Jabs DA, Van Natta ML, Thorne JE, Weinberg DV, Meredith TA, Kuppermann BD, et al. Course of cytomegalovirus retinitis in the era of highly active antiretroviral therapy: 2. Second eye involvement and retinal detachment. Ophthalmology. 2004 Dec. 111 (12):2232-9. [QxMD MEDLINE Link].
Ude IN, Yeh S, Shantha JG. Cytomegalovirus retinitis in the highly active anti-retroviral therapy era. Ann Eye Sci. 2022 Mar. 7:9. [QxMD MEDLINE Link]. [Full Text].
Baumal CR, Levin AV, Read SE. Cytomegalovirus retinitis in immunosuppressed children. Am J Ophthalmol. 1999 May. 127 (5):550-8. [QxMD MEDLINE Link].
Freeman WR, Quiceno JI, Crapotta JA, Listhaus A, Munguia D, Aguilar MF. Surgical repair of rhegmatogenous retinal detachment in immunosuppressed patients with cytomegalovirus retinitis. Ophthalmology. 1992 Mar. 99 (3):466-74. [QxMD MEDLINE Link].
Foxworth MK 2nd, Wilms IR, Brookman RR, Crewe S, Adler SP. Prevalence of CMV infection among sexually active adolescents: a matched case-control study. Adolesc Health Med Ther. 2014. 5:73-8. [QxMD MEDLINE Link].
McAuliffe PF, Hall MJ, Castro-Malaspina H, Heinemann MH. Use of the ganciclovir implant for treating cytomegalovirus retinitis secondary to immunosuppression after bone marrow transplantation. Am J Ophthalmol. 1997 May. 123(5):702-3. [QxMD MEDLINE Link].
Hiwarkar P, Gajdosova E, Qasim W, Worth A, Breuer J, Chiesa R, et al. Frequent Occurrence of Cytomegalovirus Retinitis During Immune Reconstitution Warrants Regular Ophthalmic Screening in High-Risk Pediatric Allogeneic Hematopoietic Stem Cell Transplant Recipients. Clin Infect Dis. 2014 May 7. [QxMD MEDLINE Link].
Jeon S, Lee WK, Lee Y, Lee DG, Lee JW. Risk Factors for Cytomegalovirus Retinitis in Patients with Cytomegalovirus Viremia after Hematopoietic Stem Cell Transplantation. Ophthalmology. 2012 May 30. [QxMD MEDLINE Link].
Gangan PA, Besen G, Munguia D, Freeman WR. Macular serous exudation in patients with acquired immunodeficiency syndrome and cytomegalovirus retinitis. Am J Ophthalmol. 1994 Aug 15. 118 (2):212-9. [QxMD MEDLINE Link].
Murray HW, Knox DL, Green WR, Susel RM. Cytomegalovirus retinitis in adults. A manifestation of disseminated viral infection. Am J Med. 1977 Oct. 63(4):574-84. [QxMD MEDLINE Link].
Egbert PR, Pollard RB, Gallagher JG, Merigan TC. Cytomegalovirus retinitis in immunosuppressed hosts. II. Ocular manifestations. Ann Intern Med. 1980 Nov. 93(5):664-70. [QxMD MEDLINE Link].
Whitcup SM. Cytomegalovirus Retinitis in the Era of Highly Active Antiretroviral Therapy. JAMA. 2000. 283 No. 5:653-657.
Mitchell SM, Membrey WL, Youle MS, et al. Cytomegalovirus retinitis after the initiation of highly active antiretroviral therapy: a 2 year prospective study. Br J Ophthalmol. 1999 Jun. 83(6):652-5. [QxMD MEDLINE Link].
Zegans M, Marsh B, Walton RC. Cytomegalovirus retinitis in the era of highly active antiretroviral therapy. Int Ophthalmol Clin. 2000 Spring. 40(2):127-35. [QxMD MEDLINE Link].
Holbrook JT, Colvin R, van Natta ML, Thorne JE, Bardsley M, Jabs DA. Evaluation of the United States public health service guidelines for discontinuation of anticytomegalovirus therapy after immune recovery in patients with cytomegalovirus retinitis. Am J Ophthalmol. 2011 Oct. 152(4):628-637.e1. [QxMD MEDLINE Link]. [Full Text].
Oldfield EC 3rd. Evaluation of chronic diarrhea in patients with human immunodeficiency virus infection. Rev Gastroenterol Disord. 2002 Fall. 2 (4):176-88. [QxMD MEDLINE Link].
Baumal CR, Levin AV, Read SE. Cytomegalovirus retinitis in immunosuppressed children. Am J Ophthalmol. 1999 May. 127(5):550-8. [QxMD MEDLINE Link].
Sugar EA, Jabs DA, Ahuja A, Thorne JE, Danis RP, Meinert CL. Incidence of cytomegalovirus retinitis in the era of highly active antiretroviral therapy. Am J Ophthalmol. 2012 Jun. 153(6):1016-1024.e5. [QxMD MEDLINE Link]. [Full Text].
Kempen JH, Sugar EA, Lyon AT, Lewis RA, Jabs DA, Heinemann MH, et al. Risk of Cataract in Persons with Cytomegalovirus Retinitis and the Acquired Immune Deficiency Syndrome. Ophthalmology. 2012 Jul 30. [QxMD MEDLINE Link].
Knox CM, Chandler D, Short GA, Margolis TP. Polymerase chain reaction-based assays of vitreous samples for the diagnosis of viral retinitis. Use in diagnostic dilemmas. Ophthalmology. 1998 Jan. 105(1):37-44; discussion 44-5. [QxMD MEDLINE Link].
Grant AD, Djomand G, De Cock KM. Natural history and spectrum of disease in adults with HIV/AIDS in Africa. AIDS. 1997. 11 Suppl B:S43-54. [QxMD MEDLINE Link].
Kestelyn P. The epidemiology of CMV retinitis in Africa. Ocul Immunol Inflamm. 1999 Dec. 7(3-4):173-7. [QxMD MEDLINE Link].
Heiden D, Saranchuk P. CMV retinitis in China and SE Asia: the way forward. BMC Infect Dis. 2011 Nov 24. 11:327. [QxMD MEDLINE Link]. [Full Text].
Gross JG, Bozzette SA, Mathews WC, et al. Longitudinal study of cytomegalovirus retinitis in acquired immune deficiency syndrome. Ophthalmology. 1990 May. 97(5):681-6. [QxMD MEDLINE Link].
Lim JI, Enger C, Haller JA, et al. Improved visual results after surgical repair of cytomegalovirus- related retinal detachments. Ophthalmology. 1994 Feb. 101(2):264-9. [QxMD MEDLINE Link].
Studies of Ocular Complications of AIDS (SOCA) Research Group. Foscarnet-Ganciclovir Cytomegalovirus Retinitis Trial. 4. Visual outcomes. Studies of Ocular Complications of AIDS Research Group in collaboration with the AIDS Clinical Trials Group. Ophthalmology. 1994 Jul. 101(7):1250-61. [QxMD MEDLINE Link].
Thorne JE, Holbrook JT, Jabs DA, Kempen JH, Nichols C, Meinert CL. Effect of cytomegalovirus retinitis on the risk of visual acuity loss among patients with AIDS. Ophthalmology. 2007 Mar. 114(3):591-8. [QxMD MEDLINE Link].
Holbrook JT, Jabs DA, Weinberg DV. Visual loss in patients with cytomegalovirus retinitis and acquired immunodeficiency syndrome before widespread availability of highly active antiretroviral therapy. Arch Ophthalmol. 2003 Jan. 121(1):99-107. [QxMD MEDLINE Link].
Studies of Ocular Complications of AIDS (SOCA) Research Group. Rhegmatogenous retinal detachment in patients with cytomegalovirus retinitis: the Foscarnet-Ganciclovir Cytomegalovirus Retinitis Trial. The Studies of Ocular Complications of AIDS (SOCA) Research Group in Collaboration with the AIDS Clinical Trials G. Am J Ophthalmol. 1997 Jul. 124(1):61-70. [QxMD MEDLINE Link].
Sandy CJ, Bloom PA, Graham EM, et al. Retinal detachment in AIDS-related cytomegalovirus retinitis. Eye. 1995. 9 ( Pt 3):277-81. [QxMD MEDLINE Link].
Boyraz-Ikiz HD, Witmer JP, Frissen PH. Cytomegalovirus (re)activation plays no role in the ocular vitritis observed after initiation of highly active antiretroviral therapy. AIDS. 1999 May 7. 13(7):867. [QxMD MEDLINE Link].
Holland GN. New issues in the management of patients with AIDS-related cytomegalovirus retinitis. Arch Ophthalmol. 2000 May. 118(5):704-6. [QxMD MEDLINE Link].
Kempen JH, Min YI, Freeman WR, Holland GN, Friedberg DN, Dieterich DT, et al. Risk of immune recovery uveitis in patients with AIDS and cytomegalovirus retinitis. Ophthalmology. 2006 Apr. 113(4):684-94. [QxMD MEDLINE Link].
Karavellas MP, Plummer DJ, Macdonald JC, et al. Incidence of immune recovery vitritis in cytomegalovirus retinitis patients following institution of successful highly active antiretroviral therapy. J Infect Dis. 1999 Mar. 179(3):697-700. [QxMD MEDLINE Link].
Nguyen QD, Kempen JH, Bolton SG, et al. Immune recovery uveitis in patients with AIDS and cytomegalovirus retinitis after highly active antiretroviral therapy. Am J Ophthalmol. 2000 May. 129(5):634-9. [QxMD MEDLINE Link].
Ruiz-Cruz M, Barrera CA, Ablanedo-Terrazas Y, Reyes-Terán G. Proposed Clinical Case Definition for Cytomegalovirus-Immune Recovery Retinitis. Clin Infect Dis. 2014 Apr 24. [QxMD MEDLINE Link].
Jabs DA, Ahuja A, Van Natta M, Lyon A, Srivastava S, Gangaputra S. Course of cytomegalovirus retinitis in the era of highly active antiretroviral therapy: five-year outcomes. Ophthalmology. 2010 Nov. 117(11):2152-61.e1-2. [QxMD MEDLINE Link].
Bowen EF, Griffiths PD, Davey CC, et al. Lessons from the natural history of cytomegalovirus. AIDS. 1996 Nov. 10 Suppl 1:S37-41. [QxMD MEDLINE Link].
Bowen EF, Wilson P, Atkins M, et al. Natural history of untreated cytomegalovirus retinitis. Lancet. 1995 Dec 23-30. 346(8991-8992):1671-3. [QxMD MEDLINE Link].
Bloom PA, Sandy CJ, Migdal CS, et al. Visual prognosis of AIDS patients with cytomegalovirus retinitis. Eye. 1995. 9 ( Pt 6):697-702. [QxMD MEDLINE Link].
McCutchan JA. Clinical impact of cytomegalovirus infections of the nervous system in patients with AIDS. Clin Infect Dis. 1995 Oct. 21 Suppl 2:S196-201. [QxMD MEDLINE Link].
McCutchan JA. Cytomegalovirus infections of the nervous system in patients with AIDS. Clin Infect Dis. 1995 Apr. 20(4):747-54. [QxMD MEDLINE Link].
Brody JM, Butrus SI, Laby DM, et al. Anterior segment findings in AIDS patients with cytomegalovirus retinitis. Graefes Arch Clin Exp Ophthalmol. 1995 Jun. 233(6):374-6. [QxMD MEDLINE Link].
Biswas J, Madhavan HN, George AE, et al. Ocular lesions associated with HIV infection in India: a series of 100 consecutive patients evaluated at a referral center. Am J Ophthalmol. 2000 Jan. 129(1):9-15. [QxMD MEDLINE Link].
Studies of Ocular Complications of AIDS (SOCA) Research Group. Foscarnet-Ganciclovir Cytomegalovirus Retinitis Trial: 5. Clinical features of cytomegalovirus retinitis at diagnosis. Studies of ocular complications of AIDS Research Group in collaboration with the AIDS Clinical Trials Group. Am J Ophthalmol. 1997 Aug. 124(2):141-57. [QxMD MEDLINE Link].
Biswas J, Raizada S, Gopal L, et al. Bilateral frosted branch angiitis and cytomegalovirus retinitis in acquired immunodeficiency syndrome. Indian J Ophthalmol. 1999 Sep. 47(3):195-7. [QxMD MEDLINE Link].
Mansour AM, Li HK. Frosted retinal periphlebitis in the acquired immunodeficiency syndrome. Ophthalmologica. 1993. 207(4):182-6. [QxMD MEDLINE Link].
Saran BR, Pomilla PV. Retinal vascular nonperfusion and retinal neovascularization as a consequence of cytomegalovirus retinitis and cryptococcal choroiditis. Retina. 1996. 16(6):510-2. [QxMD MEDLINE Link].
Mansor AM, Li HK. Cytomegalovirus optic neuritis: characteristics, therapy and survival. Ophthalmologica. 1995. 209(5):260-6. [QxMD MEDLINE Link].
Kempen JH, Jabs DA, Wilson LA. Risk of vision loss in patients with cytomegalovirus retinitis and the acquired immunodeficiency syndrome. Arch Ophthalmol. 2003 Apr. 121(4):466-76. [QxMD MEDLINE Link].
Kempen JH, Jabs DA, Wilson LA. Incidence of cytomegalovirus (CMV) retinitis in second eyes of patients with the acquired immune deficiency syndrome and unilateral CMV retinitis. Am J Ophthalmol. 2005 Jun. 139(6):1028-34. [QxMD MEDLINE Link].
Pertel P, Hirschtick R, Phair J, et al. Risk of developing cytomegalovirus retinitis in persons infected with the human immunodeficiency virus. J Acquir Immune Defic Syndr. 1992. 5(11):1069-74. [QxMD MEDLINE Link].
Nasir MA, Jaffe GJ. Cytomegalovirus retinitis associated with Hodgkin''s disease. Retina. 1996. 16(4):324-7. [QxMD MEDLINE Link].
Holland GN, Vaudaux JD, Jeng SM, Yu F, Goldenberg DT, Folz IC, et al. Characteristics of untreated AIDS-related cytomegalovirus retinitis. I. Findings before the era of highly active antiretroviral therapy (1988 to 1994). Am J Ophthalmol. 2008 Jan. 145(1):5-11. [QxMD MEDLINE Link].
Holland GN, Vaudaux JD, Shiramizu KM, Yu F, Goldenberg DT, Gupta A, et al. Characteristics of untreated AIDS-related cytomegalovirus retinitis. II. Findings in the era of highly active antiretroviral therapy (1997 to 2000). Am J Ophthalmol. 2008 Jan. 145(1):12-22. [QxMD MEDLINE Link].
Davis JL, Hummer J, Feuer WJ. Laser photocoagulation for retinal detachments and retinal tears in cytomegalovirus retinitis. Ophthalmology. 1997 Dec. 104(12):2053-60; discussion 2060-1. [QxMD MEDLINE Link].
Ross SA, Novak Z, Pati S, Boppana SB. Overview of the diagnosis of cytomegalovirus infection. Infect Disord Drug Targets. 2011 Oct. 11 (5):466-74. [QxMD MEDLINE Link].
Hu H, Jabs DA, Forman MS, Martin BK, Dunn JP, Weinberg DV, et al. Comparison of cytomegalovirus (CMV) UL97 gene sequences in the blood and vitreous of patients with acquired immunodeficiency syndrome and CMV retinitis. J Infect Dis. 2002 Apr 1. 185 (7):861-7. [QxMD MEDLINE Link].
Jabs DA, Martin BK, Forman MS, Ricks MO, Cytomegalovirus Retinitis and Viral Resistance Research Group. Cytomegalovirus (CMV) blood DNA load, CMV retinitis progression, and occurrence of resistant CMV in patients with CMV retinitis. J Infect Dis. 2005 Aug 15. 192 (4):640-9. [QxMD MEDLINE Link].
Liu Y, Chen AS, Kamphaengkham S, Leenasirimakul P, Jirawison C, Ausayakhun S, et al. Diagnostic Utility of Ocular Symptoms and Vision for Cytomegalovirus Retinitis. PLoS One. 2016. 11 (10):e0165564. [QxMD MEDLINE Link].
Phillips AN, Lazzarin A, Gonzales-Lahoz J, et al. Factors associated with the CD4+ lymphocyte count at diagnosis of acquired immunodeficiency syndrome. The AIDS IN EUROPE Study Group. J Clin Epidemiol. 1996 Nov. 49(11):1253-8. [QxMD MEDLINE Link].
Baldassano V, Dunn JP, Feinberg J, Jabs DA. Cytomegalovirus retinitis and low CD4+ T-lymphocyte counts. N Engl J Med. 1995 Sep 7. 333(10):670. [QxMD MEDLINE Link].
Sandy CJ, Ferris JD, Bloom PA, et al. Screening for cytomegalovirus retinitis in HIV-positive and AIDS patients. QJM. 1995 Dec. 88(12):899-903. [QxMD MEDLINE Link].
Holbrook JT, Davis MD, Hubbard LD, et al. Risk factors for advancement of cytomegalovirus retinitis in patients with acquired immunodeficiency syndrome. Studies of Ocular Complications of AIDS Research Group. Arch Ophthalmol. 2000 Sep. 118(9):1196-204. [QxMD MEDLINE Link].
Chernoff DN, Miner RC, Hoo BS, et al. Quantification of cytomegalovirus DNA in peripheral blood leukocytes by a branched-DNA signal amplification assay. J Clin Microbiol. 1997 Nov. 35(11):2740-4. [QxMD MEDLINE Link].
Rasmussen L, Morris S, Zipeto D, et al. Quantitation of human cytomegalovirus DNA from peripheral blood cells of human immunodeficiency virus-infected patients could predict cytomegalovirus retinitis. J Infect Dis. 1995 Jan. 171(1):177-82. [QxMD MEDLINE Link].
Tufail A, Moe AA, Miller MJ, et al. Quantitative cytomegalovirus DNA level in the blood and its relationship to cytomegalovirus retinitis in patients with acquired immune deficiency syndrome. Ophthalmology. 1999 Jan. 106(1):133-41. [QxMD MEDLINE Link].
Wattanamano P, Clayton JL, Kopicko JJ, et al. Comparison of three assays for cytomegalovirus detection in AIDS patients at risk for retinitis. J Clin Microbiol. 2000 Feb. 38(2):727-32. [QxMD MEDLINE Link].
Liu JH, Hsu WM, Wong WW, et al. Using conjunctival swab with polymerase chain reaction to aid diagnosis of cytomegalovirus retinitis in AIDS patients. Ophthalmologica. 2000. 214(2):126-30. [QxMD MEDLINE Link].
Sugita S, Shimizu N, Watanabe K, Mizukami M, Morio T, Sugamoto Y, et al. Use of multiplex PCR and real-time PCR to detect human herpes virus genome in ocular fluids of patients with uveitis. Br J Ophthalmol. 2008 Jul. 92(7):928-32. [QxMD MEDLINE Link].
Fuchs AV, Wolf E, Scheider A, Jager H, Kampik A. [Cytomegalovirus (CMV) retinitis in AIDS. Gancilovir implantation in comparison with systemic therapy]. Ophthalmologe. 1999 Jan. 96(1):11-5. [QxMD MEDLINE Link].
Musch DC, Martin DF, Gordon JF, et al. Treatment of cytomegalovirus retinitis with a sustained-release ganciclovir implant. The Ganciclovir Implant Study Group. N Engl J Med. 1997 Jul 10. 337(2):83-90. [QxMD MEDLINE Link].
Guembel HO, Krieglsteiner S, Rosenkranz C, et al. Complications after implantation of intraocular devices in patients with cytomegalovirus retinitis. Graefes Arch Clin Exp Ophthalmol. 1999 Oct. 237(10):824-9. [QxMD MEDLINE Link].
Oktavec KC, Nolan K, Brown DM, Dunn JP, Livingston AG, Thorne JE. Clinical outcomes in patients with cytomegalovirus retinitis treated with ganciclovir implant. Am J Ophthalmol. 2012 Apr. 153(4):728-33, 733.e1-2. [QxMD MEDLINE Link].
Boyer DS, Posalski J. Potential complication associated with removal of ganciclovir implants. Am J Ophthalmol. 1999 Mar. 127(3):349-50. [QxMD MEDLINE Link].
Freeman WR, Friedberg DN, Berry C, et al. Risk factors for development of rhegmatogenous retinal detachment in patients with cytomegalovirus retinitis. Am J Ophthalmol. 1993 Dec 15. 116(6):713-20. [QxMD MEDLINE Link].
Baumal CR, Reichel E. Management of cytomegalovirus-related rhegmatogenous retinal detachments. Ophthalmic Surg Lasers. 1998 Nov. 29(11):916-25. [QxMD MEDLINE Link].
Davis JL, Serfass MS, Lai MY, et al. Silicone oil in repair of retinal detachments caused by necrotizing retinitis in HIV infection. Arch Ophthalmol. 1995 Nov. 113(11):1401-9. [QxMD MEDLINE Link].
Freeman WR. Retinal detachment in cytomegalovirus retinitis: should our approach be changed?. Retina. 1999. 19(4):271-3. [QxMD MEDLINE Link].
Ross WH, Bryan JS, Barloon AS. Management of retinal detachments secondary to cytomegalovirus retinitis. Can J Ophthalmol. 1994 Jun. 29(3):129-33. [QxMD MEDLINE Link].
Diaz-Llopis M, España E, Muñoz G, Navea A, Chipont E, Cano J, et al. High dose intravitreal foscarnet in the treatment of cytomegalovirus retinitis in AIDS. Br J Ophthalmol. 1994 Feb. 78 (2):120-4. [QxMD MEDLINE Link].
Kirsch LS, Arevalo JF, De Clercq E, Chavez de la Paz E, Munguia D, Garcia R, et al. Phase I/II study of intravitreal cidofovir for the treatment of cytomegalovirus retinitis in patients with the acquired immunodeficiency syndrome. Am J Ophthalmol. 1995 Apr. 119 (4):466-76. [QxMD MEDLINE Link].
Erice A, Jordan MC, Chace BA, et al. Ganciclovir treatment of cytomegalovirus disease in transplant recipients and other immunocompromised hosts. JAMA. 1987 Jun 12. 257(22):3082-7. [QxMD MEDLINE Link].
Jensen OA, Gerstoft J, Thomsen HK, Marner K. Cytomegalovirus retinitis in the acquired immunodeficiency syndrome (AIDS). Light-microscopical, ultrastructural and immunohistochemical examination of a case. Acta Ophthalmol (Copenh). 1984 Feb. 62(1):1-9. [QxMD MEDLINE Link].
Pecorella I, Ciardi A, Credendino A, et al. Ocular, cerebral and systemic interrelationships of cytomegalovirus infection in a post-mortem study of AIDS patients. Eye. 1999 Dec. 13 ( Pt 6):781-5. [QxMD MEDLINE Link].
Jabs DA, Van Natta ML, Holbrook JT, Kempen JH, Meinert CL, Davis MD. Longitudinal study of the ocular complications of AIDS: 2. Ocular examination results at enrollment. Ophthalmology. 2007 Apr. 114(4):787-93. [QxMD MEDLINE Link].
Jabs DA, Van Natta ML, Thorne JE, et al. Course of cytomegalovirus retinitis in the era of highly active antiretroviral therapy: 1. Retinitis progression. Ophthalmology. 2004 Dec. 111(12):2224-31. [QxMD MEDLINE Link].
Jabs DA, Van Natta ML, Thorne JE, et al. Course of cytomegalovirus retinitis in the era of highly active antiretroviral therapy: 2. Second eye involvement and retinal detachment. Ophthalmology. 2004 Dec. 111(12):2232-9. [QxMD MEDLINE Link].
Banker AS. Posterior segment manifestations of human immunodeficiency virus/acquired immune deficiency syndrome. Indian J Ophthalmol. 2008 Sep-Oct. 56 (5):377-83. [QxMD MEDLINE Link].
Wong JX, Wong EP, Teoh SC. Outcomes of cytomegalovirus retinitis-related retinal detachment surgery in acquired immunodeficiency syndrome patients in an Asian population. BMC Ophthalmol. 2014 Nov 27. 14:150. [QxMD MEDLINE Link].
Stewart MW. Optimal management of cytomegalovirus retinitis in patients with AIDS. Clin Ophthalmol. 2010 Apr 26. 4:285-99. [QxMD MEDLINE Link].
Tasiopoulou A, Urzua CA, Lightman S. Successful treatment of cytomegalovirus retinitis with oral/intravitreal antivirals in HIV-negative patients with lymphoma. Eye (Lond). 2022 Oct 3. [QxMD MEDLINE Link].
D'Aquila R, Walker B. Exploring the benefits and limits of highly active antiretroviral therapy. JAMA. 1999 Nov 3. 282(17):1668-9. [QxMD MEDLINE Link].
Doan S, Cochereau I, Guvenisik N, et al. Cytomegalovirus retinitis in HIV-infected patients with and without highly active antiretroviral therapy. Am J Ophthalmol. 1999 Aug. 128(2):250-1. [QxMD MEDLINE Link].
Kedhar SR, Jabs DA. Cytomegalovirus retinitis in the era of highly active antiretroviral therapy. Herpes. 2007 Dec. 14(3):66-71. [QxMD MEDLINE Link].
Macdonald JC, Torriani FJ, Morse LS, et al. Lack of reactivation of cytomegalovirus (CMV) retinitis after stopping CMV maintenance therapy in AIDS patients with sustained elevations in CD4 T cells in response to highly active antiretroviral therapy. J Infect Dis. 1998 May. 177(5):1182-7. [QxMD MEDLINE Link].
Margolis TP. Discontinuation of anticytomegalovirus therapy in patients with HIV infection and cytomegalovirus retinitis. Surv Ophthalmol. 2000 Mar-Apr. 44(5):455. [QxMD MEDLINE Link].
Soriano V, Dona C, Rodriguez-Rosado R, et al. Discontinuation of secondary prophylaxis for opportunistic infections in HIV-infected patients receiving highly active antiretroviral therapy. AIDS. 2000 Mar 10. 14(4):383-6. [QxMD MEDLINE Link].
Nasemann JE, Mutsch A, Wiltfang R, Klauss V. Early pars plana vitrectomy without buckling procedure in cytomegalovirus retinitis-induced retinal detachment. Retina. 1995. 15(2):111-6. [QxMD MEDLINE Link].
Althaus C, Loeffler KU, Schimkat M, et al. Prophylactic argon laser coagulation for rhegmatogenous retinal detachment in AIDS patients with cytomegalovirus retinitis. Graefes Arch Clin Exp Ophthalmol. 1998 May. 236(5):359-64. [QxMD MEDLINE Link].
Meffert SA, Ai E. Laser photocoagulation prophylaxis for CMV retinal detachments. Ophthalmology. 1998 Aug. 105(8):1353-5. [QxMD MEDLINE Link].
Martin DF, Dunn JP, Davis JL, et al. Use of the ganciclovir implant for the treatment of cytomegalovirus retinitis in the era of potent antiretroviral therapy: recommendations of the International AIDS Society-USA panel. Am J Ophthalmol. 1999 Mar. 127(3):329-39. [QxMD MEDLINE Link].
Sanborn GE, Anand R, Torti RE, et al. Sustained-release ganciclovir therapy for treatment of cytomegalovirus retinitis. Use of an intravitreal device. Arch Ophthalmol. 1992 Feb. 110(2):188-95. [QxMD MEDLINE Link].
Martin DF, Ferris FL, Parks DJ, et al. Ganciclovir implant exchange. Timing, surgical procedure, and complications. Arch Ophthalmol. 1997 Nov. 115(11):1389-94. [QxMD MEDLINE Link].
Roth DB, Feuer WJ, Blenke AJ, Davis JL. Treatment of recurrent cytomegalovirus retinitis with the ganciclovir implant. Am J Ophthalmol. 1999 Mar. 127(3):276-82. [QxMD MEDLINE Link].
Lim JI, Wolitz RA, Dowling AH, et al. Visual and anatomic outcomes associated with posterior segment complications after ganciclovir implant procedures in patients with AIDS and cytomegalovirus retinitis. Am J Ophthalmol. 1999 Mar. 127(3):288-93. [QxMD MEDLINE Link].
Desatnik HR, Foster RE, Lowder CY. Treatment of clinically resistant cytomegalovirus retinitis with combined intravitreal injections of ganciclovir and foscarnet. Am J Ophthalmol. 1996 Jul. 122(1):121-3. [QxMD MEDLINE Link].
Agarwal A, Kumari N, Trehan A, Khadwal A, Dogra MR, Gupta V, et al. Outcome of cytomegalovirus retinitis in immunocompromised patients without Human Immunodeficiency Virus treated with intravitreal ganciclovir injection. Graefes Arch Clin Exp Ophthalmol. 2014 Feb 21. [QxMD MEDLINE Link].
Gilbert C, Handfield J, Toma E, et al. Emergence and prevalence of cytomegalovirus UL97 mutations associated with ganciclovir resistance in AIDS patients. AIDS. 1998 Jan 22. 12(2):125-9. [QxMD MEDLINE Link].
Jabs DA, Enger C, Dunn JP, et al. Cytomegalovirus retinitis and viral resistance: 3. Culture results. CMV Retinitis and Viral Resistance Study Group. Am J Ophthalmol. 1998 Oct. 126(4):543-9. [QxMD MEDLINE Link].
Jabs DA, Enger C, Forman M, et al. Incidence of foscarnet resistance and cidofovir resistance in patients treated for cytomegalovirus retinitis. The Cytomegalovirus Retinitis and Viral Resistance Study Group. Antimicrob Agents Chemother. 1998 Sep. 42(9):2240-4. [QxMD MEDLINE Link].
Hardy WD. Combined ganciclovir and recombinant human granulocyte-macrophage colony-stimulating factor in the treatment of cytomegalovirus retinitis in AIDS patients. J Acquir Immune Defic Syndr. 1991. 4 Suppl 1:S22-8. [QxMD MEDLINE Link].
Hardy WD. Management strategies for patients with cytomegalovirus retinitis. J Acquir Immune Defic Syndr Hum Retrovirol. 1997. 14 Suppl 1:S7-12. [QxMD MEDLINE Link].
Jacobson MA, Wilson S, Stanley H, et al. Phase I study of combination therapy with intravenous cidofovir and oral ganciclovir for cytomegalovirus retinitis in patients with AIDS. Clin Infect Dis. 1999 Mar. 28(3):528-33. [QxMD MEDLINE Link].
Jabs DA. Design of clinical trials for drug combinations: cytomegalovirus retinitis--foscarnet and ganciclovir. The CMV retinitis retreatment trial. Antiviral Res. 1996 Jan. 29(1):69-71. [QxMD MEDLINE Link].
Spector SA, Weingeist T, Pollard RB, Dieterich DT, Samo T, Benson CA, et al. A randomized, controlled study of intravenous ganciclovir therapy for cytomegalovirus peripheral retinitis in patients with AIDS. AIDS Clinical Trials Group and Cytomegalovirus Cooperative Study Group. J Infect Dis. 1993 Sep. 168 (3):557-63. [QxMD MEDLINE Link].
Gane E, Saliba F, Valdecasas GJ, O'Grady J, Pescovitz MD, Lyman S, et al. Randomised trial of efficacy and safety of oral ganciclovir in the prevention of cytomegalovirus disease in liver-transplant recipients. The Oral Ganciclovir International Transplantation Study Group [corrected]. Lancet. 1997 Dec 13. 350 (9093):1729-33. [QxMD MEDLINE Link].
Nishijima T, Yashiro S, Teruya K, Kikuchi Y, Katai N, Oka S, et al. Routine Eye Screening by an Ophthalmologist Is Clinically Useful for HIV-1-Infected Patients with CD4 Count Less than 200 /μL. PLoS One. 2015. 10 (9):e0136747. [QxMD MEDLINE Link].
Akerele T, Lightman S. Current and novel agents for the treatment of cytomegalovirus retinitis. Drugs R D. 1999 Nov. 2(5):289-97. [QxMD MEDLINE Link].
Holland GN. Treatment options for cytomegalovirus retinitis: a time for reassessment. Arch Ophthalmol. 1999 Nov. 117(11):1549-50. [QxMD MEDLINE Link].
Whitley RJ, Jacobson MA, Friedberg DN, et al. Guidelines for the treatment of cytomegalovirus diseases in patients with AIDS in the era of potent antiretroviral therapy: recommendations of an international panel. International AIDS Society-USA. Arch Intern Med. 1998 May 11. 158(9):957-69. [QxMD MEDLINE Link].
Marwick C. First "antisense" drug will treat CMV retinitis. JAMA. 1998 Sep 9. 280(10):871. [QxMD MEDLINE Link].
Studies of Ocular Complications of AIDS (SOCA) Research Group. Cytomegalovirus (CMV) culture results, drug resistance, and clinical outcome in patients with AIDS and CMV retinitis treated with foscarnet or ganciclovir. Studies of Ocular Complications of AIDS (SOCA) in collaboration with the AIDS Clinical Trial Gr. J Infect Dis. 1997 Jul. 176(1):50-8. [QxMD MEDLINE Link].
Drew WL, Ives D, Lalezari JP, et al. Oral ganciclovir as maintenance treatment for cytomegalovirus retinitis in patients with AIDS. Syntex Cooperative Oral Ganciclovir Study Group. N Engl J Med. 1995 Sep 7. 333(10):615-20. [QxMD MEDLINE Link].
Holland GN, Buhles WC Jr, Mastre B, Kaplan HJ. A controlled retrospective study of ganciclovir treatment for cytomegalovirus retinopathy. Use of a standardized system for the assessment of disease outcome. UCLA CMV Retinopathy. Study Group. Arch Ophthalmol. 1989 Dec. 107(12):1759-66. [QxMD MEDLINE Link].
Kuppermann BD, Quiceno JI, Flores-Aguilar M, et al. Intravitreal ganciclovir concentration after intravenous administration in AIDS patients with cytomegalovirus retinitis: implications for therapy. J Infect Dis. 1993 Dec. 168(6):1506-9. [QxMD MEDLINE Link].
Goldberg DE, Wang H, Azen SP. Long term visual outcome of patients with cytomegalovirus retinitis treated with highly active antiretroviral therapy. Br J Ophthalmol. 2003 Jul. 87(7):853-5. [QxMD MEDLINE Link].
Whitcup SM. Cytomegalovirus retinitis in the era of highly active antiretroviral therapy. JAMA. 2000 Feb 2. 283(5):653-7. [QxMD MEDLINE Link].
Whitcup, SM, Fortin, E, Linblad, AS. Discontinuation of Anticytomegalovirus Therapy in Patients With HIV Infection and Cytomegalovirus Retinits. JAMA. 1999. 282:1633-1637.
Martin DF, Sierra-Madero J, Walmsley S. A controlled trial of valganciclovir as induction therapy for cytomegalovirus retinitis. N Engl J Med. 2002 Apr 11. 346(15):1119-26. [QxMD MEDLINE Link].
Brown F, Banken L, Saywell K, Arum I. Pharmacokinetics of valganciclovir and ganciclovir following multiple oral dosages of valganciclovir in HIV- and CMV-seropositive volunteers. Clin Pharmacokinet. 1999 Aug. 37(2):167-76. [QxMD MEDLINE Link].
Stalder N, Sudre P, Olmari M, et al. Cytomegalovirus retinitis: decreased risk of bilaterality with increased use of systemic treatment. Swiss HIV Cohort Study Group. Clin Infect Dis. 1997 Apr. 24(4):620-4. [QxMD MEDLINE Link].
Spector SA, Busch DF, Follansbee S, et al. Pharmacokinetic, safety, and antiviral profiles of oral ganciclovir in persons infected with human immunodeficiency virus: a phase I/II study. AIDS Clinical Trials Group, and Cytomegalovirus Cooperative Study Group. J Infect Dis. 1995 Jun. 171(6):1431-7. [QxMD MEDLINE Link].
Spector SA, McKinley GF, Lalezari JP, et al. Oral ganciclovir for the prevention of cytomegalovirus disease in persons with AIDS. Roche Cooperative Oral Ganciclovir Study Group. N Engl J Med. 1996 Jun 6. 334(23):1491-7. [QxMD MEDLINE Link].
Squires KE. Oral ganciclovir for cytomegalovirus retinitis in patients with AIDS: results of two randomized studies. AIDS. 1996 Dec. 10 Suppl 4:S13-8. [QxMD MEDLINE Link].
Cvetkovic RS, Wellington K. Valganciclovir: a review of its use in the management of CMV infection and disease in immunocompromised patients. Drugs. 2005. 65(6):859-78. [QxMD MEDLINE Link].
Danner SA, Matheron S. Cytomegalovirus retinitis in AIDS patients: a comparative study of intravenous and oral ganciclovir as maintenance therapy. AIDS. 1996 Dec. 10 Suppl 4:S7-11. [QxMD MEDLINE Link].
Spector SA, Weingeist T, Pollard RB, et al. A randomized, controlled study of intravenous ganciclovir therapy for cytomegalovirus peripheral retinitis in patients with AIDS. AIDS Clinical Trials Group and Cytomegalovirus Cooperative Study Group. J Infect Dis. 1993 Sep. 168(3):557-63. [QxMD MEDLINE Link].
Lietman PS. Clinical pharmacology: foscarnet. Am J Med. 1992 Feb 14. 92(2A):8S-11S. [QxMD MEDLINE Link].
Lalezari JP. Cidofovir: a new therapy for cytomegalovirus retinitis. J Acquir Immune Defic Syndr Hum Retrovirol. 1997. 14 Suppl 1:S22-6. [QxMD MEDLINE Link].
Lalezari JP, Holland GN, Kramer F, et al. Randomized, controlled study of the safety and efficacy of intravenous cidofovir for the treatment of relapsing cytomegalovirus retinitis in patients with AIDS. J Acquir Immune Defic Syndr Hum Retrovirol. 1998 Apr 1. 17(4):339-44. [QxMD MEDLINE Link].
Plosker GL, Noble S. Cidofovir: a review of its use in cytomegalovirus retinitis in patients with AIDS. Drugs. 1999 Aug. 58(2):325-45. [QxMD MEDLINE Link].
Rahhal FM, Arevalo JF, Munguia D, et al. Intravitreal cidofovir for the maintenance treatment of cytomegalovirus retinitis. Ophthalmology. 1996 Jul. 103(7):1078-83. [QxMD MEDLINE Link].
Studies of Ocular Complications of AIDS (SOCA) Research Group. Parenteral cidofovir for cytomegalovirus retinitis in patients with AIDS: the HPMPC peripheral cytomegalovirus retinitis trial. A randomized, controlled trial. Studies of Ocular complications of AIDS Research Group in Collaboration with the AIDS Clini. Ann Intern Med. 1997 Feb 15. 126(4):264-74. [QxMD MEDLINE Link].
Drusano GL, Aweeka F, Gambertoglio J, et al. Relationship between foscarnet exposure, baseline cytomegalovirus (CMV) blood culture and the time to progression of CMV retinitis in HIV- positive patients. AIDS. 1996 Sep. 10(10):1113-9. [QxMD MEDLINE Link].
Harb GE, Bacchetti P, Jacobson MA. Survival of patients with AIDS and cytomegalovirus disease treated with ganciclovir or foscarnet. AIDS. 1991 Aug. 5(8):959-65. [QxMD MEDLINE Link].
Jabs DA. Controversies in the treatment of cytomegalovirus retinitis: foscarnet versus ganciclovir. Infect Agents Dis. 1995 Sep. 4(3):131-42. [QxMD MEDLINE Link].
Ambati J, Wynne KB, Angerame MC, Robinson MR. Anterior uveitis associated with intravenous cidofovir use in patients with cytomegalovirus retinitis. Br J Ophthalmol. 1999 Oct. 83(10):1153-8. [QxMD MEDLINE Link].
Cochereau I, Doan S, Diraison MC, et al. Uveitis in patients treated with intravenous cidofovir. Ocul Immunol Inflamm. 1999 Dec. 7(3-4):223-9. [QxMD MEDLINE Link].
Studies of Ocular Complications of AIDS (SOCA) Research Group. Morbidity and toxic effects associated with ganciclovir or foscarnet therapy in a randomized cytomegalovirus retinitis trial. Studies of ocular complications of AIDS Research Group, in collaboration with the AIDS Clinical Trials Group. Arch Intern Med. 1995 Jan 9. 155(1):65-74. [QxMD MEDLINE Link].
Tseng AL, Mortimer CB, Salit IE. Iritis associated with intravenous cidofovir. Ann Pharmacother. 1999 Feb. 33(2):167-71. [QxMD MEDLINE Link].
Studies of Ocular Complications of AIDS (SOCA) Research Group. Combination foscarnet and ganciclovir therapy vs monotherapy for the treatment of relapsed cytomegalovirus retinitis in patients with AIDS. The Cytomegalovirus Retreatment Trial. The Studies of Ocular Complications of AIDS Research Group in Collaborat. Arch Ophthalmol. 1996 Jan. 114(1):23-33. [QxMD MEDLINE Link].
Studies of Ocular Complications of AIDS (SOCA) Research Group. MSL-109 adjuvant therapy for cytomegalovirus retinitis in patients with acquired immunodeficiency syndrome: the Monoclonal Antibody Cytomegalovirus Retinitis Trial. The Studies of Ocular Complications of AIDS Research Group. AIDS Clinical Trials Group. Arch Ophthalmol. 1997 Dec. 115(12):1528-36. [QxMD MEDLINE Link].
Walsh JC, Jones CD, Barnes EA, et al. Increasing survival in AIDS patients with cytomegalovirus retinitis treated with combination antiretroviral therapy including HIV protease inhibitors. AIDS. 1998 Apr 16. 12(6):613-8. [QxMD MEDLINE Link].
Martin DF, Kuppermann BD, Wolitz RA, et al. Oral ganciclovir for patients with cytomegalovirus retinitis treated with a ganciclovir implant. Roche Ganciclovir Study Group. N Engl J Med. 1999 Apr 8. 340(14):1063-70. [QxMD MEDLINE Link].
Slatter MA, Gennery AR. Advances in the treatment of severe combined immunodeficiency. Clin Immunol. 2022 Sep. 242:109084. [QxMD MEDLINE Link].
Ozcan PY, Celik HT, Sonmez K, Celik M. Necrotizing Retinitis Secondary to Congenital Cytomegalovirus Infection Associated with Severe Combined Immunodeficiency. Case Rep Ophthalmol Med. 2016. 2016:1495639. [QxMD MEDLINE Link].
Azen SP, Scott IU, Flynn HW Jr, et al. Silicone oil in the repair of complex retinal detachments. A prospective observational multicenter study. Ophthalmology. 1998 Sep. 105(9):1587-97. [QxMD MEDLINE Link].
Elkins BS, Holland GN, Opremcak EM, et al. Ocular toxoplasmosis misdiagnosed as cytomegalovirus retinopathy in immunocompromised patients. Ophthalmology. 1994 Mar. 101(3):499-507. [QxMD MEDLINE Link].
Davis JL. Differential diagnosis of CMV retinitis. Ocul Immunol Inflamm. 1999 Dec. 7(3-4):159-66. [QxMD MEDLINE Link].
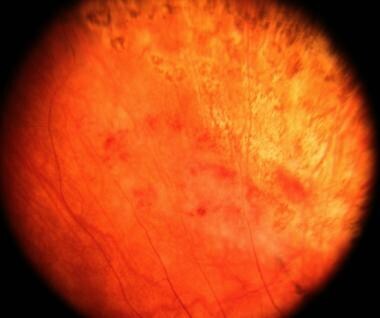
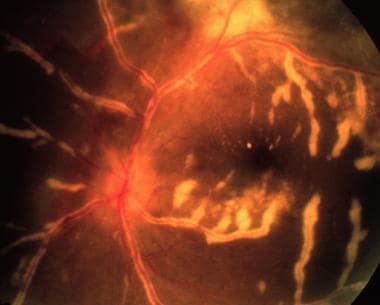
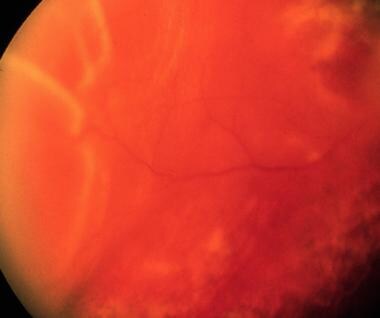
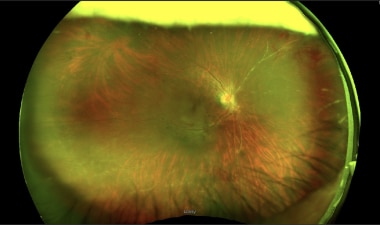 Wide-field fundus photograph illustrating numerous blood vessels within the inferior and nasal periphery that appear attenuated and without flowing blood.
Wide-field fundus photograph illustrating numerous blood vessels within the inferior and nasal periphery that appear attenuated and without flowing blood.