Advertisement
Advertisement
December 2023 Supplement
Sponsored By Surmodics, Inc.
Preliminary Clinical Evidence on Pounce™ Thrombectomy System Performance
A conversation with Dr. Bruce H. Gray.
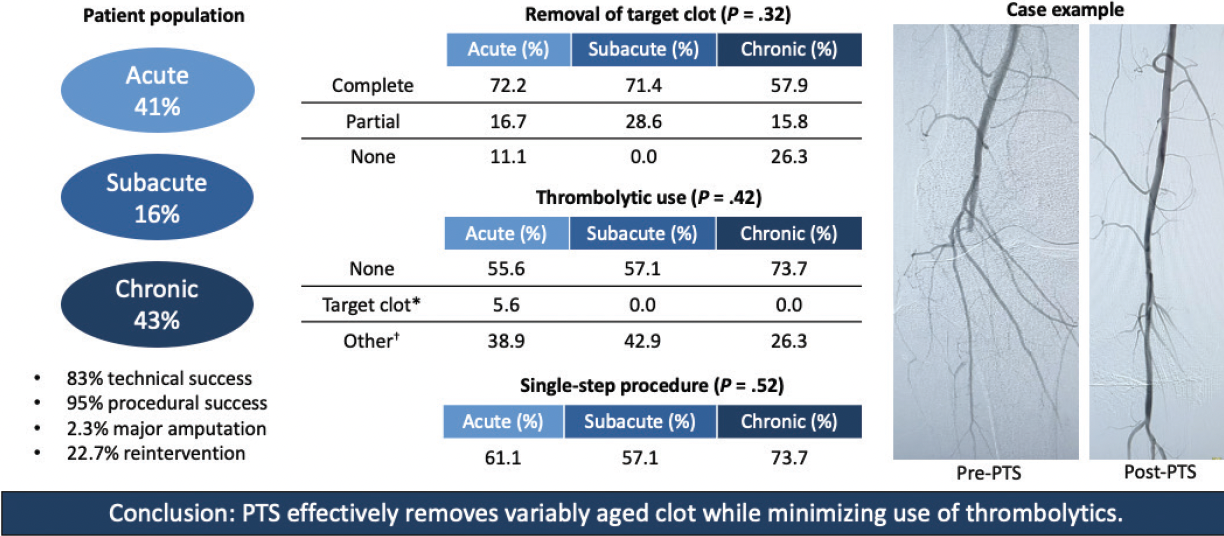
We spoke with Dr. Bruce H. Gray about his recently published study1 on the use of the Pounce™ Thrombectomy System (Surmodics, Inc.) for treatment of acute and chronic peripheral arterial occlusions. The study retrospectively examined 44 consecutive patients treated for lower extremity limb ischemia with suspected thrombus using the Pounce™ System at Prisma Health System, Greenville, South Carolina.
Recognizing that this was a preliminary study, what do you feel were the most notable findings?
Figure 1 summarizes what I consider to be key findings. We achieved 83% technical success in effectively removing thrombus from the peripheral arterial segments where the Pounce™ System was used.* This is particularly noteworthy because, unlike previous studies of arterial thrombectomy devices,2-5 our study population included patients with subacute (15-30 days of symptoms) and chronic (> 30 days) limb ischemia in addition to acute limb ischemia (≤ 14 days). In just 1 of 44 cases, thrombolysis was used to resolve thrombus at a Pounce™ System treatment site. Most patients treated with thrombolysis had remote or distal clot not attempted with the Pounce™ System due to the system’s indicated vessel range. Overall, most patients included in the study could be treated with a single-step procedure.
Clot removal was less complete in patients with longer-standing ischemia compared with those with shorter-standing ischemia. This is not surprising, as these patients will tend to have more chronic, wall-adherent thrombus. In my experience, this type of residua can be treated like plaque without concern for distal embolization. The central theme of treating these patients centers on treating thrombus like thrombus and plaque like plaque.
Finally, although the device performed robustly in terms of thrombus removal and restoration of pulsatile flow, reintervention was not uncommon. Having a pristine angiographic result after a procedure is not enough—these patients need careful post-procedural management and aggressive anticoagulation.
Just to be clear, how do you define a “single-step” procedure?
A single-step procedure implies that at the time of a diagnostic arteriogram, the Pounce™ Thrombectomy System is used immediately, accompanied by any additional technique to treat underlying disease (ie, plain/drug-coated balloon angioplasty, plain/drug-eluting/covered stents), facilitating same-day discharge. The patient doesn’t have to be admitted. This avoids catheter-directed thrombolysis (CDT), which entails bleeding risk, intensive care unit admission, repeat contrast injections, and the inconvenience of repeat angiographic radiation and sedation.
Can you describe your use of CDT for the patients in this study?
We used CDT predominantly in vessels not indicated for the Pounce™ System. CDT was a primary treatment in 15 patients whose clots were located outside the Pounce™ System’s zone of treatment. As I mentioned, we performed CDT as a secondary treatment to improve initial results with the Pounce™ System in just 1 of 44 cases.
The study covered your first 44 uses of the Pounce™ System for lower extremity interventions. Did you see a change in your overall use of CDT during the study?
Prior to my use of the Pounce™ System, I would typically use thrombolytic therapy in about two-thirds to three-quarters of lower extremity ischemia cases. This rate dropped significantly when I began using the Pounce™ System and continued to drop as I accumulated experience with the device. The paper reports overall use of thrombolytic therapy in about one-third (36.4%) of cases but does not show the downward trajectory of my use of CDT during the study period.
What was your selection criteria for the Pounce™ device?
As I’ve said before, the “feel” of the clot tells you a lot about how easily it can be removed. Occlusions that are thrombus-dominant are easy to cross with a straight guidewire and can easily be treated with the Pounce™ System. In my experience, too many operators decide how to treat a patient’s leg without assessing the occlusion itself. A patient’s clinical history, important as it is, does not provide a definitive assessment of “age of thrombus,” and treatment decisions made solely based on history may exclude many patients who might benefit from addressing the thrombotic component of occlusions.
What else influenced your patient selection for the Pounce™ System?
Patient comorbidity is a crucial consideration. Many patients have multiple heart, lung, or kidney comorbidities that make them less than ideal for surgery or multiple contrast-requiring procedures, not to mention an interruption of their antiplatelet or anticoagulation medications. I’m hesitant to use treatments that may induce hemolysis or volume loss in these patients, and I’d much prefer to resolve their ischemia in a one-step procedure without thrombolytics. Given its simple mechanism of action, the Pounce™ System was less intimidating to me to use for such patients.
What was your treatment approach for patients with lesions that were not able to be traversed by a guidewire?
Failure of the wire to traverse the lesion easily doesn’t mean a patient cannot be treated with endovascular techniques; it just means thrombectomy may not be helpful. That goes for thrombolytics as well, since CDT works predominantly for fresh clot.6 Therefore, lesions that are not easily traversable with a guidewire can be treated as “plaque only,” or you may consider surgery in these cases. Likewise, if you can traverse the lesion but you do not retrieve any material via thrombectomy, in my experience this is predictive that surgical thrombectomy would be unsuccessful and that a bypass procedure may be necessary.
Keep in mind that most peripheral arterial occlusions are composed of thrombus and plaque. We have to think beyond coronary artery occlusion pathobiology, in which the fibrous cap of a plaque ruptures and the platelet plug forms, causing acute symptoms such as myocardial infarction. Leg symptoms can range from minimal to severe, with thrombus burden ranging from minimal to partial to predominate to complete. Balloon angioplasty alone can be helpful with minimal clot, as in a coronary artery, but is often ineffective in peripheral arterial occlusions. Therefore, my approach is to remove clot first, then treat the underlying plaque using tools designed to do that.
Although the patient population in this study included a full range of clot chronicity (as defined by duration of symptoms), most patients had a relatively low level of ischemic severity (74% Rutherford class 2a). Do you see this as a limitation of the study?
No, I see this as a strength. In my experience, Rutherford class 2a is associated with subacute or chronic clot, whereas Rutherford class 2b, although a higher level of ischemic severity, is associated with acute clot. I have found that any thrombectomy device can remove acute clot—you can just suck it out. There are not a lot of devices that can remove subacute or chronic material. This is an important consideration, as the data sets we have for other thrombectomy devices tend only to include patients with < 15 days of ischemia.2-5
How did your use of the Pounce™ System change over time?
The question with a new device is always, “when do I default back to what I know will work?” Initially, I used the Pounce™ device only for easily guidewire-traversable occlusions in the superficial femoral artery/popliteal segment and used thrombolytic therapy to treat concomitant tibial artery clot (the Pounce™ System is indicated for treatment of vessels 3.5-6 mm in diameter). With experience, my comfort zone expanded to include more appropriate-size tibial arteries than I initially tried to tackle with the device, and I developed a better feel for how much is enough in terms of clot removal. In general, I became less likely to revert to CDT and I became slower to put in a balloon—if you’re ballooning residual clot, sometimes that will embolize. So, my overall need for other modalities lessened as I accumulated experience with the Pounce™ System.
What was your typical approach to treating limb ischemia before using the Pounce™ System and to what degree, if any, did the availability of the Pounce™ device change this approach?
Prior to using the Pounce™ System, I would typically use mechanical thrombectomy to decrease the clot burden and then use thrombolytic therapy to clean up the residual thrombus. I had experience with most other mechanical devices on the market. The Pounce™ System quickly became my go-to device because it could minimize the need for thrombolytic therapy, thereby allowing many patients to be treated as outpatients. This helps to avoid hospitalization and subsequent next-day procedures.
The key to any treatment for ischemic limbs is reestablishing flow. The better the flow, the better the lysis and pain reduction for the patient. The Pounce™ System allowed me to reestablish robust flow earlier compared to other devices I’ve used.
*In the study, technical success of the Pounce™ System was defined as the effective removal of thrombus from the treated arterial segment in which it was used.
Caution: Federal (US) law restricts the Pounce™ Thrombectomy System to sale by or on the order of a physician. Please refer to the product’s Instructions for Use for indications, contraindications, warnings, and precautions. SURMODICS, POUNCE, and SURMODICS and POUNCE logos are trademarks of Surmodics, Inc. and/or its affiliates. Third-party trademarks are the property of their respective owners.
1. Gray BH, Wheibe E, Dicks AB, et al. Pounce thrombectomy system to treat acute and chronic peripheral arterial occlusions.Ann Vasc Surg. 2023;96:104-114. doi: 10.1016/j.avsg.2023.05.019
2. de Donato G, Pasqui E, Sponza M, et al. Safety and efficacy of vacuum assisted thrombo-aspiration in patients with acute lower limb ischaemia: the INDIAN trial.Eur J Vasc Endovas Surg. 2021;61:820-828. doi: 10.1016/j.ejvs.2021.01.004
3. Gandhi SS, Ewing JA, Cooper E, et al. Comparison of low-dose catheter-directed thrombolysis with and without pharmacomechanical thrombectomy for acute lower extremity ischemia.Ann Vasc Surg. 2018;46:178-186. doi: 10.1016/j.avsg.2017.07.008
4. Gong M, He X, Zhao B, et al. Endovascular revascularization strategies using catheter-based thrombectomy versus conventional catheter-directed thrombolysis for acute limb ischemia.Thromb J. 2021;19:96. doi: 10.1186/s12959-021-00349-9
5. Maldonado TS, Powell A, Wendorff H, et al. Safety and efficacy of mechanical aspiration thrombectomy at 30-days for patients with lower extremity acute limb ischemia (STRIDE).J Vasc Surg. Published online November 4, 2023. doi: 10.1016/j.jvs.2023.10.062
6. Results of a prospective randomized trial evaluating surgery versus thrombolysis for ischemia of the lower extremity. The STILE trial.Ann Surg. 1994;220:251-266. doi: 10.1097/00000658-199409000-00003

Advertisement
Advertisement