 2013;19:142–7. https://doi.org/10.1097/SPV.0b013e31827e857c.
-
7
Anantawat T, Manonai J, Wattanayingcharoenchai R, Sarit-apirak S. Impact of a vaginal pessary on the quality of life in women with pelvic organ prolapse. Asian Biomed 2016;10:249–52. https://doi.org/10.5372/1905-7415.1003.487.
-
8
Armstrong K, Dessie S, Modest A, Hacker M, Hota L. The effect of vaginal oestrogen on pessary usage. Neurourol Urodyn 2014:18–21.
-
9
Atnip SD. Pessary use and management for pelvic organ prolapse. Obstet Gynecol Clin North Am 2009;36:541–63. https://doi.org/10.1016/j.ogc.2009.08.010.
-
10
Bai SW, Yoon BS, Kwon JY, Shin JS, Kim SK, Park KH. Survey of the characteristics and satisfaction degree of the patients using a pessary. Int Urogynecol J Pelvic Floor Dysfunct 2005;16:182–6; discussion 186. https://doi.org/10.1007/s00192-004-1226-9.
-
11
Bastani P, Solbian FE, Mokhtarkhani M, Yegani S, Kabiri N. Effects of vaginal pessaries on symptoms associated with pelvic organ prolapse. Int.J.Urol. 2014
-
12
Bastani P, Danandeh Osgui N. Improvement of concomitant symptoms of pelvic organ prolapsed with applied pessary. Clin Exp Obstet Gynecol 2019;46:42–4. https://doi.org/10.12891/ceog4309.2019.
-
13
Bezerra LS, Vasconcelos CT, Vasconcelos Neto J, Bezerra KD, Saboia DM, Oria MO, Do Nascimento TS, Reboucas RN,Viana VF. Adherence and follow-up to pessary using educational video: Prospective court. Int Urogynecol J 2017;28:S183–4.
-
14
Brincat C, Kenton K, Pat Fitzgerald M, Brubaker L. Sexual activity predicts continued pessary use. Am J Obstet Gynecol 2004;191:198–200. https://doi.org/10.1016/j.ajog.2004.03.083.
-
15
Broens-Oostveen MC, Mom RM, Lagro-Janssen ALM. [Genital prolapse; treatment and course in four general practices]. Ned Tijdschr Geneeskd 2004;148:1444–8.
-
16
Bugge C, Adams EJ, Gopinath D, Reid F. Pessaries (mechanical devices) for pelvic organ prolapse in women. Cochrane Database Syst Rev. 2013;2013. https://doi.org/10.1002/14651858.CD004010.pub3.
-
17
Bulchandani S, Toozs-Hobson P, Verghese T, Latthe P. Does vaginal oestrogen treatment with support pessaries in vaginal prolapse reduce complications? Post Reprod Heal 2015;21:141–5. https://doi.org/10.1177/2053369115614704.
-
18
Chan MC, Hyakutake M, Yaskina M, Schulz JA. What Are the Clinical Factors That Are Predictive of Persistent Pessary Use at 12 Months? J Obstet Gynaecol Can 2019;41:1276–81. https://doi.org/10.1016/j.jogc.2018.11.015.
-
19
Cheung R, Chan S, Lee L. Factors associated with dislodgment of vaginal pessary within one year. Int Urogynecol J Pelvic Floor Dysfunct 2016;27:S132–3.
-
20
Cheung R, Lee L, Chan S. Does levator ani muscle injury affect the efficacy of vaginal pessary in women with pelvic organ prolapse. Int Urogynecology J 281 Suppl 1 (S96-S97) Date Publ 1 Jun 2017 2018:20–2.
-
21
Cheung RY-K, Lee L-L, Chung TK-H, Chan SS-C. Predictors for dislodgment of vaginal pessary within one year in women with pelvic organ prolapse. Journal of Obstetrics and Gynaecology Research. 2017
-
22
Cheung RYK, Lee JHS, Lee LL, Chung TKH, Chan SSC. Vaginal Pessary in Women With Symptomatic Pelvic Organ Prolapse: A Randomized Controlled Trial. Obstet Gynecol 2016;128:73–80. https://doi.org/10.1097/AOG.0000000000001489.
-
23
Chien C-W, Lo T-S, Tseng L-H, Lin Y-H, Hsieh W-C, Lee S-J. Long-term Outcomes of Self-Management Gellhorn Pessary for Symptomatic Pelvic Organ Prolapse. Female Pelvic Med Reconstr Surg 2019. https://doi.org/10.1097/SPV.0000000000000770.
-
24
Clemons JL, Aguilar VC, Sokol ER, Jackson ND, Myers DL. Patient characteristics that are associated with continued pessary use versus surgery after 1 year. Am J Obstet Gynecol 2004;191:159–64. https://doi.org/10.1016/j.ajog.2004.04.048.
-
25
Coelho SCA, Marangoni-Junior M, Brito LGO, Castro EB de, Juliato CRT. Quality of life and vaginal symptoms of postmenopausal women using pessary for pelvic organ prolapse: a prospective study. Rev. Assoc Med Bras 2018;64:1103–7. https://doi.org/10.1590/1806-9282.64.12.1103.
-
26
Daneel L, te West NI, Moore KH. Does monthly self-removal of vaginal ring pessaries for stress incontinence/prolapse reduce complication rates? A 5 year audit. Neurourol Urodyn 2016:5–8.
-
27
Davila GW. Vaginal prolapse: management with nonsurgical techniques. Postgrad Med 1996;99:171–176,181,184–185.
-
28
Dekker JH, Burger H. Authors’ reply to the comment by Hanis et al. on “Predictors of unsuccessful pessary fitting in women with prolapse: a cross-sectional study in general practice,” by Panman et al. Int Urogynecol J 2017;28:1441. https://doi.org/10.1007/s00192-017-3421-5.
-
29
Deng M, Ding J, Ai F, Zhu L. Successful use of the Gellhorn pessary as a second-line pessary in women with advanced pelvic organ prolapse. Menopause 2017;24:1277–81. https://doi.org/10.1097/GME.0000000000000909.
-
30
Deng M, Ding J, Ai F, Zhu L. Clinical use of ring with support pessary for advanced pelvic organ prolapse and predictors of its short-term successful use. Menopause 2017;24:954–8. https://doi.org/10.1097/GME.0000000000000859.
-
31
Dengler EG, Mounsey LA, Gines F, Agha M, Long T, Geller EJ. Defecatory dysfunction and other clinical variables are predictors of pessary discontinuation. Int Urogynecol J 2019;30:1111–6. https://doi.org/10.1007/s00192-018-3777-1.
-
32
Dessie SG, Armstrong K, Modest AM, Hacker MR, Hota LS. Effect of vaginal oestrogen on pessary use. Int Urogynecol J 2016;27:1423–9. https://doi.org/10.1007/s00192-016-3000-1.
-
33
Ding J, Chen C, Song X-C, Zhang L, Deng M, Zhu L. Changes in Prolapse and Urinary Symptoms After Successful Fitting of a Ring Pessary With Support in Women With Advanced Pelvic Organ Prolapse: A Prospective Study. Urology 2016;87:70–5. https://doi.org/10.1016/j.urology.2015.07.025.
-
34
Ding J, Song X Chen, Deng M, Zhu L. Which factors should be considered in choosing pessary type and size for pelvic organ prolapse patients in a fitting trial? Int Urogynecol J 2016;27:1867–71. https://doi.org/10.1007/s00192-016-3051-3.
-
35
Duenas JL, Miceli A. Effectiveness of a continuous-use ring-shaped vaginal pessary without support for advanced pelvic organ prolapse in postmenopausal women. Int Urogynecol J 2018;29:1629–36. https://doi.org/10.1007/s00192-018-3586-6.
-
36
Dwyer L, Kearney R. Conservative management of pelvic organ prolapse. Obstet Gynaecol Reprod Med 2018;28:15–21. https://doi.org/10.1016/j.ogrm.2017.10.005.
-
37
Eberhard J, Geissbühler V. Pessary treatment in urogynaecology and obstetrics. Gynakol Prax 2002;26:119–33.
-
38
Espitia De La Hoz FJ. O-06 Evaluation of Quality of Life in Climacteric Women With Genital Prolapse after the Use of Pessary. J Sex Med 2017;14:e373–4. https://doi.org/10.1016/j.jsxm.2017.10.016.
-
39
Fitchett JR, Bhatta S, Sherpa TY, Malla BS, A Fitchett EJ, Samen A, et al. Non-surgical interventions for pelvic organ prolapse in rural Nepal: a prospective monitoring and evaluation study. JRSM Open 2015;6:2054270415608117. https://doi.org/10.1177/2054270415608117.
-
40
Friedman S, Sandhu KS, Wang C, Mikhail MS, Banks E. Factors influencing long-term pessary use: Reply by the authors. Int Urogynecol J 2011;22:1047. https://doi.org/10.1007/s00192-011-1393-4.
-
41
Friedman S, Sandhu KS, Wang C, Mikhail MS, Banks E. Factors influencing long-term pessary use. Int Urogynecol J 2010;21:673–8. https://doi.org/10.1007/s00192-009-1080-x.
-
42
Fritzinger KG, Newman DK, Dinkin E. Use of a pessary for the management of pelvic organ prolapse. Lippincotts Prim Care Pract 1997;1:431–6.
-
43
Geoffrion R, Zhang T, Lee T, Cundiff GW. Clinical characteristics associated with unsuccessful pessary fitting outcomes. Obstet Gynecol Surv 2014;69:79–81. https://doi.org/10.1097/01.ogx.0000444678.89257.5f.
-
44
Goodman R.W.;Komesu Y.M.;McFadden B.L.;Rogers R.G. Do pessaries prevent prolapse progression? Female Pelvic Med Reconstr Surg 182 SUPPL 1 (S25-S26) 2015:4–6.
-
45
Griebling TL. Re: Natural History of Pessary Use in Women Aged 65–74 versus 75 Years and Older with Pelvic Organ Prolapse: A 12-Year Study. J Urol 2017;197:1321. https://doi.org/10.1016/j.juro.2017.02.041.
-
46
Griebling TL. Vaginal pessaries for treatment of pelvic organ prolapse in elderly women. Curr Opin Urol 2016;26:201–6. https://doi.org/10.1097/MOU.0000000000000266.
-
47
Griffin M, Kim Y, Roberts R, Abed H. Pessary use as a first line treatment for pelvic floor disorders. Neurourol Urodynamics 34 SUPPL 1 (S74) 2015;34:S2–98. https://doi.org/10.1002/nau.22738.
-
48
Gupta P, Ehlert MJ, Bartley JM. Diagnosis and management of complex pelvic floor disorders in women. J Clin Outcomes Manag 2015;22:275–85.
-
49
Gupta A, Cox X, Dunivan GC, Gaskins JT, Rogers RG, Iglesia CB, et al. Desire for Continued Pessary Use Among Women of Hispanic and Non-Hispanic Ethnic Backgrounds for Pelvic Floor Disorders. Female Pelvic Med Reconstr Surg 2020;26:287–98. https://doi.org/10.1097/SPV.
-
50
Hagen S, Thakar R. Conservative management of pelvic organ prolapse. Obstet Gynaecol Reprod Med 2015;25:91–5. https://doi.org/10.1016/j.ogrm.2015.01.006.
-
51
Handa VL, Jones M. Do pessaries prevent the progression of pelvic organ prolapse? IUJ 2002;13:349–52. https://doi.org/10.1007/s001920200078.
-
52
Hanis SM, Khazaei S, Ayubi E, Mansori K. Comment on: Predictors of unsuccessful pessary fitting in women with prolapse: a cross-sectional study in general practice. Int Urogynecol J 2017;28:1439. https://doi.org/10.1007/s00192-017-3359-7.
-
53
Hanson L-AM, Schulz JA, Flood CG, Cooley B, Tam F. Vaginal pessaries in managing women with pelvic organ prolapse and urinary incontinence: patient characteristics and factors contributing to success. Int Urogynecol J Pelvic Floor Dysfunct 2006;17:155–9. https://doi.org/10.1007/s00192-005-1362-x.
-
54
Hassler A, Michael K. The pessary, a method for treating pelvic organ prolapse. J Diagnostic Med Sonogr 2005;21:12–6. https://doi.org/10.1177/8756479304272678.
-
55
Hooper GL. Person-Centered Care for Patients with Pessaries. Nurs Clin North Am 2018;53:289–301. https://doi.org/10.1016/j.cnur.2018.01.006.
-
56
Hsieh M-F, Tsai H-W, Liou W-S, Lo C-C, Lin Z-H, An Y-F, et al. Long-term compliance of vaginal pessaries: Does stress urinary incontinence matter? Medicine (Baltimore) 2019;98:e15063. https://doi.org/10.1097/MD.0000000000015063.
-
57
Jacobson NS, Taney J, Overbey J, Hardart A, J.A. F. Pessary use for managementofpelvic organ prolapse in atertiary care center: A retrospective review. Female Pelvic Med Reconstr Surg 235 Suppl 1(S90-S91)2017:3–5. https://doi.org/10.1097/SPV.0000000000000479.
-
58
Johannes O., Promberger R., Nmeth Z. Vaginal cube pessaries for genital prolapse. Climacteric 2014;17:48–108. https://doi.org/10.3109/13697137.2014.893733.
-
59
Jones KA, Harmanli O. Pessary use in pelvic organ prolapse and urinary incontinence. Rev. Obstet Gynecol 2010;3:3–9.
-
60
Komesu YM, Rogers RG, Rode MA, Craig EC, Gallegos KA, Montoya AR, et al. Pelvic floor symptom changes in pessary users. Am J Obstet Gynecol 2007;197:620.e1–620.e6. https://doi.org/10.1016/j.ajog.2007.08.013.
-
61
Komesu YM, Rogers RG, Rode MA, Craig EC, Schrader RM, Gallegos KA, et al. Patient-selected goal attainment for pessary wearers: what is the clinical relevance? Am J Obstet Gynecol 2008;198:577.e1–5. https://doi.org/10.1016/j.ajog.2007.12.033.
-
62
Krause H. Pessary use in pelvic organ prolapse. BJOG Int J Obstet Gynaecol. 2015
-
63
Kuhn A, Bapst D, Stadlmayr W, Vits K, Mueller MD. Sexual and organ function in patients with symptomatic prolapse: are pessaries helpful? Fertil Steril 2009;91:1914–8. https://doi.org/10.1016/j.fertnstert.2008.02.142.
-
64
Lalani S, Izett ML, Welford K, Lyons A, Kupelian A, Vashisht A. Outcomes of nurse-led pessary clinic for pelvic organ prolapse. Female Pelvic Med Reconstr Surg. 2019
-
65
Lamers BHC, Broekman BMW, Milani AL. Pessary treatment for pelvic organ prolapse and health-related quality of life: A review. Int Urogynecol J 2011;22:637–44. https://doi.org/10.1007/s00192-011-1390-7.
-
66
Lee HSJ, Cheung YR, Chan SS. Efficacy and complications of vaginal ring pessary in pelvic organ prolapse. Neurourol Urodyn 2014:1–2.
-
67
Lewthwaite BJ, Staley D, Girouard L, Maslow K. Characteristics of women with continued use of vaginal pessaries. Urol Nurs 2013;33:171–6.
-
68
Lone F, Thakar R, Sultan AH. One-year prospective comparison of vaginal pessaries and surgery for pelvic organ prolapse using the validated ICIQ-VS and ICIQ-UI (SF) questionnaires. Int Urogynecol J 2015;26:1305–12. https://doi.org/10.1007/s00192-015-2686-9.
-
69
Lone F, Thakar R, Sultan AH, Karamalis G. A 5-year prospective study of vaginal pessary use for pelvic organ prolapse. Int J Gynaecol Obstet 2011;114:56–9. https://doi.org/10.1016/j.ijgo.2011.02.006.
-
70
Lowenstein L, Gamble T, Sanses TVD, van Raalte H, Carberry C, Jakus S, et al. Changes in sexual function after treatment for prolapse are related to the improvement in body image perception. J Sex Med 2010;7:1023–8. https://doi.org/10.1111/j.1743-6109.2009.01586.x.
-
71
Manonai J, Sarit-Apirak S, Udomsubpayakul U. Vaginal ring pessary use for pelvic organ prolapse: Continuation rates and predictors of continued use. Menopause 2019;26:665–9. https://doi.org/10.1097/GME.0000000000001277.
-
72
Mao M, Ai F, Kang J, Zhang Y, Liang S, Zhou Y, et al. Successful long-term use of Gellhorn pessary and the effect on symptoms and quality of life in women with symptomatic pelvic organ prolapse. Menopause 2019;26:145–51. https://doi.org/10.1097/GME.0000000000001197.
-
73
Mao M, Ai F, Zhang Y, Kang J, Liang S, Xu T, et al. Changes in the symptoms and quality of life of women with symptomatic pelvic organ prolapse fitted with a ring with support pessary. Maturitas 2018;117:51–6. https://doi.org/10.1016/j.maturitas.2018.09.003.
-
74
Mao M, Xu T, Kang J, Zhang Y, Ai F, Zhou Y, et al. Factors associated with long-term pessary use in women with symptomatic pelvic organ prolapse. Climacteric 2019;22:478–82. https://doi.org/10.1080/13697137.2019.1582623.
-
75
Matsubara S. Factors influencing long-term pessary use: comment. Int Urogynecol J 2011;22:1045; author reply 1046. https://doi.org/10.1007/s00192-011-1394-3.
-
76
Nojima S, Wang L, S; Y Iwadare J, Nokazi N, Kanaeda T, et al. Long-term use of the vaginal ring pessary for pelvic organ prolapse-over 2 years follow up. Int Urogynecol J Pelvic Floor Dysfunct 2009;20 Suppl 3:241–491. https://doi.org/10.1007/s00192-009-0982-y.
-
77
Onwude JL. Genital prolapse in women. BMJ Clin Evid 2007;2007.
-
78
Onwude JL. Genital prolapse in women. BMJ Clin Evid 2009;2009.
-
79
Onwude JL. Genital prolapse in women. BMJ Clin Evid 2012;2012.
-
80
Panman CMCR, Wiegersma M, Kollen BJ, Berger MY, Lisman-van Leeuwen Y, Vermeulen KM, et al. Effectiveness and cost-effectiveness of pessary treatment compared with pelvic floor muscle training in older women with pelvic organ prolapse: 2-year follow-up of a randomized controlled trial in primary care. Menopause 2016;23:1307–18. https://doi.org/10.1097/GME.0000000000000706.
-
81
Patel M, Mellen C, O’Sullivan DM, LaSala CA. Impact of pessary use on prolapse symptoms, quality of life, and body image. Am J Obstet Gynecol 2010;202:499.e1–4. https://doi.org/10.1016/j.ajog.2010.01.019.
-
82
Patel MS, Mellen C, O’Sullivan DM, Lasala CA. Pessary use and impact on quality of life and body image. Female Pelvic Med Reconstr Surg 2011;17:298–301. https://doi.org/10.1097/SPV.0b013e31823a8186.
-
83
Pezzella M., Iervolino SA., Passaretta A., Torella M., Colacurci N. Sexual funstion among women using a pessary for pelvic organ prolapse. Neurourol Urodyn 2017;36:S5–87. https://doi.org/10.1002/nau.23302.
-
84
Pizarro-Berdichevsky J, Pattillo A, Blumel B, Gonzalez S, Arellano M, Cuevas R, et al. Prospective comparative results: Of pessary use in patients with symptomatic pelvic organ prolapse in patients above or below 65 years of age. Neurourol Urodyn 2015;34:S2–98. https://doi.org/10.1002/nau.22738.
-
85
Pizarro-Berdichevsky J, Pattillo A, Blumel B, Gonzalez S, Arellano M, Cuevas R, et al. Pessary use in patients with symptomatic pelvic organ prolapse-12 month prospective study of factors predictive of subjective improvement. Int Urogynecol J 2016;27:19–149. https://doi.org/10.1007/s00192-016-3042-4.
-
86
Poma PA. Nonsurgical management of genital prolapse. A review and recommendations for clinical practice. J Reprod Med 2000;45:789–97.
-
87
Powers K, Lazarou G, Wang A, LaCombe J, Bensinger G, Greston WM, et al. Pessary use in advanced pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct 2006;17:160–4. https://doi.org/10.1007/s00192-005-1311-8.
-
88
Radnia N, Hajhashemi M, Eftekhar T, Deldar M, Mohajeri T, Sohbati S, et al. Patient Satisfaction and Symptoms Improvement in Women Using a Vginal Pessary for The Treatment of Pelvic Organ Prolapse. J Med Life 2019;12:271–5. https://doi.org/10.25122/jml-2019-0042.
-
89
Ralph C, Pohlhammer S, Blumel B, Pizarro-Berdichevsky J. Pessary use for symptomatic pelvic organ prolapse (SYMP POP) in patients <=65 years: Feasibility retrospective study. Neurourol Urodyn 2014;33:162–266. https://doi.org/10.1002/nau.22577.
-
90
Ramsay S, Bouchard F, Tu LM. Pelvic Organ Prolapse and Pessary Use: Is It a Viable Long Term Treatment Option? J Urol 2012;187:1–3. https://doi.org/10.1016/j.juro.2012.02.2310.
-
91
Ramsay S, Bouchard F, Tu LM, Sherbrooke U De. Long term outcomes of pessary use in women with pelvic organ prolapse. Neurourol Urodynamics 2011;30.
-
92
Robert M, Govan AJ, Lohani U, Uprety A. Feasibility of using pessaries for treatment of pelvic organ prolapse in rural Nepal. Int J Gynaecol Obstet 2017;136:325–30. https://doi.org/10.1002/ijgo.12061.
-
93
Robert M, Schulz JA, Harvey M-A. Technical update on pessary use. JOGC 2013;35:664–74. https://doi.org/10.1016/S1701-2163(15)30888-4.
-
94
Sarit-Apirak S, Manonai J. Vaginal pessary use for pelvic organ prolapse in thai women. Female Pelvic MedReconstrSurg 2014;20:151–368.
-
95
Sarma S, Ying T, Moore KH. Long-term vaginal ring pessary use: discontinuation rates and adverse events. BJOG 2009;116:1715–21. https://doi.org/10.1111/j.1471-0528.2009.02380.x.
-
96
Scarabelot K, Pereira F, Ghizzo L, Willing J, Virtuoso J. Use of pessary in the treatment of pelvic floor dysfunctions: A systematic review. Physiother Q 2018;26:1–8. https://doi.org/10.5114/pq.2018.74704.
-
97
Shayo BC, Masenga GG, Rasch V. Vaginal pessaries in the management of symptomatic pelvic organ prolapse in rural Kilimanjaro, Tanzania: a pre-post interventional study. Int Urogynecol J 2019;30:1313–21. https://doi.org/10.1007/s00192-018-3748-6.
-
98
Sitavarin S, Wattanayingcharoenchai R, Manonai J, Sarit-apirak S, Chittacharoen A. The characteristics and satisfaction of the patients using vaginal pessaries. J Med Assoc Thai 2009;92:744–7.
-
99
Srikrishna S, Cardozo L. How Best to Manage the Posterior Compartment. Curr. Bladder Dysfunct.Rep. 2013
-
100
Sulak PJ, Kuehl TJ, Shull BL. Vaginal pessaries and their use in pelvic relaxation. J Reprod Med 1993;38:919–23.
-
101
Takashima Y, Dancz C, Ozel B. Factors associated with pessary discontinuation: A retrospective review. Neurourol Urodyn 2016. https://doi.org/10.1002/nau.22967.
-
102
Tan GI, Balakrishnan S. Factors that predict the medium-term success of the use of pessaries for symptomatic pelvic organ prolapse. IntUrogynecolJ 2018;10:1–15.
-
103
Tasic L, Jurisic A, Jankovic S, Karadzov N. Vaginal pessary is the best option for some women. Maturitas 2017;100:182. https://doi.org/10.1016/j.maturitas.2017.03.213.
-
104
te West NID, Moore KH. Recent Developments in the Non-surgical Management of Pelvic Organ Prolapse. Curr Obstet Gynecol Rep 2014;3:172–9. https://doi.org/10.1007/s13669-014-0087-6.
-
105
Tso C, Lee W, Austin-Ketch T, Winkler H, Zitkus B. Nonsurgical Treatment Options for Women With Pelvic Organ Prolapse. Nurs Womens Health 2018;22:228–39. https://doi.org/10.1016/j.nwh.2018.03.007.
-
106
Urzua M, Alvarez J, Rondini C, M M. Pessary use in pelvic organ prolapse in women. Int Urogynecol J 2017;28:1–282. https://doi.org/10.1007/s00192-017-3337-0.
-
107
van Geelen JM, Dwyer PL. Where to for pelvic organ prolapse treatment after the FDA pronouncements? A systematic review of the recent literature. Int Urogynecol J 2013;24:707–18. https://doi.org/10.1007/s00192-012-2025-3.
-
108
Vanherpe P, Ghesquière S. Use of pessaries in the treatment of pelvic organ prolapse. Tijdschr Geneeskd 2015;71:596–603. https://doi.org/10.2143/TVG.71.09.2001854.
-
109
Williams KS, Wolff BJ, Lind LR, Winkler HA. Vaginal oestrogen reduces adverse events in patients with pelvic organ prolapse managed with a pessary. Female Pelvic Med Reconstr Surg 2015;21:S76–7.
-
110
Withayajiakkhajorn P, Limbutara W, Gorsagun C. Pessary expulsion rate and risk factors for expulsion in women with pelvic organ prolapsed in southern Thailand. Int Urogynecol J 2018;15:2017–9.
-
111
Wlazlak E, Kociszewski J, Krzycka M, Pazdrak M, Wlazlak W, Kluz T, et al. Daily used cube pessaries in women with pelvic organprolapse: Fitting, influence on pelvic floor function. Int Urogynecol J 2017;28:1–282. https://doi.org/10.1007/s00192-017-3337-0.
-
112
Wlazlak E, Kociszewski J, Krzycka M, Wlazlak W, Dunicz A, Surkont G. Ultrasound evaluation of the influence of cube pessaries on female’s pelvic floor. Neurourol Urodyn 2018:2018–21.
-
113
Wolff BJ., Williams KS., Lind LR., Winkler HA., Shalom DF. Predictive factors for long-term pessary use and discontinuation: A retrospective cohort study. Female Pelvic Med Reconstr Surg 2001;21:55–6.
-
114
Wolff B, Williams K, Winkler A, Lind L, Shalom D. Pessary types and discontinuation rates in patients with advanced pelvic organ prolapse. Int Urogynecol J 2017;28:993–7. https://doi.org/10.1007/s00192-016-3228-9.
-
115
Yimphong T, Temtanakitpaisan T, Buppasiri P, Chongsomchai C, Kanchaiyaphum S. Discontinuation rate and adverse events after 1 year of vaginal pessary use in women with pelvic organ prolapse. Int Urogynecol J 2018;29:1123–8. https://doi.org/10.1007/s00192-017-3445-x.
-
116
Zhu L, Mao M. Factors Associated with Long-Term Pessary Use in Women with Symptomatic Pelvic Organ Prolapse. J Minim Invasive Gynecol 2019;26:S210–1. https://doi.org/10.1016/j.jmig.2019.09.437.
-
117
Zhu L., Mao M., Ai F. Changes of symptoms and quality of life in women with symptomatic pelvic organ prolapse fitted with ring with support pessary: A long-term study. Int Urogynecol J 2018;10:1–15.
-
118
Li B, Chen Q, Zhang J, Yu C, Zhang L, Chen L. A prospective study of pessary use for severe pelvic organ prolapse: 3-year follow-up outcomes. Arch Gynecol Obstet 2020;301:1213–8. https://doi.org/10.1007/s00404-020-05526-1.
-
119
Yoshimura K, Morotomi N, Fukuda K, Kubo T, Taniguchi H. Changes of intravaginal microbiota and inflammation after self-replacement ring pessary therapy compared to continuous ring pessary usage for pelvic organ prolapse. J Obstet Gynaecol Res 2020;46:931–8. https://doi.org/10.1111/jog.14242.
Appendix B List of the authors contacted during the review process
Phase | Authors | Reason contact | Response | Conclusion | |
|---|---|---|---|---|---|
Screening process | Triepels et al. | Unclear time to follow-up | Yes | < 3 months | Abstract included |
Yang et al. | Abstract on the same data reported in the paper? | Yes | Abstract on the same data reported in the paper | Abstract considered as a duplicate | |
Eberhard et al. | Record not retrieved | No | – | Not included | |
Fritzinger et al. | Record not retrieved | No | – | Not included | |
Poma | Record not retrieved | No | – | Not included | |
Data analysis | Cheung et al. | Overlap study populations?1,2 | Yes | Yes | Paper with the biggest sample for meta-analysis |
Cheung et al. | Missing data in the two groups on BMI and no. vaginal deliveries | Yes | BMI: 7 in drop pessary group and 18 in pessary group; vaginal delivery: 7 in drop pessary group and 27 in pessary group | Data used for meta-analysis | |
Clemons et al. | Mean and SD of GH and TVL | Dichotomous data used in the analysis in which imputed data were included | |||
Cundiff et al. | Mean and SD of age, prevalence of white ethnicity in the two groups | Yes | Data provided | Data used for meta-analysis | |
Ding et al. | Mean and SD of BMI, gravidity, parity | No | Data imputed for the analysis in which imputed data were included | ||
Fernando et al. | Mean and SD of age, parity | No | OR used as input data (age provided as dichotomous variable: only used in the analysis in which imputed data were included) | ||
Geoffrion et al. | Mean and SD of age | Yes | Data provided | Data used for meta-analysis | |
Jones et al. | Mean and SD of parity | No | Data imputed for the analysis in which imputed data were included | ||
Ko et al. | Mean and SD of age, BMI, parity | No | Since data could not be imputed, not used for the analysis | ||
Lekskulchai et al. | Mean and SD of age, parity, length of the perineal body, GH | No | Data imputed for the analysis in which imputed data were included | ||
Maito et al. | Mean and SD of age, pelvic floor strength, vaginal parity; prevalence of prior POP procedure, hysterectomy, urinary incontinence procedure, grade 3 or 4 of POP, urinary incontinence in the two groups | No | Since data could not be imputed, study not included in the meta-analysis | ||
Manchana et al. | Overlap study populations?11,12 | No | – | Paper with the biggest sample for meta-analysis | |
Manchana et al. | Mean and SD of parity | No | Data imputed for the analysis in which imputed data were included | ||
Mao et al. | Mean and SD of gravidity, no. vaginal deliveries, TVL, vaginal introitus, GH; prevalence of menopausal women in the two groups | No | Data imputed for the analysis in which imputed data were included (when possible) | ||
Mokrzycki et al. | Mean and SD of vaginal parity | No | P value of a t-test and sample sizes of the two groups used as input data | ||
Mutone et al. | Mean and SD of age, BMI, levator ani strength, GH, perineal body length, TVL | Yes | Data not available | Data imputed and BMI used as dichotomous variable for the analysis in which imputed data were included | |
Nemeth et al. 2013 | Mean and SD of age, BMI, parity | No | Data imputed for the analysis in which imputed data were included (when possible) | ||
Nguyen et al. | SD of age, mean and SD of parity, number of women with pre-existing SUI and SUI after POP reduction in the two groups | No | P value of a t-test and sample sizes of the two groups used for age. Largest SD reported by other studies used for parity in the analysis in which imputed data were included. Groups with pre-existing SUI and SUI after POP could not be separated | ||
Panman et al. | Mean and SD of age, BMI, parity, CRADI-8, pelvic floor strength, GH, TVL | No | Data imputed for the analysis in which imputed data were included | ||
Paterson et al. | Mean and SD of hiatal distance on contraction. Data on levator avulsion. | No | Since data could not be imputed, study not included in the meta-analysis | ||
Ramsay et al. | Prevalence of prior hysterectomy, prior POP surgery, predominant anterior, apical, posterior POP compartment, POP stage 3–4, stress urinary incontinence in the two groups; mean and SD of number of vaginal deliveries | No | Since data could not be imputed, study not included in the meta-analysis | ||
Wu et al. | Mean and SD of age and parity | Yes | Data not available | Not included in the meta-analysis | |
Cho et al. | Clarifications on their results | No | – | Results described according to our understanding. Conference abstract: not included in the meta-analysis | |
Hooper et al. | Clarifications on their results | Yes | Grade of POP and prior hysterectomy predictors of unsuccessful fitting at 1 week | Results described according to authors. Conference abstract: not included in the meta-analysis | |
Appendix C. Each table shows the parameters of one specific domain. For each parameter the studies in which it was assessed on univariate and/or multivariate analysis are reported as well as whether it was significant or not
Appendix C1 Demographics domain
Parameter | Univariate analysis assessment | Significant univariate analysis | Multivariate analysis Assessment | Significant multivariate analysis |
|---|---|---|---|---|
Age | Cheung et al. 2017 Cheung et al. 2018 Clemons et al. Cundiff et al. Ding et al. Fernando et al. Geoffrion et al. Jones et al. Ko et al. Lekskulchai et al. Manchana, 2011 Manchana et al. 2012 Mao et al. Markle et al. Mokrzycki et al. Mutone et al. Nemeth et al. 2013 Nemeth et al. 2017 Nguyen et al. Ramsay et al. Wu et al. Yamada et al. Yang et al. Turel et al. Cho et al. | Cundiff et al. Fernando et al. Geoffrion et al. Mao et al. Wu et al. | Fernando et al. Geoffrion et al. Maito et al. Mao et al. Panman et al. | Geoffrion et al. Panman et al. |
BMI/weight | Cheung et al. 2017 Cheung et al. 2018 Ding et al. Geoffrion et al. Ko et al. Lekskulchai et al. Manchana et al. 2012 Mao et al. Markle et al. Mutone et al. Nemeth et al. 2013 Nemeth et al. 2017 Nguyen et al. Yang et al. Turel et al. Cho et al. | Mao et al. Mutone et al. | Cheung et al. 2018 Maito et al. Mao et al. Panman et al. | Mao et al. Panman et al. |
Menopause | Cheung et al. 2017 Cheung et al. 2018 Geoffrion et al. Jones et al. Ko et al. Manchana et al. 2012 Mao et al. Markle et al. Mokrzycki et al. Nemeth et al. 2013 Nguyen et al. Yang et al. Turel et al. Cho et al. | Mao et al. Turel et al. | Mao et al. Turel et al. | Turel et al. |
Ethnicity | Clemons et al. Cundiff et al. Fernando et al. Geoffrion et al. Cho et al. | Cundiff et al. Cho et al. | Fernando et al. | – |
Appendix C2 Obstetric history domain
Parameter | Univariate analysis assessment | Significant univariate analysis | Multivariate analysis Assessment | Significant multivariate analysis |
|---|---|---|---|---|
Gravidity | Ding et al. Geoffrion et al. Mao et al. Yang et al. | – | – | – |
Parity/ n. vaginal deliveries | Cheung et al. 2017 Cheung et al. 2018 Clemons et al. Ding et al. Fernando et al. Geoffrion et al. Jones et al. Ko et al. Lekskulchai et al. Manchana, 2011 Manchana et al. 2012 Mao et al. Markle et al. Mokrzycki et al. Nemeth et al. 2013 Nemeth et al. 2017 Nguyen et al. Ramsay et al. Wu et al. Yamada et al. Yang et al. Turel et al. Cho et al. | Fernando et al. Nemeth et al. 2013 Nemeth et al. 2017 Yang et al. | Fernando et al. Maito et al. Nemeth et al. 2017 | Fernando et al. |
Largest baby | Cheung et al. 2018 Ding et al. Geoffrion et al. Mao et al. | Geoffrion et al. | Panman et al. Geoffrion et al. | – |
Assisted vaginal delivery | Geoffrion et al. | – | – | – |
Tear into rectum | Geoffrion et al. | – | – | – |
Appendix C3 (Uro) gynaecological symptoms and medications domain
Parameter | Univariate analysis assessment | Significant univariate analysis | Multivariate analysis assessment | Significant multivariate analysis |
|---|---|---|---|---|
Urinary symptoms | Clemons et al. Ding et al. Geoffrion et al. Manchana et al. 2012 Mao et al. Markle et al. Mokrzycki et al. Nguyen et al. Ramsay et al. Wu et al. Zhu et al. | Mokrzycki et al. Nguyen et al. Wu et al. | Maito et al. Nguyen et al. | Nguyen et al. |
De novo urinary incontinence | Ding et al. Ko et al. Nguyen et al. | Ko et al. Nguyen et al. | – | – |
Sexually active | Cheung et al. 2017 Cheung et al. 2018 Clemons et al. Geoffrion et al. Manchana et al. 2012 Markle et al. Ramsay et al. Cho et al. | Cho et al. | – | – |
Age of onset/duration symptoms | Mokrzycki et al. Yang et al. | – | – | – |
Vaginal hormones | Geoffrion et al. Jones et al. Cho et al. | – | – | – |
Oral hormones | Clemons et al. Geoffrion et al. Jones et al. Markle et al. Nguyen et al. Wu et al. | – | – | – |
Postvoidal residual | Geoffrion et al. | – | – | – |
Vaginal atrophy | Clemons et al. Mokrzycki et al. Ramsay et al. | – | – | – |
Anal incontinence | – | – | Maito et al. | – |
Pelvic pressure/lower backache | Nemeth et al. 2013 | – | – | – |
Discomfort | Ramsay et al. | – | – | – |
POP necessitating manual reduction | Ramsay et al. | – | – | – |
Appendix C4 Prior surgeries domain
Parameter | Univariate analysis assessment | Significant univariate analysis | Multivariate analysis Assessment | Significant multivariate analysis |
|---|---|---|---|---|
Hysterectomy | Cheung et al. 2017 Cheung et al. 2018 Clemons et al. Ding et al. Fernando et al. Jones et al. Geoffrion et al. Manchana, 2011 Manchana et al. 2012 Mao et al. Markle et al. Mutone et al. Nemeth et al. 2013 Nemeth et al. 2017 Nguyen et al. Ramsay et al. Wu et al. Yamada et al. Yang et al. Turel et al. Cho et al. Hooper et al. Umachanger et al. | Fernando et al. Markle et al. Mutone et al. Nemeth et al. 2013 Nemeth et al. 2017 Ramsay et al. Cho et al. Hooper et al. Umachanger et al | Fernando et al. Maito et al. Nemeth et al. 2017 Panman et al. Turel et al. | Fernando et al. Maito et al. Turel et al. |
POP surgery | Clemons et al. Ding et al. Fernando et al. Jones et al. Geoffrion et al. Mao et al. Markle et al. Mutone et al. Nemeth et al. 2013 Nemeth et al. 2017 Nguyen et al. Ramsay et al. Wu et al. Turel et al. Cho et al. Zhu et al. | Fernando et al. Mao et al. Mutone et al. Nemeth et al. 2013 Nemeth et al. 2017 Nguyen et al. Ramsay et al. Cho et al. | Fernando et al. Maito et al. Mao et al. Nemeth et al. 2017 Nguyen et al. Panman et al. | Maito et al. Nemeth et al. 2017 Nguyen et al. |
Pelvic surgery | Geoffrion et al. Mokrzycki et al. Wu et al. Zhu et al. Umachanger et al. | Umachanger et al. Wu et al. | Panman et al. | – |
Incontinence surgery | Geoffrion et al. Markle et al. Nguyen et al. Wu et al. | – | Maito et al. | – |
Appendix C5 General history domain
Parameter | Univariate analysis assessment | Significant univariate analysis | Multivariate analysis assessment | Significant multivariate analysis |
|---|---|---|---|---|
Comorbidities | Ding et al. Ko et al. Manchana et al. 2012 Yang et al. | Ko et al. | Maito et al. | – |
Poor surgical candidate | Clemons et al. | – | – | – |
Smoking | Ding et al. Geoffrion et al. Nguyen et al. Turel et al. | Geoffrion et al. | Geoffrion et al. | Geoffrion et al. |
Family support | Ding et al. Ko et al. | Ko et al. | – | – |
Constipation | Ding et al. Ramsay et al. | – | Maito et al. | – |
Desire of surgery at the 1st visit | Clemons et al. | – | – | – |
Appendix C6 Questionnaires domain
Parameter | Univariate analysis assessment | Significant univariate analysis | Multivariate analysis Assessment | Significant multivariate analysis |
|---|---|---|---|---|
PFDI-20 | Jones et al. Geoffrion et al. Yang et al | – | – | – |
POPDI-6 | Geoffrion et al. Yang et al. | – | – | – |
UDI-6 | Geoffrion et al. Yang et al. | – | – | – |
CRADI-8 | Geoffrion et al. Yang et al. | Yang et al. | – | – |
PFIQ-7 | Geoffrion et al. Yang et al. | – | – | – |
POPIQ-7 | Geoffrion et al. Yang et al. | – | – | – |
UIQ-7 | Geoffrion et al. Yang et al. | – | – | – |
CRAIQ-7 | Geoffrion et al. Yang et al. | – | – | – |
PEQ | Geoffrion et al. | – | – | – |
Appendix C7 POP and pelvic floor assessment domain
Parameter | Univariate analysis assessment | Significant univariate analysis | Multivariate analysis Assessment | Significant multivariate analysis |
|---|---|---|---|---|
Compartment | Cheung et al. 2017 Cheung et al. 2018 Clemons et al. Ding et al. Fernando et al. Jones et al. Geoffrion et al. Lekskulchai et al. Mao et al. Markle et al. Mokrzycki et al. Mutone et al. Ramsay et al. Yamada et al. Turel et al. Zhu et al. | Cheung et al. 2017 Cheung et al. 2018 Lekskulchai et al. Mao et al. Mutone et al. Turel et al. Ramsay et al. Yamada et al. | Cheung et al. 2017 Cheung et al. 2018 Maito et al. Mao et al. Panman et al. | Cheung et al. 2018 Maito et al. |
Stage | Cheung et al. 2017 Cheung et al. 2018 Clemons et al. Ding et al. Fernando et al. Jones et al. Geoffrion et al. Ko et al. Manchana, 2011 Manchana et al. 2012 Mao et al. Markle et al. Mokrzycki et al. Mutone et al. Nemeth et al. 2013 Nguyen et al. Ramsay et al. Yamada et al. Cho et al. Hooper et al. Zhu et al. | Cheung et al. 2017 Cheung et al. 2018 Yamada et al. Cho et al. Hooper et al. | Cheung et al. 2017 Cheung et al. 2018 Geoffrion et al. Maito et al. Panman et al. | Cheung et al. 2017 Cheung et al. 2018 Geoffrion et al. |
TVL | Cheung et al. 2018 Clemons et al. Ding et al. Jones et al. Lekskulchai et al. Manchana, 2011 Mao et al. Markle et al. Mutone et al. Turel et al. Zhu et al. | Cheung et al. 2018 Clemons et al. Lekskulchai et al. Manchana 2011 Mao et al. Markle et al. | Cheung et al. 2018 Mao et al. Markle et al. | Mao et al. |
Introitus width | Clemons et al. Manchana, 2011 Mao et al. Zhu et al. | Clemons et al. Manchana, 2011 | – | – |
GH | Cheung et al. 2018 Clemons et al. Ding et al. Jones et al. Lekskulchai et al. Manchana, 2011 Mao et al. Markle et al. Mutone et al. Turel et al. | Cheung et al. 2018 | Cheung et al. 2018 | Cheung et al. 2018 |
Pb | Cheung et al. 2018 Jones et al. Lekskulchai et al. Markle et al. Mutone et al. Turel et al. Wu et al | Turel et al. Jones et al. | Turel et al. Jones et al. | Jones et al. |
GH + Pb | Turel et al. | Turel et al. | Turel et al. | Turel et al. |
GH/TVL | Ding et al. Geoffrion et al. Markle et al. | Markle et al. | Geoffrion et al. Markle et al. | Geoffrion et al. |
Pelvic floor strength | Geoffrion et al. Mutone et al. Turel et al. | – | Maito et al. Panman et al. | Panman et al. |
Appendix C8 Pessary domain
Parameter | Univariate analysis assessment | Significant univariate analysis | Multivariate analysis Assessment | Significant multivariate analysis |
|---|---|---|---|---|
Type | Fernando et al. Jones et al. Mutone et al. Wu et al. Cho et al. | Mutone et al. Cho et al. | Fernando et al. | – |
Size | Nemeth et al. 2013 | – | – | – |
Self-insertion | Ding et al. Ko et al. | – | – | – |
Insertion ease | Nemeth et al. 2013 | Nemeth et al. 2013 | – | – |
Appendix C9 Imaging domain
Parameter | Univariate analysis assessment | Significant univariate analysis | Multivariate analysis Assessment | Significant multivariate analysis |
|---|---|---|---|---|
TPUS | Cheung et al. 2017 Paterson et al. Turel et al. | Cheung et al. 2017 Paterson et al. Turel et al. | Cheung et al. 2017 Turel et al. | Cheung et al. 2017 |
MRI | Triepels et al. | Triepels et al. | – | – |
Appendix D Forest plots of the non-significant parameters (imputed data excluded)

Appendix D.1. Forest plot for the association of white ethnicity with the outcome of pessary fitting up to 3 months follow-up (N = 521)

Appendix D.2. Forest plot for the association of “number of pregnancies” (N = 401) with the outcome of pessary fitting up to 3 months follow-up

Appendix D.3. Forest plot for the association of number of deliveries (N = 1402) with the outcome of pessary fitting up to 3 months follow-up

Appendix D.4. Forest plot for the association of number of vaginal deliveries with the outcome of pessary fitting up to 3 months follow-up (N = 301)

Appendix D.5. Forest plot for the association of largest baby (i.e. > 8 lbs. in Ding et al. and Geoffrion et al.; > 4 kg in Mao et al.) with the outcome of pessary fitting up to 3 months follow-up (N = 507)

Appendix D.6. Forest plot for the association of sexually active with the outcome of pessary fitting up to 3 months follow-up (N = 1085)

Appendix D.7. Forest plot for the association of hormonal replacement therapy with the outcome of pessary fitting up to 3 months follow-up (N = 663)

Appendix D.8. Forest plot for the association of “smoking” with the outcome of pessary fitting up to 3 months follow-up (N = 470)

Appendix D.9. Forest plot for the association of predominant anterior compartment with the outcome of pessary fitting up to 3 months follow-up (N = 1615). In case of predominant multiple compartments (e.g. maximum POP stadium in the anterior and apical compartment), the patient was included in all relevant groups (e.g. predominant anterior compartment POP and predominant apical compartment POP)

Appendix D.10. Forest plot for the association of predominant apical compartment with the outcome of pessary fitting up to 3 months follow-up (N = 1504). In case of predominant multiple compartments (e.g. maximum POP stadium in the anterior and apical compartment), the patient was included in all relevant groups (e.g. predominant anterior compartment POP and predominant apical compartment POP)

Appendix D.11. Forest plot for the association of “predominant posterior compartment” with the outcome of pessary fitting up to 3 months follow-up (N = 1534). In case of predominant multiple compartments (e.g. maximum POP stadium in the anterior and apical compartment), the patient was included in all relevant groups (e.g. predominant anterior compartment POP and predominant apical compartment POP)

Appendix D.12. Forest plot for the association of prolapse stage 3 or 4 with the outcome of pessary fitting up to 3 months follow-up (N = 1658)

Appendix D.13. Forest plot for the association of GH (i.e. genital hiatus) with the outcome of pessary fitting up to 3 months follow-up (N = 941)

Appendix D.14. Forest plot for the association of perineal body with the outcome of pessary fitting up to 3 months follow-up (N = 860). A = success, B = failure

Appendix D.15. Forest plot for the association of GH/TVL with the outcome of pessary fitting up to 3 months follow-up (N = 340)

Appendix D.16. Forest plot for the association of pelvic floor strength with the outcome of pessary fitting up to 3 months follow-up (N = 185)
Appendix E Results of the meta-analysis including imputed data (only parameters requiring data imputation are shown)
Parameter | OR (95% CI) | z-value | p value | Heterogeneity | Trim and fill | Studies included | ||||
|---|---|---|---|---|---|---|---|---|---|---|
Q value | df (Q) | p value | I-squared | OR (95% CI) | Q value | |||||
Demographics | ||||||||||
Age | 0.69 (0.58–0.82) | −4.22 | 0.00 | 24.26 | 19 | 0.19 | 21.70 | 0.71 (0.60–0.85) | 28.35 | 2, 3, 4, 5, 6′, 7, 8, 10°, 13, 14, 15, 16, 17°, 18°, 19, 20, 21°, 24, 26, 27 |
BMI | 1.45 (1.21–1.75) | 3.93 | 0.00 | 10.67 | 10 | 0.38 | 6.28 | 1.29 (1.07–1.56) | 17.49 | 2, 5′, 7, 13, 14, 15, 17′, 19, 21°, 24, 27 |
Obstetric history | ||||||||||
No. pregnancies | 0.80 (0.57–1.14) | −1.24 | 0.22 | 0.84 | 3 | 0.84 | 0.00 | – | – | 5°, 7, 14°, 26 |
No. deliveries | 0.80 (0.59–1.08) | −1.43 | 0.15 | 46.62 | 14 | 0.00 | 69.97 | – | – | 2°, 3, 5°, 6, 7, 8°, 10°, 13°, 18°, 19, 20°, 21°, 24°, 26, 27 |
No. vaginal deliveries | 0.90 (0.65–1.26) | −0.60 | 0.55 | 6.05 | 4 | 0.20 | 33.92 | – | – | 2°, 7, 14°, 15, 16 |
Largest baby | 1.53 (0.81–2.88) | 1.30 | 0.19 | 10.52 | 4 | 0.03 | 61.97 | – | – | 2, 5′, 7′, 14′, 21° |
Questionnaires | ||||||||||
CRADI-8 | 2.04 (1.37–3.04) | 3.49 | 0.00 | 0.73 | 2 | 0.69 | 0.00 | 2.04 (1.37–3.04) | 0.73 | 7, 21°, 27 |
POP and pelvic floor assessment | ||||||||||
TVL | 0.44 (0.25–0.78) | −2.79 | 0.01 | 75.99 | 10 | 0.00 | 86.84 | 0.47 (0.27–0.83) | 77.81 | 2, 3′, 5, 8, 10, 12′, 14°, 15, 17°, 21°, 24 |
GH | 0.51 (0.91–1.62) | −0.33 | 0.74 | 90.59 | 10 | 0.00 | 88.96 | – | – | 2, 3′, 5, 8, 10°, 12′, 14°, 15, 17°, 21°, 24 |
Perineal body | 1.24 (0.91–1.69) | 1.35 | 0.18 | 10.07 | 5 | 0.07 | 50.36 | – | – | 2, 8, 10°, 15, 17°, 24 |
Introitus width | 2.71 (1.61–4.58) | 3.73 | 0.00 | 1.82 | 2 | 0.40 | 0.00 | 2.29 (1.33–3.94) | 4.42 | 3′, 12′, 14° |
Pelvic floor strength | 0.57 (0.29–1.13) | −1.62 | 0.11 | 11.04 | 3 | 0.01 | 72.83 | – | – | 7, 17°, 21′, 24 |
Appendix F1 Forest plots of the significant parameters including imputed data (only parameters requiring data imputation are shown)

Appendix F1.1 Forest plot for the association of age with successful pessary fitting up to 3 months follow-up (N = 3838)

Appendix F1.2. Forest plot for the association of BMI (N = 2787) with unsuccessful pessary fitting up to 3 months follow-up

Appendix F1.3. Forest plot for the association of CRADI-8 (i.e. Colorectal-Anal Distress Inventory-8) scores with unsuccessful pessary fitting up to 3 months follow-up (N = 478)

Appendix F1.4. Forest plot for the association of TVL (i.e. total vaginal length) with successful pessary fitting up to 3 months follow-up (N = 2139). A = success, B = failure

Appendix F1.5. Forest plot for the association of introitus width with unsuccessful pessary fitting up to 3 months follow-up (N = 543)
Appendix F2 Forest plots of the non-significant parameters including imputed data (only parameters requiring data imputation are shown)

Appendix F2.1. Forest plot for the association of number of pregnancies (N = 825) with the outcome of pessary fitting up to 3 months follow-up

Appendix F2.2. Forest plot for the association of number of deliveries with the outcome of pessary fitting up to 3 months follow-up (N = 2790)

Appendix F2.3. Forest plot for the association of number of vaginal deliveries with the outcome of pessary fitting up to 3 months follow-up (N = 1138)

Appendix F2.4. Forest plot for the association of largest baby with the outcome of pessary fitting up to 3 months follow-up (N = 997)

Appendix F2.5. Forest plot for the association of GH (i.e. genital hiatus) with the outcome of pessary fitting up to 3 months follow-up (N = 2140)

Appendix F2.6. Forest plot for the association of perineal body with the outcome of pessary fitting up to 3 months follow-up (N = 1438)

Appendix F2.7. Forest plot for the association of pelvic floor strength with the outcome of pessary fitting up to 3 months follow-up (N = 647)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Manzini, C., Morsinkhof, L.M., van der Vaart, C.H. et al. Parameters associated with unsuccessful pessary fitting for pelvic organ prolapse up to three months follow-up: a systematic review and meta-analysis. Int Urogynecol J 33, 1719–1763 (2022). https://doi.org/10.1007/s00192-021-05015-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-021-05015-2